Abstract
Objective
This study aimed to evaluate swallowing dysfunction in patients with spinal and bulbar muscular atrophy and to identify the most appropriate method of assessing swallowing dysfunction using a videofluoroscopic swallowing study.
Methods
In the videofluoroscopic swallowing study, patients were instructed to swallow 3 mL of 40% weight/volume barium sulfate twice, and the pharyngeal residue was measured. We used three different methods to quantify the pharyngeal barium residue and an eight-point scale to evaluate the laryngeal penetration leading to aspiration pneumoniae.
Patients
We assessed 111 patients with spinal and bulbar muscular atrophy who weren't undergoing disease-specific treatment.
Results
Our results showed that the pharyngeal barium residue after initial swallowing correlated better with the bulbar-related functional rating scales than that after multiple deglutition. This correlation was vague when the data from patients whose barium residue was >50% were eliminated. In addition, evaluating the pharyngeal residue after initial swallowing proved to be the most sensitive method with regard to laryngeal penetration.
Conclusion
This study showed that the pharyngeal barium residue after initial swallowing was the most appropriate parameter for quantitatively assessing the degree of dysphagia using a videofluoroscopic swallowing study and suggests that this method may predict laryngeal penetration and aspiration in patients with spinal and bulbar muscular atrophy.
Keywords: spinal and bulbar muscular atrophy, swallowing dysfunction, motor neuron disease, pharyngeal barium residue, videofluoroscopic swallowing study
Introduction
Spinal and bulbar muscular atrophy (SBMA), also known as Kennedy's disease, is an adult-onset, hereditary neuromuscular disease characterized by muscle atrophy, weakness, contraction fasciculation, and bulbar involvement (1-3). The progression of neurological deficits is usually slow in patients with SBMA, with the average interval between the onset of symptoms and death being approximately 20 years (4). Bulbar palsy occurs in almost all patients with SBMA, and the incidence rate of aspiration pneumonia is high in advanced cases. Indeed, a previous study on the natural history of SBMA revealed that, of the 15 patients who died during the study, pneumonia was identified as the cause of death in 8 (4). Therefore, the degree of bulbar palsy is an essential factor that defines the prognosis of patients with SBMA, as it directly causes life-threatening aspiration pneumonia.
To evaluate the degree of dysphagia, spatial analyses of a videofluoroscopic swallowing study (VFSS) is a useful tool. One of the most important findings of the VFSS in patients with SBMA is the presence of pharyngeal barium residue (5,6). Barium residue in the pharynx indicates that some barium remains in the throat without being swallowed; this is the most frequent pathological finding directly connected with aspiration. However, the optimum procedure for measuring the pharyngeal barium residue has not been established for patients with SBMA.
Therefore, in this study, we aimed to evaluate swallowing dysfunction in patients with SBMA using a VFSS. We also attempted to determine the most appropriate procedure for measuring pharyngeal barium residue for the assessment of swallowing dysfunction.
Materials and Methods
Patient population
A total of 111 patients with clinical and genetic diagnoses of SBMA were recruited. All of the patients with SBMA underwent VFSS at Nagoya University Hospital from August 2003 to September 2010. We also evaluated the patients' backgrounds and physical function at the time of the VFSS. None of the subjects had undergone treatment with leuprorelin acetate or other similar drugs at the time of the VFSS.
Outcome measures
VFSS and penetration aspiration score (PAS)
During the VFSS, the patients were instructed to swallow 3 mL of 40% weight/volume (w/v) barium sulfate twice in a standing position and were viewed in the lateral plane. The irradiation area was confined to the oral, pharyngeal, laryngeal, and upper esophageal areas to avoid unnecessary irradiation exposure. Each swallow was recorded at least 20 seconds after the initial swallowing. The VFSS data were recorded on a Mini DV digital video tape (Sony, Japan) at 30 frames per second. All of the quantitative parameters were measured by 2 independent evaluators who had been blinded to the subjects' backgrounds in accordance with standard procedures (7,8). Representative VFSS data are shown in Fig. 1.
Figure 1.
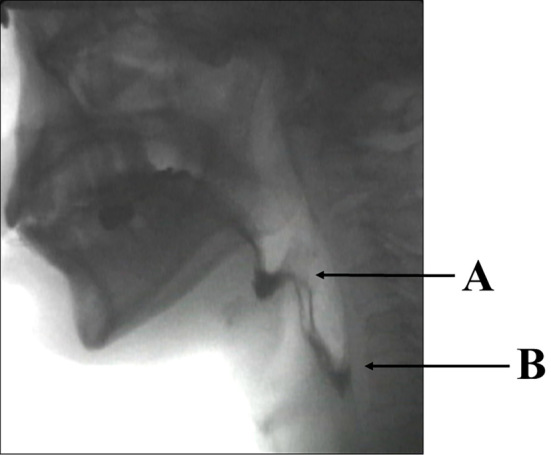
A representative result of a videofluoroscopic swallowing study (VFSS). The pharyngeal barium residue is the total amount pooling in the epiglottic vallecular (A) and piriform recess (B).
The quantitative findings were evaluated using Logemann's videofluorographic examination, in which the pharyngeal barium residue is defined by the incomplete clearance of the bolus in many location of the pharynx such as vallecular space, pyriform sinus, and pharyngeal posterior wall. The two evaluators discussed and agreed on the details of the definitions of the VFSS findings before performing the measurement in accordance with previously described definitions (9). In the present study, the pharyngeal residue was measured using a semi-quantitative scale: 0%, 2%, 5%, 10%, 20%, 30%, 40%, 50%, 60%, 70%, 80%, 90%, 100%. These figures mean the percentage of the pharyngeal residue in the total amount of barium the subjects swallowed (3 mL). The pharyngeal residue was only measured following swallowing of the first 3 mL of barium because the value of the first residue directly affects the value of the second residue.
Two methods for interpreting radiograms have been proposed for the measurement of the pharyngeal barium residue in order to assess swallowing dysfunction in patients with SBMA (6). The first method, known as the multiple deglutition (MD) method, measures the pharyngeal barium residue after piecemeal deglutition; this is because multiple repeated swallowing is frequently observed in patients with SBMA who attempt to empty a bolus from the oral cavity. The second method, the initial swallowing (IS) method, measures the pharyngeal barium residue after initial swallowing even if the swallowing was multiple deglutition, because the initial swallowing is thought to reflect the patients' swallowing function directly (7). In cases where the pharyngeal barium residue after initial swallowing is >50%, the residue values may be chance findings and not precisely reflective of the subject's swallowing function, as patients with SBMA often fail to swallow the barium on the first swallow of a multiple repeated swallowing; they often efficiently swallow the barium on the second or later swallow. Therefore, we also used the modified IS method, which excluded the data from cases with >50% residue after the initial swallow from the analysis. Accordingly, to evaluate the pharyngeal barium residue, we used three assessment methods: the MD, IS, and modified IS methods.
For aspiration and penetration findings, which are important indicators of aspiration pneumoniae (10,11), we used the eight-point scale PAS (12) to describe penetration and aspiration events. The scores are primarily determined by the depth to which material passes into the airway and by whether or not material entering the airway is expelled (with a score of 8 indicating the worst aspiration). Acceptable intra- and inter-rater reliability for the scale have been established, which is sufficient to support its introduction into clinical practice (12). The absence of the laryngeal penetration was defined as a rating of 1 point by either evaluator; 2 or more points indicated that the materials entered the airway (12). The mean score of the two raters was adopted. We evaluated the PAS independently from the barium residue, as it was same regardless of the method used (MD, IS, and modified IS methods).
Motor function score
At the time of the VFSS, we measured the Revised Amyotrophic Lateral Sclerosis Functional Rating Scale (ALSFRS-R) bulbar-related items and the Norris Bulbar score (NBS).
The ALSFRS is a validated questionnaire-based scale that measures the physical function while performing activities of daily living in patients with ALS (13). The ALSFRS-R was introduced to correct for the disproportionate weighting of limb and bulbar symptoms compared with respiratory dysfunction. The ALSFRS-R was translated into Japanese and validated (14). The ALSFRS-R consists of five domains: three bulbar-related items (speech, salivation, and swallowing), two upper limb-related items (handwriting, and cutting food and handling utensils), two trunk-related items (dressing and hygiene, and turning in bed and adjusting the bed clothes), two lower limb-related items (walking and climbing stairs), and three respiration-related items (dyspnea, orthopnea, and respiratory insufficiency).
The Modified Norris Scale is another rating scale for ALS, which consists of two parts: the Limb Norris Score and the Norris Bulbar Score. The Limb Norris Score has 21 items to evaluate limb function, and the Norris Bulbar Score has 13 items to assess bulbar function. Each item is rated in 4 ordinal categories; therefore, the best possible scores are 63 and 39, respectively. The original version was translated into Japanese and validated (15).
Genetic analysis
We extracted genomic DNA from the peripheral blood of patients with SBMA using conventional techniques. We carried out polymerase chain reaction (PCR) amplification of the CAG repeat in the androgen receptor gene (AR) using a fluorescent-labeled forward primer (5'-TCCAGAATCTGTTCCAGAGGTGC-3') and an unlabeled reverse primer (5'-TGGCCTCGCTCAGGATGTCTTTAAG-3'). The details of the PCR conditions have been described previously (16). Aliquots of the PCR products were combined with loading dye and separated by electrophoresis using an autoread sequencer (SQ-5500; Hitachi Electronics Engineering, Tokyo, Japan). The size of the PCR standard was determined by direct sequencing, as described previously (16).
Statistical analyses
Statistical analyses were performed with the IBM SPSS Statistics software program, version 23.0 (IBM Japan, Tokyo, Japan). Descriptive variables, such as the mean, standard deviation (SD), and range, were used to summarize the quantitative measures. The relationship between two values was calculated using Spearman's correlation coefficient.
Ethics
This study was conducted in accordance with the Declaration of Helsinki. All patients provided their written informed consent to participate in this study and in the genetic analyses. The participants were free to withdraw from the study at any time for any reason. The Ethics Committee of Nagoya University Graduate School of Medicine approved the study. Confidentiality was ensured by assigning a study code to each participant. All studies conformed to the Ethics Guidelines for Human Genome/Gene Analysis Research and the Ethics Guidelines for Epidemiological Studies endorsed by the Japanese government.
Results
Patient characteristics
A total of 111 patients with SBMA were included (Table 1). The characteristics of the study population, such as the age at onset, age at the first evaluation, and CAG repeat length in the AR gene, were similar to those of previous studies (4,6,17). The clinical, biochemical, and hormonal profiles are also shown in Table 1. The features of these profiles were also similar to those in previous studies.
Table 1.
Clinical and Genetic Features of 111 Patients with Spinal and Bulbar Muscular Atrophy (SBMA) at Baseline.
| Demographics | Mean ± SD (range) |
|---|---|
| Age at first evaluation (years) | 53.2 ± 10.4 (27–81) |
| Disease duration (years) | 11.0 ± 8.0 (1–57) |
| Age at onset (years) | 42.2 ± 11.8 (8–68) |
| CAG repeat length in the AR gene (number) | 48.2 ± 3.4 (40–57) |
| Functional parameters | Mean ± S.D. (range) |
| ALSFRS-R bulbar-related items | 10.6 ± 1.5 (5–12) |
| NBS | 33.5 ± 4.2 (20–39) |
| Biochemical and hormonal parameters | Mean ± S.D. (range) |
| Creatine kinase (IU/L) | 846 ± 493 (100–2,132) |
| Testosterone (μg/dL) | 6.96 ± 2.55 (2.24–17.82) |
ALSFRS-R: Revised Amyotrophic Lateral Sclerosis Functional Rating Scale, LNS: Limb Norris Score, NBS: Norris Bulbar Score, AR: Androgen Receptor, SD: Standard Deviation
Statistical summary of the VFSS data
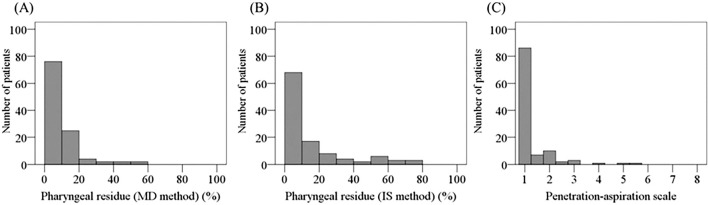
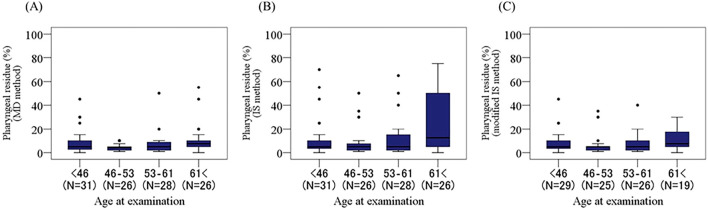
The distribution of the pharyngeal barium residue measured by two different methods (the MD and IS methods) and that of the penetration-aspiration score are shown in Fig. 2 and Table 2. Fig. 3 shows the pharyngeal barium residue in relation to the age at the examination using boxplots. The age at the examination was divided into four quartiles. These figures indicated that the amount of pharyngeal residue increased with the age at the examination when the IS method, but not the MD or modified IS method, was used.
Figure 2.
The distribution of the pharyngeal residue and the penetration-aspiration scale in patients with spinal and bulbar muscular atrophy (SBMA). The penetration-aspiration scale (C). The pharyngeal barium residue was evaluated by two proposed methods, the multiple deglutition method (MD) method (A), and the initial swallowing (IS) method (B).
Table 2.
Statistical Summary of Pharyngeal Residue and the Penetration-aspiration Scale.
| Pharyngeal residue (IS method) | Pharyngeal residue (MD method) | Penetration-aspiration scale | |
|---|---|---|---|
| Mean ± SD (%) | 14.0 ± 18.2 | 8.0 ± 9.6 | 1.3 ± 0.8 |
| (Range, %) | (0–75) | (0–55) | (1.0–5.5) |
| Skewness | 1.88 ± 0.23 | 3.12 ± 0.23 | 3.47 ± 0.23 |
| Kurtosis | 2.56 ± 0.46 | 10.69 ± 0.46 | 13.84 ± 0.46 |
Figure 3.
Boxplots of the pharyngeal barium residue by the age at the examination. The pharyngeal barium residue increased with the age at the examination when we used the IS method (B), which measures the residue after initial swallowing, but not when we used the MS method (A), which measures the residue after piecemeal deglutition, or the modified IS method (C), which excludes the data from patients whose residue is >50% when using the IS method.
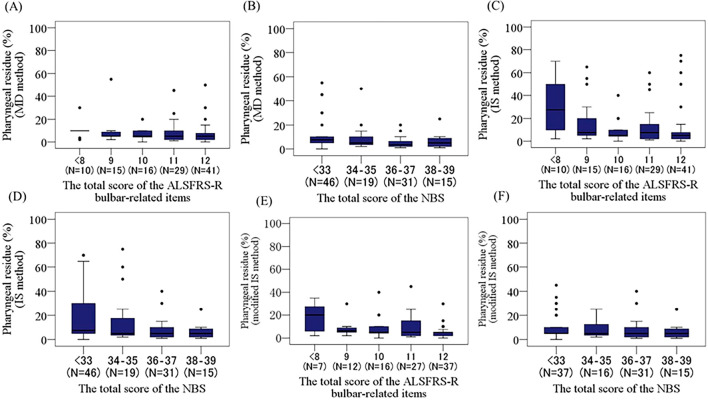
Boxplots of the pharyngeal barium residue by the swallowing function severity as measured by the swallowing functional rating scales
The boxplots in Fig. 4 illustrate the relationship between the pharyngeal barium residue quantified using three methods (MD, IS, and modified IS) and the severity of dysphagia measured by the swallowing functional rating scales. The total scores of the 3 ALSFRS-R bulbar-related items were divided into 5 categories (0-8, 9, 10, 11, and 12), and those of the NBS were divided into 4 categories (0-33, 34-35, 36-37, and 38-39). When we compared the findings among the measurement methods, the pharyngeal barium residue measured by the IS method correlated best with swallowing dysfunction evaluated by the swallowing functional rating scales (r=-0.243, p=0.010 with the ALSFRS-R bulbar-related items: r=-0.299, p=0.001 with the NBS).
Figure 4.
Boxplots of the pharyngeal barium residues by the swallowing function severity measured by the swallowing functional rating scales, the ALSFRS-R (A, C, E), and the NBS (B, D, E). The pharyngeal barium residue correlated well with swallowing dysfunction as evaluated by the functional rating scales when we employed the IS method, which measures the residue after initial swallowing.
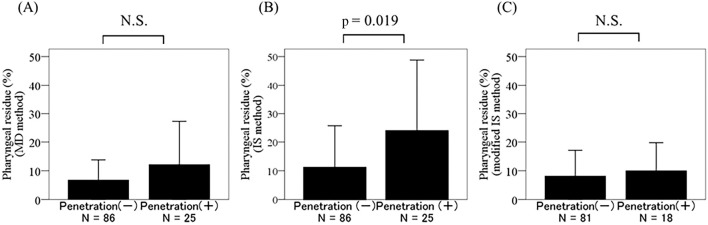
A comparison of the pharyngeal barium residue between patients with and without penetration
We then investigated which of the three pharyngeal barium residue measurement methods best reflected barium penetration into the larynx, as laryngeal penetration directly leads to aspiration pneumoniae (10,11) (Fig. 5). The results demonstrated a statistically significant difference between patients with and without penetration only using the IS method, not the MD or modified IS method, suggesting that the pharyngeal barium residue measured by the IS method is the most appropriate index for predicting aspiration or risk of aspiration in patients with SBMA.
Figure 5.
Comparison of pharyngeal barium residues between patients with and without penetration. A statistically significant difference was seen only when we used the initial swallowing (IS) method (B), which measures the residue after initial swallowing.
Discussion
Progressive dysphagia is a serious symptom in patients with SBMA and directly leads to fatal aspiration pneumonia (4). Patients with SBMA may have overt or subclinical bulbar palsy, even if their limb and truncal symptoms are mild (18,19). Therefore, an appropriate method for quantitatively evaluating dysphasia is crucial for clinical SBMA research. The most appropriate quantitative assessment for aspiration risk is expected to be correlated with aspiration frequency. In this respect, the pharyngeal barium residue is an important predictor of aspiration pneumonia, as it correlates well with aspiration frequency (20,21). However, no methods of evaluating the pharyngeal barium residue have been established for use in patients with SBMA. In this study, the pharyngeal barium residue was evaluated two-dimensionally using VFSS. Although the residue should be assessed three-dimensionally, since the actual residue is distributed three-dimensionally, a two-dimensional VFSS may thus be useful as a method of evaluating swallowing dysfunction (22). Therefore, in the present study, we used a two-dimensional VFSS to assess the pharyngeal residue.
In this study, we aimed to identify the most appropriate method for assessing the pharyngeal barium residue by comparing three evaluation methods: MD, IS, and modified IS. Our study results suggested that the IS method was the most appropriate way of evaluating swallowing dysfunction. The pharyngeal barium residue in patients with laryngeal penetration was significantly higher than in those without laryngeal penetration when the residue was evaluated by the IS method. In contrast, there were no marked differences between the patients with and without laryngeal penetration when we used the MD or modified IS method. It is important to use measurements that are strongly correlated with laryngeal penetration because the degree of penetration has been identified as a significant risk factor for developing aspiration pneumonia (23,24).
Previous studies have also indicated that the IS method is the best for evaluating patients' swallowing disability, as this method directly reflects the total swallowing function (5,6,9,21). The MD method, by contrast, has potential drawbacks. First, the MD method may overestimate the swallowing function because it evaluates the barium residue only after the patient has swallowed multiple times. Second, evaluating piecemeal deglutition may differ among raters in the MD method. Third, multiple deglutitions might compensate for the initial swallowing and might not reflect the patient's true swallowing function.
One limitation of the present study is that the barium residue was evaluated two-dimensionally, not three-dimensionally. Although the two-dimensional evaluation of barium residue in the VFSS is a practical, established method, the reliability of which has been confirmed (22), a novel imaging technique needs to be developed for a precise assessment of swallowing, in addition to the refinement of the evaluation methods we discussed.
In conclusion, this study revealed that the IS method was the most appropriate way to assess the degree of dysphagia quantitatively using VF and suggests that this method may predict laryngeal penetration and aspiration pneumonia in patients with SBMA.
The authors state that they have no Conflict of Interest (COI).
Financial Support
This study was supported by Grant-in-Aids (KAKENHI) from the MEXT, Japan (Nos.26293206, 26670440, 26670439, and 16K15480), grants from MHLW, Japan, the Project Promoting Clinical Trials for Development of New Drugs and Medical Devices (Japan Medical Association) from Japan Agency for Medical Research and development (AMED), and research grants from AMED (Nos. 15ek0109025 and 15ek0109165).
Atsushi Hashizume and Haruhiko Banno contributed equally to this work.
Acknowledgement
We acknowledge and thank all patients and their families for participating in this study.
References
- 1. Kennedy WR, Alter M, Sung JH. Progressive proximal spinal and bulbar muscular atrophy of late onset. A sex-linked recessive trait. Neurology 18: 671-680, 1968. [DOI] [PubMed] [Google Scholar]
- 2. Sperfeld AD, Karitzky J, Brummer D, et al. . X-linked bulbospinal neuronopathy: Kennedy disease. Arch Neurol 59: 1921-1926, 2002. [DOI] [PubMed] [Google Scholar]
- 3. Sobue G, Hashizume Y, Mukai E, Hirayama M, Mitsuma T, Takahashi A. X-linked recessive bulbospinal neuronopathy. A clinicopathological study. Brain 112: 209-232, 1989. [DOI] [PubMed] [Google Scholar]
- 4. Atsuta N, Watanabe H, Ito M, et al. . Natural history of spinal and bulbar muscular atrophy (SBMA): a study of 223 Japanese patients. Brain 129: 1446-1455, 2006. [DOI] [PubMed] [Google Scholar]
- 5. Banno H, Katsuno M, Suzuki K, et al. . Phase 2 trial of leuprorelin in patients with spinal and bulbar muscular atrophy. Ann Neurol 65: 140-150, 2009. [DOI] [PubMed] [Google Scholar]
- 6. Katsuno M, Banno H, Suzuki K, et al. . Efficacy and safety of leuprorelin in patients with spinal and bulbar muscular atrophy (JASMITT study): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet Neurol 9: 875-884, 2010. [DOI] [PubMed] [Google Scholar]
- 7. Logemann JA, Kahrilas PJ, Kobara M, Vakil NB. The benefit of head rotation on pharyngoesophageal dysphagia. Arch Phys Med Rehabil 70: 767-771, 1989. [PubMed] [Google Scholar]
- 8. Logemann JA, Pauloski BR, Rademaker AW, Colangelo LA, Kahrilas PJ, Smith CH. Temporal and biomechanical characteristics of oropharyngeal swallow in younger and older men. J Speech Lang Hear Res 43: 1264-1274, 2000. [DOI] [PubMed] [Google Scholar]
- 9. Logemann JA. In: Evaluation and treatment of swallowing disorders. 2nd edition PRO-ED, Inc., Austin, TX, 1998: . [Google Scholar]
- 10. Takahashi N, Kikutani T, Tamura F, Groher M, Kuboki T. Videoendoscopic assessment of swallowing function to predict the future incidence of pneumonia of the elderly. J Oral Rehabil 39: 429-437, 2012. [DOI] [PubMed] [Google Scholar]
- 11. Pikus L, Levine MS, Yang YX, et al. . Videofluoroscopic studies of swallowing dysfunction and the relative risk of pneumonia. 180: 1613-1616, 2003. [DOI] [PubMed] [Google Scholar]
- 12. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia 11: 93-98, 1996. [DOI] [PubMed] [Google Scholar]
- 13. The ALS CNTF treatment study (ACTS) phase I-II Study Group The amyotrophic lateral sclerosis functional rating scale. Assessment of activities of daily living in patients with amyotrophic lateral sclerosis. Arch Neurol 53: 141-147, 1996. [PubMed] [Google Scholar]
- 14. Ohashi Y, Tashiro K, Itoyama Y, et al. . Study of functional rating scale for amyotrophic lateral sclerosis: revised ALSFRS (ALSFRS-R) Japanese version. No To Shinkei (in Japanese, Abstract in English) 53: 346-355, 2001. [PubMed] [Google Scholar]
- 15. Oda E, Ohashi Y, Tashiro K, Mizuno Y, Kowa H, Yanagisawa N. Reliability and factorial structure of a rating scale for amyotrophic lateral sclerosis. No To Shinkei 53: 346-355, 2001(in Japanese, Abstract in English). [PubMed] [Google Scholar]
- 16. Doyu M, Sobue G, Mukai E, et al. . Severity of X-linked recessive bulbospinal neuronopathy correlates with size of the tandem CAG repeat in androgen receptor gene. Ann Neurol 32: 707-710, 1992. [DOI] [PubMed] [Google Scholar]
- 17. Fernández-Rhodes LE, Kokkinis AD, White MJ, et al. . Efficacy and safety of dutasteride in patients with spinal and bulbar muscular atrophy: a randomised placebo-controlled trial. Lancet Neurol 10: 140-147, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Warnecke T, Oelenberg S, Teismann I, et al. . Dysphagia in X-linked bulbospinal muscular atrophy (Kennedy disease). Neuromuscul Disord 19: 704-708, 2009. [DOI] [PubMed] [Google Scholar]
- 19. Mano T, Katsuno M, Banno H, et al. . Tongue pressure as a novel biomarker of spinal and bulbar muscular atrophy. Neurology 82: 255-262, 2014. [DOI] [PubMed] [Google Scholar]
- 20. Eisenhuber E, Schima W, Schober E, et al. . Videofluoroscopic assessment of patients with dysphagia: pharyngeal retention is a predictive factor for aspiration. AJR Am J Roentgenol 178: 393-398, 2002. [DOI] [PubMed] [Google Scholar]
- 21. Logemann JA, Williams RB, Rademaker A, Pauloski BR, Lazarus CL, Cook I. The relationship between observations and measures of oral and pharyngeal residue from videofluorography and scintigraphy. Dysphagia 20: 226-231, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chaves Rde D, Mangilli LD, Sassi FC, et al. . Two-dimensional perceptual videofluoroscopic swallowing analysis of the pharyngeal phase in patients older than 50 years. Arq Bras Cir Dig 26: 274-279, 2013. [DOI] [PubMed] [Google Scholar]
- 23. Pikus L, Levine MS, Yang YX, et al. . Videofluoroscopic studies of swallowing dysfunction and the relative risk of pneumonia. Am J Roentgenol 180: 1613-1616, 2003. [DOI] [PubMed] [Google Scholar]
- 24. Takahashi N, Kikutani T, Tamura F, Groher M, Kuboki T. Videoendoscopic assessment of swallowing function to predict the future incidence of pneumonia of the elderly. J Oral Rehabil 39: 429-437, 2012. [DOI] [PubMed] [Google Scholar]