Abstract
Anticoagulant-related nephropathy (ARN) was initially described in patients on warfarin (as warfarin-related nephropathy) and recently in those using dabigatran. Herein, we report clinical history and kidney biopsy findings in a patient on apixaban (Eliquis). Initiation of treatment with apixaban resulted in aggravation of preexisting mild acute kidney injury (AKI). A few days after apixaban therapy, the patient became oligoanuric, and kidney biopsy showed severe acute tubular necrosis with numerous occlusive red blood cell casts. Only one out of 68 glomeruli with open capillary loops had small segmental cellular crescent. Therefore, there was major discrepancy between the degree of glomerular injury and the glomerular hematuria. Considering that the onset of this AKI was associated with apixaban treatment initiation, we propose that this patient had ARN associated with factor Xa inhibitor (apixaban), which has not previously been described. Monitoring of kidney function is recommended after initiation of anticoagulant therapy.
Keywords: Acute kidney injury, Anticoagulant-related nephropathy, Kidney biopsy
Introduction
Warfarin-related nephropathy (WRN) occurs in warfarin-treated patients who develop unexpected acute kidney injury (AKI) in the setting of supra-therapeutic international normalized ratio [1–3]. Kidney biopsy after reversal of the coagulopathy reveals severe glomerular hemorrhage (tubules filled with red blood cell [RBC] casts). Patients with chronic kidney disease (CKD) are particularly susceptible to WRN [1,2]. There is emerging evidence that WRN is only a subset of a broader anticoagulant-related nephropathy (ARN). AKI associated with dabigatran (a direct thrombin inhibitor) use has been reported in humans [4,5] and experimental animals [6]. Recent data from large clinical trials using direct oral anticoagulants (DOAC) indicate that there is a significant decline in kidney function in patients on anticoagulation, even though this decline is less rapid in patients on dabigatran then on warfarin [7,8].
Until now, there has been no evidence that Factor Xa inhibitors can induce ARN. Herein, we report a patient who developed severe oligoanuric AKI shortly after initiation of treatment with apixaban (Eliquis, Bristol-Myers Squibb, New York, NY, USA) and provide kidney biopsy data supporting that the AKI was, at least mildly, associated with ARN.
Case report
Clinical history
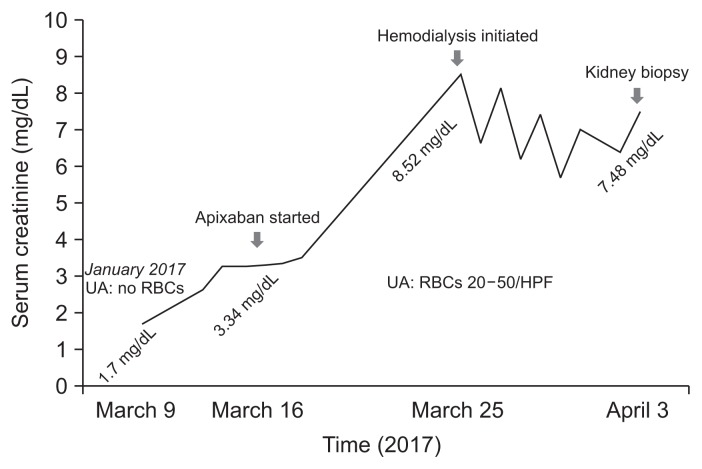
The patient was an 82-year-old Caucasian female with history of hypertension, chronic obstructive pulmonary disease (COPD), coronary artery disease, congestive heart failure, and CKD stage III with baseline serum creatinine between 1.5 and 2.0 mg/dL. In 2013, she was found to have methicillin-resistant Staphylococcus aureus (MRSA) nasal colonization. On March 9, 2017, she presented with symptoms of COPD exacerbation and AKI with a serum creatinine of 1.7 mg/dL. Her serum creati-nine plateaued at a 3.26 mg/dL by March 13, 2017 (Fig. 1). She developed new-onset atrial fibrillation, for which treatment with apixaban (Eliquis) was initiated on March 15, 2017. The dose of apixaban was 2.5 mg (per oral, twice a day), based on her age over 80 and creatinine over 1.5 mg/dL.
Figure 1. Serum creatinine changes in association with apixaban treatment.
Changes in serum creatinine level are shown by a solid line. Initiation of treatment with apixaban and kidney biopsy time are depicted by arrows. Hematuria prior and after apixaban therapy is shown as urinalysis (UA). Specific dates are depicted on the X axis, and the corresponding serum creatinine levels are shown above.
HPF, high power field; RBC, red blood cell.
The patient had a CHAD2-VASC score of 6, and rate control was achieved. The plan was to cardiovert in 3 to 4 weeks, but she spontaneously converted to normal sinus rhythm during that time. Based on her echocardiogram performed on March 31, 2017, non-valvular atrial fibrillation was diagnosed (only mild mitral regurgitation reported).
Serum creatinine was 3.5 mg/dL on March 25, 2017, and she was noted to have 1.1 g of proteinuria on a spot urine protein: creatinine ratio. She presented on March 25, 2017 with oligoanuria and serum creatinine of 8.52 mg/dL; hemodialysis was initiated.
The patient did not exhibit any symptoms or adverse effects that were attributable to apixaban, such as overt hemorrhage. For this reason, Factor Xa level was not tested. However, a urinalysis did reveal microscopic hematuria in the setting of a Foley catheter.
Urinalysis at the time of this presentation showed a large amount of blood, with 20–50 RBCs per high power field, which was not apparent two months prior (Fig. 1). She was found to be positive for p-ANCA (perinuclear anti-neutrophil cytoplasmic antibodies; subsequent testing of antibody to myeloperoxidase [MPO] was negative at < 0.2), whereas cytoplasmic ANCA (c-ANCA), antinuclear antibody (ANA), and anti-glomerular basement membrane (GBM) antibodies were negative, as was her hepatitis profile. Serum complement levels and rheumatoid factor were normal. During her first admission, she was given steroids for COPD exacerbation. During the second admission, she received three doses of methylprednisolone (Solu-Medrol) 500 mg/day starting on March 26, 2017 for suspected ANCA-related vasculitis. Three sets of blood cultures drawn over both admissions were all negative, and transthoracic echocardiogram was negative for vegetation. The patient remained afebrile throughout both admissions. A kidney biopsy was performed on April 3, 2017 after apixaban was stopped; however, she did receive subcutaneous heparin. Unfortunately, the patient remains dialysis dependent as of August 2017.
Pathologic findings
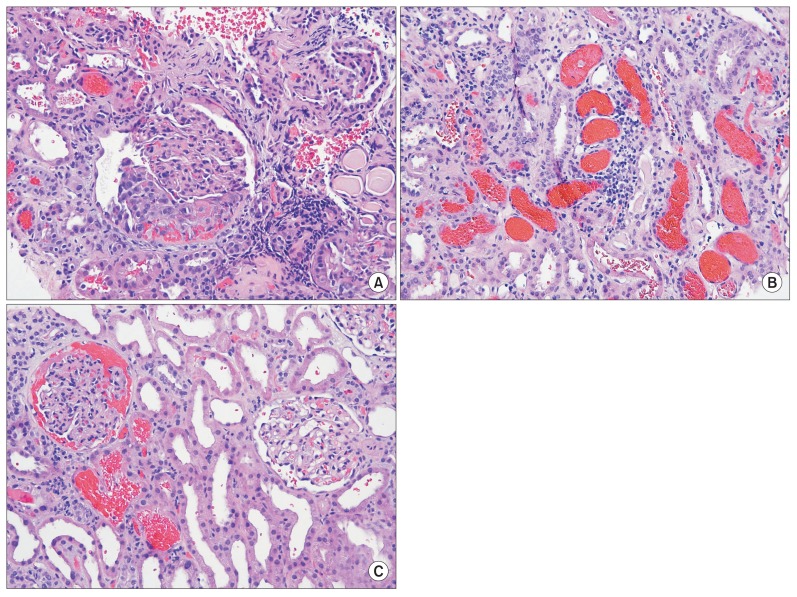
The kidney biopsy specimen contained 7 cores of renal parenchyma. Tissue submitted for light microscopy contained an ample amount of renal cortex. Paraffin sections were stained with hematoxylin and eosin, periodic acid-Schiff (PAS), PAS-trichrome [9], and methenamine silver stains. Up to 157 glomeruli per section were identified by light microscopy. At least 107 of these glomeruli were obsolescent and localized to the areas of renal cortical scarring. Distant from the scar tissue, there were 50 glomeruli, and up to 22 of them were obsolescent, scattered throughout the non-scarred renal cortex. In one glomerulus, a small segmental cellular crescent was noted (Fig. 2A). In three additional glomeruli, small segmental areas of necrosis were present without associated cellular crescents. The remaining glomeruli with open capillary loops appeared unremarkable. A striking finding was the prominent acute tubular injury with flattening and irregularities of the tubular epithelium in most tubules. Numerous tubules were occluded by RBC casts (Fig. 2B). Occasional glomerular RBC filled Bowman’s space (Fig. 2C). There was mild to moderate interstitial edema associated with mild to moderate interstitial inflammatory cell infiltrate. The inflammatory cells were mainly mononuclear cells admixed with occasional plasma cells and a few polymorphonuclear leukocytes. The degrees of interstitial fibrosis and tubular atrophy in the non-scarred areas were mild to moderate (approximately 30%). Interlobular and arcuate arteries in the non-scarred areas showed mild to moderate fibrous intimal thickening. Arteriolar hyaline change was moderate and focal.
Figure 2. Light microscopy kidney biopsy findings (H&E stain).
(A) A single small segmental cellular crescent is noted in one out of 68 glomeruli with open capillary loops (×100). (B) Numerous occlusive red blood cell casts were seen in the tubules. Acute tubular necrosis is present (×100). (C) Red blood cells were filling Bowman’s space in some glomeruli (×200).
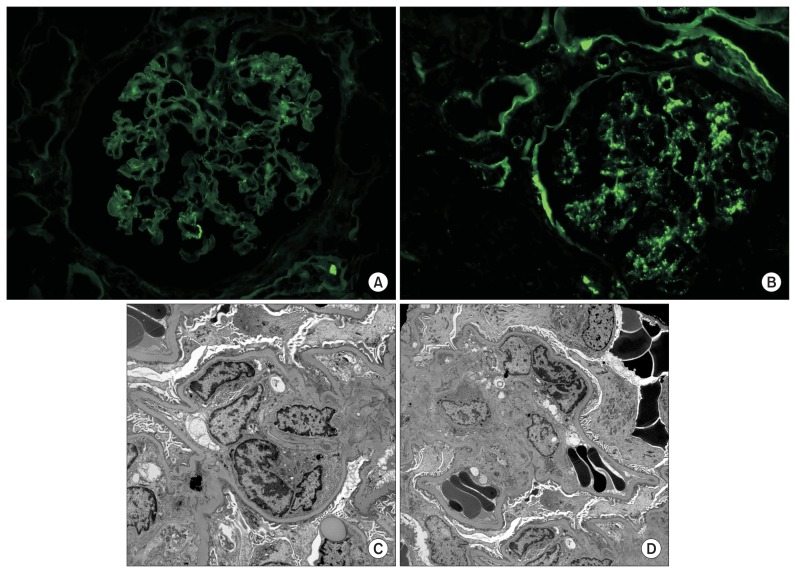
Frozen sections cut from the tissue submitted for immunofluorescence contained renal cortex with up to 54 glomeruli. Portions of the frozen sections were also scarred, and 37 glomeruli were obsolescent. Cellular crescents or glomerular necrosis was not seen. Direct immunofluorescence with the standard panel of antibodies was performed. Mild diffuse granular mesangial staining for C3 and mild diffuse but segmental granular mesangial staining for immunoglobulin A (IgA) and kappa and lambda light chains was seen in the glomeruli (Fig. 3A, B). All other stains were negative in the glomeruli.
Figure 3. Immunofluorescence and electron microscopy findings.
(A) Trace segmental granular staining in the mesangium was seen by direct immunofluorescence with an antibody to immunoglobulin A (fluorescein isothiocyanate [FITC], ×400). (B) Mild granular staining in the mesangium was seen by direct immunofluorescence with an antibody to C3 (FITC, ×400). (C) Occasional small electron dense deposits were seen in the mesangium by ultrastructural examination (×5,000). (D) Dysmorphic red blood cells in Bowman’s space were seen by electron microscopy. Of note, no deposits were seen in the glomerular basement membrane of the mesangium in this segment of the glomerulus (×4,000).
Semi-thin sections of the tissue submitted for electron microscopy contained renal cortex with one light microscopically unremarkable glomerulus. Ultrastructurally, scattered small mesangial and intramembranous electron-dense deposits were identified (Fig. 3C). The GBM was of normal thickness and texture. Podocyte foot process effacement was mild. No endothelial tubuloreticular inclusions were identified. Dysmorphic RBCs were seen in Bowman’s space (Fig. 3D).
The etiology of this chronic kidney injury is difficult to determine based on kidney biopsy findings alone. Globally sclerosed glomeruli did not show obvious fibrous crescents; therefore, they are probably not related to crescentic glomerulonephritis. Because of the somewhat zonal renal cortical scarring, it is possible that this chronic kidney injury is of the vascular origin and might be related to antiphospholipid antibodies, preeclampsia, or other vasculopathies. Chronic pyelonephritis/reflux nephropathy is also a consideration, but this diagnosis could not be made based on the kidney biopsy findings alone. It is difficult to differentiate between IgA nephropathy and infection-related glomerulonephritis based on kidney biopsy findings. However, the absence of hematuria history favors infection-associated glomerulonephritis.
Discussion
To the best of our knowledge, this is the first case report of AKI associated with treatment with a Factor Xa inhibitor. We and others previously reported several cases of AKI associated with warfarin or dabigatran [3–5,10,11].
The clinical history and kidney biopsy findings in this patient strongly indicate that an oligoanuric AKI can be associated with anticoagulation therapy. Clinically, serum creatinine was increased from baseline before the initiation of anticoagulation in the present patient, but it was plateauing. After starting apixaban, serum creatinine significantly increased (from 3.2 to 8.5 mg/dL) within a few days, and the patient became oligoanuric. This was associated with new hematuria. All of these clinical symptoms have been seen in patients with WRN or dabigatran-associated AKI. Pathologic findings showed significant discrepancy between the number of tubular RBC casts and the degree of glomerular injury. The most striking biopsy finding was prominent glomerular hematuria, and the occlusive RBC casts likely contributed to the oligoanuric AKI. Even though patient had positive p-ANCA, a subsequent test for MPO antibody was negative. There was only one cellular crescent in the entire biopsy specimen with at least 68 non-sclerotic glomeruli, and only three glomeruli showed small areas of segmental necrosis. Therefore, there is a major discrepancy between the degree of AKI, the degree of acute tubular necrosis with occlusive RBC casts, and the subtle crescentic and necrotizing glomerular changes. The presence of mild, mainly mesangial IgA- and C3-containing immune complex deposition is also unusual in ANCA-associated glomerulonephritis. In our experience, focal crescentic glomerulonephritis can be associated with infection, including endocarditis [12]. The pattern of C3-dominant glomerular immune complex deposits raises the possibility of an underlying staphylococcus infection, in spite of negative blood cultures. It is of interest that this patient was found to have nasal colonization of MRSA in 2013. Also, ANCA can be positive in 20–30% of patients with infection-associated glomerulonephritis [12]. The rapid decline in kidney function with oligoanuria developed after starting anticoagulation with apixaban; therefore, we believe that anticoagulation aggravated preexisting kidney injury and resulted in severe glomerular hemorrhage with occlusive RBC casts and ATN, which are features of ARN. One of the possible etiologies for this ARN is preexisting AKI; because renal excretion accounts for about 27% of the total clearance of apixaban [13], it is possible that there was an overdose of apixaban associated with reduced elimination of the drug. However, even without the overdose, anticoagulation might have increased glomerular hematuria in this patient with very focal segmental and necrotizing glomerulonephritis and mild mesangial immune complex deposits.
There is growing evidence that ARN is a potentially serious complication of anticoagulation therapy. In addition to warfarin, there are several recent case reports that AKI with hematuria and RBC tubular casts can develop in patients on dabigatran treatment [4,11]. The most rigorous attempt to understand the renal risks of warfarin versus DOAC was the recent retrospective analysis of RE-LY [8]. That analysis showed substantial glomerular filtration rate (eGFR) loss during follow up in both the warfarin and dabigatran cohorts, at about 2–3 mL/min/year. This is two to three times greater than the expected eGFR decline attributable to aging (1 mL/min/year) [14].
In conclusion, we present the first documented by kidney biopsy evidence that patients on anticoagulation treatment with Factor Xa inhibitor can develop glomerular hematuria and AKI. In this particular patient, there was a constellation of other factors that probably was responsible for this AKI; nevertheless, this is a confirmation that another class of DOAC can induce AKI in susceptible patients. We suggest that kidney function should be closely monitored in all CKD patients after initiation of anticoagulation therapy.
Footnotes
Conflicts of interest
All authors have no conflicts of interest to declare.
References
- 1.Brodsky SV, Collins M, Park E, et al. Warfarin therapy that results in an International Normalization Ratio above the therapeutic range is associated with accelerated progression of chronic kidney disease. Nephron Clin Pract. 2010;115:c142–c146. doi: 10.1159/000312877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brodsky SV, Nadasdy T, Rovin BH, et al. Warfarin-related nephropathy occurs in patients with and without chronic kidney disease and is associated with an increased mortality rate. Kidney Int. 2011;80:181–189. doi: 10.1038/ki.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brodsky SV, Satoskar A, Chen J, et al. Acute kidney injury during warfarin therapy associated with obstructive tubular red blood cell casts: a report of 9 cases. Am J Kidney Dis. 2009;54:1121–1126. doi: 10.1053/j.ajkd.2009.04.024. [DOI] [PubMed] [Google Scholar]
- 4.Kadiyala D, Brewster UC, Moeckel GW. Dabigatran induced acute kidney injury. Proceedings of The American Society of Nephrology annual meeting; November 1–4, 2012; San Diego. San Diego: The American Society of Nephrology; 2012. FR-PO1122. [Google Scholar]
- 5.Berger R, Salhanick SD, Chase M, Ganetsky M. Hemorrhagic complications in emergency department patients who are receiving dabigatran compared with warfarin. Ann Emerg Med. 2013;61:475–479. doi: 10.1016/j.annemergmed.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 6.Ryan M, Ware K, Qamri Z, et al. Warfarin-related nephropathy is the tip of the iceberg: direct thrombin inhibitor dabigatran induces glomerular hemorrhage with acute kidney injury in rats. Nephrol Dial Transplant. 2014;29:2228–2234. doi: 10.1093/ndt/gft380. [DOI] [PubMed] [Google Scholar]
- 7.Wheeler DS, Giugliano RP, Rangaswami J. Anticoagulation-related nephropathy. J Thromb Haemost. 2016;14:461–467. doi: 10.1111/jth.13229. [DOI] [PubMed] [Google Scholar]
- 8.Böhm M, Ezekowitz MD, Connolly SJ, et al. Changes in renal function in patients with atrial fibrillation: an analysis from the RE-LY trial. J Am Coll Cardiol. 2015;65:2481–2493. doi: 10.1016/j.jacc.2015.03.577. [DOI] [PubMed] [Google Scholar]
- 9.Brodsky SV, Albawardi A, Satoskar AA, Nadasdy G, Nadasdy T. When one plus one equals more than two--a novel stain for renal biopsies is a combination of two classical stains. Histol Histopathol. 2010;25:1379–1383. doi: 10.14670/HH-25.1379. [DOI] [PubMed] [Google Scholar]
- 10.Mendonca S, Gupta D, Valsan A, Tewari R. Warfarin related acute kidney injury: A case report. Indian J Nephrol. 2017;27:78–80. doi: 10.4103/0971-4065.177142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Escoli R, Santos P, Andrade S, Carvalho F. Dabigatran-related nephropathy in a patient with undiagnosed IgA nephropathy. Case Rep Nephrol. 2015;2015:298261. doi: 10.1155/2015/298261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Satoskar AA, Suleiman S, Ayoub I, et al. Staphylococcus infection-associated GN - spectrum of IgA staining and prevalence of ANCA in a single-center cohort. Clin J Am Soc Nephrol. 2017;12:39–49. doi: 10.2215/CJN.05070516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hellfritzsch M, Damkier P, Pottegård A, Grønlykke T, Grove EL. Inconsistencies in reporting of renal elimination among NOACs: the case of apixaban. Pharmacoepidemiol Drug Saf. 2016;25:346–348. doi: 10.1002/pds.3916. [DOI] [PubMed] [Google Scholar]
- 14.Glassock RJ, Rule AD. Aging and the kidneys: anatomy, physiology and consequences for defining chronic kidney disease. Nephron. 2016;134:25–29. doi: 10.1159/000445450. [DOI] [PubMed] [Google Scholar]