Abstract
BACKGROUND:
Newborns who are prenatally exposed to methadone are at risk for neonatal abstinence syndrome and the associated excess weight loss and poor weight gain. This pilot feasibility study aimed to evaluate early caloric enhancement on weight patterns among infants born to women receiving methadone maintenance therapy while pregnant.
METHODS:
In this double-blind pilot feasibility study, we randomly assigned infants with fetal methadone exposure to 24 or 20 kcal/oz formula from days 3 to 21. Randomization was stratified by any breastfeeding, sex of the infant, and gestational age. Eligible infants were ≥35 weeks’ gestation and weighed ≥2200 g. Outcomes were days to weight nadir, maximum percent weight loss, days to birth weight, percentage weight change per day, and feasibility.
RESULTS:
A total of 49 infants were randomly assigned (22 to standard- and 27 to high-calorie formula); groups had comparable demographic characteristics. Main outcomes comparing standard- to high-calorie formula groups were not significant (days to weight nadir, 5.0 vs 4.4 days; P = .20; maximum percent weight loss, −9.4% vs −8.6%; P = .15; days to birth weight, 14.7 vs 13.6 days; P = .07); however, in longitudinal analyses (days 4 to 21), the high-calorie group had a higher percent weight gained per day compared with the standard-calorie group (P <.001). There were high levels of protocol adherence, and no adverse effects were observed.
CONCLUSIONS:
Study findings suggest that early initiation of high-calorie formula for infants with prenatal methadone exposure may be beneficial for weight gain; evaluation in a larger study is warranted.
Opioid use during pregnancy has tripled during the last decade, and as a result, increasing numbers of newborns experience neonatal abstinence syndrome (NAS).1,2 Among infants exposed to long-acting opioids, such as methadone, 50% to 75% will develop symptoms requiring pharmacologic treatment.3–6 NAS signs and symptoms interfere with infant feeding in a variety of ways and thus impair an infant’s nutritional status. High muscle tone, jitteriness, sweating, excessive crying, vomiting, and diarrhea increase the caloric needs of infants. Weak and uncoordinated suckling associated with opioid withdrawal can impair infants’ abilities to consume adequate calories.7,8 Thus, experts in the field of neonatology have suggested that infants who are withdrawing from opioids may require additional calories.9–11
Because of a lack of prospective studies to support nutritional management, currently, infants who are being observed or treated for NAS are fed a wide variety of diets.12 Findings from a recent national survey on the management of NAS reported that in one-third of nurseries, opioid-exposed infants are fed caloric-enhanced formula or breast milk.12 Three retrospective studies in which researchers evaluated weight patterns in opioid-exposed infants support this need.11,13–15 They found that methadone-exposed infants lost excessive weight, returned to their birth weight later than unexposed infants, and many experience hyperphagia. These studies suggest increased caloric needs of methadone-exposed infants. In a medical record review at our own institution for weight patterns among 202 infants with fetal opioid exposure, we found weight loss to be more problematic in infants who are exposed to methadone than to in those exposed to other opioids. Therefore, we focused our work on methadone-exposed infants only.
Early caloric enhancement for infants who are exposed to methadone is conceptually appealing, readily available, easy to implement, and could result in improved weight management. Therefore, in this randomized clinical study, we aimed to explore the feasibility of using of high-calorie formula among methadone-exposed newborns to prevent excessive weight loss and late return to birth weight. We hypothesized that infants who were fed high-calorie formula from early infancy would have earlier weight nadir, a lower maximum percent weight loss, and a faster return to birth weight than those who were fed standard-calorie formula.
Methods
We conducted a randomized, double-blind intervention study of standard- (20 kcal/oz) versus high-calorie (24 kcal/oz) formula on weight trajectory among infants whose mothers were prescribed methadone during pregnancy. This feasibility study was not powered to demonstrate a statistically significant impact on outcomes but rather to assess method feasibility, safety, and outcome trends. Infants received study formula from days 3 to 21, the peak time of NAS symptoms, and had follow-up visits at months 1 and 3.
Study Population
Mothers were eligible if they were 18 to 45 years of age, received methadone from a licensed treatment program during pregnancy, and delivered at a large, urban hospital. We recruited women both during pregnancy with intention to deliver at the hospital and within 48 hours of birth. Women who intended to place their infants for adoption were excluded. Infants were randomly assigned before 72 hours of life if their birth weight was at least 2200 g, gestational age was at least 35 weeks, no major congenital malformations that could interfere with feeding or weight gain were identified, and the infants were not admitted to the NICU for more than 24 hours for medical conditions other than NAS treatment before 3 days of life. Premixed 24 kcal/oz soy formula was not available; therefore, mothers planning to use soy formula were also excluded.
Randomization
Eligible infants were randomly assigned within strata defined by gestational age groups (35–36, 37–38, and ≥39 weeks), sex (male or female), and feeding method (any breast milk or all formula). Assignment sequences, generated in blocks of 6 for each stratum by using SPSS (IBM SPSS Statistics, IBM Corporation, Armonk, NY), were provided by the statistician directly to the pharmacist. Parents, nurses, pediatric providers, and study staff were blinded to formula assignment. Only the hospital pharmacist who prepared labels covering the original labels, the statistician, and the medical monitor had access to randomization lists before the study’s completion.
Treatment
Infants received study formula (Enfamil 20 or 24 kcal/oz ready-to-feed formula with randomization labels covering the original labels) beginning at 72 hours of life on demand every 3 to 4 hours (hospital routine). At study initiation, Enfamil was the only cow milk–based, term infant formula sold in ready-to-feed bottles in both 20 and 24 kcal/oz concentrations. Infants remained on study formula through 21 days of life. Infants discharged from the hospital before age 21 days were provided with study formula for the remaining protocol days.
Breastfeeding is associated with better NAS outcomes; therefore, per hospital routine, women were counseled on the benefits of breastfeeding and were offered breastfeeding support. Women were included in the study regardless of their breastfeeding plans. To account for feeding method, randomization was stratified by feeding method in the first 48 hours (any breast milk versus all formula). Infants were fed on the basis of the following priority and availability: breastfeeding at the breast, expressed breast milk, and then study formula.
Nurses were instructed to record each feeding (type and volume) on flowsheets (hospital routine). At discharge, parents were given instruction on how to maintain daily feeding logs (volume and type). For breastfeeding, feeding was recorded without a volume. A portable scale (seca model 334; seca, Chino, CA) was provided for daily weights at home. Research staff contacted mothers daily to review weights and feeding and reminded mothers to stop study formula at day 21. When a mother could not be reached by telephone, staff visited mothers at home or at their methadone treatment programs.
Opioid-exposed infants born at the hospital were cared for by using a standard protocol,16 which included assessing NAS with the modified Finnegan Scale and treating them with morphine as first-line pharmacologic management.
Safety Measures
Guidelines for stopping study formula were established before study initiation, including changing to open-label, high-calorie formula if the infant was still losing weight at 10 days, lost >15% of his or her birth weight, or was not gaining at least 15 g per day by 14 days, and changing to open-label, standard-calorie formula if the infant was gaining an average of 75 g per day over a 2-week interval. An infant with cow milk–based formula intolerance, as determined clinically by the infant’s doctor, would be taken off study formula but remain in the study under intention-to-treat analysis. An infant’s doctor could request that the assigned formula be stopped at his or her discretion. Finally, infants with ≥10 stools per day and who were still losing weight after day 10 would have electrolytes obtained.
Primary Outcomes
Primary outcome measures were days to weight nadir, maximum percent weight loss, days to return to birth weight, and percentage weight change per day from days 4 to 21. Infants were weighed at birth, 24 hours of life, and then daily by using a scale accurate to ±2 g. Starting at 48 hours of life, study infants were weighed twice each day by nursing staff. If the 2 weights differed by more than 10 g, nurses weighed infants a third time, and the 2 closest weights were averaged to determine that day’s weight. Parents of infants who were discharged before 21 days of age and were not back to their birth weight for 2 consecutive days were loaned a portable infant scale. Parents received scale training and were provided written instructions on triple weighing procedures until the infants were 21 days old or had 2 consecutive days at greater than their birth weight. Infants were triple weighed and measured at their 1- and 3-month visits by study staff.
Feasibility
Feasibility was assessed by the ability to obtain daily weights after discharge, return of loaned infant scales, follow-up rates, and adherence to weighing protocols.
Data Analysis
Baseline demographic and clinical characteristics for mothers and infants were compared by using χ2 tests and Fisher exact tests for categorical variables and t tests for continuous variables. All statistical tests were performed by using a 2-tailed α level of .05.
Outcomes for infants who were randomly assigned to standard- versus high-calorie formula were compared with the following statistical methods: days to weight nadir and return to birth weight with log-rank tests; maximum percent weight loss with t tests; and daily percent weight loss (or gain) from days 4 to 21 with mixed-effects linear regression, inclusion of a day-squared term, and an interaction between days-squared and treatment to allow for nonlinearity in the effect of high-calorie formula on percent weight gain. The primary analysis was intention-to-treat with infants retained in the assigned groups for the study duration.
We also conducted a post hoc analysis of percent weight gain with pattern of formula received (rather than intention to treat) as the independent variable. There were 4 patterns of formula given: always standard-calorie, always high-calorie, standard- changed to high-calorie (either by protocol rules or an infant’s doctor), and high- changed to standard-calorie soy formula. This 4-category variable was used as a covariate in the post hoc analyses.
Human subject approval was obtained from our university. Women in the study signed written, informed consent forms and releases of information for themselves and their infants.
Results
Randomization
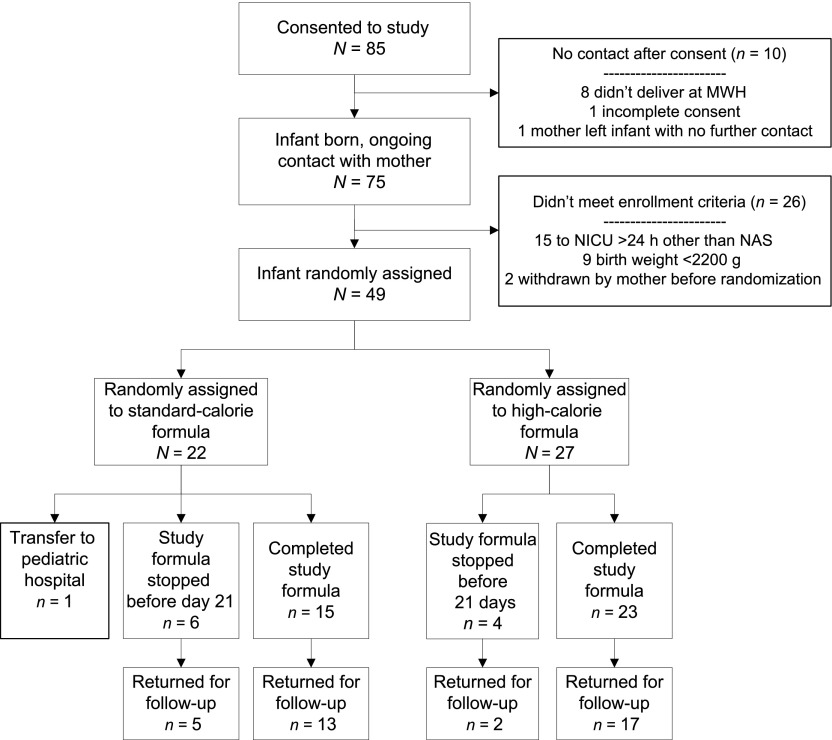
Among 85 mother-infant dyads who consented from July 2010 through August 2012, 10 were lost to follow-up before randomization, 26 did not meet eligibility for randomization (primarily because their NICU stays were longer than 24 hours and birth weights were <2200 g), and 49 were randomly assigned (Fig 1).
FIGURE 1.
Consort diagram. MWH, Magee-Womens Hospital.
Demographics
Mother-infant dyad groups were comparable in nearly all characteristics (Table 1). Infants in the high-calorie group were marginally smaller than infants in the standard-calorie group (P = .07 for birth weight and P = .08 for birth length). The majority of mothers were white, Medicaid insured, smoked during pregnancy, and began methadone therapy before their second trimester. The mean and median daily methadone dose was 112 mg (SD: 64.9 mg) and 100 mg (range: 10 to 225 mg) for women whose infants were in the standard-calorie compared with 95 mg (SD: 37.5 mg) and 95 mg (range: 20 to 160 mg) for those in the high-calorie group (P = .24). There were no significant differences between groups in the percentage of infants treated for NAS and the number of days treated for NAS. Fewer than half of infants were ever fed breast milk, and none were exclusively breastfed. Among infants who received any breast milk, the proportion of breast milk feeding at days 1 to 14 were comparable.
TABLE 1.
Comparison of Demographic Characteristics by Formula Randomization Group
| Characteristics | Standard-Calorie Group, N = 22 | High-Calorie Group, N = 27 | Pa | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Mother | |||||
| White race | 20 | 91 | 26 | 96 | .19 |
| Age, y | |||||
| 18–24 | 7 | 33 | 8 | 30 | .15 |
| 25−29 | 6 | 29 | 15 | 56 | |
| ≥30 | 8 | 38 | 4 | 15 | |
| Primiparous | 5 | 23 | 7 | 26 | 1.00 |
| Public insurance | 20 | 90 | 24 | 93 | 1.00 |
| Cesarean delivery | 4 | 18 | 7 | 26 | .73 |
| Prepregnancy BMIb | |||||
| Underweight (<18.5) | 1 | 5 | 3 | 12 | .10 |
| Normal weight (18.5–24.9) | 11 | 52 | 10 | 40 | |
| Overweight (25.0–29.9) | 4 | 19 | 11 | 44 | |
| Obese (≥30.00) | 5 | 24 | 1 | 4 | |
| Smoked during pregnancyc | 20 | 91 | 21 | 78 | .27 |
| <1 pack per d | 9 | 47 | 11 | 55 | .87 |
| ≥1 pack per d | 10 | 53 | 9 | 45 | |
| Hepatitis C–positive | 12 | 60 | 17 | 63 | .57 |
| Methadone dose at delivery | |||||
| <100 mg per d | 11 | 50 | 10 | 40 | .49 |
| ≥100 mg per d | 11 | 50 | 15 | 60 | |
| Methadone treatment started | |||||
| Before pregnancy | 12 | 55 | 12 | 44 | .64 |
| First trimester | 4 | 18 | 8 | 30 | |
| Second to third trimester | 6 | 28 | 7 | 26 | |
| Urine drug screen at delivery positive for illicit drug | 3 | 14 | 8 | 30 | .30 |
| Infant | |||||
| Female sex | 12 | 54 | 15 | 56 | .94 |
| Race | |||||
| White | 18 | 82 | 24 | 89 | .67 |
| African American | 1 | 5 | 0 | 0 | |
| Biracial | 3 | 14 | 3 | 11 | |
| Gestational age, wk | |||||
| 35–36 | 3 | 14 | 1 | 4 | .42 |
| 37–38 | 6 | 27 | 10 | 37 | |
| ≥39 | 13 | 59 | 16 | 59 | |
| Ever treated for NAS | 16 | 73 | 18 | 67 | .76 |
| Ever fed breast milk | 8 | 36 | 13 | 48 | .56 |
| >50% breast milk feeds on day 3 | 1 | 5 | 2 | 7 | 1.00 |
| Any breast milk at discharge | 4 | 15 | 6 | 22 | .73 |
| Infant screen at delivery positive for drug other than methadone | 0 | 0 | 6 | 22 | .03 |
| Mean (SD) | Median (Range) | Mean (SD) | Median (Range) | Pd | |
| Birth wt, kg | 3.05 (0.50) | 3.09 (2.32 to 3.88) | 2.82 (0.36) | 2.89 (2.29 to 3.45) | .07 |
| Birth length, cm | 47.4 (2.1) | 48 (42.5 to 50) | 46.4 (2.0) | 47 (43 to 50.8) | .08 |
| Birth head circumference, cm | 33.2 (1.9) | 33.5 (29.5 to 37.5) | 32.6 (1.3) | 32.2 (30.5 to 34.8) | .23 |
| Days treated for NASe | 14.4 (7.0) | 13 (4 to 29) | 17.1 (9.0) | 15 (7 to 46) | .34 |
Based on Fisher's exact test when the frequency in any cell was <8, and chi square if all cell sizes 8 or more.
Three subjects had missing maternal BMI data.
Two subjects had a missing quantity of cigarette use.
Based on t tests of comparison for independent means.
Only infants treated for NAS.
Primary Outcomes (Intent to Treat)
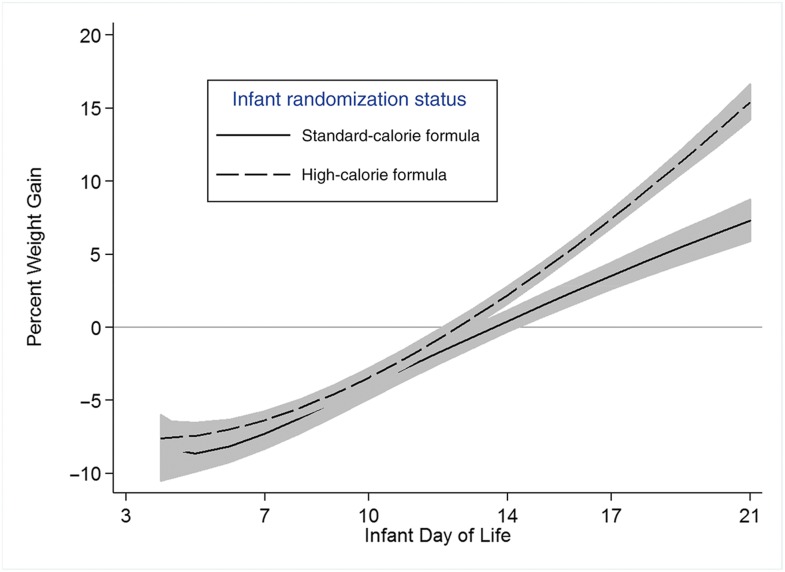
Before starting with the study formula, the groups had comparable percentages of weight loss at day 3. There were no statistically significant differences in primary outcomes between the high- and standard-calorie formula groups, but trends favored the high-calorie group (Table 2). The longitudinal model (Fig 2) of percentage weight change per day with assigned formula demonstrates that infants in both groups gained increasingly more weight over time, but this increase was larger for infants in the high-calorie group compared with infants in the standard-calorie group (P <.001).
TABLE 2.
Primary Outcome Measures by Randomized Feeding Group (Intention to Treat)
| Outcome Measures | Standard-Calorie Formula | High-Calorie Formula | Pa | ||
|---|---|---|---|---|---|
| Mean (SD) | Median (Range) | Mean (SD) | Median (Range) | ||
| Days to weight nadir | N = 22 | N = 27 | |||
| 5.0 | 5 (2 to 8) | 4.4 | 4 (2 to 8) | .20 | |
| Days to return to birth wt | N = 20b | N = 26b | |||
| 14.7 | 14.5 (9 to 21) | 13.6 | 14 (8 to 20) | .08 | |
| Maximum weight loss, %c | −9.4 (2.6) | −9.7 (−13.8 to −5.1) | −8.6 (2.3) | −9.2 (−13.6 to −3.6) | .15 |
| Average daily weight gain after return to birth wt, %d | 0.67 (0.69) | 0.43 (0.01 to 3.7) | 0.81 (0.65) | 0.70 (0.01 to 3.3) | .11 |
Time to event data statistics is based on log-rank statistics.
Two infants from the standard-calorie group and 1 infant from the high-calorie group were lost to follow-up before returning to birth weight and were excluded from that analysis.
Based on longitudinal estimates excluding day of life.
Maximum percent weight loss (or gain) statistics are based on t tests with assumed equal variances.
FIGURE 2.
Results of the longitudinal analyses of weight change over time for infants in the 2 treatment groups. The lines represent the mean percent weight gain, and the shaded areas are the 95% confidence intervals of the lines. The differences in the 2 lines are a function of days; the lines diverge more as the days increase, which necessitates a day-squared term. The increase in percent weight gain between days 4 and 21 was estimated by −12% + 0.62% × day + 0.02% × day2 for the standard-calorie group and by −9% + 0.01% × day + 0.06 × day2 for the high-calorie group. Overall, the model with treatment, day and day2, and the interactions of treatment by day and treatment by day2 has a χ2 (degrees of freedom = 5) of 4316.67 and a P value <.001. All individual terms and interactions had a P value <.08.
There were no significant differences between groups in the mean daily volume of feeding, 182 vs 188 mL/kg per day (P = .9), from days 3 to 14. Infants in the 2 groups had comparable weights, lengths, and head circumferences at their 1- and 3-month follow-up visits.
Post Hoc Analyses
Because this was a feasibility study designed to inform a larger study, we also conducted post hoc longitudinal analyses based on actual feeding patterns in addition to the intention-to-treat analysis. We grouped infants into 4 groups: always standard-calorie (n = 16), changed from standard- to high-calorie (n = 6), changed from high- to standard-calorie (n = 3), and always high-calorie soy formula (n = 24). The always high-calorie group had a significantly higher percent gain per day than the always standard-calorie group (0.005) whereas infants who changed from the standard- to high-calorie formula had a significantly lower percent weight gain than the always standard-calorie infants (P <.0001). The 6 infants in the standard-calorie changed to high-calorie group compared with the 16 in the standard-calorie not changed to high-calorie group were more likely to be treated for NAS (67% vs 37%), and their mothers were older (31 vs 27 years; P = .05) and more likely to be prescribed higher doses of methadone during pregnancy (0.05). Care must be taken to interpret these finding because this is a small group, and decisions to move infants to high-calorie formula were made by nonstudy physicians (n = 4) as well as according to the study protocol (n = 2). It is likely that the significant covariates are confounded.
Feasibility and Safety
Ten infants stopped taking the study formula before day 21 (Table 3). Three infants from the high-calorie group were changed to soy formula on the basis of a pediatrician’s (n = 1) or the mother’s (n = 2) decision. One infant in the high-calorie (4%) and 6 in the standard-calorie group (27%) were changed to open-label, high-calorie formula because of concern for slow weight gain. Despite these formula changes, outcomes were analyzed by using an intention-to-treat model.
TABLE 3.
Infants Removed From Assigned Study Formula
| No. Infants | Day Study Formula Stopped | Reason for Removala |
|---|---|---|
| High-calorie group (n = 4) | ||
| 2 | 6, 9 | Placed on standard-calorie soy formula for maternal concern with milk allergy |
| 1 | 5 | Placed on standard-calorie soy formula by pediatrician for concern of milk allergy |
| 1 | 6 | Placed on open-label, high-calorie, cow milk formula for wt loss of 10.3% |
| Standard-calorie group (n = 6) changed to high-calorie formula | ||
| 2 | 4, 6 | Doctors withdrew infants from study and placed on high-calorie, cow milk formula for wt loss of 13.8% (day 4) and 11.5% (day 6) |
| 1 | 11 | Infant was discharged to foster care. Primary care provider wanted infant on high-calorie formula; weight loss was 3.9% |
| 1 | 12 | Infant had wt loss of 11.3% at day 12 and slow wt gain from days 6 to 12 (9 g per d) |
| 1 | 14b | Infant had wt loss of 6.36% at day 14b |
| 1 | 16b | Infant had wt loss of 8.8% at day 16b |
| Infants lost to follow-up before reaching birth wt or day 21 | ||
| High-calorie group (n = 6) | ||
| 6 | 8, 14, 16, 18(2), 19 | Lost to follow-up after discharge from the hospital |
| Standard calorie group (n = 3) | ||
| 2a | 15, 18 | Lost to follow-up at discharge from hospital |
| 1 | 9 | Transfer to pediatric hospital for surgical consult |
Infants remained in analyses until they were discharged from the hospital or mothers stopped reporting weights.
Met predetermined criteria of not gaining at least 15 g per day by day 14.
The mean number of stools per day from days 3 to 14 was not different between groups (mean for both was 3.75 per day; P = .45), and no infants met protocol criteria for electrolyte analysis. Hyperphagia (>190 mL/kg per day) was common, with 66% of infants demonstrating hyperphagia between days 7 and 14. There was no difference in the proportion of infants who experienced hyperphagia by group. Infants in both groups had a significantly greater maximum percent weight loss compared with published literature on healthy newborn weight changes.17
Although the infants were hospitalized, adherence to study protocol was excellent; nearly all infants had repeated daily weights by nursing staff, and the repeated daily weights were within 10 g of each other for >95% of the measurements. Weights were available for all infants at day 7, and weights for 46 (94%) infants were available at day 14 (29 infants were hospitalized, and 17 were home). Only 7 of the 49 (14%) mothers did not report weights for their infants after discharge.
Discussion
This is the first double-blind randomized trial in which researchers compare high-calorie to standard-calorie formula for infants with prenatal methadone exposure. In this feasibility study, we found that introducing high-calorie formula preventively resulted in a nonsignificant trend toward an earlier return to birth weight and significantly larger daily weight gains. High levels of adherence to protocols were observed, and no adverse effects were observed.
Currently, there is significant variation in the nutritional management of infants with NAS.12 Some hospitals introduce high-calorie formula to opioid-exposed infants preventively whereas others wait and start only after infants demonstrate excessive or persistent weight loss.12
This variation is not surprising given the limited previous data to support evidence-based nutritional interventions. Weinberger11 reported that among 101 methadone-exposed newborns, those treated for NAS compared with those not treated lost more weight, reached weight nadir later, and returned to birth weight later. Dryden et al15 reported that among 354 methadone-exposed infants, the median maximal weight losses were 10.2% and 8.5% for breast- and formula-fed infants, respectively, which are significantly more than for unexposed infants. Martinez et al14 found that among 44 methadone-exposed infants, 56% had hyperphagia (>190 mL/kg per day) by 2 weeks of age. Like Weinberger et al13 and Dryden et al,15 we found that methadone-exposed infants experience a higher percent weight loss, later weight nadir, and later return to birth weight than what’s described for healthy infants.17,18 Like Martinez et al,14 we found that 66% of infants were hyperphagic between 7 and 14 days and similarly conclude that hyperphagia likely represents the need for additional calories for infants who are withdrawing from methadone compared with healthy infants.
We established a priori criteria for stopping randomized formula but also allowed the infants’ doctors to stop study formula without breaking blind. Six infants in the standard-calorie group (27%) experienced excessive weight loss requiring a change to open-label, high-calorie formula. In our intention-to-treat analysis, this change would have biased our results to the null. Three infants from the high-calorie group were changed to soy formula at either their pediatricians’ or mothers’ request. It is possible that this perceived formula intolerance was due to the higher caloric content. Again, this change would bias our intention-to-treat analysis for our main outcome measures to the null. We did not observe a difference in the number of stools per day among infants in the 2 groups.
It is important to consider breastfeeding in studies of NAS because findings consistently demonstrate that infants who are fed breast milk compared with formula experience less severe NAS and are less likely to need pharmacologic treatment for NAS.19–23 In our study, we stratified randomization by feeding method (any breast milk or all formula). Women in this study were counseled on the benefits of breastfeeding and were offered hands-on support from medical and research staff. The breastfeeding rate we report is better than what has been reported by others. Wachman et al24 reported that among a similar population, only one-quarter of women who were delivering at their Baby-Friendly–designated hospital and deemed eligible to breastfeed (based on predetermined criteria) did so, and most breastfed for a short duration and not exclusively. Women in our study also breastfed at low rates; fewer than half ever breastfed, and most stopped after just a few days. The national rate of any breastfeeding at the time of this study exceeded 75%.25 Given the small number of infants receiving significant quantities of breast milk, we are not able to draw conclusions from this study about breast milk feeding on weight gain and loss. However, Dryden et al15 reported that methadone-exposed infants who were exclusively breastfed had earlier weight nadir compared with those who were fed formula or a combination of formula and breast milk. As explained by Jansson et al,10 despite the specific benefits of breastfeeding, breastfeeding for this population is challenging and usually of limited duration.
There are a number of limitations to this feasibility study. It was a small sample, and the formula exposure was of limited duration; infants received study formula only from days 3 to 21, which is the time of maximum NAS symptoms. Of infants, ∼35% (26 of 75; mostly infants enrolled during pregnancy) did not meet randomization criteria largely because of admission to the NICU for issues other than NAS and low birth weight. The high rate of low birth weight, prematurity, or NICU care for conditions other than NAS underscores the high-risk status of this population. Furthermore, we only enrolled infants who were exposed to methadone and not to buprenorphine or other opioids. These selection criteria limit the generalizability of the study but are crucial for informing larger follow-up studies.
The study findings suggest that early initiation of high-calorie formula may improve weight gain patterns for infants with prenatal methadone exposure. Starting high-calorie formula was not associated with increased stool output. If confirmed in a larger study, consideration should be given to proactively starting high-calorie formula when breast milk is not available rather than waiting until infants with NAS experience excessive weight loss or inadequate weight gain.
Acknowledgments
We acknowledge Magee-Womens Hospital of UPMC’s newborn nursery and the NICU staff, the staff at the Children’s Home of Pittsburgh, Ray Cefola, PharmD, research pharmacist at Magee-Womens Hospital, and the mothers and infants who participated in this study.
Footnotes
Dr Bogen contributed to the conception, design, acquisition of data, analysis and interpretation of data, and drafting of the article; Dr Hanusa contributed to the design, analysis and interpretation of data, and drafting of the article; Ms Baker contributed to the acquisition of data, analysis and interpretation of data, and drafting of the article; Dr Medoff-Cooper contributed to the design, interpretation of data, and drafting of the article; Dr Cohlan contributed to the analysis and interpretation of data and drafting of the article; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the National Institute on Drug Abuse (R21 DA029257) and the Magee-Womens Clinical Research Center (M01RR00056). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Patrick SW, Schumacher RE, Benneyworth BD, Krans EE, McAllister JM, Davis MM. Neonatal abstinence syndrome and associated health care expenditures: United States, 2000-2009. JAMA. 2012;307(18):1934–1940 [DOI] [PubMed] [Google Scholar]
- 2.Tolia VN, Patrick SW, Bennett MM, et al. Increasing incidence of the neonatal abstinence syndrome in U.S. neonatal ICUs. N Engl J Med. 2015;372(22):2118–2126 [DOI] [PubMed] [Google Scholar]
- 3.Arlettaz R, Kashiwagi M, Das-Kundu S, Fauchère JC, Lang A, Bucher HU. Methadone maintenance program in pregnancy in a Swiss perinatal center (II): neonatal outcome and social resources. Acta Obstet Gynecol Scand. 2005;84(2):145–150 [DOI] [PubMed] [Google Scholar]
- 4.Lifshitz M, Gavrilov V, Galil A, Landau D. A four year survey of neonatal narcotic withdrawal: evaluation and treatment. Isr Med Assoc J. 2001;3(1):17–20 [PubMed] [Google Scholar]
- 5.Maas U, Kattner E, Weingart-Jesse B, Schäfer A, Obladen M. Infrequent neonatal opiate withdrawal following maternal methadone detoxification during pregnancy. J Perinat Med. 1990;18(2):111–118 [DOI] [PubMed] [Google Scholar]
- 6.Sharpe C, Kuschel C. Outcomes of infants born to mothers receiving methadone for pain management in pregnancy. Arch Dis Child Fetal Neonatal Ed. 2004;89(1):F33–F36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gewolb IH, Fishman D, Qureshi MA, Vice FL. Coordination of suck-swallow-respiration in infants born to mothers with drug-abuse problems. Dev Med Child Neurol. 2004;46(10):700–705 [PubMed] [Google Scholar]
- 8.LaGasse LL, Messinger D, Lester BM, et al. Prenatal drug exposure and maternal and infant feeding behaviour. Arch Dis Child Fetal Neonatal Ed. 2003;88(5):F391–F399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Finnegan LP, Connaughton JF, Jr, Kron RE, Emich JP. Neonatal abstinence syndrome: assessment and management. Addict Dis. 1975;2(1–2):141–158 [PubMed] [Google Scholar]
- 10.Jansson LM, Velez M, Harrow C. Methadone maintenance and lactation: a review of the literature and current management guidelines. J Hum Lact. 2004;20(1):62–71 [DOI] [PubMed] [Google Scholar]
- 11.Weinberger SM, Kandall SR, Doberczak TM, Thornton JC, Bernstein J. Early weight-change patterns in neonatal abstinence. Am J Dis Child. 1986;140(8):829–832 [DOI] [PubMed] [Google Scholar]
- 12.Bogen DL, Whalen BL, Kair LR, Vining M, King BA. Wide variation found in care of opioid-exposed newborns. Acad Pediatr. 2017;17(4):374–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weinberger SM, Kandall SR, Doberczak TM, Loewenstein W, Thorton JC, Bernstein JL. Weight change patterns in neonatal abstinence. Pediatr Res. 1984;18:329A. [DOI] [PubMed] [Google Scholar]
- 14.Martinez A, Kastner B, Taeusch HW. Hyperphagia in neonates withdrawing from methadone. Arch Dis Child Fetal Neonatal Ed. 1999;80(3):F178–F182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dryden C, Young D, Campbell N, Mactier H. Postnatal weight loss in substitute methadone-exposed infants: implications for the management of breast feeding. Arch Dis Child Fetal Neonatal Ed. 2012;97(3):F214–F216 [DOI] [PubMed] [Google Scholar]
- 16.Gateway Health. Neonatal abstinence syndrome clinical management document. 2010. Available at: https://www.gatewayhealthplan.com/Portals/0/provider_forms/PAMA_neonatal.pdf?ver=2017-08-03-222508-177. Accessed November 8, 2017
- 17.Macdonald PD, Ross SR, Grant L, Young D. Neonatal weight loss in breast and formula fed infants. Arch Dis Child Fetal Neonatal Ed. 2003;88(6):F472–F476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miller JR, Flaherman VJ, Schaefer EW, et al. Early weight loss nomograms for formula fed newborns. Hosp Pediatr. 2015;5(5):263–268 [DOI] [PubMed] [Google Scholar]
- 19.Abdel-Latif ME, Pinner J, Clews S, Cooke F, Lui K, Oei J. Effects of breast milk on the severity and outcome of neonatal abstinence syndrome among infants of drug-dependent mothers. Pediatrics. 2006;117(6). Available at: www.pediatrics.org/cgi/content/full/117/6/e1163 [DOI] [PubMed] [Google Scholar]
- 20.Dryden C, Young D, Hepburn M, Mactier H. Maternal methadone use in pregnancy: factors associated with the development of neonatal abstinence syndrome and implications for healthcare resources. BJOG. 2009;116(5):665–671 [DOI] [PubMed] [Google Scholar]
- 21.McQueen KA, Murphy-Oikonen J, Gerlach K, Montelpare W. The impact of infant feeding method on neonatal abstinence scores of methadone-exposed infants. Adv Neonatal Care. 2011;11(4):282–290 [DOI] [PubMed] [Google Scholar]
- 22.Pritham UA, Paul JA, Hayes MJ. Opioid dependency in pregnancy and length of stay for neonatal abstinence syndrome. J Obstet Gynecol Neonatal Nurs. 2012;41(2):180–190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Welle-Strand GK, Skurtveit S, Jansson LM, Bakstad B, Bjarkø L, Ravndal E. Breastfeeding reduces the need for withdrawal treatment in opioid-exposed infants. Acta Paediatr. 2013;102(11):1060–1066 [DOI] [PubMed] [Google Scholar]
- 24.Wachman EM, Byun J, Philipp BL. Breastfeeding rates among mothers of infants with neonatal abstinence syndrome. Breastfeed Med. 2010;5(4):159–164 [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention. Breastfeeding among US children born 2002–2014, CDC national immunization survey. 2014. Available at: www.cdc.gov/breastfeeding/data/nis_data/index.htm. Accessed October 20, 2014