STRUCTURED ABSTRACT
Objective
Patients discharged to Skilled Nursing Facilities (SNFs) have worse outcomes than those discharged to home, but whether this is due to differences in facility-level factors in addition to patient characteristics is not known. We aimed to determine whether SNF-level factors including nurse staffing and patient density are associated with outcomes after acute hospitalization for trauma or surgery.
Design, Setting, Participants, & Measurements
Retrospective study of patients discharged to Medicare-certified SNFs after trauma or major surgery from 2007–2009. We measured the ratio of beds per nurse and the proportion of trauma and surgery patients at each facility (density). Outcomes were one-year mortality, hospital readmission, and failure to discharge home at first discharge disposition.
Results
For 389,133 patients (mean age 78 years, 63% female) admitted to 3,707 SNFs, mortality was 26%, hospital readmission 26%, and failure to discharge home 44%. After adjusting for patient-level factors, SNFs with fewer beds per nurse had lower odds of mortality (OR: trauma 0.84 [95% CI: 0.77–0.91]; surgery 0.80 [0.75–0.86]), readmission (OR: trauma 0.81 [0.74–0.88]; surgery 0.71 [0.65–0.76]) and failure to discharge home (OR: trauma 0.82 [0.74–0.91]; surgery 0.66 [0.60–0.72]). SNFs with greater density of specialty patients (>4.3% surgery, >14.1% trauma) had lower odds of readmission (OR: trauma 0.59 [0.53–0.66]; surgery 0.62 [0.58–0.67]) and failure to discharge home (OR: trauma 0.48 [0.43–0.55]; surgery 0.45 [0.42–0.49]).
Conclusion
There are modifiable SNF-level factors that influence long-term outcomes and may be targets for intervention. Staffing standardization and SNF specialization may reduce variation of quality in post-acute care.
Keywords: Skilled nursing facility, post-acute care, outcomes, trauma, surgery, nursing
INTRODUCTION
Patients who experience trauma, like those who undergo major surgery, have unique care needs following acute hospitalization including wound care, management of orthopedic repairs, and rehabilitation for traumatic brain injury. Over the past two decades, length of stay (LOS) after surgery has decreased but at the cost of more admissions to post-acute care (PAC) facilities as well as more frequent hospital readmissions.1 After major trauma, one in four patients will be discharged to PAC facilities.2 While quality improvement for both trauma and surgery patients has focused on hospital-based care, the increased risk of mortality extends well beyond the acute hospitalization,3–5 including at skilled nursing facilities (SNFs) where potentially preventable adverse events (AEs) are frequently reported and lead to hospital readmission.6,7 SNF-related AEs, including falls, medication errors, and infections, cause serious harm and nearly 25% of patients experience an unplanned hospital readmission.6,8–10 The Department of Health and Human Services estimated that in 2014, 22% of Medicare beneficiaries experienced AEs during their SNF stays—costing $2.8 billion annually in subsequent hospital treatment for harm occurring while admitted to SNFs.11
Prior studies have identified patient-level factors that are associated with poor outcomes after discharge to SNFs.13–17 The role of SNF-level factors in the occurrence of AEs and readmission, however, is poorly understood and may be an opportunity for targeted interventions for improving clinical outcomes. Hospitals have become increasingly specialized and trauma care regionalized, but there is little knowledge of the effect of specialization in the trauma or surgical population on AEs and its relation to hospital readmission in PAC.18–20 We hypothesized that SNFs with greater experience in caring for specialized patient populations (e.g. SNFs with patient panels comprised of more trauma or surgical patients) demonstrate favorable outcomes and that nurse staffing ratios may also play a role in long-term outcomes in PAC.21 In this study, we aimed to determine whether potentially modifiable facility-level factors were associated with outcomes measured by clinically significant events in a patient’s transition through PAC: hospital readmission, failure to discharge to home, and death.
METHODS
We performed a retrospective study of Medicare beneficiaries from a non-random sample of five states between 2007 and 2009. Washington, California, Texas, Florida, and New York were selected as geographically diverse states with large populations that represent a variety of patient demographics. Data was obtained from the Centers for Medicare and Medicaid Services (CMS) through the Research Data Assistance Center (University of Minnesota). CMS Master Beneficiary Summary File (MBSF) data was linked by social security number with hospitalization claims from the Medicare Provider Analysis and Review (MEDPAR) file, SNF-admission data using the Minimum Data Set (MDS), and with vital statistics from the National Death Index (NDI). This study was approved by the University of Washington Human Subjects Division institutional review board.
Cohort Selection
Adult patients hospitalized for trauma or major surgery based upon diagnosis (ICD-9) and procedure codes (CPT) (Appendix) who were subsequently admitted to Medicare-certified SNFs between January 1st, 2007 and December 31st, 2009 were selected for inclusion from five large states in around the country. Major surgeries were selected by procedure codes for operations that typically require inpatient admission. Patients were excluded if they had resided in a SNF in the prior six months, had a terminal diagnosis on SNF admission, or were receiving hospice care within the first week of SNF admission as documented in the MDS (an assessment performed at the time of a patient’s admission to a SNF). Using claims from the MEDPAR file, we collected patient demographics (age and gender), Charlson Comorbidity Index (CCI, Deyo definition)22, hospital LOS, and Intensive Care Unit (ICU) LOS as applicable. The following patient factors were obtained from the MDS: Activity of Daily Living (ADL) scores, assessed cognitive level, the need for parenteral nutrition or tube feeds, and the presence of pressure ulcers.
Exposures
Facility-level data, including number of beds and number of employed nurses (Registered Nurses (RN) with higher levels of training and Licensed Practical Nurses (LPN) with lower levels of training) for each SNF was obtained from Medicare’s Provider of Services (POS) File during the first quarter of the study. Cross-sectional sampling of the number of nurses at each facility provided an estimate of employment patterns for the entire study period. We derived the following facility-level factors which may be associated with patient outcomes: First, Bed:Nurse ratio was defined as the number of facility beds per full time equivalent (FTE) nurse (either RN or LPN) employed at each SNF. Second, we derived staffing ratios by nurse type (i.e.Bed:RN & Bed:LPN). Third, we calculated the ratio of LPNs per RN. Lastly, as a measure of a SNF’s degree of experience with specialty patients, density was defined as the proportion of a facility’s total patient census made up by patients with either a history of trauma or major surgery.
Outcomes
We measured each patients’ first discharge disposition after SNF admission during three years of follow up through 2012. Patient deaths were identified with NDI data through 2010. Outcomes were hospital readmission, failure to discharge home on the first disposition (including discharge to rehabilitation facility, long-term acute care, or hospice), and one-year mortality.
Missing Data for Clinical Factors
Missing data was present from 0.3 to 7.3% of clinical variables. We performed ten iterations of multivariate imputation using chained equations to generate plausible values for records with missing data.23,24 Common factors used in predicting the missing values included age, gender, CCI, ICU LOS, presence of pressure ulcers and category of surgical procedures. Sensitivity analysis showed no differences between cases with complete and imputed data.
Analysis
We anticipated that outcomes from SNFs with very few trauma or surgical admissions during the three year study period would bias assessment of outcomes therefore we excluded SNFs in the lowest quartile for volume of trauma or surgical admissions (853 facilities with <9 trauma or surgical admissions (2983 patients, <1% of the initial cohort)). There were two primary analyses in this study: First, in an analysis of variability at SNFs we used multivariate logistic regression models (accounting for clustering effects at the SNF level) to calculate risk-adjusted event rates for mortality, hospital readmission and failure to discharge home from each SNF in the study. “Expected” event rates are reported after risk adjustment for patient level factors associated with adverse outcomes (age, sex, CCI, ADL score, history of ICU stay, parenteral nutrition use, presence of pressure ulcers, cognitive status, emergency admission status (surgical patients) and Injury Severity Score for trauma patients. We report observed-to-expected event ratios (O/E ratio) and corresponding 95% confidence intervals (CI) for each outcome by facility. Second, in adjusted analysis of SNFs facility-level factors and patient outcomes, we divided SNFs into quintiles by Bed:Nurse ratio, LPN:RN ratio, and trauma/surgical density. Logistic regression models were used to calculate the adjusted odds ratio (OR) and 95% CI of death, hospital readmission and failure to discharge home after controlling for all relevant clinical and demographic factors described above. Reference groups were defined as the lowest quintile. All statistical analyses were performed using Stata software version 12.0 (Stata-Corp, College Station, Texas).
RESULTS
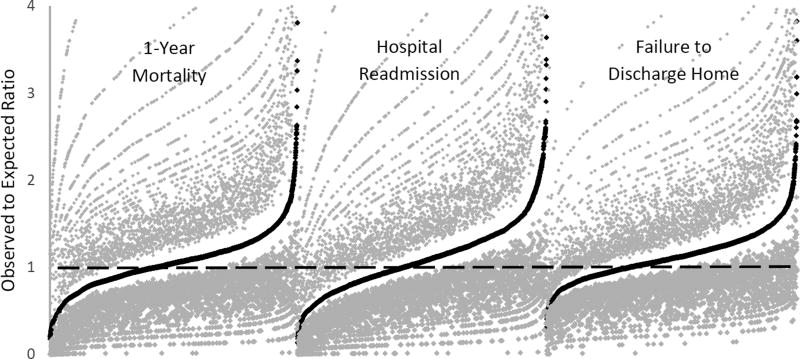
A total of 389,133 patients met inclusion criteria, of which 21% (n=83,207) had a history of trauma (mean age 82 years, 72% female) and 79% (n=305,926) had major surgery (mean age 77 years, 60% female). Patients were admitted to a total of 3,707 SNFs (2,798 admitted trauma patients, 2,844 admitted surgery patients). One-year mortality was 23% for trauma patients and 26% for surgery patients. Hospital readmission and failure to discharge home occurred for 24% and 48% of trauma patients respectively, and 27% and 43% of surgery patients, respectively. After adjusting for patient-specific factors, the O/E ratios for mortality, hospital readmission and failure to discharge home varied widely among SNFs (Figure 1).
Figure 1.
Rank ordered observed to expected ratios for one-year mortality, hospital readmission, and failure to discharge home among SNF’s admitting patients after major surgery. Gray dots represent 95% Confidence Intervals.
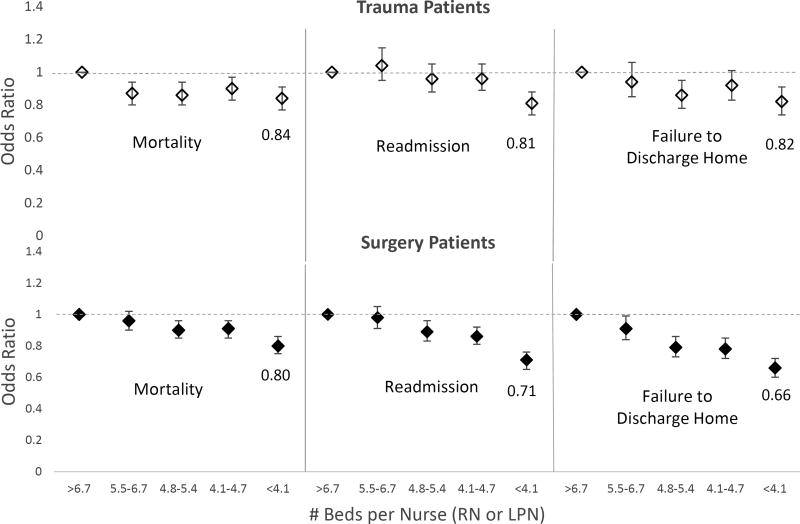
Lower Bed:Nurse ratios were associated with better outcomes. SNFs in the lowest quintile for Bed:Nurse ratio (<4.1 beds per nurse (RN or LPN)) had significantly lower odds of one-year mortality (OR: trauma 0.84, 95% CI [0.77–0.91]; surgery 0.80 [0.75–0.86]), hospital readmission (OR: trauma 0.81 [0.74–0.88]; surgery 0.71 [0.65–0.76]) and failure to discharge home (OR: trauma 0.82 [0.74–0.91]; surgery 0.66 [0.60–0.72]) compared with a reference group of SNFs with >6.7 beds per nurse. Figure 2 demonstrates odds of each outcome among five quintiles of Bed:Nurse ratios. When examining the effect of nurses with higher levels of training, lower Bed:RN ratios were consistently associated with better outcomes. SNFs in the lowest quintile for Bed:RN ratio (<12 beds per RN) had significantly lower odds of one-year mortality (OR: trauma 0.77 [0.71–83]; surgery 0.80 [0.75–0.86]), hospital readmission (OR: trauma 0.70 [0.64–0.76]; surgery 0.70 [0.65–0.75]), and failure to discharge home (OR: trauma 0.76 [0.68–0.84]; surgery 0.73 [0.67–0.79]) compared with a reference group of SNFs with >49 beds per RN. When measuring ratios of LPNs (nurses with lower levels of training than RNs), this effect was not seen. SNFs in the lowest quintile for Bed:LPN ratio (<5.3 beds per LPN), demonstrated no difference in one-year mortality (OR: trauma 1.01 [0.93–1.09]; surgery 0.94 [0.88–1.01]) compared with SNFs with >10 beds per LPN. Among surgery patients, lower Bed:LPN ratio was associated with lower odds of readmission (OR: 0.87 [0.80–0.95]) and failure to discharge home (OR: 0.82 [0.75–0.91]) however among trauma patients there was no difference (readmission OR 1.01 [0.93–1.10]; failure to discharge home OR: 0.97 [0.88–1.07]).
Figure 2.
Odds of one-year mortality, hospital readmission, and failure to discharge home by quintiles of Bed:Nurse ratio (either RN or LPN). Reference groups are the SNFs with the greatest number of Beds per Nurse.
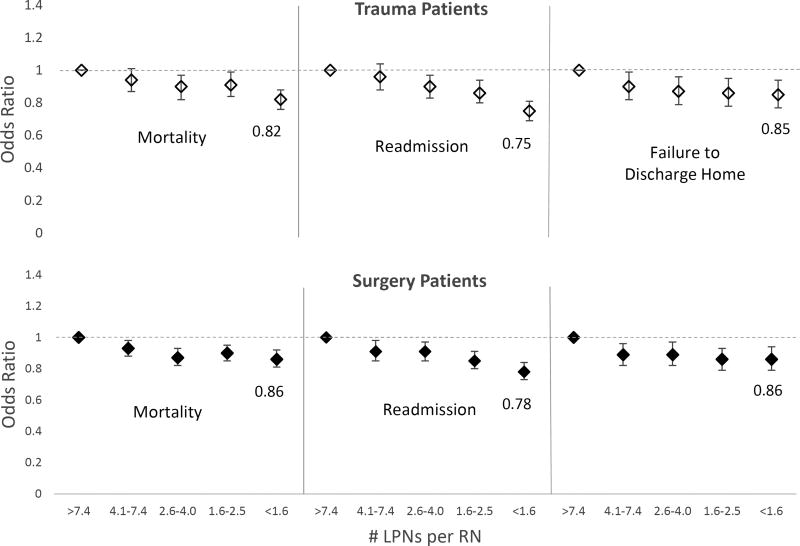
We then examined the ratio to LPN to RN in a SNF’s workforce. There was evidence that a higher ratio of LPNs to RNs confers worse outcomes. SNFs with fewer than 1.6 LPNs per RN had lower odds of mortality (OR: trauma 0.82 [0.76–0.88]; surgery 0.86 [0.81–0.92]) readmission (OR: trauma 0.75 [0.69–0.81]; surgery 0.78 [0.73–0.84]), and failure to discharge home (OR: trauma 0.85 [0.77–0.94]; surgery 0.86 [0.79–0.94]) compared to SNFs with greater than 7.4 LPNs per RN (Figure 3).
Figure 3.
Odds of one-year mortality, hospital readmission and failure to discharge home by quintiles of LPN:RN ratio. Reference groups are the SNFs with the most LPNs per RN.
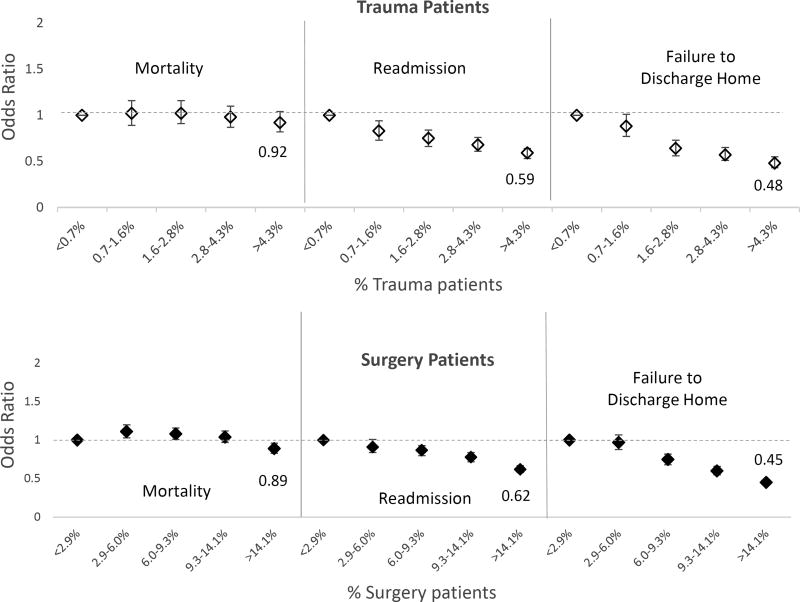
Lastly, although SNFs with higher trauma density (>4.3% of patients admitted after trauma) were not associated with differences in odds of mortality (OR 0.92 [0.82–1.04]), facilities with higher surgical density (>14.1% of patients admitted after surgery) were associated with lower odds of mortality (OR 0.89 [0.83–0.96]). For both trauma and surgical patients, higher density was associated with significantly lower odds hospital readmission (OR: trauma 0.59 [0.53–0.66]; surgery 0.62 [0.58–0.67]) and had a higher odds of successful discharge home (failure to discharge home OR: trauma 0.48 [0.43–0.55]; surgery 0.45 [0.42–0.49]) compared with SNFs in the lowest quintile for density (<0.7% trauma, <2.9% surgery) (Figure 4). We separately modeled patient volume and found that hospitals with the highest volumes of trauma and surgery patients were associated with significantly lower odds of adverse outcomes.
Figure 4.
Odds of one-year mortality, hospital readmission, and failure to discharge home by quintiles of trauma and surgical density. Reference groups are the SNFs with the lowest trauma and surgical density.
DISCUSSION
After controlling for patient-level factors that are associated with poor clinical outcomes,25 we observed wide variability in mortality, readmission, and discharge to home for trauma and surgical patients at SNFs in five states. This study demonstrates that facility-level factors, which are potentially modifiable, are also associated with important outcomes in PAC at SNFs. We have shown that, when controlling for patient differences, fewer beds per nurse are associated with reduced odds of adverse outcomes, however this association was consistent only among RNs and not LPNs. SNFs with lower LPN to RN ratios also had more favorable outcomes suggesting that substitution by nurses with lower levels of training may lead to patient harm. We also report an association of higher trauma and surgical patient density with lower odds of hospital readmission and discharge to home. This study adds important knowledge to the evidence that PAC facility-level factors are associated with multiple important patient outcomes. These factors may be targets for quality improvement of care in the post-acute setting and should be further explored.
AE that occur at SNFs often lead to hospital readmission and at significant cost. In the era of bundled payments, integrated health systems are expected to cover a patient’s entire course, from acute hospitalization through PAC. These systems will need to adapt by identifying excess costs. In 2013, a report from the Institute of Medicine identified that PAC accounts for 73% of the variability in Medicare spending.26 Rates of rehospitalization from SNFs are also heterogeneous and vary considerably by region.27 Despite this, there remains a gap in understanding optimal structural components of SNFs. The relationship of higher patient volume and improved clinical outcomes has been demonstrated and hospitals performing high volume surgeries exhibit lower rates of complications and mortality.28,29 A volume-outcome relationship suggests that institutions with more experience caring for patients with unique care needs are less likely to incur AEs. To date, however, there has been limited study on volume and outcomes in PAC30–32. A 2010 study of SNFs with high volume admissions demonstrated lower rates of functional decline in patients compared with the low volume SNFs.33 In 2015, Gozalo et al. demonstrated that a facility’s volume of hip fracture patients influenced short term outcomes including discharge to home.34 In our study, we build upon existing evidence by measuring specialized patient density as an estimate of a facility’s experience in caring for patients with specific nursing care needs (e.g. surgical wound care). We have demonstrated that a relationship exists between patient-specific volume (i.e. density) and both short- and medium-term outcomes in the PAC period. By identifying structural metrics related to favorable outcomes, we propose that partnerships between SNFs and hospitals can facilitate specialization. In this study, both trauma and surgery patients represented a minority of patients at nearly all SNFs, therefore developing trauma- or surgery-specific facilities may present unique challenges. Nonetheless, in our region, specialization of SNFs has become an area of interest for the purpose of improving quality of post-acute care.
To date, studies of nurse staffing in PAC have generated mixed findings.35 While higher staffing levels at nursing homes has been associated with improved patient-level behaviors such as sleep, appetite and social engagement,36 a 2007 study of SNF patients did not identify an association between patient-time with licensed nurses and functional outcomes.37 Another study of Medicare patients at SNFs identified an association with greater RN hours and lower prevalence of pressure ulcers while greater LPN hours was associated with higher prevalence of pressure ulcers and a decline in ADLs.38 Other studies have identified that nurse staffing may play a role in the quality of mental health care received at SNFs.39 In our study, we identified a clear association between fewer beds per nurse (either RN or LPN) and favorable outcomes. It was noteworthy that while lower Bed:RN ratios were associated with favorable mortality, readmission and disposition outcomes, lower Bed:LPN ratios did not carry the same convincing association. There are several possible explanations for this observation. RNs are nurses with two to four years of training and are responsible for medication administration, clinical surveillance and early detection of patient deterioration.21,40 In contrast, LPNs typically have one year of training and provide basic nursing care, aid with ADLs and measure vital signs.41 Nurse staffing ratios may be a surrogate marker for other quality processes or reflect improved clinician awareness, training, and recognition of patient decompensation allowing for “rescue” of those patients at risk for clinical decline. The additional knowledge basis, nursing leadership, and care coordination of RNs in PAC may lead to earlier recognition of AEs in specialized patient populations. Because facilities typically have minimum staffing requirements, substitution of RNs with LPNs may explain the less favorable outcomes seen at facilities with the fewest RN per LPN. While further investigation into the role of skilled nurses for specialized patients is warranted, these findings support regulation of staffing ratios in PAC.
There are a number of limitations to this study. First, CMS data does not represent all patients receiving PAC. Despite this, SNF populations are a majority elderly population typically insured by Medicare. Second, data for this study was derived from patients in only five states. Due to limited funding, a nationwide Medicare sample was not possible, but states in this study were selected for their heterogeneous populations from a variety of regions throughout the country. As such, we believe that these findings are generalizable to the United States population. Third, although the MDS and POS datasets provide valuable insights into facility-level metrics, we acknowledge there are likely other unmeasured factors that contribute to AEs and outcomes such as indicators of decline in patient function during SNF residence. Defining functional decline, however, was not possible with the available data. Further, there is seasonal variability in trauma admissions that is not directly captured directly by our metric of trauma patient density and which may play a role in outcomes. Despite this limitation, SNFs that admit more trauma patients during all periods reflect higher trauma patient density. Although these limitations are present, we believe that this study reveals novel information on facility-level factors in PAC outcomes that supports future work in improving care at SNFs.
CONCLUSIONS
While previous studies have identified patient-level and hospital factors that predict AEs in PAC, research into facility-level factors influencing outcomes at SNFs has been lacking. This study demonstrates that higher nursing ratios as well as greater facility experience with specialized patients are associated with favorable outcomes in the trauma and surgical population. In particular, fewer beds per RN was associated with not only lower rates of hospital readmission but also lower odds of 1-year mortality. These findings have important policy implications for quality improvement at SNFs and further research should focus on clarifying targets for interventions to decrease the extensive variability of outcomes seen in the PAC SNF population.
Table 1.
Demographics and characteristics of trauma and surgical patients.
| Characteristics | Trauma* | Surgical | Total | |
|---|---|---|---|---|
| 83,207 | 305,926 | 389,133 | ||
| Age (Mean (SD)) | 82.4 (9.7) | 77.2 (10.7) | 78.3(10.7) | |
| Age Category | ||||
| <65 | 3,655 (4.4) | 29,081 (9.5) | 32,736 (8.4) | |
| 65–74 | 11,150 (13.4) | 77,822 (25.4) | 88,972 (22.9) | |
| 75–84 | 28,411 (34.1) | 118,807 (38.8) | 147,218 (37.8) | |
| ≥85 | 39,991 (48.1) | 80,216 (26.2) | 120,207 (30.9) | |
| Gender (% Male) | 27.7 | 39.9 | 37.3 | |
| Admission Priority (N (%)) | ||||
| Emergency/Urgent | 83,207 (100) | 198,852 (64.9) | 282,059 (72.5) | |
| Elective | -- | 107,074 (35.1) | 107,074 (27.5) | |
| Charlson Comorbidity Index (%) | ||||
| 0–3 | 15.4 | 26.6 | 24.2 | |
| 4–6 | 72.8 | 60.4 | 63.0 | |
| 7–9 | 11.3 | 12.3 | 12.1 | |
| >9 | 0.5 | 0.8 | 0.7 | |
| Injury Severity Score (%) | ||||
| 0–9 | 78.9 | -- | -- | |
| 10–15 | 10.8 | -- | -- | |
| 16–24 | 8.9 | -- | -- | |
| 25–75 | 1.4 | -- | -- | |
| Procedure Type | ||||
| Neurosurgical | -- | 17,224 (5.6) | -- | |
| Head & Neck | -- | 7,913 (2.6) | -- | |
| Cardiothoracic | -- | 42,066 (13.8) | -- | |
| Abdominopelvic | -- | 69,223 (22.6) | -- | |
| Orthopedic | -- | 99,000 (32.4) | -- | |
| Skin & Soft Tissue | -- | 18,498 (6.1) | -- | |
| Open Vascular | -- | 37,021 (12.1) | -- | |
| Endovascular | -- | 5,071 (1.7) | -- | |
| Spine | -- | 9,910 (3.2) | -- | |
| Hospital LOS (Median(IQR)) | 5 (4.0) | 7 (9.0) | 7 (8.0) | |
| ICU Stay (%) | 23.1 | 34.7 | 32.2 | |
| ICU LOS (Median(IQR))** | 4 (4.0) | 5 (7.0) | 5 (6.0) | |
| MDS-ADL (Mean(SD)) | 4.1 (1.1) | 3.7 (1.3) | 3.8 (1.3) | |
| Cognitive Scoring % | ||||
| Fully Independent | 49.4 | 62.9 | 60.0 | |
| Modified Independence | 23.4 | 19.3 | 20.2 | |
| Moderately Impaired | 22.7 | 14.0 | 15.9 | |
| Severely Impaired | 4.4 | 3.8 | 3.9 | |
| Parenteral Nutrition (%) | 10.5 | 11.4 | 11.2 | |
| Tube Feeds (%) | 2.0 | 7.0 | 5.9 | |
| Pressure Ulcers at SNF Admission (%) | 28.8 | 28.4 | 28.5 | |
While some trauma patients may have also undergone surgery, these patients were analyzed in the trauma cohort
Calculated only among patients with ICU stay.
Acknowledgments
We would like to thank Erika Wolff, PhD and Anna Shaffer from the Surgical Outcomes Research Center for technical assistance with this manuscript. This research was funded by Washington State’s Life Science Discovery Fund and the Agency for Healthcare Research and Quality Grant Number 1 R01 HS 20025-01 through the Comparative Effectiveness Research Translation Network (CERTAIN) and the Harborview Injury Prevention Research Center. This research was also supported by a research training grant from the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under Award Number T32DK070555. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
ABBREVIATIONS
- ADL
activities of daily living
- AE
adverse events
- CCI
Charlson Comorbidity Index
- CI
confidence interval
- CMS
Center for Medicare and Medicaid Services
- CPT
Current Procedural Terminology
- ICD
International Classification of Diseases, 9th revision
- ICU
Intensive Care Unit
- LPN
Licensed Practical Nurse
- LOS
length of stay
- MEDPAR
Medicare Provider Analysis and Review
- NDI
National Death Index
- O/E
observed-to-expected ratio
- OR
odds ratio
- PAC
post-acute care
- POS
Provider of Services
- RN
Registered Nurse
- SNF
Skilled nursing facility
APPENDIX
International Classification of Diseases-9 (ICD-9) Diagnosis Codes and Current Procedural Terminology (CPT) Codes selected for patient inclusion
Trauma Diagnoses:
CPT: 80000–90500; 92500–93000; 94000–95000
Surgical Procedures (ICD-9):
Neurosurgical: 100–500; 760–770
Head & Neck: 800–1700; 1800–3200; 4040; 7600–7700; 600–700
Cardiothoracic: 3200–3800; 4060, 4240–4260; 50–60; 3900–3910; 780–800
Abdominopelvic: 4300–7600; 91–94; 700–750
Orthopedic: 70–80; 7700–8100; 8110–8130; 8140–8160; 8170–8300; 8400–8460; 8470–8500
Skin & soft tissue: 4030; 4050; 8300–8400; 8500–8700
Vascular: 3800–3900; 3910–3960
Endovascular: 20–30; 60–70; 3970–3980; 3990
Spine: 8460; 8100–8110; 8130–8140; 8160–8170
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST STATEMENT: The authors have no conflicts of interest to disclose related to this work.
References
- 1.Cram P, Lu X, Kaboli PJ, et al. Clinical characteristics and outcomes of Medicare patients undergoing total hip arthroplasty, 1991–2008. Jama. 2011;305(15):1560–1567. doi: 10.1001/jama.2011.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davidson GH, Hamlat Ca, Rivara FP, Koepsell TD, Jurkovich GJ, Arbabi S. Long-term survival of adult trauma patients. JAMA. 2011;305(10):1001–1007. doi: 10.1001/jama.2011.259. [DOI] [PubMed] [Google Scholar]
- 3.Fleischman RJ, Adams AL, Hedges JR, Ma OJ, Mullins RJ, Newgard CD. The Optimum Follow-Up Period for Assessing Mortality Outcomes in Injured Older Adults. J Am Geriatr Soc. 2010;58(10):1843–1849. doi: 10.1111/j.1532-5415.2010.03065.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Claridge JA, Leukhardt WH, Golob JF, McCoy AM, Malangoni MA. Moving Beyond Traditional Measurement of Mortality after Injury: Evaluation of Risks for Late Death. J Am Coll Surg. 2010;210(5):788–794. doi: 10.1016/j.jamcollsurg.2009.12.035. [DOI] [PubMed] [Google Scholar]
- 5.Yu P, Chang DC, Osen HB, Talamini MA. NSQIP reveals significant incidence of death following discharge. J Surg Res. 2011;170(2):e217–e224. doi: 10.1016/j.jss.2011.05.040. [DOI] [PubMed] [Google Scholar]
- 6.Ouslander JG, Perloe M, Givens JH, Kluge L, Rutland T, Lamb G. Reducing Potentially Avoidable Hospitalizations of Nursing Home Residents: Results of a Pilot Quality Improvement Project. J Am Med Dir Assoc. 2009;10(9):644–652. doi: 10.1016/j.jamda.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 7.Auerbach AD, Kripalani S, Vasilevskis EE, et al. Preventability and Causes of Readmissions in a National Cohort of General Medicine Patients. JAMA Intern Med. 2016;176(4):484–493. doi: 10.1001/jamainternmed.2015.7863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hagino T, Ochiai S, Sato E, Watanabe Y, Senga S, Haro H. Prognostic prediction in patients with hip fracture: risk factors predicting difficulties with discharge to own home. J Orthop Traumatol. 2011;12(2):77–80. doi: 10.1007/s10195-011-0138-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Heal Aff. 2010;29(1):57–64. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 11.Levinson DR. Adverse events in skilled nursing facilities: National Incidence among medicare beneficiaries. 2014 Feb;:1–69. doi:OEI-06-11-00370. [Google Scholar]
- 12.Burke RE, Kripalani S, Vasilevskis EE, Schnipper JL. Moving beyond readmission penalties: Creating an ideal process to improve transitional care. J Hosp Med. 2013;8(2):102–109. doi: 10.1002/jhm.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wunsch H, Guerra C, Barnato AE, Angus DC, Li G, Linde-Zwirble WT. Three-year outcomes for Medicare beneficiaries who survive intensive care. Jama. 2010;303(9):849–856. doi: 10.1001/jama.2010.216. [DOI] [PubMed] [Google Scholar]
- 14.Aitken LM, Burmeister E, Lang J, Chaboyer W, Richmond TS. Characteristics and outcomes of injured older adults after hospital admission. J Am Geriatr Soc. 2010;58(3):442–449. doi: 10.1111/j.1532-5415.2010.02728.x. [DOI] [PubMed] [Google Scholar]
- 15.Ventura T, Harrison-Felix C, Carlson N, et al. Mortality After Discharge From Acute Care Hospitalization With Traumatic Brain Injury: A Population-Based Study. Arch Phys Med Rehabil. 2010;91(1):20–29. doi: 10.1016/j.apmr.2009.08.151. [DOI] [PubMed] [Google Scholar]
- 16.Colantonio A, Escobar MD, Chipman M, et al. Predictors of postacute mortality following traumatic brain injury in a seriously injured population. J Trauma. 2008;64(4):876–882. doi: 10.1097/TA.0b013e31804d493e. [DOI] [PubMed] [Google Scholar]
- 17.Legner VJ, Massarweh NN, Symons RG, McCormick WC, Flum DR. The significance of discharge to skilled care after abdominopelvic surgery in older adults. Ann Surg. 2009;249(2):250–255. doi: 10.1097/SLA.0b013e318195e12f. [DOI] [PubMed] [Google Scholar]
- 18.Malik A, Bell CM, Stukel TA, Urbach DR. Recurrence of inguinal hernias repaired in a large hernia surgical specialty hospital and general hospitals in Ontario, Canada. Can J Surg. 2016;59(1):19–25. doi: 10.1503/cjs.003915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mesman R, Westert GP, Berden BJMM, Faber MJ. Why do high-volume hospitals achieve better outcomes? A systematic review about intermediate factors in volume-outcome relationships. Health Policy (New York) 2015;119(8):1055–1067. doi: 10.1016/j.healthpol.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 20.Billingsley KG. Surgeon and Hospital Characteristics as Predictors of Major Adverse Outcomes Following Colon Cancer Surgery. Arch Surg. 2007;142(1):23. doi: 10.1001/archsurg.142.1.23. [DOI] [PubMed] [Google Scholar]
- 21.Aiken LH. Hospital Nurse Staffing and Patient Mortality, Nurse Burnout, and Job Dissatisfaction. JAMA. 2002;288(16):1987. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- 22.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. http://www.ncbi.nlm.nih.gov/pubmed/1607900. [DOI] [PubMed] [Google Scholar]
- 23.van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med. 1999;18(6):681–694. doi: 10.1002/(sici)1097-0258(19990330)18:6<681::aid-sim71>3.0.co;2-r. http://www.ncbi.nlm.nih.gov/pubmed/10204197. [DOI] [PubMed] [Google Scholar]
- 24.Sterne JAC, White IR, Carlin JB, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393. doi: 10.1136/bmj.b2393. http://www.ncbi.nlm.nih.gov/pubmed/19564179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hakkarainen TW, Arbabi S, Willis MM, Davidson GH, Flum DR. Outcomes of Patients Discharged to Skilled Nursing Facilities After Acute Care Hospitalizations. Ann Surg. 2015:1. doi: 10.1097/SLA.0000000000001367. XX(X) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Congress of the United States. Geographic Variation in Health Care Spending. 2008 Feb;:1–31. http://www.cbo.gov/ftpdocs/89xx/doc8972/02-15-GeogHealth.pdf.
- 27.Mor V, Intrator O, Feng Z, Grabowski DC. The Revolving Door of Rehospitalization From Skilled Nursing Facilities. Heal Aff. 2010;29(1):57–64. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Birkmeyer JD, Finlayson SR, Tosteson aN, Sharp SM, Warshaw aL, Fisher ES. Effect of hospital volume on in-hospital mortality with pancreaticoduodenectomy. Surgery. 1999;125(3):250–256. doi: 10.1016/S0039-6060(99)70234-5. [DOI] [PubMed] [Google Scholar]
- 29.Hata T, Motoi F, Ishida M, et al. Effect of Hospital Volume on Surgical Outcomes After Pancreaticoduodenectomy: A Systematic Review and Meta-analysis. Ann Surg. :1–9. doi: 10.1097/SLA.0000000000001437. 9000;Publish Ah(X) [DOI] [PubMed] [Google Scholar]
- 30.Hakkarainen TW, Ayoung-Chee P, Alfonso R, Arbabi S, Flum DR. Structure, process, and outcomes in skilled nursing facilities: Understanding what happens to surgical patients when they cannot go home. A systematic review. J Surg Res. 2015;193(2):772–780. doi: 10.1016/j.jss.2014.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Holstege MS, Zekveld IG, Caljouw MAA, et al. Relationship of Patient Volume and Service Concentration With Outcome in Geriatric Rehabilitation. J Am Med Dir Assoc. 2013;14(10):731–735. doi: 10.1016/j.jamda.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 32.Kauh B, Polak T, Hazelett S, Hua K, Allen K. A Pilot Study: Post-Acute Geriatric Rehabilitation Versus Usual Care in Skilled Nursing Facilities. J Am Med Dir Assoc. 2005;6(5):321–326. doi: 10.1016/j.jamda.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 33.Li Y, Cai X, Mukamel DB, Glance LG. The Volume-Outcome Relationship in Nursing Home Care. Med Care. 2010;48(1):52–57. doi: 10.1097/MLR.0b013e3181bd4603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gozalo P, Leland NE, Christian TJ, Mor V, Teno JM. Volume Matters: Returning Home After Hip Fracture. J Am Geriatr Soc. 2015;63(10):2043–2051. doi: 10.1111/jgs.13677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Decker FH. Nursing Staff and the Outcomes of Nursing Home Stays. Med Care. 2006;44(9):812–821. doi: 10.1097/01.mlr.0000218832.24637.2e. [DOI] [PubMed] [Google Scholar]
- 36.Bates-Jensen BM, Schnelle JF, Alessi CA, Al-Samarrai NR, Levy-Storms L. The Effects of Staffing on In-Bed Times of Nursing Home Residents. J Am Geriatr Soc. 2004;52(6):931–938. doi: 10.1111/j.1532-5415.2004.52260.x. [DOI] [PubMed] [Google Scholar]
- 37.Arling G, Kane RL, Mueller C, Bershadsky J, Degenholtz HB. Nursing effort and quality of care for nursing home residents. Gerontologist. 2007;47(5):672–682. doi: 10.1093/geront/47.5.672. http://www.ncbi.nlm.nih.gov/pubmed/17989409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bostick JE. Relationship of nursing personnel and nursing home care quality. J Nurs Care Qual. 2002;19(2):130–136. doi: 10.1097/00001786-200404000-00010. http://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=109877411&site=ehost-live. [DOI] [PubMed] [Google Scholar]
- 39.Grabowski DC, Aschbrenner KA, Rome VF, Bartels SJ. Quality of Mental Health Care for Nursing Home Residents: A Literature Review. Med Care Res Rev. 2010;67(6):1–25. doi: 10.1177/1077558710362538.Quality. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aiken LH. Educational Levels of Hospital Nurses and Surgical Patient Mortality. JAMA J Am Med Assoc. 2003;290(12):1617–1623. doi: 10.1001/jama.290.12.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ottem P, Overton C. RN and LPN accountabilities and responsibilities. Nurs BC. 2000;32(3):19–22. http://www.ncbi.nlm.nih.gov/pubmed/11249344. [PubMed] [Google Scholar]