Abstract
Purpose
Given projected U.S. physician shortages across all specialties that will likely impact underserved areas disproportionately, the authors sought to explore factors most correlated with medical school graduates’ intention to work with underserved populations (IWUP).
Method
Data from the 2010–2012 Association of American Medical Colleges Medical School Graduation Questionnaire (n = 40,846) were analyzed. Variables (demographics, career preference, debt burden, intention to enter loan forgiveness programs) were examined using chi-squared tests and logistic regression models.
Results
Respondents included 49.5% (20,228/40,846) women, 16.6% (6,771/40,837) underrepresented minorities (URMs), and 32.4% (13,034/37,342) with primary care intent. The median educational debt was $160,000. Respondents who were women (adjusted odds ratio [aOR] 1.59, 95% confidence interval [CI] 1.49, 1.70), URMs (aOR 2.50, 95% CI 2.30, 2.72), intended to enter loan forgiveness programs (aOR 2.44, 95% CI 2.26, 2.63), intended to practice primary care (aOR 1.65, 95% CI 1.54, 1.76), and intended to emphasize non-clinical careers (aOR 1.23, 95% CI 1.11, 1.37) had greater odds of reporting IWUP. Among those who chose specialties and careers with a non-clinical emphasis, and among those with greater burdens of educational and consumer debt, URMs were nearly twice as likely as other minorities and whites to report IWUP.
Conclusions
Findings suggest physician characteristics that may be associated with filling workforce gaps in underserved areas. Restructuring financial incentive programs to support physician leaders and specialists with characteristics associated with IWUP may complement similar policies in primary care and can have key impacts on health equity in underserved areas.
As more Americans enroll in health insurance plans under the Patient Protection and Affordable Care Act (ACA) against the backdrop of a predicted physician shortage by 2030,1 there is a call to action to recruit physicians to serve in Medically Underserved Areas and Health Professional Shortage Areas in the United States.2,3 Although institutional, state, and national policies exist to increase the primary care workforce,4–10 little effort has been focused on improving access to specialty and subspecialty care, which are lacking in urban and rural underserved areas11–15--despite the roughly two-thirds majority of specialists among physicians in current practice nationwide.16 Compounding this problem are the trends of fewer U.S. medical school graduates intending to pursue full-time clinical practice; more graduates choosing specialization; and more young physicians heading into alternative careers (e.g. academic appointments, research, government positions).17–19 How these trends will affect medical school graduates’ decisions to work with medically underserved populations remains largely uncharacterized.
While it is well-established that underrepresented minority (URM) physicians are more likely to practice in underserved areas compared with non-Hispanic white physicians20–22 little is known about URM physicians who decide to pursue non-primary care career paths. One California study found that URM physicians who specialized were more likely to work in underserved areas than their white counterparts23; however, other factors mediating this workforce distribution were not fully examined. Independent of race/ethnicity, there are conflicting studies on the impact of debt on career preferences24–30; in most cases, these studies have not addressed intention to work with underserved populations (IWUP). A systematic review published in 2009 found that financial incentive programs have placed large numbers of health professionals in underserved areas, but the authors were unable to conclude whether this was due to the incentive programs or self-selection by participants.24
Given the projected physician shortages that will likely impact underserved areas disproportionately, we sought to explore key factors that may affect medical school graduates’ IWUP, including URM status, career preference (e.g., primary care or specialty care, clinical or non-clinical paths), debt burden, and intention to enter loan forgiveness programs after medical school graduation. We hypothesized that regardless of career preference and debt burden, URMs would be more likely report IWUP and plan to take advantage of loan forgiveness programs when compared with whites and other minorities. Through our analysis of the Association of American Medical Colleges (AAMC) 2010–2012 Medical School Graduation Questionnaire (GQ) dataset, we sought to provide information that is relevant to the workforce and can help inform policies that support equitable distribution of physicians, including specialists and those in key leadership roles, in the most underserved areas across the United States.
Method
Data source and survey design
The GQ is an annual, nationally representative Internet-based survey administered by the AAMC to graduating students at U.S. MD-granting medical schools. The GQ contains questions relevant to our analysis, including items on debt burden upon graduation, career preferences, and race/ethnicity. Survey participation is voluntary and classified as confidential, and some medical schools provide incentives for participation. Our analysis focused on combined de-identified data from the 2010–2012 GQ surveys (n = 40,846 respondents). The study protocol was reviewed and deemed non-human subjects research and exempted by the University of California, San Francisco Institutional Review Board.
Outcome variable
IWUP was identified by a “yes” response to the item “Do you plan to locate your practice in an underserved area?” (n = 11,330) and/or to the question “Regardless of location, do you plan to care primarily for an underserved population?” (n = 6,712). Respondents with missing, unknown, or conflicting responses to these questions were cross-checked using responses to a third question, “If yes, what location do you plan to practice? Inner city, rural, other.” Any response to this question--which was a follow-up to “Do you plan to locate your practice in an underserved area?”--was considered an affirmatory answer for IWUP. By this process, we identified a total of 13,034 respondents who indicated IWUP. While the GQ questions have changed slightly throughout the years, prior studies have used this outcome measure and we compared the consistency of results across other AAMC surveys including the Matriculating Student Questionnaire (MSQ), which uses the same IWUP questions.31,32
Descriptive and independent variables
We analyzed demographic variables including gender and race/ethnicity. We defined URM status by combining the 2003 AAMC definition of URM with the 2004 AAMC definition of underrepresented in medicine33: African American, Mexican American, mainland Puerto Rican, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, Cuban, Commonwealth Puerto Rican, other Hispanic/Latino, Vietnamese, Filipino, and other Southeast Asian. Respondents who self-identified as URMs accounted for 16.6% (6,771/40,837) of the study sample. Non-URM and non-white respondents, hereon referred to as other minorities (18.9%; 7,710/40,837), included those who self-identified as other Asian, Chinese, Korean, Japanese, Indian/Pakistani, Asian Indian, and Pakistani. Respondents who self-identified as white and not Hispanic/Latino were categorized as white (64.5%; 26,356/40,837). Because respondents could choose multiple races, we classified those who chose a combination of URM, other minority, and/or white as the least populous group. For example, if a respondent chose African American, Chinese, and white, we classified that respondent as URM. We excluded cases where race and Hispanic/Latino ethnicity responses were both missing (n = 9). If the respondent chose white and Hispanic/Latino ethnicity, we classified the individual as URM. If race was missing but the respondent indicated he or she was not Hispanic/Latino, we classified the individual as white.
We grouped career preference into two dichotomous variables: specialty (primary care career or specialty career) and type of practice (clinical emphasis or non-clinical emphasis). Primary care career was defined as family medicine, general internal medicine, general pediatrics, and internal medicine/pediatrics. Specialty career was defined as any non-primary care specialty (e.g., neurology, radiology, surgery). Respondents who answered “No” or “Undecided” to the question “Are you planning to become board certified in a specialty?” were excluded from the analysis (approximately 15% of the sample). We did not consider future intention of a fellowship after residency as indicating a specialty since one may still practice family medicine, for instance, after a fellowship. Non-clinical emphasis was defined as indicating medical or health care administration without practice, a state or federal government agency, full-time basic science teaching or research, or non-university research scientist, or as choosing “other” without specifying a scope of practice. Clinical emphasis included full or part-time practice whether as academic faculty or in non-academic, hospital, salaried, or solo practice. Respondents who answered “undecided” to the item “Indicate your career intention from the different activities listed below” were excluded from the analysis.
We grouped debt burden into two categorical variables: educational debt and consumer debt. Educational debt level was defined as any undergraduate loan debt plus medical school loan debt. Consumer debt level was based on the response to the question, “Please enter in the total amount of non-educational, consumer debt that you are legally required to repay. Note: Do not include home mortgage debt.” For simplicity, a three-tiered categorical variable was constructed for each type of debt and categorized based on median debt levels and obtaining even distributions. Intention to enter loan-forgiveness programs was based on a “yes” response to the question “Do you plan to enter into a loan-forgiveness program?”
Dual advanced degree was defined as any of the following combinations of degree programs completed upon graduation: MS–MD, MD–JD, MD–PhD, MD–other, MA–MD, MD–MBA, MD–MPH, MD–MPA, or MD–DDS.
Statistical analysis
We estimated proportional differences in outcome of IWUP by gender, URM status, dual advanced degree, career preference (using two variables: specialty and type of practice), debt burden (using two variables: educational debt and consumer debt), and intention to enter loan forgiveness programs. Chi-squared tests were used to test whether the differences in proportions were statistically significant. We ran multivariable logistic regression models to determine if any of the independent (predictor) variables were independently associated with IWUP. In all models, IWUP was regressed on gender, URM status, career preference, dual advanced degree, and debt burden. In Model 2, we examined the additional effects of intention to enter loan forgiveness programs. We constructed additional models (not shown) to test interaction terms: between URM status and educational debt level, and URM status and intention to enter loan forgiveness programs. Analyses were conducted using STATA version 12.1 (Stata Corp, College Station, Texas).
Results
Of the 2010–2012 GQ respondents (n = 40,846), 49.5% (20,228/40,846) were women, 16.6% (6,771/40,837) were URMs, and 32.4% (13,034/37,342) intended to practice primary care. The median educational debt owed was $160,000.
Factors associated with IWUP
Table 1 presents the proportions of respondents who reported IWUP by demographic and other characteristics. By gender, 41.5% (7,699/18,561) of women compared with 28.4% (5,335/18,781) of men reported IWUP. By URM status, 54.8 % (3,327/6,071) of URMs reported IWUP, as compared with 29.1% (2,006/6,889) of other minorities and 31.6% (7,698/24,376) of whites. IWUP was reported by 41.2% (4,179/10,142) of respondents who intended to enter a primary care career compared with 27.6% (5,832/21,151) of those who intended to pursue a specialty career. Of those who intended to pursue careers with a nonclinical emphasis, 39.1% (1,335/3,418) reported IWUP, whereas 35.4% (9,911/27,979) of those who planned to practice clinical medicine reported IWUP. There appeared to be a dose-response pattern for educational debt and IWUP, whereby a greater proportion of respondents with higher debt levels reported IWUP. Likewise, greater proportions of those with consumer debt levels ≥ $10,000 reported greater IWUP. Finally, of the respondents who reported intention to enter loan forgiveness programs, 53.9% (5,415/10,047) reported IWUP.
Table 1.
Intention to Work With Underserved Populations (IWUP) Among 2010–2012 AAMC Medical School Graduation Questionnaire Respondents (n = 40,846), by Demographic and Other Characteristics
| Independent variable (n; N)a | IWUP reported,b n (%) | P value |
|---|---|---|
| Gender (37,342; 40,846) | < .001 | |
| Women | 7,699/18,561 (41.5) | |
| Men | 5,335/18,781 (28.4) | |
| URM status (37,336; 40,837) | < .001 | |
| URMc | 3,327/6,071 (54.8) | |
| Other minorityd | 2,006/6,889 (29.1) | |
| White | 7,698/24,376 (31.6) | |
| Degree type (37,342; 40,846) | < .001 | |
| MD | 12,354/35,111 (35.2) | |
| Dual advanced degree (e.g., MD–PhD, MD–MPH) | 680/2,231 (30.5) | |
| Specialty (31,293; 31,444) | < .001 | |
| Primary care careere | 4,179/10,142 (41.2) | |
| Specialty careerf | 5,832/21,151 (27.6) | |
| Type of practice (31,397; 31,425) | < .001 | |
| Clinical emphasis | 9,911/27,979 (35.4) | |
| Nonclinical emphasis | 1,335/3,418 (39.1) | |
| Educational debtg (28,650; 28,679) | < .001 | |
| ≤ $49,999 | 1,618/5,873 (27.6) | |
| $50,000–199,999 | 4,902/13,691 (35.8) | |
| ≥ $200,000 | 3,450/9,086 (38.0) | |
| Consumer debth (28,127; 28,165) | < .001 | |
| ≤ $9,999 | 7,726/22,922 (33.7) | |
| $10,000–19,999 | 1,196/3,086 (38.8) | |
| ≥ $20,000 | 817/2,119 (38.6) | |
| Intention to enter loan forgiveness programs (37,088; 37,132) | 5,415/10,047 (53.9) | < .001 |
Abbreviations: AAMC indicates Association of American Medical Colleges; URM, underrepresented minority; MPH, master of public health.
n = Number of respondents who answered both predictor and outcome variable questions; N = total number of respondents who answered the predictor variable question.
IWUP was identified by a “yes” response to the item “Do you plan to locate your practice in an underserved area?” and/or to the question “Regardless of location, do you plan to care primarily for an underserved population?”
URM was defined as self-identification as African American, Mexican American, mainland Puerto Rican, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, Cuban, Commonwealth Puerto Rican, other Hispanic/Latino, Vietnamese, Filipino, and other Southeast Asian.
Other minority was defined as self-identification as other Asian, Chinese, Korean, Japanese, Indian/Pakistani, Asian Indian, and Pakistani.
Primary care career was defined as family medicine, general internal medicine, general pediatrics, and internal medicine/pediatrics.
Specialty career was defined as any non-primary care specialty (e.g., neurology, radiology, surgery, etc.).
Educational debt includes both undergraduate and medical school loan debt.
Consumer debt does not include mortgage debt.
Patterns in IWUP by URM status
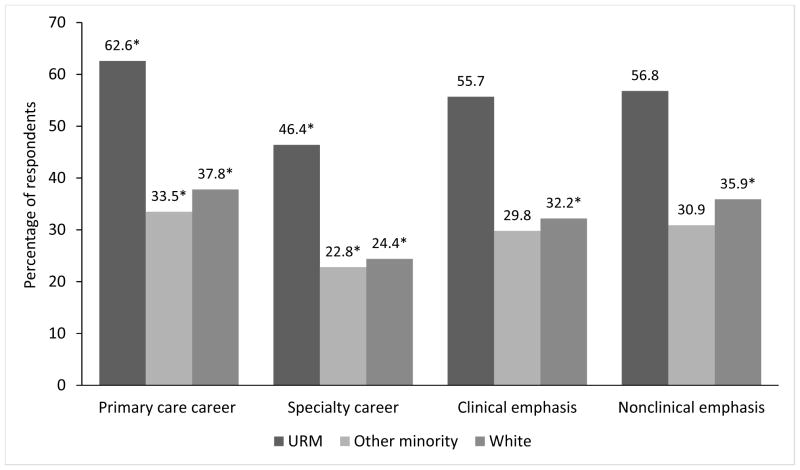
Figure 1 depicts the proportions of respondents who reported IWUP by career preference and URM status. Across each career type, greater proportions of URMs reported IWUP as compared with other minorities and whites. Nearly 63% (1,079/1,723) of URMs who chose primary care careers reported IWUP, as compared with 33.5% (642/1,916) of other minorities and 37.8% (2,457/6,501) of whites. Nearly twice the proportion of URMs who chose specialty careers reported IWUP (46.4%; 1,530/3,299), as compared with other minorities (22.8%; 859/3,764) and whites (24.4%; 3,442/14,086). Even among URMs who chose careers with a non-clinical emphasis, 56.8% (370/651) reported IWUP.
Figure 1.
Percentage of respondents with intention to work with underserved populations (IWUP) by career preference and underrepresented minority (URM) status, 2010–2012 Association of American Medical Colleges Medical School Graduation Questionnaire (n = 40,4846 medical school graduates).
*P < .001 for within group estimates
Among respondents who reported intention to enter loan forgiveness programs (data not shown), nearly half (49.3%; 4,974/10,095) indicated they would pursue Public Service Loan Forgiveness (PSLF). Other programs indicated by respondents included the National Health Service Corps (NHSC; 10.7%; 1,080/10,095); the Indian Health Service (IHS, which is responsible for American Indian and Alaska Native health in the United States; 1.1%; 110/10,095); other hospital programs (e.g., sign-on bonus; 14%; 1,408/10,095); and state programs (12.9%; 1,306/10,095).
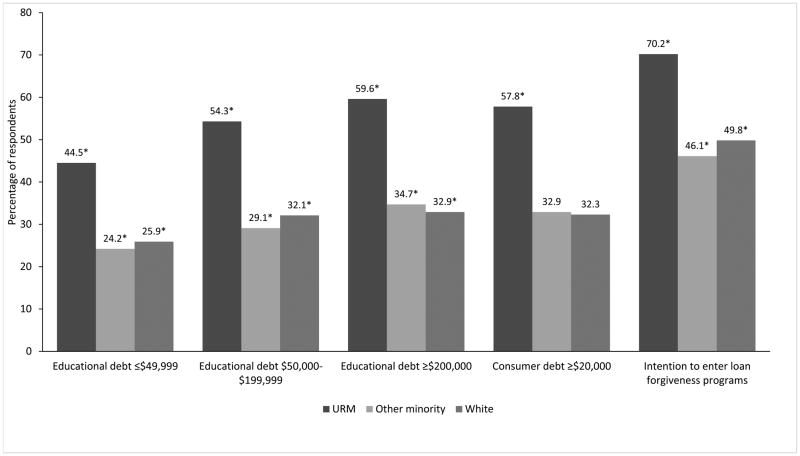
Figure 2 illustrates the effects of educational debt, consumer debt, and intention to enter loan forgiveness programs on IWUP by URM status. The graph suggests a dose-response pattern between increasing educational debt and IWUP, regardless of URM status. Even at the highest levels of educational debt (≥ $200,000) and of consumer debt (≥ $20,000), the proportion of URMs who reported IWUP was nearly twice that of other minorities and whites. Intention to enter loan forgiveness programs alone seemed to draw the highest proportion of respondents who reported IWUP: 70.2% (1,600/2,280) of URMs, 46.1% (624/1,355) of other minorities, and 49.8% (3,190/6,411) of whites. In a subanalysis (data not shown), a greater proportion of URMs (86.1%; 4,222/4,901) had higher educational debt levels (debt ≥ $50,000), as compared with other minorities (70.1%; 3,587/5,120) and whites (80.3; 14,987/18,654), P < .001. Similarly, significantly greater proportions of URMs (10.7%; 516/4,840) had higher levels of consumer debt (≥ $20,000), as compared with other minorities (3.5%; 171/4,900) and whites (7.8%; 1,433/18,421), P < .001.
Figure 2.
Percentage of respondents with intention to work with underserved populations (IWUP) by debt levels, intention to enter loan forgiveness programs, and underrepresented minority (URM) status, 2010–2012 Association of American Medical Colleges Medical School Graduation Questionnaire (n = 40,4846 medical school graduates).
*P < .001 for within group estimates
Predictors of IWUP: Multivariable models
Table 2 presents two multivariable logistic regression models and corresponding adjusted odds ratios after controlling for different factors (independent variables) that may affect or predict IWUP. In both models, women, URM, primary care career, and non-clinical emphasis were strongly predictive of IWUP. Model 1 showed an association between increasing educational and consumer debt and IWUP. However, when intention to enter loan forgiveness programs was added into Model 2, the association between educational and consumer debt and IWUP disappeared. Having a dual advanced degree was predictive of not reporting IWUP in either model. In Model 2, women had 1.59 odds (95% CI 1.49, 1.70) of reporting IWUP as compared with men. URMs had 2.50 odds (95% CI 2.30, 2.72) of reporting IWUP as compared with whites, even after controlling for debt burden, intention to enter loan forgiveness programs, gender, dual advanced degree, and career preference. These adjusted odds ratios comparing (1) women with men and (2) URMs with whites are somewhat similar to those reported in a prior study using 1996–2000 AAMC MSQ data that identified predictors of matriculating medical students’ plans to practice in underserved areas upon graduation.31 Respondents who indicated a preference for primary care careers had 1.65 odds (95% CI 1.54, 1.76) of reporting IWUP as compared with those planning to go into specialty careers. Those who indicated a non-clinical emphasis to their careers had 1.23 odds (95% CI 1.11, 1.37) of reporting IWUP as compared with those who indicated a clinical emphasis. Both models appeared to fit the data reasonably well given that the Hosmer-Lemeshow goodness-of-fit tests were not statistically significant.
Table 2.
Adjusted Odds Ratios for Intention to Work With Underserved Populations (IWUP)a Among 2010–2012 AAMC Medical School Graduation Questionnaire Respondents (n=40,846), by Demographic and Other Characteristics
| Independent variables | Model 1b aOR (95% CI) (n = 18,601)c | P value | Model 2b aOR (95% CI) (n = 18,575)c | P value |
|---|---|---|---|---|
| Gender | ||||
| Women | 1.61 (1.51, 1.72) | < .001 | 1.59 (1.49, 1.70) | < .001 |
| Men | 1 | 1 | ||
| URM status | ||||
| URMd | 2.62 (2.41, 2.85) | < .001 | 2.50 (2.30, 2.72) | < .001 |
| Other minoritye | 0.94 (0.86, 1.03) | .16 | 0.95 (0.87, 1.04) | .32 |
| White | 1 | 1 | ||
| Specialty | ||||
| Primary care careerf | 1.81 (1.69, 1.93) | < .001 | 1.65 (1.54, 1.76) | < .001 |
| Specialty careerg | 1 | 1 | ||
| Type of practice | ||||
| Nonclinical emphasis | 1.27 (1.15, 1.41) | < .001 | 1.23 (1.11, 1.37) | < .001 |
| Clinical emphasis | 1 | |||
| Educational debth | ||||
| ≤ $49,999 | 1 | 1 | ||
| $50,000–199,999 | 1.33 (1.23, 1.46) | < .001 | 1.05 (0.96, 1.15) | .26 |
| ≥ $200,000 | 1.61 (1.47, 1.77) | < .001 | 1.1 (0.99, 1.21) | .07 |
| Consumer debti | ||||
| ≤ $9,999 | 1 | 1 | ||
| $10,000–19,999 | 1.07 (0.96, 1.18) | .22 | 1.02 (0.91, 1.13) | .74 |
| ≥ $20,000 | 1.16 (1.02, 1.31) | < .05 | 1.12 (0.98, 1.27) | .09 |
| Dual advanced degree (e.g., MD–PhD, MD–MPH) | 0.83 (0.73, 0.95) | < .01 | 0.79 (0.69, 0.91) | < .001 |
| Intention to enter loan forgiveness programs | 2.44 (2.26, 2.63) | < .001 | ||
Abbreviations: AAMC indicates Association of American Medical Colleges; aOR, adjusted odds ratio; CI, confidence interval; URM, underrepresented minority; MPH, master of public health.
IWUP was defined as a “yes” response to the item “Do you plan to locate your practice in an underserved area?” and/or to the question “Regardless of location, do you plan to care primarily for an underserved population?”
Hosmer-Lemeshow Test: Model 1 chi-squared = 0.0626; Model 2 chi-squared = 0.1145
The n in this column heading refers to sample size in this model.
URM was defined as self-identification as African American, Mexican American, mainland Puerto Rican, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, Cuban, Commonwealth Puerto Rican, other Hispanic/Latino, Vietnamese, Filipino, and other Southeast Asian.
Other minority was defined as self-identification as other Asian, Chinese, Korean, Japanese, Indian/Pakistani, Asian Indian, and Pakistani.
Primary care career was defined as family medicine, general internal medicine, general pediatrics, and internal medicine/pediatrics.
Specialty career was defined as any non-primary care specialty (e.g., neurology, radiology, surgery, etc.).
Educational debt includes both undergraduate and medical school loan debt.
Consumer debt does not include mortgage debt.
When the models were stratified by intention to enter loan forgiveness programs, the associations between women, URM, primary care career, and IWUP were statistically significant (data not shown). Logistic regression models stratified by URM status yielded similar results. Logistic regression models were also run with only complete cases, and the results were essentially identical (data not shown). A chi-squared test between intention to enter loan forgiveness programs and IWUP was statistically significant (P < .001). Null findings from the analyses included interaction terms between URM status and educational debt, and URM status and intention to enter loan forgiveness programs (P values not statistically significant).
Discussion
To the best of our knowledge, this study using 2010–2012 AAMC GQ data is the first study to show that greater proportions of U.S. medical school graduates who were women, self-identified as URMs, intended to enter loan forgiveness programs after graduation, chose primary care careers, and preferred a non-clinical career path reported IWUP, as compared with those who did not have these characteristics. There was no association between debt burden and IWUP after controlling for intention to enter loan forgiveness programs. This finding counters a common perception that a large debt burden is a primary reason for medical school graduates not to work with underserved populations.34 Equally important, among those who chose specialty careers and careers with a non-clinical emphasis, URMs were nearly twice as likely as other minorities and whites to report IWUP. Among those with greater burdens of educational and consumer debt, URMs were nearly twice as likely as other minorities and whites to report IWUP. This illuminates a disparity in educational and consumer debt by URM status--a disparity that is present despite URMs’ intentions to fill critical workforce gaps.
Given the nature of most loan forgiveness programs that require service in underserved areas (e.g., PSLF, IHS, NHSC), the association between intention to enter loan forgiveness programs and IWUP was expected. However, our analysis provides valuable insights into how to better identify physicians who will work with underserved populations, regardless of career choice. Our findings can inform future efforts in restructuring financial incentive programs that could potentially support specialists and physician leaders with personal characteristics associated with IWUP. Such restructuring is particularly important given the projected nationwide specialist physician shortages of 33,500 to 61,800 by 2030.1 As an example, in a physician satisfaction survey within IHS, 86% of physicians indicated a moderate to urgent need for specialists in their service areas, and only 11% said they had ready access to specialists (0–7 days).35 Our analysis suggests that restructuring loan repayment programs to target female and URM specialists who indicate IWUP could help mitigate specialist shortages in underserved areas. At the same time, targeting URMs could offer a structural intervention to help to alleviate their disproportionate levels of educational debt.
A large body of evidence supports the effectiveness of financial incentive programs, such as loan repayment, in the recruitment and retention of physicians. A systematic review showed that incentive programs, in general, are successful in retaining physicians: Participants may not stay at the site of their original placements after their service obligations are fulfilled, but they are more likely to work in underserved areas in the long term, as compared with non-participants.24 An evaluation of the NHSC program (preferred by 10.7% of respondents in our study sample who intended to enter loan forgiveness programs) showed a 55% retention rate of clinicians in underserved areas 10 years after their service obligations were completed.36 Even more popular is the PSLF program, which was preferred by 49.3% of respondents in our study sample who indicated they intended to enter loan forgiveness programs. This program represents a means of alleviating debt for individuals employed at public or nonprofit institutions, regardless of profession or specialty, after they have made 120 qualifying loan repayments. However, citing the need to reduce inefficiencies and to focus on the needs of undergraduate borrowers, the fiscal year 2018 budget of the U.S. Government proposes eliminating the program altogether.37 Indeed, another study suggested that targeting PSLF loan repayment for work performed in Medically Underserved Areas, or for specialties that meet underserved areas’ societal needs could be useful and more equitable in retaining physicians in these communities, as opposed to the broad criteria that PSLF currently requires.38
That 56.8% of URMs interested in non-clinical careers reported IWUP suggests interventions such as diversifying the academic medicine pipeline could have a favorable impact on underserved populations. For example, in the United States there is a lack of diversity among academic medicine faculty (only 7.6% URM nationwide),39 and among the highest ranks of academic medicine, less than 8% of all medical school deans are black or Latino.40 URM faculty are usually disproportionately represented in institutional diversity efforts, and they face promotion inequities as well as other forms of subtle inequities.41 If the faculty pipeline is diversified with faculty who have personal characteristics associated with IWUP, these faculty may be able to contribute to a mission of excellence and inclusivity and to a social mission of reaching the most medically underserved populations by influencing the next generation of physicians.
Cultivating future physician leaders with IWUP represents an important innovation that could inform several key systems that deliver or impact health in the United States. Incentive programs provided through the IHS, the National Institutes of Health (for those interested in a research career), and the NHSC, for example, could consider incentivizing leadership development pathways for physicians working in research or governmental careers that align with organizational missions of achieving health equity for underserved populations.
Certainly, further research on policy innovation and program implementation is needed to help advance strategies that can increase and retain physicians in underserved areas.
Limitations
The AAMC GQ is a cross-sectional annual survey that includes items regarding IWUP in the United States. Respondents’ eventual career choices and entry into loan forgiveness programs were not verified. The way in which URM was classified in the GQ may have led to an overestimation of the actual number of URMs in this study (e.g., if more than one race was reported). To mitigate this possibility, our analysis adjusted the URM category by excluding minority groups that were not underrepresented in medicine. Given that the AAMC GQ data came aggregated, we were unable to analyze responses by year or class. The estimates of specialty and type of career may have been underestimated given that respondents who chose “undecided” (approximately 15%) were excluded from the relevant analysis. Factors that affect IWUP are extensive, and this study did not take into account other personal, institutional, or even practice characteristics outlined in the literature. Finally, lack of access to health care in rural and underserved areas is an international phenomenon that could be looked at more broadly for potential solutions.
That being said, our analysis examined three years of aggregated GQ data with a sample size and power sufficient for generating reliable estimates across multiple strata. Moreover, to address potential selection bias in those who voluntarily participated in the survey, we referenced trends in all graduates of U.S. MD-granting medical schools by gender and race/ethnicity for the same time period. Our gender and race/ethnicity distribution results in this study were identical to the gender and race/ethnicity distribution of all medical school graduates for the corresponding time frame (17% URM, 48% female).42 Our analysis is also the first of its kind to examine career preference, URM status, debt burden, and intention to enter loan forgiveness programs, together in one model, to predict IWUP. Results from other studies examining the role of debt on career preference have generally been mixed.24–30 Prior studies have not examined the role of loan forgiveness programs as a potential mediator or moderator.
Conclusions
Our findings suggest physician characteristics associated with filling critical workforce gaps. Innovative strategies to restructure financial incentive programs and increase workforce diversity could enhance and complement similar programs in primary care. Cultivating key physician leaders in health equity, diversifying the academic medicine pipeline, and ensuring systems-based changes in underserved areas represent potentially sustainable upstream approaches for helping the U.S. health care system achieve greater equity in the quality and availability of care for all.
Acknowledgments
The authors thank the staff at the Association of American Medical Colleges for their technical support of the project, in particular, their assistance with the management of the Medical School Graduation Questionnaire dataset and approval of the manuscript.
Funding/Support: The project was supported in part by the Resource Centers for Minority Aging Research program at the National Institute on Aging (NIA). E.J.. Pérez-Stable’s time at the University of California, San Francisco was supported with funding from the National Institutes of Health (P30 AG15272). The NIA had no involvement in any aspect of the study design, data analysis, or interpretation of the results.
Footnotes
Other disclosures: None reported.
Ethical approval: The study protocol was reviewed and deemed non-human subjects research and exempted by the University of California, San Francisco Institutional Review Board (October 2012).
Disclaimer: The findings and conclusions in this article are those of the authors and do not necessarily represent the views or the official position(s) of the National Institutes of Health or any of the sponsoring organizations and agencies of the U.S. government, the Los Angeles County Department of Public Health, the California Department of Public Health, the University of California San Francisco School of Medicine, or of the Association of American Medical Colleges or any other agency or organization mentioned in the text.
Previous presentations: Association of American Indian Physicians Annual Meeting, August 2015, Tulalip, Washington.
Contributor Information
Andrea N. Garcia, Fellow with the National Clinician Scholars Program at the University of California, Los Angeles. At the time of submission, the author was a general and preventive medicine resident, California Department of Public Health, Sacramento, California, assigned to the Division of Chronic Disease and Injury Prevention, Los Angeles County Department of Public Health, Los Angeles, California. The project was conceived while the author was a medical student at the University of California, San Francisco, San Francisco, California.
Tony Kuo, Adjunct associate professor of epidemiology, UCLA Fielding School of Public Health and Health Sciences, and associate professor of family medicine, David Geffen School of Medicine at UCLA, Los Angeles, California. The author also directs the Division of Chronic Disease and Injury Prevention and the Office of Senior Health, Los Angeles County Department of Public Health, Los Angeles, California.
Lisa Arangua, Policy analyst, Division of Chronic Disease and Injury Prevention, Los Angeles County Department of Public Health, Los Angeles, California.
Eliseo J. Pérez-Stable, Director, National Institute on Minority Health and Health Disparities, National Institutes of Health, Bethesda, Maryland. This project was conceived while the author was professor of medicine and chief, Division of General Internal Medicine, Department of Medicine, and director, Medical Effectiveness Research Center for Diverse Populations, University of California, San Francisco, San Francisco, California.
References
- 1.Prepared for the Association of American Medical Colleges. Washington, DC: Association of American Medical Colleges; 2017. The Complexities of Physician Supply and Demand 2017 Update: Projections From 2015 to 2030. IHS Markit. [Google Scholar]
- 2.Institute of Medicine. Graduate Medical Education That Meets the Nation’s Health Needs. Washington, DC: The National Academies Press; 2014. [PubMed] [Google Scholar]
- 3.Freeman J, Ferrer RL, Greiner KA. Viewpoint: Developing a physician workforce for America’s disadvantaged. Acad Med. 2007;82(2):133–8. doi: 10.1097/ACM.0b013e31802d8d242. [DOI] [PubMed] [Google Scholar]
- 4.National Health Service Corps. [Accessed June 29, 2017];NHSC Loan Repayment Program. http://nhsc.hrsa.gov/loanrepayment/loanrepaymentprogram.html.
- 5.Indian Health Service. [Accessed June 29, 2017];Loan Repayment Program. http://www.ihs.gov/loanrepayment/
- 6.Davis K, Abrams M, Stremikis K. How the Affordable Care Act will strengthen the nation’s primary care foundation. J Gen Intern Med. 2011;26(10):1201–3. doi: 10.1007/s11606-011-1720-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. [Accessed June 29, 2017];Health Care and Education Reconciliation Act of 2010, 42 USC §1305. Public Law 111–152. 2010 Mar 30; https://www.gpo.gov/fdsys/pkg/PLAW-111publ152/pdf/PLAW-111publ152.pdf.
- 8.Goodfellow A, Ulloa JG, Dowling PT, Talamantes E, Chheda S, Bone C, Moreno G. Predictors of primary care physician practice location in underserved urban or rural areas in the United States: A systematic literature review. Acad Med. 2016;91(9):1313–21. doi: 10.1097/ACM.0000000000001203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lipkin M, Zabar SR, Kalet AL, Laponis R, Kachur E, Anderson M, Gillespie CC. Two decades of Title VII support of a primary care residency: Process and outcomes. Acad Med. 2008;83(11):1064–70. doi: 10.1097/ACM.0b013e31818928ab. [DOI] [PubMed] [Google Scholar]
- 10.Pathman DE, Konrad TR, King TS, Taylor DH, Jr, Koch GG. Outcomes of states’ scholarship, loan repayment, and related programs for physicians. Med Care. 2004;42(6):560–8. doi: 10.1097/01.mlr.0000128003.81622.ef. [DOI] [PubMed] [Google Scholar]
- 11.MacDowell M, Glasser M, Fitts M, Nielsen K, Hunsaker M. A national view of rural health workforce issues in the USA. Rural Remote Health. 2010;10(3):1531. [PMC free article] [PubMed] [Google Scholar]
- 12.Williams TE, Jr, Satiani B, Ellison EC. A comparison of future recruitment needs in urban and rural hospitals: The rural imperative. Surgery. 2011;150(4):617–25. doi: 10.1016/j.surg.2011.07.047. [DOI] [PubMed] [Google Scholar]
- 13.Stanley A, Cantor JC, Guarnaccia P. Holes in the safety net: A case study of access to prescription drugs and specialty care. J Urban Health. 2008;85(4):555–571. doi: 10.1007/s11524-008-9282-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mayer M. Disparities in geographic access to pediatric subspecialty care. Matern Child Health J. 2008;12:624–632. doi: 10.1007/s10995-007-0275-3. [DOI] [PubMed] [Google Scholar]
- 15.Cook NL, Hicks LS, O’Malley AJ, Keegan T, Guadagnoli E, Landon BE. Access to specialty care and medical services in community health centers. Health Aff (Millwood) 2007;26(5):1459–68. doi: 10.1377/hlthaff.26.5.1459. [DOI] [PubMed] [Google Scholar]
- 16.Association of American Medical Colleges. 2016 Physician Specialty Data Report. Washington, DC: Association of American Medical Colleges; 2016. [Accessed July 5, 2017]. https://www.aamc.org/data/workforce/reports/457712/2016-specialty-databook.html. [Google Scholar]
- 17.Jeffe DB, Andriole DA, Hageman HL, Whelan AJ. The changing paradigm of contemporary U.S. allopathic medical school graduates’ career paths: Analysis of the 1997–2004 national AAMC Graduation Questionnaire database. Acad Med. 2007;82(9):888–94. doi: 10.1097/ACM.0b013e31812f797e. [DOI] [PubMed] [Google Scholar]
- 18.Donini-Lenhoff F, Hedrick H. Growth of specialization in graduate medical education. JAMA. 2000;284(10):1284–89. doi: 10.1001/jama.284.10.1284. [DOI] [PubMed] [Google Scholar]
- 19.Brotherton S, Etzel S. Graduate Medical Education, 2009–2010. JAMA. 2010;304(11):1255–70. doi: 10.1001/jama.2010.1273. [DOI] [PubMed] [Google Scholar]
- 20.Saha S, Guiton G, Wimmers PF, Wilkerson L. Student body racial and ethnic composition and diversity-related outcomes in US medical schools. JAMA. 2008;300(10):1135–45. doi: 10.1001/jama.300.10.1135. [DOI] [PubMed] [Google Scholar]
- 21.Komaromy M, Grumbach K, Drake M, Vranizan K, Lurie N, Keane D, Bindman AB. The role of black and Hispanic physicians in providing health care for underserved populations. N Engl J Med. 1996;334:1305–1310. doi: 10.1056/NEJM199605163342006. [DOI] [PubMed] [Google Scholar]
- 22.Xierali IM, Castillo-Page L, Conrad S, Nivet MA. Analyzing Physician workforce racial and ethnic composition associations: Geographic distribution (part II). Association of American Medical Colleges. [Accessed July 3, 2017];Analysis in Brief. 2014 14(9) https://www.aamc.org/download/401814/data/aug2014aibpart2.pdf. [Google Scholar]
- 23.Walker KO, Moreno G, Grumbach K. The association among specialty, race, ethnicity, and practice location among California physicians in diverse specialties. J Natl Med Assoc. 2012;104(1–2):46–52. doi: 10.1016/s0027-9684(15)30126-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bärnighausen T, Bloom DE. Financial incentives for return of service in underserved areas: A systematic review. BMC Health Serv Res. 2009;9:86. doi: 10.1186/1472-6963-9-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dugger RA, El-Sayed AM, Messina C, Bronson R, Galea S. The health policy attitudes of American medical students: A pilot survey. PLoS One. 2015;10(10):e0140656. doi: 10.1371/journal.pone.0140656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McDonald FS, West CP, Popkave C, Kolars JC. Educational debt and reported career plans among internal medicine residents. Ann Intern Med. 2008;149(6):416–20. doi: 10.7326/0003-4819-149-6-200809160-00008. [DOI] [PubMed] [Google Scholar]
- 27.Rosenblatt RA, Andrilla CH. The impact of U.S. medical students’ debt on their choice of primary care careers: An analysis of data from the 2002 Medical School Graduation Questionnaire. Acad Med. 2005;80(9):815–9. doi: 10.1097/00001888-200509000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Phillips JP, Petterson SM, Bazemore AW, Phillips RL. A retrospective analysis of the relationship between medical student debt and primary care practice in the United States. Ann Fam Med. 2014;12(6):542–9. doi: 10.1370/afm.1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Phillips JP, Weismantel DP, Gold KJ, Schwenk TL. Medical student debt and primary care specialty intentions. Fam Med. 2010;42(9):616–22. [PubMed] [Google Scholar]
- 30.Phillips RL, Jr, Dodoo MS, Petterson S, et al. Specialty and Geographic Distribution of the Physician Workforce: What Influences Medical Student and Resident Choices? Washington, DC: Robert Graham Center; 2009. [Google Scholar]
- 31.Andriole DA, Jeffe DB. Characteristics of medical-school matriculants who participated in postbaccalaureate-premedical programs. Acad Med. 2011;86(2):201–210. doi: 10.1097/ACM.0b013e3182045076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grbic D, Slapar F. Changes in medical students’ intentions to serve the underserved: Matriculation to graduation. Association of American Medical Colleges. [Accessed July 3, 2017];Analysis in Brief. 2010 9(8) https://www.aamc.org/download/137518/data/aib_vol9_no8.pdf. [Google Scholar]
- 33.Association of American Medical Colleges. [Accessed June 29, 2017];Underrepresented in Medicine Definition. https://www.aamc.org/initiatives/urm/
- 34.Walker KO, Ryan G, Ramey R, et al. Recruiting and retaining primary care physicians in urban underserved communities: The importance of having a mission to serve. Am J Public Health. 2010;100(11):2168–2175. doi: 10.2105/AJPH.2009.181669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Indian Health Service. 2011 Survey of physician practice patterns & satisfaction: A survey examining the practice characteristics, morale levels, and recruiting needs of Indian health program physicians. Rockville, MD: Indian Health Service; 2011. [Google Scholar]
- 36.National Health Service Corps. NHSC Clinician Retention: A Story of Dedication and Commitment. Washington, DC: U.S. Department of Health and Human Services, Health Resources and Services Administration; 2012. [Google Scholar]
- 37.Office of Management and Budget. Budget of the U.S. Government: A New Foundation for American Greatness: Fiscal Year 2018. Washington, DC: U.S. Government Printing Office; 2017. [Accessed July 5, 2017]. https://www.whitehouse.gov/sites/whitehouse.gov/files/omb/budget/fy2018/budget.pdf. [Google Scholar]
- 38.Friedman AB, Grischkan JA, Dorsey ER, George BP. Forgiven but not relieved: US physician workforce consequences of changes to public service loan forgiveness. J Gen Intern Med. 2016;31(10):1237–41. doi: 10.1007/s11606-016-3767-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Association of American Medical Colleges. [Accessed June 29, 2017];Faculty Roster. U.S. Medical School Faculty, 2014. Table 3: Rank and Race/Ethnicity. https://www.aamc.org/data/facultyroster/reports/420598/usmsf14.html.
- 40.Yu PT, Parsa PV, Hassanein O, Rogers SO, Chang DC. Minorities struggle to advance in academic medicine: A 12-y review of diversity at the highest levels of America’s teaching institutions. J Surg Res. 2013;182(2):212–8. doi: 10.1016/j.jss.2012.06.049. [DOI] [PubMed] [Google Scholar]
- 41.Rodríguez JE, Campbell KM, Pololi LH. Addressing disparities in academic medicine: What of the minority tax? BMC Med Educ. 2015;15:6. doi: 10.1186/s12909-015-0290-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Association of American Medical Colleges. [Accessed July 5, 2017];Table B-2: Total Graduates by U.S. medical school, sex, and year. https://www.aamc.org/data/facts/enrollmentgraduate/148670/total-grads-by-school-gender.html.