Abstract
Publisher's Note: This article has a companion Point by Brass et al.
Publisher's Note: Join in the discussion of these articles at Blood Advances Community Conversations.
Platelets have classically been well recognized for their crucial role in hemostasis; however, it is increasingly evident that platelets are more versatile than originally thought because they possess a large variety of nonhemostatic immunologic functions as well.1 Crosstalk exists between these 2 major functions as inflammation influences both coagulation2 and the immune functions of platelets.3 In this report, we will focus on and advocate for the emerging role of platelet immune functions in a nonhemostatic and inflammatory setting. This includes the ability of platelets to battle invading pathogens during inflammation and to communicate with a large variety of effector cells through an array of different mechanisms.
Platelets initiate their antimicrobial host defense by sensing the presence of pathogens or inflammation through, for example, their multiple immune receptors such as immunoglobulin or complement receptors and Toll-like receptors (TLRs).4 This enables them to bind and recognize invading pathogens and/or their derived microbial products. For instance, platelet TLR4 can bind lipopolysaccharide (a bacterial gram-negative endotoxin) and was shown to induce thrombocytopenia in vivo.5-11 In addition, platelet TLR7 has been suggested to mediate host survival and platelet counts during infection with encephalomyocarditis virus in mice, independently of thrombosis.12
Platelets are also able to retain pathogens by harboring viruses, bacteria, or parasites on their plasma membrane or intracellularly.13-19 Activated platelets were shown to inhibit the growth of the bacterium Staphylococcus aureus through encapsulating the bacteria and secreting the anti-microbial peptide β-defensin to promote the formation of neutrophil extracellular traps (NETs).20 Alternatively, bacterial trapping of methicillin-resistant S aureus and Bacillus cereus has also been shown to occur on hepatic Kupffer cells through a mechanism dependent on engagement of the platelet adhesion receptor glycoprotein (GP)1b.21 In addition, during sepsis, platelet TLR4 was shown to activate neutrophils causing them to release NETs, thereby trapping bacteria in hepatic and pulmonary blood vessels.22
Platelets cannot only detect and retain the pathogens they encounter, they are also able to eliminate them. An elegant example of this was illustrated in studies showing that activated platelets killed the intraerythrocytic malarial parasite Plasmodium falciparum14 through a mechanism involving platelet factor 4 (PF4 or CXCL4) and the erythrocyte Duffy antigen receptor (Fy).23 In another study, it was demonstrated that platelet TLR2 was required for the formation of platelet–neutrophil aggregates that enhanced the phagocytosis of periodontopathogens.24 Furthermore, platelets were found to redirect the course of the blood-borne bacteria Listeria monocytogenes from less immunogenic phagocytes toward the more immunologically active splenic CD8α+ dendritic cells (DCs) in a GPIb- and complement C3–dependent manner.25 Taken together, platelets have the ability to increase the clearance rate of infectious agents and strongly enhance the development of immunity to the infection.
Another way that platelets can actively modulate immune responses is through release of several immune mediators such as platelet CD40L, which is released into the circulation on platelet activation. CD40L can trigger T-cell responses following infection with L monocytogenes26,27 and is able to bind to DCs, thereby impairing DC differentiation, suppressing proinflammatory cytokines, and increasing the secretion of the anti-inflammatory cytokine interleukin-10 (IL-10).28 Through CD40L, platelets are also able to stimulate B-cell differentiation and antibody class switching.29,30 Furthermore, platelets have the ability to secrete a plethora of cytokines and chemokines,4 which not only affects hemostasis and wound repair31 but also various pro- and anti-inflammatory immune responses. For example, the platelet-derived immunosuppressive cytokine transforming growth factor-β is present at low levels during active immune thrombocytopenia; however, on successful treatment of immune thrombocytopenia, the levels of transforming growth factor-β were observed to normalize.32 This correlated with normalized T-regulatory cell numbers and suppression of the immune response.33 In addition, platelet-derived IL-33 was recently suggested to induce eosinophilic airway inflammation.34 On the other hand, PF4 was found to be a negative regulator of Th17 differentiation, thereby limiting cardiac allograft rejection in a murine cardiac transplant model.35
Platelets also release microparticles, which are small extracellular vesicles (the majority are ∼200 nm in diameter) produced via blebbing and fission of the plasma membrane. Although several cells can produce microparticles, platelets appear to be highly effective in their production compared with other cell types.36 Platelet microparticles express membrane phosphatidylserine37 but express only modest levels of tissue factor and appear to have a less defined role in coagulation compared with monocyte-derived microparticles, which express both phosphatidylserine and tissue factor on their surface.38 Platelet microparticles have been associated with immunologic conditions such as platelet activation during inflammation.39,40 For instance, an elevation of platelet microparticles was observed in the blood and synovial fluid of patients with rheumatoid arthritis.41 Several platelet surface receptors have been shown to trigger the formation of platelet microparticles such as GPVI during rheumatoid arthritis,41 TLR4 signaling via lipopolysaccharide during sepsis,42 and FcγRIIa, which may be targeted by immune complexes (of bacterial components or influenza viral epitopes).43,44 The GPVI- and TLR4-mediated signals were also associated with increased IL-1 levels, illustrating their proinflammatory effects. Functionally, platelet microparticles can facilitate communication of platelets with other cells as they can carry a large variety of substances such as various cytokines or chemokines (eg, IL-1, RANTES), lipid mediators, enzymes, surface receptors like CD40L, autoantigens, transcription factors, and respiratory competent mitochondria, all of which can regulate immune functions.3,39,40,45-48 In addition, anucleate platelets contain significant amounts of RNA including mRNA, microRNA, ribosomal and transfer RNA, and antisense RNA (noncoding RNA).49-65 Interestingly, platelets carry the molecular machinery for mRNA translation into proteins and the RNAs may also be transferred to target cells such as endothelial cells via platelet microparticles.49,61-63,65 The interaction between platelets and endothelial cells is complex and well described in the literature, particularly in the setting of atherosclerosis, an inflammatory disease state characterized by immune cell interactions with the vascular wall.29,66
Platelets contain 2 different types of major histocompatibility complex (MHC) class I molecules: plasma-membrane bound or intracellular.67 The plasma-membrane–bound platelet MHC class I is denatured as it is adsorbed from the plasma and induces an immunosuppressive effect on CD8+ T cells during, for example, skin graft rejection.68 On the other hand, the intracellular MHC class I molecules are intact but are only expressed upon platelet activation and can activate antigen-specific CD8+ T cells, as was demonstrated in vivo using an experimental mouse model of cerebral malaria.69
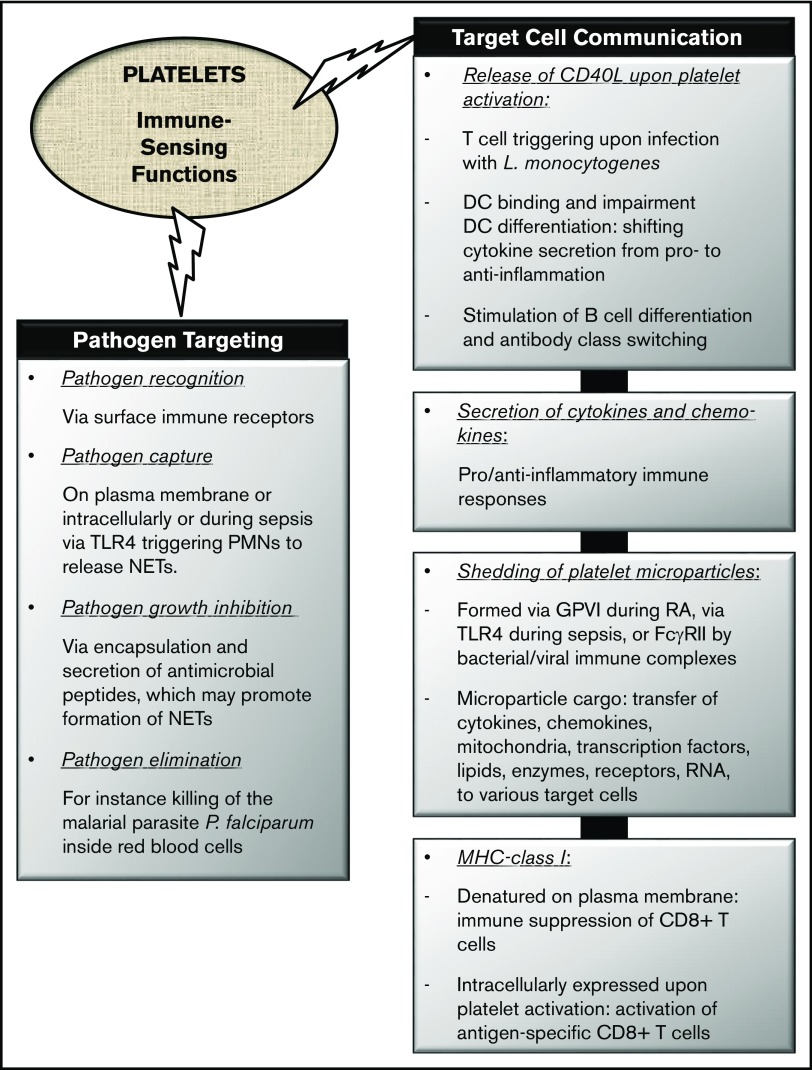
In conclusion, platelets have prominent capabilities in antimicrobial host defense and in regulating the immune functions of a large number of immune cells through their diverse surface receptors and secretion of several mediators. They can also traffic their shed platelet microparticles carrying a heterogeneous immunoregulatory cargo. The immune-sensing functions of platelets are schematically summarized in Figure 1. We therefore strongly encourage further research into the immune-sensing capacity of platelets, which may potentially open up new therapeutic avenues to explore in various disease settings.
Figure 1.
Immune-sensing functions of platelets. The nonhemostatic immune-sensing functions of platelets are generally depicted as pathogen targeting and target cell communication. RA, rheumatoid arthritis.
Acknowledgments
This work was supported by grants from Health Canada and Canadian Blood Services (J.W.S.). R.K. is the recipient of a postdoctoral fellowship from the Canadian Blood Services.
Authorship
Contribution: R.K. wrote the first draft and edited the manuscript; and J.W.S. edited the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: John W. Semple, Lund University, BMC C14, Klinikgatan 26, 221 84 Lund, Sweden; e-mail: john_w.semple@med.lu.se.
References
- 1.Kapur R, Semple JW. The nonhemostatic immune functions of platelets. Semin Hematol. 2016;53(Suppl 1):S2-S6. [DOI] [PubMed] [Google Scholar]
- 2.Foley JH, Conway EM. Cross talk pathways between coagulation and inflammation. Circ Res. 2016;118(9):1392-1408. [DOI] [PubMed] [Google Scholar]
- 3.Kapur R, Zufferey A, Boilard E, Semple JW. Nouvelle cuisine: platelets served with inflammation. J Immunol. 2015;194(12):5579-5587. [DOI] [PubMed] [Google Scholar]
- 4.Semple JW, Italiano JE Jr, Freedman J. Platelets and the immune continuum. Nat Rev Immunol. 2011;11(4):264-274. [DOI] [PubMed] [Google Scholar]
- 5.Andonegui G, Kerfoot SM, McNagny K, Ebbert KV, Patel KD, Kubes P. Platelets express functional Toll-like receptor-4. Blood. 2005;106(7):2417-2423. [DOI] [PubMed] [Google Scholar]
- 6.Cognasse F, Hamzeh H, Chavarin P, Acquart S, Genin C, Garraud O. Evidence of Toll-like receptor molecules on human platelets. Immunol Cell Biol. 2005;83(2):196-198. [DOI] [PubMed] [Google Scholar]
- 7.Aslam R, Speck ER, Kim M, et al. Platelet Toll-like receptor expression modulates lipopolysaccharide-induced thrombocytopenia and tumor necrosis factor-alpha production in vivo. Blood. 2006;107(2):637-641. [DOI] [PubMed] [Google Scholar]
- 8.Semple JW, Aslam R, Kim M, Speck ER, Freedman J. Platelet-bound lipopolysaccharide enhances Fc receptor-mediated phagocytosis of IgG-opsonized platelets. Blood. 2007;109(11):4803-4805. [DOI] [PubMed] [Google Scholar]
- 9.Patrignani P, Di Febbo C, Tacconelli S, et al. Reduced thromboxane biosynthesis in carriers of toll-like receptor 4 polymorphisms in vivo. Blood. 2006;107(9):3572-3574. [DOI] [PubMed] [Google Scholar]
- 10.Ståhl AL, Svensson M, Mörgelin M, et al. Lipopolysaccharide from enterohemorrhagic Escherichia coli binds to platelets through TLR4 and CD62 and is detected on circulating platelets in patients with hemolytic uremic syndrome. Blood. 2006;108(1):167-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang G, Han J, Welch EJ, et al. Lipopolysaccharide stimulates platelet secretion and potentiates platelet aggregation via TLR4/MyD88 and the cGMP-dependent protein kinase pathway. J Immunol. 2009;182(12):7997-8004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koupenova M, Vitseva O, MacKay CR, et al. Platelet-TLR7 mediates host survival and platelet count during viral infection in the absence of platelet-dependent thrombosis. Blood. 2014;124(5):791-802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Youssefian T, Drouin A, Massé JM, Guichard J, Cramer EM. Host defense role of platelets: engulfment of HIV and Staphylococcus aureus occurs in a specific subcellular compartment and is enhanced by platelet activation. Blood. 2002;99(11):4021-4029. [DOI] [PubMed] [Google Scholar]
- 14.McMorran BJ, Marshall VM, de Graaf C, et al. Platelets kill intraerythrocytic malarial parasites and mediate survival to infection. Science. 2009;323(5915):797-800. [DOI] [PubMed] [Google Scholar]
- 15.Flaujac C, Boukour S, Cramer-Bordé E. Platelets and viruses: an ambivalent relationship. Cell Mol Life Sci. 2010;67(4):545-556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Assinger A. Platelets and infection—an emerging role of platelets in viral infection. Front Immunol. 2014;5:649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yeaman MR. Bacterial-platelet interactions: virulence meets host defense. Future Microbiol. 2010;5(3):471-506. [DOI] [PubMed] [Google Scholar]
- 18.Yeaman MR. Platelets in defense against bacterial pathogens. Cell Mol Life Sci. 2010;67(4):525-544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kerrigan SW, Cox D. Platelet-bacterial interactions. Cell Mol Life Sci. 2010;67(4):513-523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kraemer BF, Campbell RA, Schwertz H, et al. Novel anti-bacterial activities of β-defensin 1 in human platelets: suppression of pathogen growth and signaling of neutrophil extracellular trap formation. PLoS Pathog. 2011;7(11):e1002355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wong CH, Jenne CN, Petri B, Chrobok NL, Kubes P. Nucleation of platelets with blood-borne pathogens on Kupffer cells precedes other innate immunity and contributes to bacterial clearance. Nat Immunol. 2013;14(8):785-792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clark SR, Ma AC, Tavener SA, et al. Platelet TLR4 activates neutrophil extracellular traps to ensnare bacteria in septic blood. Nat Med. 2007;13(4):463-469. [DOI] [PubMed] [Google Scholar]
- 23.McMorran BJ, Wieczorski L, Drysdale KE, et al. Platelet factor 4 and Duffy antigen required for platelet killing of Plasmodium falciparum. Science. 2012;338(6112):1348-1351. [DOI] [PubMed] [Google Scholar]
- 24.Assinger A, Laky M, Schabbauer G, et al. Efficient phagocytosis of periodontopathogens by neutrophils requires plasma factors, platelets and TLR2. J Thromb Haemost. 2011;9(4):799-809. [DOI] [PubMed] [Google Scholar]
- 25.Verschoor A, Neuenhahn M, Navarini AA, et al. A platelet-mediated system for shuttling blood-borne bacteria to CD8α+ dendritic cells depends on glycoprotein GPIb and complement C3. Nat Immunol. 2011;12(12):1194-1201. [DOI] [PubMed] [Google Scholar]
- 26.Elzey BD, Schmidt NW, Crist SA, et al. Platelet-derived CD154 enables T-cell priming and protection against Listeria monocytogenes challenge. Blood. 2008;111(7):3684-3691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Iannacone M, Sitia G, Isogawa M, et al. Platelets mediate cytotoxic T lymphocyte-induced liver damage. Nat Med. 2005;11(11):1167-1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kissel K, Berber S, Nockher A, Santoso S, Bein G, Hackstein H. Human platelets target dendritic cell differentiation and production of proinflammatory cytokines. Transfusion. 2006;46(5):818-827. [DOI] [PubMed] [Google Scholar]
- 29.von Hundelshausen P, Weber C. Platelets as immune cells: bridging inflammation and cardiovascular disease. Circ Res. 2007;100(1):27-40. [DOI] [PubMed] [Google Scholar]
- 30.Elzey BD, Tian J, Jensen RJ, et al. Platelet-mediated modulation of adaptive immunity. A communication link between innate and adaptive immune compartments. Immunity. 2003;19(1):9-19. [DOI] [PubMed] [Google Scholar]
- 31.Mazzucco L, Borzini P, Gope R. Platelet-derived factors involved in tissue repair-from signal to function. Transfus Med Rev. 2010;24(3):218-234. [DOI] [PubMed] [Google Scholar]
- 32.Assoian RK, Komoriya A, Meyers CA, Miller DM, Sporn MB. Transforming growth factor-beta in human platelets. Identification of a major storage site, purification, and characterization. J Biol Chem. 1983;258(11):7155-7160. [PubMed] [Google Scholar]
- 33.McKenzie CG, Guo L, Freedman J, Semple JW. Cellular immune dysfunction in immune thrombocytopenia (ITP). Br J Haematol. 2013;163(1):10-23. [DOI] [PubMed] [Google Scholar]
- 34.Takeda T, Unno H, Morita H, et al. Platelets constitutively express IL-33 protein and modulate eosinophilic airway inflammation [published online ahead of print April 4, 2016]. J Allergy Clin Immunol. doi:10.1016/j.jaci.2016.01.032. [DOI] [PubMed] [Google Scholar]
- 35.Shi G, Field DJ, Ko KA, et al. Platelet factor 4 limits Th17 differentiation and cardiac allograft rejection. J Clin Invest. 2014;124(2):543-552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arraud N, Linares R, Tan S, et al. Extracellular vesicles from blood plasma: determination of their morphology, size, phenotype and concentration. J Thromb Haemost. 2014;12(5):614-627. [DOI] [PubMed] [Google Scholar]
- 37.Morel O, Jesel L, Freyssinet JM, Toti F. Cellular mechanisms underlying the formation of circulating microparticles. Arterioscler Thromb Vasc Biol. 2011;31(1):15-26. [DOI] [PubMed] [Google Scholar]
- 38.Owens AP III, Mackman N. Microparticles in hemostasis and thrombosis. Circ Res. 2011;108(10):1284-1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nurden AT. Platelets, inflammation and tissue regeneration. Thromb Haemost. 2011;105(Suppl 1):S13-S33. [DOI] [PubMed] [Google Scholar]
- 40.Reid VL, Webster NR. Role of microparticles in sepsis. Br J Anaesth. 2012;109(4):503-513. [DOI] [PubMed] [Google Scholar]
- 41.Boilard E, Nigrovic PA, Larabee K, et al. Platelets amplify inflammation in arthritis via collagen-dependent microparticle production. Science. 2010;327(5965):580-583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brown GT, McIntyre TM. Lipopolysaccharide signaling without a nucleus: kinase cascades stimulate platelet shedding of proinflammatory IL-1β-rich microparticles. J Immunol. 2011;186(9):5489-5496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Boilard E, Paré G, Rousseau M, et al. Influenza virus H1N1 activates platelets through FcγRIIA signaling and thrombin generation. Blood. 2014;123(18):2854-2863. [DOI] [PubMed] [Google Scholar]
- 44.Sun D, Popescu NI, Raisley B, et al. Bacillus anthracis peptidoglycan activates human platelets through FcγRII and complement. Blood. 2013;122(4):571-579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cloutier N, Tan S, Boudreau LH, et al. The exposure of autoantigens by microparticles underlies the formation of potent inflammatory components: the microparticle-associated immune complexes. EMBO Mol Med. 2013;5(2):235-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Boudreau LH, Duchez AC, Cloutier N, et al. Platelets release mitochondria serving as substrate for bactericidal group IIA-secreted phospholipase A2 to promote inflammation. Blood. 2014;124(14):2173-2183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ray DM, Spinelli SL, Pollock SJ, et al. Peroxisome proliferator-activated receptor gamma and retinoid X receptor transcription factors are released from activated human platelets and shed in microparticles. Thromb Haemost. 2008;99(1):86-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Garcia BA, Smalley DM, Cho H, Shabanowitz J, Ley K, Hunt DF. The platelet microparticle proteome. J Proteome Res. 2005;4(5):1516-1521. [DOI] [PubMed] [Google Scholar]
- 49.Laffont B, Corduan A, Plé H, et al. Activated platelets can deliver mRNA regulatory Ago2•microRNA complexes to endothelial cells via microparticles. Blood. 2013;122(2):253-261. [DOI] [PubMed] [Google Scholar]
- 50.Rowley JW, Oler AJ, Tolley ND, et al. Genome-wide RNA-seq analysis of human and mouse platelet transcriptomes. Blood. 2011;118(14):e101-e111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rowley JW, Schwertz H, Weyrich AS. Platelet mRNA: the meaning behind the message. Curr Opin Hematol. 2012;19(5):385-391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lood C, Amisten S, Gullstrand B, et al. Platelet transcriptional profile and protein expression in patients with systemic lupus erythematosus: up-regulation of the type I interferon system is strongly associated with vascular disease. Blood. 2010;116(11):1951-1957. [DOI] [PubMed] [Google Scholar]
- 53.Healy AM, Pickard MD, Pradhan AD, et al. Platelet expression profiling and clinical validation of myeloid-related protein-14 as a novel determinant of cardiovascular events. Circulation. 2006;113(19):2278-2284. [DOI] [PubMed] [Google Scholar]
- 54.Goodall AH, Burns P, Salles I, et al. ; Bloodomics Consortium. Transcription profiling in human platelets reveals LRRFIP1 as a novel protein regulating platelet function. Blood. 2010;116(22):4646-4656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Simon LM, Edelstein LC, Nagalla S, et al. Human platelet microRNA-mRNA networks associated with age and gender revealed by integrated plateletomics. Blood. 2014;123(16):e37-e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Edelstein LC, Simon LM, Montoya RT, et al. Racial differences in human platelet PAR4 reactivity reflect expression of PCTP and miR-376c. Nat Med. 2013;19(12):1609-1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Plé H, Maltais M, Corduan A, Rousseau G, Madore F, Provost P. Alteration of the platelet transcriptome in chronic kidney disease. Thromb Haemost. 2012;108(4):605-615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McManus DD, Beaulieu LM, Mick E, et al. Relationship among circulating inflammatory proteins, platelet gene expression, and cardiovascular risk. Arterioscler Thromb Vasc Biol. 2013;33(11):2666-2673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Freedman JE, Larson MG, Tanriverdi K, et al. Relation of platelet and leukocyte inflammatory transcripts to body mass index in the Framingham heart study. Circulation. 2010;122(2):119-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Raghavachari N, Xu X, Harris A, et al. Amplified expression profiling of platelet transcriptome reveals changes in arginine metabolic pathways in patients with sickle cell disease. Circulation. 2007;115(12):1551-1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Risitano A, Beaulieu LM, Vitseva O, Freedman JE. Platelets and platelet-like particles mediate intercellular RNA transfer. Blood. 2012;119(26):6288-6295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Clancy L, Freedman JE. New paradigms in thrombosis: novel mediators and biomarkers platelet RNA transfer. J Thromb Thrombolysis. 2014;37(1):12-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gidlöf O, van der Brug M, Ohman J, et al. Platelets activated during myocardial infarction release functional miRNA, which can be taken up by endothelial cells and regulate ICAM1 expression. Blood. 2013;121(19):3908-3917, S1-S26. [DOI] [PubMed] [Google Scholar]
- 64.Landry P, Plante I, Ouellet DL, Perron MP, Rousseau G, Provost P. Existence of a microRNA pathway in anucleate platelets. Nat Struct Mol Biol. 2009;16(9):961-966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rondina MT, Weyrich AS. Regulation of the genetic code in megakaryocytes and platelets. J Thromb Haemost. 2015;13(Suppl 1):S26-S32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Libby P, Lichtman AH, Hansson GK. Immune effector mechanisms implicated in atherosclerosis: from mice to humans. Immunity. 2013;38(6):1092-1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shulman NR, Aster RH, Pearson HA, Hiller MC. Immunoreactions involving platelet. VI. Reactions of maternal isoantibodies responsible for neonatal purpura. Differentiation of a second platelet antigen system. J Clin Invest. 1962;41:1059-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Aslam R, Speck ER, Kim M, Freedman J, Semple JW. Transfusion-related immunomodulation by platelets is dependent on their expression of MHC Class I molecules and is independent of white cells. Transfusion. 2008;48(9):1778-1786. [DOI] [PubMed] [Google Scholar]
- 69.Chapman LM, Aggrey AA, Field DJ, et al. Platelets present antigen in the context of MHC class I. J Immunol. 2012;189(2):916-923. [DOI] [PMC free article] [PubMed] [Google Scholar]