Abstract
Publisher's Note: This article has a companion Counterpoint by Kapur and Semple.
Publisher's Note: Join in the discussion of these articles at Blood Advances Community Conversations.
This is an exciting time for clinicians and scientists interested in platelet biology. Improved imaging methods allow platelets to be observed in action in animal models in real time at ever greater resolution. Expanding proteomic and genetic data sets lend themselves to better understanding platelet activation. New gene editing methods make it easier, faster, and less expensive to test new ideas using transgenic animal models. Combining systems biology approaches with computational methods encourages a broader perspective on platelet activation and makes it possible to develop ideas in silico that can then be tested in vivo. One result has been an opportunity to revisit prevailing wisdom about the hemostatic response, extending and occasionally refuting what has come before.
Systems biology is the study of complex interactions, some of whose properties can be understood only when multiple cells or multiple pathways are considered. Here we will consider 2 examples in which improved methods and a systems-oriented approach have provided insights into the most basic of platelet functions: participation in the hemostatic response to injury. The first example considers the ways in which the simple act of piling up of platelets at a site of injury helps to calibrate the hemostatic response by altering the environment in which platelet activation occurs. The second example considers how individual signaling events within platelets form an integrated network whose properties emerge from the individual pathways.
Achieving hemostasis: piling up platelets changes everything
Penetrating injuries trigger platelet activation by the local accumulation of platelet agonists. Some agonists, such as collagen, are stationary; others, such as thrombin, adenosine diphosphate (ADP), and thromboxane A2 (TxA2) are mobile. Platelet activation is commonly considered with an agonist-centric perspective, but this perspective omits the impact of the local environment, which changes rapidly as platelets and fibrin accumulate. Recent evidence suggests that formation of a hemostatic thrombus first promotes and then limits platelet activation by providing a sheltered environment in which agonists can accumulate. Thus, there is a reciprocal, rather than a unidirectional, relationship between platelet activation and thrombus structure (Figure 1A). Because this relationship emerges as platelets pile up, it is worth considering how it happens.
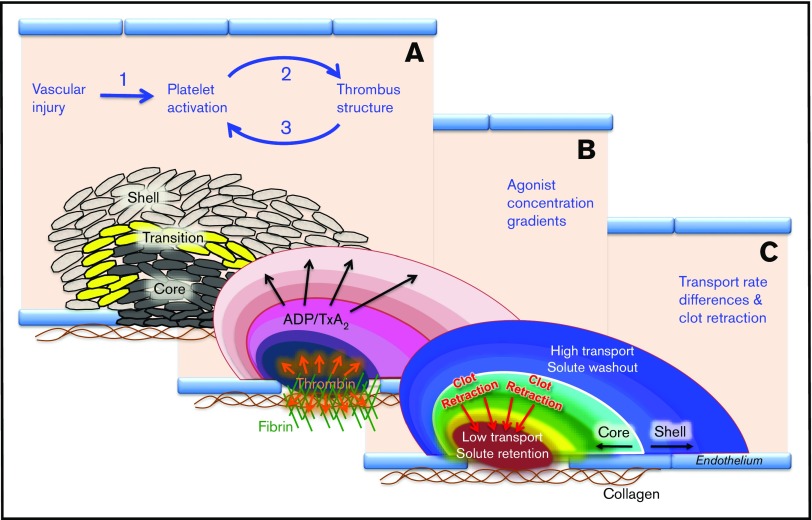
Figure 1.
A systems view of the hemostatic response to penetrating injuries. High-resolution confocal fluorescence microscopy studies performed in mice show that the hemostatic structure has a characteristic architecture whose properties emerge as platelets accumulate, altering local conditions. (A) Presence of a core of highly activated, densely packed platelets overlaid with a shell of loosely packed, less activated platelets and the transition zone that exists between them. (B) Manner in which soluble platelet agonists such as thrombin, ADP, and TxA2 form concentration gradients radiating from the site of injury. (C) Distribution of the agonists is determined in part by differences in transport rates in the narrowing gaps between platelets, gaps whose dimensions decrease as clot retraction proceeds.
Although platelet behavior has been studied for over a century, recent advances in intravital imaging pioneered by the Furie laboratory1-3 and others4-9 have made it possible to observe the hemostatic response in mice in real time at high resolution. Those studies show that platelet activation in this setting is heterogeneous. Although some platelets change shape, secrete their granule contents, and become procoagulant, others display only minimal external signs of activation. The result is a gradient of platelet activation with a core of fully activated platelets, a shell of less activated platelets, and a transition zone between them (Figure 1A).7
Among the properties that distinguish the core from the shell is packing density, which is greater in the core.7 Tight packing slows the movement of soluble molecules in the gaps between platelets, which shrink as the thrombus retracts.10,11 The core is where most of the fibrin is found and where clot retraction would be expected to have the greatest impact (Figure 1B). As packing density increases, transport becomes dominated by diffusion rather than convection, slowing movement to an even greater extent (Figure 1C).10-12
Regional differences in packing density also affect the distribution of platelet agonists. The result is the appearance of concentration gradients in which the distribution of each agonist is also affected by its physical properties and binding to other molecules. Individual platelets are exposed to combinations of agonists whose concentrations vary over time (Figure 1B). Submaximal concentrations of multiple platelet agonists can have additive or even synergistic effects.13 Thrombin is the main driver of full platelet activation in the thrombus core. TxA2 and ADP are primarily drivers for the thrombus shell.7,14 The impact of packing density is demonstrated by studies showing a mutation in αIIbβ3 that impairs clot retraction decreases thrombin activity and reduces platelet activation.11,15 Studies performed in silico extend the observational studies and provide hypotheses that can be tested in vivo and in vitro.10,16,17
Most of the studies summarized in Figure 1 were performed in the mouse microvasculature using a laser or a sharpened probe to make small holes in arterioles and venules. To what extent are the results applicable to people? Human platelets cannot readily be studied in vivo. However, when studied in a microfluidics device that incorporates collagen, tissue factor, and the transmural pressure drop that normally occurs following vascular injury, human platelets form an inner core of fully activated platelets overlaid by a shell of less activated platelets just as mouse platelets do in vivo.18
What about events in arteries and veins, rather than arterioles and venules? Primarily for technical reasons, high-resolution imaging studies have largely been limited to the microvasculature. However, there has been progress.9,19-21 More work needs to be done, but the initial message appears to be the same. In both settings, the piling up of platelets changes everything by producing a local environment in which agonists accumulate.
The platelet signaling network is an integrating engine
Most of what is known about the platelet signaling network was worked out one pathway at a time. The first part of this essay shows that platelets within a growing hemostatic mass are exposed to combinations of agonists, any of which may be present below optimal concentrations. Agonist receptors are not generic. Each agonist has a unique receptor set that can couple to the platelet signaling network in different ways (Figure 2).22 Thrombin, for example, activates 2 members of the protease-activated receptor family on human platelets, PAR1 and PAR4, allowing it to signal through the heterotrimeric G proteins, Gq, G12, and, directly or indirectly in platelets, Gi2. PAR1 produces a quick burst of signaling; PAR4 a more sustained response. ADP activates P2Y1 and P2Y12, the latter coupled to Gi2 and the former to Gq. Signals mediated by Gq activate phospholipase Cβ, leading to increased cytosolic Ca2+, activation of Rap1b, and, ultimately, to the activation of αIIbβ3.23,24 Gi2 inhibits cyclic adenosine monophosphate (cAMP) formation, activates Akt, and promotes integrin activation by inhibiting Rap1b inactivation.25 Once αIIbβ3 has been activated, integrin-dependent signaling promotes clot retraction, increasing packing density and slowing solute transport.
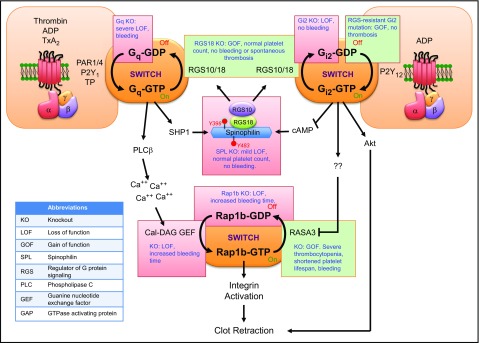
Figure 2.
Integrating the platelet signaling network to obtain an optimal response. Although platelet signaling pathways were originally described one at a time, they form a closely regulated network that both promotes and limits the hemostatic response. The figure focuses on events downstream of the G protein–coupled receptors for thrombin, ADP, and TxA2. It illustrates 2 GTP-dependent switching points or nodes in the network, crosstalk between pathways, and the presence of regulatory loops that affect information flow through the nodes. The green and red boxes summarize transgenic mouse models associated with gain or loss of function, respectively. References are in the text.
The platelet signaling network makes possible a measured response to agonists in part because of feedback loops and nodes within the network where signaling pathways converge. Examples include Gq, Gi2, and Rap1b (Figure 2). The activity state of each of these is determined by whether they are bound to guanosine triphosphate (GTP) or guanosine diphosphate (GDP), the GDP-bound state being inactive. In effect, these are on/off switches. Replacement of GDP with GTP is promoted by a guanine nucleotide exchange factor (GEF), which for Gq and Gi2 is an agonist-occupied receptor and for Rap1b is CalDAG-GEF1. Restoration of the inactive state is accelerated by a GTPase activating proteins (GAP). For Gq and Gi2 the primary GAPs in platelets are RGS10 and RGS18.26-28 For Rap1b, the primary GAP is Rasa3.25,29
Network integration occurs in part by regulating the balance of GEF and GAP activity. The availability of RGS10 and RGS18 is regulated by spinophilin (SPL), which sequesters both in resting platelets, and by 14-3-3γ, which binds RGS proteins in activated platelets.26,30 Dissociation of SPL/RGS complexes occurs after a brief delay, creating a negative feedback loop when platelets are activated by thrombin or TxA2.26 As an example of pathway convergence, dissociation of the SPL/RGS complex also occurs when endothelium-derived PGI2 suppresses platelet activation by raising platelet cAMP levels (Figure 2).31 For Rap1b, regulation occurs at the level of Rasa3, whose ability to act as a GAP is inhibited by signaling downstream of Gi2.25,32 Rap1b33 and CalDAG-GEF1,34,35 like spinophilin, are targets for cAMP-dependent phosphorylation.
How can the relative contributions of these regulatory events be assessed? One way is with transgenic mice (Figure 2). Deletion of Gi2α36,37 or Gqα38 produces a loss of function phenotype, as does deleting spinophilin or introducing a missense mutation in spinophilin that mimics the effects of cAMP-dependent phosphorylation.26,31 In contrast, deleting either RGS1827,39 or RGS10 (Peisong Ma and L.F.B., unpublished observations, 2015), or introducing a mutation in Gi2α that makes it resistant to RGS proteins,7,40 produces a gain of function. These effects are not of equivalent magnitude: deleting Gq causes spontaneous bleeding, but deleting Gi2 does not.36-38 Neither gain-of-function mutation appears to cause spontaneous thrombosis. The RGS-insensitive Gi2 mutation causes expansion of the thrombus shell without affecting the size of the core.7
Mutations at the level of Rap1b are equally informative about network integration. Deleting Rap1b causes a loss of function phenotype with a prolonged tail bleeding time and increased time to occlusion.41 Deleting CalDAG-GEF1 also causes a loss of function42 as do CalDAG-GEF1 mutations in humans.43,44 Deleting Rasa3 causes severe thrombocytopenia, bleeding, and increased embryonic and perinatal lethality.25,29 The thrombocytopenia is believed to be due to spontaneous platelet activation and shortened platelet survival.25 These observations speak to the importance of Rasa3 at the Rap1b network integration point.
In summary, recent studies show that platelets possess an integrated signaling network rather than a collection of independent pathways. Packing density and therefore transport rates help determine agonist distribution and concentration. Activity at network nodes determines how large the hemostatic mass will grow.
Is any of this clinically relevant?
There are several ways that the 2 examples cited here can inform decision making by hematologists, cardiologists, and pharmaceutical companies. First, they provide a context to better understand why platelets express receptors for so many different agonists. Second, they suggest that the strengths and limitations of some commonly used antiplatelet agents reflect not only their half-lives, affinities, and off-rates, but also where they work on the platelet signaling network and how well they penetrate thrombus structure. For example, observational studies performed in vivo suggest that widely prescribed P2Y12 antagonists impair hemostasis and reduce recurrent thrombotic events by destabilizing the thrombus shell with comparatively little impact on the thrombus core, at least in the microcirculation where these studies were performed. Finally, the data suggest that tests of on-treatment platelet function in patient taking antiplatelet agents need to be designed to better reproduce the complex conditions that the observational studies show exists within a growing thrombus. Computational studies that recapitulate platelet accumulation and transport may prove helpful in this regard, especially as the simulations become even more refined.10,17,45-50
Acknowledgments
This work was supported by National Institutes of Health, National Heart, Lung and Blood Institute grants P01 HL40387, P01 HL120846, and R01 HL103419.
Authorship
Contribution: All authors contributed to the ideas expressed in the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Lawrence F. Brass, University of Pennsylvania, Room 815 BRB-II, 421 Curie Blvd, Philadelphia, PA 19104; e-mail: brass@mail.med.upenn.edu.
References
- 1.Falati S, Gross P, Merrill-Skoloff G, Furie BC, Furie B. Real-time in vivo imaging of platelets, tissue factor and fibrin during arterial thrombus formation in the mouse. Nat Med. 2002;8(10):1175-1181. [DOI] [PubMed] [Google Scholar]
- 2.Falati S, Gross PL, Merrill-Skoloff G, et al. . In vivo models of platelet function and thrombosis: study of real-time thrombus formation. Methods Mol Biol. 2004;272:187-197. [DOI] [PubMed] [Google Scholar]
- 3.Celi A, Merrill-Skoloff G, Gross P, et al. . Thrombus formation: direct real-time observation and digital analysis of thrombus assembly in a living mouse by confocal and widefield intravital microscopy. J Thromb Haemost. 2003;1(1):60-68. [DOI] [PubMed] [Google Scholar]
- 4.oude Egbrink MG, Tangelder GJ, Slaaf DW, Reneman RS. Thromboembolic reaction following wall puncture in arterioles and venules of the rabbit mesentery. Thromb Haemost. 1988;59(1):23-28. [PubMed] [Google Scholar]
- 5.Rosen ED, Raymond S, Zollman A, et al. . Laser-induced noninvasive vascular injury models in mice generate platelet- and coagulation-dependent thrombi. Am J Pathol. 2001;158(5):1613-1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Gestel MA, Heemskerk JW, Slaaf DW, et al. . Real-time detection of activation patterns in individual platelets during thromboembolism in vivo: differences between thrombus growth and embolus formation. J Vasc Res. 2002;39(6):534-543. [DOI] [PubMed] [Google Scholar]
- 7.Stalker TJ, Traxler EA, Wu J, et al. . Hierarchical organization in the hemostatic response and its relationship to the platelet-signaling network. Blood. 2013;121(10):1875-1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kamocka MM, Mu J, Liu X, et al. . Two-photon intravital imaging of thrombus development. J Biomed Opt. 2010;15(1):016020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cooley BC. In vivo fluorescence imaging of large-vessel thrombosis in mice. Arterioscler Thromb Vasc Biol. 2011;31(6):1351-1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tomaiuolo M, Stalker TJ, Welsh JD, Diamond SL, Sinno T, Brass LF. A systems approach to hemostasis: 2. Computational analysis of molecular transport in the thrombus microenvironment. Blood. 2014;124(11):1816-1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stalker TJ, Welsh JD, Tomaiuolo M, et al. . A systems approach to hemostasis: 3. Thrombus consolidation regulates intrathrombus solute transport and local thrombin activity. Blood. 2014;124(11):1824-1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Welsh JD, Stalker TJ, Voronov R, et al. . A systems approach to hemostasis: 1. The interdependence of thrombus architecture and agonist movements in the gaps between platelets. Blood. 2014;124(11):1808-1815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chatterjee MS, Purvis JE, Brass LF, Diamond SL. Pairwise agonist scanning predicts cellular signaling responses to combinatorial stimuli. Nat Biotechnol. 2010;28(7):727-732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Welsh JD, Colace TV, Muthard RW, Stalker TJ, Brass LF, Diamond SL. Platelet-targeting sensor reveals thrombin gradients within blood clots forming in microfluidic assays and in mouse. J Thromb Haemost. 2012;10(11):2344-2353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Law DA, DeGuzman FR, Heiser P, Ministri-Madrid K, Killeen N, Phillips DR. Integrin cytoplasmic tyrosine motif is required for outside-in alphaIIbbeta3 signalling and platelet function. Nature. 1999;401(6755):808-811. [DOI] [PubMed] [Google Scholar]
- 16.Fogelson AL, Neeves KB. Fluid mechanics of blood clot formation. Annu Rev Fluid Mech. 2015;47:377-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Flamm MH, Colace TV, Chatterjee MS, et al. . Multiscale prediction of patient-specific platelet function under flow. Blood. 2012;120(1):190-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Muthard RW, Diamond SL. Side view thrombosis microfluidic device with controllable wall shear rate and transthrombus pressure gradient. Lab Chip. 2013;13(10):1883-1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Getz TM, Piatt R, Petrich BG, Monroe D, Mackman N, Bergmeier W. Novel mouse hemostasis model for real-time determination of bleeding time and hemostatic plug composition. J Thromb Haemost. 2015;13(3):417-425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cooley BC. Murine arterial thrombus induction mechanism influences subsequent thrombodynamics. Thromb Res. 2015;135(5):939-943. [DOI] [PubMed] [Google Scholar]
- 21.Welsh JD, Stalker TJ, Diamond SL, Brass LF. Real time intravital imaging of thrombus formation in the mouse femoral artery reveals critical differences from events in the microvasculature. J Thromb Haemost. 2015;13(Suppl 2):108. [Google Scholar]
- 22.Stalker TJ, Newman DK, Ma P, Wannemacher KM, Brass LF Platelet signaling. Handb Exp Pharmacol. 2012(210):59-85. [DOI] [PMC free article] [PubMed]
- 23.Bertoni A, Tadokoro S, Eto K, et al. . Relationships between Rap1b, affinity modulation of integrin alpha IIbbeta 3, and the actin cytoskeleton. J Biol Chem. 2002;277(28):25715-25721. [DOI] [PubMed] [Google Scholar]
- 24.Shattil SJ, Kim C, Ginsberg MH. The final steps of integrin activation: the end game. Nat Rev Mol Cell Biol. 2010;11(4):288-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stefanini L, Paul DS, Robledo RF, et al. . RASA3 is a critical inhibitor of RAP1-dependent platelet activation. J Clin Invest. 2015;125(4):1419-1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ma P, Cierniewska A, Signarvic R, et al. . A newly identified complex of spinophilin and the tyrosine phosphatase, SHP-1, modulates platelet activation by regulating G protein-dependent signaling. Blood. 2012;119(8):1935-1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Delesque-Touchard N, Pendaries C, Volle-Challier C, et al. . Regulator of G-protein signaling 18 controls both platelet generation and function. PLoS One. 2014;9(11):e113215.25405900 [Google Scholar]
- 28.Rowley JW, Oler AJ, Tolley ND, et al. . Genome-wide RNA-seq analysis of human and mouse platelet transcriptomes. Blood. 2011;118(14):e101-e111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Molina-Ortiz P, Polizzi S, Ramery E, et al. . Rasa3 controls megakaryocyte Rap1 activation, integrin signaling and differentiation into proplatelet. PLoS Genet. 2014;10(6):e1004420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gegenbauer K, Elia G, Blanco-Fernandez A, Smolenski A. Regulator of G-protein signaling 18 integrates activating and inhibitory signaling in platelets. Blood. 2012;119(16):3799-3807. [DOI] [PubMed] [Google Scholar]
- 31.Ma P, Ou K, Sinnamon AJ, Jiang H, Siderovski DP, Brass LF. Modulating platelet reactivity through control of RGS18 availability. Blood. 2015;126(24):2611-2620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lova P, Paganini S, Sinigaglia F, Balduini C, Torti M. A Gi-dependent pathway is required for activation of the small GTPase Rap1B in human platelets. J Biol Chem. 2002;277(14):12009-12015. [DOI] [PubMed] [Google Scholar]
- 33.Siess W, Winegar DA, Lapetina EG. Rap1-B is phosphorylated by protein kinase A in intact human platelets. Biochem Biophys Res Commun. 1990;170(2):944-950. [DOI] [PubMed] [Google Scholar]
- 34.Guidetti GF, Manganaro D, Consonni A, Canobbio I, Balduini C, Torti M. Phosphorylation of the guanine-nucleotide-exchange factor CalDAG-GEFI by protein kinase A regulates Ca(2+)-dependent activation of platelet Rap1b GTPase. Biochem J. 2013;453(1):115-123. [DOI] [PubMed] [Google Scholar]
- 35.Subramanian H, Zahedi RP, Sickmann A, Walter U, Gambaryan S. Phosphorylation of CalDAG-GEFI by protein kinase A prevents Rap1b activation. J Thromb Haemost. 2013;11(8):1574-1582. [DOI] [PubMed] [Google Scholar]
- 36.Jantzen HM, Milstone DS, Gousset L, Conley PB, Mortensen RM. Impaired activation of murine platelets lacking G alpha(i2). J Clin Invest. 2001;108(3):477-483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yang J, Wu J, Jiang H, et al. . Signaling through Gi family members in platelets. Redundancy and specificity in the regulation of adenylyl cyclase and other effectors. J Biol Chem. 2002;277(48):46035-46042. [DOI] [PubMed] [Google Scholar]
- 38.Offermanns S, Toombs CF, Hu YH, Simon MI. Defective platelet activation in G alpha(q)-deficient mice. Nature. 1997;389(6647):183-186. [DOI] [PubMed] [Google Scholar]
- 39.Alshbool FZ, Karim ZA, Vemana HP, Conlon C, Lin OA, Khasawneh FT. The regulator of G-protein signaling 18 regulates platelet aggregation, hemostasis and thrombosis. Biochem Biophys Res Commun. 2015;462(4):378-382. [DOI] [PubMed] [Google Scholar]
- 40.Signarvic RS, Cierniewska A, Stalker TJ, et al. . RGS/Gi2alpha interactions modulate platelet accumulation and thrombus formation at sites of vascular injury. Blood. 2010;116(26):6092-6100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chrzanowska-Wodnicka M, Smyth SS, Schoenwaelder SM, Fischer TH, White GC II. Rap1b is required for normal platelet function and hemostasis in mice. J Clin Invest. 2005;115(3):680-687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Crittenden JR, Bergmeier W, Zhang Y, et al. . CalDAG-GEFI integrates signaling for platelet aggregation and thrombus formation. Nat Med. 2004;10(9):982-986. [DOI] [PubMed] [Google Scholar]
- 43.Canault M, Ghalloussi D, Grosdidier C, et al. . Human CalDAG-GEFI gene (RASGRP2) mutation affects platelet function and causes severe bleeding. J Exp Med. 2014;211(7):1349-1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lozano ML, Cook A, Bastida JM, et al. . Novel mutations in RASGRP2 encoding for CalDAG-GEFI abrogate Rap1 activation causing platelet dysfunction. Blood. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Voronov RS, Stalker TJ, Brass LF, Diamond SL. Simulation of intrathrombus fluid and solute transport using in vivo clot structures with single platelet resolution. Ann Biomed Eng. 2013;41(6):1297-1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang W, King MR. Multiscale modeling of platelet adhesion and thrombus growth. Ann Biomed Eng. 2012;40(11):2345-2354. [DOI] [PubMed] [Google Scholar]
- 47.Leiderman K, Fogelson AL Grow with the flow: a spatial-temporal model of platelet deposition and blood coagulation under flow. Math Med Biol 2011;28(1):47-84. [DOI] [PMC free article] [PubMed]
- 48.Leiderman K, Fogelson AL. The influence of hindered transport on the development of platelet thrombi under flow. Bull Math Biol. 2013;75(8):1255-1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kim OV, Xu Z, Rosen ED, Alber MS. Fibrin networks regulate protein transport during thrombus development. PLOS Comput Biol. 2013;9(6):e1003095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xu Z, Lioi J, Mu J, et al. . A multiscale model of venous thrombus formation with surface-mediated control of blood coagulation cascade. Biophys J. 2010;98(9):1723-1732. [DOI] [PMC free article] [PubMed] [Google Scholar]