Abstract
Objectives
This study sought to investigate the proportion of patients with suspected sinusitis referred for radiological examination who have radiologically verified sinusitis of odontogenic origin and to describe this type of sinusitis.
Study Design
This investigation is a retrospective study.
Methods
A total of 303 sinus examinations involving cone beam computed tomography (CBCT) performed at Sunderby Hospital, Luleå, Sweden in 2012 were independently reviewed by two radiologists. The number of cases of maxillary sinusitis and the correlation between maxillary sinusitis and odontogenic infections were determined.
Results
Overall, 24% of the verified cases of sinusitis were odontogenic. An odontogenic origin was identified in 40% of unilateral maxillary sinusitis cases but only 6% of bilateral maxillary sinusitis cases (p = 0.0015). Forty‐nine out of 54 patients with periapical destruction had adjacent mucosal swelling in the maxillary sinus, but only 15 of these patients satisfied the criteria for sinusitis.
Conclusion
The present study confirms the close relationship between odontogenic infections and unilateral maxillary sinusitis.
Level of Evidence 4
Keywords: computed tomography, radiology, dental infection, periapical abscess, sinusitis
INTRODUCTION
The most common cause of rhinosinusitis is virus‐induced upper respiratory tract infections (URTI) with a secondary bacterial infection in the sinuses. Rhinosinusitis is normally successfully treated with decongestants and sometimes antibiotics but can occasionally be therapy‐resistant or even recurrent. In such cases, radiologic examination is often required to exclude an alternative aetiology or to facilitate other treatment options.1
The relationship between odontogenic infections and maxillary sinusitis is well established.2, 3 Roots of the molars in the upper jaw are usually extremely close to or in direct contact with the maxillary sinus. Odontogenic infections are either endodontic (caused by infections of the dental pulp) or periodontal, (involving a tooth's supporting tissues). Such infections require specific dental treatment that addresses their cause(s). If patients with these infections are treated with antibiotics alone, the infection often temporarily subsides but subsequently recurs. It is therefore important to identify whether sinusitis is caused by an odontogenic infection to provide appropriate treatment.3
In older studies, the prevalence of odontogenic sinusitis among all sinusitis cases has been estimated to be 10–15%.4, 5 In these investigations, radiological examinations to evaluate the teeth and the possibility of odontogenic infection were performed using two‐dimensional techniques, such as intra‐oral and/or panoramic X‐ray assessments. In recent studies involving the use of three‐dimensional radiologic techniques such as multislice computed tomography (MSCT) or cone beam computed tomography (CBCT), odontogenic sinusitis has been reported at higher frequencies of up to 40% of chronic sinusitis patients.6, 7 These results can potentially be attributed to the use of more thorough radiological methods but could also reflect differences in definitions of sinusitis. It is also important to differentiate between unilateral and bilateral sinusitis.8, 9
CBCT is a form of three‐dimensional computed tomography in which hard tissues, such as bones and teeth, can be imaged in an extremely detailed manner; thus, this approach can readily demonstrate the apical pathology of the maxillary molars. Even small apical destructions that may be difficult or impossible to detect using two‐dimensional techniques can be detected using CBCT.10, 11
The aim of this study was to investigate the proportion of patients with suspected sinusitis referred for radiological examination who have radiologically verified sinusitis of odontogenic origin and describe this type of sinusitis.
MATERIALS AND METHODS
All CBCT scans performed due to suspicion of sinusitis in the Radiology Department of Sunderby Hospital in 2012 were included in this study. Patients referred for control of healing, patients with known polyposis, and patients referred due to trauma or suspicion of systemic disease or a tumor (and who therefore required contrast‐enhanced MSCT) were excluded. Examinations were identified from the hospital's radiological information system (RIS; Sectra), and imaging data were retrieved from the local radiological image archive. CBCT examinations were performed using an Accuitomo 170 unit (J. Morita Corporation, Osaka, Japan). The exposure factors were 85 kV and 4 mAs with 180° rotation. The image field was 17 × 12 cm (diameter × height) or 14 × 10 cm depending on the size of the patient. A stack of axial slices with a thickness of 1 mm was used to create axial, coronal and sagittal reconstructions with a thickness of 1.25 mm.
Two observers retrospectively conducted independent reviews of all examinations. Prior to these reviews, a procedure to calibrate the two observers’ interpretations was performed; during this calibration process, 20 sinus examinations not included in the study were examined independently, and criteria for defining sinusitis were established.
In the reviewed cases, when observers disagreed, examinations were re‐reviewed jointly to reach consensus. As part of the examination protocols, the following findings were recorded.
Mucosal thickening in the sinuses was determined, and gas/fluid levels were classified into three categories (grade 1, <1/3 of the maxillary sinus; grade 2, 1/3‐2/3 of the maxillary sinus; grade 3, >2/3 of the maxillary sinus). Occlusion of maxillary sinus ostia, root canal fillings, periapical changes, marginal bone defects, and loss of bone between the tooth and the maxillary sinus were noted. The patient's sex and age, the month of examination, and the type of health care provider that referred the patient were also registered.
A detected pathology was classified as ongoing sinusitis based on the following radiological criteria: gas/fluid level in the maxillary sinuses, with or without adjacent mucosal swelling, or a totally congested maxillary sinus without other signs of polyposis or tumors. Concurrent involvement of other sinuses was also registered. Sinusitis was classified as unilateral if a strictly unilateral pattern or a clear predominantly unilateral pattern was detected for all sinuses (Fig. 1). Medical records of all patients exhibiting any radiological sinus pathology were reviewed.
Figure 1.
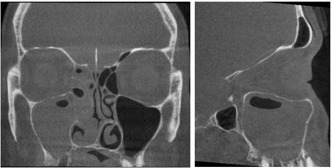
Unilateral odontogenic sinusitis of the right maxillary sinus and ethmoidal cells on the same side.
Tooth number 17 (second molar on the right side of the upper jaw) has been extracted due to periapical infection. There is a loss of bone between the extraction socket and the maxillary sinus. Fluid level is found in the maxillary sinus.
This study was approved by the regional ethics committee of Umeå University (dnr 2013‐228‐31M). IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp. was used for descriptive statistical analysis. The OpenEpi program was used for calculations related to standard chi‐square tests. A p‐value < 0.05 was considered statistically significant.
RESULTS
A total of 346 CBCT examinations were performed in 2012 at Sunderby Hospital due to suspected sinusitis. Forty‐three patients were excluded in accordance with the aforementioned criteria. Among the 303 patients included in the study with suspected sinusitis symptoms, 87 patients had no sinus pathology (Table 1). The remaining 216 patients had sinus pathology, such as retention cysts, mucosal swelling, or sinusitis, based on the definitions provided above. Sixty‐six of the included patients (22%) had radiologically verified sinusitis according to our definition of this condition (Fig. 2). Medical records revealed that all of these patients showed obvious clinical findings, such as nasal pus discharge or pus on sinus puncture.
Table 1.
Demographic Characteristic of Patients Included in the Study.
| Gender | |
| Male | n = 128 (42.2%) |
| Female | n = 175 (57.8%) |
| Mean age (years) | |
| All patients | 49 |
| Sinusitis | 50 |
| Bilateral | 47 |
| Unilateral | 52 |
| Non‐odontogenic unilateral | 46 |
| Odontogenic unilateral | 60 |
Figure 2.
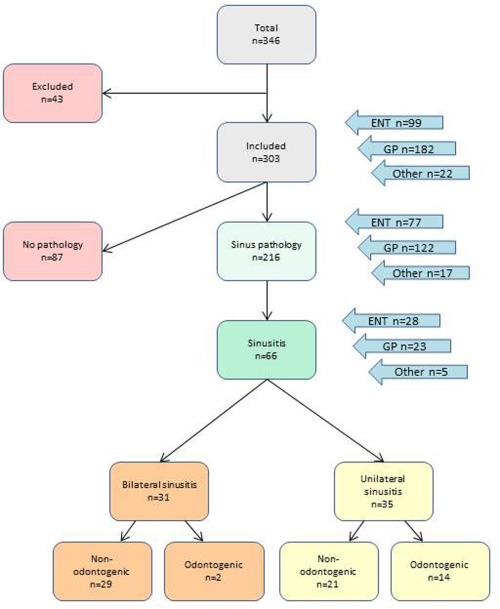
Flow chart showing the distribution of sinus pathology among patients that was examined with Cone Beam Computed Tomography (CBCT) during 2012 at Sunderby Hospital. Referees are shown by arrows on the right.
ENT, Ear, nose, and throat specialist; GP, General Practitioner; Others, Dentists or specialists other than ENT
Overall, 35 and 31 of the verified sinusitis cases were considered unilateral and bilateral, respectively. Among the unilateral cases, 14 out of 35 cases (40%) had odontogenic causes; among the bilateral cases, 2 out of 31 cases (6%) had odontogenic causes. The difference between these frequencies was statistically significant (p = 0.0015). An odontogenic cause of radiologically verified sinusitis was thus identified in 16 (24%) of 66 patients (Table 2).
Table 2.
Cross Table of Proportion of Odontogenic Sinusitis Versus Laterality.
| Odontogenic | Non‐odontogenic | Total | |
|---|---|---|---|
| Unilateral sinusitis | 14a | 21 | 35 |
| Bilateral sinusitis | 2a | 29 | 31 |
| Total | 16 | 50 | 66 |
p‐value = 0.0015
Fifty‐four of the examined patients exhibited periapical pathology. Among these patients, 49 patients (90%) had adjacent mucosal swelling in the maxillary sinus on the same side. Twenty‐four patients had mucosal swelling in less than 1/3 of the maxillary sinus, and 25 patients had mucosal swelling in more than 1/3 of the maxillary sinus. Fifteen patients with periapical pathology satisfied our definition of ongoing maxillary sinusitis based on gas/fluid levels or total congestion of the maxillary sinus (Fig. 3). Thirteen patients had extensive marginal destruction, and 11 of these patients exhibited adjacent mucosal swelling. One of these patients had ongoing sinusitis (Fig. 4).
Figure 3.
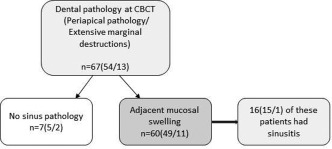
Dental pathology at CBCT
Adjacent mucosal swelling nearby a periapical‐ or an extensive marginal destruction.
Figure 4.
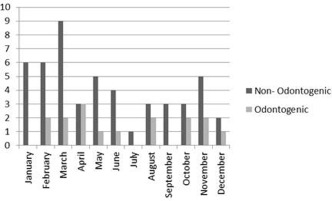
Distribution of sinusitis over the year according to examination month. A more even distribution is seen in the group of odontogenic sinusitis then in the group of non‐odontogenic sinusitis.
Among patients with odontogenic unilateral sinusitis, 78% of subjects were 40–69 years of age (and 64% of subjects were 50–69 years of age); the mean age was 60 years, and the age range was 39–81 years. Patients with non‐odontogenic unilateral sinusitis ranged from teenagers to elderly individuals and exhibited a more even age distribution (mean age, 46 years; range, 19–82 years). No seasonal variation was observed with respect to odontogenic sinusitis. Non‐odontogenic sinusitis was detected in 42% of cases examined between January and March and in 66% of cases examined between January and June (Fig. 5).
Figure 5.
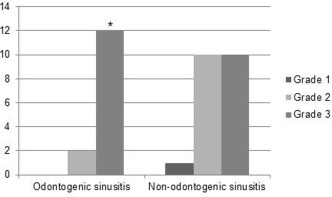
Fluid level, including mucosal swelling, in the maxillary sinus.
Grade 1: Fluid level, less than 1/3 of the maxillary sinus is congested.
Grade 2: Fluid level, 1/3‐ 2/3 of the maxillary sinus is congested.
Grade 3: Fluid level, more than 2/3 of the maxillary sinus is congested.
* = The proportion of patients with grade 3 congestion was higher (p = 0.04) in the odontogenic group.
Patients with odontogenic unilateral sinusitis had significantly more swelling and congestion of the maxillary sinuses (p = 0.0397) than patients with non‐odontogenic unilateral sinusitis. In 86% of odontogenic unilateral sinusitis cases, fluid and mucosal swelling were detected in more than 2/3 of the maxillary sinus (grade 3), whereas the corresponding statistic for cases of non‐odontogenic unilateral sinusitis was 45% (Fig. 6).
DISCUSSION
CBCT, which is a relatively new technique, has assumed a significant role in diagnoses of teeth, jaws and sinuses. The most frequent medical conditions of the sinuses can be diagnosed radiologically using this approach. CBCT also provides optimal imaging of supporting tissue surrounding teeth to enable the detection of odontogenic causes of sinusitis.
In the present study, we found that 22% of the patients referred to the radiology department with suspected sinusitis were radiologically verified to have ongoing sinusitis. Furthermore, an odontogenic cause was identified in 24% of cases of radiologically verified sinusitis; this percentage is higher than the corresponding percentages reported in older studies.4, 5 Frequencies of sinusitis of odontogenic origin reported in these older studies are often cited. However, the methods used to assess dental and sinus pathologies have changed over time. Ericsson used “clinical experience” as a reference, and Melén et al. used a combination of clinical assessment and plain film radiology.2, 4 Melén et al. concluded that 40.6% of all cases of chronic sinusitis were odontogenic.
In this study, 40% of cases of unilateral verified sinusitis had an odontogenic origin, a result comparable to the corresponding finding of 36% obtained by Bomeli et al. if fluid levels were used as a criterion for sinusitis.6 The criterion used to diagnose maxillary sinusitis and the selection of patients have critical effects on observed outcomes. Matsumoto et al. found that in patients treated in an ENT/oral surgery clinic, 70% of cases of unilateral sinusitis were of odontogenic origin.9 In our study, however, the only criterion used to select patients was clinical suspicion of sinusitis. Patients included in the study could have a combination of different symptoms, but in all cases the clinician referred the patients for radiology suspecting sinusitis. Since the study was retrospective, we were not able to set an absolute criterion for which symptoms we wanted to have in the referral.
In this investigation, we only included patients with clinically suspected sinusitis, thereby minimizing the risk of over‐interpretation of radiological findings. Furthermore, we utilized a strict definition for radiologically diagnosing sinusitis that required certain fluid level findings or a totally congested maxillary sinus without other signs of polyposis. Certain prior studies have used a broader definition of sinusitis, such as the presence of mucosal swelling, including small local mucosal reactions, without clinical findings correlated with ongoing sinusitis.12 This definition differs from international criteria regarding the definition of sinusitis1. In contrast to studies that reached conclusions based solely on radiographic findings, the present investigation used a combination of radiological characteristics and clinical records. Thus, given our strict criteria, chronic sinusitis without fluid levels would not be recorded as ongoing sinusitis in this study. The figures presented in our study are only representative of the group of patients referred for radiology due to suspected ongoing sinusitis, regardless of duration.
Sixty of 67 (90%) patients with periapical or marginal pathology on radiographic examination had adjacent local mucosal swelling; this result was comparable to that obtained by Ariji, who found a corresponding percentage of approximately 89%.13 However, periapical and marginal destruction can cause basal mucosal thickening to varying degrees. These findings therefore should be interpreted as indicative of a natural reaction to a low‐grade infection from an adjacent tooth rather than sinusitis. Only 16 of these 67 patients had ongoing odontogenic sinusitis according to our definition.
Another factor that could contribute to uncertainty regarding the frequency of sinusitis of odontogenic origin is the fact that periapical destruction is not always the cause of sinusitis, even if the sinuses are filled with fluid, particularly if bilateral sinusitis is observed. To avoid such uncertainties, we reviewed patient records and verified the presence of pus with a typical foul smell characteristic of anaerobic mouth flora.
Approximately 79% of the patients with odontogenic sinusitis were 40–69 years of age; this result was consistent with the fact that the teeth causing most of these infections had been present in the mouth for many years.3 Younger individuals in the Swedish population have fewer restored teeth than their older counterparts; this characteristic could explain why we did not find odontogenic sinusitis in any children/teenagers. In addition, based on current practices, the dental treatment that younger Swedes may have received has generally been minimally invasive dentistry, a form of dental treatment that reduces the risk of secondary caries and crown and root fractures.14
Grade 3 fluid levels were found significantly more frequently among patients with odontogenic sinusitis than among other patients. The significance of this difference is unclear. It can be speculated that compared with other sinusitis‐related infections, odontogenic infections exhibit a different bacterial composition with more anaerobic flora, resulting in fewer clinical symptoms.15, 16 Such circumstances could lead to patients with odontogenic sinusitis being misdiagnosed for a long duration and therefore examined at later stages involving greater disease progression. Other studies have reported similar patterns and frequencies with respect to fluid levels in the presence of odontogenic sinusitis.6, 15
CONCLUSION
In the present study, we found that ongoing sinusitis had an odontogenic origin in 24% of cases. Moreover, this investigation indicated that up to 40% of cases of radiologically verified unilateral maxillary sinusitis involved an odontogenic origin; this result emphasizes that both radiologists and clinicians must be aware of this aetiology in such cases since appropriate dental treatment is often needed to permanently cure patients.
ACKNOWLEDGMENTS
The study was financed by the County Council of Norrbotten, Sweden. We would also like to thank Robert Lundqvist for statistical assistance and Fernando Mota de Almeida for valuable contributions.
There are no conflicts of interest.
BIBLIOGRAPHY
- 1. Fokkens WJ, Lund VJ, Mullol J, Bachert C. EPOS. Rhinology 2012;50(23):5. [DOI] [PubMed] [Google Scholar]
- 2. Melen I, Lindahl L, Andreasson L, Rundcrantz H. Chronic maxillary sinusitis. Definition, diagnosis and relation to dental infections and nasal polyposis. Acta Otolaryngol 1986;101(3–4):320–327. [DOI] [PubMed] [Google Scholar]
- 3. Legert KG, Zimmerman M, Stierna P. Sinusitis of odontogenic origin: Pathophysiological implications of early treatment. Acta Otolaryngol 2004;124(6):655–663. [DOI] [PubMed] [Google Scholar]
- 4. Ericson S. Conventional and computerized imaging of maxillary sinus pathology related to dental problems. Oral Maxillofac Surg Clin North Am 1992;4(1):153–181. [Google Scholar]
- 5. Maloney P, Doku H. Maxillary sinusitis of odontogenic origin. J Can Dent Assoc 1968;34(11):591–603. [PubMed] [Google Scholar]
- 6. Bomeli SR, Branstetter BF, 4th, Ferguson BJ. Frequency of a dental source for acute maxillary sinusitis. Laryngoscope 2009;119(3):580–584. [DOI] [PubMed] [Google Scholar]
- 7. Lechien JR, Filleul O, de Araujo PC, Hsieh JW, Chantrain G, Saussez S. Chronic maxillary rhinosinusitis of dental origin: A systematic review of 674 patient cases. Int J Otolaryngol 2014. doi: 10. 1155/2014/465173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Patel NA, Ferguson BJ. Odontogenic sinusitis: An ancient but underappreciated cause of maxillary sinusitis. Curr Opin Otolaryngol Head Neck Surg 2012;20(1):24–28. [DOI] [PubMed] [Google Scholar]
- 9. Matsumoto Y, Ikeda T, Yokoi H, Kohno N. Association between odontogenic infections and unilateral sinus opacification. Auris Nasus Larynx 2015;42(4):288–293. [DOI] [PubMed] [Google Scholar]
- 10. Suomalainen A, Vehmas T, Kortesniemi M, Robinson S, Peltola J. Accuracy of linear measurements using dental cone beam and conventional multislice computed tomography. Dentomaxillofac Radiol 2008;37(1):10–17. [DOI] [PubMed] [Google Scholar]
- 11. Lofthag‐Hansen S, Thilander‐Klang A, Grondahl K. Evaluation of subjective image quality in relation to diagnostic task for cone beam computed tomography with different fields of view. Eur J Radiol 2011;80(2):483–488. [DOI] [PubMed] [Google Scholar]
- 12. Maillet M, Bowles WR, McClanahan SL, John MT, Ahmad M. Cone‐beam computed tomography evaluation of maxillary sinusitis. J Endod. 2011;37(6):753–757. [DOI] [PubMed] [Google Scholar]
- 13. Ariji Y, Obayashi N, Goto M, et al. Roots of the maxillary first and second molars in horizontal relation to alveolar cortical plates and maxillary sinus: Computed tomography assessment for infection spread. Clin Oral Investig 2006;10(1):35–41. [DOI] [PubMed] [Google Scholar]
- 14. Murdoch‐Kinch CA, McLean ME. Minimally invasive dentistry. J Am Dent Assoc 2003;134(1):87–95. [DOI] [PubMed] [Google Scholar]
- 15. Brook I. Microbiology of acute and chronic maxillary sinusitis associated with an odontogenic origin. Laryngoscope 2005;115(5):823–825. [DOI] [PubMed] [Google Scholar]
- 16. Puglisi S, Privitera S, Maiolino L, et al. Bacteriological findings and antimicrobial resistance in odontogenic and non‐odontogenic chronic maxillary sinusitis. J Med Microbiol 2011;60(9):1353–1359. [DOI] [PubMed] [Google Scholar]


