Abstract
Objectives
Person-centered care (PCC), which considers nursing home resident preferences in care delivery, has been linked to important outcomes such as improved quality of life, resident satisfaction with care, and mood and reduced behavioral symptoms for residents with dementia. Delivery of PCC fundamentally relies on knowledge of resident preferences. The Minimum Data Set 3.0 (MDS) Preference Assessment Tool (PAT) is a standardized, abbreviated assessment that facilitates systematic examination of preferences from a population of nursing home residents. However, it is unknown how well the PAT discriminates preferences across residents or items. The purpose of this study was to use MDS PAT data to describe: 1) overall resident preferences, 2) variation in preferences across items, and 3) variation in preferences across residents.
Data
Data from admission Minimum Data Set 3.0 assessments between October 1, 2011 and December 31, 2011 were used for this study.
Sample
A nationally representative sample of 244,718 residents over the age of 65 years who were able to complete the resident interview version of preference, cognition, and depression assessments were included.
Measurements
Importance ratings of sixteen daily care and activity preferences were the primary outcome measures. Resident factors including function (MDS ADL-Long Form), depression (PHQ9), cognitive impairment (BIMS), and sociodemographics (age, race, gender, and marital status) were used as predictors of important preferences.
Analysis
Overall preferences were examined using descriptive statistics. Proportional differences tests were used to describe variation across items. Logistic regression was used to describe variation in preferences across residents.
Results
The majority of residents rated all 16 preferences important. However, there was variation across items and residents. Involvement of family in care and individualizing daily care and activities were rated important by the largest proportion of residents. Several resident factors including cognitive impairment, depression, gender, and race were significant predictors of preferences.
Conclusions
Findings demonstrate the PAT captures variation in preferences across items and residents. Residents with possible depression and cognitive impairment were less likely to rate preferences important than residents without those conditions. Non-Caucasians and males reported some preferences differently than Caucasians and females. Additional assessment and care planning may be important for these residents. More research is needed to determine the factors that influence preferences and the ways to incorporate them into care.
Keywords: nursing homes, patient preference, resident-centered care, patient-centered care, culture change, older adults
Multiple national quality organizations including Advancing Excellence, the American Health Care Association, and the Centers for Medicare and Medicaid Services (CMS)1,2 have promoted the transformation of nursing homes to person-centered care (PCC) environments where resident autonomy and personhood is respected and residents receive care according to their preferences3,4. Providing PCC that considers resident preferences has been linked to important outcomes such as improved quality of life5, resident satisfaction with care5, and mood6 and reduced behavioral symptoms for residents with dementia7,8. As such, the national effort toward PCC delivery has continued to expand with a nationally representative survey in 2010 showing 85% of facilities were in the process of implementing some form of PCC9.
Delivery of PCC fundamentally relies on knowledge of resident preferences. The MDS 3.0, with its revision in 2010 to include resident voice10, provides one opportunity to learn about resident preferences for daily care and activities. The MDS 3.0 Preference Assessment Tool (PAT) is a standardized, abbreviated assessment that makes systematic examination of preferences from a population of nursing home residents possible. The PAT may help clinicians develop an understanding of what is important to residents11. However, it is unknown how well the PAT discriminates preferences across residents or items. The purpose of this study was to use MDS PAT data to describe: 1) overall resident preferences, 2) variation in preferences across items, and 3) variation in preferences across residents.
Methods
Sample
Data were drawn from a cross-sectional sample of admission MDS assessments collected nationally between October 1, 2011 and December 31, 2011. All residents 65 years of age and older and who completed the resident interview version of the PAT, cognition (BIMS), and depression (PHQ9) MDS assessments were included. Residents who were comatose, had more than one admission in 2011, or had family or staff report their preferences were excluded. Residents were marked as primary respondent for 90% (item F0600), family for 8% (item F0600), and staff (item F0700) for 3% of non-missing preference records in the full 2011 MDS file. All criteria and MDS items used to determine the final sample are shown in Table 1.
Table 1.
Criteria applied to obtain final sample.
| Criteria Applied | MDS Item | Remaining Records | Remaining Persons |
|---|---|---|---|
| Full MDS 2011 dataset | N/A | 16,326,279 | 2,774,778 |
| Entry Date after 2011 | A1600 ≥ 2011 | 12,762,711 | 2,249,588 |
| SNF assessments only | A0200 = 1 | 12,762,711 | 2,249,588 |
| Admission entry only | A1700 = 1 | 9,231,454 | 2,036,637 |
| Age ≥65 | Age calculated based on A0900 | 9,214,013 | 2,035,834 |
| Admission assessment | A0310A = 01 | 1,849,734 | 1,527,246 |
| First assessment | A0310E = 1 | 1,640,495 | 1,378,727 |
| Residents not comatose | B0100 = 0 | 1,638,416 | 1,377,202 |
| Residents who should be interviewed with PAT | F0300 = 1 | 1,548,357 | 1,310,983 |
| Residents who were the primary respondent on the PAT | F0600 = 1 | 1,425,446 | 1,214,412 |
| Residents who should be interviewed with the BIMS | C0100 = 1 | 1,381,897 | 1,181,181 |
| Residents able to complete the BIMS | C0500 ≠ 99 | 1,357,775 | 1,162,126 |
| Residents who should be interviewed with the PHQ9 | D0100 = 1 | 1,342,704 | 1,150,630 |
| Residents able to complete the PHQ9 | D0300 ≠ 99 | 1,334,523 | 1,144,194 |
| Residents who had a single admission record | N/A | 985,954 | 985,954 |
| Residents assessed between Oct–Dec 2011 | Oct 01 2011 ≤ A1600 ≤ Dec 31 2011 | 244,718 | 244,718 |
Measures
Preferences
The PAT found in MDS Section F, items F0400A-F0400H, assesses the importance of 16 different care and activity preferences (Table 2, Supplemental Digital Content 1). The resident interview version was used for this study. Response options include; 1=very important, 2=somewhat important, 3=not very important, 4=not important at all, 5=important, but can’t do or no choice12.
Table 2.
Preference assessment items.
| Preference | Shortened Description (in text) | Label (in tables) |
|---|---|---|
| “While you are in this facility how important is it to you to …?” | ||
| choose what clothes to wear | Choosing clothes to wear | CLOTHES |
| take care of your personal belongings or things | Caring for belongings | CARE |
| choose between a tub bath, shower, bed bath, or sponge bath | Choosing bath | BATH |
| have snacks available between meals | Having snacks available | SNACK |
| choose own bedtime | Choosing bedtime | BED |
| have your family or a close friend involved in discussion about your care | Having family involved | FAMILY |
| be able to use the phone in private | Using phone privately | PHONE |
| have a place to lock your things to keep them safe | Locking belongings | LOCK |
| have a book, newspaper, and magazines to read | Having reading materials | READ |
| listen to music you like | Listening to music | MUSIC |
| be around animals such as pets | Being around animals | ANIMAL |
| keep up with the news | Keeping up with news | NEWS |
| do things with groups of people | Doing things with groups | GROUP |
| do your favorite activities | Doing favorite activities | FAVRTE |
| go outside to get fresh air when the weather is good | Getting fresh air | FRESH |
| participate in religious services or practices | Participating in religion | RELIG |
Function
Function was estimated using the MDS ADL-Long Form summary score which is calculated from scores on MDS Section G items G01101A, G01101B, G01101E, G01101G, G01101H, G01101I, and G01101J. These items address level of performance (0=independent, 1=supervision, 2=limited assistance, 3=extensive assistance, 4=total dependence) as scored by staff observation on seven activities of daily living (dressing, personal hygiene, bed mobility, transfer, eating, toilet use, locomotion on unit). Activities that occurred two or fewer times per week (scores of 7 or 8 on the MDS) were recoded as totally dependent. Scores range from 0–28 with higher scores indicating more impairment13,14.
Depression
Depression was determined using the total score on the Patient Health Questionnaire-9 (PHQ9) from MDS Section D item D0300. The PHQ-9 is a valid instrument15 that screens for signs and symptoms of depression using the presence and frequency of nine mood symptoms. Scores of 0–4 suggest no depression, 5–9 mild depression, 10–14 moderate depression, 15–19 moderately severe depression, and 20–27 severe depression16. A score of 10 or higher has a high specificity and sensitivity for detecting major depression17. For this analysis, scores were dichotomized as depressed (scores ≥10) or not depressed (scores ≤9). Staff complete the assessment based on resident responses to the items during an interview.
Cognitive impairment
Cognitive impairment was determined using the total severity score on the Brief Interview for Mental Status (BIMS) from MDS Section C item C0500. Staff complete the assessment based on resident responses during an interview. The BIMS assesses repetition, recall and temporal orientation with nine questions and possible total scores ranging from 0–15. Scores of 13–15 indicate no or mild cognitive impairment, 8–12 moderate impairment, and 0–7 severe impairment18.
Sociodemographics
Age, race, gender, and marital status reported in MDS Section A, items A0900, A1000, A0800, and A1200 were included in this study. Race was re-categorized as Caucasian, African American, Hispanic, or Other which included Asian, Native Hawaiian or Other Pacific Islander, American Indian or Alaska Native, or multiracial. Marital status was recoded as Married or Not Married. Not Married individuals were those who indicated they were widowed, single, or divorced.
Analysis
Descriptive statistics for sample characteristics and preference responses were calculated. Preference responses were then dichotomized into ‘important’ (includes very important, somewhat important, and important but can’t do or no choice) and ‘not important’ (includes not very important and not important at all) for the remaining analyses. Proportional difference tests were conducted and an arcsine transformation applied to determine Cohen’s h effect size. Logistic regression was used (16 separate models, one for each preference) to analyze the relationship between resident characteristics and ‘important’ preferences. Items coded ‘9 - no response’ were excluded in the analysis. The amount excluded ranged from 0.03%–0.17% across items. Given the large sample size, odds ratios were converted to effect sizes to provide the magnitude of the significant results. All analyses were conducted in Excel and SAS Enterprise Guide 7.1 software. The study was approved by the University of Wisconsin Institutional Review Board and William S. Middleton Memorial Veterans Hospital Research & Development Committee.
Results
A total of 244,718 residents from 14,492 facilities representing all 50 states, the District of Columbia and Puerto Rico were included. The majority of residents were non-Hispanic whites, not married, and female with a mean age of 81 years old. Approximately 36% of residents had some level of cognitive impairment and just over 7% had PHQ-9 scores suggesting possible depression. The mean functional score was 16.63 (Table 3).
Table 3.
Sample characteristics.
| Characteristic | Mean (SD)/Freq(%) |
|---|---|
| Age | 81.02 (8.19) |
| Female | 160,053 (65.42) |
| Race | |
| Caucasian | 207,767 (87.06) |
| African American | 18,833 (7.89) |
| Hispanic | 8,146 (3.41) |
| Other* | 3,915 (1.64) |
| Married | 80,770 (33.65) |
| Depressed (PHQ9 ≥ 10) | 17,361 (7.11) |
| Cognitive Impairment | |
| Intact (BIMS Score 13–15) | 153,540 (62.91) |
| Moderate (BIMS Score 8–12) | 57,274 (23.47) |
| Severe (BIMS Score 0–7) | 33,253 (13.62) |
| Function (MDS ADL Long Form Score 0–28) | 16.63 (4.63) |
Note. Sample sizes do not always equal 244,718 due to missing data.
Includes Asian, Native Hawaiian or Other Pacific Islander, American Indian or Alaska Native, or multiracial.
Overall Resident Preferences
There was variation in the distribution of importance ratings across items. (Figures 1 and 2). Five daily care and three activity items were highly skewed toward very important responses. Notably over 80% of residents rated having family involved very important. Over 60% of residents reported caring for belongings, choosing bedtime, getting fresh air, and keeping up with news as very important. In contrast, less than 40% of residents rated using phone privately, locking belongings, being around animals, and doing things with groups as very important. Few residents rated preferences unimportant – locking belongings and being around animals as exceptions. Over 13% of residents rated locking belongings and being around animals not important at all whereas the average proportion of residents to respond not important at all on other preferences was only about 4%. At most, only 2% of residents responded important, but can’t do/no choice to a preference (doing favorite activities).
Figure 1.
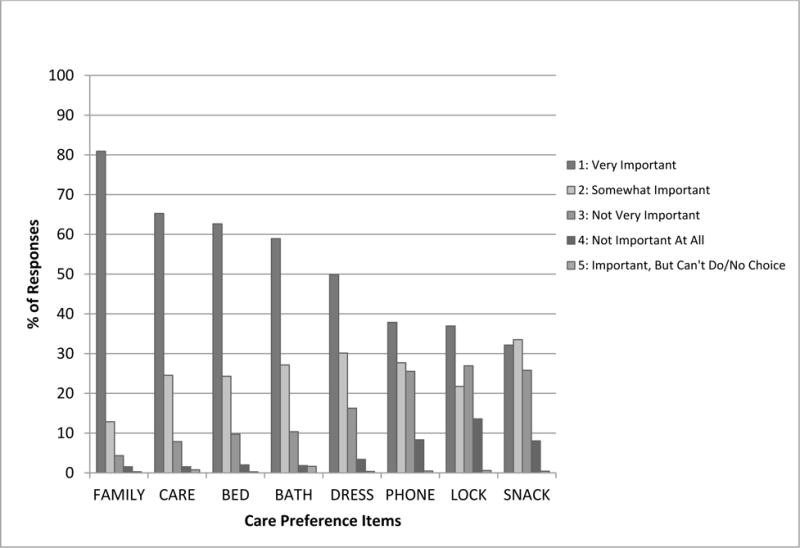
Frequency of importance ratings on care preferences.
Figure 2.
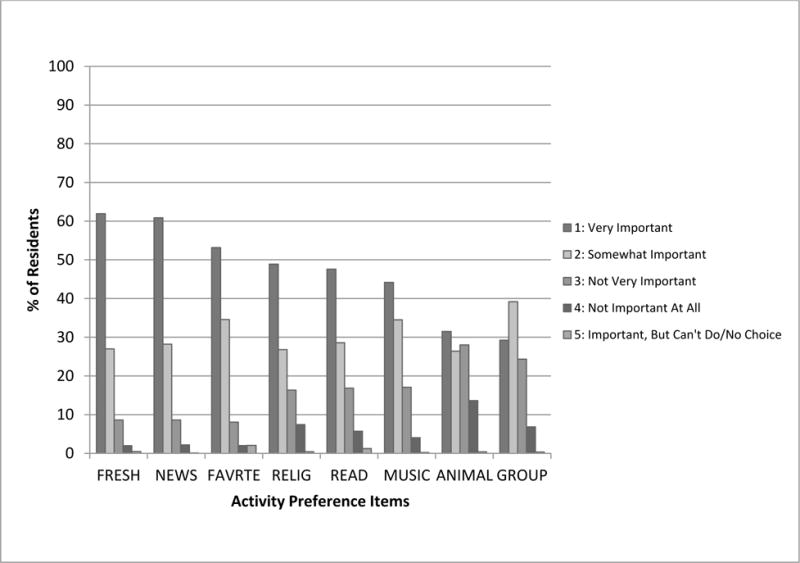
Frequency of importance ratings on activity preferences.
Variation Across Items
After dichotomizing responses into important and not important, significant differences remained in the proportion of residents rating each preference important (Table 4), although the majority of residents rated all 16 items as either very important or somewhat important. Having family involved was most preferred - it was rated important significantly more frequently than 70% of other preferences. Caring for belongings, doing favorite activities, keeping up with news, choosing bedtime, getting fresh air, and choosing bath were highly preferred. Each was rated important more frequently than 60% of other preferences. Choosing clothes, listening to music, having reading materials, participating in religion, and doing things with groups were marginally preferred, being rated important more frequently than 13–33% of other preferences. Having snacks, using the phone privately, and being around animals were less preferred as they were rated important less more frequently than other items.
Table 4.
Cohen’s h effect size for proportional differences in preferences.
| FAMILY | CARE | FVRTE | NEWS | BED | FRESH | BATH | DRESS | MUSIC | READ | RELIG | GROUP | SNACK | PHONE | ANIMAL | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CARE | 0.125 | ||||||||||||||
| FVRTE | 0.131 | 0.006 | |||||||||||||
| NEWS | 0.174 | 0.049 | 0.043 | ||||||||||||
| BED | 0.193 | 0.067 | 0.061 | 0.019 | |||||||||||
| FRESH | 0.207 | 0.081 | 0.075 | 0.033 | 0.014 | ||||||||||
| BATH | 0.207 | 0.082 | 0.076 | 0.033 | 0.014 | 0.001 | |||||||||
| DRESS | 0.418 | 0.292 | 0.286 | 0.244 | 0.225 | 0.211 | 0.210 | ||||||||
| MUSIC | 0.451 | 0.325 | 0.319 | 0.277 | 0.258 | 0.244 | 0.243 | 0.033 | |||||||
| READ | 0.492 | 0.366 | 0.360 | 0.318 | 0.299 | 0.285 | 0.284 | 0.074 | 0.041 | ||||||
| RELIG | 0.533 | 0.408 | 0.402 | 0.359 | 0.340 | 0.326 | 0.326 | 0.115 | 0.083 | 0.041 | |||||
| GROUP | 0.686 | 0.561 | 0.555 | 0.512 | 0.493 | 0.479 | 0.479 | 0.269 | 0.236 | 0.195 | 0.153 | ||||
| SNACK | 0.738 | 0.613 | 0.607 | 0.564 | 0.545 | 0.531 | 0.557 | 0.320 | 0.287 | 0.246 | 0.205 | 0.052 | |||
| PHONE | 0.768 | 0.642 | 0.636 | 0.594 | 0.575 | 0.561 | 0.560 | 0.350 | 0.317 | 0.276 | 0.235 | 0.082 | 0.030 | ||
| ANIMAL | 0.896 | 0.771 | 0.765 | 0.722 | 0.704 | 0.690 | 0.689 | 0.479 | 0.446 | 0.405 | 0.363 | 0.210 | 0.158 | 0.129 | |
| LOCK | 0.929 | 0.803 | 0.797 | 0.755 | 0.736 | 0.722 | 0.721 | 0.511 | 0.478 | 0.437 | 0.396 | 0.242 | 0.191 | 0.161 | 0.032 |
Note. Confidence intervals not shown; the 95% confidence margin of error for each proportion was less than +/- 0.001.
Light gray = small effect (h≥0.20)
Medium gray = moderate effect (h≥0.50)
Dark gray = large effect (h≥0.80)
Variation Across Residents
In the logistic regression, several resident characteristics were significant predictors of rating PAT items as important (Tables 5 & 6). There were small and moderate effects (both positive and negative) for 10 of the 16 preferences. Possible depression and cognitive impairment were associated with lower odds of rating nearly half of the preferences important. Race predicted most preferences. African Americans and Hispanics were more likely than Caucasians to report most preferences important. All races were less likely than Caucasians to rate being around animals important. Females were more likely than males to rate five of the preferences important. Marital status, function, and age were not consistently or significantly associated with preferences with the exception of married individuals being more likely than unmarried individuals to rate having family involved important.
Table 5.
Odds ratios [95% CI] for resident characteristics predicting important daily care preferences
| FAMILY | CARE | BED | BATH | DRESS | PHONE | LOCK | SNACK | ||
|---|---|---|---|---|---|---|---|---|---|
| Female |
1.488‡ [1.433, 1.545] |
1.367 [1.325, 1.409] |
1.167 [1.134, 1.201] |
1.336 [1.299, 1.373] |
1.844‡ [1.803, 1.885] |
1.146 [1.125, 1.168] |
0.972 [0.954, 0.990] |
0.894 [0.877, 0.912] |
|
| Married |
2.164‡ [2.072, 2.260] |
0.921 [0.892, 0.950] |
0.990 [0.962, 1.020] |
1.040 [1.010, 1.070] |
0.976 [0.953, 0.998] |
0.983 [0.964, 1.002] |
0.901 [0.884, 0.990] |
0.877 [0.860, 0.894] |
|
| Afr Amer | 1.349 [1.259, 1.445] |
1.296 [1.222, 1.374] |
1.035 [0.985, 1.088] |
1.279 [1.215, 1.347] |
1.517†‡ [1.452, 1.585] |
1.340 [1.295, 1.386] |
1.557‡ [1.507, 1.609] |
1.649‡ [1.590, 1.710] |
|
| Hispanic |
1.629‡ [1.454, 1.825] |
1.433‡ [1.311, 1.567] |
1.097 [1.018, 1.181] |
1.574‡ [1.449, 1.708] |
1.860‡ [1.736, 1.993] |
1.118 [1.065, 1.174] |
1.408 [1.343, 1.476] |
1.952‡ [1.845, 2.066] |
|
| Other Race | 1.119 [0.969, 1.293] |
0.749 [0.679, 0.826] |
0.830 [0.755, 0.913] |
1.136 [1.025, 1.259] |
1.035 [0.954, 1.123] |
0.910 [0.851, 0.973] |
0.934 [0.875, 0.996] |
1.314 [1.223, 1.413] |
|
| Mod Cog Imp | 0.921 [0.882, 0.963] |
0.788‡ [0.761, 0.816] |
0.827 [0.802, 0.854] |
0.775 [0.751, 0.799] |
0.926 [0.903, 0.950] |
0.821 [0.804, 0.839] |
1.016 [0.995, 1.037] |
1.085 [1.062, 1.109] |
|
| Sev Cog Imp | 0.752 [0.713, 0.793] |
0.623 [0.599, 0.648] |
0.671‡ [0.647, 0.696] |
0.564†‡ [0.544, 0.584] |
0.885 [0.857, 0.913] |
0.650‡ [0.634, 0.667] |
1.000 [0.975, 1.025] |
1.256 [1.222, 1.291] |
|
| Depressed | 0.88 [0.832, 0.949] |
0.763‡ [0.726, 0.802] |
0.824 [0.786, 0.864] |
0.867 [0.828, 0.909] |
0.698‡ [0.673, 0.725] |
0.903 [0.873, 0.933] |
0.937 [0.908, 0.968] |
0.817 [0.791, 0.845] |
|
| Function | 1.037 [1.034, 1.041] |
0.956 [0.952, 0.959] |
0.976 [0.973, 0.979] |
0.986 [0.983, 0.988] |
0.969 [0.967, 0.972] |
0.985 [0.984, 0.987] |
0.991 [0.989, 0.992] |
1.005 [1.003, 1.007] |
|
| Age | 1.034 [1.031, 1.036] |
0.987 [0.986, 0.989] |
0.991 [0.990, 0.993] |
0.922 [0.990, 0.994] |
0.996 [0.955, 0.997] |
0.979 [0.978, 0.980] |
0.989 [0.988, 0.990] |
0.978 [0.977, 0.979] |
|
| Goodness of Fit Statistics | |||||||||
| AIC | 99247.09§ | 138675.80§ | 160864.20§ | 164939.94§ | 222212.35§ | 296036.94§ | 315983.76§ | 292259.87§ | |
| SC | 99361.06§ | 138789.77§ | 160978.17§ | 165053.91§ | 222326.33§ | 296150.92§ | 316097.72§ | 292373.85§ | |
| LR | 2890.06† | 2789.31† | 1385.44† | 2221.64† | 5071.38† | 4576.90† | 1758.50† | 3858.02† | |
| HL | 97.20* | 10.92 | 9.16 | 12.31 | 19.819* | 13.61 | 22.54* | 11.63 | |
| MZ | 0.1832 | 0.1275 | 0.0552 | 0.0816 | 0.1242 | 0.0813 | 0.0313 | 0.0762 | |
Note.
p≤0.05
p≤0.001
Small positive or negative effect (1.44 ≤OR ≤ 0.70)
value ≤ intercept only model
Reference group for race comparisons = Caucasian
Reference group for Cognitive Impairment = No impairment
Afr Amer = African American
Mod Cog Imp = Moderate Cognitive Impairment
Severe Cog Imp = Severe Cognitive Impairment
AIC = Akaike Information Criterion, SC = Schwarz Criterion, LR = Likelihood ratio, HL = Hosmer Lemeshow, MZ = McKelvey-Zavoina R2
Table 6.
Odds ratios [95% CI] for resident characteristics predicting important activity preferences
| FRESH | NEWS | FAVRTE | RELIG | READ | MUSIC | ANIMAL | GROUP | |
|---|---|---|---|---|---|---|---|---|
| Female | 0.802 [0.779, 0.826] |
0.860 [0.835, 0.886] |
1.252 [1.215, 1.291] |
1.931‡ [1.891, 1.971] |
1.492‡ [1.461, 1.524] |
1.256 [1.228, 1.283] |
1.058 [1.039, 1.078] |
1.467‡ [1.439, 1.496] |
| Married | 0.996 [0.967, 1.025] |
1.134 [1.100, 1.170] |
0.952 [0.923, 0.982] |
1.130 [1.106, 1.155] |
1.145 [1.120, 1.171] |
0.939 [0.918, 0.961] |
0.974 [0.956, 0.993] |
0.977 [0.958, 0.997] |
| Afr Amer | 1.177 [1.119, 1.239] |
1.324 [1.255, 1.398] |
1.288 [1.216, 1.365] |
3.098‖ [2.951, 3.252] |
0.979 [0.944, 1.016] |
1.671‡ [1.599, 1.746] |
0.528‡ [0.512, 0.545] |
1.656‡ [1.596, 1.718] |
| Hispanic | 1.304 [1.205, 1.410] |
0.976 [0.909, 1.049] |
1.333 [1.223, 1.453] |
2.686‖ [2.508, 2.878] |
0.852 [0.809, 0.898] |
1.645‡ [1.542, 1.755] |
0.862 [0.824, 0.903] |
1.718‡ [1.627, 1.815] |
| Other Race | 1.025 [0.926, 1.135] |
0.813 [0.739, 0.896] |
1.207 [1.073, 1.358] |
1.084 [1.005, 1.169] |
0.884 [0.820, 0.953] |
1.019 [0.941, 1.104] |
0.499‡ [0.468, 0.533] |
1.360 [1.263, 1.464] |
| Mod Cog Imp | 1.025 [0.993, 1.058] |
0.660‡ [0.639, 0.682] |
0.835 [0.807, 0.864] |
1.064 [1.039, 1.090] |
0.782 [0.763, 0.801] |
1.170 [1.141, 1.200] |
1.122 [1.100, 1.146] |
1.046 [1.023, 1.069] |
| Sev Cog Imp | 1.072 [1.031, 1.115] |
0.418‡ [0.403, 0.433] |
0.744 [0.715, 0.776] |
1.170 [1.134, 1.207] |
0.673‡ [0.654, 0.693] |
1.391 [1.345, 1.438] |
1.253 [1.221, 1.285] |
1.226 [1.192, 1.261] |
| Depressed |
0.773‡ [0.739, 0.810] |
0.675‡ [0.645, 0.706] |
0.577‡ [0.551, 0.604] |
0.850 [0.820, 0.882] |
0.718‡ [0.693, 0.745] |
0.794 [0.765, 0.825] |
0.945 [0.915, 0.976] |
0.658‡ [0.636, 0.680] |
| Function | 0.978 [0.975, 0.981] |
1.000 [0.997, 1.003] |
0.990 [0.986, 0.993] |
0.998 [0.996, 1.000] |
0.983 [0.980, 0.985] |
1.007 [1.005, 1.009] |
1.007 [1.005, 1.009] |
0.995 [0.993, 0.997] |
| Age | 0.991 [0.990, 0.993] |
1.008 [1.006, 1.010] |
0.998 [0.996, 1.000] |
1.018 [1.017, 1.020] |
1.001 [0.999, 1.002] |
1.006 [1.005, 1.007] |
0.985 [0.984, 0.986] |
1.008 [1.006, 1.009] |
| Goodness of Fit Statistics | ||||||||
| AIC | 165412.79§ | 153492.24§ | 141672.78§ | 246974.08§ | 242855.47§ | 233335.13§ | 312845.77§ | 283302.37§ |
| SC | 165526.77§ | 153606.21§ | 141786.75§ | 247088.05§ | 242969.45§ | 233449.11§ | 312959.75§ | 283416.35§ |
| LR | 893.84† | 2872.10† | 1280.57† | 8222.94† | 3206.92† | 2298.37† | 2652.01† | 3995.30† |
| HL | 3.28 | 29.59* | 8.75 | 43.32* | 32.68* | 50.97* | 22.64* | 10.88 |
| MZ | 0.0379 | 0.1047 | 0.0561 | 0.1841 | 0.0723 | .0622 | 0.0447 | .0768 |
Note.
p≤0.05
p≤0.001
Small positive or negative effect (1.44 ≤OR ≤ 0.70)
Value ≤ intercept only model
Moderate positive effect (OR ≥ 2.47)
Reference group for race comparisons = Caucasian
Reference group for Cognitive Impairment = No impairment
Afr Amer = African American
Mod Cog Imp = Moderate Cognitive Impairment
Severe Cog Imp = Severe Cognitive Impairment
AIC = Akaike Information Criterion, SC = Schwarz Criterion, LR = Likelihood ratio, HL = Hosmer Lemeshow, MZ = McKelvey-Zavoina R2
Discussion
The results of this study demonstrate all items in the PAT were important to the majority of residents, suggesting the questionnaire assesses important preferences. However, the findings also demonstrate the PAT measures variation in resident preferences both across items and individuals. These variations may have practical implications and highlight several areas and resident subgroups where systematic approaches to care planning may be useful, and others where a high level of individualization may be needed.
Across items, some preferences were consistently rated important. Consistent with other research19, having family involved in discussions about care was rated important most frequently. Person-centered care philosophy is highly grounded in the assumption that autonomy and individual choice are important to residents3,20. However, the results of this study suggest focusing PCC practices on family involvement may be just as critical as providing care and activity choices and options for residents. More research on the type and intensity of family integration in decision-making is needed.
After family involvement, several items were also rated important fairly consistently that reflect an interest in choice and individualized care (e.g. caring for one’s own belongings, choosing one’s bedtime). This finding supports the continued need for systematic changes to practices facility-wide to support choice and individualization such as flexible wake, sleep and meal schedules that accommodate residents decisions about their own bedtimes and mealtimes for example. The third most frequently reported preference, engaging in one’s favorite activities represents a highly individualized preference with numerous potential permutations that could make it difficult to systematically address at a facility level. PCC philosophy embraces spontaneity in activities and engagement in meaningful activity. However, meaningful activities can be rare21 in nursing homes and more research is needed to better understand how to scale up and implement varied, spontaneous, meaningful, and individualized activities in sustainable ways.
Other preferences, such as being around animals, locking belongings, and having snacks between meals were not consistently rated important. This suggests a possible need to structure care less systematically and accommodate more individualization in these areas. Some models of PCC promote certain practices at a system level, making it important to consider how to balance the group approaches with individual preferences in these areas. As an example, some PCC models emphasize integration of animals in the facility22. If a facility implements such a model, considering ways to accommodate the preferences of residents who do not want to be around animals may be important.
The present study highlights subtle but meaningful differences in the importance of preferences across residents. Possible depression and cognitive impairment are associated with a lower likelihood of rating many preferences important. This suggests identification and treatment of depression and involvement of proxy reporters for residents with cognitive impairment may be critical to assessment and care planning for these residents. Treatment for depression was not controlled in this study and research is needed to examine the relationship between depression, depression treatment, and preferences. It is also unclear if cognitive impairment influences preferences, the expression of preferences, or the ability to assess preferences. Longitudinal research is needed to understand how the development and worsening of cognitive impairment impacts preferences. Past research has demonstrated that assessment of care quality23 and knowledge of certain care preferences such as for end of life treatment24 can vary between residents and proxies. Research is needed to examine the congruence of daily care and activity preference reports between residents, family, and staff to understand the reliability of proxy preference reports for residents with cognitive impairment.
Preferences also varied by race and gender. Religion was found to be more important to African Americans and Hispanics than Caucasians. This is consistent with research that has demonstrated higher religiosity among African Americans and Hispanics than Caucasians25,26 and suggests additional consideration of type and intensity of religious choices for non-Caucasian residents or in facilities with high diversity may be needed. Further, given that females were more likely than males to rate most preferences important, research is needed to learn more about male preferences for daily care and activities. There may be a practical need to adapt preference assessments and care planning in facilities with high proportions of male residents such as VA Community Living Centers.
While some resident characteristics were found to be significant predictors of preferences, others were not and of those that were, they explained only a small amount of variation in preferences. Function and age were not significant predictors of preferences. Similar to the response shift that occurs in health related quality of life where individuals rate quality of life the same even as health declines27, this finding could suggest resident perceptions of important preferences do not change as residents age or lose function. Alternatively, it could suggest the items reflect important preferences despite age or level of function. Longitudinal research is needed to better understand the relationship of age and function and preferences. Further, the small amount of variation explained by resident characteristics is consistent with other research that has shown there are situational dependencies in preferences28. More research is needed to determine the factors that influence preferences.
While not a central goal of the study, the data also revealed that residents rarely reported preferences as ‘Important But Can’t Do/No Choice’. This may indicate residents generally do not feel they have restricted choices or options and may be an indication that PCC is exceedingly widespread. Alternatively, residents may not report a lack of choice or ability. It is possible the assessment process makes it difficult for residents to report lack of choice or that admission is too early for residents to make an assessment of their capacities and options in the facility. Nonetheless, some residents did use this option with it being selected more often for favorite activities and reading.
Nationally, there is a significant amount of support for PCC. The results of this study suggest the focus in PCC to individualize care is important to the vast majority of residents. Previous research however, has highlighted a gap in fulfillment of preferences like these in practice. Prior observational studies have suggested that staff provide little to no choice about many aspects of daily care29–31 which could undermine efforts to provide person-centered care. The research reported here is only the first step in understanding the relevance of preferences for daily care. Future research that examines translation of preference assessment into practice is a critical next step to ensure resident preferences are fulfilled and person-centered care delivered.
Limitations
Only residents who could complete the resident interview versions of the preferences, cognition, and mood assessments were included and results might not generalize to staff observations of preferences for those residents who cannot complete the interview. Whether residents were appropriately screened and correctly assessed using the resident interview version of the PAT was not examined directly in this study. Consistent with rates of resident interview for the BIMS, PHQ9 and pain assessments32, approximately 90% of the records in the full dataset were marked as residents should be interviewed using the PAT. However, approximately, 6% of residents were classified as rarely/never understood, suggesting perhaps not all eligible residents were interviewed. Future studies are needed to determine how often residents are appropriately screened for the PAT and the significance and factors related to inappropriate screening.
Previous research has suggested residents may accommodate their preferences and expectations for care to reflect facility routines30,33. The use of admission assessments in this study may reflect what resident preferences look like before accommodation happens. However, it is unknown how quickly residents accommodate to the environment or what impact that accommodation might have on how residents rate preferences assessed in the PAT. Preferences may therefore be different if assessed at different points in time and residents who have different expectations about their length of stay (ie. short or long) may report preferences differently. Future research is needed to characterize differences in preferences between long and short stay residents, examine how preferences change over the course of a stay, and determine the factors that can assist residents in expressing and sustaining their preferences over time.
Finally, only residents aged 65 and older were included precluding generalizing results to younger residents. assessor, facility, and geographic effects were not controlled in this study and further research is needed to determine whether those factors are associated with preferences.
Conclusions
Despite a national emphasis on PCC, it is unclear how to best assess resident preferences and integrate them in to daily care. The MDS 3.0 PAT is a standardized tool that can be useful as an initial, abbreviated approach for capturing variation in resident preferences. This study highlights how some preferences are consistently important to residents and others that are highly individual. This finding may have implications for structuring care delivery in ways that balance the needs of groups of residents with those of individuals. The results also demonstrate that preferences vary across residents. Additional assessment and care planning may be needed for residents with depression or cognitive impairment as well as non-Caucasians and males. More research is needed to understand how to best use knowledge of resident preferences to guide care planning or deliver daily care.
Supplementary Material
Acknowledgments
Support for VA/CMS data is provided by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development, VA Information Resource Center (Project Numbers SDR 02-237 and 98-004). Postdoctoral training support and traineeship support was provided during the conduct of this study by the William S. Middleton Veterans Affairs Hospital in Madison, WI and the VA Office of Academic Affairs. The views and content expressed in this article is solely the responsibility of the authors and does not necessarily reflect the official views of the Department of Veteran Affairs or the U.S. government.
References
- 1.Simmons SF, Rahman AN. Next steps for achieving person-centered care in nursing homes. J Am Med Dir Assoc. 2014;15:615. doi: 10.1016/j.jamda.2014.06.008. http://dx.doi.org/10.1016/j.jamda.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 2.Miller SC, Looze J, Shield R, et al. Culture change practice in US nursing homes: Prevalence and variation by state Medicaid reimbursement policies. Gerontologist. 2014;54:434–445. doi: 10.1093/geront/gnt020. https://doi.org/10.1093/geront/gnt020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Koren MJ. Person-centered care for nursing home residents: The culture-change movement. Health Aff. 2010;29:312–317. doi: 10.1377/hlthaff.2009.0966. https://doi.org/10.1377/hlthaff.2009.0966. [DOI] [PubMed] [Google Scholar]
- 4.Pioneer Network. What is culture change. n.d.; Available from: https://www.pioneernetwork.net/CultureChange/Whatis/
- 5.Kane RA, Lum TY, Cutler LJ, et al. Resident outcomes in small-house nursing homes: A longitudinal evaluation of the initial Green House program. J Am Geriatr Soc. 2007;55:832–839. doi: 10.1111/j.1532-5415.2007.01169.x. http://doi.org/10.1111/j.1532-5415.2007.01169.x. [DOI] [PubMed] [Google Scholar]
- 6.Robinson SB, Rosher RB. Tangling with the barriers to culture change: Creating a resident-centered nursing home environment. J Gerontol Nurs. 2006;32:19. doi: 10.3928/00989134-20061001-04. [DOI] [PubMed] [Google Scholar]
- 7.Sloane PD, Hoeffer B, Mitchell CM, et al. Effect of person-centered showering and the towel bath on bathing-associated aggression, agitation, and discomfort in nursing home residents with dementia: A randomized, controlled trial. J Am Geriatr Soc. 2004;52:1795–1804. doi: 10.1111/j.1532-5415.2004.52501.x. [DOI] [PubMed] [Google Scholar]
- 8.Chenoweth L, King MT, Jeon YH, et al. Caring for Aged Dementia Care Resident Study (CADRES) of person-centred care, dementia-care mapping, and usual care in dementia: A cluster-randomised trial. Lancet Neurol. 2009;8:317–325. doi: 10.1016/S1474-4422(09)70045-6. [DOI] [PubMed] [Google Scholar]
- 9.Elliot A, Cohen LW, Reed D, et al. A “recipe” for culture change? Findings from the THRIVE survey of culture change adopters. Gerontologist. 2014;54:S17–S24. doi: 10.1093/geront/gnt133. https://doi.org/10.1093/geront/gnt133. [DOI] [PubMed] [Google Scholar]
- 10.Saliba D, Buchanan J. Making the investment count: Revision of the Minimum Data Set for nursing homes, MDS 3.0. J Am Med Dir Assoc. 2012;13:602–610. doi: 10.1016/j.jamda.2012.06.002. http://doi.org/10.1016/j.jamda.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 11.Morley JE. Minimum data set 3.0: A giant step forward. J Am Med Dir Assoc. 2013;14:1–3. doi: 10.1016/j.jamda.2012.10.014. http://doi.org/10.1016/j.jamda.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 12.Housen P, Shannon GR, Simon B, et al. Why not just ask the resident? Refinement of a preference assessment tool for nursing homes. J Gerontol Nurs. 2009;35:40–49. doi: 10.3928/00989134-20091001-01. https://doi.org/10.3928/00989134-20091001-01. [DOI] [PubMed] [Google Scholar]
- 13.Wysocki A, Thomas KS, Mor V. Functional improvement among short-stay nursing home residents in the MDS 3.0. J Am Med Dir Assoc. 2015;16:470–474. doi: 10.1016/j.jamda.2014.11.018. http://doi.org/10.1016/j.jamda.2014.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. J Gerontol A Bio Sci Med Sci. 1999;54:M546–M553. doi: 10.1093/gerona/54.11.m546. [DOI] [PubMed] [Google Scholar]
- 15.Saliba D, DiFilippo S, Edelen MO, et al. Testing the PHQ-9 interview and observational versions (PHQ-9 OV) for MDS 3.0. J Am Med Dir Assoc. 2012;13:618–625. doi: 10.1016/j.jamda.2012.06.003. http://doi.org/10.1016/j.jamda.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 16.Saliba D, Jones M, Streim J, et al. Overview of significant changes in the Minimum Data Set for nursing homes version 3.0. J Am Med Dir Assoc. 2012;13:595–601. doi: 10.1016/j.jamda.2012.06.001. https://doi.org/10.1016/j.jamda.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 17.Kroencke K, Spitzer R, Williams J. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. https://doi.org/10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saliba D, Buchanan J, Edelen MO, et al. MDS 3.0: Brief interview for mental status. J Am Med Dir Assoc. 2012;13:611–617. doi: 10.1016/j.jamda.2012.06.004. https://doi.org/10.1016/j.jamda.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 19.Bangerter LR, Van Haitsma K, Heid AR, et al. “Make me feel at ease and at home”: Differential care preferences of nursing home residents. Gerontologist. 2016;56:702–713. doi: 10.1093/geront/gnv026. https://doi.org./10.1093/geront/gnv026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.White-Chu EF, Graves WJ, Godfrey SM, et al. Beyond the medical model: The culture change revolution in long-term care. J Am Med Dir Assoc. 2009;10:370–378. doi: 10.1016/j.jamda.2009.04.004. https://doi.org/10.1016/j.jamda.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 21.Morley JE, Philpot CD, Gill D, et al. Meaningful activities in the nursing home. J Am Med Dir Assoc. 2014;15:79. doi: 10.1016/j.jamda.2013.11.022. http://doi.org/10.1016/j.jamda.2013.11.022. [DOI] [PubMed] [Google Scholar]
- 22.Eden Alternative. The principles of the Eden Alternative. n.d.; Available from: http://www.edenalt.org/about-the-eden-alternative/mission-vision-values/
- 23.Kane RL, Kane RA, Bershadsky B, et al. Proxy sources for information on nursing home residents’ quality of life. J Gerontol B Psychol Sci Soc Sci. 2005;60:S318–S325. doi: 10.1093/geronb/60.6.s318. [DOI] [PubMed] [Google Scholar]
- 24.Shalowitz DI, Garrett-Mayer E, Wendler D. The accuracy of surrogate decision makers: A systematic review. Arch Intern Med. 2006;166:493–497. doi: 10.1001/archinte.166.5.493. https://doi.org/10.1001/archinte.166.5.493. [DOI] [PubMed] [Google Scholar]
- 25.Levin J, Chatters LM, Taylor RJ. Religion, health and medicine in African Americans: Implications for physicians. J Natl Med Assoc. 2005;97:237. [PMC free article] [PubMed] [Google Scholar]
- 26.Gillum F, Griffith DM. Prayer and spiritual practices for health reasons among American adults: The role of race and ethnicity. J Relig Health. 2010;49:283–295. doi: 10.1007/s10943-009-9249-7. https://doi.org/10.1007/s10943-009-9249-7. [DOI] [PubMed] [Google Scholar]
- 27.Schwartz CE, Bode R, Repucci N, et al. The clinical significance of adaptation to changing health: A meta-analysis of response shift. Qual Life Res. 2006;15:1533–1550. doi: 10.1007/s11136-006-0025-9. https://doi.org/10.1007/s11136-006-0025-9. [DOI] [PubMed] [Google Scholar]
- 28.Heid AR, Eshraghi K, Duntzee CI, et al. “It depends”: Reasons why nursing home residents change their minds about care preferences. Gerontologist. 2016;56:243–255. doi: 10.1093/geront/gnu040. https://doi.org/10.1093/geront/gnu040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Simmons SF, Rahman A, Beuscher L, et al. Resident-directed long-term care: Staff provision of choice during morning care. Gerontologist. 2011;51:867–875. doi: 10.1093/geront/gnr066. https://doi.org/10.1093/geront/gnr066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Simmons SF, Durkin DW, Rahman AN, et al. Resident characteristics related to the lack of morning care provision in long-term care. Gerontologist. 2012;53:151–161. doi: 10.1093/geront/gns065. https://doi.org/10.1093/geront/gns065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schnelle JF, Bertrand R, Hurd D, et al. Resident choice and the survey process: The need for standardized observation and transparency. Gerontologist. 2009;49:517–524. doi: 10.1093/geront/gnp050. https://doi.org/10.1093/geront/gnp050. [DOI] [PubMed] [Google Scholar]
- 32.Thomas KS, Wysocki A, Intrator O, et al. Finding Gertrude: The resident’s voice in Minimum Data Set 3.0. J Am Med Dir Assoc. 2014;15:802–806. doi: 10.1016/j.jamda.2014.01.012. https://doi.org/10.1016/j.jamda.2014.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Simmons S, Levy-Storms L. The effect of staff care practices on nursing home residents’ preferences: Implications for individualizing care. J Nutr Health Aging. 2006;10:216. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


