Abstract
Although an essential nutrient, manganese (Mn) can be toxic at high doses. There is, however, uncertainty regarding the effects of chronic low-level Mn-exposure. This review provides an overview of Mn-related brain and functional changes based on studies of a cohort of asymptomatic welders who had lower Mn-exposure than in most previous work. In welders with low-level Mn-exposure, we found: 1) Mn may accumulate in the brain in a non-linear fashion: MRI R1 (1/T1) signals significantly increased only after a critical level of exposure was reached (e.g., ≥300 welding hours in the past 90 days prior to MRI). Moreover, R1 may be a more sensitive marker to capture short-term dynamic changes in Mn accumulation than the pallidal index [T1-weighted intensity ratio of the globus pallidus vs. frontal white matter], a traditional marker for Mn accumulation; 2) Chronic Mn-exposure may lead to microstructural changes as indicated by lower diffusion tensor fractional anisotropy values in the basal ganglia (BG), especially when welding years exceeded more than 30 years; 3) Mn-related subtle motor dysfunctions can be captured sensitively by synergy metrics (indices for movement stability), whereas traditional fine motor tasks failed to detect any significant differences; and 4) Iron (Fe) also may play a role in welding-related neurotoxicity, especially at low-level Mn-exposure, evidenced by higher R2* values (an estimate for brain Fe accumulation) in the BG. Moreover, higher R2* values were associated with lower phonemic fluency performance. These findings may guide future studies and the development of occupation- and public health-related polices involving Mn-exposure.
Keywords: Welders, Manganese, R1, Pallidal Index, Fractional Anisotropy, Synergy
Effects of occupational manganese exposure on the central nervous system
Manganese (Mn) is an essential nutrient but can be neurotoxic to the central nervous system (CNS) at high doses, and has been associated with neurobehavioral disorders such as manganese-induced parkinsonism (Cersosimo and Koller, 2006; Colosimo and Guidi, 2009; Guilarte and Gonzales, 2015). Mn toxicity is of great public health importance because “hundreds of thousands of workers in the United States and millions of workers worldwide are exposed to [Mn-rich] welding aerosols on a daily basis” (Antonini et al., 2009). The neurological symptoms from extremely high level Mn-exposure consist initially of reduced response speed, irritability, intellectual deficits, mood changes, and compulsive behaviors, and progress to more prominent, irreversible neurological dysfunction upon protracted exposure (Guilarte, 2013; Hauser et al., 1996; Huang et al., 1993; Mergler and Baldwin, 1997; Pal et al., 1999). Neuronal degeneration and/or dysfunctional dopamine release also have been reported in basal ganglia (BG) areas including the globus pallidus, striatum, and substantia nigra pars reticulata (Colosimo and Guidi, 2009; Criswell et al., 2012; Guilarte, 2010; Guilarte, 2013; Guilarte et al., 2008; Khalid et al., 2011; Perl and Olanow, 2007). Recently, Racette et al. (2012) reported that Mn-exposed workers had a higher prevalence of parkinsonian features compared to unexposed workers, and the parkinsonian symptoms assessed by UPDRS (Unified Parkinson’s Disease Rating Scale)-III motor scores increased with cumulative long-term Mn-exposure (Racette et al., 2016).
Establishing reliable, quantitative in vivo biomarkers for Mn brain accumulation, particularly tissue dosage to the brain, has been challenging (Bader et al., 1999), and significant effort has been expended to discover surrogate biomarkers of Mn-related neurotoxicity. Several cellular and neurochemical studies using animal models have been conducted to understand possible mechanisms of Mn toxicity (Aschner and Dorman, 2006; Benedetto et al., 2009; Dobson et al., 2004; Erikson et al., 2006; Iavicoli et al., 2009; Jones and Miller, 2008; Levy and Nassetta, 2003; Norenberg and Rao, 2007; O’Neal and Zheng, 2015; Sidoryk-Wegrzynowicz and Aschner, 2013a, b; Takeda, 2003; Wright and Baccarelli, 2007; Yokel, 2006). It is known that influx of Mn into the brain is carrier-mediated, e.g., through divalent metal transporter-1 (DMT-1), transferrin, or ZIP8 (O’Neal and Zheng, 2015) that are located at the interface of the blood-brain-barrier (BBB). The major route for transport of Mn into the brain is via the BBB, but inhaled Mn can enter the brain via the olfactory pathway or through the blood-cerebrospinal fluid (CSF) barrier (Schmitt et al., 2011; Zoni et al., 2012). Efflux of Mn from the brain is by slow diffusion (Yokel, 2009), and the average half-life in brain has been estimated to be between 52–74 days (Crossgrove and Zheng, 2004; Newland et al., 1987), leading to potential accumulation. Excessive Mn brain accumulation following acute and/or chronic exposure to Mn, and problems with adequate Mn clearance from brain (e.g., mutations in the SLC30A10 gene), likely cause neurotoxic effects in the CNS (Leyva-Illades et al., 2014). For example, disruptions in several neurotransmitter systems, including dysfunctional dopaminergic activity, have been reported (Guilarte et al., 2008; Perl and Olanow, 2007), and disrupted glutamate and γ-aminobutyric acid (GABA) systems have been suggested (Burton et al., 2009; Sidoryk-Wegrzynowicz and Aschner, 2013a).
In humans, welders have been among the most studied occupational groups since Mn is one of the major elements in many types of welding fumes (Burgess, 1995). Prior studies of welders have documented subclinical motor and non-motor symptoms that do not meet criteria for occupational manganism (Bowler et al., 2006a; Bowler et al., 2006b; Bowler et al., 2007a; Bowler et al., 2007b; Chang et al., 2009; Cowan et al., 2009a; Cowan et al., 2009b; Ellingsen et al., 2008; Simon-Sanchez et al., 2009), with several reporting significant associations between Mn-exposure and subclinical symptoms (Chang et al., 2009; Meyer-Baron et al., 2013; Simon-Sanchez et al., 2009).
Recently, magnetic resonance imaging (MRI) markers have been used to examine Mn-related brain and functional changes. For example, Mn brain accumulation has been linked to higher MRI T1-weighted (T1W) intensity and/or T1 relaxation rate (R1: 1/T1) that was greatest in the globus pallidus (GP; Dorman et al., 2006b; Kim et al., 1999). These changes have been associated with slower motor function (Chang et al., 2009; Dion et al., 2016; Shin et al., 2007) and/or with poorer performance in working memory and executive function (Chang et al., 2009). Mn-induced volume decrease also was reported in the GP and cerebellum, and these correlated with reduced performance in fine motor and executive function tasks in full-time welders (Chang et al., 2013).
There is, however, uncertainty regarding the effects of the chronic low-level Mn-exposure that probably is most relevant to occupational and public health. This is due partly to the lack of an objective and sensitive in vivo marker of low-level Mn accumulation in brain. In the present review, we provide an overview of Mn-related brain and functional changes based on studies of a cohort of asymptomatic welders with welding exposures lower than most previous studies.
Establishment of a Pennsylvania-based welder cohort with chronic, low Mn exposure
Subjects
We recruited both our welders and controls locally from the community around the Penn State Milton S. Hershey Medical Center and nearby Harrisburg, PA, as well as from the Philadelphia, PA area (Lee et al., 2015). In contrast to many of prior studies (Chang et al., 2009; Choi et al., 2007; Long et al., 2014) that purposefully recruited subjects from high exposure, full-time professionals (e.g., boilermakers and shipyard workers) who may or may not reside locally, we recruited both full- and half-time welders only locally. A total of 80 subjects were recruited at baseline, 48 with and 32 without a history of welding exposure. Of these, 43 welders and 31 controls completed the MRI acquisition with good quality images. Welders, defined as subjects who had welded at any point in their lifetime, represented several different trade groups (e.g., boilermakers, pipefitters, and a variety of different manufacturing jobs). Out of 43 welders, 35 were active welders and 7 welders did not weld during the 90 days prior to study participation. For the 35 active welders, the duration between the last time they welded and study participation varied between ~1–5 days. For the 7 welders without welding during the 90 days prior to study participation, the duration between welding cessation and data collection varied between 5–180 months. Controls were volunteers from the same regional community with various occupations that did not have any lifetime history of welding. All subjects were male and answered negatively for past diagnosis of Parkinson’s or other neurological disorders. All subjects were ascertained to be free of any obvious neurological and movement deficits using the UPDRS-III (Goetz et al., 2008) with a threshold score of <15 (Lee et al., 2015). Subjective symptoms were evaluated by UPDRS-I and -II that assess non-motor (I) and motor (II) experiences of daily living (Goetz et al., 2008).
Assessment of the cohort
Exposure and behavioral function assessment
We estimated welding exposure using the following measures: recent hours welding, brazing, or soldering [HrsW90 = (weeks worked) * (h/week) * (fraction of time worked related directly to welding)]; the E90 (an estimate of the cumulative 90 day exposure to Mn, past 90 days); lifetime exposure [cumulative lifetime welding years (YrsW = years spent welding during the subjects’ life)]; and the ELT (an estimate of cumulative exposure to inhaled Mn over the individual’s life, lifetime) (Lee et al., 2015). In addition, whole blood metal (Fe and Mn) levels were obtained. To assess behavioral functions, UPDRS-III and Grooved Pegboard test (traditional motor and fine motor tasks), single- and multi-finger pressing tasks (for synergy metrics), and standardized neuropsychological tests were administered (Lee et al., 2017; Lewis et al., 2016b). All blood, MRI, and behavioral measurements were collected on the same day.
Estimations of brain MRI measurements: We used state-of-the-art MRI techniques on a Siemens 3 T scanner (Magnetom Trio, Siemens Medical Solutions, Erlangen, Germany) with an 8-channel head coil to acquire high-resolution T1-weighted (T1W), T2-weighted (T2W), rapid T1 mapping (to assess R1), a multigradient-echo sequence [to estimate the apparent transverse relaxation rate: R2* (1/T2*)], and diffusion tensor images (DTI). Bilateral basal ganglia (BG) structures [GP, putamen (PUT), and caudate nucleus (CN)] were selected as regions of interest (ROI) (Chang et al., 2009; Criswell et al., 2012; Dorman et al., 2006b).
Characteristics of the cohort
Our PA-based welders demonstrated exposure levels that were lower than most previous studies: As seen in Table 1, the mean blood Mn level was 10.7 ± 3.2 ng/mL, a value similar to that reported from a large European study of welders (i.e., 10.3 ng/mL; Pesch et al., 2012), but considerably lower compared to other studies [e.g., blood Mn>14.2 ng/mL (Chang et al., 2009; Choi et al., 2007; Criswell et al., 2012; Ellingsen et al., 2015). Our welders reported an E90 of 2.4 ± 2.0 mg-days/m3, translating to ca. 0.08 mg/m3 for an eight-hr time weighted average (TW). Our welders also had an average of ~250 ± 200 (SD) HrsW90 in the 90-day period prior to the study visit, approximately equivalent to what a half-time welder completely engaged in welding would report. In addition, the MRI pallidal index (PI; a traditional marker for brain Mn accumulation) in our welders (mean PI =109.5) was lower compared to several other studies [PI>112; (Chang et al., 2009; Choi et al., 2007; Criswell et al., 2012)]. Together, all Mn-related exposure measurements (blood Mn, HrsW90, E90, and PI values) indicated that the welders in this PA-based cohort generally had relatively low Mn exposure.
Table 1.
Summary statistics for demographics (I), exposure metrics, and blood metals (II) in welders and controls.
| Controls (N=32) Mean ± SD |
Welders (N=48) Mean ± SD |
Raw p-values |
|
|---|---|---|---|
| I. Demographics | |||
| Age (years) | 43.4 ± 11.2 | 48.0 ± 10.8 | 0.075 |
| Education (years) | 16.2 ± 2.4 | 12.8 ± 1.7 | <0.001 |
| ALT (IU/L) | 37.7 ± 16.5 | 39.8 ± 16.7 | 0.684 |
| BMI (kg/m2) | 26.0 ± 3.3 | 29.2 ± 5.3 | 0.004 |
| Hemoglobin | 14.8 ± 0.8 | 15.2 ± 1.0 | 0.102 |
| Smokers (%) | 3.2% | 15.2% | 0.091 |
| Cigarettes/day (no.) | 13.0 ± 12.0 | 20.2 ± 13.5 | 0.303 |
| UPDRS-I | 1.0 ± 1.9 | 1.7 ± 2.0 | 0.125 |
| UPDRS-II | 3.9 ± 3.1 | 4.6 ± 3.5 | 0.383 |
| UPDRS-III | 1.5 ± 2.1 | 1.9 ± 2.4 | 0.461 |
|
| |||
| II. Exposure metrics and Blood Metal levels | |||
| HrsW (hours) | 0 ± 0 (0) | 248 ± 195 | <0.001 |
| E90 mg-days/m3 | 0.0027 ± 0 | 2.4 ± 2.0 | <0.001 |
| YrsW (years) | 0 ± 0 (0) | 25.8 ± 10.6 | <0.001 |
| ELT mg-years/m3 | 0.0013 ± 0.0004 | 1.2± 0.8 | <0.001 |
| Mn (ng/mL) | 8.8 ± 2.5 | 10.7 ± 3.2 | <0.001 |
| Fe (μg/mL) | 498 ± 75 | 551 ± 56 | <0.001 |
Data represent the mean ± SD. Demographic (I) and blood metal (II) measures were compared between controls and welders using analysis of variance (ANOVA) for demographic and blood metal data. Abbreviations: ALT-alanine aminotransferase; BMI-body mass index; UPDRS-Unified Parkinson’s Disease Rating Scale-motor scores.
R1 (1/T1) signals capture non-linear, short-term Mn accumulation
Mn brain accumulation has been linked to higher MRI T1W intensity (Dorman et al., 2006b; Kim et al., 1999) because Mn has paramagnetic characteristics that can shorten the MRI longitudinal relaxation time (T1) and increase T1W intensity. Moreover, T1 signals are relatively selective for estimating Mn brain accumulation because Mn has the highest T1 relaxivity (6.67/mM/sec) of all metals, higher even than the contrast agent gadolinium (5.0/mM/sec). Previous studies reported significant linear correlations between Mn content and T1 relaxation rates (R1; 1/T1) in metal-doped rat brain homogenates starting from a Mn concentration of zero (r=0.98; Gallez et al., 2001) and between the R1 signal and Mn concentration in the basal ganglia of rats (rs≥ 0.84) (Gallez et al., 2001; Kim et al., 1999). Other paramagnetic metals in welding fumes have lower T1 relaxivity (e.g., Fe2+=0.01 and Cu2+=0.5) (Gallez et al., 2001; Yilmaz et al., 1999). Traditionally, T1W intensity imaging has been used to assess Mn accumulation in brain tissue (Baker et al., 2015; Pal et al., 1999) by means of the PI, the ratio of T1W intensity in the GP [where Mn appears to accumulate most significantly (Dorman et al., 2006b)] compared to intensity in the frontal white matter (FWM). The PI, however, may not be sensitive to Mn exposure especially when the exposure level is low because Mn also can enter the FWM, as well as regions other than the GP (Choi et al., 2007; Dorman et al., 2006b; Guilarte et al., 2006; Lee et al., 2015). Theoretically, this would make the PI less accurate than R1 (1/T1) in assessing the concentration of Mn in the brain (Choi et al., 2007; Dorman et al., 2006b; Lee et al., 2015).
The study of PA-based welders with low Mn-exposure utilized the R1 signal to capture sensitively low-level Mn brain accumulation. The results showed that there were no significant group differences in PI or R1 values in any ROIs (Figure 1a–b), different from the majority of the welding-related literature where higher PI or R1 values in the GP were reported (Choi et al., 2007; Criswell et al., 2012). Interestingly, the R1 signal showed a non-linear relationship with HrsW90 (welding hours, past 90 days), such that R1 did not start to increase until HrsW90 exceeded ~300 hours (Figure 1c). Conversely, the traditional PI failed to show any association with either short- or long-term exposure metrics. Subsequent subgroup analyses revealed that welders with HrsW90 <300 hours were indistinguishable from controls (in Mn blood metal and R1 values), whereas R1 values in the BG were elevated for welders with HrsW90 >300 hours compared to the lower level exposed welders with HrsW90 <300 (Lee et al., 2015). These data suggest that there may be a threshold above which homeostatic Mn regulation may be broken and brain Mn levels may start increasing. This non-linear pattern of Mn brain concentration also was predicted by physiologically-based pharmacokinetic (PBPK) models (Nong et al., 2009; Nong et al., 2008; Schroeter et al., 2010) that originally were developed based on animal (rats and nonhuman primates) data (Nong et al., 2009; Nong et al., 2008) and verified with experimental animal studies (Dorman et al., 2004; Dorman et al., 2006a; Tapin et al., 2006). When the PBPK model was scaled to human data, the model also predicted that the concentration of Mn in the GP would be unchanged when air Mn levels were below 0.1 mg/m3 for 8 h/day over 90 days (Schroeter et al., 2010), supportive of non-linear Mn accumulation in human brains. The application of the PBPK model to humans was validated based on multiple empirical human studies by using air Mn level as the input and blood Mn levels as the predicted outcome variables (Ramoju et al., 2017), although validation using human pathological data is lacking. It is not straightforward, however, to estimate how 300 HrsW90 translates to air concentration and further studies are needed to elucidate this. Nevertheless, the non-linear Mn accumulation pattern is relevant to occupational and public health because it may contribute to determining tolerable and safe threshold limit values of Mn exposure.
Figure 1.
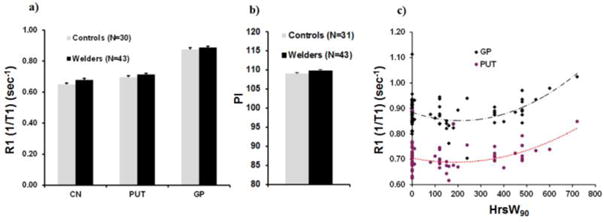
a) MRI longitudinal relaxation rates (R1) in basal ganglia regions of interest [caudate nucleus (CN), putamen (PUT), globus pallidus (GP)] for welders and controls; b) PI (pallidal index) for welders and controls. Data represent the mean ± standard errors (SEM).; c) R1 in the globus pallidus (GP) and putamen (PUT) as a function of welding hours (HrsW90) collapsed across welders and controls [modified from Lee et al. (2015)].
A one-year follow-up analysis was conducted on this cohort that demonstrated changes in R1 values in all ROIs correlated with changes in HrsW90 (the short-term welding exposure metric), whereas blood Mn levels or the PI value failed to show any associations with changes in HrsW90 (Lewis et al., 2016a). This result is consistent with a previous finding that the GP T1 relaxation time (1/R1) in Mn-exposed monkeys was lowest after 120 days of Mn-exposure, but returned to control values two months after cessation of Mn-exposure, suggesting that R1 may sensitively capture the temporal dynamics of Mn brain accumulation and clearance (Han et al., 2008). Collectively, the data from our analyses of welders exposed to low-level of Mn suggest that R1 may serve as a more sensitive marker to gauge Mn accumulation (especially at low-level exposures) than PI, by sensitively capturing the non-linear, short-term dynamics of Mn brain accumulation.
Microstructural changes related to chronic Mn exposure
Although previous studies were able to establish some biomarkers for Mn brain accumulation, the relationship between Mn brain accumulation and neuronal pathology, especially at subclinical exposure levels, still is unclear. Diffusion weighted imaging (DWI; Schaefer et al., 2000) and DTI (Basser and Pierpaoli, 1996; Le Bihan et al., 2001) are MRI sequences that can assess tissue microstructural properties by measuring diffusion, the random translational motion of water molecules (Basser and Pierpaoli, 1996). There has been a growing effort to link the MRI modality to Mn-related microstructural changes, but the findings have been inconsistent. For example, there has been one report of greater (7%) mean diffusivity (MD), an overall diffusion magnitude measure, in the GP of Mn-overloaded methcathinone abusers (Stepens et al., 2010). Conversely, other studies have reported lower GP apparent diffusion coefficient (ADC) values of DWI, an estimate of the magnitude of diffusion for one specific gradient direction (comparable to DTI MD) in asymptomatic welders (Criswell et al., 2012) or in a subject with Mn toxicity (McKinney et al., 2004). No studies, however, have demonstrated an association between the diffusion imaging findings and degree of welding exposure.
It recently has been demonstrated that DTI fractional anisotropy (FA), a diffusion anisotropy measure that traditionally has been used to measure white matter properties and the connectivity between brain gray matter regions, may capture microstructural integrity in subcortical gray matter structures (Chan et al., 2007; Hashimoto et al., 2009; Yoshikawa et al., 2004). For example, schizophrenia patients had significantly lower FA values in the GP compared to controls (Hashimoto et al., 2009), suggestive of microstructural changes.
Thus, we investigated whether DTI measures (especially FA) may detect microstructural changes in the BG of asymptomatic welders with chronic, low-level exposure. Results showed a non-significant MD increase (1.9%) (Figure 2a), but a significant decrease (4.4%) in FA values in the GP (Figure 2b) for welders compared to controls. Moreover, GP FA values in welders showed non-linear relationships with YrsW (welding years; a long-term exposure metric), blood Mn levels, and PI values such that GP FA values decreased after a critical level of YrsW (e.g., >30 years) or blood Mn (e.g., >13 ng/mL) was reached, whereas they decreased with increasing PI values and then reached a plateau at the highest PI values (see Figure 2c–e for data patterns and statistics). In addition, a stepwise regression analysis that collapsed welders and controls demonstrated that the YrsW and PI were significant predictors of GP FA values. Conversely, GP FA values did not show any relationship with short-term exposure metrics (HrsW and E90), blood Cu and Fe levels, or R2* values (an estimate for brain Fe accumulation).
Figure 2.
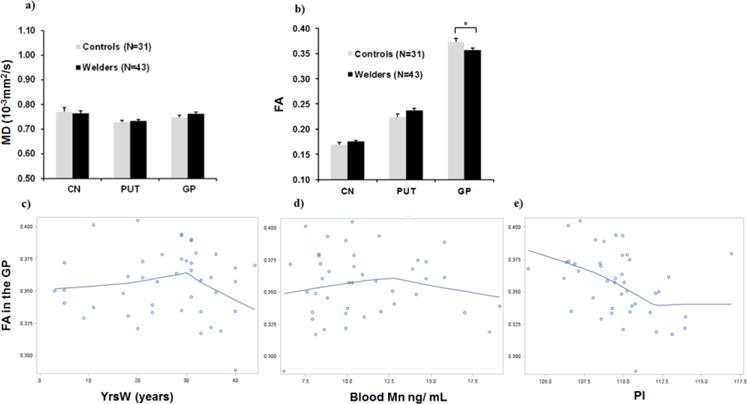
MRI Diffusion tensor imaging (DTI) in basal ganglia regions of interest [caudate nucleus (CN), putamen (PUT), globus pallidus (GP)] a) Mean diffusivity (MD); b) Fractional anisotropy (FA). Data represent the mean ± standard errors (SEM). The FA difference in the GP between welders and controls is significant (raw p= 0.004) using repeated measures analyses of variance based on mixed models by treating group (controls versus welders) as a between-subjects factor and ROI as a within-subjects factor and adjusting for age, BMI (body mass index), and R2* values. This difference remained significant after correction for multiple comparisons (3 ROIs to be compared) using the Stepdown Bonferroni method (Holm, 1979) to control the familywise error rate (FWER) at p= 0.05 (denoted by *). LOWESS plots depicting the relationship of FA in the GP with c) the exposure measurement of lifetime welding years (YrsW; a second-order polynomial relationship, ß=−0.0002, R2=0.13, p=0.028); d) whole blood Mn level (a second-order polynomial relationship, ß=−0.0008, R2=0.11, p=0.036); and e) the pallidal index (PI; a significant third-order polynomial relationship, ß= 0.0002, R2= 0.30, p=0.009) within welders. [from Lee et al. (2016a)].
These results suggest that; first, the observed GP FA group difference may be due, at least partly, to chronic welding exposure in welders; and second, the significant non-linear associations between GP FA values and Mn-exposure measurements (blood Mn and PI), along with the absence of any associations between GP FA and Fe exposure measurements (blood Fe and R2*), suggest that the GP FA group difference likely is related to Mn exposure, although the influence of other unmeasured co-exposures cannot be ruled out. The lack of group differences in R1 and PI measures, however, indicates that the GP FA group difference may not be due to current Mn brain accumulation per se, especially when the exposure level is low. Note that both R1 and PI signals decay with time (Han et al., 2008; Kim, 2004; Nelson et al., 1993) and thus these MRI markers may reflect short-term rather than long-term cumulative Mn exposure more sensitively. The lack of the R1 and PI group differences also is in contrast to the majority of other welding-related studies and likely indicates that our welders have low-level exposures and the GP FA difference would be exacerbated with increasing Mn exposures.
Collectively, these results suggest that lower GP FA values may capture microstructural changes associated with long-term Mn-exposure. This finding is important because it implies that FA may serve as a useful early marker for microstructural changes that may gauge Mn neurotoxicity in asymptomatic welders. Furthermore, even very low levels of Mn-exposure may lead to microstructural changes if welding is chronic (Lee et al., 2016a).
Synergy metrics may capture subtle motor function decline related to Mn exposure
The overall weight of the literature supports the hypothesis that there is compromised function after Mn exposure (even in asymptomatic welders) (Bowler et al., 2006a; Bowler et al., 2006b; Bowler et al., 2007a; Bowler et al., 2007b; Chang et al., 2009; Cowan et al., 2009a; Cowan et al., 2009b; Ellingsen et al., 2008; Simon-Sanchez et al., 2009). For example, a meta-analysis of eight studies examining 579 Mn-exposed and 433 unexposed workers reported slower motor performance and declines in attention, short-term memory, and executive function (Meyer-Baron et al., 2013). It is, however, unclear if there are functional deficits after lower level Mn exposure like our cohort. Because traditional standard tests were developed to detect differences for patient populations, there is a need to develop more sensitive tests that can detect subtle differences that may occur in welders with low-level Mn-exposure.
Movement stability is crucial for successful everyday motor performance because all natural human movements are performed in a poorly predictable environment and involve varying internal states. For example, when a welder is involved in his/her labor activity, the non-dominant hand typically ensures stability of the object of welding while the dominant hand controls the torch. Both sub-actions likely are based on varying contributions of elements such as joints, digits, and muscles, rather than on fixed, stereotypical patterns of their involvement (Schöner, 1995). Loss of stability of motor performance may cause spills, falls, dropped objects, illegible writing, and stuttering, but it also may be subtle and not observable with the naked eye. Our hypothesis was that this may occur in subclinical, asymptomatic welders. Indeed, previous studies reported that Mn-exposed subjects experienced issues with balance and tasks requiring maintaining stability (Bouchard et al., 2007; Bowler et al., 2007b; Ellingsen et al., 2008; Mergler et al., 1994; Zoni et al., 2007), suggesting that motor tasks that can quantify motor stability may sensitively capture Mn-related early motor function decline.
Until recently, there were no methods that could quantify directly movement stability across the repertoire of everyday actions that involve multi-digit object manipulation, multi-joint reaching, and/or whole-body actions. Such methods have been recently developed based on the principle of abundance (Gelfand and Latash, 1998; Latash, 2012) and the uncontrolled manifold hypothesis (Scholz and Schoner, 1999). By utilizing these methods, a motor synergy index (an estimate for motor stability) was developed to explain disordered movements such as those observed in PD (Latash, 2008; Latash and Huang, 2015; Park et al., 2010). Note that overt Mn neurotoxicity is known to have similarities to PD (Bowler et al., 2007a; Cersosimo and Koller, 2006) due to common features of basal ganglia dysfunction (Criswell et al., 2012; Dorman et al., 2006a; Lee et al., 2015; Lee et al., 2016a), although Mn-induced parkinsonism can be differentiated from PD by, for example, lack of response to levodopa, the most common PD drug (Ostiguy et al., 2006).
Our team demonstrated recently that in PD and parkinsonism, the altered BG function results in decreased synergy indices (measure of movement stability) and anticipatory synergy adjustments (ASA, measurement of agility; ability to modify steady states in preparation to a quick action) (Jo et al., 2015a; Jo et al., 2015b; Park et al., 2013; Park et al., 2012). This suggests impairment both in creating task-specific motor stability (Schöner, 1995) and adjusting it by preparing a quick action in PD (Olafsdottir et al., 2005). Most importantly, we found lower synergy index values in early-stage PD patients, even in the asymptomatic side (Park et al., 2012), suggesting that reduced motor stability may precede the actual clinically detectable balance problems. This finding hinted the possibility that the synergy index may serve as a useful tool to sensitively capture even subtle premorbid deficits in movement stability of our welder cohort.
In the current study of our PA-based welders with low-level Mn-exposure, we implemented single- and multi-finger pressing tasks to acquire motor synergy index in order to capture alterations in movement stability as an early behavioral marker of Mn-exposure in our welder cohort (Lewis et al., 2016b). In a subset of the current PA-based cohort (20 right-handed welders and 13 matched controls), subjects were asked to use four fingers of the right or left hand, with each finger pressing on its own button equipped with a force sensor. The subjects were tested for ~20 s and asked to match total force with the template force shown on the screen (pressing during a steady state). Subjects then were asked to produce a quick force pulse at a target force level. In addition, conventional motor tasks (the UPDRS-III to gauge gross motor functions of tremor, rigidity, and balance; and the Grooved Pegboard test to measure fine motor dexterity) were administered. During the Grooved Pegboard test, subjects were asked to rotate and insert 25 pegs, one at a time, to fit in holes as quickly as possible. The behavioral performance on these tests then was related to welding-related MRI makers [R1, PI, R2*, and DTI; estimates of welding-related metal (Mn and Fe) accumulation and microstructural changes, respectively].
The data indicated that the synergy index during steady state (an index of stability) was significantly lower in welders, particularly in the left hand, compared to controls, whereas the anticipatory synergy adjustments (indices of agility) were not significantly different between welders and controls. Welder and controls also were similar regarding UPDRS-III or Grooved Pegboard test scores (Lewis et al., 2016b). These data revealed that welders display selective deficits in hand movement stability compared to controls, even though conventional motor tasks failed to show any significant differences. Collectively, these findings suggest that synergy metrics may serve as a very sensitive marker to detect motor function decline in welders. Most interestingly, lower synergy index values in the left hand of welders were associated significantly with lower FA values in the GP (Figure 3), an MRI marker reflecting microstructural changes associated with long-term Mn exposure. The synergy indices were not, however, associated with PI and R1 values, markers for Mn accumulation per se. The finding of a strong and significant association between the synergy index and GP FA values, the region known to have the highest susceptibility for Mn accumulation, suggests that the decline in motor stability can be measured sensitively, and is related to Mn-induced microstructural changes in the GP (Lee et al., 2016a; Lewis et al., 2016b). These data lead to a better understanding of the link between Mn-related microstructural changes and functional consequences, but need to be replicated in a larger cohort. Nevertheless, the results suggest that the multi-digit synergy index can capture subclinical motor changes in asymptomatic welders, and may serve as a sensitive marker for basal ganglia dysfunction in Mn-exposed welders.
Figure 3.
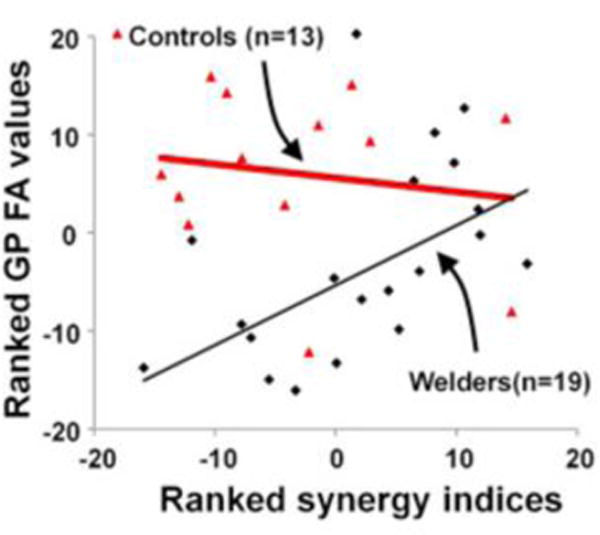
Scatter plot comparing ranked fractional anisotropy (FA) values in the globus pallidus (GP) (y-axis) with ranked synergy index (x-axis). For welders, there was a significant Spearman’s correlation between left GP FA and synergy index values after adjustment for age: R=0.731, p=0.0006 [from Lewis et al. (2016b)].
Neurotoxic effects of Fe at low-level Mn exposure
Welding fumes contain several metals including copper (Cu), Mn, and Fe that may interact to influence welding-related neurotoxicity. Although airborne Fe concentrations are about ten-fold greater than those of Mn (Ellingsen et al., 2006; Flynn and Susi, 2009) and whole blood Fe levels are much higher than those of Mn (Lu et al., 2005), past welding-related studies have focused on Mn accumulation in brain (Choi et al., 2007; Lee et al., 2015), with few studies examining brain deposition of Fe in welders or mine workers (Criswell et al., 2015; Long et al., 2014).
Similar to Mn, Fe is an essential element that can be neurotoxic at higher doses (Sipe et al., 2002). Fe uptake into brain is affected by several factors including particle size and the presence of other metals such as Mn and Cu. For example, Fe and Mn may compete for common transporters such as transferrin (Erikson et al., 2004), and Cu overload may decrease Fe brain uptake (Crowe and Morgan, 1996). Thus, increased levels of welding-related metals other than Fe (e.g., Mn, Cu, etc.) may influence its uptake into the brain and vice versa. For MRI, Fe has paramagnetic characteristics and shortens the apparent transverse relaxation time (T2*; Haacke et al., 2005). Thus, one of the commonly used methods to assess Fe brain accumulation is measurement of the T2* relaxation rate (R2*; 1/T2*). Indeed, several neuroimaging studies (Gelman et al., 1999; Peran et al., 2010) established associations between R2* values in selected brain areas (including the basal ganglia) and brain Fe content estimated from the postmortem data of Hallgren and Sourander (Gerlach et al., 1994; Hallgren and Sourander, 1958). R2* values, however, may be affected by the presence of other paramagnetic metals (e.g., Cu and Mn) that are common in welding (Vymazal et al., 1993). For example, increased R1 and R2 values occurred when there was elevated Mn exposure without additional Fe (Fitsanakis et al., 2010).
Studies examining Fe brain accumulation in welding or Mn-exposure are sparse and inconsistent. Long et al. (2014) assessed Fe concentration via T2* and, when compared to controls, found full-time welders had lower T2* values in the frontal cortex, but no difference in selected subcortical regions of interest (ROIs; e.g., GP, thalamus, and hippocampus). A recent study in deceased mine workers reported no difference in Fe tissue concentrations in the BG compared to controls (Criswell et al., 2015), although increased Fe tissue concentration was reported in the BG of Mn-exposed monkeys (Olanow et al., 1996). Studies examining possible associations between neurobehavioral performances and welding-related Fe accumulation are not available. It is also important to note that R2* consists of both susceptibility and the transverse relaxation rate that may be influenced by local cellular structural properties (Duyn and Schenck, 2017; Haacke et al., 2005). Recently, quantitative susceptibility mapping (QSM) has been demonstrated to capture only susceptibility, thus making it a better tissue Fe marker (Haacke et al., 2005; Wang and Liu, 2014). Future studies integrating QSM are warranted to determine whether Fe deposition occurs in welders.
Increased R2* in the caudate nucleus in the absence of increased R1 or PI values
Our study of PA-based welders with low-level Mn-exposure utilized R2* as a surrogate marker for Fe brain accumulation, and found higher whole blood Fe levels and higher R2* values compared to controls. The higher R2* values were selective for the CN (Figure 4a), not other regions of the BG. They also were correlated positively with blood Fe levels after adjustment for confounders (including R1 values and blood Cu and Mn levels), although there were no group differences in R1 values in any ROI. Together, these results suggest that increased R2* may be associated with increased exposure specifically to Fe (Lee et al., 2016b). Whereas past welding-related studies focused on Mn accumulation in the BG (predominantly in the GP), our PA-based study of welders with low-level Mn-exposures was the first human study to delineate increased R2* values in the BG (predominantly in the CN). It is unclear why higher R2* values were found in the CN and not in the PUT and GP. Nevertheless, because Fe has been implied in a number of neurotoxic and/or neurodegenerative process (Jellinger et al., 1990; Snyder and Connor, 2009; Ward et al., 2014), it is possible that higher Fe accumulation in the CN may underlie cognitive declines reported in welding-related neurotoxicity.
Figure 4.
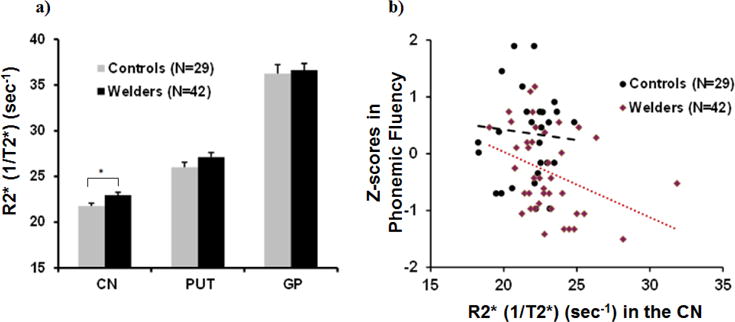
a) MRI apparent transverse relaxation rates (R2*) in basal ganglia regions of interest [caudate nucleus (CN), putamen (PUT), globus pallidus (GP)] for welders and controls. The R2* difference in the CN between welders and controls is significant (raw p= 0.018) using repeated measures analyses of variance based on mixed models with adjustment for age, BMI, and R1 values. Data represent the mean ± standard errors (SEM). This difference remained significant after correction for multiple comparisons using the Stepdown Bonferroni method (Holm, 1979) (denoted by *); b) Scatter plot comparing z-scores on the Phonemic Fluency subtest (y-axis) with R2* values in the CN (x-axis): For welders, there was a significant Pearson’s correlation between R2* in the CN and Phonemic Fluency scores after adjustment for age: R= R=−0.468, p=0.007) [modified from (Lee et al., 2017; Lee et al., 2016b)].
Increased R2* in the caudate nucleus was associated with lower phonemic fluency performance
Our cohort of welders scored lower in all individual tests of comprehensive neuropsychological tests including the cognitive domains of processing/psychomotor speed, executive function, language, learning/memory, visuospatial processing, and attention/working memory (Lee et al., 2017). The most pronounced deficits were observed in the domains of processing/psychomotor speed and executive function, but only the Phonemic Fluency test (where subjects generate words beginning with a particular letter) remained significant after correction for multiple comparisons. These results suggest that mental processes such as updating speed, strategic search, and clustering (or strategic response organization) that are involved in Phonemic Fluency processing may be among the earliest cognitive changes occurring in asymptomatic welders with low Mn exposure. In addition, test scores on the Phonemic Fluency test were reliably and inversely correlated with R2* values in the CN in welders (Figure 4b), but not with PI and R1 values in any ROI. Moreover, R2* values in the CN were a significant predictor for Phonemic Fluency performance after controlling for a number of confounders.
Along with the finding of higher CN R2* values for welders, these neuropsychological results suggest that some welding-related neurobehavioral changes may be due to, at least in part, by Fe rather than Mn brain accumulation, particularly in the CN. This may be especially relevant when the exposure level is relatively low and Mn neurotoxic effects are not yet discernible. In addition to the well-documented involvement of the frontal cortex (Baldo et al., 2006) in the Phonemic Fluency test, there also is an influence of the CN (Grogan et al., 2009). Yet, the dynamics of Fe accumulation and its association with neurobehavioral performance may change if Mn exposure becomes higher. A study of 137 welders exposed to a Mn air concentration of 0.21 mg/m3 (range: 0.001–3.2) showed higher serum Mn, but no increase (or even lower) serum Fe and ferritin compared to controls (Ellingsen et al., 2015). Previous animal studies also showed increased Mn but decreased Fe brain concentrations when rats were fed with both Mn- and Fe-supplemented food (Fitsanakis et al., 2010; Zhang et al., 2009). These studies suggest that Fe uptake to the brain could be attenuated by the presence of higher levels of Mn. Nevertheless, the findings of higher R2* values and its association with cognitive decline underscore the importance of accounting for Fe effects in welders with low-level Mn exposure that may help guide future studies and the development of occupation- and public health-related polices in relation to Mn exposure.
Concluding remarks and future directions
There have been significant efforts to seek surrogate biomarkers of Mn-related neurotoxicity. Based on data gleaned from experiments with an asymptomatic welder cohort with relatively low-level Mn-exposure, several conclusions have been drawn: 1) Mn may start accumulating significantly in the brain once a critical level of exposure is reached (e.g., recent welding hours >300; assessed via the R1 measurement); 2) long-term Mn exposure (e.g., lifetime welding years >30) may lead to microstructural changes (assessed via FA changes) even at low-level exposures; 3) synergy metrics can be a tool to capture early motor function decline; and 4) it is important to investigate the effects of welding-related metals other than Mn in situations of low-level Mn exposure where Mn-related neurotoxic effects are not obvious. These findings may guide future studies and the development of occupation- and public health-related tools and polices involving Mn exposure. It is important to replicate the current results in a larger sample size and a different cohort to generalize the findings. It also would be meaningful to test whether the observed brain and functional changes at low-level Mn exposure are reversible, and/or contribute to the susceptibility to future development of neurodegenerative disorders such as Parkinson’s disease or related disorders.
Highlights.
Manganese may accumulate in the brain in a non-linear fashion: MRI R1 (1/T1) signals significantly increased only after a critical level of exposure was reached (e.g., ≥300 welding hours in the past 90 days prior to MRI).
Chronic Mn-exposure may lead to microstructural changes as indicated by lower diffusion tensor fractional anisotropy values in the basal ganglia (BG), especially when welding years exceeded more than 30 years.
Mn-related subtle motor dysfunctions can be captured sensitively by synergy metrics (indices for movement stability), whereas traditional fine motor tasks failed to detect any significant differences.
Iron may also play a role in welding-related neurotoxicity, especially at low-level Mn-exposure.
Acknowledgments
We would like to thank all the volunteers who participated in this research. In addition we are indebted to the many individuals who helped insure its success, including: Melissa Santos and Susan Kocher for subject coordination, recruitment, blood sample handling, and data entry; Pam Susi and Pete Stafford of CPWR; Mark Garrett, John Clark, and Joe Jacoby of the international Brotherhood of Boilermakers; Fred Cosenza and all members of the Safety Committee for the Philadelphia Building and Construction Trades Council; Ed McGehean of the Steamfitters Local Union 420; Jim Stewart of the Operating Engineers; Sean Gerie of the Brotherhood of Maintenance of Way Employees Division Teamsters Rail Conference; and Terry Peck of Local 520 Plumbers, Pipefitters and HVAC.
Funding
This work was supported by R01 ES019672 and R01 NS082151 from the National Institutes of Health, the Hershey Medical Center General Clinical Research Center (National Center for Research Resources, Grant UL1 RR033184 that is now at the National Center for Advancing Translational Sciences, Grant UL1 TR000127), and the PA Department of Health Tobacco CURE Funds.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Contributions:
| Author Name | Contributions | |
| Eun-Young Lee | elee@pennstatehealth.psu.edu | 1A, 2A, 2B, 2C, 3A, 3B |
| Michael R. Flynn | mflynn@email.unc.edu | 1A, 1B, 1C, 2C, 3B |
| Mechelle M. Lewis | mlewis5@pennstatehealth.psu.edu | 1A, 1B, 1C, 2C, 3A, 3B |
| Richard B. Mailman | rmailman@psu.edu | 1A, 2C, 3B |
| Xuemei Huang | xuemei@psu.edu | 1A, 1B, 1C, 2C, 3A, 3B |
| 1. Research project: | A. Conception | B. Organization | C. Execution |
| 2. Statistical Analysis: | A. Design | B. Execution | C. Review & critique |
| 3. Manuscript: | A. Writing of first draft | B. Review & critique |
Conflict of interest disclosures:
The authors do not have any financial conflicts of interest to disclose.
References
- Antonini JM, Sriram K, Benkovic SA, Roberts JR, Stone S, Chen BT, Schwegler-Berry D, Jefferson AM, Billig BK, Felton CM, Hammer MA, Ma F, Frazer DG, O’Callaghan JP, Miller DB. Mild steel welding fume causes manganese accumulation and subtle neuroinflammatory changes but not overt neuronal damage in discrete brain regions of rats after short-term inhalation exposure. Neurotoxicology. 2009;30:915–925. doi: 10.1016/j.neuro.2009.09.006. [DOI] [PubMed] [Google Scholar]
- Aschner M, Dorman DC. Manganese: pharmacokinetics and molecular mechanisms of brain uptake. Toxicol Rev. 2006;25:147–154. doi: 10.2165/00139709-200625030-00002. [DOI] [PubMed] [Google Scholar]
- Bader M, Dietz MC, Ihrig A, Triebig G. Biomonitoring of manganese in blood, urine and axillary hair following low-dose exposure during the manufacture of dry cell batteries. Int Arch Occup Environ Health. 1999;72:521–527. doi: 10.1007/s004200050410. [DOI] [PubMed] [Google Scholar]
- Baker MG, Simpson CD, Sheppard L, Stover B, Morton J, Cocker J, Seixas N. Variance components of short-term biomarkers of manganese exposure in an inception cohort of welding trainees. J Trace Elem Med Biol. 2015;29:123–129. doi: 10.1016/j.jtemb.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldo JV, Schwartz S, Wilkins D, Dronkers NF. Role of frontal versus temporal cortex in verbal fluency as revealed by voxel-based lesion symptom mapping. Journal of the International Neuropsychological Society: JINS. 2006;12:896–900. doi: 10.1017/S1355617706061078. [DOI] [PubMed] [Google Scholar]
- Basser PJ, Pierpaoli C. Microstructural and physiological features of tissues elucidated by quantitative-diffusion-tensor MRI. J Magn Reson B. 1996;111:209–219. doi: 10.1006/jmrb.1996.0086. [DOI] [PubMed] [Google Scholar]
- Benedetto A, Au C, Aschner M. Manganese-induced dopaminergic neurodegeneration: insights into mechanisms and genetics shared with Parkinson’s disease. Chem Rev. 2009;109:4862–4884. doi: 10.1021/cr800536y. [DOI] [PubMed] [Google Scholar]
- Bouchard M, Mergler D, Baldwin M, Panisset M, Bowler R, Roels HA. Neurobehavioral functioning after cessation of manganese exposure: a follow-up after 14 years. Am J Ind Med. 2007;50:831–840. doi: 10.1002/ajim.20407. [DOI] [PubMed] [Google Scholar]
- Bowler RM, Gysens S, Diamond E, Nakagawa S, Drezgic M, Roels HA. Manganese exposure: neuropsychological and neurological symptoms and effects in welders. Neurotoxicology. 2006a;27:315–326. doi: 10.1016/j.neuro.2005.10.007. [DOI] [PubMed] [Google Scholar]
- Bowler RM, Koller W, Schulz PE. Parkinsonism due to manganism in a welder: neurological and neuropsychological sequelae. Neurotoxicology. 2006b;27:327–332. doi: 10.1016/j.neuro.2005.10.011. [DOI] [PubMed] [Google Scholar]
- Bowler RM, Nakagawa S, Drezgic M, Roels HA, Park RM, Diamond E, Mergler D, Bouchard M, Bowler RP, Koller W. Sequelae of fume exposure in confined space welding: a neurological and neuropsychological case series. Neurotoxicology. 2007a;28:298–311. doi: 10.1016/j.neuro.2006.11.001. [DOI] [PubMed] [Google Scholar]
- Bowler RM, Roels HA, Nakagawa S, Drezgic M, Diamond E, Park R, Koller W, Bowler RP, Mergler D, Bouchard M, Smith D, Gwiazda R, Doty RL. Dose-effect relationships between manganese exposure and neurological, neuropsychological and pulmonary function in confined space bridge welders. Occup Environ Med. 2007b;64:167–177. doi: 10.1136/oem.2006.028761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess WA. Recognition of Health Hazards in Industry: A Review of Materials and Processes, Second Edition. Journal of Chemical Education. 1995;72:A109. [Google Scholar]
- Burton NC, Schneider JS, Syversen T, Guilarte TR. Effects of chronic manganese exposure on glutamatergic and GABAergic neurotransmitter markers in the non-human primate brain. Toxicological sciences. 2009:kfp124. doi: 10.1093/toxsci/kfp124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cersosimo MG, Koller WC. The diagnosis of manganese-induced parkinsonism. Neurotoxicology. 2006;27:340–346. doi: 10.1016/j.neuro.2005.10.006. [DOI] [PubMed] [Google Scholar]
- Chan LL, Rumpel H, Yap K, Lee E, Loo HV, Ho GL, Fook-Chong S, Yuen Y, Tan EK. Case control study of diffusion tensor imaging in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2007;78:1383–1386. doi: 10.1136/jnnp.2007.121525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang Y, Jin SU, Kim Y, Shin KM, Lee HJ, Kim SH, Ahn JH, Park SJ, Jeong KS, Weon YC, Lee H. Decreased brain volumes in manganese-exposed welders. Neurotoxicology. 2013;37:182–189. doi: 10.1016/j.neuro.2013.05.003. [DOI] [PubMed] [Google Scholar]
- Chang Y, Kim Y, Woo ST, Song HJ, Kim SH, Lee H, Kwon YJ, Ahn JH, Park SJ, Chung IS, Jeong KS. High signal intensity on magnetic resonance imaging is a better predictor of neurobehavioral performances than blood manganese in asymptomatic welders. Neurotoxicology. 2009;30:555–563. doi: 10.1016/j.neuro.2009.04.002. [DOI] [PubMed] [Google Scholar]
- Choi DS, Kim EA, Cheong HK, Khang HS, Ryoo JW, Cho JM, Sakong J, Park I. Evaluation of MR signal index for the assessment of occupational manganese exposure of welders by measurement of local proton T1 relaxation time. Neurotoxicology. 2007;28:284–289. doi: 10.1016/j.neuro.2006.05.020. [DOI] [PubMed] [Google Scholar]
- Colosimo C, Guidi M. Parkinsonism due to ephedrone neurotoxicity: a case report. European journal of neurology. 2009;16 doi: 10.1111/j.1468-1331.2009.02606.x. [DOI] [PubMed] [Google Scholar]
- Cowan DM, Fan Q, Zou Y, Shi X, Chen J, Aschner M, Rosenthal FS, Zheng W. Manganese exposure among smelting workers: blood manganese-iron ratio as a novel tool for manganese exposure assessment. Biomarkers. 2009a;14:3–16. doi: 10.1080/13547500902730672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowan DM, Zheng W, Zou Y, Shi X, Chen J, Rosenthal FS, Fan Q. Manganese exposure among smelting workers: relationship between blood manganese-iron ratio and early onset neurobehavioral alterations. Neurotoxicology. 2009b;30:1214–1222. doi: 10.1016/j.neuro.2009.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Criswell SR, Nelson G, Gonzalez-Cuyar LF, Huang J, Shimony JS, Checkoway H, Simpson CD, Dills R, Seixas NS, Racette BA. Ex vivo magnetic resonance imaging in South African manganese mine workers. Neurotoxicology. 2015;49:8–14. doi: 10.1016/j.neuro.2015.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Criswell SR, Perlmutter JS, Huang JL, Golchin N, Flores HP, Hobson A, Aschner M, Erikson KM, Checkoway H, Racette BA. Basal ganglia intensity indices and diffusion weighted imaging in manganese-exposed welders. Occup Environ Med. 2012;69:437–443. doi: 10.1136/oemed-2011-100119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crossgrove J, Zheng W. Manganese toxicity upon overexposure. NMR in Biomedicine. 2004;17:544–553. doi: 10.1002/nbm.931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowe A, Morgan EH. Iron and copper interact during their uptake and deposition in the brain and other organs of developing rats exposed to dietary excess of the two metals. J Nutr. 1996;126:183–194. doi: 10.1093/jn/126.1.183. [DOI] [PubMed] [Google Scholar]
- Dion LA, Bouchard MF, Sauve S, Barbeau B, Tucholka A, Major P, Gilbert G, Mergler D, Saint-Amour D. MRI pallidal signal in children exposed to manganese in drinking water. Neurotoxicology. 2016;53:124–131. doi: 10.1016/j.neuro.2016.01.004. [DOI] [PubMed] [Google Scholar]
- Dobson AW, Erikson KM, Aschner M. Manganese neurotoxicity. Ann N Y Acad Sci. 2004;1012:115–128. doi: 10.1196/annals.1306.009. [DOI] [PubMed] [Google Scholar]
- Dorman DC, McManus BE, Marshall MW, James RA, Struve MF. Old age and gender influence the pharmacokinetics of inhaled manganese sulfate and manganese phosphate in rats. Toxicology and applied pharmacology. 2004;197:113–124. doi: 10.1016/j.taap.2004.02.010. [DOI] [PubMed] [Google Scholar]
- Dorman DC, Struve MF, Marshall MW, Parkinson CU, James RA, Wong BA. Tissue manganese concentrations in young male rhesus monkeys following subchronic manganese sulfate inhalation. Toxicol Sci. 2006a;92:201–210. doi: 10.1093/toxsci/kfj206. [DOI] [PubMed] [Google Scholar]
- Dorman DC, Struve MF, Wong BA, Dye JA, Robertson ID. Correlation of brain magnetic resonance imaging changes with pallidal manganese concentrations in rhesus monkeys following subchronic manganese inhalation. Toxicol Sci. 2006b;92:219–227. doi: 10.1093/toxsci/kfj209. [DOI] [PubMed] [Google Scholar]
- Duyn JH, Schenck J. Contributions to magnetic susceptibility of brain tissue. NMR Biomed. 2017;30 doi: 10.1002/nbm.3546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellingsen DG, Chashchin M, Bast-Pettersen R, Zibarev E, Thomassen Y, Chashchin V. A follow-up study of neurobehavioral functions in welders exposed to manganese. Neurotoxicology. 2015;47:8–16. doi: 10.1016/j.neuro.2014.12.012. [DOI] [PubMed] [Google Scholar]
- Ellingsen DG, Dubeikovskaya L, Dahl K, Chashchin M, Chashchin V, Zibarev E, Thomassen Y. Air exposure assessment and biological monitoring of manganese and other major welding fume components in welders. Journal of Environmental Monitoring. 2006;8:1078–1086. doi: 10.1039/b605549d. [DOI] [PubMed] [Google Scholar]
- Ellingsen DG, Konstantinov R, Bast-Pettersen R, Merkurjeva L, Chashchin M, Thomassen Y, Chashchin V. A neurobehavioral study of current and former welders exposed to manganese. Neurotoxicology. 2008;29:48–59. doi: 10.1016/j.neuro.2007.08.014. [DOI] [PubMed] [Google Scholar]
- Erikson KM, Dorman DC, Fitsanakis V, Lash LH, Aschner M. Alterations of oxidative stress biomarkers due to in utero and neonatal exposures of airborne manganese. Biol Trace Elem Res. 2006;111:199–215. doi: 10.1385/BTER:111:1:199. [DOI] [PubMed] [Google Scholar]
- Erikson KM, Syversen T, Steinnes E, Aschner M. Globus pallidus: a target brain region for divalent metal accumulation associated with dietary iron deficiency. The Journal of nutritional biochemistry. 2004;15:335–341. doi: 10.1016/j.jnutbio.2003.12.006. [DOI] [PubMed] [Google Scholar]
- Fitsanakis VA, Zhang N, Garcia S, Aschner M. Manganese (Mn) and iron (Fe): interdependency of transport and regulation. Neurotoxicity research. 2010;18:124–131. doi: 10.1007/s12640-009-9130-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn MR, Susi P. Modeling mixed exposures: an application to welding fumes in the construction trades. Stochastic Environmental Research and Risk Assessment 2009 [Google Scholar]
- Gallez B, Demeure R, Baudelet C, Abdelouahab N, Beghein N, Jordan B, Geurts M, Roels HA. Non invasive quantification of manganese deposits in the rat brain by local measurement of NMR proton T 1 relaxation times. Neurotoxicology. 2001;22:387–392. doi: 10.1016/s0161-813x(01)00020-1. [DOI] [PubMed] [Google Scholar]
- Gelfand IM, Latash ML. On the problem of adequate language in motor control. Motor Control. 1998;2:306–313. doi: 10.1123/mcj.2.4.306. [DOI] [PubMed] [Google Scholar]
- Gelman N, Gorell JM, Barker PB, Savage RM, Spickler EM, Windham JP, Knight RA. MR imaging of human brain at 3.0 T: preliminary report on transverse relaxation rates and relation to estimated iron content. Radiology. 1999;210:759–767. doi: 10.1148/radiology.210.3.r99fe41759. [DOI] [PubMed] [Google Scholar]
- Gerlach M, Ben-Shachar D, Riederer P, Youdim MB. Altered brain metabolism of iron as a cause of neurodegenerative diseases? J Neurochem. 1994;63:793–807. doi: 10.1046/j.1471-4159.1994.63030793.x. [DOI] [PubMed] [Google Scholar]
- Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, Poewe W, Sampaio C, Stern MB, Dodel R, Dubois B, Holloway R, Jankovic J, Kulisevsky J, Lang AE, Lees A, Leurgans S, LeWitt PA, Nyenhuis D, Olanow CW, Rascol O, Schrag A, Teresi JA, van Hilten JJ, LaPelle N. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord. 2008;23:2129–2170. doi: 10.1002/mds.22340. [DOI] [PubMed] [Google Scholar]
- Grogan A, Green DW, Ali N, Crinion JT, Price CJ. Structural correlates of semantic and phonemic fluency ability in first and second languages. Cereb Cortex. 2009;19:2690–2698. doi: 10.1093/cercor/bhp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guilarte TR. Manganese and Parkinson’s disease: a critical review and new findings. Environmental health perspectives. 2010:1071–1080. doi: 10.1289/ehp.0901748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guilarte TR. Manganese neurotoxicity: new perspectives from behavioral, neuroimaging, and neuropathological studies in humans and non-human primates. Front Aging Neurosci. 2013;5:23. doi: 10.3389/fnagi.2013.00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guilarte TR, Burton NC, McGlothan JL, Verina T, Zhou Y, Alexander M, Pham L, Griswold M, Wong DF, Syversen T. Impairment of nigrostriatal dopamine neurotransmission by manganese is mediated by pre-synaptic mechanism (s): implications to manganese-induced parkinsonism. Journal of neurochemistry. 2008;107:1236–1247. doi: 10.1111/j.1471-4159.2008.05695.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guilarte TR, Gonzales KK. Manganese-induced parkinsonism is not idiopathic Parkinson’s disease: environmental and genetic evidence. Toxicological Sciences. 2015;146:204–212. doi: 10.1093/toxsci/kfv099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guilarte TR, McGlothan JL, Degaonkar M, Chen MK, Barker PB, Syversen T, Schneider JS. Evidence for cortical dysfunction and widespread manganese accumulation in the nonhuman primate brain following chronic manganese exposure: a 1H-MRS and MRI study. Toxicol Sci. 2006;94:351–358. doi: 10.1093/toxsci/kfl106. [DOI] [PubMed] [Google Scholar]
- Haacke EM, Cheng NY, House MJ, Liu Q, Neelavalli J, Ogg RJ, Khan A, Ayaz M, Kirsch W, Obenaus A. Imaging iron stores in the brain using magnetic resonance imaging. Magn Reson Imaging. 2005;23:1–25. doi: 10.1016/j.mri.2004.10.001. [DOI] [PubMed] [Google Scholar]
- Hallgren B, Sourander P. The effect of age on the non-haemin iron in the human brain. Journal of neurochemistry. 1958;3:41–51. doi: 10.1111/j.1471-4159.1958.tb12607.x. [DOI] [PubMed] [Google Scholar]
- Han JH, Chung YH, Park JD, Kim CY, Yang SO, Khang HS, Cheong HK, Lee JS, Ha CS, Song CW, Kwon IH, Sung JH, Heo JD, Kim NY, Huang M, Cho MH, Yu IJ. Recovery from welding-fume-exposure-induced MRI T1 signal intensities after cessation of welding-fume exposure in brains of cynomolgus monkeys. Inhal Toxicol. 2008;20:1075–1083. doi: 10.1080/08958370802116634. [DOI] [PubMed] [Google Scholar]
- Hashimoto R, Mori T, Nemoto K, Moriguchi Y, Noguchi H, Nakabayashi T, Hori H, Harada S, Kunugi H, Saitoh O. Abnormal microstructures of the basal ganglia in schizophrenia revealed by diffusion tensor imaging. The World Journal of Biological Psychiatry. 2009;10:65–69. doi: 10.1080/15622970701762536. [DOI] [PubMed] [Google Scholar]
- Hauser RA, Zesiewicz TA, Martinez C, Rosemurgy AS, Olanow C. Blood manganese correlates with brain magnetic resonance imaging changes in patients with liver disease. The Canadian journal of neurological sciences Le journal canadien des sciences neurologiques. 1996;23:95–98. doi: 10.1017/s0317167100038786. [DOI] [PubMed] [Google Scholar]
- Holm S. A simple sequentially rejective multiple test procedure. Scandinavian journal of statistics. 1979:65–70. [Google Scholar]
- Huang CC, Lu CS, Chu NS, Hochberg F, Lilienfeld D, Olanow W, Calne DB. Progression after chronic manganese exposure. Neurology. 1993;43:1479–1483. doi: 10.1212/wnl.43.8.1479. [DOI] [PubMed] [Google Scholar]
- Iavicoli I, Fontana L, Bergamaschi A. The effects of metals as endocrine disruptors. J Toxicol Environ Health B Crit Rev. 2009;12:206–223. doi: 10.1080/10937400902902062. [DOI] [PubMed] [Google Scholar]
- Jellinger K, Paulus W, Grundke-Iqbal I, Riederer P, Youdim MB. Brain iron and ferritin in Parkinson’s and Alzheimer’s diseases. J Neural Transm Park Dis Dement Sect. 1990;2:327–340. doi: 10.1007/BF02252926. [DOI] [PubMed] [Google Scholar]
- Jo HJ, Ambike S, Lewis MM, Huang X, Latash ML. Finger force changes in the absence of visual feedback in patients with Parkinson’s disease. Clin Neurophysiol. 2015a doi: 10.1016/j.clinph.2015.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jo HJ, Park J, Lewis MM, Huang X, Latash ML. Prehension synergies and hand function in early-stage Parkinson’s disease. Exp Brain Res. 2015b;233:425–440. doi: 10.1007/s00221-014-4130-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones DC, Miller GW. The effects of environmental neurotoxicants on the dopaminergic system: A possible role in drug addiction. Biochem Pharmacol. 2008;76:569–581. doi: 10.1016/j.bcp.2008.05.010. [DOI] [PubMed] [Google Scholar]
- Khalid M, Aoun RA, Mathews TA. Altered striatal dopamine release following a sub-acute exposure to manganese. Journal of neuroscience methods. 2011;202:182–191. doi: 10.1016/j.jneumeth.2011.06.019. [DOI] [PubMed] [Google Scholar]
- Kim SH, Chang KH, Chi JG, Cheong HK, Kim JY, Kim YM, Han MH. Sequential change of MR signal intensity of the brain after manganese administration in rabbits. Correlation with manganese concentration and histopathologic findings. Invest Radiol. 1999;34:383–393. doi: 10.1097/00004424-199906000-00001. [DOI] [PubMed] [Google Scholar]
- Kim Y. High signal intensities on T1-weighted MRI as a biomarker of exposure to manganese. Ind Health. 2004;42:111–115. doi: 10.2486/indhealth.42.111. [DOI] [PubMed] [Google Scholar]
- Latash ML. Synergy. Oxford University Press; USA: 2008. p. 432. [Google Scholar]
- Latash ML. The bliss (not the problem) of motor abundance (not redundancy) Exp Brain Res. 2012;217:1–5. doi: 10.1007/s00221-012-3000-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latash ML, Huang X. Neural control of movement stability: Lessons from studies of neurological patients. Neuroscience. 2015;301:39–48. doi: 10.1016/j.neuroscience.2015.05.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Bihan D, Mangin JF, Poupon C, Clark CA, Pappata S, Molko N, Chabriat H. Diffusion tensor imaging: concepts and applications. J Magn Reson Imaging. 2001;13:534–546. doi: 10.1002/jmri.1076. [DOI] [PubMed] [Google Scholar]
- Lee EY, Eslinger PJ, Flynn MR, Wagner D, Du G, Lewis MM, Kong L, Mailman RB, Huang X. Association of neurobehavioral performance with R2* in the caudate nucleus of asymptomatic welders. Neurotoxicology. 2017;58:66–74. doi: 10.1016/j.neuro.2016.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee EY, Flynn MR, Du G, Lewis MM, Fry R, Herring AH, Van Buren E, Van Buren S, Smeester L, Kong L, Yang Q, Mailman RB, Huang X. T1 Relaxation Rate (R1) Indicates Nonlinear Mn Accumulation in Brain Tissue of Welders With Low-Level Exposure. Toxicol Sci. 2015;146:281–289. doi: 10.1093/toxsci/kfv088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee EY, Flynn MR, Du G, Lewis MM, Herring AH, Van Buren E, Van Buren S, Kong L, Mailman RB, Huang X. Editor’s Highlight: Lower Fractional Anisotropy in the Globus Pallidus of Asymptomatic Welders, a Marker for Long-Term Welding Exposure. Toxicol Sci. 2016a;153:165–173. doi: 10.1093/toxsci/kfw116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee EY, Flynn MR, Du G, Li Y, Lewis MM, Herring AH, Van Buren E, Van Buren S, Kong L, Fry RC, Snyder AM, Connor JR, Yang QX, Mailman RB, Huang X. Increased R2* in the Caudate Nucleus of Asymptomatic Welders. Toxicol Sci. 2016b;150:369–377. doi: 10.1093/toxsci/kfw003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy BS, Nassetta WJ. Neurologic effects of manganese in humans: a review. Int J Occup Environ Health. 2003;9:153–163. doi: 10.1179/oeh.2003.9.2.153. [DOI] [PubMed] [Google Scholar]
- Lewis MM, Flynn MR, Lee EY, Van Buren S, Van Buren E, Du G, Fry RC, Herring AH, Kong L, Mailman RB, Huang X. Longitudinal T1 relaxation rate (R1) captures changes in short-term Mn exposure in welders. Neurotoxicology. 2016a;57:39–44. doi: 10.1016/j.neuro.2016.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis MM, Lee EY, Jo HJ, Du G, Park J, Flynn MR, Kong L, Latash ML, Huang X. Synergy as a new and sensitive marker of basal ganglia dysfunction: A study of asymptomatic welders. Neurotoxicology. 2016b;56:76–85. doi: 10.1016/j.neuro.2016.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyva-Illades D, Chen P, Zogzas CE, Hutchens S, Mercado JM, Swaim CD, Morrisett RA, Bowman AB, Aschner M, Mukhopadhyay S. SLC30A10 is a cell surface-localized manganese efflux transporter, and parkinsonism-causing mutations block its intracellular trafficking and efflux activity. Journal of Neuroscience. 2014;34:14079–14095. doi: 10.1523/JNEUROSCI.2329-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long Z, Jiang YM, Li XR, Fadel W, Xu J, Yeh CL, Long LL, Luo HL, Harezlak J, Murdoch JB, Zheng W, Dydak U. Vulnerability of welders to manganese exposure–a neuroimaging study. Neurotoxicology. 2014;45:285–292. doi: 10.1016/j.neuro.2014.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu L, Zhang L-l, Li GJ, Guo W, Liang W, Zheng W. Alteration of serum concentrations of manganese, iron, ferritin, and transferrin receptor following exposure to welding fumes among career welders. Neurotoxicology. 2005;26:257–265. doi: 10.1016/j.neuro.2004.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinney AM, Filice RW, Teksam M, Casey S, Truwit C, Clark HB, Woon C, Liu HY. Diffusion abnormalities of the globi pallidi in manganese neurotoxicity. Neuroradiology. 2004;46:291–295. doi: 10.1007/s00234-004-1179-1. [DOI] [PubMed] [Google Scholar]
- Mergler D, Baldwin M. Early manifestations of manganese neurotoxicity in humans: an update. Environ Res. 1997;73:92–100. doi: 10.1006/enrs.1997.3710. [DOI] [PubMed] [Google Scholar]
- Mergler D, Huel G, Bowler R, Iregren A, Belanger S, Baldwin M, Tardif R, Smargiassi A, Martin L. Nervous system dysfunction among workers with long-term exposure to manganese. Environ Res. 1994;64:151–180. doi: 10.1006/enrs.1994.1013. [DOI] [PubMed] [Google Scholar]
- Meyer-Baron M, Schaper M, Knapp G, Lucchini R, Zoni S, Bast-Pettersen R, Ellingsen DG, Thomassen Y, He S, Yuan H, Niu Q, Wang XL, Yang YJ, Iregren A, Sjogren B, Blond M, Laursen P, Netterstrom B, Mergler D, Bowler R, van Thriel C. The neurobehavioral impact of manganese: results and challenges obtained by a meta-analysis of individual participant data. Neurotoxicology. 2013;36:1–9. doi: 10.1016/j.neuro.2013.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson K, Golnick J, Korn T, Angle C. Manganese encephalopathy: utility of early magnetic resonance imaging. Br J Ind Med. 1993;50:510–513. doi: 10.1136/oem.50.6.510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newland MC, Cox C, Hamada R, Oberdorster G, Weiss B. The clearance of manganese chloride in the primate. FundamApplToxicol. 1987;9:314–328. doi: 10.1016/0272-0590(87)90054-6. [DOI] [PubMed] [Google Scholar]
- Nong A, Taylor MD, Clewell HJ, Dorman DC, Andersen ME. Manganese tissue dosimetry in rats and monkeys: accounting for dietary and inhaled Mn with physiologically based pharmacokinetic modeling. Toxicological sciences. 2009;108:22–34. doi: 10.1093/toxsci/kfn264. [DOI] [PubMed] [Google Scholar]
- Nong A, Teeguarden JG, Clewell HJ, III, Dorman DC, Andersen ME. Pharmacokinetic modeling of manganese in the rat IV: Assessing factors that contribute to brain accumulation during inhalation exposure. Journal of Toxicology and Environmental Health, Part A. 2008;71:413–426. doi: 10.1080/15287390701838697. [DOI] [PubMed] [Google Scholar]
- Norenberg MD, Rao KV. The mitochondrial permeability transition in neurologic disease. Neurochem Int. 2007;50:983–997. doi: 10.1016/j.neuint.2007.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neal SL, Zheng W. Manganese toxicity upon overexposure: a decade in review. Current environmental health reports. 2015;2:315–328. doi: 10.1007/s40572-015-0056-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olafsdottir H, Yoshida N, Zatsiorsky VM, Latash ML. Anticipatory covariation of finger forces during self-paced and reaction time force production. Neurosci Lett. 2005;381:92–96. doi: 10.1016/j.neulet.2005.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olanow CW, Good PF, Shinotoh H, Hewitt KA, Vingerhoets F, Snow BJ, Beal MF, Calne DB, Perl DP. Manganese intoxication in the rhesus monkey: a clinical, imaging, pathologic, and biochemical study. Neurology. 1996;46:492–498. doi: 10.1212/wnl.46.2.492. [DOI] [PubMed] [Google Scholar]
- Ostiguy C, Asselin P, Malo S. The emergence of manganese-related health problems in Quebec: an integrated approach to evaluation, diagnosis, management and control. Neurotoxicology. 2006;27:350–356. doi: 10.1016/j.neuro.2005.11.001. [DOI] [PubMed] [Google Scholar]
- Pal PK, Samii A, Calne DB. Manganese neurotoxicity: a review of clinical features, imaging and pathology. Neurotoxicology. 1999;20:227–238. [PubMed] [Google Scholar]
- Park J, Jo HJ, Lewis MM, Huang X, Latash ML. Effects of Parkinson’s disease on optimization and structure of variance in multi-finger tasks. Exp Brain Res. 2013;231:51–63. doi: 10.1007/s00221-013-3665-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J, Wu YH, Lewis MM, Huang X, Latash ML. Changes in multifinger interaction and coordination in Parkinson’s disease. J Neurophysiol. 2012;108:915–924. doi: 10.1152/jn.00043.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J, Zatsiorsky VM, Latash ML. Optimality vs. variability: an example of multi-finger redundant tasks. Exp Brain Res. 2010;207:119–132. doi: 10.1007/s00221-010-2440-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peran P, Cherubini A, Assogna F, Piras F, Quattrocchi C, Peppe A, Celsis P, Rascol O, Demonet JF, Stefani A, Pierantozzi M, Pontieri FE, Caltagirone C, Spalletta G, Sabatini U. Magnetic resonance imaging markers of Parkinson’s disease nigrostriatal signature. Brain. 2010;133:3423–3433. doi: 10.1093/brain/awq212. [DOI] [PubMed] [Google Scholar]
- Perl DP, Olanow CW. The neuropathology of manganese-induced Parkinsonism. Journal of Neuropathology & Experimental Neurology. 2007;66:675–682. doi: 10.1097/nen.0b013e31812503cf. [DOI] [PubMed] [Google Scholar]
- Pesch B, Weiss T, Kendzia B, Henry J, Lehnert M, Lotz A, Heinze E, Käfferlein HU, Van Gelder R, Berges M. Levels and predictors of airborne and internal exposure to manganese and iron among welders. Journal of Exposure Science and Environmental Epidemiology. 2012;22:291–298. doi: 10.1038/jes.2012.9. [DOI] [PubMed] [Google Scholar]
- Racette BA, Criswell SR, Lundin JI, Hobson A, Seixas N, Kotzbauer PT, Evanoff BA, Perlmutter JS, Zhang J, Sheppard L. Increased risk of parkinsonism associated with welding exposure. Neurotoxicology. 2012;33:1356–1361. doi: 10.1016/j.neuro.2012.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racette BA, Nielsen SS, Criswell SR, Sheppard L, Seixas N, Warden MN, Checkoway H. Dose-dependent progression of parkinsonism in manganese-exposed welders. Neurology. 2016 doi: 10.1212/WNL.0000000000003533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramoju SP, Mattison DR, Milton B, McGough D, Shilnikova N, Clewell HJ, Yoon M, Taylor MD, Krewski D, Andersen ME. The application of PBPK models in estimating human brain tissue manganese concentrations. Neurotoxicology. 2017;58:226–237. doi: 10.1016/j.neuro.2016.12.001. [DOI] [PubMed] [Google Scholar]
- Schöner G. Recent developments and problems in human movement science and their conceptual implications. Ecolog Psychol. 1995;8:291–314. [Google Scholar]
- Schaefer PW, Grant PE, Gonzalez RG. Diffusion-weighted MR imaging of the brain. Radiology. 2000;217:331–345. doi: 10.1148/radiology.217.2.r00nv24331. [DOI] [PubMed] [Google Scholar]
- Schmitt C, Strazielle N, Richaud P, Bouron A, Ghersi-Egea JF. Active transport at the blood-CSF barrier contributes to manganese influx into the brain. Journal of neurochemistry. 2011;117:747–756. doi: 10.1111/j.1471-4159.2011.07246.x. [DOI] [PubMed] [Google Scholar]
- Scholz JP, Schoner G. The uncontrolled manifold concept: identifying control variables for a functional task. Exp Brain Res. 1999;126:289–306. doi: 10.1007/s002210050738. [DOI] [PubMed] [Google Scholar]
- Schroeter JD, Nong A, Yoon M, Taylor MD, Dorman DC, Andersen ME, Clewell HJ. Analysis of manganese tracer kinetics and target tissue dosimetry in monkeys and humans with multi-route physiologically-based pharmacokinetic models. Toxicological sciences. 2010:kfq389. doi: 10.1093/toxsci/kfq389. [DOI] [PubMed] [Google Scholar]
- Shin YC, Kim E, Cheong HK, Cho S, Sakong J, Kim KS, Yang JS, Jin YW, Kang SK, Kim Y. High signal intensity on magnetic resonance imaging as a predictor of neurobehavioral performance of workers exposed to manganese. Neurotoxicology. 2007;28:257–262. doi: 10.1016/j.neuro.2006.03.014. [DOI] [PubMed] [Google Scholar]
- Sidoryk-Wegrzynowicz M, Aschner M. Manganese toxicity in the central nervous system: the glutamine/glutamate-gamma-aminobutyric acid cycle. J Intern Med. 2013a;273:466–477. doi: 10.1111/joim.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidoryk-Wegrzynowicz M, Aschner M. Role of astrocytes in manganese mediated neurotoxicity. BMC Pharmacol Toxicol. 2013b;14:23. doi: 10.1186/2050-6511-14-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon-Sanchez J, Schulte C, Bras JM, Sharma M, Gibbs JR, Berg D, Paisan-Ruiz C, Lichtner P, Scholz SW, Hernandez DG, Kruger R, Federoff M, Klein C, Goate A, Perlmutter J, Bonin M, Nalls MA, Illig T, Gieger C, Houlden H, Steffens M, Okun MS, Racette BA, Cookson MR, Foote KD, Fernandez HH, Traynor BJ, Schreiber S, Arepalli S, Zonozi R, Gwinn K, van der Brug M, Lopez G, Chanock SJ, Schatzkin A, Park Y, Hollenbeck A, Gao J, Huang X, Wood NW, Lorenz D, Deuschl G, Chen H, Riess O, Hardy JA, Singleton AB, Gasser T. Genome-wide association study reveals genetic risk underlying Parkinson’s disease. Nat Genet. 2009;41:1308–1312. doi: 10.1038/ng.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sipe JC, Lee P, Beutler E. Brain iron metabolism and neurodegenerative disorders. Developmental neuroscience. 2002;24:188–196. doi: 10.1159/000065701. [DOI] [PubMed] [Google Scholar]
- Snyder AM, Connor JR. Iron, the substantia nigra and related neurological disorders. Biochim Biophys Acta. 2009;1790:606–614. doi: 10.1016/j.bbagen.2008.08.005. [DOI] [PubMed] [Google Scholar]
- Stepens A, Stagg CJ, Platkajis A, Boudrias MH, Johansen-Berg H, Donaghy M. White matter abnormalities in methcathinone abusers with an extrapyramidal syndrome. Brain. 2010;133:3676–3684. doi: 10.1093/brain/awq281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeda A. Manganese action in brain function. Brain Res Brain Res Rev. 2003;41:79–87. doi: 10.1016/s0165-0173(02)00234-5. [DOI] [PubMed] [Google Scholar]
- Tapin D, Kennedy G, Lambert J, Zayed J. Bioaccumulation and locomotor effects of manganese sulfate in Sprague–Dawley rats following subchronic (90 days) inhalation exposure. Toxicology and applied pharmacology. 2006;211:166–174. doi: 10.1016/j.taap.2005.07.007. [DOI] [PubMed] [Google Scholar]
- Vymazal J, Bulte JW, Frank JA, Chiro GD, Brooks RA. Frequency dependence of MR relaxation times I. Paramagnetic ions. Journal of Magnetic Resonance Imaging. 1993;3:637–640. doi: 10.1002/jmri.1880030413. [DOI] [PubMed] [Google Scholar]
- Wang Y, Liu T. Quantitative susceptibility mapping (QSM): Decoding MRI data for a tissue magnetic biomarker. Magn Reson Med. 2014 doi: 10.1002/mrm.25358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward RJ, Zucca FA, Duyn JH, Crichton RR, Zecca L. The role of iron in brain ageing and neurodegenerative disorders. The Lancet Neurology. 2014;13:1045–1060. doi: 10.1016/S1474-4422(14)70117-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright RO, Baccarelli A. Metals and neurotoxicology. J Nutr. 2007;137:2809–2813. doi: 10.1093/jn/137.12.2809. [DOI] [PubMed] [Google Scholar]
- Yilmaz A, Yurdakoc M, Isik B. Influence of transition metal ions on NMR proton T1 relaxation times of serum, blood, and red cells. BiolTrace ElemRes. 1999;67:187–193. doi: 10.1007/BF02784073. [DOI] [PubMed] [Google Scholar]
- Yokel RA. Blood-brain barrier flux of aluminum, manganese, iron and other metals suspected to contribute to metal-induced neurodegeneration. J Alzheimers Dis. 2006;10:223–253. doi: 10.3233/jad-2006-102-309. [DOI] [PubMed] [Google Scholar]
- Yokel RA. Manganese flux across the blood-brain barrier. Neuromolecular Med. 2009;11:297–310. doi: 10.1007/s12017-009-8101-2. [DOI] [PubMed] [Google Scholar]
- Yoshikawa K, Nakata Y, Yamada K, Nakagawa M. Early pathological changes in the parkinsonian brain demonstrated by diffusion tensor MRI. J Neurol Neurosurg Psychiatry. 2004;75:481–484. doi: 10.1136/jnnp.2003.021873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang N, Fitsanakis VA, Erikson KM, Aschner M, Avison MJ, Gore JC. A model for the analysis of competitive relaxation effects of manganese and iron in vivo. NMR in biomedicine. 2009;22:391–404. doi: 10.1002/nbm.1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoni S, Albini E, Lucchini R. Neuropsychological testing for the assessment of manganese neurotoxicity: a review and a proposal. Am J Ind Med. 2007;50:812–830. doi: 10.1002/ajim.20518. [DOI] [PubMed] [Google Scholar]
- Zoni S, Bonetti G, Lucchini R. Olfactory functions at the intersection between environmental exposure to manganese and Parkinsonism. Journal of Trace Elements in Medicine and Biology. 2012;26:179–182. doi: 10.1016/j.jtemb.2012.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]


