Abstract
We report a case of liver abscess and portal vein thrombosis, which occurred due to diverticulitis at the terminal ileum in a 59-year-old man. The patient underwent a barium fluoroscopic examination 1 month before presenting to our hospital. He also showed liver dysfunction due to thrombosis at the superior mesenteric and portal veins. His inflammation gradually subsided after the initiation of treatment, but the recovery was not sufficient. Thus, surgery was performed. The patient condition improved after surgery and he was discharged. Barium examinations are relatively safe, but can sometimes cause severe adverse effects in patients with certain risk factors, and an appropriate diagnosis and treatment are necessary when symptoms appear.
Keywords: barium, liver abscess, diverticulitis, superior mesenteric vein thrombosis, portal vein thrombosis
Introduction
Barium fluoroscopy is in general use for cancer screening especially in Japan, and it is said to be a safe medical examination. There have been only few reports of serious adverse effects of barium fluoroscopy. Here, we describe 59-year-old male recovered from liver abscess and portal vein thrombosis due to ileal diverticulitis mediated by barium fluoroscopic examination.
Case Report
A 59-year-old Japanese man visited our hospital because of fatigue and loss of appetite, which had begun 3 days prior to his visit. He felt feverish, but showed specific symptoms. His vital signs on presentation were as follows: body temperature, 38.5℃; blood pressure, 154/75 mmHg; heart rate, 102 beats/min, respiration rate, 30 breaths/min, and SpO2, 100% on room air. The findings of physical examination were normal, with the exception of icteric conjunctiva and slight oppressive lower abdominal pain. His initial laboratory data suggested inflammation, a reduced platelets count, disseminated intravascular coagulation (DIC), and liver dysfunction. His full laboratory data are shown in Table.
Table.
Laboratory Data Obtained on Admission.
| Laboratory Data | |
|---|---|
| White blood cell count (per mm3) | 11,600 |
| Differential count (%) | |
| Neutrophils | 92 |
| Band forms | 7 |
| Lymphocytes | 5 |
| Atypical lymphocytes | 0 |
| Monocytes | 3 |
| Metamyelocytes | 0 |
| Eosinophils | 0 |
| Myelocytes | 0 |
| Red blood cell counts (*106 per mm3) | 4.46 |
| Hemoglobin (g/dL) | 14 |
| Hematocrit (%) | 39.6 |
| Platelets (*104 per mm3) | 6 |
| Prothrombin time (PT) (%) | 81 |
| PT-international normalized ratio (INR) | 1.12 |
| Activated partial thromboplastin time (APTT) (sec) | 32.4 |
| Fibrinogen (mg/dL) | 591 |
| Fibrinogen degradation product (FDP) (μg/dL) | 49.72 |
| D-dimer (μg/dL) | 13.86 |
| Anti-Thrombin III (%) | 74 |
| Protein C (%) | 44 |
| Protein S (%) | 74 |
| Blood urea nitrogen (mg/dL) | 22.3 |
| Creatinine (mg/dL) | 1.15 |
| C-reactive protein (mg/dL) | 21.7 |
| Total protein (g/dL) | 6.5 |
| Albumin (g/dL) | 2.8 |
| Na (mEq/L) | 132 |
| K (mEq/L) | 3.8 |
| Cl (mEq/L) | 96 |
| Total bilirubin (mg/dL) | 7.3 |
| Direct bilirubin (mg/dL) | 5.7 |
| ALP (U/L) | 754 |
| γ-GTP (U/L) | 413 |
| AST (U/L) | 71 |
| ALT (U/L) | 90 |
| LDH (U/L) | 261 |
| AMY (IU/L) | 119 |
| CK (U/L) | 156 |
| Glc (mg/dL) | 252 |
| HbA1c (%) | 6.6 |
| PCT (ng/mL) | 11.34 |
The patient’s laboratory data from admission shows inflammation, reduced platelets, disseminated intravascular coagulation, and liver dysfunction. γ-GTP: gamma-glutamyl transpeptidase, ALP: alkaline phosphatase, AST: aspartate aminotransferase, ALT: alanine aminotransferase, LDH: lactate dehydrogenase, AMY: amylase, CK: creatine kinase, Gl: glucose, PCT: procalcitonin
The plain chest and abdominal radiography results were normal with the exception of a high-density area in the lower right abdomen (Fig. 1). Abdominal echography revealed a low-echoic and mixed pattern of liver lesion (S8), cholecystolithiasis, and a gall bladder polyp (Fig. 2). A contrast-enhanced computed tomography (CT) scan of the abdomen showed superior mesenteric vein thrombosis (SMVT), portal vein thrombosis (PVT), a low-density liver lesion (S8), and a high-density foreign body at the terminal ileum with surrounding inflammatory reactions (Fig. 3).
Figure 1.
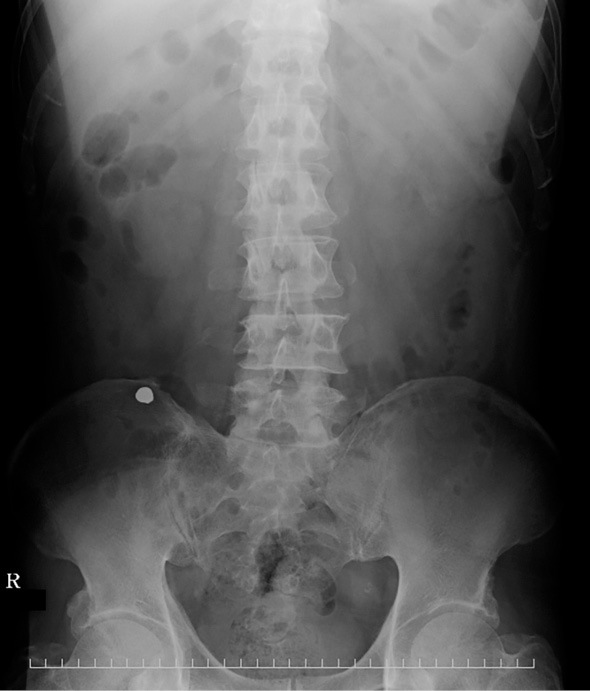
A plain abdominal radiograph shows a high-density area in the lower right abdominal area. The circular shape indicates that the object is artificial.
Figure 2.

Abdominal ultrasonography shows a low-echoic mixed area in the S8 liver lesion.
Figure 3.
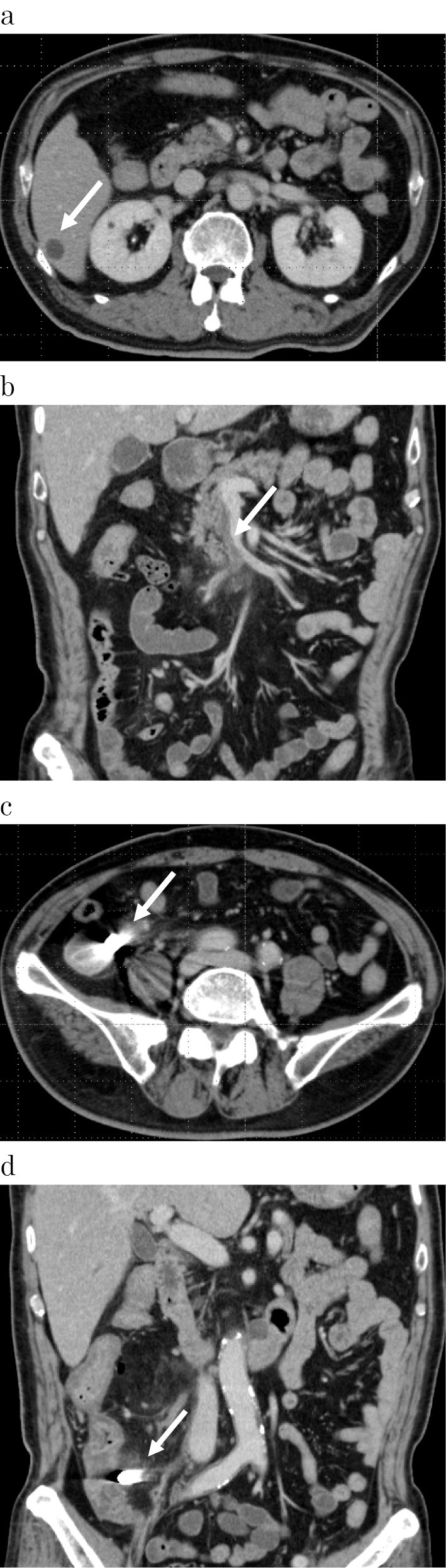
Contrast-enhanced computed tomography shows a low-density area in the S8 liver lesion (a), portal vein thrombosis (b), and the high-density area shown in Fig. 1 (c and d).
Based on these symptoms and data, the patient was diagnosed with SMVT, PVT, a low-density liver lesion, intraperitoneal infection, disseminated intravascular coagulation, and foreign bodies at the terminal ileum, and he was admitted to our hospital. Antibiotics treatment was initiated to treat the infection, heparin was administered to treat PVT, and recombinant-thrombomodulin treatment was initiated to treat DIC (Fig. 4). Meropenem was selected due to presence of sepsis and DIC.
Figure 4.

A schematic illustration showing the clinical progress of inflammation and liver dysfunction and treatment of the patient. CMZ: cefmetazole, CRP: C-reactive protein, CT: computed tomography, MEPM: meropenem, Plt: platelets, R-ThM: recombinant thrombomodulin, WBC: white blood cells. Heparin was started at a dose of 18,000 U/day and was finally increased to 20,000 U/day. Warfarin was started at a dose of 1.0 mg/day, and was increased by 1.0 mg/day until reaching a final dose of 3.0 mg/day. R-ThM was administered at a dose of 22,800 U/day for 5 days.
His medical history included a gastric ulcer, diabetes mellitus, atherothrombotic cerebral infarction, myocardial infarction, and hypertension. Approximately 10 days after his admission, he told us that he had undergone a barium fluoroscopic examination approximately 1 month prior to visiting our hospital. Thus, the foreign body at the terminal ileum was thought to be barium that he had ingested.
The medication was effective and his inflammation and laboratory data gradually improved, but the SMVT and PVT remained and warfarin therapy was started.
A blood culture showed the presence of Morganella morganii on the 5th day of hospitalization. We changed the antibiotic to cefmetazole in accordance with the blood culture susceptibility. Thrombomodulin was stopped because the blood coagulation test data normalized on that day.
However, the patient's inflammation did not subside completely. His C-reactive protein (CRP) concentration plateaued at around 3.0-5.0 mg/dL. We thought that the foreign body at the terminal ileum was the cause of the continued inflammation and performed colonoscopy on the 19th day of hospitalization. During endoscopy, mucosal redness was observed at the terminal ileum, and pus flowed from that area with scope stimulation. However, no barium mass was found (Fig. 5).
Figure 5.

An endoscopic image obtained at the terminal ileum shows mucosal redness and pus flowing from that area.
In spite of drainage with colonoscopy, the inflammation persisted. Contrast-enhanced CT on the 25th day revealed ring enhancement of the low-density liver lesion (S8), suggesting a liver abscess (Fig. 6). Drainage of the liver abscess was attempted on the 38th day of hospitalization, but no pus was suctioned.
Figure 6.

Contrast-enhanced computed tomography taken on the 25th day of hospitalization shows abscess-like ring enhancement in the S8 liver lesion.
Because inflammation remained, we decided to perform ileocecal resection to remove the abscess and the barium on the 48th day of hospitalization. The operation was performed safely, and the inflammation resolved. The patient left the hospital on the 63rd day of hospitalization. Warfarin was discontinued at 1 month after the operation.
A pathological specimen of the terminal ileum showed diverticulitis, inflammatory thickening of the intestinal tract wall, barium crystals, and granulomas around the diverticulum (Fig. 7).
Figure 7.

A resected histopathological specimen shows barium crystals [a: Hematoxylin and Eosin (H&E) staining ×400; and b: H&E staining ×400, polarization microscope] and granulomas around the diverticulum (c: H&E staining ×400; and d: H&E staining ×400, polarization microscope).
Discussion
Barium fluoroscopy is commonly used for routine medical examinations, especially in Japan. It is relatively safe, but some adverse effects have been reported. Intratracheal aspiration, hypersensitivity, intraabdominal leakage, intravasation, and gastrointestinal obstruction are the most commonly reported adverse effects. The intake of barium sometimes reported to cause intestinal perforation in 3 of 1,013,000 people (1). People who develop intestinal perforation usually have an underlying disease, such as cancer or diverticulum. In our case, the patient had diverticulitis. Medication was administered, but the inflammation persisted; thus surgery was performed. Although we could not detect perforation in the pathological specimens of the present case, an abscess was found and perforation or penetration was suspected. We attempted to treat the patient conservatively with medication for one and a half month, which led to a gradual improvement of the inflammation. If a perforation had been present, it is possible that the hole could have closed due to the effects of the medication. The removal of intraperitoneal barium should be performed in the early stages after the manifestation of symptoms because barium cannot be absorbed, and it can cause abscesses and granulomas due to long-term inflammation (2, 3).
Additionally, the patient in this case showed SMVT and PVT due to inflammation at the terminal ileum. The inflammation was so severe that liver abscess and dysfunction were apparent. SMVT and PVT are relatively rare, and 80% of cases are reported to have secondary causes, such as malignant tumor or trauma (4). Microorganisms are often observed in blood cultures in these cases (5). We could not find any other cases of SMVT and PVT due to a barium examination; thus the present case seemed to be a very rare case.
Diverticulum of the small intestine is a rare disease. Only 0.3-4.5% of autopsy cases show diverticulum of the small intestine that is not Meckel's diverticulum (5). Approximately 5-19% of diverticula of the small intestine cause perforation (6).
Although a severe inflammatory reaction occurred in the intraperitoneum, the patient in our case showed only slight lower abdominal pain, which may have been related to the position of the diverticulum. It was noted in one case report that only 63.4% of people with perforation of the small intestine report abdominal pain. There is also abundant mesentery near the terminal ileum around the intestinal diverticulum, which can serve as a breakwater. The mesentery also forms a bulkhead, and the inflamed tissue can repress the spread of inflammation (7).
In summary, barium fluoroscopy is a relatively safe examination, but it can sometimes cause severe adverse effects. If a patient presents with SMVT, PVT, and liver abscess, an early diagnosis is needed and the inflammation should be sufficiently controlled. Surgery may also be required in some cases.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Shibuya D, Konno Y, Aida S, Kato K, Shimada T. Complications of gastric mass screening by indirect fluororadiography. J Gastroenterol Cancer Screen 44: 251-258, 2006. [Google Scholar]
- 2. Zheutlin N, Lasser EC, Rigler LG. Clinical studies on effect of barium in the peritoneal cavity following rupture of the colon. Surgery 32: 967-979, 1952. [PubMed] [Google Scholar]
- 3. Nahrwold DL, Isch JH, Benner DA, Miller RE. Effect of fluid administration and operation on the mortality rate in barium peritonitis. Surgery 70: 778-781, 1971. [PubMed] [Google Scholar]
- 4. Fukutomi S, Yasutomi J, Kusashio K, Suzuki M, Fukao K, Miyazaki M. A case of acute appendicitis complicated with superior mesenteric vein thrombosis. Jpn J Surg Assoc 69: 581-585, 2008(in Japanese, Abstract in English). [Google Scholar]
- 5. Chang YS, Min SY, Joo SH, Lee SH. Septic thrombophlebitis of the porto-mesenteric veins as a complication of acute appendicitis. World J Gastroenterol 14: 4580-4582, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Longo WE, Vernava AM 3rd. Clinical implications of jejunoileal diverticular disease. Dis Colon Rectum 35: 381-388, 1992. [DOI] [PubMed] [Google Scholar]
- 7. Yanagisawa S, Ozawa A, Ishibashi H, Arai K. A case of mesenteric abscess caused by penetrated diverticulum of the terminal ileum. Jpn J Gastroenterol Surg 37: 1577-1581, 2004. [Google Scholar]


