Abstract
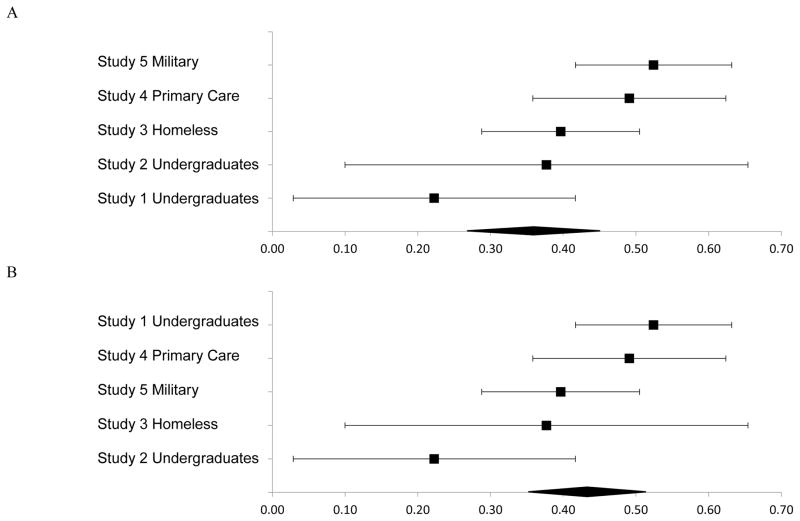
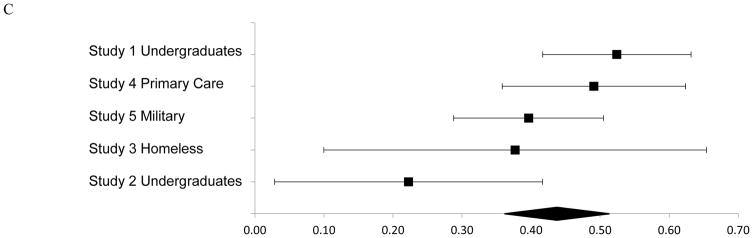
Perceived social problem-solving deficits are associated with suicide risk; however, little research has examined the mechanisms underlying this relationship. The interpersonal theory of suicide proposes two mechanisms in the pathogenesis of suicidal desire: intractable feelings of thwarted belongingness (TB) and perceived burdensomeness (PB). This study tested whether TB and PB serve as explanatory links in the relationship between perceived social problem-solving (SPS) deficits and suicide-related behaviors cross-sectionally and longitudinally. The specificity of TB and PB was evaluated by testing depression as a rival mediator. Self-report measures of perceived SPS deficits, TB, PB, suicidal ideation, and depression were administered in five adult samples: 336 and 105 undergraduates from two universities, 53 homeless individuals, 222 primary care patients, and 329 military members. Bias-corrected bootstrap mediation and meta-analyses were conducted to examine the magnitude of the direct and indirect effects, and the proposed mediation paths were tested using zero-inflated negative binomial regressions. TB and PB were significant parallel mediators of the relationship between perceived SPS deficits and ideation cross-sectionally, beyond depression. Longitudinally and beyond depression, in one study, both TB and PB emerged as significant explanatory factors, and in the other, only PB was a significant mediator. Findings supported the specificity of TB and PB: depression and SPS deficits were not significant mediators. The relationship between perceived SPS deficits and ideation was explained by interpersonal theory variables, particularly PB. Findings support a novel application of the interpersonal theory, and bolster a growing compendium of literature implicating perceived SPS deficits in suicide risk.
Keywords: problem solving, perceived burdensomeness, thwarted belongingness, suicidal ideation, interpersonal theory of suicide
Suicide is a leading cause of death in the United States (U.S.; CDC, 2015) and it is estimated that suicidal ideation, plans, and attempts occur at even greater rates. For instance, in 2013, an estimated 9.3 million adults (3.9% of the U.S. population) thought about suicide, 1.3 million attempted suicide, and 41,149 died by suicide (CDC, 2015). In order to improve suicide prevention strategies and treatments, it is important to better understand modifiable factors that predict risk, and the mechanisms that may be driving their relationship with suicide risk.
Social problem-solving deficits, or difficulties identifying problems and generating appropriate solutions, is one of the most robust cognitive risk factors associated with suicide-related behaviors (c.f. cognitive rigidity; D’Zurilla & Nezu, 1982, 1990; Rudd, Rajab, & Dahm, 1994; Shneidman, 1957). Deficits in social problem-solving ability may be characterized by a negative problem orientation (viewing problems as threats, doubting problem-solving abilities, tendency to be frustrated when facing problems), an impulsive/careless style (attempting to solve problems hurriedly or not in a thorough manner), and/or an avoidant style (passivity, inaction, procrastination, overdependence on others). Indeed, social problem-solving deficits have been consistently identified as a suicide risk factor across various demographic groups (McAuliffe et al., 2006; McLaughlin, Miller, & Warwick, 1996; Pollock & Williams, 2004; Roskar, Bucik, & Valentin, 2007; Speckens & Hawton, 2005). For example, Pollock and Williams (2004) and Linehan and colleagues (1987) both found that suicide attempters demonstrated greater passivity in their problem-solving approach in comparison to non-suicidal psychiatric inpatients, consistent with an avoidant problem-solving style. In another study of suicide attempters’ problem-solving approach, higher rates of impulsivity and carelessness, and a tendency to adopt a negative outlook on problems were found (Ghahramanlou-Holloway, Bhar, Brown, Olsen, & Beck, 2012). Across twenty-two studies examining social problem-solving deficits among suicide attempters, ideators, and non-suicidal controls, social problem-solving deficits were consistently found in attempters, including the inability to generate multiple solutions and tendency to view problems as threats to well-being (Speckens & Hawton, 2005). Conversely, enhanced problem-solving abilities have been associated with decreased suicide risk (e.g., Hirsch, Chang, & Jeglic, 2012). Of particular import, treatments targeting problem-solving abilities have been demonstrated to decrease suicide risk among individuals with a history of suicide attempts (e.g., Cognitive Therapy, Ghahramanlou-Holloway et al., 2012; Problem-Solving Therapy, Stewart, Quinn, Plever, & Brett, 2009). Although converging evidence suggests that general social problem-solving deficits are important suicide-related correlates, little research has examined the mechanisms underlying their relationship.
Research investigating potential underlying mechanisms has implicated nonspecific autobiographical memory recall in the link between social problem-solving deficits and suicide risk (Evans, Williams, O’Loughlin, & Howells, 1992). However, findings are mixed, with some studies failing to find support for memory deficits as the explanatory factor (Kremers, Spinhoven, Van der Does, & Van Dyck, 2006). Others have proposed that depressive symptoms explain this association (Reinecke et al., 2001); however, here too, findings have been inconclusive. Some studies have reported null mediation findings (e.g., Harrington et al., 2000), and one review noted that most studies only entered depression as a covariate and did not test for mediation (Speckens & Hawton, 2005). Thus, the mechanisms underlying the relationship between social problem-solving deficits and suicide risk have yet to be fully established.
One theory that may illuminate the link between these variables is the interpersonal theory of suicide (Joiner, 2005; Van Orden et al., 2010). Building on early theories of social needs (Baumeister & Leary, 1995), the interpersonal theory proposes that individuals desire suicide when they simultaneously experience intractable feelings of perceived burdensomeness (i.e., belief that one’s life places a burden on family, friends, and/or society) and thwarted belongingness (i.e., feeling that one is disconnected from others). Further, this theory proposes that those who die by suicide not only desire suicide, but also possess the capability for suicide (i.e., increased pain tolerance and fearlessness about death). Core predictions of the interpersonal theory have been supported across a variety of populations (Christensen, Batterham, Soubelet, & Mackinnon, 2012; Chu et al., under review; Cukrowicz, Jahn, Graham, Poindexter, & William, 2013; Hagan, Podlogar, Chu, & Joiner, 2015; Silva et al., 2016; Stanley, Hom, Rogers, Hagan, & Joiner, 2016). Although a systematic review that did not include a meta-analytic component found that some theory predictions have remained heretofore untested (e.g., the role of hopelessness about the tractability of thwarted belongingness and perceived burdensomeness; Ma, Batterham, Calear, & Han, 2016), a more recent meta-analysis conducted by Chu and colleagues (under review) found support for the interpersonal theory propositions, albeit effect sizes were small. Indeed, both Ma et al. (2016) and Chu et al. (under review) suggest that more research on the theory is needed—a call to which the present study responds. Given that the interpersonal theory posits that thwarted belongingness and perceived burdensomeness are proximal predictors of suicidal desire, it is possible that thwarted belongingness and perceived burdensomeness explain the relationship between social problem-solving deficits, a distal suicide risk factor, and suicide risk.
Although no studies have directly examined the relationship between social problem-solving deficits and thwarted belongingness and perceived burdensomeness, researchers have long established the importance of successful interpersonal functioning in psychological well-being (Baumeister & Leary, 1995; Deci & Ryan, 2012). Indeed, there has been research linking greater levels of social problem-solving ability with successful interpersonal functioning. This is not surprising as those who are able to adaptively cope with interpersonal challenges may also have greater social confidence and skills, and consequently, develop and maintain a stronger social support network (D’Zurilla & Nezu, 2010; D’Zurilla, Nezu, & Maydeu-Olivares, 2002; Lui, Lee, Greenwood, & Ross, 2012). These individuals may be more likely to rely on their social network in times of distress, which may mitigate feelings of thwarted belongingness and further ameliorate suicide risk. Those who do not actively pursue solutions may not engage social support networks appropriately or fear being rebuffed (Chao, 2011; Friedman, 2006; Jakupcak et al., 2014), which could contribute to an increased sense of isolation from others.
Further, effective interpersonal functioning and stronger bonds with others may increase feelings that one is valued, an integral part of society, and not a burden on others. Indeed, research on social role valorization highlights the negative impact of being devalued by society, including being cast into a negative social role and as a burden on society (Wolfensberger, 2000). Additionally, researchers have found that the ability to solve problems and manage daily stressors may result in increased feelings of self-efficacy and a reduced perception of being a burden on others (Marks, Allegrante, & Lorig, 2005; Robinson-Smith, Johnston, & Allen, 2000). As noted above, those who do not pursue solutions may fear negative social consequences, such as criticisms from others, which may contribute to increased perceptions of burdensomeness on others. These findings suggest that the ability to problem solve effectively may diminish perceived burdensomeness and, in turn, suicide risk.
Altogether, results suggest that conversely, individuals with perceived deficits in social problem-solving ability (i.e., passivity and impulsivity, a negative mindset when facing problems) may be less interpersonally effective, which could lead to greater interpersonal conflict, decreased social connection, and increased feelings of thwarted belongingness. Additionally, an ineffective problem-solving approach may diminish feelings of self-efficacy and social value, thereby increasing feelings of perceived burdensomeness.
Present Study
Although social problem-solving deficits have been linked to interpersonal difficulties and suicide risk, there is a paucity of information on how thwarted interpersonal needs may explain these associations from the perspective of the interpersonal theory. This manuscript addresses this gap in the literature by examining the mediating roles of thwarted belongingness and perceived burdensomeness in the relationship between perceived social problem-solving deficits and suicidal ideation in five different samples. As research has indicated that perceived burdensomeness may be a more robust predictor of suicidal ideation than thwarted belongingness cross-sectionally (e.g., Bryan et al., 2010; Chu et al., 2016a) and prospectively (Chu et al., 2016c), we tested perceived burdensomeness and thwarted belongingness as both parallel and individual mediators of the relationship between perceived social problem-solving deficits and ideation. We hypothesized that perceived problem-solving deficits would be positively associated with thwarted belongingness, perceived burdensomeness, and suicidal ideation, and thwarted belongingness and perceived burdensomeness would mediate the relationship between perceived social problem-solving deficits and ideation. Specifically, perceived social problem-solving deficits would emerge as a distal suicide risk factor and the interpersonal theory variables would be proximal risk factors (Figure 1).
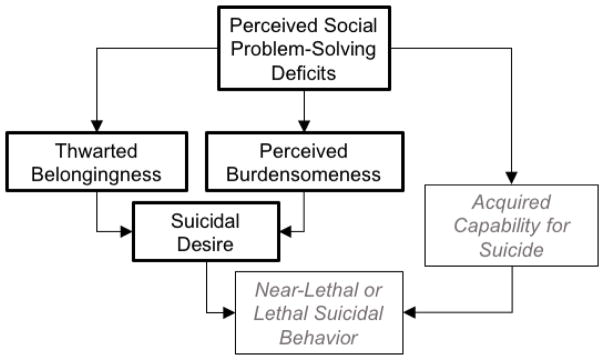
Figure 1.
Hypothesized explanatory model for the association between perceived social problem-solving deficits and near-lethal or lethal suicidal behavior from the perspective of the Interpersonal Theory of Suicide (Joiner, 2005). Constructs denoted in gray were not specifically evaluated in this study.
To strengthen findings, we evaluated the specificity of the two proposed mediators. First, we examined whether perceived social problem-solving deficits (independent variable) and thwarted belongingness and perceived burdensomeness (mediators) were interchangeable in their roles. We predicted that perceived social problem-solving deficits would not mediate the relationship between the interpersonal theory variables and ideation. Next, we tested an alternative explanatory mechanism—depressive symptoms—that has been linked to both social problem-solving deficits and suicidal symptoms (Speckens & Hawton, 2005). We postulated that depressive symptoms would not account for their relationship, which supports the robustness of our two proposed mediators. Additionally, in Studies 1, 2, and 5 where the suicide-related dependent variable demonstrated excess zeroes, we examined the proposed mediation pathways using zero inflated negative binomial regressions; we expected that the pattern of findings would remain the same even after accounting for excess zeroes. Finally, we conducted meta-analyses to examine the strength of the direct and indirect relationships between these variables across the five studies. For brevity and clarity, in all study methods and results, we refer to thwarted belongingness and perceived burdensomeness as TB and PB, respectively.
The Institutional Review Board (IRB) at East Tennessee State University approved the study procedures for Study 1 (“ETSU PEAKS: Local Baseline Evaluation,” protocol #: c0210.26e-ETSU), Study 3 (“Characterization of Rural, Middle, and Older Adult Primary Care Patients with Chronic Medical Problems,” protocol #: 08-222s), and Study 4 (“Characterization of Rural, Middle, and Older Adult Primary Care Patients with Chronic Medical Problems,” protocol #: 08-222s). Study 2 was approved by the IRB at Florida State University (“Memory Perspective & Mental Rehearsal: Role of Cognitions in Suicidal Behavior,” protocol #: 2013.10048). Study 5 was approved by the IRB of Texas A&M University (IRB title and protocol # not available) and the USAMRMC (Human Research Protection Office).
Study 1: Undergraduate Students
First, we examined the relationship between perceived social problem-solving deficits and suicidal symptoms through the pathways of thwarted belongingness and perceived burdensomeness in an undergraduate student sample. We predicted that thwarted belongingness and perceived burdensomeness would significantly account for the relationship between perceived social problem-solving deficits and suicide risk.1
Study 1 Method
Participants
Participants were 336 undergraduates attending a large university located in the Southeastern U.S. (participant details in Table 1).
Table 1.
Participant Demographic Information for All Studies (N, %).
| Variables | Study 1 (N=336) | Study 2 (N=105) | Study 3 (N=53) | Study 4 (N=222) | Study 5 (N=329) |
|---|---|---|---|---|---|
| Undergraduates | Undergraduates | Homeless Individuals | Primary Care Patients | Service Members | |
| Age Mean (SD) | 21.8 (5.3) years | 19.3 (2.5) years | 49.0 (11.6) years | 44.1 (12.4) years | 22.2 (2.8) years |
| Age Range | 17–58 years | 18–35 years | 23–69 years | 19–79 years | 18–37 years |
| Female | 225, 66.6% | 70, 65.4% | 16, 30.2% | 137, 61.7% | 56, 17.0% |
|
| |||||
| Ethnicity and Race | |||||
|
| |||||
| Hispanic/Latino | 6, 1.8% | 82, 76.6% | 2, 3.8% | 7, 3.2% | 35, 10.6% |
| Caucasian/White | 294, 87.5% | 86, 80.4% | 39, 73.6% | 193, 86.9% | 200, 60.8% |
| African American/Black | 18, 5.41% | 8, 7.5% | 8, 15.1% | 16, 7.2% | 84, 25.5% |
| Asian/Pacific Islander | 10, 3.0% | 6, 5.6% | 0, 0% | 1, 0.5% | 5, 1.5% |
| American Indian/Alaskan Native | n/a | 1, 0.9% | 3, 5.7% | 2, 0.9% | 4, 1.2% |
| Other | n/a | 3, 2.9% | n/a | n/a | 1, 0.3% |
| Missing | 8, 2.4% | 1, 0.9% | 1, 1.9% | 3, 1.4% | n/a |
|
| |||||
| Suicidal Symptom History | |||||
|
| |||||
| Lifetime Suicidal Ideation | 50, 14.8% | 14, 13.1% | 11, 20.8% | 123, 55.4% | 132, 40.1% |
| No History of Suicide Attempts | 304, 90.5% | 88, 83.8% | 44, 83.0% | 181, 81.5% | 162, 49.2% |
| Lifetime Suicide Attempt | 22, 6.6% | 17, 15.9% | 9, 17.0% | 41, 18.5% | 167, 50.8% |
| 1 Previous Attempt | 11, 3.3% | 10, 9.5% | n/a | n/a | 103, 31.3% |
| 2+ Previous Attempts | 11, 3.3% | 7, 6.7% | n/a | n/a | 64, 19.5% |
| Missing | 10, 3.0% | n/a | n/a | n/a | n/a |
Note. N/A = data were not available.
Procedure
All participants provided electronic informed consent prior to initiating study procedures, which involved completing an online battery of questionnaires, and were compensated with course credit. Participants received a debriefing form that included mental health resources. Study 1 data have been previously used to investigate the relationship between suicide risk and traumatic events (Chang & Hirsch, 2015; Chang et al., 2017a; 2017b; 2015c), and risk factors for depression (Chang et al., 2015a; 2015b; Muyan et al., 2015).
Measures
Suicide Risk
The Suicidal Behaviors Questionnaire-Revised (SBQ-R; Osman et al., 2001) is a 4-item measure of suicidal behaviors including lifetime history of ideation and future likelihood of suicidal behavior. Each question is scored on a 7-point Likert-type scale ranging from 1 to 7. Items were summed for a total score and higher scores indicated higher frequency or severity of risk. Total scores ranged from 3 to 18; however, for zero inflated models, the suicide risk total score was adjusted by subtracting 3 points from all scores in order to obtain a low-end zero score. This measure has demonstrated good internal consistency across samples, including college undergraduates and adult psychiatric inpatients (0.76–0.88), and adequate discriminant validity when discriminating suicidal versus non-suicidal inpatients (standardized estimate=0.79; Osman et al., 2001). In this study, internal consistency was good (α=0.81).
Perceived social problem-solving ability
The Social Problem-Solving Inventory-Revised-Short Form (SPSI-R-SF; D’Zurilla et al., 2002) was used to assess perceived social problem-solving deficits. This 25-item questionnaire is scored using a 5-point Likert-type scale ranging from 0 to 4. The SPSI-R-SF assesses two constructive or adaptive social problem-solving dimensions and three dysfunctional dimensions, yielding a total score and five subscales scores (positive problem orientation, rational problem solving, negative problem orientation, impulsive/careless style, and avoidant style; D’Zurilla et al., 2002). Low scores on positive dimensions and high scores on negative dimensions indicate greater deficits in social problem-solving ability. The five-factor structure of the SPSI-R-SF has been validated (CFI=0.91; D’Zurilla et al., 2002; Maydeu-Olivares & D’Zurilla, 1997). Across collegiate, clinical, and community samples (D’Zurilla et al., 2002; Hawkins, Sofronoff, & Sheffield, 2009; Morera et al., 2006; Nezu, Nezu, & Perri, 1989; Spence, Sheffield, & Donovan, 2002), the SPSI-R-SF has demonstrated good internal consistency (α=0.73–0.79), and test-retest reliability over three weeks (r=0.91). Given the focus of this study on general problem-solving deficits as distal suicide risk factors, we used the SPSI-R-SF total score, which was calculated by reverse-scoring the positive items and summing all negative and reverse-scored positive items. Thus, higher total scores are indicative of greater perceived social problem-solving deficits. Internal consistency was excellent (α=0.92).
Thwarted belongingness, perceived burdensomeness
The Interpersonal Needs Questionnaire-18 (INQ-18; Van Orden, Cukrowicz, Witte, & Joiner, 2012) was used to assess TB and PB. Items are rated on a 7-point Likert scale ranging from 1 to 7 (Van Orden et al., 2012). The 9-item TB subscale (INQ-TB) measures the extent to which the individual feels connected to other people, and the 9-item PB subscale (INQ-PB) assesses perceptions that one is a burden on others. Each subscale score ranges from 9 to 63. Where indicated, items were reverse scored; higher scores indicate greater severity. In this study, the PB and TB scales both exhibited excellent internal consistency (both αs=0.92).
Rival mediator
A comprehensive measure of depression symptoms was not available in this sample (a point that we discuss below and remedy in Study 2); however, the National College Health Association Measure (NCHA, Original Version; American College Health Association, 2009) is a 123-item measure of physical and mental health-related activities and behaviors, and each item was designed to be used individually. In this study, one item assessing depressive symptoms (i.e., impacting academic functioning) in the preceding year was used.
Statistical analyses
First, variables of interested were evaluated descriptively and Pearson correlation coefficients (r) were generated to examine between-variable associations. Prior to conducting primary analyses, data across all samples were screened for outliers and violations of normality. In Study 1, two variables evidenced potentially problematic levels of skew and kurtosis (SBQ-R total, INQ-TB); therefore, robust Maximum Likelihood (MLR) was selected as the estimation method for our analyses. Full information maximum likelihood estimation (FIML) maximizes the likelihood of the model given the data and assumes multivariate normality. Thus, FIML was used to handle missing data. When data are non-normal, FIML can be used (with MLR) to obtain standard errors and test statistics robust to non-normality (Brown, 2006).
Structural equation analyses using MPlus 7 were used to the test the following models: (A) TB and PB (INQ) as parallel mediators of the relationship between perceived social problem-solving deficits (SPSI-SF-R) and suicide risk (SBQ-R), controlling for depressive symptoms; (B) TB as an individual mediator of the relationship between perceived social problem-solving deficits and suicide risk, controlling for depressive symptoms; (C) PB as an individual mediator of the relationship between perceived social problem-solving deficits and suicide risk, controlling for depressive symptoms; (D) perceived social problem-solving deficits as the mediator of the association between TB and PB and suicidal ideation, controlling for depressive symptoms; and (E) depressive symptoms as the mediator of the relationship between perceived social problem-solving deficits and suicide risk, controlling for TB and PB. Previous research has shown age and sex differences in suicide risk (Beautrais, 2001; Van Orden et al., 2010); therefore, age and sex were covaried in all models.
In all five mediation models, 10,000 bootstrapped samples were drawn from the data, and bias-corrected 95% confidence intervals were used to estimate the indirect effects of each of the resampled datasets. This statistical approach estimates path coefficients and generates bootstrapped confidence intervals for total and specific indirect effects of X on Y through one or more mediator variable(s) M, while adjusting all paths for the potential influence of covariates not proposed as mediators in the model. If a true zero falls between the upper and lower confidence intervals, there is no significant indirect effect of the mediators.
In line with recommendations from Brown (2006) and Hu and Bentler (1999), several indices were used to evaluate model fit. The chi-square statistic (χ2) and the standardized root mean square residual (SRMR), were used as indices of absolute fit, with non-significance of χ2 indicating perfect fit and SRMR values less than 0.10 indicating adequate fit and less than 0.08 indicating good fit. The Root Mean Square Error of Approximation (RMSEA) is a parsimony-corrected fit statistic and RMSEA values less than 0.05 are interpreted as good fit and values between 0.06 and 0.08 indicate adequate fit. The Comparative Fit Index (CFI) and Tucker-Lewis Index (TLI) were used as indices of comparative fit, with CFI and TLI values between .90 and .95 indicating adequate model fit.
Finally, given prior research highlighting the need for tests of zero inflation in suicide-related research in non-clinical samples (Cukrowicz et al., 2013), we examined our suicide-related outcome variables for excess zeroes. Inspection of the histogram for our outcome variable, suicide risk, indicated relatively large numbers of zero-value responses as a proportion of the total Study 1 sample size (SBQ-R = 197/336). Thus, consistent with Cukrowciz et al. (2013), zero-inflated models were employed as these models allow for simultaneous estimation of both the zero and positive responses in the data (Greene, 2012). Due to the combination of overdispersion and excess zeros in the data, ZINB regressions were conducted using Stata 13 to confirm the α, β, c, and c’ pathways of our proposed mediator models (see Figure 2). Vuong’s test (Vuong, 1989) was employed to verify the utility of the ZINB model by evaluating the ZINB regression against the standard negative binomial regression (Atkins & Gallop, 2007); statistical significance of Vuong’s test supports the ZINB model.
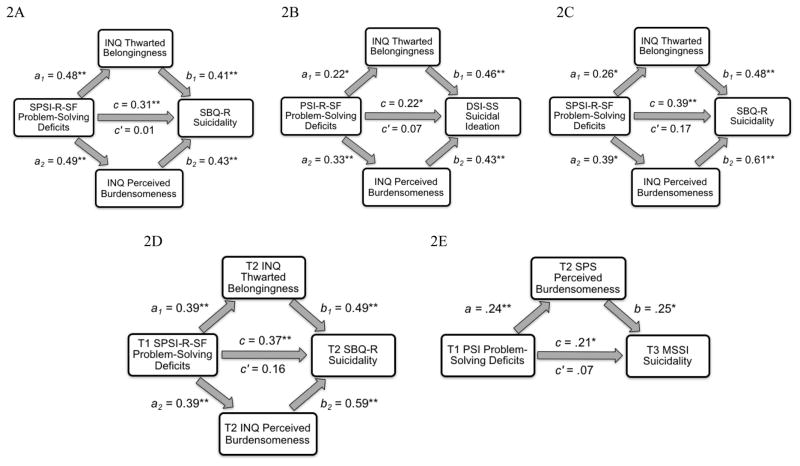
Figure 2.
Standardized regression coefficients for the cross-sectional relationship between deficits in problem-solving ability and suicidal ideation as mediated by thwarted interpersonal needs in Study 1 (2A), Study 2 (2B), Study 3 (2C), Study 4 (2D; T1 = Time 1, baseline. T2 = Time 2, 6–12 months after baseline), and Study 5 (2E; T1 = Time 1, baseline. T2 = Time 2, 1 month after baseline. T3 = Time 3, 6 months after baseline).
Note. * p < 0.05; ** p < 0.001. SPSI = Social Problem-Solving Inventory. INQ = Interpersonal Needs Questionnaire. SBQ-R = Suicidal Behavior Questionnaire-Revised. PSI-R-SF = Problem-Solving Inventory-Revised-Short Form. DSI-SS = Depressive Symptom Inventory – Suicidality Subscale. SBQ-R = Suicidal Behavior Questionnaire-Revised.
Power
With regard to power, previous research has indicated that a sample size of 53 is required to be adequately powered (0.80) to detect moderate effect sizes for the α path and large effect sizes for the β path using a bias-corrected bootstrap mediation approach (Fritz & MacKinnon, 2007). Thus, with our sample size of 336, we were adequately powered for mediation analyses. Additionally, based on Monte Carlo simulations (Wolf, Harrington, Clark, & Miller, 2013), there was sufficient power to evaluate model fit indices in Study 1.
Study 1 Results
Preliminary Analyses
Means, standard deviations, and correlations between all Study 1 variables are in Table 2. As hypothesized, deficits in perceived social problem-solving deficits were significantly and positively related to TB, PB, and suicide risk (r=0.32–0.49, ps<0.001).
Table 2.
All Study Variable Means, Standard Deviations and Correlations.
| Study 1 – Undergraduates | 1. | 2. | 3. | 4. | -- | -- | N | Mean | SD | Range | Skew |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. INQ-18 Thwarted Belongingness | -- | 334 | 24.34 | 11.80 | 9–57 | 0.41 | |||||
| 2. INQ-18 Perceived Burdensomeness | 0.781** | -- | 334 | 20.24 | 10.95 | 9–61 | 0.90 | ||||
| 3. SBQ-R Suicide Risk | 0.406** | 0.433** | -- | 336 | 4.74 | 2.73 | 3–14 | 1.58 | |||
| 4. SPSI-R Social Problem-Solving Deficits | 0.481** | 0.488** | 0.319** | -- | 334 | 31.13 | 13.30 | 4–78 | 0.37 | ||
|
| |||||||||||
| Study 2 – Undergraduates | 1. | 2. | 3. | 4. | -- | -- | N | Mean | SD | Range | Skew |
|
| |||||||||||
| 1. INQ-15 Thwarted Belongingness | -- | 105 | 21.37 | 11.21 | 9–59 | 1.19 | |||||
| 2. INQ-15 Perceived Burdensomeness | 0.467** | -- | 105 | 8.41 | 4.69 | 6–32 | 1.45 | ||||
| 3. DSI-SS Suicidal Ideation | 0.457** | 0.431** | -- | 105 | 0.39 | 1.03 | 0–5 | 2.21 | |||
| 4. PSI-R-SF Social Problem-Solving Deficits | 0.219* | 0.330** | 0.221* | -- | 105 | 41.74 | 12.31 | 16–84 | 0.97 | ||
|
| |||||||||||
| Study 3 – Homeless Individuals | 1. | 2. | 3. | 4. | -- | -- | N | Mean | SD | Range | Skew |
|
| |||||||||||
| 1. INQ-15 Thwarted Belongingness | -- | 53 | 36.09 | 13.40 | 9–63 | −0.18 | |||||
| 2. INQ-15 Perceived Burdensomeness | 0.539** | -- | 53 | 15.98 | 9.97 | 5–42 | 0.90 | ||||
| 3. SBQ-R Suicide Risk | 0.476** | 0.612** | -- | 53 | 7.32 | 4.00 | 3–16 | 0.65 | |||
| 4. SPSI-R Social Problem-Solving Deficits | 0.360* | 0.391* | 0.391* | -- | 53 | 37.36 | 17.43 | 4–80 | 0.12 | ||
|
| |||||||||||
| Study 4 – Primary Care Patients | 1. | 2. | 3. | 4. | 5. | 6. | N | Mean | SD | Range | Skew |
|
| |||||||||||
| 1. T1 INQ-15 Thwarted Belongingness | -- | 216 | 31.24 | 14.00 | 9–63 | 0.06 | |||||
| 2. T1 INQ-15 Perceived Burdensomeness | 0.634** | -- | 222 | 15.86 | 10.67 | 6–42 | 0.91 | ||||
| 3. T1 SBQ-R Suicide Risk | 0.519** | 0.614** | -- | 217 | 6.25 | 3.66 | 3–18 | 1.01 | |||
| 4. T2 INQ-15 Thwarted Belongingness | 0.525** | 0.480** | 0.472** | -- | 98 | 27.17 | 13.44 | 9–57 | 0.43 | ||
| 5. T2 INQ-15 Perceived Burdensomeness | 0.411** | 0.593** | 0.480** | 0.701** | -- | 99 | 14.15 | 10.39 | 6–42 | 1.28 | |
| 6. T2 SBQ-R Suicide Risk | 0.465** | 0.556** | 0.755** | 0.487** | 0.586** | -- | 99 | 5.98 | 3.61 | 3–18 | 1.22 |
| 7. T1 SPSI-R Social Problem-Solving Deficits | 0.455** | 0.479** | 0.381** | 0.392** | 0.392** | 0.365** | 221 | 34.90 | 18.39 | 1–96 | 0.66 |
|
| |||||||||||
| Study 5 – Military Service Members | 1. | 2. | 3. | 4. | 5. | 6. | N | Mean | SD | Range | Skew |
|
| |||||||||||
| 1. T1 SPS Thwarted Belongingness | -- | 329 | 11.72 | 4.50 | 3–21 | −0.04 | |||||
| 2. T1 SPS Perceived Burdensomeness | 0.711** | -- | 329 | 8.44 | 3.48 | 4–16 | 0.33 | ||||
| 3. T1 MSSI Suicidal Ideation | 0.423** | 0.521** | -- | 329 | 23.39 | 10.32 | 0–51 | −0.22 | |||
| 4. T2 SPS Thwarted Belongingness | 0.427** | 0.325** | 0.282** | -- | 251 | 9.35 | 4.06 | 3–21 | 0.40 | ||
| 5. T2 SPS Perceived Burdensomeness | 0.255** | 0.399** | 0.313** | 0.652** | -- | 251 | 6.80 | 2.82 | 3–16 | 0.95 | |
| 6. T3 MSSI Suicidal Ideation | 0.156* | 0.173* | 0.239** | 0.262** | 0.245* | -- | 139 | 3.78 | 8.37 | 0–40 | 1.29 |
| 7. T1 PSI Social Problem-Solving Deficits | 0.377** | 0.471** | 0.369** | 0.198* | 0.237** | 0.214* | 308 | 108.32 | 25.39 | 35–175 | −0.15 |
Note.
p < 0.05;
p ≤ 0.001.
INQ = Interpersonal Needs Questionnaire. SBQ-R = Suicidal Behavior Questionnaire – Revised. DSI-SS = Depressive Symptom Inventory- Suicidality Subscale. PSI-R-SF = Problem Solving Inventory-Revised-Short-Form. SPSI-R = Social Problem Solving Inventory-Revised. SPS = Suicide Probability Scale. MSSI = Modified Scale for Suicidal Ideation. PSI = Problem Solving Inventory. Study 4: T1 = Time 1. T2 = Time 2, 6 months after T1. Study 5: T2 = Time 2, 1 month after T1. T3 = Time 3, 6 months after T1.
TB and PB as Parallel Mediators
We examined TB and PB as parallel mediators of the relationship between perceived social problem-solving deficits and suicide risk, controlling for age and sex. This model demonstrated excellent model fit (χ2(1) = 0.005, p = 0.94; RMSEA (90%CI) = 0.01 (0.01, 0.03), CFI/TLI = 0.99, 0.96; SRMR = 0.01). All α and β pathways in the mediation model were significant. The direct effect of perceived social problem-solving deficits on suicide risk was not significant after accounting for TB and PB, indicating mediation. The indirect effect of TB and PB on the relationship between perceived social problem-solving deficits and suicide risk, controlling for age and sex, was estimated to be between 0.0287 and 0.0648, indicating significance as the 95% confidence interval did not cross zero. The pattern of findings remained the same after controlling for depressive symptoms with the overall regression model explaining a significant amount of variance in suicide risk (R2=0.26, b=0.040, SE=0.01, 95%CI=0.0244, 0.0567; Figure 2A; see Table 3 for details).
Table 3.
Summary of the Main Results for Models in All Studies.
| Study 1 – Undergraduates | SPS->TB | TB->SI | SPS->PB | PB->SI | Direct Effect | Indirect Effect | 95%CI | |
|---|---|---|---|---|---|---|---|---|
| A: Main | R2=0.26, F[6,318]=18.61*** | b=0.42***, SE=0.04 | b=0.03*, SE=0.02 | b=0.40***, SE=0.04 | b=0.07**, SE=0.02 | b=0.03, SE=0.01 | b=0.042, SE=0.008 | 0.0256, 0.0586 |
| B: TB | R2=0.24, F[5,319]=19.75*** | -- | -- | -- | -- | b=0.040**, SE=0.01 | b=0.032, SE=0.008 | 0.0183, 0.0478 |
| C: PB | R2=0.26, F[5,319]=21.94*** | -- | -- | -- | -- | b=0.040**, SE=0.01 | b=0.038, SE=0.01 | 0.0231, 0.0555 |
|
| ||||||||
| Study 2 – Undergraduates | SPS->TB | TB->SI | SPS->PB | PB->SI | Direct Effect | Indirect Effect | 95%CI | |
|
| ||||||||
| A: Main | R2=0.44, F[6,98]=12.96*** | b=0.25**, SE=0.09 | b=0.02***, SE=0.005 | b=0.13**, SE=0.04 | b=0.03**, SE=0.01 | b=0.002, SE=0.004 | b=0.026, SE=0.02 | 0.0021, 0.0073 |
| B: TB | R2=0.43, F[5,99]=14.78*** | -- | -- | -- | -- | b=0.003, SE=0.004 | b=0.006, SE=0.003 | 0.0018, 0.0125 |
| C: PB | R2=0.44, F[5,99]=15.38*** | -- | -- | -- | -- | b=0.002, SE=0.004 | b=0.007, SE=0.003 | 0.0023, 0.0159 |
|
| ||||||||
| Study 3 – Homeless Individuals | SPS->TB | TB->SI | SPS->PB | PB->SI | Direct Effect | Indirect Effect | 95%CI | |
|
| ||||||||
| A: Main | R2=0.54, F[6,46]=8.88*** | b=0.20**, SE=0.11 | b=0.06**, SE=0.04 | b=0.21**, SE=0.08 | b=0.16**, SE=0.06 | b=0.04, SE=0.03 | b=0.046, SE=0.03 | 0.0015, 0.1017 |
| B: TB | R2=0.50, F[5,47]=9.54*** | -- | -- | -- | -- | b=0.058*, SE=0.03 | b=0.0237, SE=0.02 | −0.0169, 0.0151 |
| C: PB | R2=0.53, F[5,47]=10.55*** | -- | -- | -- | -- | b=0.0387, SE=0.0275 | b=0.0433, SE=0.02 | 0.0070, 0.0936 |
|
| ||||||||
| Study 4 – Primary Care Patients | SPS->TB | TB->SI | SPS->PB | PB->SI | Direct Effect | Indirect Effect | 95%CI | |
|
| ||||||||
| A: Main | R2=0.44, F[6,182]=27.79*** | b=0.34***, SE=0.05 | b = 0.06**, SE=0.02 | b=0.25***, SE=0.04 | b=0.16***, SE=0.03 | b=0.004, SE=0.01 | b=0.0224, SE=0.0084 | 0.0093, 0.0431 |
| B: TB | R2=0.35, F[5,183]=19.99*** | -- | -- | -- | -- | b=0.0177, SE=0.01 | b=0.0084, SE=0.005 | 0.0110, 0.0204 |
| C: PB | R2=0.43, F[5,188]=27.98*** | -- | -- | -- | -- | b=0.0079, SE=0.01 | b=0.0189, SE=0.01 | 0.0068, 0.0374 |
| D: Main | R2=0.33, F[6,80]=6.61*** | b=0.28***, SE=0.07 | b=0.03**, SE=0.03 | b=0.22***, SE=0.05 | b=0.15***, SE=0.04 | b=0.001, SE=0.02 | b=0.0324, SE=0.01 | 0.0111, 0.0720 |
| E: TB | R2=0.25, F[5,81]=5.34*** | -- | -- | -- | -- | b=0.0223, SE=0.02 | b=0.0113, SE=0.0087 | 0.0003, 0.0391 |
| F: PB | R2=0.33, F[5,83]=8.07*** | -- | -- | -- | -- | b=0.0044, SE=0.02 | b=0.0298, SE=0.01 | 0.0088, 0.0629 |
|
| ||||||||
| Study 5 – Military Service Members | SPS->TB | TB->SI | SPS->PB | PB->SI | Direct Effect | Indirect Effect | 95%CI | |
|
| ||||||||
| A: Main | R2=0.36, F[6,225]=20.63*** | b=0.07***, SE=0.01 | b=0.19*, SE=0.04 | b=0.06***, SE=0.01 | b=1.22***, SE=0.20 | b=0.05, SE=0.03 | b=0.0928, SE=0.02 | 0.0676, 0.1348 |
| B: TB | R2=0.26, F[5,226]=15.75*** | -- | -- | -- | -- | b=0.0986**, SE=0.03 | b=0.0532, SE=0.01 | 0.0300, 0.0835 |
| C: PB | R2=0.35, F[5,227]=24.75*** | -- | -- | -- | -- | b=0.0525*, SE=0.03 | b=0.0971, SE=0.02 | 0.0678, 0.1335 |
| D: Main | R2=0.10, F[7,111]=1.82 | b=0.04**, SE=0.01 | b=−0.06, SE = 0.23 | b=0.02*, SE=0.01 | b=0.80*, SE=0.36 | b=0.0163, SE=0.03 | b=0.009, SE=0.01 | −0.0074, 0.0496 |
| E: TB | R2=0.06, F[6,112]=1.17 | -- | -- | -- | -- | b=0.0201, SE=0.04 | b=0.0047, SE=0.01 | −0.0035, 0.0319 |
| F: PB | R2=0.10, F[6,113]=3.34* | -- | -- | -- | -- | b=0.016, SE=0.03 | b=0.0175, SE=0.01 | 0.0047, 0.0425 |
Note.
p < 0.05;
p ≤ 0.01,
p ≤ 0.001.
SPS = perceived social problem-solving deficits. TB = thwarted belongingness. PB = perceived burdensomeness. SI = suicidal ideation.
A) Cross-Sectional Main Test: TB and PB as parallel mediators of the relationship between perceived social problem-solving ability (IV) and suicidal ideation (DV), controlling for depression, age and sex. For Study 5, results from Time 1 are presented.
B) Cross-Sectional TB Individually: TB as the mediator of the relationship between perceived social problem-solving ability (IV) and suicidal ideation (DV), controlling for depression, age and sex. For Study 5, results from Time 1 are presented.
C) Cross-Sectional PB Individually: PB as the mediator of the relationship between perceived social problem-solving ability (IV) and suicidal ideation (DV), controlling for depression, age and sex. For Study 5, results from Time 1 are presented.
D) Longitudinal Main Test: see A). Study 4 (SPS Time 1 -> TB/PB Time 2 -> SI Time 2); Study 5 (SPS Time 1 -> TB/PB Time 2 -> SI Time 3).
E) Longitudinal TB Individually: see B). Study 4 (SPS Time 1 -> TB Time 2 -> SI Time 2); Study 5 (SPS Time 1 -> TB Time 2 -> SI Time 3).
F) Longitudinal PB Individually: see C). Study 4 (SPS Time 1 -> PB Time 2 -> SI Time 2); Study 5 (SPS Time 1 -> PB Time 2 -> SI Time 3).
ZINB regression model results were consistent with hypotheses. TB (estimate = 0.049, SE = 0.009, p < 0.001, Wald χ2 = 35.60) and PB (estimate = 0.053, SE = 0.008, p < 0.001, Wald χ2 = 34.33), individually, were both significantly associated with suicide risk. The model with social problem solving deficits as a predictor of suicide risk, controlling for age and sex, was significant, with Wald χ2 equal to 18.54, p < 0.001. Social problem-solving deficits were significantly associated with suicide risk (estimate = 0.033, robust SE = 0.008, p < 0.001). When TB and PB were included into the model, the Wald χ2 value was significant (16.10, p < 0.001). However, the main effect of social problem solving deficits on suicide risk was no longer significant (estimate = 0.015, SE = 0.008, p = 0.08). While the ZINB results are consistent with our proposed pathways, Vuong’s test (Vuong, 1989) was not significant (p < 0.001), which supports the ZINB models.
Specificity of TB and PB as Mediators
Mediation analyses reversing the variables in the α path indicated that the effect of TB (β=−0.001; 95%CI=−0.003, 0.001) and PB (β=−0.001; 95%CI=−0.0029, 0.001) on suicide risk was not significantly mediated by perceived social problem-solving deficits, which supports the specificity of the roles of the independent variable (social problem-solving deficits) and the mediators (TB, PB). Depressive symptoms did not mediate the relationship between perceived social problem-solving deficits and suicide risk, controlling for TB, PB, age and sex (b=−0.004, SE=0.060; 95%CI=−0.029, 0.008).
TB and PB as Individual Mediators
When TB was tested as an individual mediator, the direct effect of perceived social problem-solving deficits on suicide risk remained significant after accounting for TB and the indirect effect of TB was significant, estimated to be between 0.0183 and 0.0478 (R2=0.0807, κ2=0.1479). The overall model was significant (R2=0.24) and the goodness-of-fit ranged from poor to excellent (χ2(1) = 1.43, p = 0.33; RMSEA (90%CI) = 0.06 (0.04, 0.09), CFI/TLI = 0.81, 0.77; SRMR = 0.07). A similar pattern emerged for PB: the direct effect of perceived social problem-solving deficits on suicide risk remained significant after accounting for PB and the indirect effect of PB was significant, estimated to be between 0.0231 and 0.0555 (R2=0.0850, κ2=0.1639). For PB as an individual mediator, the overall model was significant (R2=0.26) and goodness-of-fit ranged from good to excellent (χ2(1) = 1.05, p = 0.10; RMSEA (90%CI) = 0.05 (0.03, 0.06), CFI/TLI = 0.89, 0.90; SRMR = 0.06).
Study 1 Discussion
Study 1 tested our hypotheses in an undergraduate student sample. Our hypotheses were supported—consistent with previous research (McAuliffe et al., 2006; McLaughlin, Miller, & Warwick, 1996), greater perceived social problem-solving deficits were associated with higher levels of thwarted interpersonal needs and, in turn, more severe suicide risk. Our findings were consistent with the interpersonal theory and showed that thwarted belongingness and perceived burdensomeness were significant explanatory links. In line with these findings, the model including both thwarted belongingness and perceived burdensomeness as mediators exhibited excellent fit. Individually, thwarted belongingness and perceived burdensomeness only partially mediated the association between perceived social problem-solving deficits and suicide risk.
Consistent with prior research suggesting that perceived burdensomeness may be a stronger predictor than thwarted belongingness (e.g., Bryan et al., 2010), our findings indicated that the individual mediator model with perceived burdensomeness accounted for a similar amount of variance in suicide as the model with both mediators. Additionally, the two models with perceived burdensomeness demonstrated good to excellent fit, while the individual mediator model with thwarted belongingness exhibited poorer fit indices. These findings may indicate that the inclusion of thwarted belongingness does not significantly improve our ability to predict variance in suicide risk or that perceived burdensomeness is a more robust predictor of risk.
Of note, this pattern of results remained significant even after accounting for depression, sex and age. Prior research has demonstrated that depressive symptoms are not only robustly linked to suicide risk (Ellis & Rutherford, 2008), but also to social problem-solving deficits (Speckens & Hawton, 2005). Therefore, that our findings remained significant even after controlling for depression highlights the robustness of the interpersonal theory variables. Additionally, analyses with depression as the mediator indicated that depression did not mediate the relationship between perceived social problem-solving deficits and suicide risk, controlling for thwarted belongingness and perceived burdensomeness. Further, the proposed pathways in our mediation models were supported when analyses were conducted to account for an excess of zeroes in our suicide risk outcome variable. These findings, altogether, further bolster the specificity and robustness of our proposed hypotheses.
Study 1 had four primary limitations. First, the sample was undergraduate students who are generally high functioning; thus, results may not generalize to clinical populations. Second, by virtue of their student status, it could be that individuals in Study 1 had higher baseline levels of perceived social problem-solving deficits (e.g., navigating the social sphere of a university, including courses and living with peers). Third, data for Study 1 were cross-sectional, limiting our ability to establish temporality in the meditational pathways, although it is emphasized that reversing the independent and mediator variables did not produce a significant model. Finally, in this sample, only one item was used to measure depressive symptoms and the use of more robust measures of depression would strengthen these results. Given that this is the first study, to our knowledge, to examine this hypothesis in an undergraduate sample, replication is needed.
Study 2: Undergraduate Students
In Study 2, we sought to replicate Study 1 in a different sample of undergraduate students. As in Study 1, we hypothesized that thwarted belongingness and perceived burdensomeness would, again, emerge as significant explanatory factors.
Study 2 Method
Participants
Participants were 105 students recruited from the undergraduate psychology subject pool at a large, public university located in the Southern U.S. (details in Table 1). Notably, data for Studies 1 and 2 were collected from different universities.
Procedure
Respondents provided informed consent, filled out a series of self-report questionnaires, and were provided with mental health resources during debriefing. Data for Study 2 were obtained as part of a larger study on autobiographical recall and suicidal ideation (see Chu et al., 2015a for details). These data have previously been used to examine the relationship between suicide risk and fear of negative evaluation (Chu et al., 2015b) and psychopathy (Brislin, Buchman-Schmitt, Patrick, & Joiner, 2016; Buchman-Schmitt et al., 2016).
Measures
Suicidal ideation
The Depressive Symptom Inventory-Suicidality Subscale (DSI-SS; Metalsky & Joiner, 1997), a 4-item self-report measure, was used to assess the frequency and intensity of suicidal thoughts in the previous two weeks. Scores range from 0 to 3 with higher scores reflect an increased severity of suicidal ideation. Prior studies have reported good validity and psychometric properties (Joiner, Pfaff, & Acres, 2002). Both the DSI-SS and SBQ-R, which was utilized in Study 1, have been identified to have particularly strong psychometric properties relative to other self-report measures of suicide risk (Batterham et al., 2015). In this study, the internal consistency of the DSI-SS was good (α=0.80).
Perceived social problem-solving ability
The Problem-Solving Inventory-Revised-Short Form (PSI-R-SF; Maydeu-Olivares & D’Zurilla, 1997) is a 16-item, 6-point Likert-type self-report measure of perceived social problem-solving capabilities. The PSI-R-SF assesses two adaptive problem-solving abilities (problem-solving self-efficacy, problem-solving skills). Previous research indicates that these two scales are consistent with the construct of social problem-solving ability (Maydeu-Olivares & D’Zurilla, 1997). In this study, total score, which was calculated by reverse-coding positive items and summing all items, was used to represent perceived social problem-solving deficits. Consistent with Heppner (1988), Form B was used in this study. In this sample, internal consistency was excellent (α=0.90).
Thwarted belongingness, perceived burdensomeness
The 15-item INQ (Van Orden et al., 2012) was used to assess TB and PB. Similar to the INQ-18 used in Study 1, a 7-point Likert scale, ranging from 1 to 7 was used. In the 15-item version, the 6-item INQ-PB ranges from 6 to 42 and the 9-item INQ-TB ranges from 9 to 63. Internal consistency was excellent for both the INQ-TB and INQ-PB (αs=0.91,0.94, respectively).
Rival mediator
The Beck Depression Inventory-Second Edition (BDI-2; Beck, Steer & Brown, 1996) was used to measure depressive symptom severity. The 21 items are rated on 4-point Likert scale ranging from 0 to 3. In this study, a total score was generated by summing all the items except item 9, which assesses suicidal thoughts and wishes, as this item overlaps with the dependent variable. Internal consistency was excellent (α=0.90).
Statistical analyses
The approach in Study 2 was the same as that of Study 1. However, in Study 2, depressive symptoms (BDI-2) was entered as the rival mediator. With regard to the normality of residuals, one variable (DSI-SS) in this sample evidenced significant skew (Skew = 2.10; Kolmogoroz-Smirnov statistic = 0.291, p<0.001), which was addressed using MLR. Again, FIML was used to handle missing data. With a sample of 105, we were adequately powered for mediation analyses (Fritz & MacKinnon, 2007). In Study 2, there was also a relatively large proportion of zero responses in our outcome variable (88/105); thus, ZINB regression analyses were conducted to evaluate the proposed paths in our mediation models.
Study 2 Results
Preliminary Analyses
Study variable details are provided in Table 2. Consistent with hypotheses and Study 1, significant positive correlations emerged between perceived social problem-solving deficits and TB, PB, and suicidal ideation (r=0.22–0.33, ps<0.05).
TB and PB as Parallel Mediators
As in Study 1, when TB and PB were entered as parallel mediators of the relationship between perceived social problem-solving deficits and suicidal ideation, controlling for age and sex. Again, the goodness-of-fit ranged from adequate to excellent (χ2(1) = 1.03, p = 0.51; RMSEA (90%CI) = 0.05 (0.03, 0.06), CFI/TLI = 0.96, 0.87; SRMR = 0.03). All α and β pathways in this mediation model were significant. The direct effect of deficits in problem-solving ability on suicidal ideation was not significant after accounting for TB and PB and the indirect effect of TB and PB on the relationship between deficits in problem-solving ability and suicidal ideation was estimated to be between 0.0035 and 0.0164, which is significant. Again, the pattern of findings remained the same after controlling for depressive symptoms and the overall regression model explained significant variance in suicidal ideation (R2=0.44, b=0.026, SE=0.002, 95%CI=0.0021, 0.0073; Figure 2B; Table 3).
Again, ZINB regression model results supported bootstrap mediation analyses. Thwarted belongingness (estimate = 0.07, SE = 0.021, p = 0.001, Wald χ2 = 22.52) and perceived burdensomeness (estimate = 0.175, SE = 0.061, p = 0.004, Wald χ2 = 18.57), individually, were both significantly associated with suicidal ideation. The model with social problem solving deficits as a predictor of suicidal ideation, controlling for age and sex, was significant, with Wald χ2 equal to 18.07, p < 0.001. Social problem-solving deficits were significantly associated with suicidal ideation (estimate = 0.029, robust SE = 0.011, p = 0.006). When thwarted belongingness and perceived burdensomeness were included into the model, the Wald χ2 value was significant (13.67, p < 0.001). However, the main effect of social problem solving deficits on suicidal ideation was no longer significant (estimate = 0.021, SE = 0.024, p = 0.38). Again, Vuong’s test (Vuong, 1989) was not significant (p = 0.72), which does not support the ZINB model.
Specificity of TB and PB
Again, we tested for specificity. The effect of TB (β=0.008; 95%CI=−0.017, 0.011) and PB (β=0.012; 95%CI=−0.003, 0.032) on suicidal ideation was not significantly mediated by perceived social problem-solving deficits, which supports the specificity of the roles of the independent variable (perceived social problem-solving deficits) and the mediators (TB, PB). Further, depressive symptoms did not mediate the relationship between perceived social problem-solving deficits and suicidal ideation, controlling for TB, PB, age and sex (b=0.0002, SE=0.002; 95%CI=−0.0031, 0.0042).
TB and PB as Individual Mediators
Finally, we evaluated TB and PB as individual mediators. When TB was entered as an individual mediator, the overall regression model was significant (R2=0.43) and the direct effect of perceived social problem-solving deficits on suicidal ideation was not significant after accounting for TB (see Table 3). The indirect effect of TB was significant and estimated to be between 0.0018 and 0.0125 (R2=0.0335, κ2=0.0971). The majority of the fit statistics for this model indicated adequate fit (χ2(1) = 1.96, p = 0.27; RMSEA (90%CI) = 0.09 (0.08, 0.11), CFI/TLI = 0.90, 0.79; SRMR = 0.10). Similarly, for analyses examining PB as an individual mediator, the overall regression model was significant (R2=0.44) and the direct effect was not significant after accounting for PB. The indirect effect of PB was significant and estimated to be between 0.0023 and 0.0159 (R2=0.0850, κ2=0.1639). This model exhibited excellent fit (χ2(1) = 1.81, p = 0.41; RMSEA (90%CI) = 0.02 (0.01, 0.04), CFI/TLI = 0.98, 0.96; SRMR = 0.01).
Study 2 Discussion
Results from Study 2, which were consistent with Study 1 and the interpersonal theory of suicide, contributed additional support for our study hypotheses. Specifically, among another sample of undergraduate students, perceived social problem-solving deficits were associated with thwarted interpersonal needs and greater levels of suicidal thoughts. These findings are consistent with prior research findings that perceived social problem-solving deficits are correlated with suicide-related behaviors (McAuliffe et al., 2006). As before, our findings indicated that the interpersonal theory constructs provide a mechanistic explanation. In contrast to Study 1, thwarted belongingness and perceived burdensomeness were both significant individual and parallel mediators. Nonetheless, consistent with Study 1, while the model with thwarted belongingness as an individual mediator exhibited somewhat poor fit, the two-mediator model and the perceived burdensomeness-only model both exhibited excellent fit and accounted for a similar amount of variance in suicide risk. This again implies that perceived burdensomeness may be a more important indicator of risk.
Additionally, we found support for the specificity of perceived burdensomeness and thwarted belongingness as parallel mediators, as perceived social problem-solving deficits did not significantly mediate the relationship between the interpersonal theory variables and suicidal ideation, and depression did not significantly account for the relationship between perceived social problem-solving deficits and suicidal ideation. Importantly, the measure of depressive symptoms used in this study exhibited excellent internal consistency, which bolsters these findings. Further, as in Study 1, the proposed pathways of the mediation models were supported by analyses accounting for the excess zeroes, which provides additional support for our findings.
Limitations of Study 2 must be acknowledged. For one, although young adults have high rates of suicidal ideation and are, thus, an important population for research, this sample was relatively high-functioning as all participants were university students; future research using samples from high-risk populations (e.g., military, inpatient) would be useful. As in Study 1, undergraduate students have more opportunities for social connection. Thus, research in samples with fewer interpersonal resources is an important next step. Finally, Study 2 used a cross-sectional design, which precludes confirmation of temporality.
Study 3: Homeless Individuals
Given that Studies 1 and 2 were limited to undergraduate students with greater opportunities for interpersonal connection, we aimed to replicate these findings among a sample of homeless individuals with a smaller network of interpersonal resources. We expected a similar pattern of findings for Study 3, such that thwarted belongingness and perceived burdensomeness would serve as explanatory links.
Study 3 Method
Participants
Participants were 53 adults recruited from a Southeastern U.S. community day center that provides services, including primary and mental healthcare, to homeless individuals (see Table 1).
Procedure
All participants provided informed consent, and were compensated upon completion of a battery of questionnaires. Respondents were provided with mental health and suicide prevention resources. Of note, these data have not been previously published.
Measures
Suicide risk
The SBQ-R was used in analyses and internal consistency was good (α=0.81).
Perceived social problem-solving ability
The SPSI-R-SF was used and internal consistency was excellent (α=0.95).
Thwarted belongingness, perceived burdensomeness
The INQ-PB and INQ-TB subscales of the INQ-15 both exhibited good-to-excellent internal consistency (αs=0.91,0.86, respectively).
Rival mediator
The Patient Health Questionnaire-9 (PHQ-9; Kroenke & Spitzer, 2001) is a 9-item measure of depressive symptoms. Item 9, which measures suicidal ideation and death, was removed to avoid redundancy with the dependent variable. Items are rated on a 4-point Likert scale ranging from 0 to 3. Internal consistency was excellent (α=0.91).
Statistical analyses
The analytical approach remained unchanged. Missing data in this study were addressed using FIML and given the sample size of 53, we were adequately powered for mediation analyses (Fritz & MacKinnon, 2007). However, in this study, we were significantly underpowered to evaluate model fit indices (Wolf, Harrington, Clark, & Miller, 2013). In Study 3, although inspection of the histogram for our outcome variable did not reveal an excess of zero responses (15/53), we were underpowered (<0.80) to conduct ZINB regressions to confirm whether a zero-inflated model better fits these data.
Study 3 Results
Preliminary Analyses
See Table 2 for variable details. Significant positive correlations emerged between perceived social problem-solving deficits, TB, PB, and suicide risk (r=0.36–0.39, ps<0.05).
TB and PB as Parallel Mediators
As in Studies 1 and 2, TB and PB were first examined as parallel mediators, controlling for age and sex. As before, all α and β pathways in the mediation model were significant (Table 3). The direct effect of perceived social problem-solving deficits on suicide risk was not significant after accounting for TB and PB (p=0.20). The indirect effect of TB and PB on the relationship between perceived social problem-solving deficits and suicide risk was significant and estimated to be between 0.0056 and 0.0987 (Figure 2C). Notably, the pattern of findings remained the same after accounting for depressive symptoms and the overall regression model explained a significant portion of the variance in suicide risk (R2=0.52; b=0.0456, SE=0.03, 95%CI=0.0015, 0.1017).
Specificity of TB and PB
With regard to specificity, the effect of TB (β=0.012; 95%CI=−0.021, 0.095) and PB (β=0.059; 95%CI=−0.003, 0.179) on suicide risk was not significantly mediated by social problem-solving ability, which supports the specificity of the mediators. Depressive symptoms did not mediate the relationship between social problem-solving ability and suicide risk, controlling for TB, PB, age and sex (b=−0.0037, SE=0.013; 95%CI=−0.0284, 0.0282).
TB and PB as Individual Mediators
When TB was entered as an individual mediator, the overall regression model explained a significant portion of variance in suicide risk, controlling for depression, age and sex (R2=0.50). The direct effect of social problem-solving deficits on suicide risk remained significant after accounting for TB and the indirect effect of TB was estimated to be between −0.0169 and 0.1017, which is not significant as the 95% confidence interval crossed zero. For analyses examining PB as an individual mediator, the overall regression model was significant (R2=0.53) and the direct effect of social problem-solving deficits on suicide risk was not significant after accounting for PB (p=0.17). The indirect effect of PB was significant and estimated to be between 0.0070 and 0.0936 (R2=0.1257, κ2=0.2191).
Study 3 Discussion
Again, in Study 3, our results were consistent with previous research and provided support for our hypotheses. That is, among a sample of homeless individuals, perceived social problem-solving deficits were associated with more severe suicide risk and thwarted interpersonal needs. As before, thwarted belongingness and perceived burdensomeness accounted for the relationship between perceived social-problem-solving deficits and suicide risk. In this sample, individually, thwarted belongingness was not a significant mediator while perceived burdensomeness emerged as a significant mediator. The two models with perceived burdensomeness accounted for more variance in suicide risk than the model with thwarted belongingness as the main predictor. Again, these findings appear to be supportive of previous research indicating perceived burdensomeness may be more robust (Bryan et al., 2010). As in the previous studies, a rival mediator—depressive symptoms—did not demonstrate a mediating effect, highlighting the specificity of thwarted belongingness and perceived burdensomeness.
This was the first study, to our knowledge, to examine the relationship between constructs of the interpersonal theory and suicide-related behaviors in a sample of homeless individuals. Findings from Study 3 are especially important given the high rates of psychiatric diagnoses and suicidal ideation and behavior among homeless individuals, particularly those with a history of mental illness (Prigerson, Desai, Liu-Mares, & Rosenheck, 2003), and the lack of research on suicidal symptoms in this population. Additionally, homeless individuals tend to have fewer interpersonal resources (Hwang et al., 2009); thus, our findings are exceptionally relevant for impacting psychological well-being in this population.
Despite replicating findings from Studies 1 and 2 in a demographically distinct sample, several limitations should be noted. Namely, the sample size used in Study 3, though adequate for bootstrap bias-corrected mediations (Fritz & MacKinnon, 2007), was limited and diminished our ability to detect smaller effects, to examine any potential impact of excess zeroes on our study conclusions, and to evaluate model fit. Thus, future studies using larger samples will be needed to verify these findings in this population. Further, this sample, though high-risk and greatly understudied, may not generate generalizable findings; replication of this research in other samples is needed. Finally, as in Studies 1 and 2, Study 3 also utilized cross-sectional data, thus reducing our ability to determine the predictive validity of our hypotheses.
Study 4: Primary Care Patients
Given that Studies 1, 2, and 3 were cross-sectional, we sought to examine the predictive utility of our hypothesis in Study 4 using a longitudinal study design. Specifically, we investigated the prospective relationship between perceived social problem-solving deficits and suicide risk in a sample of adult primary care patients. As before, we predicted that study variables would be significantly related and the interpersonal theory variables would emerge as significant parallel mediators, cross-sectionally and longitudinally.
Study 4 Method
Participants
Participants were 222 adult patients receiving treatment from a Southeastern primary care clinic located in the U.S. that serves low-income and uninsured individuals (Table 1).
Procedure
Patients completed self-report measures at baseline (Time 1; n=216–222) and at follow-up (Time 2; n=98–99). Although patients were asked to complete assessments after 6 months, the follow-up period ranged from 6 to 12 months (M=8) due to difficulties establishing contact with participants and desire to minimize the amount of missing data. All participants provided informed consent at both time points and were monetarily compensated upon study completion. Data used for Study 4 have been previously used to evaluate the links between insomnia (Chu et al., 2017) and neuroticism (Walker, Chang, & Hirsch, in press) and suicide risk.
Measures
Suicide risk
The SBQ-R was used and internal consistency was good at Times 1 and 2 (αs=0.86,0.84, respectively).
Perceived social problem-solving ability
The SPSI-SF-R was measured at Time 1 and internal consistency was excellent (α=0.93).
Thwarted belongingness, perceived burdensomeness
The INQ-15 was used and internal consistency was good-to-excellent for the INQ-TB and INQ-PB at Time 1 (αs=0.89,0.93, respectively) and Time 2 (αs=0.89,0.94, respectively).
Rival mediator
The PHQ-9 (without item 9-suicide risk) was used to measure depressive symptoms at Time 1 and internal consistency was excellent (α=0.91).
Statistical analyses
Study 4’s analytical approach was the same as that of Studies 1, 2 and 3; however, with the longitudinal design, we were able to evaluate our hypotheses cross-sectionally at Time 1 and then prospectively, across Times 1 and 2. Further, independent t-tests were used to compare those who did and did not complete the measures at Time 2 as 124 participants did not complete Time 2. A test of missing data indicated that data were not missing at random, Little’s Missing Completely At Random (MCAR) χ2(33) = 47.21, p = 0.052. To address this issue, FIML was used to handle missing data. As our sample size ranged from 98 to 222, we were sufficiently powered for mediation analyses (Fritz & MacKinnon, 2007). As in Study 3, all participants in Study 4 endorsed at least some suicidal thoughts and other related risk factors, thus, our outcome variable did not exhibit an excess of zero responses at Time 1 (46/222) or Time 2 (16/98).
Study 4 Results
Preliminary Analyses
See Table 2 for details on Study 4 variables. As expected, significant positive correlations emerged between perceived social problem-solving deficits and TB, PB, and suicide risk at all time points (r=0.37–0.48, ps<0.001). Individuals who participated at Time 2 and those who only completed Time 1 did not significantly differ on demographic and key study variables at Time 1, including age (t(213)=−2.180, p=0.10), sex (t(220)=−0.67, p=0.50), ethnicity (t(219)=1.11, p=0.27), perceived social problem-solving deficits (t(219)=1.25, p=0.21), thwarted belongingness (t(214)=0.81, p=0.50), perceived burdensomeness (t(220)=0.80, p=0.42), and suicide risk (t(215)=1.40, p=0.16).
TB and PB as Cross-Sectional Parallel Mediators
First, we tested TB and PB as parallel mediators of the relationship between perceived social problem-solving deficits and suicide risk cross-sectionally at Time 1, controlling for age and sex. Goodness-of-fit indices were, again, adequate to excellent (χ2(1) = 1.75, p = 0.53; RMSEA (90%CI) = 0.06 (0.01, 0.10), CFI/TLI = 0.91, 0.98; SRMR = 0.05). All α and β pathways in this mediation model were significant. The direct effect of perceived social problem-solving deficits on suicide risk was not significant after accounting for TB and PB (p=0.21), indicating mediation. The indirect effect of TB and PB on the relationship between perceived social problem-solving deficits and suicide risk was estimated to be between 0.0398 and 0.0801 (95%CI), indicating significance. Notably, the pattern of findings remained the same after controlling for depression and the overall model accounted for a significant amount of variance in suicide risk (R2=0.44, b=0.0224, SE=0.0084, 95%CI=0.009, 0.0431; Table 3).
Specificity of TB and PB as Cross-Sectional Mediators
With regard to mediator specificity, mediation analyses indicated that the effect of TB (β=−0.003; 95%CI=−0.054, 0.054) and PB (β<0.001; 95%CI=−0.020, 0.012) on suicide risk was not significantly mediated by social problem-solving ability, which supports the specificity of the mediators. Again, depressive symptoms also did not mediate the relationship between social problem-solving ability and suicide risk, controlling for TB, PB, age and sex (b=0.0045, SE=0.035; 95%CI=−0.002, 0.0140).
TB and PB as Cross-Sectional Individual Mediators
When TB was entered as an individual mediator, the overall regression model explained a significant portion of variance in suicide risk, controlling for depression, age and sex (R2=0.35). The direct effect of perceived social problem-solving deficits on suicide risk was not significant after accounting for TB (p=0.21). The indirect effect of TB was estimated to be between 0.0110 and 0.0204 (95%CI) and was significant (R2=0.1133, κ2=0.1906). The majority of the fit statistics for this model indicated adequate fit (χ2(1) = 1.28, p = 0.46; RMSEA (90%CI) = 0.08 (0.06, 0.11), CFI/TLI = 0.87, 0.85; SRMR = 0.11). When PB was entered as an individual mediator, the overall regression model explained a significant portion of variance in suicide risk, beyond depression, age, and sex (R2=0.43). The direct effect of perceived social problem-solving deficits on suicide risk was not significant after accounting for PB (p=0.55) and the indirect effect of PB was significant and estimated to be between 0.0068 and 0.0374 (95%CI; R2=0.1316, κ2=0.2517). The fit statistics for this model indicated excellent fit (χ2(1) = 1.68, p = 0.30; RMSEA (90%CI) = 0.07 (0.05, 0.09), CFI/TLI = 0.95, 0.94; SRMR = 0.05).
TB and PB as Prospective Parallel Mediators
Second, using a longitudinal approach, we tested TB and PB at Time 1 as parallel mediators of the relationship between perceived social problem-solving deficits at Time 1 and suicide risk at Time 2, controlling for suicide risk at Time 1, age and sex. Goodness-of-fit indices indicated poor to adequate (χ2(1) = 3.16, p = 0.03; RMSEA (90%CI) = 0.07 (0.05, 0.09); CFI/TLI = 0.59, 0.99; SRMR = 0.16). All α and β pathways in this mediation model were significant. The direct effect of perceived social problem-solving deficits on suicide risk was not significant after accounting for TB and PB (p=0.07). The indirect effect of TB and PB on the relationship between perceived social problem-solving deficits and suicide risk was estimated to be between 0.0155 and 0.0780 (95%CI;), indicating significance. When additionally controlling for depression, the overall regression model explained a significant portion of the variance in suicide risk (R2=0.28), and the indirect effect was significant (b=0.0324, SE=0.012, 95%CI=0.0111, 0.0720; Table 3; Figure 2D).
Specificity of TB and PB as Prospective Mediators
Again, mediation analyses indicated that the effect of TB (β=0.041; 95%CI=−0.005, 0.132) and PB (β=0.032; 95%CI=−0.004, 0.216) on suicide risk was not significantly mediated by social problem-solving ability, supporting the specificity of our hypothesized mediators. Depressive symptoms did not mediate the relationship between social problem-solving ability and suicide risk, controlling for TB, PB, age and sex (b=0.0066, SE=0.0071; 95%CI=−0.0021, 0.0273).
TB and PB as Prospective Individual Mediators
Finally, when TB was entered as an individual mediator, the overall regression model explained a significant portion of variance in suicide risk, controlling for depression, age and sex (R2=0.25, F[5,81]=5.34, p<0.001), the direct effect of perceived social problem-solving deficits on suicide risk was not significant after accounting for TB (p=0.32), and the indirect effect of TB was significant (95%CI = 0.003, 0.0391; R2=0.1054, κ2=0.1766). Fit statistics for this model indicated adequate to good fit (χ2(1) = 1.96, p = 0.27; RMSEA (90%CI) = 0.09 (0.08, 0.11), CFI/TLI = 0.90, 0.79; SRMR = 0.10). For analyses examining PB as an individual mediator, the overall regression model also explained a significant portion of variance in suicide risk (R2=0.33), the direct effect of perceived social problem-solving deficits on suicide risk was not significant after accounting for PB (p=0.84). The indirect effect of PB was significant and estimated to be between 0.0088 and 0.0629 (95%CI; R2=0.1267, κ2=0.2507). This model demonstrated excellent fit (χ2(1) = 2.01, p = 0.08; RMSEA (90%CI) = 0.06 (0.03, 0.08), CFI/TLI = 0.98, 0.95; SRMR = 0.09).
Study 4 Discussion
Consistent with Studies 1,2, and 3, Study 4 results supported our overall hypotheses. Findings highlighted that there is a cross-sectional and prospective relationship between deficits in problem-solving abilities and suicide risk. Importantly, thwarted belongingness and perceived burdensomeness provide a mechanistic explanation for this link both cross-sectionally and longitudinally, which underscores the predictive validity of our results. In this sample, thwarted belongingness and perceived burdensomeness also emerged as significant individual mediators. As in Studies 1 to 3, it is also notable that across both time points, the pattern of findings remained significant even after accounting for depression and depression was not a significant mediator, which supports the robustness and specificity of our findings.
Interestingly, the mediation model with both mediators and that with only thwarted belongingness both exhibited poor to adequate fit while the model with perceived burdensomeness as an individual mediator exhibited excellent fit. Both models that included perceived burdensomeness as a predictor, cross-sectionally and longitudinally, accounted for more variance in suicide risk than the model with only thwarted belongingness. Again, this suggests that perceived burdensomeness is a particularly important predictor of suicide risk, which is in line with recent research examining thwarted belongingness and perceived burdensomeness as longitudinal suicide risk predictors (Chu et al., 2016c; Ma et al., 2016).
This study, which extended findings to a sample of low-income, primary care patients is particularly useful, as many individuals who die by suicide visit a primary care clinician instead of a specialist mental health provider (Luoma, Martin, & Pearson, 2002). Specifically, previous research has shown that in the month prior to death, 45% of suicide decedents contacted their primary care provider and even higher rates are seen in older adult decedents (Luoma et al., 2002). This finding underscores the relevance of this setting in efforts to understand factors contributing to increased suicide risk as these settings represent key catchment areas for at-risk individuals. Although this study did not select for individuals with increased suicide risk, the number of patients in this sample who reported suicide risk on the SBQ-R (55.4%, n=123) is significantly higher compared to other studies with middle-aged and older adults, and adolescent samples, which have reported prevalence rates ranging from 1.0%–14.3% (Heisel et al., 2010; Schulberg et al., 2004; Unützer et al., 2006; Wintersteen, 2010). The severity of this sample further highlights the relevance of our findings.
Study 4’s limitations should be noted. For one, the single follow-up time point of approximately 8 months was not sufficient to capture the dynamic nature of suicidal thoughts (Bryan & Rudd, 2016) and fluctuations in thwarted belongingness and perceived burdensomeness. Therefore, future research prospectively examining the role of problem-solving deficits in the etiology of suicidal thoughts and behaviors should utilize multiple time points. Relatedly, a minimum of three time points would also allow for the most conventional mediation test of interpersonal theory variables (Maric, Wiers, & Prins, 2012). It is also important to note that the sample utilized for Sample 4 was of lower socioeconomic status and, thus, caution is warranted when generalizing these findings to other sociodemographic groups.
Study 5: Military Service Members
In Study 5, we aimed to address previous limitations and extend findings from Studies 1, 2, 3, and 4 to a sample of military service members, who often have a greater prevalence and severity of suicide-related symptoms. We utilized a longitudinal study design with three time points. Again, we expected that thwarted belongingness and perceived burdensomeness would emerge as significant explanatory links, cross-sectionally and longitudinally.
Study 5 Method
Participants
Participants were 329 service members recruited from four U.S. Army Medical Center-affiliated sites (details in Table 1).
Procedure
After providing informed consent, participants completed baseline diagnostic interview and self-report measures. Follow-up assessments were completed five times over the course of two years. In this study, only baseline (Time 1, n=308–329), one-month (Time 2, n=251) and six-month (Time 3, n=139) follow-up data were used due to limited sample sizes at the remaining follow-up time points. Data for Study 5 were obtained as part of a larger treatment efficiency study examining young adults at high risk suicidal behaviors (i.e., referred for treatment following a suicide attempt, and/or those with a history of mood, adjustment or alcohol use disorders, and current suicidal ideation; see Rudd et al., 1996). These data have been previously used to examine problem-solving ability in the context of positive emotions (Joiner et al., 2001), mood/anxiety disorders (Joiner et al., 2003), and hopelessness and ideation (Dixon, 1994). Additionally, data for Study 5 have also been used to examine the relationship between suicidality and antisocial personality symptoms (Chu, Buchman-Schmitt, Joiner, & Rudd, 2016), negative life events (Joiner & Rudd, 2000), attempt history (Rudd, Joiner, & Rajab, 1996), the interpersonal theory (Joiner et al., 2009), a suicidal ideation scale (Joiner, Rudd, & Rajab, 1997), childhood diagnoses (Rudd, Joiner, & Rumzek, 2004), insomnia and loneliness (Hom et al., 2017).
Measures
Suicidal ideation
The Modified Scale for Suicidal Ideation (MSSI; Miller, Norman, Bishop, & Dow, 1986) is an 18-item clinician-administered measure of suicidal ideation in the last year. Total scores range from 0 to 54 and higher scores indicate greater suicidal symptoms. The MSSI has excellent reliability (α = 0.94), construct validity, and inter-rater reliability (Miller et al., 1986). Interrater reliability for the MSSI was unavailable in this study due to limitations in resources; however, as expected (Miller et al., 1986), the MSSI was significantly and positively correlated with self-reported depressive symptoms (BDI; r=0.45) and hopelessness (Beck Hopelessness Scale; r=0.49). In this study, internal consistency for the MSSI was good at Times 1, 2, and 3 (αs=0.88,0.89,0.86, respectively).
Social problem-solving ability
The original, 35-item PSI (Heppner, 1988; Heppner & Petersen, 1982) was used to assess social problem-solving ability. Items on the PSI are rated on a 6-point Likert scale and items assessing adaptive problem-solving approaches were reverse-scored. The total PSI score, which ranges from 35 to 210, was generated by summing all items and indicates perceived social problem-solving deficits. Again, Form B of the PSI was used (Heppner, 1988). The PSI has previously evidenced adequate-to-excellent reliability (α=0.72–0.90) and similarly, in this study, internal consistency was excellent at Time 1 (α=0.92).
Thwarted belongingness, perceived burdensomeness
The INQ was not available. Thus, consistent with Joiner and colleagues’ (2009) approach, proxy items were selected from the Suicide Probability Scale (SPS; Cull & Gill, 1988) to capture TB and PB (see Table 4 for a comparison of items on the INQ-TB/INQ-PB with SPS-TB/SPS-PB). The SPS is a 36-item measure of feelings and behaviors that may indicate increased suicide risk. Items on the SPS are rated on a 4-point Likert scale ranging from none of the time to all of the time. Five items from the SPS were used to measure TB (SPS-TB: items 2,9,10,12,23) and four items from the SPS were used to measure PB (SPS-PB: items 6,15,17,24).
Table 4.
Thwarted Belongingness and Perceived Burdensomeness: Comparison of the Items from the Interpersonal Needs Questionnaire-18 to Proxy Items Used in Study 5 from the Suicide Probability Scale.
| Thwarted Belongingness | Perceived Burdensomeness | ||
|---|---|---|---|
| INQ-18 | SPS | INQ-18 | SPS |
| Item 10: These days, other people care about me. (R) | Item 2: I feel many people care for me deeply. (R) | Item 5: These days I think I contribute to the well-being of the people in my life. (R) | Item 6: I feel there is much I can do which is worthwhile. (R) |
|
| |||
| Item 14: These days, I feel disconnected from other people. | Item 9: I feel isolated from people. | Item 3: These days I think I have failed the people in my life. | Item 15: I feel I am not able to do many things well. |
|
| |||
| Item 13: These days, I am fortunate to have many caring and supportive friends. (R) | Item 10: I feel many people appreciate the real me. (R) | Item 7: These days I think the people in my life wish they could be rid of me. | Item 17: I think that no one will miss me when I am gone. |
|
| |||
| Item 11: These days, I feel like I belong. (R) | Item 12: I feel so lonely I cannot stand it. | Item 1: These days the people in my life would be better off if I were gone. | Item 24: I feel that people would be better off if I were dead. |
|
| |||
| Item 16: These days, I feel that there are people I can turn to in times of need. (R) | Item 23: I feel I don’t have many friends I can count on. | ||
Note. (R) = item is reverse-scored. INQ= Interpersonal Needs Questionnaire-18, items are rated on a 7-point Likert scale ranging from 1-not true for me at all to 7-very true for me. SPS = Suicide Probability Scale, items are rated on 4-point Likert scale ranging from 0-none of the time to 3-all of the time.
The INQ was not available in Study 5. Consistent with Joiner and colleagues’ (2009) approach, proxy items were selected from the SPS to represent thwarted belongingness and perceived burdensomeness.
With regard to validity, face validity appeared adequate as indicated by significant, moderate, positive correlations between SPS-TB and SPS-PB and depressive symptoms, suicidal ideation, and hopelessness (Joiner et al., 2009), which are comparable to those reported by Van Orden and colleagues using the INQ (2008). There is also evidence for validity from a previous study of undergraduates (Witte & Joiner, 2008): these SPS-TB items were moderately related to the INQ-TB (r=.52, p<0.001) and weakly related to INQ-PB (r=0.30, p<0.01); and SPS-PB items were moderately correlated with the INQ-PB (r=.56, p<0.001) and weakly related to INQ-TB (r=0.28, p<0.01). Finally, in this sample, results from principal axis factor analyses (two-factor, oblique rotation) indicated that items with content most relevant to the constructs of interest loaded highly on the expected factors. For example, the item with the highest loading (0.70) for SPS-PB was: I feel people would be better off if I were dead; the item with highest loading (0.87) for SPS-TB was: I feel many people care for me deeply. Further, the internal consistency was adequate for the SPS-TB and SPS-PB at Time 1 (αs=0.73, 0.71, respectively) and Time 2 (αs=0.74, 0.77, respectively). For details, see Joiner and colleagues’ (2009) study, which used this sample and the same proxy items for the interpersonal theory variables.
Rival mediator
The BDI-I was used (Beck, Ward, Mendelson, Mock, & Erbaugh, 1961). Internal consistency of this measure was excellent (α=0.91).
Statistical analyses
Consistent with Study 4, we first tested our hypotheses using a cross-sectional approach at Time 1. However, in Study 5, three time points were available; thus, we examined our longitudinal hypotheses across Times 1, 2, and 3. Given attrition across time points, one-way ANOVA was used to compare those who completed measures at all three time points to those who only completed Times 1 and 2, and those who only completed Time 1. As in Study 4, missing data analyses indicated that data were not missing at random, Little’s MCAR χ2(200) = 266.367, p = 0.001. Missing data were again handled using FIML. Given that the sample size ranged from 139 to 329, we were sufficiently powered for bias-corrected bootstrap mediation analyses (Fritz & MacKinnon, 2007). In Study 5, our outcome variable did not exhibit an excess of zero responses at Time 1 (1/329); however, an excess of zeroes was noted on the histograms of our outcome variables at Time 2 (160/251) and Time 3 (110/139). ZINB regression analyses were conducted for our cross-sectional models with Time 2 ideation and Time 3 ideation as dependent variables, and for the longitudinal models using Time 3 ideation as the outcome; again, Vuong’s Test (Vuong, 1989) was used to evaluate the ZINB model.
Study 5 Results
Preliminary Analyses
See Table 2 for Study 5 details. Consistent with hypotheses and the previous four studies, significant positive correlations emerged between perceived social problem-solving deficits, the interpersonal theory variables, and suicidal ideation at all time points (r=0.20–0.47, ps<0.05). With regard to participant variations in study completion, no significant differences in Time 1 demographic and key study variables emerged, including age (F(328)=0.91, p=0.40), sex (F(329)=0.56, p=0.57), ethnicity (F(329)=0.35, p=0.32), suicidal ideation (F(329)=2.43, p=0.09), perceived social problem-solving deficits (F(305)=0.81, p=0.45), thwarted belongingness (F(324)=0.16, p=0.85), and perceived burdensomeness (F(325)=0.20, p=0.82).
TB and PB as Cross-Sectional Parallel Mediators
We tested TB and PB as parallel mediators of the relationship between perceived social problem-solving deficits and suicidal ideation cross-sectionally at Time 1, controlling for age and sex. Goodness-of-fit indices indicated excellent fit (χ2(1) = 0.03, p = 0.87; RMSEA (90%CI) = 0.01 (0.01, 0.08); CFI/TLI = 0.99, 1.12; SRMR = 0.002). All α and β paths were significant and the direct effect of deficits in problem-solving ability on suicidal ideation were no longer significant after accounting for the effects of TB and PB (p=0.09). The indirect effect of TB and PB on the relationship between perceived social problem-solving deficits and suicidal ideation was significant and estimated to be between 0.0637 and 0.1220 (95%CI). Findings remained significant despite controlling for depressive symptoms and the overall regression model explained a significant portion of the variance in suicidal ideation (R2=0.36, b=0.0982, SE=0.02, 95%CI=0.0676, 0.1348; Table 3).
We also conducted the same analyses at Times 2 and 3, cross-sectionally. Notably, the pattern of findings was consistent with our conjectures, such that the indirect effect of social problem-solving ability on suicidal ideation through the two interpersonal theory variables was significant beyond depressive symptoms, age, and sex at Time 2 (n=234, R2=0.28, b=0.0367, SE=0.02, 95%CI=0.0108, 0.0705) and similarly, at Time 3 (n=135, R2=0.30, b=0.0762, SE=0.03, 95%CI=0.0267, 0.1525).
ZINB regression model results also supported our hypotheses. At Time 2, thwarted belongingness (estimate = 0.172, SE = 0.040, p < 0.001, Wald χ2 = 18.27) and perceived burdensomeness (estimate = 0.247, SE = 0.064, p < 0.001, Wald χ2 = 15.09), individually, were both significantly associated with suicidal ideation. Directly, social problem-solving deficits were significantly associated with suicidal ideation, beyond age and sex (estimate = 0.024, robust SE = 0.007, p = 0.001, Wald χ2 = 11.37). When thwarted belongingness and perceived burdensomeness were included, the main effect of social problem solving deficits on suicidal ideation was no longer significant (estimate = 0.010, SE = 0.008, p = 0.22; Wald χ2 = 1.49). Vuong’s test (Vuong, 1989) was significant (p < 0.001) and supports the ZINB model.
At Time 3, thwarted belongingness (estimate = 0.177, SE = 0.089, p = 0.047, Wald χ2 = 3.95) and perceived burdensomeness (estimate = 0.330, SE = 0.138, p = 0.017, Wald χ2 = 5.72), individually, were both significantly associated with suicidal ideation. Directly, social problem-solving deficits were significantly associated with suicidal ideation, beyond age and sex (estimate = 0.041, robust SE = 0.016, p = 0.011, Wald χ2 = 6.40). When thwarted belongingness and perceived burdensomeness were included, the main effect of social problem solving deficits on suicidal ideation was no longer significant (estimate = 0.019, SE = 0.024, p = 0.43; Wald χ2 = 0.62). Vuong’s test (Vuong, 1989) was significant (p < 0.001), which supports the ZINB model.
Specificity of TB and PB as Cross-Sectional Mediators
At Time 1, mediation analyses indicated that the effect of TB (β=−0.080; 95% CI=−0.323, 0.088) and PB (β=−0.009; 95%CI=−0.119, 0.030) on suicidal ideation was not significantly mediated by social problem-solving ability. Further, depressive symptoms did not mediate the relationship between social problem-solving ability and suicidal ideation, controlling for TB, PB, age and sex (b=0.0013, SE=0.0255; 95%CI=−0.0014, 0.0108), supporting the specificity of our hypotheses.
TB and PB as Cross-Sectional Individual Mediators
When TB was entered as an individual mediator, the overall regression model explained a significant portion of variance in suicidal ideation, controlling for depression, age and sex (R2=0.26). The direct effect of perceived social problem-solving deficits on suicidal ideation remained significant after accounting for TB (p=0.002). The indirect effect of TB was significant and estimated to be between 0.0300 and 0.0835 (95%CI; R2=0.0860, κ2=0.1252). Fit statistics for this model indicated adequate fit to excellent (χ2(1) = 2.09, p = 0.08; RMSEA (90%CI) = 0.10 (0.08, 0.12), CFI/TLI = 0.92, 0.91; SRMR = 0.11). For analyses examining PB as an individual mediator, the overall regression model explained a significant portion of variance in suicidal ideation, controlling for depression, age and sex (R2=0.35). The direct effect of perceived social problem-solving deficits on suicidal ideation remained significant after accounting for PB (p=0.04). The indirect effect of PB was estimated to be between 0.0678 and 0.1335 (95%CI), indicating significance (R2=0.1183, κ2=0.2063). The majority of the fit statistics for this model indicated adequate fit (χ2(1) = 1.25, p = 0.57; RMSEA (90%CI) = 0.04 (0.02, 0.05), CFI/TLI = 0.97, 0.98; SRMR = 0.07).
Cross-sectionally, at Time 2, TB (b=0.0513, SE=0.01, 95%CI=0.0401, 0.1123; R2=0.0938, κ2=0.1307) and PB (b=0.0734, SE=0.02, 95%CI=0.0298, 0.0826; R2=0.1201, κ2=0.1737) were both significant individual mediators; however, the direct effects on suicidal ideation remained significant (TB-p=0.003; PB-p=0.006), suggesting partial mediation. At Time 3, TB (b=0.0396, SE=0.02, 95%CI=0.0104, 0.0845; R2=0.0580, κ2=0.0923) and PB (b=0.0741, SE=0.03, 95%CI=0.0307, 0.1391; R2=0.0836, κ2=0.1799) were both significant individual mediators. While the direct effect of PB as an individual mediator was not significant (p=0.18), suggesting mediation, the direct effect of TB remained significant (p=0.02), indicating partial mediation.
TB and PB as Prospective Parallel Mediators
Next, using a longitudinal approach, we tested TB and PB at Time 2 as parallel mediators of the relationship between perceived social problem-solving deficits at Time 1 and suicidal ideation at Time 3, controlling for suicidal ideation at Time 1, age and sex. The majority of the fit statistics for this model indicated poor to adequate fit (χ2(1) = 6.01, p = 0.02; RMSEA (90%CI) = 0.08 (0.06, 0.11), CFI/TLI = 0.81, 0.92; SRMR = 0.10). Both α paths and the β path from PB to suicidal ideation were significant; however, the β path from TB to suicidal ideation was not significant. The direct effect was not significant (p=0.43) and the indirect effect of TB and PB on the relationship between perceived deficits in problem-solving ability and ideation was estimated to be between −0.0017 and 0.0496 and not significant as the 95% confidence interval crossed zero. After additionally controlling for depression, the overall regression model did not explain a significant portion of the variance in suicidal ideation (R2=0.10, p=0.09), although there was a trend toward significance (b=0.009. SE = 0.01, 95%CI = −0.0074, 0.0469; Table 3). Given that this model was not significant, we did not evaluate its specificity.
ZINB regression model results indicated that Time 2 thwarted belongingness (estimate = 0.095, SE = 0.086, p = 0.27, Wald χ2 = 1.21) and Time 2 perceived burdensomeness (estimate = 0.163, SE = 0.131, p = 0.21, Wald χ2 = 1.54), individually, were not significantly associated with Time 3 suicidal ideation. Time 1 social problem-solving deficits were not significantly associated with Time 3 suicidal ideation (estimate = 0.011, robust SE = 0.015, p = 0.45, Wald χ2 = 0.57). When thwarted belongingness and perceived burdensomeness were included into the model, the main effect of social problem solving deficits on suicidal ideation was, as expected, non-significant (estimate = 0.006, SE = 0.016, p = 0.68). Vuong’s test (Vuong, 1989) was significant (p < 0.001), which supports the ZINB model.
PB as a Prospective Individual Mediator
We examined PB at Time 2 as an individual mediator of the relationship between perceived social problem-solving deficits at Time 1 and suicidal ideation at Time 3, controlling for age and sex. The direct effect of deficits in problem-solving ability on suicidal ideation was no longer significant after accounting for PB (p=0.45). The indirect effect of PB on the relationship between deficits in problem-solving ability and suicidal ideation was significant and estimated to be between 0.0010 and 0.0473 (95%CI; R2=0.0079, κ2=0.0420). Goodness-of-fit indices largely indicated excellent fit (χ2(1) = 2.59, p = 0.11; RMSEA (90%CI) = 0.09 (0.01, 0.25); CFI/TLI = 0.98, 0.86; SRMR = 0.03). When depression is included into the model, the overall regression model explained a significant portion of the variance in suicidal ideation at Time 3 (R2=0.10, b=0.0175, SE=0.01, 95%CI = 0.0047, 0.0425; Table 3; Figure 2E).
Specificity of PB as an Individual Mediator
Mediation analyses indicated that the effect of PB on suicidal ideation was not significantly mediated by social problem-solving ability (b=0.0460, SE=0.0678; 95%CI=−0.0505, 0.2381). Depressive symptoms did not mediate the prospective relationship between social problem-solving ability and suicidal ideation, controlling for PB, age and sex (b=−0.0007, SE=0.0034; 95%CI=−0.0134, 0.0027), supporting the specificity of PB as the mediator.
TB as a Prospective Individual Mediator
Finally, when TB was entered as an individual mediator, the overall regression model did not explain a significant portion of variance in suicidal ideation, controlling for depression, age and sex (R2=0.06). The direct effect of perceived social problem-solving deficits on suicidal ideation was not significant after accounting for TB (b=0.0201, SE=0.04 p=0.56). The indirect effect of TB was estimated to be between −0.0035 and 0.0319 (95%CI) and not significant. Fit indices for this model indicated adequate fit (χ2(1) = 3.01, p = 0.12; RMSEA (90%CI) = 0.08 (0.07, 0.09), CFI/TLI = 0.92, 0.74; SRMR = 0.11).
Study 5 Discussion
In Study 5, we tested our hypotheses in a sample of high-risk young adults who were active duty in the military, using a prospective study design. One strength of this study is the nature of the sample—acutely suicidal military service members who presented to inpatient psychiatry. Given the high rates of suicide-related symptoms among military service members, these findings are particularly useful for understanding severe suicide risk. Importantly, in contrast to Study 4, three-time-points were available in this study, strengthening our prospective findings.
Results from Study 5 partially supported our overall hypotheses. That is, consistent with our previous four studies, the relationship between perceived social problem-solving deficits and suicidal ideation was mediated by both thwarted belongingness and perceived burdensomeness cross-sectionally at all three time points, even after accounting for depression, age and sex. Depression, a robust suicide risk factor, was not a significant mediator. This underscores the specificity of the interpersonal theory variables as explanatory links. Individually, thwarted belongingness and perceived burdensomeness only partially accounted for the cross-sectional relationship between these variables. Again, cross-sectionally, the two-mediator model and the perceived burdensomeness-only model accounted for more variance in suicidal ideation than the thwarted belongingness-only model.
In contrast to Study 4, our longitudinal results indicated that only perceived burdensomeness was a significant mediator of the prospective relationship between perceived problem-solving deficits and suicidal ideation, not thwarted belongingness or both. Indeed, the model with perceived burdensomeness as an individual mediator exhibited excellent fit while the models with both mediators and only thwarted belongingness demonstrated poor to adequate fit. Given the military culture of community and comradery, which facilitates social connections among service members, one explanation for this pattern of findings is that feelings of social disconnection are not as marked in military settings. However, the military cultural ethos also emphasizes duty, mission, patriotism, and honor; thus, in contrast, feelings that one is a burden on one’s family, fellow soldiers, or even one’s country, may be particularly pernicious. An alternative and compatible explanation is that this finding is not limited to the military population and perceived burdensomeness is, in general, a more potent predictor of suicide risk, which is in line with recent studies in various samples (Bryan et al., 2010; Chu et al., 2016a; Ma et al., 2016). However, it is notable that in this sample, little overall variance in suicide risk was accounted for by our proposed predictors relative to Studies 1 to 4 and the cross-sectional results in this Study (R2 ~ 0.10 vs. R2 ~ 0.25–0.45). Further, after accounting for excess zeroes, results indicated non-significant relationships between all variables. This may indicate that among military service members, social problem-solving deficits may not be a particularly robust predictor of future suicidal ideation.
From a methodological and measurement perspective, the alternative operationalization of the interpersonal theory variables in Study 5 may provide a separate yet equally viable explanation for the lack of an observed relationship between these variables, and the differences from Study 4. Our use of pre-existing data limited our ability to specifically measure the constructs of thwarted belongingness and perceived burdensomeness utilizing a measure designed for that specific purpose (i.e., the INQ). On the other hand, we partially replicated results from Studies 1–4 using a distinct measurement approach. Future research among this high-risk population and others, using longitudinal designs and comparable assessment instruments, is needed to substantiate and clarify our findings.
Meta-Analysis of Cross-Sectional Results
To further consolidate the effects found across these five studies, we conducted meta-analyses of the effects of perceived social problem-solving deficits on thwarted belongingness, perceived burdensomeness, and suicidal ideation, and the indirect effects of thwarted belongingness and perceived burdensomeness on the cross-sectional relationship between perceived social problem-solving deficits and suicidal ideation from each sample. Given that only two longitudinal effects were available and of these, one relied on proxy measures of the interpersonal theory variables, we were underpowered to meta-analyze the longitudinal effect.
Methods
To examine the direct effects of perceived social problem-solving deficits on thwarted interpersonal needs and suicidal ideation, Pearson’s r bivariate correlations between perceived social problem-solving deficits, thwarted belongingness, perceived burdensomeness, and suicidal ideation were recorded for each study. Effect sizes were transformed to Fisher’s zs and weighted for the purpose of analysis, but the effect sizes presented were re-transformed to Pearson’s r for ease of interpretation.
Consistent with recommendations by Cheung and Cheung (2016), the two-stage meta-analytic structural equation modeling approach was used to examine the indirect effects. In the first stage, the correlation matrices were synthesized and the homogeneity of the correlation matrices was evaluated on the basis of the chi-square statistic and the goodness-of-fit indices. If the correlation matrices are homogenous, in the second stage, the pooled matrix is treated as the observed matrix and a mediational model is fitted to the matrix to evaluate model fit using MPlus.
To evaluate direct and indirect effects, random effects models were used as samples, design and effect sizes were expected to differ across studies and this approach allows for a greater degree of generalizability to other populations. Effect sizes were weighted, and we examined the significance of the Q-test to determine whether there was substantial heterogeneity of effect sizes. We also report the I2 statistic, which indicates how much of the variability across studies is due to heterogeneity as opposed to chance due to sampling error (0.25 = small heterogeneity; 0.50 = medium heterogeneity; 0.75 = large heterogeneity). Because we were underpowered to examine covariates as potential moderators across studies (Borenstein et al., 2009), no moderation analyses were conducted. Regarding dependent effect sizes, Study 5 reported multiple effects across time-points. To ensure that we were including the most conservative effects in our meta-analysis, we used only one effect from that sample (baseline).
Results
All effect sizes and 95% confidence intervals are presented in a forest plot (Figure 3). First, we examined the effect of perceived social problem-solving deficits on suicidal ideation. The heterogeneity was high for the total effect (p<0.001, I2 = 83.0%, Q = 23.5, N = 1044). The test of the null was significant, with a moderate-to-large effect size (r = 0.36, p<0.001, 95% CI [0.30, 0.42]; Figure 3A). This indicates that across these five cross-sectional studies, the association between perceived social problem-solving deficits and suicidal ideation is significant and moderate-to-large in magnitude. Next, we examined the effect of perceived social problem-solving deficits on thwarted belongingness. The heterogeneity was high for the total effect (p<0.001, I2 = 90.6%, Q = 42.5, N = 1044). The test of the null was significant, with a moderate-to-large effect size (r = 0.42, p<0.001, 95% CI [0.28, 0.56]; Figure 3B). Additionally, we examined the effect of perceived social problem-solving deficits on perceived burdensomeness. Effect sizes and 95% confidence intervals are presented in a forest plot (see Figure 3C). The heterogeneity was high for the total effect (p<0.001, I2 = 70.4%, Q = 13.5, N = 1044). The test of the null was significant, with a moderate-to-large effect size (r = 0.51, p<0.001, 95% CI [0.44, 0.58]; Figure 3C). Overall, this indicates that across these five studies, perceived social problem-solving deficits were significantly associated with suicidal ideation, thwarted belongingness, and perceived burdensomeness, and these associations were all moderate-to-large in magnitude.
Figure 3.
Forest plots of the Fisher’s z effect sizes [95% CI] of relationship between social problem solving deficits and (3A) suicidal ideation, (3B) thwarted belongingness, and (3C) perceived burdensomeness.
Finally, we examined the indirect effect of the interpersonal theory variables on the relationship between perceived social problem-solving deficits and suicidal ideation across the five studies. The pooled correlation matrices were homogenous (χ2(4) = 15.41, p < 0.001, RMSEA=0.024, CFI=0.89). The Q-test was significant (56.2), and the I2 value (89.1%) indicated that a large degree of variability was due to heterogeneity rather than chance. The test of the null was significant, with a moderate-to-large indirect effect size (b = 0.044, p < 0.001, 95% CI [0.025, 0.063]).
Discussion
These results further underscore the strength of the direct and indirect effects of thwarted belongingness and perceived burdensomeness on the relationship between perceived social problem-solving deficits and suicidal ideation. Findings emphasize the importance of examining and delineating this relationship. Perhaps most notably, our analyses included a number of distinct participant samples (military, community, and undergraduate populations). Despite demographic variations across samples, our effect sizes were moderate-to-large, highlighting the robustness of these effects. Although these analyses afforded us the opportunity to pool together findings across five studies, due to the lack of common covariate measures (i.e., dichotomous and continuous depressive symptom measures) and insufficient longitudinal data across studies, we were unable to examine the impact of covariates and longitudinal design in this study. Finally, as samples sizes were moderate in this manuscript, these results may be strengthened with the inclusion of more studies testing these relationships.
General Discussion
In this manuscript, we explored the relationship between perceived social problem-solving deficits, thwarted interpersonal needs, and suicidal ideation. Overall, our findings add to the growing body of research that implicates disrupted interpersonal functioning in the etiology of psychological disorders and suicidal ideation. For this reason, our results have significant scientific and clinical implications.
Importantly, this was the first study to call attention to the role of thwarted belongingness and perceived burdensomeness as important mechanisms of action between perceived social problem-solving deficits and suicidal ideation. Across five different studies, our meta-analytic and mediational findings reveal one consistent message—perceived social problem-solving deficits were associated with suicidal ideation, and this relationship may be explained by thwarted belongingness and perceived burdensomeness. Importantly, these different samples encompassed a broad spectrum of individuals who were demographically and clinically diverse with regard to their severity of suicide-related symptoms and mental health. This is notable as it implies that deficits in problem-solving ability not only negatively impact those who are vulnerable to psychiatric illnesses, but also the general population.
Consistent with the interpersonal theory of suicide, our results suggested that thwarted belongingness and perceived burdensomeness served as explanatory mechanisms. This result adds to the mounting research implicating these variables as mediators in the relationship between suicidal symptoms and risk factors, including non-suicidal self-injury and pain (e.g., Chu et al., 2016c; Hirsch, Cukrowicz, & Walker, 2016). Altogether, findings suggest thwarted belongingness and perceived burdensomeness are proximal risk factors for suicidal desire that account for the relationship between various distal risk factors, such as social problem-solving ability, and suicide risk.
Furthermore, we were not only able to replicate our findings cross-sectionally across samples, but we also extended support for our hypotheses by incorporating longitudinal study designs in Studies 4 and 5. Longitudinally, our findings were mixed: beyond depression, thwarted belongingness and perceived burdensomeness remained significant in Study 4’s primary care patient sample, and in Study 5’s military sample, only perceived burdensomeness was a significant mediator. It should be noted that cross-sectionally, across the five samples, the model with perceived burdensomeness as an individual mediator exhibited good to excellent fit and accounted for approximately the same amount of variance in our outcome variables as the model with both mediators. This further implies that perceived burdensomeness may be a more robust predictor of risk than thwarted belongingness. With the limited emphasis on the prospective relationship between perceived social problem-solving deficits and suicidal ideation (Speckens & Hawton, 2005) and recent reviews of the interpersonal theory corroborating Study 5 results (Ma et al., 2016), replication of the present longitudinal research will be vital for understanding the role of perceived burdensomeness and the discrepancy in our findings.
Our findings suggest that there may be a developmental or learning-based aspect to the interpersonal theory of suicide, in that social problem-solving ability develops across the lifespan and, perhaps, as a result of exposure to modeling (Blanchard-Fields, 2007; D’Zurilla & Nezu, 2010); thus, our results imply that long-term deficits in problem-solving ability may contribute to the vulnerability of perceiving thwarted interpersonal needs. It will be important to examine this model in adolescent and older adult samples to determine whether developmental changes in social problem-solving ability impact suicide risk over the lifespan. Having knowledge of potential precursors to thwarted interpersonal needs, as well as an understanding of the downstream risk-inducing or buffering effects of problem-solving deficits and capabilities, is important in prioritizing the development and implementation of successful interventions, and provides clinicians with therapeutic targets to effect change in their patients’ suicide risk.
As such, our results have clinical implications for suicide treatment and prevention efforts. First, our results provide further support for the utility of Problem-Solving Therapy, which may improve the ability to identify a salient problem, generate alternative solutions, and assess the efficacy of this solution (Ghahramanlou-Holloway et al., 2012; Stewart et al., 2009). When successfully applied, the ability to manage everyday problems, such as financial stress or relationship strain, may increase a patient’s self-efficacy, thereby reducing feelings of burdensomeness and decreasing suicide risk (Marks et al., 2005; McAuley et al., 2006; Robinson-Smith et al., 2000).
Given that thwarted belongingness and perceived burdensomeness may in part explain the relationship between perceived problem-solving deficits and suicide risk, treatments targeting both problem-solving deficits and interpersonal functioning would be useful needed. To target thwarted belongingness and perceived burdensomeness, Cognitive Behavioral Analysis Systems Psychotherapy or Cognitive-Behavioral Therapy (CBT) with adjunctive Behavioral Activation may be employed to help patients identify maladaptive or distorted cognitions that underlie feelings of isolation or perceptions of burden, and to strengthen social support networks (Beckner, Vella, Howard, & Mohr, 2010; McCullough, 2003; Stangier, Schramm, Heidenreich, Berger, & Clark, 2011). Alternatively, Interpersonal Therapy, which focuses on improving the quality of interpersonal relationships, may serve to decrease feelings of thwarted belongingness and perceived burdensomeness (Beckner et al., 2010; de Mello, de Jesus Mari, Bacaltchuk, Verdeli, & Neugebauer, 2005). These therapies are not only useful for improving social functioning but also for targeting suicide-related symptoms (e.g., brief CBT, Rudd et al., 2015; CBASP, Forkmann et al., 2016).
Our results suggest that a multi-orientation approach that simultaneously targets social problem-solving deficits and feelings of thwarted belongingness and perceived burdensomeness may be valuable for mitigating risk. This is particularly beneficial as treatment may be flexibly tailored to the patient, and clinicians, regardless of their clinical orientation, can therapeutically impact social functioning and problem-solving ability. For example, findings from the present study suggest that current suicide risk interventions could be augmented by a module or modules targeting social problem-solving deficits and interpersonal functioning. Further, these results are consistent with the growing research supporting the utility of increasing connectedness through peer support as an intervention for mental illness and suicide risk (e.g., Van Orden et al., 2013). On a population-wide scale, implementation of psychoeducational, social and problem-solving skills programs in schools and community centers may also prove useful for promoting mental health and preventing suicide. Indeed, public health is the cornerstone of suicide prevention (Knox et al., 2004), and as such, future research would benefit from understanding the relevance of our findings to public health promotion efforts. Nevertheless, findings from this single investigation, although replicated across five sample, cannot be used to definitively establish a public health promotion strategy. Here, too, we welcome further research in this domain.
Strengths, Limitations, and Future Directions
A notable strength of this multi-study manuscript was the use of a robust analytic approach to examine the relationship between problem-solving deficits, thwarted interpersonal needs, and suicidal ideation. Furthermore, the generalizability of our findings was bolstered by the inclusion of multiple vulnerable populations, including primary care, homeless, and military samples. Studies 4 and 5, in particular, allowed us to evaluate the prospective relationship between problem-solving deficits and suicidal ideation and to identify thwarted interpersonal needs as explanatory factors in this relationship.
Nonetheless, our novel results should be interpreted in the context of limitations. For one, the interpersonal theory posits that thwarted belongingness and perceived burdensomeness are proximal indictors of suicidal desire (Van Orden et al., 2010), the use of the SBQ-R in Studies 1, 3, and 4 limits our findings as this measure assesses suicidal ideation and behavior, not ideation specifically. Indeed, recent interpersonal theory studies (e.g., Chu et al., 2016a; under review) have highlighted this important limitation and it is therefore important for replication studies to use measures that are theoretically compatible. Relatedly, this study relied solely on self-report questionnaires, which, although necessary and useful in suicide-related research (Eyman & Eyman, 1990; Kaplan et al., 1994), may be subject to the influence of demand characteristics, such as social desirability. Therefore, underreporting of suicidal behavior may be a possibility. Future research using implicit measurements of suicidal ideation (e.g., implicit association test; Nock et al., 2010) will be useful for decreasing the impact of stigma and other related concerns, which may contribute to inaccurate or under reporting of symptoms. Additionally, in future studies, the inclusion of behavioral measures of social-problem solving ability would also be valuable as some participants have limited insight into their behaviors. To this end, the means-end problem-solving procedure (Platt, Spivack, & Bloom, 1971), a behavioral measure of problem-solving ability that has been used in previous studies of individuals at risk for suicide (Evans, Williams, O’Loughlin, & Howells, 2009), may be useful. Notably, consistent with the results of studies using self-report measures of problem-solving deficits, Evans and colleagues (2009) found that in comparison to controls, individuals with a history of suicidal behavior supplied fewer and less-effective problem-solving strategies.
It is crucial to note that our study models accounted for somewhat modest amounts of variance in suicide risk (e.g., R2 = 0.10–0.54), which may have in part been influenced by the aforementioned methodological limitations. It is also possible that other factors (e.g., low self-esteem) may also increase perceived problem-solving deficits. Thus, the examination of third variables will be valuable in future studies. Further, despite the diversity of samples included in this study, adolescent groups were not represented in this research. Therefore, in addition to replicating the present findings, future research testing these hypotheses in younger populations will be informative, particularly regarding the developmental trajectory of suicide-related behaviors. Moreover, this study did not test the full interpersonal theory of suicide predictions, which includes the interactive effects of thwarted belongingness and perceived burdensomeness, the roles of hopelessness regarding the tractability of thwarted belongingness and perceived burdensomeness and the capability for suicide. Therefore, future research examining the role of deficits in problem-solving ability in the etiology of suicidal behaviors should consider the role of these important theoretical variables.
Overall, the current studies provide evidence for the impact of thwarted interpersonal needs on the relationship between perceived social problem-solving deficits and suicide-related behaviors in five samples. Given that our results highlight a potential mechanism by which deficits in problem-solving ability and suicidal ideation may be linked, our findings offer targets for intervention. For clinicians in psychiatric and medical settings working with patients at risk for suicide, therapeutically enhancing problem-solving ability and bolstering feelings of competence and connectedness may help to minimize current and future suicide risk.
Acknowledgments
This research was supported, in part, by a grant from the National Institute of Mental Health (T32 MH093311-04). This work was also supported by the Military Suicide Research Consortium (MSRC), an effort supported by the Office of the Assistant Secretary of Defense for Health Affairs under Award No. (W81XWH-10-2-0181). Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the MSRC or the Department of Defense.
Footnotes
Suicide risk refers to both symptoms of suicidal ideation and behavior.
References
- American College Health Association. American College Health Association-National College Health Assessment Spring 2008 Reference Group Data Report (abridged): the American College Health Association. Journal of American College Health. 2009;57(5):477. doi: 10.3200/JACH.57.5.477-488. [DOI] [PubMed] [Google Scholar]
- Batterham PJ, Calear AL, Spijker BA. The Specificity of the Interpersonal-Psychological Theory of Suicidal Behavior for Identifying Suicidal Ideation in an Online Sample. Suicide and Life-Threatening Behavior. 2015;45(4):448–460. doi: 10.1111/sltb.12140. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, Leary MR. The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Psychological Bulletin. 1995;117(3):497. [PubMed] [Google Scholar]
- Beautrais AL. Suicides and serious suicide attempts: two populations or one? Psychological Medicine. 2001;31(05):837–845. doi: 10.1017/s0033291701003889. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio TX: Psychological Corporation; 1996. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Becker-Weidman EG, Jacobs RH, Reinecke MA, Silva SG, March JS. Social problem-solving among adolescents treated for depression. Behaviour Research and Therapy. 2010;48(1):11–18. doi: 10.1016/j.brat.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckner V, Howard I, Vella L, Mohr DC. Telephone-administered psychotherapy for depression in MS patients: Moderating role of social support. Journal of Behavioral Medicine. 2010;33(1):47–59. doi: 10.1007/s10865-009-9235-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard-Fields F. Everyday problem solving and emotion: An adult developmental perspective. Current Directions in Psychological Science. 2007;16(1):26–31. [Google Scholar]
- Brislin SJ, Buchman-Schmitt JM, Joiner TE, Patrick CJ. “Do unto others”? Distinct psychopathy facets predict reduced perception and tolerance of pain. Personality Disorders: Theory, Research, and Treatment. 2016;7(3):240. doi: 10.1037/per0000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA. Confirmatory Factor Analysis for Applied Research. New York: Guilford Press; 2006. [Google Scholar]
- Bryan CJ, Rudd MD. The importance of temporal dynamics in the transition from suicidal thought to behavior. Clinical Psychology: Science and Practice. 2016;23(1):21–25. [Google Scholar]
- Bryan CJ, Morrow CE, Anestis MD, Joiner TE. A preliminary test of the interpersonal-psychological theory of suicidal behavior in a military sample. Personality and Individual Differences. 2010;48(3):347–350. [Google Scholar]
- Buchman-Schmitt JM, Brislin SJ, Venables NC, Joiner TE, Patrick CJ. Trait liabilities and specific promotive processes in psychopathology: The example of suicidal behavior. Journal of Afffective Disorders. 2016 doi: 10.1016/j.jad.2016.09.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) National Suicide Statistics at a Glance. 2015 http://www.cdc.gov/violenceprevention/suicide/
- Chang EC, Hirsch JK. Social problem solving under assault: Understanding the impact of sexual assault on the relation between social problem solving and suicidal risk in female college students. Cognitive Therapy and Research. 2015;39(3):403–413. [Google Scholar]
- Chang EC, Jilani Z, Yu T, Fowler E, Lin J, Webb JR, Hirsch JK. Fundamental dimensions of personality underlying spirituality: Further evidence for the construct validity of the RiTE measure of spirituality. Personality and Individual Differences. 2015a;75:175–178. [Google Scholar]
- Chang EC, Jilani Z, Fowler E, Yu T, Chia SW, Yu E, McCabe H, Hirsch JK. Relations between multidimensional spirituality and depressive symptoms in adults: Examining hope agency and pathways as potential mediators. Journal of Positive Psychology 2015b [Google Scholar]
- Chang EC, Lee J, Stam KR, Batterbee CN-H, Chang OD, Morris LE, Lucas AG, Yu T, Hirsch JK. A preliminary examination of negative life events and sexual assault victimization as predictors of psychological functioning in female college students: Is one more important than the other? Journal of Interpersonal Violence. 2017a doi: 10.1177/0886260517719901. [DOI] [PubMed] [Google Scholar]
- Chang EC, Yu T, Chang OD, Lee J, Stam KR, Lucas AG, Batterbee CN-H, Morris LE, Li X, Hirsch JK. Trauma under control: Does personal control moderate the relationship between trauma history and suicidal risk in college students? Journal of American College Health 2017b [Google Scholar]
- Chang EC, Yu T, Yu E, Chia S, Jilani Z, McCabe H, Hirsch JK. Hope under assault: Understanding the impact of sexual assault on the relation between hope and suicidal risk in college students. Journal of Social and Clinical Psychology. 2015c;34(3):221–238. [Google Scholar]
- Chang EC, Watkins AF, Banks KH. How adaptive and maladaptive perfectionism relate to positive and negative psychological functioning: Testing a stress-mediation model in black and white female college students. Journal of Counseling Psychology. 2004;51:93–102. [Google Scholar]
- Cheung MWL, Cheung SF. Random-effects models for meta-analytic structural equation modeling: review, issues, and illustrations. Research Synthesis Methods. 2016;7(2):140–155. doi: 10.1002/jrsm.1166. [DOI] [PubMed] [Google Scholar]
- Christensen H, Batterham PJ, Soubelet A, Mackinnon AJ. A test of the Interpersonal Theory of Suicide in a large community-based cohort. Journal of Affective Disorders. 2013;144(3):225–234. doi: 10.1016/j.jad.2012.07.002. [DOI] [PubMed] [Google Scholar]
- Chu C, Buchman-Schmitt JM, Joiner TE. Autobiographical memory perspectives in task and suicide attempt recall: A study of young adults with and without symptoms of suicidality. Cognitive Therapy and Research. 2015a;39(6):766–775. [Google Scholar]
- Chu C, Buchman-Schmitt JM, Hom MA, Stanley IH, Joiner TE. A test of the interpersonal theory of suicide in a large sample of current firefighters. Psychiatry Research. 2016a;240:26–33. doi: 10.1016/j.psychres.2016.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu C, Buchman-Schmitt JM, Moberg FB, Joiner TE. Thwarted belongingness mediates the relationship between fear of negative evaluation and suicidal ideation. Cognitive Therapy and Research. 2015b;40(1):31–37. doi: 10.1007/s10608-015-9715-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu C, Buchman-Schmitt JM, Joiner TE, Rudd MD. personality disorder symptoms and suicidality: Low desire and high plans for suicide in military inpatients and outpatients. Journal of Personality Disorders. 2016b:1–11. doi: 10.1521/pedi_2016_30_241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu C, Hom MA, Rogers ML, Stanley IH, Ringer-Moberg FB, Podlogar MC, … Joiner TE. Insomnia and suicide-related behaviors: A multi-study investigation of thwarted belongingness as a distinct explanatory factor. Journal of Affective Disorders. 2017;208:153–162. doi: 10.1016/j.jad.2016.08.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu C, Rogers ML, Joiner TE. Cross-sectional and temporal association between non-suicidal self-injury and suicidal ideation in young adults: The explanatory roles of thwarted belongingness and perceived burdensomeness. Psychiatry Research. 2016c doi: 10.1016/j.psychres.2016.07.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cull JG, Gill WS. Suicide probability scale (SPS) manual. Los Angeles: Western Psychological Services; 1988. [Google Scholar]
- Deci EL, Ryan RM. Self-determination theory. In: Van Lange PM, Kruglanski AW, Higgins E, editors. Handbook of theories of social psychology. Vol. 1. Thousand Oaks, CA: Sage Publications Ltd; 2012. pp. 416–436. [Google Scholar]
- de Mello M, de Jesus Mari J, Bacaltchuk J, Verdeli H, Neugebauer R. A systematic review of research findings on the efficacy of interpersonal therapy for depressive disorders. European Archives of Psychiatry and Clinical Neuroscience. 2005;255(2):75–82. doi: 10.1007/s00406-004-0542-x. [DOI] [PubMed] [Google Scholar]
- Dixon WA, Heppner PP, Rudd MD. Problem-solving appraisal, hopelessness, and suicide ideation: Evidence for a mediational model. Journal of Counseling Psychology. 1994;41(1):91–98. [Google Scholar]
- D’Zurilla TJ, Nezu AM. Problem-solving therapy. In: Dobson KS, editor. Handbook of Cognitive-Behavioral Therapies. 3. New York, NY: Guilford Press; 2010. pp. 197–225. [Google Scholar]
- D’Zurilla T, Nezu AM, Maydeu-Olivares A. Social Problem Solving Inventory – Revised: Technical manual. North Tonawanda, NY: Multi-Health Systems; 2002. [Google Scholar]
- Ellis TE, Rutherford B. Cognition and suicide: Two decades of progress. International Journal of Cognitive Therapy. 2008;1(1):47–68. [Google Scholar]
- Evans J, Williams JMG, O’Loughlin S, Howells K. Autobiographical memory and problem-solving strategies of parasuicide patients. Psychological Medicine. 1992;22(02):399–405. doi: 10.1017/s0033291700030348. [DOI] [PubMed] [Google Scholar]
- Eyman JR, Eyman SK. Suicide risk and assessment instruments. In: Cimbolic P, Jobes DA, editors. Youth suicide: Issues, assessment, and intervention. Springfield, IL: Charles C. Thomas; 1990. pp. 9–32. [Google Scholar]
- Forkmann T, Brakemeier EL, Teismann T, Schramm E, Michalak J. The Effects of Mindfulness-Based Cognitive Therapy and Cognitive Behavioral Analysis System of Psychotherapy added to Treatment as Usual on suicidal ideation in chronic depression: Results of a randomized-clinical trial. Journal of Affective Disorders. 2016;200:51–57. doi: 10.1016/j.jad.2016.01.047. [DOI] [PubMed] [Google Scholar]
- Fritz MS, MacKinnon DP. Required sample size to detect the mediated effect. Psychological science. 2007;18(3):233–239. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghahramanlou-Holloway MM, Bhar SS, Brown GK, Olsen CC, Beck AT. Changes in problem-solving appraisal after cognitive therapy for the prevention of suicide. Psychological Medicine. 2012;42(6):1185–1193. doi: 10.1017/S0033291711002169. [DOI] [PubMed] [Google Scholar]
- Hagan CR, Podlogar MC, Chu C, Joiner TE. Testing the interpersonal theory of suicide: The moderating role of hopelessness. International Journal of Cognitive Therapy. 2015;8(2):99–113. [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY US: Guilford Press; 2013. [Google Scholar]
- Heppner PP. The problem solving inventory: Manual. Palo Alto, CA: Consulting Psychologists Press; 1988. [Google Scholar]
- Heppner PP, Petersen CH. The development and implications of a personal problem-solving inventory. Journal of Counseling Psychology. 1982;29(1):66–75. [Google Scholar]
- Hirsch JK, Chang EC, Jeglic EL. Social problem solving and suicidal behavior: Ethnic differences in the moderating effects of loneliness and life stress. Archives of Suicide Research. 2012;16(4):303–315. doi: 10.1080/13811118.2013.722054. [DOI] [PubMed] [Google Scholar]
- Hirsch JK, Cukrowicz KC, Walker KL. Pain and Suicidal Behavior in Primary Care Patients: Mediating Role of Interpersonal Needs. International Journal of Mental Health and Addiction. 2016:1–11. [Google Scholar]
- Hom MA, Chu C, Schneider ME, Lim IC, Hirsch JK, Gutierrez PM, Joiner TE. Thwarted belongingness as an explanatory link between insomnia symptoms and suicidal ideation: Findings from three samples of military service members and veterans. Journal of Affective Disorders. 2017;209:114–123. doi: 10.1016/j.jad.2016.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling: a multidisciplinary journal. 1999;6(1):1–55. [Google Scholar]
- Hwang SW, Kirst MJ, Chiu S, Tolomiczenko G, Kiss A, Cowan L, Levinson W. Multidimensional social support and the health of homeless individuals. Journal of Urban Health. 2009;86(5):791–803. doi: 10.1007/s11524-009-9388-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner TE., Jr . Why people die by suicide. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- Joiner TE, Jr, Pettit JW, Perez M, Burns AB, Gencoz T, Gencoz F, Rudd MD. Can positive emotion influence problem-solving attitudes among suicidal adults? Professional Psychology: Research and Practice. 2001;32(5):507–512. [Google Scholar]
- Joiner TE, Pfaff JJ, Acres JG. A brief screening tool for suicidal symptoms in adolescents and young adults in general health settings: reliability and validity data from the Australian National General Practice Youth Suicide Prevention Project. Behaviour Research and Therapy. 2002;40(4):471–481. doi: 10.1016/s0005-7967(01)00017-1. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Jr, Rudd MD. Intensity and duration of suicidal crisis vary as a function of previous suicide attempts and negative life events. Journal of Consulting and Clinical Psychology. 2000;68(5):909. doi: 10.1037/0022-006X.68.5.909. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Jr, Rudd MD, Rajab MH. The Modified Scale for Suicidal Ideation: Factors of suicidality and their relation to clinical and diagnostic variables. Journal of Abnormal Psychology. 1997;106(2):260. doi: 10.1037//0021-843x.106.2.260. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Jr, Van Orden KA, Witte TK, Selby EA, Ribeiro JD, Lewis R, Rudd MD. Main predictions of the interpersonal–psychological theory of suicidal behavior: Empirical tests in two samples of young adults. Journal of Abnormal Psychology. 2009;118(3):634–646. doi: 10.1037/a0016500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner TE, Jr, Vohs KD, Rudd MD, Schmidt NB, Pettit JW. Problem-solving and cognitive scars in mood and anxiety disorders: The sting of mania. Journal of Social and Clinical Psychology. 2003;22(2):192–212. [Google Scholar]
- Kaplan ML, Asnis GM, Sanderson WC, Keswani L, DeLecuona JM, Joseph S. Suicide assessment: Clinical interview vs. self-report. Journal of Clinical Psychology. 1994;50:294–298. doi: 10.1002/1097-4679(199403)50:2<294::aid-jclp2270500224>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Knox KL, Conwell Y, Caine ED. If suicide is a public health problem, what are we doing to prevent it? American Journal of Public Health. 2004;94(1):37–45. doi: 10.2105/ajph.94.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kremers IP, Spinhoven P, Van der Does AJW, Van Dyck R. Social problem solving, autobiographical memory and future specificity in outpatients with borderline personality disorder. Clinical Psychology & Psychotherapy. 2006;13(2):131–137. [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lui ML, Lee DF, Greenwood N, Ross FM. Informal stroke caregivers’ self-appraised problem-solving abilities as a predictor of well-being and perceived social support. Journal of Clinical Nursing. 2012;21(1–2):232–242. doi: 10.1111/j.1365-2702.2011.03742.x. [DOI] [PubMed] [Google Scholar]
- Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. American Journal of Psychiatry. 2002;159(6):909–916. doi: 10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma J, Batterham PJ, Calear AL, Han J. A systematic review of the predictions of the Interpersonal-Psychological Theory of Suicidal Behavior. Clinical Psychology Review. 2016;46:34–45. doi: 10.1016/j.cpr.2016.04.008. [DOI] [PubMed] [Google Scholar]
- Maric M, Wiers RW, Prins PJ. Ten ways to improve the use of statistical mediation analysis in the practice of child and adolescent treatment research. Clinical Child and Family Psychology review. 2012;15(3):177–191. doi: 10.1007/s10567-012-0114-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks R, Allegrante JP, Lorig K. A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: Implications for health education practice (Part ii) Health Promotion Practice. 2005;6(2):148–156. doi: 10.1177/1524839904266792. [DOI] [PubMed] [Google Scholar]
- Maydeu-Olivares A, D’Zurilla TJ. A factor-analytic study of the social problem-solving inventory: An integration of theory and data. Cognitive Therapy and Research. 1997;20(2):115–133. [Google Scholar]
- McAuliffe C, Corcoran P, Keeley H, Arensman E, Bille-Brahe U, de Leo D, et al. Problem-solving ability and repetition of deliberate self-harm: A multicentre study. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 2006;36(1):45–55. doi: 10.1017/S0033291705005945. [DOI] [PubMed] [Google Scholar]
- McCullough JP. Treatment for chronic depression using cognitive behavioral analysis system of psychotherapy (CBASP) Journal of Clinical Psychology. 2003;59(8):833–846. doi: 10.1002/jclp.10176. [DOI] [PubMed] [Google Scholar]
- McLaughlin J, Miller P, Warwick H. Deliberate self-harm in adolescents: Hopelessness, depression, problems and problem-solving. Journal of Adolescence. 1996;19(6):523–532. doi: 10.1006/jado.1996.0051. [DOI] [PubMed] [Google Scholar]
- Metalsky GI, Joiner TE., Jr The hopelessness depression symptom questionnaire. Cognitive Therapy and Research. 1997;21(3):359–384. [Google Scholar]
- Miller IW, Norman WH, Bishop SB, Dow MG. The Modified Scale for Suicidal Ideation: reliability and validity. Journal of Consulting and Clinical Psychology. 1986;54(5):724–725. doi: 10.1037//0022-006x.54.5.724. [DOI] [PubMed] [Google Scholar]
- Muyan M, Chang EC, Jilani Z, Yu T, Lin J, Hirsch JK. Loneliness and negative affective conditions in adults: Is there any room for hope in predicting anxiety and depressive symptoms? Journal of Psychology:Interdisciplinary and Applied. 2015 doi: 10.1080/00223980.2015.1039474. [DOI] [PubMed] [Google Scholar]
- Nock MK, Park JM, Finn CT, Deliberto TL, Dour HJ, Banaji MR. Measuring the suicidal mind implicit cognition predicts suicidal behavior. Psychological Science. 2010;21:511–517. doi: 10.1177/0956797610364762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman A, Bagge C, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): Validation with clinical and nonclinical samples. Assessment. 2001;8:443–454. doi: 10.1177/107319110100800409. [DOI] [PubMed] [Google Scholar]
- Platt JJ, Spivack G, Bloom M. Means-end problem-solving procedure (MEPS): Manual and tentative norms. Philadelphia: Department of Mental Health Sciences, Hahnemann Medical College and Hospital; 1971. [Google Scholar]
- Pollock LR, Williams JMG. Problem-solving in suicide attempters. Psychological Medicine. 2004;34(1):163–167. doi: 10.1017/s0033291703008092. [DOI] [PubMed] [Google Scholar]
- Prigerson HG, Desai RA, Liu-Mares W, Rosenheck RA. Suicidal ideation and suicide attempts in homeless mentally ill persons. Social Psychiatry and Psychiatric Epidemiology. 2003;38(4):213–219. doi: 10.1007/s00127-003-0621-8. [DOI] [PubMed] [Google Scholar]
- Robison-Smith G, Johnston MV, Allen J. Self care self-efficacy, quality of life, and depression after stroke. Archives of Physical Medicine and Rehabilitation. 2000;81(4):460–464. doi: 10.1053/mr.2000.3863. [DOI] [PubMed] [Google Scholar]
- Roškar S, Zorko M, Bucik V, Marušič A. Problem solving for depressed suicide attempters and depressed individuals without suicide attempt. Psychiatria Danubina. 2007;19(4):296–302. [PubMed] [Google Scholar]
- Rudd MD, Bryan CJ, Wertenberger EG, Peterson AL, Young-McCaughan S, Mintz J, … Wilkinson E. Brief cognitive-behavioral therapy effects on post-treatment suicide attempts in a military sample: results of a randomized clinical trial with 2-year follow-up. American Journal of Psychiatry. 2015;172(5):441–449. doi: 10.1176/appi.ajp.2014.14070843. [DOI] [PubMed] [Google Scholar]
- Rudd MD, Joiner T, Rajab M. Relationships among suicide ideators, attempters, and multiple attempters in a young-adult sample. Journal of Abnormal Psychology. 1996;105:541–550. doi: 10.1037//0021-843x.105.4.541. [DOI] [PubMed] [Google Scholar]
- Rudd MD, Joiner TE, Rumzek H. Childhood diagnoses and later risk for multiple suicide attempts. Suicide and Life-Threatening Behavior. 2004;34(2):113–125. doi: 10.1521/suli.34.2.113.32784. [DOI] [PubMed] [Google Scholar]
- Rudd MD, Rajab MH, Dahm PF. Problem-solving appraisal in suicide ideators and attempters. American Journal of Orthopsychiatry. 1994;64(1):136–149. doi: 10.1037/h0079492. [DOI] [PubMed] [Google Scholar]
- Rudd MD, Rajab MH, Orman DT, Stulman DA, Joiner T, Dixon W. Effectiveness of an outpatient intervention targeting suicidal young adults: Preliminary results. Journal of Consulting and Clinical Psychology. 1996;64(1):179–190. doi: 10.1037//0022-006x.64.1.179. [DOI] [PubMed] [Google Scholar]
- Shneidman ES. The logic of suicide. In: Shneidman E, Farberow N, editors. Clues to suicide. New York: McGraw-Hill; 1957. pp. 31–40. [Google Scholar]
- Speckens AE, Hawton K. Social problem solving in adolescents with suicidal behavior: A systematic review. Suicide and Life-Threatening Behavior. 2005;35(4):365–387. doi: 10.1521/suli.2005.35.4.365. [DOI] [PubMed] [Google Scholar]
- Stangier U, Schramm E, Heidenreich T, Berger M, Clark DM. Cognitive therapy versus interpersonal psychotherapy in social anxiety disorder: A randomized controlled trial. Archives of General Psychiatry. 2011;68(7):692–700. doi: 10.1001/archgenpsychiatry.2011.67. [DOI] [PubMed] [Google Scholar]
- Stanley IH, Hom MA, Rogers ML, Hagan CR, Joiner TE. Understanding suicide among older adults: A review of psychological and sociological theories of suicide. Aging & Mental Health. 2016;20(2):113–122. doi: 10.1080/13607863.2015.1012045. [DOI] [PubMed] [Google Scholar]
- Stewart CD, Quinn A, Plever S, Emmerson B. Comparing cognitive behavior therapy, problem solving therapy, and treatment as usual in a high-risk population. Suicide and Life-Threatening Behavior. 2009;39(5):538–547. doi: 10.1521/suli.2009.39.5.538. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Cukrowicz KC, Witte TK, Joiner TE. Thwarted belongingness and perceived burdensomeness: Construct validity and psychometric properties of the Interpersonal Needs Questionnaire. Psychological Assessment. 2012;24(1):197–215. doi: 10.1037/a0025358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Stone DM, Rowe J, McIntosh WL, Podgorski C, Conwell Y. The Senior Connection: design and rationale of a randomized trial of peer companionship to reduce suicide risk in later life. Contemporary Clinical Trials. 2013;35(1):117–126. doi: 10.1016/j.cct.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr The Interpersonal Theory of Suicide. Psychological Review. 2010;117(2):575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Gordon KH, Bender TW, Joiner TE., Jr Suicidal desire and the capability for suicide: tests of the interpersonal-psychological theory of suicidal behavior among adults. Journal of Consulting and Clinical Psychology. 2008;76(1):72–83. doi: 10.1037/0022-006X.76.1.72. [DOI] [PubMed] [Google Scholar]
- Walker KL, Chang EC, Hirsch JK. Neuroticism and suicidal behavior: Conditional indirect effects of social problem solving and hopelessness. International Journal of Mental Health and Addiction (in press) [Google Scholar]
- Wenzel A, Brown GK, Beck AT. Cognitive therapy for suicidal patients: Scientific and clinical applications. American Psychological Association; 2009. [Google Scholar]
- Witte TK, Joiner TE. Convergent Validity of SPS items. 2008 Unpublished raw data. [Google Scholar]
- Wolf EJ, Harrington KM, Clark SL, Miller MW. Sample size requirements for structural equation models an evaluation of power, bias, and solution propriety. Educational and Psychological Measurement. 2013;73(6):913–934. doi: 10.1177/0013164413495237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfensberger W. A brief overview of social role valorization. Mental Retardation. 2000;38(2):105–123. doi: 10.1352/0047-6765(2000)038<0105:ABOOSR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]