Abstract
Objectives
To clarify the usefulness of ultrasonography for detecting hypopharyngeal cancer.
Study Design
Cross‐sectional study.
Methods
The study included 95 patients who underwent pre‐treatment ultrasonography. We evaluated the usefulness of ultrasonography for detecting primary hypopharyngeal carcinoma of each T stage and subsite, and for assessing extrahypopharyngeal invasion. Additionally, we determined the efficacy of color Doppler for evaluating primary hypopharyngeal carcinoma.
Results
The patients comprised 93 men and 2 women with a mean age of 67.5 years. The T stage (primary tumors) was T1 in 29 patients, T2 in 22, T3 in 9, and T4 in 35. Primary sites with a T stage over T3 were detected using ultrasonography in 17 patients.
Regarding primary subsites, postcricoid tumors were assessed most easily (64%), while posterior wall tumors were the most difficult to assess (25%). In 15 of 17 patients, the evaluation of extrahypopharyngeal invasion by ultrasonography matched up precisely with computed tomography findings. In addition, abnormally increased blood flow in primary hypopharyngeal cancers was recognized by color Doppler, and could be used to predict subsites.
Conclusions
Cancers at T3 and T4 hypopharyngeal primary tumors and their extrahypopharyngeal invasion were detectable using ultrasonography. Furthermore, ultrasonography was useful for assessing postcricoid tumors that were difficult to observe by flexible laryngoscopy.
Level of Evidence
4
Keywords: Hypopharyngeal cancer, ultrasonography, laryngoscopy
INTRODUCTION
Endoscopic examination is indispensable in the detection and evaluation of laryngopharyngeal lesions.1, 2 Laryngoscopy is thought to be the most effective tool for the detection of mucosal abnormalities and the evaluation of hypopharyngeal cancer.3, 4 However, it is difficult to assess the depth and extrahypopharyngeal invasion of advanced cancers. It is also often impossible to observe the caudal part of the tumor and to predict the primary subsite of bulky tumors. Furthermore, the hypopharyngeal cavity is often partly collapsed due to the laryngeal cartilage, which makes its detection using laryngoscopy difficult. Therefore, direct rigid laryngoscopy is sometimes performed under general anesthesia,5, 6 and computed tomography (CT) or magnetic resonance imaging (MRI) is necessary.7, 8, 9, 10, 11
In contrast, ultrasonography can be used to detect structures of the neck from the body surface and has a higher millimeter‐scale resolution. Therefore, this modality is expected to detect some characteristics of hypopharyngeal carcinoma that are missed by laryngoscopy. If ultrasonography can be used to address the shortcomings of laryngoscopy and to guide CT scans used to evaluate tumor spread, it may be of immense help in the medical care of individuals with hypopharyngeal cancer.
Therefore, we assessed the usefulness of ultrasonography for the evaluation of hypopharyngeal cancer.
PATIENTS AND METHODS
Patients
The study participants were patients with histologically diagnosed squamous cell carcinoma following first‐time tissue biopsy. The primary tumors were the hypopharynx, as determined by flexible laryngoscopy or upper gastrointestinal endoscopy. We conducted ultrasonographic assessments of the primary tumors in patients with hypopharyngeal cancer who had undergone cervical ultrasonography for evaluation of the cervical lymph nodes (N stage). The patients had also undergone flexible laryngoscopy and enhanced CT within three weeks of pre‐treatment ultrasonography. Ninety‐eight consecutive patients were enrolled between January 2010 and December 2016. Three patients were excluded because they did not meet the above conditions; one patient did not undergo cervical ultrasonography and two had previous neck radiotherapy. This study was approved by the Institutional Review Board of Tottori University and was performed in accordance with the Declaration of Helsinki.
Evaluation Methods
We first determined whether tumors of every T stage were assessable by transcutaneous ultrasonography. Second, we classified assessable tumors according to subsite, and determined the assessability rates of tumors at each subsite. Furthermore, we compared all tumors in terms of whether we could assess invasion into adjacent organs, which dictated their T stage (T3 or T4).
We classified T4 tumors that invaded laryngeal cartilage into two groups according to the presence or absence of extralaryngeal invasion, and determined whether the two groups were assessable by transcutaneous ultrasonography. We also compared the ultrasonographic and CT assessability of the organs invaded by the primary tumor. Finally, we determined whether the primary subsites were in agreement with those predicted on the basis of the blood flow of the primary tumor as revealed by color Doppler.
Ultrasonography
We used a Xario XG ultrasound system with a 7.5‐MHz linear transducer (Toshiba Medical System Co.; Tochigi, Japan) from January 2010 to October 2011, and an Acuson S2000 ultrasound system with a 9‐MHz linear transducer (Siemens Medical Solutions, Mountain View, CA) beginning in November 2011.
Ultrasonographic examinations were performed by two sonographers, one specializing in head and neck sonography; two otolaryngologists; and a surgeon specializing in head and neck surgery with experience in ultrasonography.
We performed ultrasonographic assessments of the primary tumor in the hypopharynx in conjunction with cervical ultrasonography to evaluate lymph node metastasis.
The patients underwent cervical ultrasonographic examination in the supine position with their necks slightly extended. At the end of the examination, while still in the same position, they underwent ultrasonographic assessment of the primary tumor in the hypopharynx. We placed the linear transducer in the transverse and sagittal planes in the central neck area. First, we observed the thyroid glands and the esophagus posterior to the thyroid glands, and then assessed whether the primary tumors were visible while scanning toward the head at the pyriform sinus of the hypopharynx, just outside of the thyroid cartilage, using gray‐scale and color Doppler imaging.
We also used ultrasonography to assess the organs invaded by the primary tumors, specifically the esophagus, thyroid/cricoid cartilage, thyroid, and prevertebral fascia. We predicted the primary subsites based on the blood flow of the primary tumor using color Doppler. Blood flow from the lateral sides indicated tumors in the pyriform sinuses, anterior blood flow indicated tumors in the postcricoid region, and posterior blood flow indicated tumors in the posterior hypopharyngeal wall.
Criteria for Assessment
In this study, we considered the primary tumors assessable when they were recognized as low‐echoic abnormal masses by non‐experts (Fig. 1). We also used abnormally increased blood flow as an adjunct in the diagnosis of primary tumor,12, 13 as there is no increased blood flow in the normal hypopharynx in the absence of tumors (Fig. 2).
Figure 1.
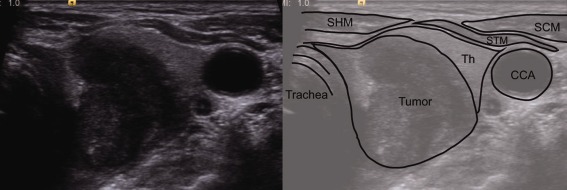
The hypopharyngeal primary tumor was revealed as a low‐echoic abnormal mass. CCA = common carotid artery; SCM = sternocleidomastoid muscle; SHM = sternohyoid muscle; STM = sternothyroid muscle; Th = thyroid.
Figure 2.
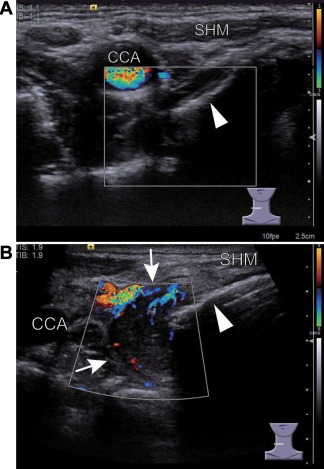
A. The normal, noncancerous hypopharynx shows no peripheral vascularity. B. Primary hypopharyngeal cancer shows increased vascularity (the white arrow). CCA = common carotid artery; SHM = sternohyoid muscle, thyroid cartilage (the white arrow head).
Statistical Analysis
Statistical analyses were performed using the SPSS software (IBM SPSS Statistics 22; IBM, Armonk, NY). We used the chi‐square test to compare the percentage of tumors in each group in which the evaluation of the primary site was deemed to be assessable by ultrasonography.
RESULTS
The characteristics of the patients are shown in Table 1. Seventeen of 95 patients had tumors that were assessable by ultrasonography. The blood flow of hypopharyngeal tumors was not assessed in four patients. There was no blood flow in the primary tumor in only one patient. In contrast, 12 patients had abnormally increased blood flow in the primary tumors.
Table 1.
Patient Characteristics.
| N | % | |
|---|---|---|
| Age, years | ||
| Median | 68 | |
| Range | 33–84 | |
| Sex | ||
| Male | 93 | 97.9 |
| Female | 2 | 2.1 |
| T classification | ||
| T1 | 29 | 30.5 |
| T2 | 22 | 23.2 |
| T3 | 9 | 9.5 |
| T4 | 35 | 36.8 |
| Subsite | ||
| Pyriform sinus | 73 | 76.8 |
| Posterior wall | 9 | 9.5 |
| Postcricoid | 13 | 13.7 |
Table 2 shows the numbers of patients with assessable and non‐assessable tumors for each T stage. No primary tumors of stage T1 or T2 were detectable. The primary tumors that were detected by ultrasonography had stages of T3 or higher. Tables 3 and 4 show the ultrasonographic assessability rates of stage T3 and T4 tumors by primary subsite and by adjacent organs invaded. Regarding primary subsites, postcricoid tumors were the most assessable (69%), while posterior wall tumors were the least assessable (20%). The assessability rates of postcricoid T3/T4 tumors and other primary tumors (pyriform sinus or posterior wall) were 69% and 32%, indicating a significant difference (P = 0.0239). The assessability rate of T4 postcricoid tumors alone was 80%, while that of other primary tumors was 36% (P = 0.0186). Regarding the assessability of tumor invasion of adjacent organs, esophageal invasion was assessable in T3 tumors (2/2 cases) by transcutaneous ultrasonography (Table 3), while thyroid invasion was assessable in T4 tumors (4/4 cases) by transcutaneous ultrasonography (Table 4). Laryngeal cartilage invasion was assessable in 34% (12/35) of T4 tumors overall; in cases with extralaryngeal invasion and those without cartilage invasion, the assessability rates were 92% (12/13) and 0% (0/22), respectively. One case with extralaryngeal invasion could not be assessed by ultrasonography because of enlarged metastatic lymph nodes.
Table 2.
The Numbers of Assessable and Non‐Assessable Patients by T Stage and Primary Subsite.
| T1 | T2 | T3 | T4 | Total | ||
|---|---|---|---|---|---|---|
| US | Assessable | 0 | 0 | 2 | 15 | 17 |
| Non‐assessable | 29 | 22 | 7 | 20 | 78 | |
| Subsite | Pyriform sinus | 26 | 19 | 4 | 24 | 73 |
| Posterior wall | 3 | 1 | 2 | 3 | 9 | |
| Postcricoid | 0 | 2 | 3 | 8 | 13 |
Table 3.
Comparison of Assessability Rates of T3 Tumor Invasion into Adjacent Organs.
| US | ||
|---|---|---|
| Assessable | Non‐assessable | |
| T3 (9) | ||
| Pyriform sinus | ||
| Esophagus (1) | 1 | 0 |
| Larynx: vocal paralysis (3) | 0 | 3 |
| Posterior wall | ||
| Larynx: vocal paralysis (1) | 0 | 1 |
| No: size > 4 cm (1) | 0 | 1 |
| Postcricoid | ||
| Esophagus (1) | 1 | 0 |
| Larynx: vocal paralysis (2) | 0 | 2 |
Table 4.
Comparison of Assessability Rates of T4 Tumor Invasion into Adjacent Organs.
| US | ||
|---|---|---|
| Assessable | Non‐assessable | |
| T4 (35) | ||
| Pyriform sinus | ||
| Laryngeal cartilage (22) | 7 | 15 |
| Posterior wall | ||
| Laryngeal cartilage (3) | 0 | 3 |
| Postcricoid | ||
| Laryngeal cartilage (5) | 3 | 2 |
| Laryngeal cartilage + thyroid (4) | 4 | 0 |
| Laryngeal cartilage + thyroid + prevertebral fascia (1) | 1 | 0 |
Invasion of Adjacent Tissue as Assessed Using Ultrasonography
The use of ultrasonography versus CT for evaluation of the invasion of adjacent tissue (esophagus, thyroid/cricoid cartilage, thyroid, prevertebral fascia) was compared for 17 patients. The results are shown in Table 5. In 15 of 17 patients, the evaluation of extrahypopharyngeal invasion by ultrasonography precisely matched the CT findings. We were unable to use ultrasonography to detect invasion of the prevertebral fascia or cricoid cartilage.
Table 5.
The Comparison Between the Ultrasonography Findings and the CT Findings to Evaluate the Invasion.
| CT | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Esophagus | Thyroid/cricoid cartilage | Thyroid gland | Prevertebral fascia | ||||||
| Positive | Negative | Positive | Negative | Positive | Negative | Positive | Negative | ||
| US | Positive | 7 | 0 | 12 | 0 | 4 | 0 | 0 | 0 |
| Negative | 0 | 10 | 1 | 4 | 0 | 13 | 1 | 16 | |
CT = computed tomography.
Prediction of the Primary Subsite
In 12 of 13 patients who were assessed using color Doppler, the primary subsites were accurately predicted based on the blood flow pattern. In one patient, the blood flow was not visualized using color Doppler.
DISCUSSION
We evaluated 95 patients with hypopharyngeal cancer to evaluate the usefulness of transcutaneous ultrasonography in detecting hypopharyngeal cancer. Our results indicated that advanced primary tumors of stages T3 or T4 were detectable by ultrasonography. In comparing primary subsites, postcricoid tumors were most easily detected by ultrasonography. In primary hypopharyngeal cancers that were assessable by ultrasonography, abnormally increased blood flow was recognized by color Doppler in all but one patient. The assessment of extrahypopharyngeal invasion using ultrasonography was in close agreement with that using CT. In addition, the subsites of hypopharyngeal cancers were predictable based on abnormal blood flow patterns detected using color Doppler.
Although advanced hypopharyngeal cancers with T3 or T4 primary tumors were detectable, ultrasonography was unable to detect T1 or T2 tumors without deep infiltration. This may be because T1 and T2 tumors are confined to the mucosa, and since the mucous membrane is in direct contact with air, ultrasound diffuses at this location due to the markedly different impedances of air and tissue. In contrast, T3 and T4 tumors are deeply infiltrative and invade adjacent organs. In this study, transcutaneous ultrasonography was able to detect invasion of the esophagus and thyroid, and also of the laryngeal cartilage as long as there was no cartilaginous infiltration.
In a comparison of primary subsites, postcricoid tumors were most easily detected by transcutaneous ultrasonography, while posterior wall tumors were the most difficult to detect. These results were the opposite of those with flexible laryngoscopic examination. The pharyngo‐esophageal border at the postcricoid region is difficult to observe with a flexible laryngoscope,14 because the cavity is partly collapsed due to the laryngeal cartilage. Our findings suggest that ultrasonography may be used to detect hypopharyngeal tumors in the postcricoid region that are difficult to observe using a laryngoscope.
Few studies have assessed laryngopharyngeal or hypopharyngeal cancer using ultrasonography.5, 6, 12, 13, 15, 16, 17, 18 Some authors demonstrated that T1 and T2 pharyngeal cancers were detectable using ultrasonography.15, 18 However, in our study, T1 and T2 tumors, which are mucosal lesions, were not observable by any of our experts. Jecker et al. also found that T2 hypopharyngeal tumors were undetectable via ultrasound.19 The shortcomings of ultrasonography include its real‐time nature and the fact that analysis is subjective and depends on examiner experience and the specific techniques used. Because the pharynx has a complex anatomy, it is difficult to study by ultrasonography, even if the examiner has experience with cervical ultrasonography.
Dhoot et al. reported that they did not assess tumor vascularity because there were currently no reports available regarding the usefulness of Doppler in hypopharyngeal cancers.13 However, in this study, we detected abnormally increased blood flow in primary hypopharyngeal tumors, a finding that may facilitate the diagnosis of hypopharyngeal cancer using ultrasonography in the future.
The ultrasonographic evaluation of extrahypopharyngeal invasion by advanced hypopharyngeal tumors yielded comparable results to CT. The American Joint Committee on Cancer staging system requires the evaluation of the following organs for T staging: larynx, esophagus, thyroid cartilage, cricoid cartilage, central compartment soft tissue, carotid artery, and prevertebral fascia.20 The larynx and the movements of the vocal folds can be evaluated using a laryngoscope.21, 22 Tumors invading central compartment tissues or those leading to the destruction of thyroid cartilage are easy to evaluate using ultrasonography, as they invade superficial structures.23, 24 In addition, esophageal invasion is readily apparent when the thyroid is used as an acoustic window. In contrast, ultrasonography cannot be used to evaluate invasion of the prevertebral fascia or cricoid cartilage. This may be due to the fact that ultrasound is attenuated at deep sites such as the prevertebral region. In addition, bulky tumors in the area of the cricoid cartilage are impenetrable by ultrasound due to their thickness and round shape.
We were able to predict the primary subsites of advanced hypopharyngeal cancers using color Doppler images, even in cases when the entire primary subsites could not to be observed by laryngoscopy due to large tumor sizes. Taken together, our data indicate that ultrasonography is useful for the detection of advanced hypopharyngeal cancer when assessing the whole tumor image, such as during preoperative evaluation.
Limitations
This study had several limitations. First, we performed ultrasonography in patients who had already been diagnosed with hypopharyngeal cancer. Second, we did not evaluate patients with hypopharyngeal cancers that were not detected using laryngoscopy. In fact, the primary subsites of almost all T1 and T2 hypopharyngeal cancers detected by laryngoscopy were the pyriform sinus and posterior wall. It is possible that T1 and T2 hypopharyngeal cancers in the postcricoid region were not detected by laryngoscopy, as the postcricoid cavity of the hypopharynx is partly collapsed due to the larynx. Therefore, it is still unclear whether T1 and T2 hypopharyngeal cancers in the postcricoid region are detectable using ultrasonography. Third, we did not assess tumor invasion through the laryngeal cartilage in this study, because this would have required changing the settings of the ultrasound system. We would have been able to assess intralaryngeal invasion if we had focused specifically on this region. Fourth, we only used a linear transducer and did not use another probe such as a convex transducer.
CONCLUSIONS
Ultrasonography was successfully used to detect hypopharyngeal tumors of stages T3 and T4 and to evaluate tumor invasion of adjacent organs, with the exception of the larynx, with results comparable to CT. Furthermore, ultrasonography was useful for assessing postcricoid tumors that were difficult to observe by flexible laryngoscopy. These results indicate that ultrasonography may compensate for the drawbacks of endoscopy with regard to examination of the hypopharynx, and, when used in combination with endoscopy, may substitute for CT in the evaluation of extrapharyngeal invasion.
ACKNOWLEDGMENT
This work was supported by JSPS KAKENHI Grant Number 16K20246.
This work was supported by JSPS KAKENHI Grant Number 16K20246.
The authors declare that no competing financial interests exist.
This manuscript will be presented at the podium session of the ABEA Annual Meeting held in conjunction with COSM at the Manchester Grand Hyatt in San Diego, April 26‐28, 2017.
BIBLIOGRAPHY
- 1. Stevens SM, Johnson EA, Pfau PR, Dailey SH. Visual evaluation of the larynx and hypopharynx during esophagogastroduodenoscopy: a safety and feasibility study. Surg Endosc. 2015;29:1209–1215. [DOI] [PubMed] [Google Scholar]
- 2. Bäck LJ, Rekola J, Raittinen L, et al. The feasibility of NBI in patients with suspected upper airway lesions: A multicenter study. Laryngoscope. 2017;127:1821–1825. [DOI] [PubMed] [Google Scholar]
- 3. Watanabe A, Tsujie H, Taniguchi M, Hosokawa M, Fujita M, Sasaki S. Laryngoscopic detection of pharyngeal carcinoma in situ with narrowband imaging. Laryngoscope. 2006;116:650–654. [DOI] [PubMed] [Google Scholar]
- 4. Puxeddu R, Sionis S, Gerosa C, Carta F. Enhanced contact endoscopy for the detection of neoangiogenesis in tumors of the larynx and hypopharynx. Laryngoscope. 2015;125:1600–1606. [DOI] [PubMed] [Google Scholar]
- 5. Desai AA, Pandya VK, Bhalani DB, Desai S, Parikh BD. Value of ultrasonography in laryngeal and laryngopharyngeal cancers. Indian J Otolaryngol Head Neck Surg. 2004;56:191–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mydlarz WK, Liu J, Blanco R, Fakhry C. Transcervical ultrasound identifies primary tumor site of unknown primary head and neck squamous cell carcinoma. Otolaryngol Head Neck Surg. 2014;151:1090–1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Keberle M, Kenn W, Hahn D. Current concepts in imaging of laryngeal and hypopharyngeal cancer. Eur Radiol. 2002;12:1672–1683. [DOI] [PubMed] [Google Scholar]
- 8. Kuno H, Onaya H, Iwata R, et al. Evaluation of cartilage invasion by laryngeal and hypopharyngeal squamous cell carcinoma with dual‐energy CT. Radiology. 2012;265:488–496. [DOI] [PubMed] [Google Scholar]
- 9. Kuno H, Onoya H, Fujii S, Ojiri H, Otani K, Satake M. Primary staging of laryngeal and hypopharyngeal cancer: CT, MR imaging and dual‐energy CT. Eur J Radiol. 2014;83:e23–35. [DOI] [PubMed] [Google Scholar]
- 10. Driessen JP, Caldas‐Magalhaes J, Janssen LM, et al. Diffusion‐weighted MR imaging in laryngeal and hypopharyngeal carcinoma: association between apparent diffusion coefficient and histologic findings. Radiology. 2014;272:456–463. [DOI] [PubMed] [Google Scholar]
- 11. Imre A, Pinar E, Erdoğan N, et al. Prevertebral space invasion in head and neck cancer: negative predictive value of imaging techniques. Ann Otol Rhinol Laryngol. 2015;124:378–383. [DOI] [PubMed] [Google Scholar]
- 12. Xia CX, Zhu Q, Cheng Y, Zhao HX, Jin ZZ. Sonographic Assessment of Hypopharyngeal carcinoma. J Ultrasound Med. 2011;30:217–225. [DOI] [PubMed] [Google Scholar]
- 13. Dhoot NM, Singh S, Choudhury B, et al. Evaluation of hypopharyngeal carcinoma using high‐resolution ultrasound: comparison with CT. J Clin Ultrasound. 2014;42:143–149. [DOI] [PubMed] [Google Scholar]
- 14. Murono S, Tsuji A, Endo K, et al. Evaluation of Modified Killian's Method: A technique to expose the hypopharyngeal space. Laryngoscope. 2014;124:2526–2530. [DOI] [PubMed] [Google Scholar]
- 15. Pan D, Zhu SY, Xu YB, Wu YF, Lun HM, Wei YY. Sonographic findings of nasopharyngeal carcinoma and its involvement in the parapharyngeal space. J Ultrasound Med. 2013;32:1041–1047. [DOI] [PubMed] [Google Scholar]
- 16. Fakhry C, Agrawal N, Califano J, et al. The use of ultrasound in the search for the primary site of unknown primary head and neck squamous cell cancers. Oral Oncol. 2014;50:640–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. De Fiori E, Conte G, Ansarin M, et al. The role of ultrasound‐guided transcutaneous tru‐cut biopsy in diagnosing untreated and recurrent laryngo‐hypopharyngeal masses. Eur J Radiol. 2016;85:158–163. [DOI] [PubMed] [Google Scholar]
- 18. Gao Y, Liu JJ, Zhu SY, Yi X. The diagnostic accuracy of ultrasonography versus endoscopy for primary nasopharyngeal carcinoma. PLoS One. 2014;9 :e99679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jecker P, Schuon R, Hlawatsch A. Ultrasound of hypopharyngeal and oesophageal cancer: possibilities and limitations to staging and planning of therapy. Ultraschall Med. 2005;26:312–317. [DOI] [PubMed] [Google Scholar]
- 20. Amin MB, Shah JP, Lydiatt W, et al. AJCC Cancer Staging System, 8th Edition, New York, NY: Springer; 2016. [Google Scholar]
- 21. Kirchner FR. Endoscopic lateralization of the vocal cord in abductor paralysis of the larynx. Laryngoscope. 1979;89:1779–1783. [DOI] [PubMed] [Google Scholar]
- 22. Woodson GE. Configuration of the glottis in laryngeal paralysis. I: Clinical study. Laryngoscope. 1993;103:1227–1234. [DOI] [PubMed] [Google Scholar]
- 23. Bakhshaee M, Davoudi Y, Mehrabi M, et al. Vasucular pattern and spectral parameters of power Doppler ultrasound as predictors of malignancy risk in thyroid nodules. Laryngoscope. 2008;118:2182–2186. [DOI] [PubMed] [Google Scholar]
- 24. Dighe M, Barr R, Bojunga J, et al. Thyroid ultrasound: state of art part 1—Thyroid ultrasound reporting and diffuse thyroid disease. Med Ultrason. 2017;19:79–93. [DOI] [PubMed] [Google Scholar]


