Abstract
Objective
To assess the role and effect of concomitant adjunctive procedures when combined with balloon dilation of the Eustachian tube (BDET), including a new technique for treating obstructive disease within the bony Eustachian tube (ET).
Study Design
Retrospective case series.
Setting
Tertiary medical center.
Subjects
Adults with persistent (≥2 years): 1) OME or non‐fixed TM retraction AND type B or C tympanogram OR 2) Consistent symptoms of barochallenge with flights or diving, all despite medical treatment for ≥6 weeks.
Methods
Balloon dilation of the cartilaginous ET (BDET) was performed under general anesthesia using concomitant myringotomy with or without tube placement if indicated. Adjunctive turbinectomy, adenoidectomy, and/or tympanoplasty were used in selected cases. For suspected disease in the bony ET, an illuminated guidewire was used for probing and clearing the lumen. Outcome measures were tympanogram, otomicroscopy, ET mucosal inflammation score, Valsalva maneuver, and PTA audiometry.
Results
67 ETs (48 patients) underwent BDET: 1) 30/67 balloon w/wo myringotomy, w/wo tube, 2) 20/67 plus adjunctive procedure or 3) 17/67 plus guidewire. Follow‐up was ranging from 0.4 to 3.4 years (mean 1.3 year, SD = 0.7). Significant improvement occurred in 79%. There was no significant difference in the failure rate comparing balloon dilation with adjunctive procedures 5/20 (25%) or without adjunctive procedures; 4/30 p = 0.45 (13%). Failure rate for BDET plus guide wire was 5/17 (29%) and resistance within the bony ET occurred in 8/17 (47%).
Conclusion
Balloon dilation of the cartilaginous ET demonstrated significant improvement despite expansion of indications that necessitated the addition of adjunctive procedures.
Level of Evidence
4
Keywords: Eustachian tube, middle ear, otitis media
INTRODUCTION
The cartilaginous part of the ET acts as a dynamic valve where tubal dilation and ventilation of the middle ear takes place.1, 2 Tubal function may occur as a spectrum ranging from dilatory dysfunction with otitis media with effusion (OME) at one end, barochallenge symptoms approaching the middle, normal function at the midpoint and patulous dysfunction at the opposite end. It is noteworthy that tubal function or dysfunction can vary on this spectrum with some disorders causing dilatory or patulous dysfunction at different times in the same patient.3, 4
ET dilatory dysfunction is most commonly caused by inflammation within the cartilaginous portion and possible etiologies could include infection (either viral5 or bacterial), nasal allergy,6 laryngopharyngeal reflux7 or primary mucosal diseases.3
Laser,8 microdebrider,9 and more recently balloon dilation of the Eustachian tube have been used to reduce refractory inflammatory tissue within the cartilaginous ET after failure of medical management and tympanostomy tubes. Laser and microdebrider are limited to removal of tissue on the postero–medial intraluminal surface of the ET orifice, but balloon dilation of the ET may have circumferential effects and benefits.10
Transnasal endoscopic balloon dilation of the cartilaginous ET was introduced in 2010 by Ockermann and colleagues11 in a pilot study of 8 patients with severe dilatory dysfunction and showed an improvement in all patients assessed by a non‐validated ET score with 2 months' follow up. Silvola et al12 conducted a prospective cohort study on 37 patients (41 ETs), mean follow‐up 2.5 years with 80% (33/41) success in patients' ability to perform Valsalva maneuver. Type A tympanograms improved from 1/41 to 23/41 (56%).
Balloon dilation has been increasingly reported, demonstrating clinical improvements and safety, but with variable indications and outcome measures and lack of controls.13 There is a lack of evidence for efficacy for balloon dilation when used concomitantly with other procedures after expanding its indications. The purpose of this study is to address the effect of adjunctive procedures when combined with balloon dilation of the ET and to introduce a new technique for addressing obstruction of the bony ET.
PATIENTS AND METHODS
This retrospective study was performed at our tertiary medical center from 2011 to 2015, and was approved by the hospital IRB. All surgeries were performed by the corresponding author.
Inclusion criteria were adults age ≥18 years with persistent (≥2 years) symptoms of: 1) Either unilateral/bilateral OME or non‐fixed tympanic membrane (TM) retraction and type B or C tympanogram, OR 2) Unilateral or bilateral baro‐challenge with flights or diving.
All patients failed to improve despite optimal medical treatment of any underlying conditions such as allergy (oral antihistamine, intranasal corticosteroid, and modified Valsalva maneuver) or reflux (patients were referred to gastroenterologist for reflux control) for ≥6 weeks. Exclusion criteria were follow‐up duration less than 6 months, prior Eustachian tube surgery, or adhesive otitis media.
All patients were tested for their ability to perform modified Valsalva maneuver. Oto‐microscopy, nasopharyngoscopy, and video endoscopy of ET function were performed. The degree of mucosal inflammation was scored using a validated instrument from 1 = normal to 4 = severe.14
High resolution computed tomography (CT) was performed to exclude dehiscence of the internal carotid artery (ICA) into the tubal lumen on all patients selected for insertion of an illuminated guidewire through the bony portion of ET. Indications for the illuminated guide wire were CT findings of persistent opacification within the bony ET or absence of evidence of ET dysfunction within the cartilaginous ET on endoscopy.
Surgical Procedures
All procedures were performed under general anesthesia. A 6 × 16 sinuplasty balloon (off‐label use, Acclarent, Irvine, CA) was used for dilation of the cartilaginous ET.
Balloon dilation technique
The balloon dilation technique has been previously described in detail as a transnasal endoscopic‐assisted (45 degree view angle, 4 mm dia, Karl Storz, CA) procedure using the sinuplasty system.12, 15 A 70‐degree guide catheter loaded with the balloon catheter was inserted along the floor of the nasal cavity. The balloon catheter was inserted gently and slowly to allow the flexible catheter to guide alone the s‐shaped curvature of the tubal lumen. Great care was taken to avoid any trauma to the mucosa with lacerations or mucosal tears. Entry into a false passage could cause bleeding or risk carotid injury and inflation outside the ET or blockage of the lumen of the catheter could cause back pressure into the middle ear during inflation. The catheter was inserted until gently meeting resistance from the bony‐cartilaginous isthmus and stopping before reaching to the bony ET. At this point of insertion, a yellow marker 31 mm from the balloon distal end would usually be at the level of ET anterior cushion (not inside the orifice as the average length of the cartilaginous ET is 25 mm.1 Balloon was inflated with saline up to 12 atm and maintained for 2 minutes in most patients or 1 minute in baro‐challenge subjects with minimal burden of inflammatory disease. If the balloon slipped outside the ET, it was deflated and reinserted into the ET again to complete the intended dilation time. A second inflation for another 1 minute (total 3 minutes) was used in cases of exceptionally severe mucosal inflammation.
Myringotomy was done for TM retraction to the Incus or promontory associated with partial middle ear effusion to facilitate early middle ear aeration. A tympanostomy tube was inserted when the middle ear was filled with mucoid effusion.
Adjunctive procedures
Adenoidectomy was performed using monopolar suction cautery (Fig. 1) passed transorally with transnasal endoscopic guidance. Adenoid tissue within the lateral recesses was distracted from fossa of Rosenmüller and then cauterized to maintain a distance from ICA. Lastly, cautery was turned down to 15 watts for light cauterization up to midline of Torus tubarius. Coblation wand was used for submucosal turbinate reduction. If there were a spur of cartilage projecting from the postero‐medial wall into the lumen of ET, preventing uniform balloon dilation, cold steel or laser resection of the spur was done. In those cases, a vertical incision was made over the medial aspect of the Torus tubarius, dissecting down to cartilage creating a mucoperichondrial flap. Scissors dissection or laser vaporization of the spur was accomplished, followed by balloon dilation.
Figure 1.
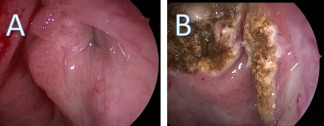
Adenoidectomy using section cautery. A: preoperative view of adenoids and tubal adenoids. B: postoperative view after performing suction cautery of the adenoids and the tubal adenoids.
Exploration of the bony ET with illuminated guidewire
In a technique similar to that described by Silvola to explore the bony ET,12 the sinuplasty balloon device allowed for insertion of an illuminated guidewire (Luma sinuplasty guidewire, 0.9 mm diameter, Acclarent, Irvine, CA) through the balloon catheter. Once in position at the isthmus, the guidewire was inserted into the balloon catheter until the light became visible at the tubal orifice. The endoscope was removed from the nose, and a 0 degree endoscope passed into the ear to see the tympanic membrane. The guidewire was marked to indicate the expected 15 mm additional insertion distance through the isthmus and bony ET to enter the middle ear. The light on the endoscope was turned down to stand‐by so that a faint red glow could be seen as the guidewire approached the middle ear in an unobstructed case. The guidewire was very slowly and gently advanced until reaching the middle ear, where the bright white light was easily observed (Fig. 2) and the guidewire then withdrawn. The TM was observed at all times to avoid contact of the guidewire with the TM, ossicles or the location of the ICA in the protympanum. It is critical to remove the guidewire entirely to maintain an open lumen in the balloon catheter during inflation to prevent backpressure from building up within the middle ear. In the event of meeting resistance during passage through the bony ET, the guidewire was moved in and out very slowly and cautiously to palpate the nature of the restriction and in the hopes that the back and forth movements might break through the resistance.
Figure 2.

Probing of the left bony Eustachian tube by the illuminated guidewire. A: intraoperative view showing introduction of the balloon until the isthmus). B: insertion of the illuminated guide wire inside the balloon catheter (arrow). C: visualization of the illuminated guide wire in the middle ear (arrow).
Post‐operative follow‐up
Patients were advised to refrain from nose blows or Valsalva maneuvers for the first week to avoid subcutaneous emphysema, especially if there had been any bleeding suggesting laceration of the mucosa. They were then asked to perform a modified Valsalva maneuver (closed nose/mouth, gentle nose blow with strong swallow) hourly while awake for the next 3 weeks.
Patients were instructed to continue their medical treatment for any associated allergy, sino‐nasal disease or laryngopharyngeal reflux as indicated. Postoperative visits were scheduled at 1, 6, and more than 12 months. Outcome measures included ability to perform modified Valsalva, otomicroscopy, tympanometry, pure tone audiometry at 500, 1000, 2000, and 3000 hertz according to the guidelines of the Committee on Hearing and Equilibrium,16 and mucosal inflammation rating score for ET.14
Criteria for clinical success after balloon dilation of the Eustachian tube were: 1) normal or mildly retracted TM by otomicroscopy, 2) type A tympanogram or type C tympanogram (if hearing was normal), and 3) asymptomatic with barochallenges. Criteria for failure were absence of the above criteria for success, including : 1) OME, moderate or severe TM retraction/atelectasis/retraction pockets by otomicroscopy; 2) type B tympanogram; or type C with decreased hearing or 3) symptoms with barochallenge.
Data Analysis
Clinical success rates were compared between the three groups (BDET, BDET plus adjunctive procedure, and BDET plus guide wire) using Fisher's exact test. For failure rate, time to event analysis was performed using the Kaplan‐Meier method and the log‐rank test. We also evaluated any change in the outcome between pre‐operative period and post‐operative period (1 month, 6 months, and 12 months). The generalized linear models using generalized estimating equations (GEE) approach were employed to account for correlations within‐individual measurements in this longitudinal data. The probabilities of intact healthy by otomicroscopy, type A tympanogram, and positive Valsalva were evaluated using the logistic regression models. Audiogram and mucosal inflammation were evaluated based on the model assuming a gamma distribution with a log link function. The differences in improvement of outcome between three groups were examined by adding the interaction terms between intervention groups and post‐operative period in the model. All statistical analyses were conducted using SAS, version 9.13 (SAS Institute, Cary, NC) and R statistical software.
RESULTS
Subjects
Out of 99 ETs (69 patients), 15 patients were lost in follow‐up and ultimately 67 ETs (48 patients) met criteria for inclusion.
Demographic data and distribution of procedures are summarized in Table 1.
Table 1.
Demographic Characteristics Among All the Study Subjects.
| Characteristics |
N (%) or mean (SD) |
|---|---|
| Patient characteristics | 48 patients |
| Male, Female | 34 (71%), 14 (29%) |
| Age (years), mean (SD) |
50 (± 16) (range 18–72) |
| Symptom duration (years), median (IQR) | 14 (5–26) |
| Chronic Rhino‐sinusitis w or w/o polyposis | 5 (10%) |
| Smoking | 3 (6%) |
| Allergies | 24 (55%) |
| Reflux | 9 (20%) |
| No. of previous tympanostomy tubes, median (IQR) | 3 (1–7) |
| Balloon dilation surgery | 67 ETs |
| Dilation without major adjunctive procedures | 30 (45%) |
| Dilation only | 24 (36%) |
| Dilation with myringotomy w or w/o tube | 6 (9%) |
| Major adjunctive/illuminated guidewire procedures | 37 (55%) |
| Dilation with adjunctive procedure | 20 (30%) |
| Dilation with illuminated guidewire | 17 (25%) |
| Indication for surgery | |
| Chronic persistent or recurrent OME | 46 (69%) |
| Chronic OME and recurrent infection | 8 (12%) |
| Barochallenge | 13 (19%) |
| Duration of follow up (years), mean (SD) |
1.3 (± 0.7) (range 0.54–3.4) |
IQR = median interquartile range); OME = otitis media with effusion; SD = standard deviation
Prior tympanostomy tubes had been performed in 55% (37/67) of ears.
Surgical Outcomes
Thirty ETs underwent BDET without guidewire exploration or adjunctive nasal or major ear operations. Of those, 24 had BDET alone, six had a myringotomy with or without tympanostomy tube.
Balloon dilations were maintained for 2 minutes in 51/67 ETs, an additional 1 minute inflation for a total of 3 minutes (due to severe mucosal disease) in 13/67 minutes, and 1 minute only in 3/67 (barochallenge with minimal inflammation).
An illuminated guide wire was passed through 17 bony ETs. It passed freely into the middle ear in 53% (9/17), while some resistance or obstruction was met in 47% (8/17) of the bony ETs. The lumen was cleared allowing for passage of the guidewire into the middle ear in each case, with the sensation that the wire had been advanced through a tight/restricted lumen, a short soft tissue web or a longer firmer, rubbery blockage.
Various adjunctive procedures (other than myringotomy/tube/guidewire) were done concomitantly with 20 balloon dilations and are summarized in Table 2.
Table 2.
Adjunctive Procedures Which Were Performed in the Balloon Plus Adjunctive Group (N = 20 ETs).
| Adjunctive Procedures | Frequency | Percent |
|---|---|---|
| Tympanoplasty, adenoidectomy | 1 | 5 |
| Adenoidectomy | 5 | 25 |
| Adenoidectomy, turbinate reduction | 1 | 5 |
| Excision of Eustachian cartilage spur | 2 | 10 |
|
Aural polypectomy, myringotomy, adenoidectomy, turbinate reduction |
1 | 5 |
| Lysis of ME Adhesions, M and T | 1 | 5 |
| M and tube removal from middle ear | 1 | 5 |
| Removal Tube, TM patch | 2 | 10 |
| Tympanoplasty ± mastoidectomy | 2 | 10 |
| Adenoidectomy, M and T | 2 | 10 |
| Adenoidectomy, TM patch | 1 | 5 |
| Turbinate reduction | 1 | 5 |
| Total | 20 | 100 |
ME = middle ear; M = myringotomy; T = tympanostomy tube insertion; TM = tympanic membrane.
Overall success rate was 79%. Type A tympanograms showed significant post‐operative improvements in all three groups: BDET group (p < 0.001), dilation plus adjunctive procedure group (p < 0.001), and dilation plus illuminated guide wire group (p = 0.05; Table 3 and Fig. 3). Otomicroscopy (intact healthy TM) findings indicated significant improvements in BDET group (p < 0.001) and dilation plus adjunctive procedure group (p = 0.027), but not in dilation plus illuminated guide wire group (p = 0.28). There was no significant difference in improvements of outcome following surgery comparing BDET group and dilation plus adjunctive procedure group (otomicroscopy, p = 0.91 and tympanogram, p = 0.40); however, there was a significant difference in improvements in the outcome comparing BDET group with balloon dilation plus illuminated guide wire (otomicroscopy, p = 0.001 and tympanogram, p = 0.05).
Table 3.
Otomicroscopy and Tympanogram Results Comparing Balloon Dilation of the Eustachian Tube Only, Balloon Dilation With Adjunctive Procedure, and Balloon Dilation With Illuminated Guidewire.
| Balloon dilation ET | Balloon dilation plus adjunctive procedure | Balloon dilation plus illuminated guide wire | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post 1 m | Post 6 m | Post 12 m | p‐value | Pre | Post 1 m | Post 6 m | Post 12 m | p‐value | Pre | Post 1 m | Post 6 m | Post 12 m | p‐value | |
| Otomicroscopy | |||||||||||||||
| Total n | 30 | 26 | 26 | 16 | 19 | 14 | 14 | 10 | 17 | 15 | 14 | 9 | |||
| Intact healthy | 7 (23%) | 15 (58%) | 18 (69%) | 11 (69%) | <0.001 | 4 (21%) | 7 (50%) | 9 (64%) | 8 (80%) | <0.001 | 1 (6%) | 2 (13%) | 2 (14%) | 3 (33%) | 0.28 |
| Perforated/tube | 5 (17%) | 5 (19%) | 2 (8%) | 1 (6%) | 3 (16%) | 2 (14%) | 3 (21%) | 1 (10%) | 3 (18%) | 9 (60%) | 7 (50%) | 2 (22%) | |||
| Retracted | 6 (20%) | 5 (19%) | 3 (12%) | 2 (13%) | 4 (21%) | 3 (21%) | 1 (7%) | 1 (10%) | 5 (41%) | 1 (7%) | 3 (21%) | 2 (22%) | |||
| Effusion | 10 (33%) | 1 (4%) | 2 (8%) | 2 (13%) | 4 (21%) | 2 (14%) | 1 (7%) | 0 (0%) | 6 (35%) | 2 (13%) | 2 (14%) | 2 (22%) | |||
| Atelectasis/retracted, adherent | 2 (7%) | 0 (0%) | 1 (4%) | 0 (0%) | 4 (21%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (12%) | 1 (7%) | 0 (0%) | 0 (0%) | |||
| Tympanogram | |||||||||||||||
| Total n | 27 | 24 | 19 | 14 | 17 | 10 | 11 | 10 | 17 | 10 | 11 | 7 | |||
| A | 7 (26%) | 14 (58%) | 13 (68%) | 9 (64%) | <0.001 | 5 (29%) | 5 (50%) | 5 (46%) | 5 (50%) | 0.027 | 1 (6%) | 2 (20%) | 3 (27%) | 2 (29%) | 0.05 |
| B | 4 (15%) | 0 (0%) | 0 (0%) | 0 (0%) | 4 (24%) | 2 (20%) | 0 (0%) | 0 (0%) | 12 (71%) | 1 (10%) | 1 (9%) | 2 (29%) | |||
| C | 12 (44%) | 6 (25%) | 4 (21%) | 3 (21%) | 5 (29%) | 1 (10%) | 2 (18%) | 3 (30%) | 4 (24%) | 0 (0%) | 2 (18%) | 1 (14%) | |||
| B/open | 4 (15%) | 4 (17%) | 2 (11%) | 2 (14%) | 3 (18%) | 2 (20%) | 4 (36%) | 2 (20%) | 0 (0%) | 7 (70%) | 5 (45%) | 2 (29%) | |||
Figure 3.
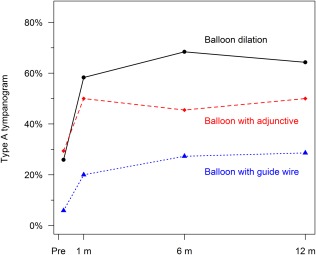
Type A tympanogram probability over time among the three groups.
 Balloon Dilation
Balloon Dilation
 Balloon with Adjunctive
Balloon with Adjunctive
 Balloon with Guidewire
Balloon with Guidewire
As shown in Table 4, Valsalva maneuver (positive valsalva) and mucosal inflammation score significantly improved in all three groups in post‐operative period (p < 0.001 for all groups), while A/B gap significantly decreased in BDET and dilation plus guide wire groups (p = 0.017 and 0.001, respectively), but not significant in dilation plus adjunctive procedures group (p = 0.73). There was no significant difference in improvements of valsalva maneuver, A/B gap closure, or mucosal inflammation score following surgery among three groups.
Table 4.
Valsalva Maneuver, Audiogram and Mucosal Inflammation Results Comparing Balloon Dilation of the Eustachian Tube Only, Balloon Dilation Plus Adjunctive Procedure, and Balloon Dilation With Illuminated Guidewire.
| Balloon dilation ET | Balloon dilation plus adjunctive procedure | Balloon dilation plus illuminated guide wire | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post 1 m | Post 6 m | Post 12 m | p‐value | Pre | Post 1 m | Post 6 m | Post 12 m | p‐value | Pre | Post 1 m | Post 6 m | Post 12 m | p‐value | |
| Valsalva | |||||||||||||||
| Total n | 30 | 22 | 19 | 11 | 18 | 8 | 8 | 6 | 15 | 5 | 1 | 7 | |||
| Positive | 6 (20%) | 20 (91%) | 17 (89%) | 11 (100%) | <0.001 | 0 (0%) | 5 (63%) | 7 (88%) | 5 (83%) | <0.001 | 2 (13%) | 3 (60%) | 1 (100%) | 7 (100%) | <0.001 |
| Negative | 24 (80%) | 2 (9%) | 2 (11%) | 0 (0%) | 18 (100%) | 3 (37%) | 1 (12%) | 1 (17%) | 13 (87%) | 2 (40%) | 0 (0%) | 0 (0%) | |||
| Audiogram | |||||||||||||||
| Total n | 27 | 18 | 13 | 12 | 15 | 6 | 8 | 8 | 14 | 12 | 11 | 7 | |||
| A/B gap | 12 (±10) | 9 (±12) | 14 (±14) | 10 (±9) | 0.017 | 15 (±13) | 10 (±10) | 10 (±7) | 15 (±17) | 0.73 | 23 (±16) | 8 (±11) | 12 (±9) | 2 (±3) | <0.001 |
| Average PTA air | 34 (±17) | 33 (±23) | 37 (±22) | 35 (±16) | 40 (±18) | 34 (±9) | 30 (±21) | 39 (±27) | 48 (±29) | 38 (±30) | 22 (±11) | 23 (±15) | |||
| Average PTA bone | 22 (±13) | 23 (±16) | 23 (±15) | 25 (±14) | 25 (±12) | 23 (±13) | 19 (±16) | 24 (±12) | 24 (±19) | 30 (±21) | 10 (±8) | 20 (±14) | |||
| Mucosal inflammation | |||||||||||||||
| Total n | 24 | 23 | 16 | 7 | 11 | 10 | 6 | 5 | 7 | 6 | 2 | 3 | |||
| Score | 2.9 (±0.3) | 1.4 (±0.6) | 1.3 (±0.5) | 1.3 (±0.5) | <0.001 | 3.2 (±0.6) | 1.9 (±0.7) | 1.3 (±0.5) | 1.4 (±0.6) | <0.001 | 2.4 (±1.0) | 1.0 (±0) | 1.5 (±0.7) | 1.3 (±0.6) | <0.001 |
A/B gap = air/bone gap; PTA = pure tone audiometry.
Overall failure rate as of the last follow‐up visit was 21% (14/67). Failure rate for dilation plus illuminated guide wire 29% (5/17) was higher than the other groups; failure rate was 25% (5/20) for dilation plus adjunctive procedures group and 13% (4/30) for the BDET group. However, there was no significant difference in time to failure among the three groups (long‐rank test p = 0.15; (Fig. 4). Failure rate by indication showed a higher failure rate 75% (6/8) among the chronic OME and infection group (recurrent AOM, recurrent infection of perforated TM) than other groups; failure rate for chronic OME group was 18% (8/45) and 0% for baro‐challenge group (p = 0.001).
Figure 4.
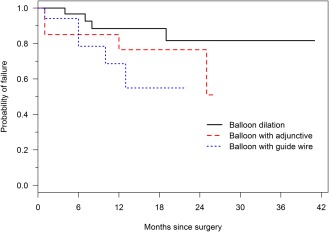
Probability of failure over time among the three groups.
 Balloon Dilation
Balloon Dilation
 Balloon with Adjunctive
Balloon with Adjunctive
 Balloon with Guidewire
Balloon with Guidewire
Adverse events
In one case a tiny perforation just anterior to the Malleus was made through the TM while inserting the illuminated guidewire because the light had been inadvertently turned off. The perforation healed spontaneously without any sequelae. Tiny mucosal tears within the ET lumen associated with self‐limited minimal bleeding occurred occasionally. One patient reported patulous ET symptoms for 2 years occurring during exercise.
DISCUSSION
This study demonstrated a beneficial effect of balloon dilation of the cartilaginous ET with or without adjunctive procedures/guidewire with overall 79% success rate and a mean follow‐up 1.3 years. There was no difference in improvement outcomes with the adjunctive procedures when compared to the BDET‐only group. The balloon dilation plus illuminated guidewire group showed a significant improvement in tympanometry, Valsalva, mucosal inflammation scores, and PTA results, but not in otomicroscopy outcome. The patients undergoing longer balloon dilation times, adjunctive procedures, or guidewire exploration of the bony ET were suspected of having a greater burden of mucosal inflammatory disease than we have previously treated with BDET alone. Despite that, the 79% overall success rate is comparable to past experience summarized in a recent systematic review.12
Balloon dilation has been shown to crush or strip off surface epithelium and to crush the lymphocytic infiltrate and follicles within the submucosa, which may allow for healing with a thin scar covered by healthy new mucosa. These results are similar to the findings after adenoidectomy.10 BDET can be thought of as an extension of adenoidectomy to remove the adenoid‐like tissue from within the tubal lumen. Therefore, the use of adjunctive procedures should be done at the discretion of the surgeon to reduce the burden of inflammatory disease as needed. Ongoing medical care may be necessary to maintain control of underlying medical conditions that caused the pathology. Careful and precise excision of the adenoid from the lateral recess is desirable when there is bulky disease interfering with tubal dilation.3
Inclusion criteria followed the consensus4 definition of dilatory ET dysfunction including negative middle ear pressure, retracted non‐adherent tympanic membrane, and consistent symptoms with barochallenge. Tympanic membrane retraction pockets likely begin with ET dilatory dysfunction, but once adhesions occur to the middle ear, inflammatory mechanisms may dominate, even after ET function may become normal or even patulous.17
McCoul and Anand18 conducted BDET with or without adjunctive nasal or sinus operations on 35 Eustachian tubes. Comparable to our results, improvements between BDET group and BDET with concurrent ESS were similar at each time point either with ETDQ‐7 symptom scores or SNOT‐22 scores. They also described passing an illuminated guidewire into the middle ear to confirm that a sinuplasty balloon catheter was correctly positioned within the lumen of the ET before inflating the balloon for BDET.
The bony ET is closely related to the ICA, sharing a thin bony plate.19 Exclusion of any dehiscence in this bony plate is mandatory before probing the ET bony portion. Resistance was met in nearly half of the guidewire group and could be from adhesions or other soft tissue that was encountered. The site of resistance within the bony ET was variable (isthmus, middle, or near middle ear).
Our results suggested a correlation between chronic ET dilatory dysfunction with recurrent AOM or recurrent infection on top of perforated TM and failure rate. Early post‐operative infection has been an important cause of failure with some association with uncontrolled underlying medical diseases such as allergy and laryngopharyngeal reflux.13 There was a higher failure rate in our balloon plus illuminated guidewire group which may be due to the higher burden of disease extending into the bony portion. Further studies are needed to evaluate the therapeutic effect of the illuminated guide wire in bony ET obstruction.
There were a number of limitations with this study, many of them inherent in the biases of a retrospective study without an external control group. However, the patients' ≥2‐year history of persistent symptoms served as their own historical controls. There were multiple interventions in this pilot trial such that the ability to control for the confounding factors or compare groups was limited. There was some exploration of optimal dilation times ranging between one to three minutes, but most were done at two minutes. Concomitant paracentesis or tube placement in some BDET patients was a confounding factor, but past studies without paracentesis have already demonstrated benefit and paracentesis has been shown to possibly reduce the recovery period of OME.20
Performance of a tympanoplasty concurrently with balloon dilation presented a significant confounding factor. However, we wished to report that there did not appear to be any negative effects of performing simultaneous tympanoplasty and that further research in this regard is indicated. The same criteria for success were applied to the healed tympanic membrane (absence of significant retraction, type A tympanogram or type C with normal hearing, absence of barochallenge complaints).
The ideal study would be a randomized controlled trial comparing tympanoplasty groups with and without balloon dilation. Assessments of Eustachian tube function would be done pre‐ and post‐operatively. The difficulty would be that it is well recognized that there are no ideal measures of ET function, so the study design would best utilize several measures.
A more practical study to be undertaken as a next step could be for a comparison of tympanoplasty outcomes of case‐controlled cohorts of patients, one with balloon dilation. Assessments of Eustachian tube function and endoscopic scoring of Eustachian tube inflammation could be done in both groups and the tympanoplasty outcomes compared between the two groups, either retrospectively or prospectively.
Care should be taken to assure that the guidewire light is turned on during its insertion. Although no significant consequences occurred in our case of TM perforation, the possibility for greater injury is apparent.
CONCLUSION
Balloon dilation of the cartilaginous ET demonstrated significant medium‐term benefit despite expansion of indications that necessitated the addition of adjunctive procedures. Illuminated guidewire exploration for identifying and treating possible obstruction within the bony ET is a novel technique that must be further studied for safety, efficacy, and improved technology is desired. Prospective studies are needed for assessment of the therapeutic effect of the illuminated guidewire exploration, the use of adjunctive procedures and standardization of the parameters used for balloon inflation.
AUTHOR CONTRIBUTIONS
Yehia Ashry, study design, data collection, manuscript Drafting, data review; Kosuke Kawai, study design, data review and analysis, review of manuscript; Dennis S. Poe (Corresponding Author), study design, data review and analysis, final review of manuscript, primary surgeon for all cases.
ACKNOWLEDGMENTS
The authors would like to acknowledge Rebecca Gore and Micayla Hinds for their contributions in data collection.
Financial Disclosures: Dennis Poe has received consultation fees from Acclarent, Inc. and OticPharma, LTD.
Conflict of Interest: The corresponding author is a consultant at Acclarent, Inc.
The contents of the manuscript were presented at the 2017 Triological Society Combined Sections Meeting, Sheraton, New Orleans, LA. January 19‐21, 2017.
BIBLIOGRAPHY
- 1. Bluestone CD, Bluestone MB. Eustachian Tube: Structure, Function, Role in Otitis Media. Lewiston, NY: BC Decker; 2005. [Google Scholar]
- 2. Poe DS, Pyykko I, Valtonen H, Silvola J. Analysis of eustachian tube function by video endoscopy. Am J Otol 2000;21:602–607. [PubMed] [Google Scholar]
- 3. Poe DS, Abou‐Halawa A, Abdel‐Razek O. Analysis of the dysfunctional eustachian tube by video endoscopy. Otol Neurotol 2001;22:590–595. [DOI] [PubMed] [Google Scholar]
- 4. Schilder AG, Bhutta MF, Butler CC, et al. Eustachian tube dysfunction: consensus statement on definition, types, clinical presentation and diagnosis. Clin Otolaryngol 2015;40:407–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Doyle WJ, Seroky JT, Angelini BL, Gulhan M, Skoner DP, Fireman P. Abnormal middle ear pressures during experimental influenza A virus infection—role of Eustachian tube function. Auris Nasus Larynx 2000;27:323–326. [DOI] [PubMed] [Google Scholar]
- 6. Ebert CS, Rose AS, Blanks DA, et al. Immune modulatory oligonucleotides in prevention of nasal allergen–induced Eustachian tube dysfunction in rats. Otolaryngol Head Neck Surg 2007;137:250–255. [DOI] [PubMed] [Google Scholar]
- 7. Miura MS, Mascaro M, Rosenfeld RM. Association between otitis media and gastroesophageal reflux: a systematic review. Otolaryngol Head Neck Surg 2012;146:345–352. [DOI] [PubMed] [Google Scholar]
- 8. Kujawski OB, Poe DS. Laser eustachian tuboplasty. Otol Neurotol 2004;25:1–8. [DOI] [PubMed] [Google Scholar]
- 9. Metson R, Pletcher SD, Poe DS. Microdebrider eustachian tuboplasty: a preliminary report. Otolaryngol Head Neck Surg 2007;136:422–427. [DOI] [PubMed] [Google Scholar]
- 10. Kivekas I, Chao WC, Faquin W, et al. Histopathology of balloon‐dilation Eustachian tuboplasty. Laryngoscope 2015;125:436–441. [DOI] [PubMed] [Google Scholar]
- 11. Ockermann T, Reineke U, Upile T, Ebmeyer J, Sudhoff HH. Balloon dilatation eustachian tuboplasty: a clinical study. Laryngoscope 2010;120:1411–1416. [DOI] [PubMed] [Google Scholar]
- 12. Silvola J, Kivekas I, Poe DS. Balloon dilation of the cartilaginous portion of the Eustachian tube. Otolaryngol Head Neck Surg 2014;151:125–130. [DOI] [PubMed] [Google Scholar]
- 13. Randrup TS, Ovesen T. Balloon Eustachian tuboplasty: a systematic review. Otolaryngol Head Neck Surg 2015;152:383–392. [DOI] [PubMed] [Google Scholar]
- 14. Kivekäs I, Pöyhönen L, Aarnisalo A, Rautiainen M, Poe D. Eustachian tube mucosal inflammation scale validation based on digital video images. Otol Neurotol 2015;36:1748–1752. [DOI] [PubMed] [Google Scholar]
- 15. Poe DS, Silvola J, Pyykko I. Balloon dilation of the cartilaginous eustachian tube. Otolaryngol Head Neck Surg 2011;144:563–569. [DOI] [PubMed] [Google Scholar]
- 16. Monsell EM. New and revised reporting guidelines from the Committee on Hearing and Equilibrium. Otolaryngol Head Neck Surg 1995;113:176–178. [DOI] [PubMed] [Google Scholar]
- 17. Poe D. Pathophysiology and Surgical Treatment of Eustachian Tube Dysfunction. Academic Dissertationthe board of the School of Medicine of the University of Tampere, Tampere, Finland December 2011. Available: https://tampub.uta.fi/bitstream/handle/10024/66848/978-951-44-8661-6.pdf?sequence=1
- 18. McCoul ED, Anand VK. Eustachian tube balloon dilation surgery. Int Forum Allergy Rhinol 2012;2:191–198. [DOI] [PubMed] [Google Scholar]
- 19. Ozturk K, Snyderman CH, Gardner PA, Fernandez‐Miranda JC. The anatomical relationship between the eustachian tube and petrous internal carotid artery. Laryngoscope 2012;122:2658–2662. [DOI] [PubMed] [Google Scholar]
- 20. Liang M, Xiong H, Cai Y, et al. Effect of the combination of balloon Eustachian tuboplasty and tympanic paracentesis on intractable chronic otitis media with effusion. Am J Otolaryngol 2016;37:442–446. [DOI] [PubMed] [Google Scholar]


