Abstract
Because no effective methods for preventing or screening for ovarian cancer exist, symptom recognition is integral to its early detection. The Centers for Disease Control and Prevention’s Inside Knowledge: Get the Facts about Gynecologic Cancer campaign was developed to raise awareness and educate women and providers about risk factors, symptoms, recommended screening, and prevention strategies for the five main gynecologic cancers, including ovarian cancer. Inside Knowledge campaign materials were utilized by CDC’s National Comprehensive Cancer Control Program grantees to educate women and providers about gynecologic cancer from 2014 to 2015. Grantees recruited participants and held educational sessions using Inside Knowledge materials. Questionnaires were given before and after the sessions to assess changes in awareness, confidence, and behavioral intentions around gynecologic cancer information and analyzed in 2016. This analysis focused on an assessment of changes related to ovarian cancer information. Participants’ knowledge increased after educational sessions. Among women, there were increases in correctly identifying that the Papanicolaou (Pap) test does not screen for ovarian cancer (89.2%) and that genetic testing is available (77.9%). There was a lower increase in knowledge that HPV is not a cause of ovarian cancer (56.4%). Providers and women reported significant increases in their confidence in their ability to talk to each other about gynecologic cancer post-session. Ovarian cancer awareness, confidence, and related behaviors increased in participants exposed to Inside Knowledge materials. Using these materials to increase knowledge could lead to more empowered patients, better provider-patient communications, and improved care for gynecologic cancers, including ovarian cancer.
Keywords: Cancer prevention, Ovarian cancer, Health education, Cancer control
Introduction
Ovarian cancer accounts for more deaths than any other gynecologic cancer, with 14,000 women dying yearly [1, 2]. Due to an aging population, these numbers are expected to increase [3]. No screening tests are currently recommended for ovarian cancer [4]. Though specific symptoms are associated with ovarian cancer, they may appear non-specific if patients or providers are unaware of their association [5]. Consequently, ovarian cancer is usually diagnosed at a late stage after the cancer has spread, leading to a poor prognosis [6]. Because there are no effective methods for prevention or screening, symptom recognition is integral to early detection of ovarian cancer.
The Inside Knowledge: Get the Facts about Gynecologic Cancer campaign was developed by the Centers for Disease Control and Prevention (CDC), in collaboration with the Department of Health and Human Services’ Office on Women’s Health, to support the Gynecologic Cancer Education and Awareness Act of 2005 (Johanna’s Law) [7]. The campaign is designed to raise awareness of the five main types of gynecologic cancer (cervical, ovarian, uterine, vaginal, and vulvar) and educate women and providers about risk factors, symptoms, recommended screening, and prevention strategies for these cancers [7]. It encourages women to understand what is normal for themselves so they can recognize any persistent changes and seek timely medical care. Inside Knowledge resources include print, broadcast, and digital public service announcements; educational materials such as brochures and fact sheets; and continuing education modules for providers.
In this study, Inside Knowledge materials were utilized by National Comprehensive Cancer Control Program (NCCCP) grantees to educate women and providers in local US communities. The NCCCP is funded by CDC to develop state, tribal, or territorial-specific cancer plans containing evidence-based interventions for preventing and controlling cancer at the community level. Grantees are well-versed in the cancer-related needs of their populations and have demonstrated success in implementing public health efforts to decrease cancer incidence, morbidity, and mortality [8, 9]. Participant knowledge and behavioral intentions around ovarian cancer were assessed after participating in NCCCP educational sessions using Inside Knowledge materials. While Inside Knowledge addresses five types of gynecologic cancers, this study analysis focuses only on changes in ovarian cancer knowledge, attitudes, and behaviors among participants.
Methods
Participants and Sessions
Participants included women aged 18 years and older and healthcare providers from eight NCCCP grantee areas: Alaska, Michigan, New Jersey, Puerto Rico, Tennessee, Texas, West Virginia, and Wisconsin in 2014 and 2015. Recruitment was carried out by grantees and included flyers, newspaper ads, email listservs, social media, and other communications advertising an educational session on gynecologic cancer.
Sessions were held in local areas determined by the grantee, to maximize participation and/or reach the most at need (those of low socioeconomic status or from traditionally underserved groups). Though recruitment methods varied somewhat and information presentation was specific to each population (i.e., educators/facilitators from local areas were used), each session followed a standardized pre-determined format, planned according to multiple learning theories including the health behavior model, the self-efficacy model, and the theory of planned behavior [10–12]. During sessions, grantees initially administered a questionnaire to establish baseline knowledge of messages in the Inside Knowledge campaign and participants’ experience with gynecologic cancer, including ovarian cancer. Trained facilitators conducted educational discussions of the Inside Knowledge materials including a print brochure, fact sheets, symptoms diary, and survivor stories. Following facilitated discussions, questionnaires were administered again to measure differences in knowledge and uptake of the information presented.
Training of all grantee-appointed facilitators was conducted in one interactive group session. Though the sessions were required to have the same format, facilitators were allowed to tailor discussions to their population for maximum impact (for instance, storytelling was used in Alaska sessions as opposed to a lecture format). Sessions were held in English, except in Puerto Rico, which used Spanish Inside Knowledge materials and conducted sessions in Spanish. All Inside Knowledge materials used were provided by CDC and are available to the public free upon request from the CDC website. Minimal incentives were provided for participants, consistent with federal government Office of Management and Budget (OMB) regulations, such as $30 gift cards for public participants and CME credits for providers.
Data Collection
The identical pre- and post-session questionnaires were designed to assess key Inside Knowledge campaign messages and controlled for participants’ prior knowledge. Public and provider questionnaires asked the same questions; however, in some cases, wording was slightly changed to ensure readability and comprehension. To maintain confidentiality, questionnaires were not linked to individual participants. Unique models of learning theory were used to develop the questionnaire. The health belief model, stating that health behavior is determined by personal beliefs about a disease including perceived (1) seriousness, (2) susceptibility, (3) benefits, and (4) barriers, was used to develop questions related to health beliefs, such as, “Please indicate how much you agree or disagree with the following statement: Women should be generally aware of gynecologic cancer signs and symptoms” [10, 13]. The self-efficacy model, relating to a sense of control over one’s environment and behavior, was used to develop questions related to confidence in talking about health issues, such as “How confident are you that you have enough information to inform your patients about ovarian cancer?” [11]. The theory of planned behavior, stating that intention is the closest prediction of behavior, was used to develop questions related to behavioral intentions, such as “Please check the box which indicates how likely you are to ‘Talk to my doctor about genetic testing for BRCA1 and BRCA2 genes and other syndromes that can be inherited’” [12]. Information on participant demographics and providers’ clinical practice characteristics was also obtained.
Questions were closed-ended and included multiple choice, five-item Likert scale, and true/false questions. Questionnaire usability testing was completed with women and providers prior to use in educational sessions. Paper questionnaires were entered into an electronic database using Snap Survey Software. Scanned surveys were reviewed by two researchers in order to correct data entry errors that occurred during the scanning process and ensure the quality of scanned data.
CDC determined that this study constituted public health practice and did not require Institutional Review Board (IRB) review. OMB reviewed and approved all data collection aspects of this study, including the questionnaires. Per OMB regulations, informed consent was obtained from all participants, and all questionnaires contained the OMB approval number 0920-0800.
Statistical Analysis
Dataset Preparation and Variables
Data analysis was performed in 2016. Prior to analysis, we examined the frequency counts and distribution of all variables. We collapsed categories for some demographic variables due to infrequent responses (e.g., age, education level, and race) to protect confidentiality. Participants selecting several or more races as their racial/ethnic background were coded as “multiple race/other.” For providers who specified “other” as their specialty, we created new specialty categories if enough similar responses were provided (e.g., pediatricians and school nurses). In some cases, participants provided more than one response to a question requiring only a single response. Some questions also allowed for more than one correct response. New dichotomous variables that indicated all correct responses versus partially or no correct responses were developed, as well as variables that recoded multiple responses to single response questions as missing. Because relatively few participants provided responses low on the Likert scales, behavioral intentions measured on a Likert scale were individually categorized as extremely likely/somewhat likely or not at all likely/not very likely/neither. Confidence levels also measured on a Likert scale were grouped as somewhat confident/extremely confident or neutral/not very confident/not at all confident.
Data Analysis
We examined the demographic characteristics of providers and women who attended the Inside Knowledge educational sessions. Because ovarian cancer was the focus of this analysis, we analyzed all survey questions specific to ovarian cancer (e.g., risk factors for ovarian cancer), and other questions that included ovarian cancer as a response option (e.g., availability of genetic testing or an effective screening test). We also included questions about symptom recognition, confidence, and behavioral intentions for gynecologic cancer overall if they were relevant to ovarian cancer. In some instances, we only analyzed the response options that were relevant to ovarian cancer (e.g., symptoms consistent with ovarian cancer). For the healthcare provider analysis, we conducted bivariate analyses between obstetricians/gynecologists (OBGYNs) and all other providers (primary care physicians, family physicians, physician assistants, nurses, etc.) because OBGYNs have been shown to have a higher level of baseline gynecologic cancer knowledge [14]. We assessed pre- to post-test differences in knowledge of risk factors, symptoms, diagnosis, behavioral intentions, and level of confidence in discussing ovarian cancer among women and both groups of providers.
SAS 9.3 (SAS Institute, Inc.; Cary, NC) was used to conduct all analyses. All statistical tests used a significance level set at alpha = 0.05, and p values were obtained from Chi-square tests or Fisher’s exact test for categorical variables.
Results
Table 1 shows the case characteristics of all participants. Most public participants were 45 years old or older (67.4%) and were most commonly white (40.8%) and Hispanic/Latino (37.2%). The majority of provider participants were between 45 and 64 years old (52.5% of obstetrician/gynecologists and 57.1% of other specialties). Most obstetrician/gynecologist providers were male (59.1%) and most providers with other specialties were female (90.9%). There were 90.4% of obstetrician/gynecologists who were Hispanic/Latino, and 58.4% of other providers were white. Most obstetrician/gynecologist providers saw a combination of inpatients and outpatients (68%) and saw 21–30 patients per day (35.9%). Relatively few providers were aware of the Inside Knowledge campaign (10% of obstetrician/gynecologists and 6.9% of other specialties), but providers agreed that gynecologic cancer was a problem in their patient population (93.3% of obstetrician/gynecologists and 80.9% of other specialties). (Table 1)
Table 1.
Characteristics of women and provider participants
| Providers
|
Public, n = 499 | |||
|---|---|---|---|---|
| Obstetrician-gynecologist, n = 106 | Other specialty, n = 259 |
|
||
| N (%) | N (%) | P value | N (%) | |
| Age* | ||||
| <35 years | 15 (14.6) | 51 (20.1) | 0.0002 | 87 (18.0) |
| 35–44 years | 13 (12.6) | 46 (18.1) | 71 (14.7) | |
| 45–54 years | 25 (24.3) | 70 (27.6) | 105 (21.7) | |
| 55–64 years | 29 (28.2) | 75 (29.5) | 113 (23.4) | |
| 65+ years | 21 (20.4) | 12 (4.7) | 108 (22.3) | |
| Gender* | ||||
| Male | 62 (59.1) | 23 (9.1) | <.0001 | N/A |
| Female | 43 (41.0) | 229 (90.9) | ||
| Race/ethnicity*a | ||||
| Hispanic/Latino | 94 (90.4) | 53 (20.6) | <.0001 | 177 (37.2) |
| American Indian/Alaska Native | – | – | 16 (3.4) | |
| Asian/Native Hawaiian/Pacific Islander | 1 (1.0) | 25 (9.7) | 9 (1.9) | |
| African-American | 1 (1.0) | 24 (9.3) | 70 (14.7) | |
| White/Caucasian | 8 (7.7) | 150 (58.4) | 194 (40.8) | |
| Multiple race/other | 0 (0) | 5 (2.0) | 10 (2.1) | |
| Specialty | ||||
| Family | N/A | 30 (11.6) | <.0001 | N/A |
| Internal | N/A | 16 (6.2) | ||
| Pediatrics | N/A | 3 (1.2) | ||
| General medicine | N/A | 10 (3.9) | ||
| OBGYN | 106 (100) | N/A | ||
| Nurse practitioner/physician’s assistant | N/A | 43 (16.6) | ||
| Nurse | N/A | 107 (41.3) | ||
| School nurse | N/A | 9 (3.5) | ||
| Other | N/A | 41 (15.8) | ||
| Work environment* | ||||
| Inpatient | 2 (1.9) | 22 (8.9) | <.0001 | N/A |
| Outpatient | 29 (28.2) | 125 (50.8) | ||
| Combination (inpatient/outpatient) | 70 (68.0) | 42 (17.1) | ||
| School | 0 | 27 (11.0) | ||
| Other | 2 (1.9) | 30 (12.2) | ||
| Average patients seen per day* | ||||
| <10 | 7 (6.8) | 58 (24.0) | <.0001 | N/A |
| 10–20 | 32 (31.1) | 84 (34.7) | ||
| 21–30 | 37 (35.9) | 46 (19.0) | ||
| 31–40 | 21 (20.4) | 24 (9.9) | ||
| 41+ | 5 (4.9) | 19 (7.9) | ||
| Not sure | 1 (1.0) | 11 (4.6) | ||
| Some high school or less | N/A | 22 (4.7) | ||
| High school graduate/GED | 68 (14.6) | |||
| Some college | 126 (27.0) | |||
| College graduate | 94 (20.2) | |||
| Graduate studies | 147 (31.6) | |||
| Other | 9 (1.9) | |||
| Awareness of IK campaign | 10 (10.0) | 17 (6.9) | 0.4340 | 93 (19.9) |
| Gynecologic cancer is a problem for my patient population (pre-session agreement) | 98 (93.3) | 203 (80.9) | N/A | |
p < 0.05 from Chi-square tests (providers only)
Race variables and Hispanic ethnicity were not mutually exclusive
Table 2 shows knowledge changes among participants after facilitated discussions of Inside Knowledge materials. Significant increases in risk factor knowledge were seen in both public and providers after educational sessions. Increases were seen for all participants post-session for correctly identifying never having given birth or infertility as a risk factor for ovarian cancer (73.6% of obstetrician/gynecologists, 77.8% of other specialty providers, and 78.1% of public participants). Public participants and providers with specialties other than obstetrician/gynecologists saw significant increases in knowledge of Ashkenazi Jewish background as a risk factor for ovarian cancer (65.9% of other specialty providers and 76.6% of public participants) and in correctly identifying all risk factors for ovarian cancer (50.0% of other specialty providers and 43.8 of public participants). After sessions, 23.1% of obstetrician/gynecologists correctly identified all risk factors for ovarian cancer. No significant increases were seen for family history as a risk factor, but presession knowledge of this risk factor was high in all participants.
Table 2.
Knowledge of ovarian cancer risk factors, signs, and symptoms among women and providers
| Question | Provider
|
Public | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Obstetrician-gynecologist
|
Other specialty
|
|
|||||||
| Pre-session knowledge N (%) | Post-session knowledge N (%) | P value* | Pre-session knowledge N (%) | Post-session knowledge N (%) | P value* | Pre-session knowledge N (%) | Post-session knowledge N (%) | P value* | |
| Risk factors | |||||||||
| Family history | 96 (91.4) | 87 (95.6) | 0.2413 | 237 (92.9) | 234 (92.9) | 0.9706 | 419 (90.5) | 403 (89.2) | 0.5032 |
| Never giving birth/infertility | 58 (55.2) | 67 (73.6) | 0.0076 | 141 (55.3) | 196 (77.8) | <.0001 | 201 (43.4) | 353 (78.1) | <.0001 |
| Ashkenazi Jewish background | 20 (19.1) | 26 (28.6) | 0.1166 | 86 (33.7) | 166 (65.9) | <.0001 | 101 (21.8) | 346 (76.6) | <.0001 |
| Risk factors for ovarian cancer (all correct). | 13 (12.4) | 21 (23.1) | 0.0486 | 46 (18.0) | 126 (50.0) | <.0001 | 41 (8.9) | 198 (43.8) | <.0001 |
| Signs and symptoms | |||||||||
| Pelvic pain/pressure | 94 (92.2) | 84 (93.3) | 0.7544 | 205 (81.7) | 223 (88.5) | 0.0318 | 334 (73.3) | 389 (89.4) | <.0001 |
| Abnormal bleeding or discharge | 17 (16.4) | 23 (25.8) | 0.1047 | 74 (29.0) | 130 (51.6) | <.0001 | 435 (95.4) | 422 (97.0) | 0.2080 |
| Abdominal or back pain | – | – | – | – | 276 (60.5) | 377 (86.7) | <.0001 | ||
| Bloating | – | – | – | – | 243 (53.3) | 379 (87.1) | <.0001 | ||
| Change in bathroom habits | – | – | – | – | 214 (46.9) | 365 (83.9) | <.0001 | ||
p values from Chi-square tests or Fisher’s exact test
Public participants showed a significant increase in post-session knowledge of pelvic pain/pressure (89.4%), abdominal or back pain (86.7%), bloating (87.1%), and changes in bathroom habits (83.9%) as symptoms of ovarian cancer (Table 2). Providers of other specialties also showed significant increases in post-session knowledge of pelvic pain/pressure (88.5%) and abnormal bleeding (51.6%) as symptoms of ovarian cancer. No significant increases in symptom knowledge were seen in obstetri- cian/gynecologists, with 93.3% correctly identifying pelvic pain/pressure and 25.8% correctly identifying abnormal bleeding or discharge as symptoms of ovarian cancer.
Figure 1 shows changes in knowledge of ovarian cancer testing and diagnostics after facilitated discussions of Inside Knowledge materials. There was a significant increase among public participants in correctly identifying that the Pap test does not screen for ovarian cancer (89.2%) and that genetic testing is available for ovarian cancer (77.9%). However, fewer public participants also correctly identified that HPV is not a cause of ovarian cancer after sessions (56.4%) than prior (68.1%). No significant changes were seen in provider knowledge for Pap testing, HPV, and genetic testing as they relate to ovarian cancer, but correct knowledge was high for all provider participants both before and after sessions, ranging from 92.1 to 96.6% for obstetrician/gynecologists and 83.1 to 98.4% for other specialties post-session.
Fig. 1.
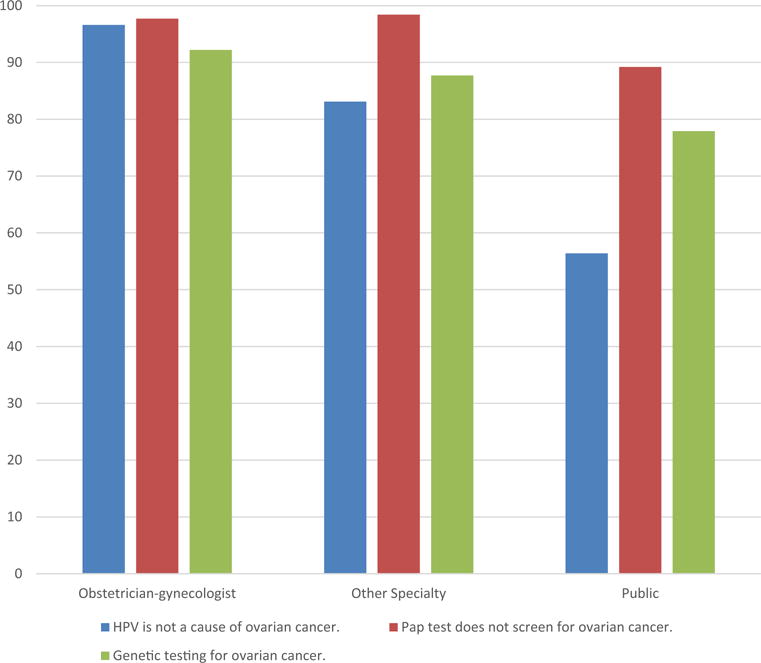
Knowledge of ovarian cancer testing and diagnostics among women and providers. Bars represent the percentage of each group (obstetricians/gynecologists, providers with other specialties, and public participants) that correctly that HPV is not a cause of ovarian cancer (blue bar), the Pap test does not screen for ovarian cancer (red bar), and genetic testing is available for ovarian cancer (green bar)
Table 3 shows provider behavioral intentions and confidence with ovarian cancer information before and after facilitated discussions of Inside Knowledge materials. All providers reported a significant increase in confidence with their ability to inform patients about ovarian cancer (97.8% of obstetrician/gynecologists and 91.0% of other specialties). Providers with other specialties also saw significant increases in their confidence to educate their patients appropriately about gynecologic cancer risks and symptoms (91.8%) and to assess symptoms of gynecologic cancer in their patients and conduct appropriate tests (85.8%). These providers also reported a significant increase after sessions in their intention to refer patients whom they suspected of having a gynecologic cancer to gynecologic oncologist. No other significant increases were seen in obstetrician/gynecologists, but post-session agreement ranged from 88.5 to 97.8% for items assessed in this group.
Table 3.
Behavioral intentions and level of confidence surrounding ovarian cancer information among women and providers
| Question | Providers
|
Public | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Obstetrician-gynecologist
|
Other specialty
|
|
|||||||
| Pre-session agreement | Post-session agreement | P value | Pre-session agreement | Post-session agreement | P value | Pre-session agreement | Post-session agreement | P value | |
| Educate my patients appropriately about gynecologic cancer risk and symptoms.a | 101 (97.1) | 86 (97.7) | 0.7908 | 210 (83.0) | 225 (91.8) | 0.0030 | – | – | – |
| Assess symptoms of gynecologic cancer in my patients and conduct appropriate tests.a | 103 (98.1) | 86 (97.7) | 0.8582 | 184 (73.6) | 205 (85.8) | 0.0008 | – | – | – |
| Refer patients suspected of a gynecologic cancer to a gynecologic oncologist.a | 92 (87.6) | 77 (88.5) | 0.8506 | 207 (81.8) | 217 (88.9) | 0.0251 | – | – | – |
| Confidence with information about ovarian cancer.b | 91 (90.1) | 88 (97.8) | 0.0290 | 130 (51.6) | 223 (91.0) | <.0001 | – | – | – |
| Talk to my doctor about genetic testing.a | – | – | – | – | – | – | 177 (46.2) | 249 (69.8) | <.0001 |
| Talk about gynecologic cancer with my family.a | – | – | – | – | – | – | 285 (68.5) | 338 (84.5) | <.0001 |
| Talk about gynecologic cancer with my friends.a | – | – | – | – | – | – | 300 (71.3) | 336 (84.2) | <.0001 |
| Bring up gynecologic cancer the next time I visit my healthcare provider.a | – | – | – | – | – | – | 303 (72.3) | 340 (87.4) | <.0001 |
| Look for more information on gynecologic cancer.a | 320 (75.5) | 351 (86.9) | <.0001 | ||||||
| Talk to my doctor about gynecologic cancer.b | 365 (77.8) | 399 (90.3) | <.0001 | ||||||
| Talk to my doctor about symptoms I may be having.b | 361 (78.1) | 376 (86.6) | 0.0009 | ||||||
p < 0.05 from Chi-square tests or Fisher’s exact test
% Somewhat likely, extremely likely
% Somewhat confident, extremely confident
Table 3 also shows public behavioral intentions and confidence with talking to their providers, friends, and family about ovarian cancer information before and after facilitated discussions of Inside Knowledge materials. After sessions, public participants reported significant increases in their confidence surrounding talking to their providers and family about gynecologic cancer, including their ability to talk to their doctor about genetic testing (69.8% agreement), talk about gynecologic cancer with their family (84.5% agreement), and talk about gynecologic cancer with their friends (84.2% agreement). Public participants also reported significant increases in their intentions to bring up gynecologic cancer the next time they visit their healthcare provider (87.4% agreement), look for more information on gynecologic cancer (86.9% agreement), talk to their doctor about gynecologic cancer (90.3%), and talk to their doctor about symptoms they may be having (86.6%).
Discussion
After facilitated discussions of Inside Knowledge materials, correct knowledge of ovarian cancer information increased for participants. Women were more confident with their ability to talk to their providers about gynecologic cancer and expressed positive intentions about discussing gynecologic cancer with families, friends, and doctors after participation. For several survey items, we found significant differences in knowledge across sites for both public and provider sessions. Women attending sessions in Wisconsin and Tennessee and providers in Puerto Rico and New Jersey tended to score lower on knowledge questions. For example, providers and women in Wisconsin and Puerto Rico were less aware that women with Ashkenazi Jewish ancestry are at increased risk for ovarian cancer. Additionally, similar to previous studies, obstetrician/gynecologists had higher baseline knowledge of ovarian cancer, but knowledge increased among all provider groups after facilitated discussions [15].
The Inside Knowledge campaign is the only campaign related to ovarian cancer that is national in scope, and its web site is consistently the most visited CDC cancer site, suggesting the need for gynecologic cancer information. In 2015 alone, these webpages received 3,732,892 visits [15]. Because of the need for this information, the campaign is currently ongoing, with media advertisements and information available to the public on the campaign website. Public health campaigns like Inside Knowledge are considered to be an effective tool by The Guide to Community Preventive Services. Many past campaigns have been used to improve awareness or promote healthy behaviors for a variety of diseases [16]. A campaign to increase awareness of symptoms associated with acute HIV infection utilizing symptom cards, print media, and targeted billboard advertising increased HIV symptom recognition [17]. Similar strategies are also being used to increase testing for hepatitis C in people born between 1945 and 1965 [18]. Antismoking campaigns using television advertising, such as the National Truth Campaign and CDC’s Tips from Former Smokers, have resulted in decreased smoking initiation, increased quit attempts [19, 20]. CDC’s Screen for Life: National Colorectal Cancer Action Campaign and the African American Women and Mass Media campaign to promote breast cancer screening are additional examples of where multimedia efforts have been used successfully to promote knowledge and behavior change [21, 22]. Similarly, this evaluation points to the success of the Inside Knowledge campaign to increase knowledge of ovarian cancer information.
Some findings point to the need to reinforce certain messages in the Inside Knowledge campaign, including clarifying the types of cancers that are HPV-associated, emphasizing abnormal bleeding as a symptom, and Ashkenazi Jewish heritage as a risk factor for ovarian cancer. In particular, even though obstetrician/gynecologists had increased baseline ovarian cancer knowledge, many failed to identify abnormal bleeding as a symptom, indicating that even this group could benefit from improved educational materials. While campaign messages likely will evolve over time, our study found overall that current Inside Knowledge materials are effective at increasing knowledge among providers and their patients.
Since there are no effective prevention or early detection methods for ovarian cancer, education may help affect cancer incidence and mortality. Further, there is a wider call for community and clinical practice linkages, and utilization of Inside Knowledge materials by the public and providers helps build these much needed linkages for ovarian cancer [23]. Because these materials are available on the Internet, free to download and print or order in hard copy, providers can have them in their offices and disseminate them to patients.
The knowledge gained from education on this topic can empower women to take greater control of their health and allow them to be more engaged patients, which can lead to improved self-management of their care and improve the relationship with their providers [24]. Providers can use this information to inform how they interact with patients on the topic of ovarian cancer and share the materials with their patients. These are important steps towards improving ovarian cancer awareness and related positive behaviors, such as women recognizing ovarian cancer symptoms and proactively seeking medical care. NCCCP grantees can also address ovarian cancer through additional avenues, such as collaborating with cancer control partners, developing position papers, promoting use of family history to identify those at increased risk, and encouraging referrals to gynecologic oncologists for specialized care.
Our analysis was subject to several limitations. For brevity, providers were only asked about the two most common symptoms of ovarian cancer, limiting our assessment of changes in their understanding of symptoms. Social desirability bias could also have affected answers of all participants to questions related to their behavioral intentions and confidence, causing them to overstate their agreement with statements presented. Finally, missing data varied among grantee datasets, potentially biasing our results if non-respondents would have answered items differently than respondents who answered all survey items. Study strengths include its design according to standard knowledge/behavioral theories, the inclusion of women from all races, including Asian/Pacific Islander and American Indian/Alaska Native from diverse areas of the United States, and the innovative and unique use of NCCCP (those engaged in the community) to identify and recruit participants to the sessions.
Conclusions
Ovarian cancer awareness, provider confidence in talking to patients about ovarian cancer, and confidence of women in talking to providers, family, and friends about gynecologic cancer, and related behaviors increased in women and providers using Inside Knowledge campaign materials. Using Inside Knowledge materials to increase knowledge could ultimately lead to more empowered patients, better providerpatient communications, and ultimately earlier diagnosis and improved care for ovarian cancer.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Compliance with Ethical Standards CDC determined that this study constituted public health practice and did not require Institutional Review Board (IRB) review. OMB reviewed and approved all data collection aspects of this study, including the questionnaires. Per OMB regulations, informed consent was obtained from all participants, and all questionnaires contained the OMB approval number 0920-0800.
Conflict of Interest The authors declare that they have no conflicts of interest.
Financial Disclosure No financial disclosures were reported by the authors of this paper.
References
- 1.Ryerson AB, et al. Annual Report to the Nation on the Status of Cancer, 1975–2012, featuring the increasing incidence of liver cancer. Cancer. 2016;122(9):1312–1337. doi: 10.1002/cncr.29936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.U.S. Cancer Statistics Working Group. United States Cancer Statistics: 1999–2012 Incidence and Mortality Web-based Report. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; 2015. Available at: www.cdcgov/uscs (accessed on December 1, 2015). 2015. [Google Scholar]
- 3.Weir HK, et al. The past, present, and future of cancer incidence in the United States: 1975 through 2020. Cancer. 2015;121(11):1827–1837. doi: 10.1002/cncr.29258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.U.S. Preventive Services Task Force. Screening for ovarian cancer. 2012 Retrieved from http://www.uspreventiveservicestaskforce.org/uspstf/uspsovar.htm.
- 5.Ebell MH, Culp MB, Radke TJ. A Systematic Review of Symptoms for the Diagnosis of Ovarian Cancer. Am J Prev Med. 2016;50(3):384–394. doi: 10.1016/j.amepre.2015.09.023. [DOI] [PubMed] [Google Scholar]
- 6.Jelovac D, Armstrong DK. Recent progress in the diagnosis and treatment of ovarian cancer. CA Cancer J Clin. 2011;61(3):183–203. doi: 10.3322/caac.20113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rim SH, et al. A national initiative for women and healthcare providers: CDC’s Inside Knowledge: Get the Facts About Gynecologic Cancer campaign. J Women’s Health. 2011;20(11):1579–1585. doi: 10.1089/jwh.2011.3202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Major A, Stewart SL. Celebrating 10 years of the National Comprehensive Cancer Control Program, 1998 to 2008. Prev Chronic Dis. 2009;6(4):A133. [PMC free article] [PubMed] [Google Scholar]
- 9.Rochester PW, et al. Comprehensive cancer control: progress and accomplishments. Cancer Causes Control. 2010;21(12):1967–1977. doi: 10.1007/s10552-010-9657-8. [DOI] [PubMed] [Google Scholar]
- 10.Hayden JA. In: Introduction to Health Behavior Theory. Jones and Bartlett Learning, editor. Burlington, MA: 2014. [Google Scholar]
- 11.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 12.Azjen I. The theory of planned behavior. Org Behav Hum Decis Process. 1991;50(2):179–211. [Google Scholar]
- 13.Hochbaum GM. In: Public Participation in Medical Screening Programs: A Socio-Psychological Study. Public Health Service, editor. US Government Printing Office; Washington, DC: p. 1958. [Google Scholar]
- 14.Cooper CP, et al. Promoting gynecologic cancer awareness at a critical juncture-where women and providers meet. J Cancer Educ. 2014;29(2):247–251. doi: 10.1007/s13187-013-0580-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Inside Knowledge: Get the Facts About Gynecologic Cancer: 2015 YEAR-END REPORT. 2015 [Google Scholar]
- 16.Robinson MN, et al. Mass media health communication campaigns combined with health-related product distribution: a community guide systematic review. Am J Prev Med. 2014;47(3):360–371. doi: 10.1016/j.amepre.2014.05.034. [DOI] [PubMed] [Google Scholar]
- 17.Stekler JD, et al. ru2hot?: A public health education campaign for men who have sex with men to increase awareness of symptoms of acute HIV infection. Sex Transm Infect. 2013;89(5):409–414. doi: 10.1136/sextrans-2012-050730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jorgensen C, Carnes CA, Downs A. “Know More Hepatitis:” CDC’s National Education Campaign to Increase Hepatitis C Testing Among People Born Between 1945 and 1965. Public Health Rep. 2016;131(Suppl 2):29–34. doi: 10.1177/00333549161310S205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McAfee T, et al. Effect of the first federally funded US antismoking national media campaign. Lancet. 2013;382(9909):2003–2011. doi: 10.1016/S0140-6736(13)61686-4. [DOI] [PubMed] [Google Scholar]
- 20.Farrelly MC, et al. The Influence of the National truth campaign on smoking initiation. Am J Prev Med. 2009;36(5):379–384. doi: 10.1016/j.amepre.2009.01.019. [DOI] [PubMed] [Google Scholar]
- 21.Ekwueme DU, et al. Analysis of the benefits and costs of a national campaign to promote colorectal cancer screening: CDC’s screen for life-national colorectal cancer action campaign. Health Promot Pract. 2014;15(5):750–758. doi: 10.1177/1524839913519446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hall IJ, et al. The African American Women and Mass Media campaign: a CDC breast cancer screening project. J Women’s Health. 2012;21(11):1107–1113. doi: 10.1089/jwh.2012.3903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krist AH, et al. Clinical and community delivery systems for preventive care: an integration framework. Am J Prev Med. 2013;45(4):508–516. doi: 10.1016/j.amepre.2013.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carman KL, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff (Millwood) 2013;32(2):223–231. doi: 10.1377/hlthaff.2012.1133. [DOI] [PubMed] [Google Scholar]


