Abstract
BACKGROUND
Maternal mortality ratios (MMR) appear to have increased in the United States over the last decade. Three potential contributing factors are (1) a shifting maternal age distribution, (2) changes in age-specific MMR, and (3) the addition of a checkbox indicating recent pregnancy on the death certificate.
OBJECTIVE
To determine the contribution of increasing maternal age on changes in MMR from 1978 to 2012 and estimate the contribution of the pregnancy checkbox on increases in MMR over the last decade.
STUDY DESIGN
Kitagawa decomposition analyses were conducted to partition the maternal age contribution to the MMR increase into 2 components: changes due to a shifting maternal age distribution and changes due to greater age-specific mortality ratios. We used National Vital Statistics System natality and mortality data. The following 5-year groupings were used: 1978–1982, 1988–1992, 1998–2002, and 2008–2012. Changes in age-specific MMRs among states that adopted the standard pregnancy checkbox onto their death certificate before 2008 (n = 23) were compared with states that had not adopted the standard pregnancy checkbox on their death certificate by the end of 2012 (n = 11) to estimate the percentage increase in the MMR due to the pregnancy checkbox.
RESULTS
Overall US MMRs for 1978–1982, 1988–1992, and 1998–2002 were 9.0, 8.1, and 9.1 deaths per 100,000 live births, respectively. There was a modest increase in the MMR between 1998–2002 and 2008–2012 in the 11 states that had not adopted the standard pregnancy checkbox on their death certificate by the end of 2012 (8.6 and 9.9 deaths per 100,000, respectively). However, the MMR more than doubled between 1998–2002 and 2008–2012 in the 23 states that adopted the standard pregnancy checkbox (9.0–22.4); this dramatic increase was almost entirely attributable to increases in age-specific MMRs (94.9%) as opposed to increases in maternal age (5.1%), with an estimated 90% of the observed change reflecting the change in maternal death identification rather than a real change in age-specific rates alone. Of all age categories, women ages 40 and older in states that adopted the standard pregnancy checkbox had the largest increase in MMR—from 31.9 to 200.5—a relative increase of 528%, which accounted for nearly one third of the overall increase. An estimated 28.8% of the observed change was potentially due to maternal death misclassification among women ≥ 40 years.
CONCLUSION
Increasing age-specific maternal mortality seems to be contributing more heavily than a changing maternal age distribution to recent increases in MMR. In states with the standard pregnancy checkbox, the vast majority of the observed change in MMR over the last decade was estimated to be due to the pregnancy checkbox, with the greatest change in MMR occurring in women ages ≥ 40 years. The addition of a pregnancy checkbox on state death certificates appears to be increasing case identification but also may be leading to maternal death misclassification, particularly for women ages ≥ 40 years.
Keywords: maternal age, maternal mortality, pregnancy, United States, vital statistics
Introduction
A national maternal mortality ratio (MMR) has not been reported since 2007 due to known differences in maternal death identification between states with and without a pregnancy checkbox. However, the United States is 1 of only 8 countries to have experienced increases in estimated MMRs over the last decade.1 Recent increases in the MMR were preceded by a period of rapid decline throughout most of the 20th century and a relatively stable MMR in the late 20th century and at the turn of the 21st century.2,3 Complete reasons for the recent increases in MMR remain unclear. Three potential contributing factors are (1) a shifting maternal age distribution, with an increasing number of older and therefore “greater-risk” women giving birth; (2) changes in age-specific MMR; and (3) the addition of a question asking about recent pregnancy status on the death certificate, resulting in increased maternal death identification.
The percentage of all births occurring among women age 35 years or older has increased from 5% in 1980 to 15% in 2012.4,5 Maternal morbidity and mortality rates increase with advanced maternal age, due in part to increased prevalence of chronic conditions (eg, hypertension, diabetes, and chronic heart disease).2,6–8 A pregnancy check-box was added to the US Standard Certificate of Death in 2003 to improve identification of maternal deaths.9 The pregnancy checkbox prompts the certifier to indicate recent pregnancy status and the time between pregnancy and death, allowing delineation of deaths while pregnant or within 42 days of pregnancy (Figure 1). Adoption of the pregnancy checkbox has varied by states, both in timing of checkbox adoption on the state death certificate and in the wording of the checkbox categories.
FIGURE 1. Pregnancy checkbox from the United States standard certificate of death.
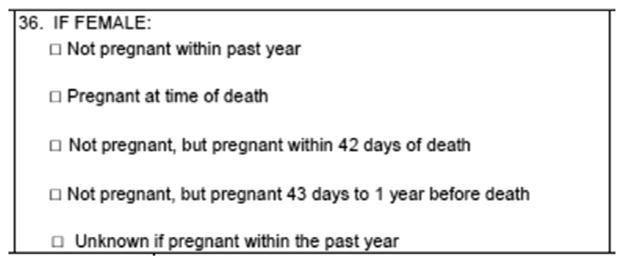
The pregnancy checkbox obtains information on whether a female decedent was not pregnant within the past year, pregnant at the time of death, pregnant within 42 days of death, pregnant between 43 days and 1 year of death, or unknown if pregnant within the past year. This information is used in combination with text written in the cause-of-death statement when coding cause of death for women 10–54 years of age. When the text in the cause-of-death statement does not specify the pregnancy (eg, hypertension) or the timeframe, pregnancy-related information in the checkbox will identify maternal deaths.
Davis et al. Maternal age and maternal mortality, United States. Am J Obstet Gynecol 2017.
Changes in MMR can be caused by changes in mortality risk across the population or changes in the distribution of subgroups with variable risk. We used natality and mortality data from the National Vital Statistics System to estimate the contribution of a shifting maternal age distribution compared with shifts in age-specific rates of maternal mortality, on changes in MMR over the last 3 decades. Lastly, we assessed the extent to which the increase in MMR over the last decade could be due to increased maternal death identification resulting from the pregnancy checkbox by comparing the change for states with and without checkbox adoption. A better understanding of the reasons for increases in MMR over the last decade could help guide public health policy and program decisions.
Materials and Methods
Data are from the National Center for Health Statistics natality and mortality files for the following time periods, where the midpoint of each is the decade start: 1978–1982, 1988–1992, 1998–2002, and 2008–2012. Five-year groupings were used due to the relatively small number of annual maternal deaths. For 2008–2012, we present MMRs for states that adopted the standard pregnancy checkbox onto their death certificate before 2008 (n = 23) and states that had not adopted the standard pregnancy checkbox on their death certificate by the end of 2012 (n = 11). States that either adopted the standard pregnancy checkbox between 2008 and 2012, or that adopted a pregnancy checkbox that differed from the standard, were excluded to prevent mixing of effects. Natality and mortality files for all years from 2000 to 2012 were used to assess the contribution of the pregnancy checkbox to changes in MMR (methods described below). Access to the state identifier was provided through the National Association for Public Health Statistics and Information Systems approval process.
All women who delivered a live birth and all maternal deaths in the United States during the aforementioned time periods were included. MMRs are presented as maternal deaths per 100,000 live births. Maternal deaths were defined by use of the World Health Organization’s criteria: “death of a woman while pregnant or within 42 days after the termination of gestation, irrespective of the duration and site of pregnancy,” where the cause-of-death codes on the death certificate were identified as complications of pregnancy, childbirth, and the puerperium in World Health Organization’s International Classification of Diseases (ICD).10 ICD versions 8–10 were used as applicable. ICD version 8 was used for 1978 and included codes 630–678, version 9 was used for 1979–1998 and included codes 630–676, and version 10 for 1999–2012 including codes A34, O00–O95, and O98–O99.10,11 ICD revisions can create breaks in the comparability of MMRs between years due to changes and additions in cause-of-death titles, and comparability ratios have been estimated to represent the net effect of each revision on cause-of-death statistics.12,13 We did not incorporate comparability ratios in our analyses because the year groupings only included 1 year from a previous ICD version and was therefore not thought to alter our overall conclusions.
Kitagawa decomposition analyses14 were used to partition the contribution of maternal age to changes in MMR from, for example, 1998–2002 to 2008–2012 into 2 components: (1) the amount due to a shifting maternal age distribution and (2) the amount due to changing age-specific mortality ratios.14 Any rate or ratio, including MMR, can be considered the product of the percentage distribution of a factor (ie, maternal age) and factor-specific ratios (ie, maternal age-specific MMRs). By use of the formula developed by Kitagawa and commonly used in perinatal epidemiology,15,16 a difference in 2 rates or MMRs, where R1 is the MMR in 1998–2002 and R2 is the MMR in 2008–2012, can be reexpressed and partitioned into differences in the distribution of maternal age and maternal age-specific MMRs.
The distributional component is determined by multiplying the difference in the proportion of births in an age-specific category (i) between 2 time periods (P2i − P1i) by the average age-specific . It is analogous to direct standardization, wherein a different age distribution is applied holding age-specific rates constant, and yields the difference in rates over time attributable to distributional changes in maternal age. The ratio component is determined by multiplying the difference in age-specific MMRs between 2 time periods by the average age-specific proportion of births. It is analogous to indirect standardization, wherein a different age-specific mortality rate is applied holding maternal age distribution constant, and yields the difference in rates over time attributable to changes in age-specific mortality rates. Live births and maternal deaths were grouped into the following maternal age categories: <20, 20–24, 25–29, 30–34, 35–39, and ≥40 years. The sum of the 2 components over all maternal age categories (i) indicates the total MMR difference due to distributional changes and age-specific mortality changes, respectively. These 2 summed components total to the overall difference in MMRs over time.
We assessed the contribution of maternal age to increasing MMR in 2008–2012 vs 1998–2002 among states that adopted the standard pregnancy checkbox onto their death certificate before 2008 separately from states that had not adopted the standard pregnancy checkbox on their death certificate by the end of 2012, to assess the change in methodology. For states that implemented the standard pregnancy check-box by 2010, age-specific MMRs for the 3 years before standard pregnancy checkbox implementation were compared with age-specific MMRs for the 3 years after implementation, excluding implementation year. Applying the relative increase in age-specific MMR between 1998–2002 and 2008–2012 from states that did not adopt the standard pregnancy checkbox by 2008, to states that adopted the standard pregnancy checkbox by 2012, we estimated the expected total and age-specific MMRs for the pregnancy checkbox states if the pregnancy check-box had not been added to death certificates. We then estimated the increase in MMR from 2008 to 2012 compared with 1998–2002 due to the pregnancy checkbox alone, using both checkbox comparison strategies.
Results
Overall US MMRs for 1978–1982, 1988–1992, and 1998–2002 were 9.0, 8.1, and 9.1 deaths per 100,000 live births, respectively. For 2008–2012, the MMR was 9.9 and 22.4 deaths per 100,000 live births in states that had not adopted the standard pregnancy check-box on their death certificate by the end of 2012 (n = 11) and states that adopted the standard pregnancy checkbox onto their death certificate before 2008 (n = 23), respectively. The change in MMR between 1998–2002 and 2008–2012 among states that implemented the standard pregnancy check-box before 2008 corresponds to a relative increase of 150% or an absolute increase of 13.4 deaths per 100,000 live births over one decade.
The percent of live births born to women younger than 25 years of age steadily decreased across all decades (49.1% in 1978–1982, 33.1% in 2008–2012) (Table 1). Simultaneously, the percent of live births born to women ages 35 years and older steadily increased from 4.7% in 1978–1982 to 13.4% in 1998–2002 and 14.5% in 2008–2012. Maternal age distribution was similar among states that did and did not adopt the standard pregnancy checkbox by 2008 and 2012, respectively (data not shown).
TABLE 1.
Maternal age-specific distribution of births, United States, selected years
| Maternal age, y | 1978–1982, % (N = 17,749,710) | 1988–1992, % (N = 20,284,601) | % changea | 1998–2002, % (N = 20,007,443) | % changea | 2008–2012, % (N = 20,284,176) | % changea |
|---|---|---|---|---|---|---|---|
| <20 | 15.4 | 12.8 | −16.9 | 11.7 | −8.6 | 9.2 | −21.4 |
| 20–24 | 33.6 | 26.6 | −20.8 | 25.0 | −6.0 | 23.9 | −4.4 |
| 25–29 | 30.8 | 30.5 | −1.0 | 26.8 | −12.1 | 28.3 | 5.6 |
| 30–34 | 15.4 | 21.3 | 38.3 | 23.0 | 8.0 | 24.0 | 4.3 |
| 35–39 | 4.0 | 7.7 | 92.5 | 11.1 | 44.2 | 11.7 | 5.4 |
| 40+ | 0.7 | 1.2 | 71.4 | 2.3 | 91.7 | 2.8 | 21.7 |
| Total | 100.0 | 100.0 | — | 100.0 | — | 100.0 | — |
All differences significant at P < .001 via the use of 2-sample z tests.
Compared with the previous decade.
Davis et al. Maternal age and maternal mortality, United States. Am J Obstet Gynecol 2017.
MMRs either decreased or remained relatively stable for all age groups between 1978–1982, 1988–1992, and 1998–2002 except for 25- to 29-year old women, where there was a 30% relative increase between 1988–1992 and 1998–2002 (Table 2). In states that adopted the standard pregnancy checkbox, MMRs increased for all age groups when we compared 2008–2012 with the previous time period. The biggest difference in MMR occurred among women ages 40 years and older, where MMR more than sextupled from 31.9 deaths per 100,000 in 1998–2002 to 200.5 deaths per 100,000 in 2008–2012 (Table 3). By contrast, there was no significant change in MMR among women ages 40 years and older in states that did not adopt the standard pregnancy checkbox, with MMRs of 39.2 and 33.7 deaths per 100,000 in 1998–2002 and 2008–2012, respectively.
TABLE 2.
Age-specific maternal mortality ratios,a United States, selected years
| Maternal age, y | 1978–1982 | 1988–1992 | % change | 1998–2002 | % changeb |
|---|---|---|---|---|---|
| <20 | 7.3 | 6.8 | −6.5c | 5.9 | −13.8c |
| 20–24 | 6.1 | 6.5 | 6.1c | 6.2 | −3.9c |
| 25–29 | 7.8 | 5.9 | −23.7 | 7.8 | 30.8 |
| 30–34 | 11.9 | 9.3 | −21.5 | 9.4 | 0.6c |
| 35–39 | 27.0 | 15.8 | −41.4 | 16.3 | 3.3c |
| 40+ | 67.6 | 36.6 | −45.8 | 34.8 | −5.1c |
| Total | 9.0 | 8.1 | −10.0 | 9.1 | 12.3 |
All differences significant at P < .01 via use of the 2-sample z tests unless otherwise noted.
Deaths per 100,000 live births;
Percent change from 1988–1992 to 1998–2002;
Not statistically significant, P > .05.
Davis et al. Maternal age and maternal mortality, United States. Am J Obstet Gynecol 2017.
TABLE 3.
Age-specific maternal mortality ratios, United States, selected years
| Maternal age, y | No standard checkbox by 2012a | Checkbox before 2008b | Expected MMRc | ||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| 1998–2002 | 2008–2012 | % change | 1998–2002 | 2008–2012 | % change | ||
| <20 | 4.6 | 5.8d | 26.1 | 5.7 | 10.8 | 89.3 | 7.2 |
|
| |||||||
| 20–24 | 6.1 | 7.2d | 18.0 | 5.8 | 13.2 | 127.8 | 6.8 |
|
| |||||||
| 25–29 | 7.1 | 7.6d | 7.0 | 8.3 | 15.4 | 86.3 | 8.8 |
|
| |||||||
| 30–34 | 7.7 | 10.3 | 33.8 | 9.2 | 18.1 | 96.1 | 12.3 |
|
| |||||||
| 35–39 | 15.6 | 15.2d | −2.6 | 15.7 | 32.7 | 108.6 | 15.3 |
|
| |||||||
| 40+ | 39.2 | 33.7d | −14.0 | 31.9 | 200.5 | 528.2 | 27.4 |
|
| |||||||
| Total | 8.6 | 9.9 | 15.1 | 9.0 | 22.4 | 149.8 | 10.3 |
|
| |||||||
| Estimated change due to revision (O-E) | 12.1 | ||||||
|
| |||||||
| % of observed change due to revisione | 90.3 | ||||||
|
| |||||||
| Estimated change due to 40+ misclassificationf | 3.9 | ||||||
|
| |||||||
| % of observed change due to 40+ misclassificationg | 28.8 | ||||||
All ratio differences significant at P < .01 via the use of 2-sample z tests unless otherwise noted.
E, expected; MMR, maternal mortality ratio, O, observed.
States include AK, AL, CA, CO, HI, MA, MD, NC, VA, WI, and WV. Note: Although MD does have a pregnancy checkbox that could produce equivalent values as to those produced by the standard checkbox, they did not adopt the standard pregnancy checkbox by 2012 and are therefore included in the “no standard checkbox” category;
States include CT, DC, DE, FL, ID, KS, MI, MT, NE, NH, NJ, NM, NY, OH, OK, OR, RI, SC, SD, TX, UT, WA, and WY;
Expected MMR without addition of pregnancy checkbox to the US Standard Certificate of Death: 1998–2002 age-specific MMR multiplied by the age-specific percent change between 1998–2002 and 2008–2012 observed in unrevised states;
Change in MMR from 1998–2002 and 2008–2012 not statistically significant, P > .05;
Expected MMR divided by the difference in the observed MMR between 1998–2002 and 2008–2012, multiplied by 100;
Difference in the observed MMR and the estimated MMR that would have occurred if women ages ≥ 40 had the same age-specific MMR as women ages <40 years;
Estimated change due to 40+ misclassification divided by the difference in the observed MMR between 1998–2002 and 2008–2012, multiplied by 100.
Davis et al. Maternal age and maternal mortality, United States. Am J Obstet Gynecol 2017.
In the first 2 decades after 1978–1982, even though there was a shift toward older maternal age there were no substantial increases in the MMR. Comparing 1988–1992 with 1978–1982, we found that reductions in age-specific MMR for all but one age group (20- to 24-year-old women) offset the contribution of a shifting age distribution, resulting in 0.9 fewer deaths per 100,000 live births. A 12% relative increase in the MMR occurred between 1988–1992 and 1998–2002 (8.1 and 9.1, respectively). Among states without the standard pregnancy checkbox (n = 11), there was a 15% relative increase in the MMR between 1998–2002 and 2008–2012 (8.6 and 9.9, respectively), with 0.9 of the 1.3 excess deaths per 100,000 attributable to changes in age-specific MMRs and 0.4 of the 1.3 excess deaths per 100,000 attributable to shifts in maternal age (Table 4). However, the MMR more than doubled between 1998–2002 and 2008–2012 in states with the standard pregnancy checkbox (n = 23; 9.0–22.4). This dramatic increase was attributable almost entirely to increases in age-specific MMRs (94.9% or 12.7 deaths per 100,000) as opposed to increases in maternal age (5.1% or 0.7 deaths per 100,000). Of all age categories, the 528% increase in MMR among women ages 40 years and older accounted for nearly one third of the total MMR increase over the decade (5.0 of 13.4 total excess maternal deaths). Among maternal deaths to women ages ≥ 40 years from 1978 to 2002, 5 deaths reportedly occurred among women ages 50–54 years, and no maternal deaths were recorded for women ages >54 years. In contrast, from 2008 to 2012, 221 maternal deaths reportedly occurred among women ages 50–54 years and 18 reportedly occurred among women ages >54 years.
TABLE 4.
Maternal age-specific components of the changes in maternal mortality ratios between 1998–2002 and 2008–2012 using Kitagawa decomposition, by standard pregnancy checkbox status, United States
| No standard checkbox by 2012a | Checkbox before 2008b | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Distribution difference | Ratio difference | Total mortality difference | Distribution difference | Ratio difference | Total Mortality difference | |
| Maternal age, y | ||||||
|
| ||||||
| <20 | ||||||
|
| ||||||
| Absolute | −0.1 | 0.1 | 0.0 | −0.2 | 0.5 | 0.3 |
|
| ||||||
| Relative %c | −9.6 | 9.3 | −0.3 | −1.5 | 3.9 | 2.4 |
|
| ||||||
| 20–24 | ||||||
|
| ||||||
| Absolute | −0.1 | 0.3 | 0.2 | −0.1 | 1.8 | 1.7 |
|
| ||||||
| Relative %c | −7.0 | 19.6 | 12.6 | −0.7 | 13.4 | 12.8 |
|
| ||||||
| 25–29 | ||||||
|
| ||||||
| Absolute | 0.1 | 0.1 | 0.2 | 0.2 | 2.0 | 2.2 |
|
| ||||||
| Relative %c | 5.9 | 10.5 | 16.4 | 1.4 | 14.7 | 16.0 |
|
| ||||||
| 30–34 | ||||||
|
| ||||||
| Absolute | 0.1 | 0.6 | 0.7 | 0.1 | 2.1 | 2.2 |
|
| ||||||
| Relative %c | 7.6 | 49.5 | 57.1 | 0.9 | 15.6 | 16.5 |
|
| ||||||
| 35–39 | ||||||
|
| ||||||
| Absolute | 0.1 | 0.0 | 0.1 | 0.1 | 1.9 | 2.1 |
|
| ||||||
| Relative %c | 11.3 | −3.1 | 8.2 | 0.9 | 14.5 | 15.3 |
|
| ||||||
| 40+ | ||||||
|
| ||||||
| Absolute | 0.2 | −0.2 | 0.1 | 0.6 | 4.4 | 5.0 |
|
| ||||||
| Relative %c | 19.1 | −13 | 6.1 | 4.2 | 32.7 | 36.9 |
|
| ||||||
| Total | ||||||
|
| ||||||
| Absolute | 0.4 | 0.9 | 1.3 | 0.7 | 12.7 | 13.4 |
|
| ||||||
| Relative %c | 27.2 | 72.8 | 100.0 | 5.1 | 94.9 | 100.0 |
States include AK, AL, CA, CO, HI, MA, MD, NC, VA, WI, and WV. Note: Although MD does have a pregnancy checkbox that could produce equivalent values as to those produced by the standard checkbox, they did not adopt the standard pregnancy checkbox by 2012 and are therefore included in the “no standard checkbox” category;
States include CT, DC, DE, FL, ID, KS, MI, MT, NE, NH, NJ, NM, NY, OH, OK, OR, RI, SC, SD, TX, UT, WA, and WY;
Absolute difference divided by total difference between 2 time periods.
Davis et al. Maternal age and maternal mortality, United States. Am J Obstet Gynecol 2017.
As outlined, states that adopted the standard pregnancy checkbox on their death certificate by 2008 had a substantially greater overall MMR from 2008 to 2012 (22.4 per 100,000 births) and a substantially greater MMR among women ages 40 years and older (200.5), compared with states that did not adopt the standard pregnancy checkbox by 2012 (total MMR: 9.9, ≥ 40 MMR: 33.7) (Table 3). Among states that adopted the standard pregnancy checkbox by 2010 (n = 34), a comparison of the 3 years before checkbox implementation with the 3 years after implementation demonstrated a similar pregnancy checkbox effect, both overall (pre: 9.6, post: 20.0) and among women ages ≥ 40 years (pre: 50.7, post: 163.7). An estimated 12.1 (54%) of the observed ratio of 22.4 deaths per 100,000 women in states that adopted the standard pregnancy checkbox, and 90.3% of the observed change in MMR between 1998–2002 and 2008–2012 in checkbox states, may be attributable to the check-box alone. If states that adopted the standard checkbox had the same increase in MMR as states that did not adopt the standard checkbox, the overall increase in MMR between 1998–2002 and 2008–2012 in states with the standard pregnancy checkbox would be 14.4% as opposed to the observed 149.8%.
Because of the observed increase in age-specific MMR for women ≥ 40 years in pregnancy checkbox states, we estimated the percent of maternal deaths among women ≥ 40 years, which may have been misclassified due to the pregnancy checkbox. We assumed the relative percentage increase in maternal deaths among women ages <40 years between 1998–2002 and 2008–2012 indicated the “true” increase resulting from improved case identification. We then applied the observed percentage increase among women ages <40 years to women ages ≥40 years to estimate the number of expected maternal deaths with the difference between observed and expected yielding the number of potentially misclassified maternal deaths among women ages ≥40 years. We estimated that 135.4 (68%) of the observed ratio of 200.5 deaths per 100,000 women ages ≥40 years in pregnancy checkbox states from 2008 to 2012 potentially were misclassified. We further estimated that 28.8% of the observed change in MMR between 1998–2002 and 2008–2012 in states with the standard pregnancy checkbox was potentially due to misclassification among women ages ≥40 years (Table 3).
Comment
In both decades immediately after 1978–1982, even though there was a shift toward older maternal age, there were no substantial increases in the MMR. However, the MMR more than doubled between 1998–2002 and 2008–2012 among states that adopted the standard pregnancy checkbox, compared with a much more modest MMR increase among states without a pregnancy checkbox, illustrating the impact of changes to identification methods. In both groups of states, increasing age-specific maternal mortality contributes more to changes in MMR in recent years than a changing maternal age distribution. For states that implemented the pregnancy checkbox before 2008, the greatest contribution comes from increasing MMRs among women ages ≥40 years.
The addition of a pregnancy checkbox on the US Standard Certificate of Death appears to be the main driver of the increases in MMR during the last decade,10,17 both by increasing maternal death case identification and potentially maternal death misclassification. Although misclassification resulting from the pregnancy checkbox may be occurring among all age groups, it is most easily identified among women at the upper end of the maternal age distribution. Current MMR estimates for 2008–2012 among women ages ≥40 years in states with the standard pregnancy checkbox (200.5 per 100,000) corresponds to more than 2.0 maternal deaths for every 1000 women ≥40 years of age who had a live birth; 1 in every 500 women 40 years and older who is pregnant would die under such a scenario were there no misclassification, a highly unlikely scenario. The Centers for Disease Control and Prevention’s Division of Reproductive Health’s Pregnancy Mortality Surveillance System collects information from vital records about deaths caused by complications of pregnancy within 1 year of the end of pregnancy but uses clinical information on death and linked birth certificates to ascribe a clinical cause of death, as opposed to ICD-10 codes used in this analysis. For a comparable time period (2006–2010), the Pregnancy Mortality Surveillance System found 275 pregnancy-related deaths per 567,154 births to women 40 years and older.2,4 The resulting pregnancy-related mortality ratio (48 per 100,000 live births) was less than one quarter of what we found for this age group using conventional vital statistics among checkbox states. The lack of granularity in the O Chapter of ICD-10 precludes a meaningful analysis of age-specific causes of death that would shed further light on the plausibility of our potential misclassification findings.
Additional contributors to the increasing MMR could include increased prevalence of chronic conditions and increased identification of maternal deaths due to changes in ICD codes, with ICD-10 including additional diagnoses to identify maternal deaths. However, changes in ICD codes are only expected to play a small role in the dramatic increase in MMR between 1998–2002 and 2008–2012, because ICD, version 10, has been used for maternal death classification since 1999 and the increase in MMR between 1988–1992 and 1998–2002 (likely due to changes between ICD-9 and ICD-10) was only 12%. Therefore, either a small or no increase in the MMR occurred between 1988–1992 and 1998–2002 even while the age distribution continued to shift. Our application of Kitagawa decomposition only took into account one variable of interest at a time (here, age). In Kitagawa analyses, age was used as a proxy for changes in chronic conditions. Although mothers of advanced maternal age may have greater rates of chronic conditions, we found a shifting maternal age distribution to be contributing less than changes in age-specific mortality ratios. Therefore, it is unlikely that adjusting for chronic conditions would alter our conclusions. In addition, maternal age and chronic disease prevalence are likely to be collinear, limiting the usefulness of adjusting for both variables. However, changes in chronic disease prevalence within age groups may be contributing to the observed increase in age-specific MMRs among 30–34-year-old women between 1998–2002 and 2008–2012 in states that did not adopt the standard pregnancy checkbox. Further investigation of how changes in chronic disease prevalence may be affecting MMRs within age groups would be a useful next step.
Accurate maternal death surveillance and MMR estimates are crucial for public health planning to reduce mortality risk during the pregnancy and postpartum periods. In the late part of the 20th century, literature emerged that pointed to consistent undercounting of maternal deaths and the limits of ICD-based identification of these events.18–21 Revising the US Standard Certificate of Death to include a question that establishes a temporal relationship to pregnancy does appear to be increasing case identification. However, incorrect reporting of recent pregnancy such as is likely with the cases at implausible ages explored in this paper may be a source of misclassified maternal deaths. We assumed that factors other than changes in maternal death identification that would affect the MMR (eg, quality of care and incidence of non-preventable causes of death) were approximately the same in states with and without the standard pregnancy checkbox. Although this is an assumption, both overall and age-specific MMR estimates were comparable in states with and without the standard pregnancy checkbox in 1998–2002 (before check-box adoption), making it unlikely that factors other than changes in maternal death identification differed enough to cause such discrepant changes in MMR between 1998–2002 and 2008–2012.
The pregnancy checkbox also may be leading to misclassified maternal deaths and inflated MMRs because temporal relationships between death and pregnancy may not always be causal relationships. We were unable to determine what percent of the excess deaths among all age groups resulting from the pregnancy checkbox are due to misclassification and what percent are due to accurate increases in case identification. There is an urgent need to discover information about the nature and causes of death identified by the pregnancy checkbox so that vital statistics can be more useful for population-based surveillance of these tragic events.22 Partnerships between state maternal mortality review committees and vital statistics offices, identifying and correcting errors upstream of death coding, may provide the best opportunity for improving reporting of the pregnancy checkbox. By improving reporting on the pregnancy checkbox, the accuracy of maternal death surveillance and MMR estimates for the United States can more effectively inform activities to eliminate preventable maternal deaths.
Footnotes
The authors report no conflict of interest.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the Health Resources and Services Administration.
References
- 1.Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, Shackelford KA, Steiner C, Heuton KR, et al. Global, regional, and national levels and causes of maternal mortality during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:980–1004. doi: 10.1016/S0140-6736(14)60696-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006–2010. Obstet Gynecol. 2015;125:5–12. doi: 10.1097/AOG.0000000000000564. [DOI] [PubMed] [Google Scholar]
- 3.Hoyert DL, Danel I, Tully P. Maternal mortality, United States and Canada, 1982–1997. Birth. 2000;27:4–11. doi: 10.1046/j.1523-536x.2000.00004.x. [DOI] [PubMed] [Google Scholar]
- 4.United States Department of Health and Human Services (US DHHS) Centers for Disease Contral and Prevention Committee, National Center for Health Statistics (NCHS), Division of Vital Statistics. [Accessed June 17, 2017];Natality public-use data 2007–2014. (2016). 2016 Feb; Available at: https://wonder.cdc.gov/natality.html.
- 5.National Center for Health Statistics. Monthly Vital Statistics Report. Hyattsville, MD: Public Health Service; 1982. Advance report of final natality statistics, 1980. [Google Scholar]
- 6.Callaghan WM, Mackay AP, Berg CJ. Identification ofsevere maternal morbidity during delivery hospitalizations, United States, 1991–2003. Am J Obstet Gynecol. 2008;199:133e1–8. doi: 10.1016/j.ajog.2007.12.020. [DOI] [PubMed] [Google Scholar]
- 7.Gilbert WM, Nesbitt TS, Danielsen B. Child-bearing beyond age 40: pregnancy outcome in 24,032 cases. Obstet Gynecol. 1999;93:9–14. doi: 10.1016/s0029-7844(98)00382-2. [DOI] [PubMed] [Google Scholar]
- 8.Callaghan WM, Berg CJ. Pregnancy-related mortality among women aged 35 years and older, United States, 1991–1997. Obstet Gynecol. 2003;102:1015–21. doi: 10.1016/s0029-7844(03)00740-3. [DOI] [PubMed] [Google Scholar]
- 9.MacKay AP, Berg CJ, Liu X, Duran C, Hoyert DL. Changes in pregnancy mortality ascertainment: United States, 1999–2005. Obstet Gynecol. 2011;118:104–10. doi: 10.1097/AOG.0b013e31821fd49d. [DOI] [PubMed] [Google Scholar]
- 10.Hoyert DL. Maternal mortality and related concepts. Vital Health Stat. 2007 Feb;3(33):1–13. [PubMed] [Google Scholar]
- 11.Callaghan WM. Overview of maternal mortality in the United States. Semin Perinatol. 2012;36:2–6. doi: 10.1053/j.semperi.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Klebba AJ, Scott JH. Estimates of selected comparability ratios based on dual coding of 1976 death certificates by the Eighth and Ninth Revisions of the International Classification of Diseases. Monthly Vital Stat Rep. 1980;(11):1–19. [Google Scholar]
- 13.Anderson RN, Miniño AM, Rosenburg HM. Comparability of cause of death between ICD–9 and ICD–10: preliminary estimates. Natl Vital Stat Rep. 2001;49:1–32. [PubMed] [Google Scholar]
- 14.Kitagawa EM. Components of a difference between two rates. J Am Stat Assoc. 1955;50:1168–94. [Google Scholar]
- 15.Sappenfield WM, Peck MG, Gilbert CS, Haynatzka VR, Bryant T. Perinatal periods of risk: phase 2 analytic methods for further investigating feto-infant mortality. Matern Child Health J. 2010;14:851–63. doi: 10.1007/s10995-010-0624-5. [DOI] [PubMed] [Google Scholar]
- 16.Callaghan WM, MacDorman MF, Shapiro-Mendoza CK, Barfield WD. Explaining the recent decrease in US infant mortality rate, 2007–2013. Am J Obstet Gynecol. 2017;216:73e1–8. doi: 10.1016/j.ajog.2016.09.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murphy SL, Kochanek KD, Xu JQ, Heron M. Deaths: final data for 2012. Natl Vital Stat Rep. 2015;63:1–117. [PubMed] [Google Scholar]
- 18.Misclassification of maternal deaths—Washington State. MMWR Morbid Mortal Wkly Rep. 1986;35:621–3. [PubMed] [Google Scholar]
- 19.Enhanced maternal mortality surveillance—North Carolina, 1988 and 1989. MMWR Morbid Mortal Wkly Rep. 1991;40:469–71. [PubMed] [Google Scholar]
- 20.Pregnancy-related mortality—Georgia, 1990–1992. MMWR Morbid Mortal Wkly Rep. 1995;44:93–6. [PubMed] [Google Scholar]
- 21.Jocums S, Mitchel EF, Jr, Entman SS, Piper JM. Monitoring maternal mortality using vital records linkage. Am J Prev Med. 1995;11:75–8. [PubMed] [Google Scholar]
- 22.MacDorman MF, Declercq E, Cabral H, Morton C. Recent increases in the U.S. maternal mortality rate: disentangling trends from measurement issues. Obstet Gynecol. 2016;128:447–55. doi: 10.1097/AOG.0000000000001556. [DOI] [PMC free article] [PubMed] [Google Scholar]


