Abstract
Background
The diagnosis and treatment of breast cancer can provoke a series of negative emotional changes in patients, further affecting their quality of life. It has been shown that patients with higher resilience have better quality of life. Social support systems are important protective factors that are necessary for the process of resilience to occur. Hence, this study aimed to investigate the role of social support in the relationship between resilience and quality of life among Chinese patients with breast cancer.
Material/Methods
A demographic-disease survey, the Chinese version of the Connor-Davidson Resilience Scale 25, Medical Outcomes Study Social Support Survey, and Functional Assessment of Cancer Therapy Breast Cancer Version 3 were used to interview 98 patients with breast cancer from a teaching hospital in Chongqing, China. Data analysis was performed by descriptive statistics, independent-sample t test, one-way ANOVA, and regression analyses.
Results
The mean scores of resilience, social support, and quality of life were 54.68, 61.73, and 80.74 respectively, which were in the moderate range. Participants with stronger social support had higher resilience and better quality of life. Social support played a partial mediator role in the relationship between resilience and quality of life. The mediation effect ratio was 28.0%.
Conclusions
Social support is essential for the development of resilience and the improvement of quality of life in Chinese patients with breast cancer. Health professionals should provide appropriate guidelines to help patients seek effective support and enhance their resilience to improve their quality of life after breast cancer.
MeSH Keywords: Breast Neoplasms; Quality of Life; Resilience, Psychological; Social Support
Background
Breast cancer has become the leading malignancy in developed countries worldwide [1]. In China, 169 000 women are diagnosed with breast cancer every year, and about 45 000 die of breast cancer [2]. Studies have indicated that the diagnosis and treatment of breast cancer provoke a series of negative emotional changes, such as considerable stress, anxiety, fear, and depression [3,4]. These emotional responses can significantly impair quality of life (QOL) outcomes [4,5].
Resilience is an ability of individuals to cope successfully with significant change, adversity, and risk [6]. A large body of evidence suggests that resilience has been employed to maintain the mental health of vulnerable populations experiencing stressful events [7–9]. In this way, resilience has been considered to be a defense mechanism to deal with cancer diagnosis and treatment-related difficulties, for example, emotional and social stressors [10]. Several researchers report that cancer patients with similar diseases and treatment status have significantly different levels of QOL, which may be due to varying levels of patient resilience [11,12]. Resilience affects many aspects of QOL, and more resilient patients with breast cancer have significantly better QOL [12,13]. However, little is known about how resilience affects QOL, especially for Chinese patients with breast cancer.
Social support refers to the various types of free assistance from a social network, which may be formal and/or informal, including emotional and physical support [14]. The literature indicates that social support systems are very important protective factors for individuals experiencing stressful events [15] and that protective factors are necessary for the process of resilience to occur [16]. Social support might be closely related to resilience [17–19].
Specifically for patients with breast cancer, social support plays a critical role in reducing cancer-related stress [20]. It has been reported that social support can alleviate the negative impact of stressful events on an individual’s well-being [21]. Stronger social support has been associated with psychological well-being in patients with breast cancer [22]. Emerging studies have also shown that enhancing social support for survivors of breast cancer can improve the outcome of QOL through moderating the effects of depressive symptoms [23,24]. Additionally, social support has also been examined as a potential mediator related to an individual’s mental health outcome [25].
According to the literature, social support has been demonstrated as an important factor for resilience and QOL outcomes of patients with breast cancer [26]. However, an explanation of the role of social support in the relationship between resilience and QOL in Chinese patients with breast cancer is lacking. Based on this association, we hypothesized that social support acts as a mediator in the relationship between resilience and QOL. A framework diagram is shown in Figure 1.
Figure 1.
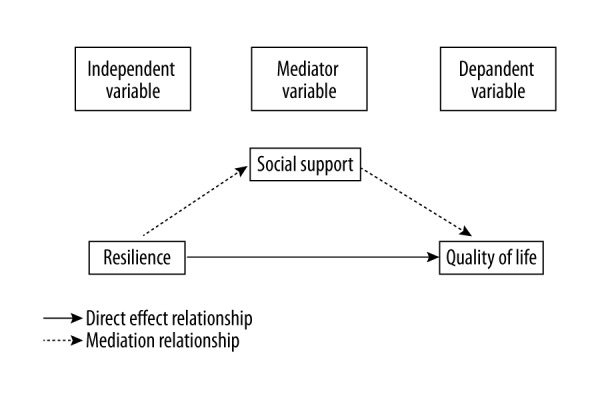
Hypothetical relationship diagram.
Therefore, this study aimed to explore the mediator role of social support in the relationship between resilience and QOL in Chinese patients with breast cancer.
Conceptual framework to guide the mediation model
Social support has been studied extensively from various theoretical perspectives [27–29]. The main effects model and the stress buffering model were considered as 2 important theoretical frameworks of social support related to physical and psychological health outcomes, which derives from stress and coping theory [29]. The main effects model indicates that social support has a direct effect on QOL, regardless of the level of stress [30]. The stress buffering model indicates that social support serves as a buffer or protector (moderator or mediator variables) associated with improved physical and mental health only when individuals are exposed to stressful conditions [31,32]. The study used the stress-buffering model to guide the mediating effect of social support in the relationship between resilience and QOL.
A mediator or moderator variable is defined as a third variable that changes the association between an independent variable and a dependent variable [33]. Mediators provide additional insight into information about the causal links between 2 strongly associated variables [34]. However, moderators alter the dose-dependent relationship between 2 weakly associated variables [34]. Based on the focus of the analysis in the current study, the mediation effect model of social support was explored in Chinese patients with breast cancer.
Material and Methods
Sample
A cross-sectional study was performed at the First Affiliated Hospital of Chongqing Medical University in China from July 2016 to January 2017. Study subjects were recruited using convenience sampling. The eligibility criteria were as follows: 1) age 18 years or older, 2) Chinese-speaking, 3) a confirmed diagnosis of breast cancer, (4) able to understand the aim of the study, and 5) able to take part in this study, including completing the questionnaire and giving advice. The subjects with serve concomitant diseases or uncomfortable medical conditions were excluded from the study. There were 120 potential participants with breast cancer who received medical care and met the eligibility criteria. Among them, 22 participants found the study uninteresting or refused to sign informed consent. Therefore, 98 participants were included (response rate=81.67%).
Procedures
The First Affiliated Hospital of Chongqing Medical University Ethics Committee approved the study and granted formal access to patients. Potentially eligible participants were identified by their physicians or nurses during a hospital visit. Participants were informed about the study before starting any procedures. Informed consent was signed by participants who agreed to participate. In order to discuss unclear questions with the participants, we used a face-to-face survey. Participants were encouraged to complete the questionnaires in a private room, and the interviews were 20 to 30 minutes in duration. Participant demographic and clinical characteristics were obtained through medical chart reviews.
Measurements
Participants’ demographic and clinical characteristics were recorded, such as participant age, marital status, number of children, education level, employment status, monthly income (in RMB), living place, insurance, time since diagnosis, stage of breast cancer, surgery type, and treatment type.
Resilience
The Chinese version of the Connor-Davidson Resilience Scale 25 (CD-RISC25) is a 25-item self-evaluation instrument used to measure participant resilience [35]. Each item was scored on a 4-point scale. The 3 subscales were tenacity, strength, and optimism. The total score ranges from 0–100 points, in which higher scores indicate higher resilience. For our study, Cronbach’s alpha was 0.95.
Social support
Social support was measured using the Chinese version of the Medical Outcomes Study which consists of emotional–informational support, tangible support, affectionate support, and positive social interactive support [36]. It is a multidimensional measure instrument with 19 items scored on a 5-point Likert scale. A higher score indicates better perceived social support. The total score ranges from 0 to 100. For our study, Cronbach’s alpha was 0.95.
Quality of life
The 36-item simplified Chinese version of the Functional Assessment of Cancer Therapy Breast Cancer (FACT-B) Version 3 was used to measure QOL in patients with breast cancer [37]. Five domains were measured: physical well-being (PWB), functional well-being (FWB), emotional well-being (EWB), social/family well-being (SWB), and breast cancer-specific concerns (BCS). The total score of the scale ranges from 0 to 144, where a higher score indicates better health. For our study, Cronbach’s alpha was 0.91.
Ethical consideration
This study was approved by the Ethics Committee of First Affiliated Hospital of Chongqing Medical University (Approval number: 2016-125). Prior to the participant interviews, each participating venue was informed and consent obtained. Informed consent was signed by all participants before the study. All the information provided by the participant was kept confidential and participants could withdraw from the research at any time. A bouquet of carnation (cost 30–40 RMB) was provided to every participant as a gift after completing this survey.
Data analysis
The Statistical Package for the Social Sciences (SPSS) 21.0 was used for data analysis. Descriptive statistics were calculated for major variables, including means and standard deviations. The t test and ANOVA were used to analyze differences in predictor and outcome variables. Pearson correlation analysis was performed to assess correlations among resilience, social support, and QOL.
A variable was defined as a mediator when it met the following conditions: (a) independent variables are strongly associated with dependent variables; (b) independent variables are related to mediator; (c) independent variables and mediator are related to dependent variables [34]. Within the correlation framework, a 3-step composite analysis was performed to test the mediating effects, which has been used in many studies [17,33,38,39]. In this study, first, social support was regressed on resilience. Second, QOL was regressed on resilience. Finally, QOL was regressed on resilience and social support. Separate coefficients for each regression equation were tested. There are 3 explanations for the results of regression coefficient examination. First, when the coefficient of the first step is not significant, mediating effects analysis is ended. Second, when the coefficients of the first and second step are significant and the coefficient for the independent variable (resilience) in the third step is not significant, this represents a significant full mediating effect. Third, when the coefficient of the first step and the second step are significant, and the coefficient for the independent variable (resilience) in the third step is less than the result of the second step, this represents a significant mediating effect, but the mediating effect is partial.
Results
Participants
The participants were 98 Chinese women. The average age of the participants was 47.02 years (SD=9.59, range=21–79). Most participants were married, and most had children. A total of 78 participants (79.6%) had less than 1 year since time of diagnosis. Regarding disease severity (stage of breast cancer), most participants were at stage II (n=40, 40.8%). Ninety-four participants (95.9%) had modified radical mastectomy, and 71 (72.4%) continuously received surgery and adjuvant chemotherapy. Other demographic information is presented in Table 1.
Table 1.
Participants’ demographic and disease characteristics (N=98).
| Characteristic | N (%) | Mean (SD) |
|---|---|---|
| Age (years) | 47.02 (9.59) | |
| Marital status | ||
| Married | 88 (89.8) | |
| Divorced | 7 (7.1) | |
| Single | 3 (3.1) | |
| Children | ||
| Yes | 89 (90.8) | |
| No | 9 (9.2) | |
| Education level | ||
| Below primary school | 12 (12.2) | |
| Junior high school | 47 (48) | |
| High school or some college | 34 (34.7) | |
| University or above | 5 (5.1) | |
| Employment status | ||
| Full-time/part-time | 21 (21.4) | |
| Retired | 16 (16.3) | |
| Unemployed | 43 (43.9) | |
| On leave due to illness | 18 (18.4) | |
| Monthly income(in RMB) | ||
| <1,000 | 13 (13.3) | |
| 1,000–3,000 | 32 (32.7) | |
| >3,000 | 53 (54.1) | |
| Living place | ||
| Provincial capital | 28 (28.6) | |
| Prefecture-level city | 25 (25.5) | |
| County | 28 (28.6) | |
| Village | 17 (17.3) | |
| Insurance | ||
| New rural co-operative medical system | 23 (23.5) | |
| Medical insurance | 68 (69.4) | |
| No | 7 (7.1) | |
| Time since diagnosis | ||
| <1year | 78 (79.6) | |
| Between 1 and 2 years | 16 (16.3) | |
| Between 2 and 5 years | 4 (4.1) | |
| Stage of breast cancer | ||
| 0 | 6 (6.1) | |
| I | 19 (19.4) | |
| II | 40 (40.8) | |
| III | 25 (25.5) | |
| IV | 8 (8.2) | |
| Surgery | ||
| Lumpectomy/breast conserving surgery | 4 (4.1) | |
| Modified radical mastectomy | 94 (95.9) | |
| Treatment type | ||
| Surgery only | 20 (20.4) | |
| Surgery + adjuvant chemotherapy | 71 (71.4) | |
| Chemotherapy | 2 (2) | |
| Others | 5 (5.1) | |
Descriptive analysis of resilience, social support, and QOL
The basic descriptive statistics of resilience, social support, and QOL are shown in Tables 2 and 3. The mean score for resilience was 54.68 (SD=16.83, range=23–93). The mean score for social support was 61.73 (SD=14.32, range=31–95), and the domain of affectionate support scored showed lower scores. Social support levels differed significantly by participant marital status (F=2.214, p=0.018), monthly income (F=4.389, p=0.015), living place (F=4.814, p=0.004), time since diagnosis (F=4.201, p=0.018), stage of breast cancer (F=6.445, p<0.001), and surgery type (t =3.770, p<0.001). The total mean score of QOL was 80.74 (SD=19.49, range=35–129), and the domains of emotional well-being and functional well-being had lower scores than the others. QOL levels differed significantly by participant monthly income (F=3.784, p=0.026), time since diagnosis (F=5.982, p=0.004), stage of breast cancer (F=9.549, p<0.001), and surgery type (t=4.095, p<0.001).
Table 2.
Descriptive data for resilience, social support, and quality of life and scores (N=98).
| Scale | Number of items | Possible range of scores | Actual range of scores | Mean (SD) | Cranach’s a |
|---|---|---|---|---|---|
| CD-RISC25 | 25 | 0–100 | 23–93 | 54.68 (16.83) | 0.95 |
| Tenancy | 13 | 0–52 | 10–49 | 27.70 (9.39) | 0.94 |
| Strength | 8 | 0–32 | 6–32 | 18.57 (5.72) | 0.88 |
| Optimism | 4 | 0–16 | 3–16 | 8.40 (2.93) | 0.63 |
| MOS-SSS-C | 19 | 0–100 | 31–95 | 61.73 (14.32) | 0.95 |
| Emotional-information support | 8 | 8–40 | 11–40 | 23.55 (7.40) | 0.92 |
| Tangible support | 4 | 4–20 | 4–20 | 14.24 (3.09) | 0.83 |
| Affectionate support | 3 | 3–15 | 4–15 | 10.49 (2.32) | 0.86 |
| Positive social interaction | 4 | 4–20 | 6–20 | 13.45 (3.17) | 0.85 |
| FACT-B | 36 | 0–144 | 35–129 | 80.74 (19.49) | 0.91 |
| Physical well-being | 7 | 0–28 | 4–28 | 17.32 (4.82) | 0.78 |
| Social/family well-being | 7 | 0–28 | 3–28 | 16.24 (5.74) | 0.86 |
| Emotional well-being | 6 | 0–24 | 1–23 | 12.87 (5.60) | 0.89 |
| Functional Well-being | 7 | 0–28 | 2–28 | 13.71 (5.47) | 0.84 |
| Additional concerns | 9 | 0–36 | 10–32 | 20.60 (4.74) | 0.62 |
CD-RISC25 – Connor-Davidson Resilience Scale 25; MOS-SSS-C – Medical Outcomes Study Social Support Survey; FACT-B – Functional Assessment of Cancer Therapy Breast Cancer.
Table 3.
The differences among sample characteristics, social support and quality of life.
| Variable | Social support | QOL | ||||
|---|---|---|---|---|---|---|
| Mean (SD) | t or F | P-value | Mean (SD) | t or F | P-value | |
| Marital status | F=4.214 | 0.018 | F=2.542 | 0.084 | ||
| Married | 63.42 (14.31) | 82.22 (19.44) | ||||
| Divorced | 50.00 (10.36) | 67.29 (17.87) | ||||
| Single | 49.67 (4.04) | 69.00 (9.84) | ||||
| Children | t=−0.354 | 0.724 | t=−1.416 | 0.678 | ||
| Yes | 61.87 (14.57) | 80.48 (19.77) | ||||
| No | 63.67 (13.34) | 83.33 (17.27) | ||||
| Education level | F=2.292 | 0.083 | F=0.496 | 0.686 | ||
| Below primary school | 59.08 (19.59) | 80.58 (26.95) | ||||
| Junior high school | 59.34 (13.96) | 78.53 (19.20) | ||||
| High school or some college | 65.24 (12.08) | 83.00 (18.01) | ||||
| University or above | 72.80 (13.88) | 86.60 (12.59) | ||||
| Employment status | F=1.792 | 0.154 | F=1.026 | 0.385 | ||
| Full-time/part-time | 64.95 (11.10) | 80.86 (17.17) | ||||
| Retired | 67.00 (15.83) | 88.25 (24.74) | ||||
| Unemployed | 58.58 (12.93) | 78.35 (20.59) | ||||
| On leave due to illness | 62.50 (14.41) | 79.67 (12.84) | ||||
| Monthly income(in RMB) | F=4.389 | 0.015 | F=3.784 | 0.026 | ||
| <1,000 | 60.69 (19.16) | 80.15 (24.80) | ||||
| 1,000–3,000 | 56.53 (12.98) | 73.56 (17.75) | ||||
| >3,000 | 65.70 (13.02) | 85.23 (18.08) | ||||
| Living place | F=4.814 | 0.004 | F=1.405 | 0.246 | ||
| Provincial capital | 69.86 (13.00) | 86.25 (23.79) | ||||
| Prefecture-level city | 61.32 (11.76) | 80.76 (14.68) | ||||
| County | 58.50 (14.45) | 78.96 (16.86) | ||||
| Village | 56.06 (15.69) | 74.59 (21.15) | ||||
| Insurance | F=2.728 | 0.070 | F=1.565 | 0.214 | ||
| New rural co-operative medical system | 56.04 (16.13) | 76.17 (20.30) | ||||
| Medical insurance | 64.01 (13.53) | 81.28 (19.49) | ||||
| No | 62.57 (13.30) | 90.57 (13.91) | ||||
| Time since diagnosis | F=4.201 | 0.018 | F=5.982 | 0.004 | ||
| <1 year | 60.37 (14.20) | 77.69 (18.95) | ||||
| Between 1 and 2 years | 65.88 (12.80) | 90.00 (15.74) | ||||
| Between 2 and 5 years | 79.25 (13.07) | 103.20 (21.31) | ||||
| Stage of breast cancer | F=6.445 | <0.001 | F=9.549 | <0.001 | ||
| 0 | 76.00 (9.63) | 103.00 (17.30) | ||||
| I | 70.89 (15.63) | 93.21 (21.04) | ||||
| II | 61.33 (12.36) | 81.12 (16.36) | ||||
| III | 56.60 (11.40) | 70.76 (11.85) | ||||
| IV | 51.13 (16.17) | 63.75 (20.21) | ||||
| Surgery type | t=3.770 | <0.001 | t=4.095 | <0.001 | ||
| Lumpectomy/breast conserving surgery | 87.00 (2.44) | 117.00 (7.26) | ||||
| Modified radical mastectomy | 69.98 (13.73) | 79.20 (18.32) | ||||
| Treatment type | F=1.522 | 0.214 | F=1.711 | 0.170 | ||
| Surgery only | 57.00 (14.89) | 74.80 (16.75) | ||||
| Surgery + adjuvant chemotherapy | 62.79 (13.77) | 81.68 (19.24) | ||||
| Chemotherapy | 73.50 (30.40) | 72.00 (36.77) | ||||
| Others | 67.00 (14.14) | 94.80 (24.25) | ||||
QOL – quality of life.
Correlation analysis among resilience, social support, and quality of life
The correlations among resilience, social support, and quality of life are shown in Table 4. Resilience and social support were found to be highly related to QOL. Resilience was positively correlated with total social support (r=0.660, p<0.01), the 4 subscales of social support, and quality of life (r=0.745, p<0.01). Total social support and its domains were also significantly correlated with QOL. Positive social interaction support and QOL had the highest correlation coefficient (r=0.909, p<0.01). The 4 subscales of social support correlated significantly with each other. Affectionate support and positive social interaction support had the highest correlation coefficient (r=0.859, p<0.01).
Table 4.
Correlation matrix for resilience, social support, and quality of life.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1 | TR | 1 | ||||||
| 2 | SS | .660** | 1 | |||||
| 3 | ES | .589** | .899** | 1 | ||||
| 4 | TS | .532** | .844** | .606** | 1 | |||
| 5 | AS | .516** | .865** | .668** | .825** | 1 | ||
| 6 | PS | .613** | .909** | .745** | .790** | .859** | 1 | |
| 7 | QOL | .745** | .737** | .668** | .626** | .540** | .660** | 1 |
TR – total resilience; SS – social support; ES – emotional-information support; TS – tangible support; AS – affectionate support; PS – positive social interaction; QOL – quality of life.
p<0.01.
The effect of social support on the relation between resilience and quality of life
Results indicated that social support can play a partial mediator role between resilience and QOL, as shown as Figure 2. In the first step, social support was regressed on resilience (β=0.491, p<0.001) after controlling for participant marital status, monthly income, living place, time since diagnosis, stage of breast cancer, and surgery type. The second step involved regressing QOL on the independent variable (resilience). Because participant monthly income, time since diagnosis, stage of breast cancer, and surgery type could affect QOL, they were controlled for in the regression by entering them into the first block of the equation. Resilience was entered into the second block. QOL significantly was regressed on resilience (β=0.569, p<0.001). In the final step, QOL was regressed on resilience and the mediator (social support). Participant monthly income, time since diagnosis, stage of breast cancer, and surgery type were entered into the first block of the equation, and resilience and social support were entered into the second block. QOL significantly was regressed on resilience (β=0.404, p<0.001) and social support (β=0.325, p<0.001), respectively. Through 3-step regression, social support had a significant mediating effect, and the mediation effect ratios were 0.491*0.325/0.569≈28.0%.
Figure 2.
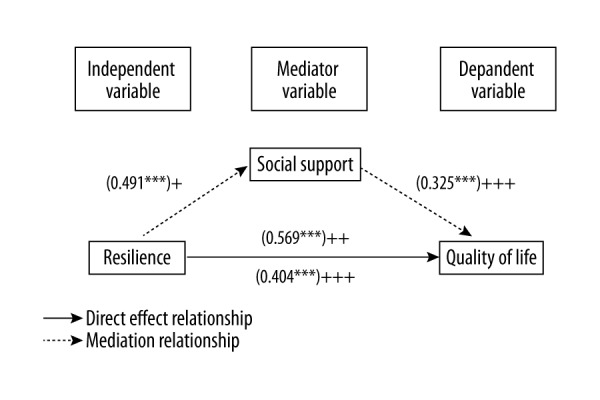
The mediator model of social support. *** p<0.001. “+” The first step represents social support regressed on resilience. “++” The second step represents quality of life regressed on resilience. “+++” The third step represents quality of life regressed on resilience and social support.
Discussion
This study explored the role of social support in the relationship between resilience and QOL among Chinese patients with breast cancer. Results indicated that social support was positively correlated with resilience and QOL. Social support plays a partial mediator role in the relationship. The results partially support our hypothesis.
In order to reduce the risk of cancer recurrence and death, most patients with breast cancer who receive medical treatment after surgery require repeated hospitalization [40]. In one study, 54.6% of hospitalized patients with cancer experienced significant emotional distress, including anxiety and depression [41]. Resilience has a positive effect on health outcomes of patients with cancer [41]. The current study found that resilience not only directly affected the QOL of patients with breast cancer, but also indirectly affected their QOL through social support.
The direct relationship between resilience and QOL was similar to the finding of Ristevska-Dimitrovska and colleagues who reported a positive relationship between resilience and QOL in women with breast cancer [12]. Some studies also reported that resilience improvement appeared to be significant for mental health recovery [8,42,43]. This may suggest that trait-resilient individuals are better able to resist negative responses generated by the diagnosis and treatment of breast cancer.
Additionally, the mediation effect of social support in the relation of resilience and QOL is similar that reported in a recent study [17]. Moreover, previous findings in other types of studies also indicated that social support acted as a mediator in the association between stress and health outcomes in the context of cancer [18,39,44]. However, few studies linked social support as a mediator of resilience and QOL in the context of cancer. Because of this, some explanations given may involve indirect evidence. On the one hand, active coping mechanisms are readily used by trait-resilient individuals when dealing with stressful life situations [43,45]. Evidence indicates the use of an active coping style partly mediated the relationship between social support and mental health [46]. Importantly, social support preceded and facilitated the use of active coping mechanisms [47]. Hence, we speculate that patients with breast cancer who have higher resiliency may use an active coping style under the influence of social support to improve their current quality of life. On the other hand, there is an explanation from the perspective of neurobiology. When patients with breast cancer perceived stressful effects of breast cancer and treatment-induced adverse effects, the hypothalamic-pituitary-adrenocortical(HPA) system involving the stress response is strongly activated [48]. Building on the results of animal and human studies, the regulation of social support heavily depends on 2 neuropeptides – oxytocin and vasopressin – which promote social behavior and may inhibit the HPA axis reactivity to stress [49–51]. Resilience to stress is associated with the regulation of noradrenergic activity produced by the HPA system within an optimal window [48]. Within this framework, resilient individuals may need the participation of social support through brain mechanisms for maintaining psychological well-being.
Although resilience can affect QOL through the mediation of social support, the mediation was partial and the mediation effect ratios were only 28.0% in our study, suggesting that other potential mediating variables contribute to the relationship between resilience and QOL. A recent study investigated medical students and found that resilience can predict psychological well-being, and that optimism plays a minor mediation role in the relationship between resilience and psychological well-being [52]. Self-efficacy was also predicted as a mediator for the effect of resilience on pain in osteoarthritic patients [53]. There may be other factors in the relationship between resilience and health outcomes, such as self-esteem, hope, and spirituality [43].
There are some limitations in the present study. First, the cross-sectional design cannot offer a precise explanation of the causal mechanisms between the 2 variables. Longitudinal studies or randomized controlled trials (RCT) will be necessary to further confirm our results. Second, the heterogeneity in our sample characteristics may have caused bias in our results. In future studies, sample size should be expanded. Third, this study is largely based on quantitative methods. Qualitative methods should be considered to explore the meaning of the relationship among resilience, social support, and QOL. Apart from this, only social support as a mediator variable was included to explore the relationship between resilience and QOL. Other factors may also have effects on the relationship in patients with breast cancer, such as optimism, self-efficacy, and self-esteem.
Conclusions
In conclusion, despite the limitations noted above, this study is the first to explore the role of social support in the relationship between resilience and QOL among Chinese patients with breast cancer. Social support should be valued as an important component of sensitive healthcare for the improvement of resilience and QOL of survivors of breast cancer. Sources of social support should be evaluated before and during treatment. Specifically, the family is one of the important social support systems for women with cancer. Therefore, husbands and other family members should be mobilized to participate in related courses or strategies. Health professionals are also an important source of social support for Chinese women with breast cancer, and should have a better understanding of these women’s experiences. Finally, appropriate guidelines should be provided to help women with breast cancer seek effective support and enhance their resilience to improve their QOL after breast cancer.
Acknowledgments
The authors would like to thank all the participants and the Department of the Breast Surgery of the First Affiliated Hospital of Chongqing Medical University.
Abbreviations
- QOL
quality of life
- CD-RISC25
Connor-Davidson Resilience Scale 25
- MOS-SSS-C
Medical Outcomes Study Social Support Survey
- FACT-B
Functional Assessment of Cancer Therapy Breast Cancer
- HPA
hypothalamic-pituitary-adrenocortical
Footnotes
Conflict of interest
None.
Source of support: Departmental sources
References
- 1.Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. Cancer J Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 2.Zheng Y, Wu C, Zhang M. The epidemic and characteristics of female breast cancer in China. China Oncol. 2013;23:561–69. [Google Scholar]
- 3.Pedersen AE, Sawatzky JA, Hack TF. The sequelae of anxiety in breast cancer: A human response to illness model. Oncol Nurs Forum. 2010;37:469–75. doi: 10.1188/10.ONF.469-475. [DOI] [PubMed] [Google Scholar]
- 4.Knobf MT. Clinical update: Psychosocial responses in breast cancer survivors. Semin Oncol Nurs. 2011;27:e1–e14. doi: 10.1016/j.soncn.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 5.Sharma N, Purkayastha A. Factors affecting quality of life in breast cancer patients: A descriptive and cross-sectional study with review of literature. J Midlife Health. 2017;8(2):75–83. doi: 10.4103/jmh.JMH_15_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee HH, Cranford JA. Does resilience moderate the associations between 4 parental problem drinking and adolescents’internalizing and externalizing 5 behaviours? A study of Korean Adolescents. Drug Alcohol Depend. 2008;96:213–21. doi: 10.1016/j.drugalcdep.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Olsson CA, Bond L, Burns JM, et al. Adolescent resilience: A concept analysis. J Adolesc. 2003;26:1–11. doi: 10.1016/s0140-1971(02)00118-5. [DOI] [PubMed] [Google Scholar]
- 8.Davydov DM, Stewart R, Ritchie K, Chaudieu I. Resilience and mental health. Clin Psychol Rev. 2010;30:479–95. doi: 10.1016/j.cpr.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 9.Reza GG, Kourosh S, Abbas E, et al. Resilience of patients with chronic physical diseases: A systematic review and meta-analysis. Iran Red Crescent Med J. 2016;18:e38562. doi: 10.5812/ircmj.38562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tugade MM, Fredrickson BL, Barrett LF. Psychological resilience and positive emotional granularity: Examining the benefits of positive emotions on coping and health. J Pers. 2004;72:1161–90. doi: 10.1111/j.1467-6494.2004.00294.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Epping-Jordan JE, Compas BE, Osowiecki DM, et al. Psychological adjustment in breast cancer: Processes of emotional distress. Health Psychol. 1999;18:315–26. doi: 10.1037//0278-6133.18.4.315. [DOI] [PubMed] [Google Scholar]
- 12.Ristevska-Dimitrovska G, Filov I, Rajchanovska D, et al. Resilience and quality of life in breast cancer patients. Open Access Maced J Med Sci. 2015;3(4):727–31. doi: 10.3889/oamjms.2015.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu Z, Liu Y, Li X, Li X. Resilience and associated factors among Mainland Chinese women newly diagnosed with breast cancer. PLoS One. 2016;11:e0167976. doi: 10.1371/journal.pone.0167976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dumont M, Provost MA. Resilience in adolescents: Protective role of social support, coping strategies, self-esteem, and social activities on experience of stress and depression. Journal of Youth and Adolescence. 1999;28:343–63. [Google Scholar]
- 15.Migerode F, Buysse A, Brondeel R. Quality of life in adolescents with a disability and their parents: The mediating role of social support and resilience. Journal of Developmental and Physical Disabilities. 2012;24:487–503. [Google Scholar]
- 16.Earvolino-Ramirez M. Resilience: A concept analysis. Nurs Forum. 2007;42:73–82. doi: 10.1111/j.1744-6198.2007.00070.x. [DOI] [PubMed] [Google Scholar]
- 17.Xu J, Ou L. Resilience and quality of life among Wenchuan earthquake survivors: The mediating role of social support. Public Health. 2014;128:430–37. doi: 10.1016/j.puhe.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 18.Costa AL, Heitkemper MM, Alencar GP, et al. Social support is a predictor of lower stress and higher quality of life and resilience in Brazilian patients with colorectal cancer. Cancer Nurs. 2017;40(5):352–60. doi: 10.1097/NCC.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 19.Somasundaram RO, Devamani KA. A comparative study on resilience, perceived social support and hopelessness among cancer patients treated with curative and palliative care. Indian J Palliat Care. 2016;22(2):135–40. doi: 10.4103/0973-1075.179606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim J, Han JY, Shaw B, et al. The roles of social support and coping strategies in predicting breast cancer patients’ emotional well-being: Testing mediation and moderation models. J Health Psychol. 2010;15:543–52. doi: 10.1177/1359105309355338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kroenke CH, Quesenberry C, Kwan ML, et al. Social networks, social support, and burden in relationships, and mortality after breast cancer diagnosis in the Life After Breast Cancer Epidemiology (LACE) study. Breast Cancer Res Treat. 2013;137:261–71. doi: 10.1007/s10549-012-2253-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shelby RA, Crespin TR, Wells-Di Gregorio SM, et al. Optimism, social support, and adjustment in African American women with breast cancer. J Behav Med. 2008;31:433–44. doi: 10.1007/s10865-008-9167-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang CY, Hsu MC. Social support as a moderator between depressive symptoms and quality of life outcomes of breast cancer survivors. Eur J Oncol Nurs. 2013;17:767–74. doi: 10.1016/j.ejon.2013.03.011. [DOI] [PubMed] [Google Scholar]
- 24.Ng CG, Mohamed S, See MH, et al. Anxiety, depression, perceived social support and quality of life in Malaysian breast cancer patients: A 1-year prospective study. Health Qual Life Outcomes. 2015;13:205. doi: 10.1186/s12955-015-0401-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hill TD, Kaplan LM, French MT, Johnson RJ. Victimization in early life and mental health in adulthood: an examination of the mediating and moderating influences of psychosocial resources. J Health Soc Behav. 2010;51:48–63. doi: 10.1177/0022146509361194. [DOI] [PubMed] [Google Scholar]
- 26.Kwan ML, Ergas IJ, Somkin CP, et al. Quality of life among women recently diagnosed with invasive breast cancer: The Pathways Study. Breast Cancer Res Treat. 2010;123:507–24. doi: 10.1007/s10549-010-0764-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hupcey JE. Clarifying the social support theory-research linkage. J Adv Nurs. 1998;27:1231–41. doi: 10.1046/j.1365-2648.1998.01231.x. [DOI] [PubMed] [Google Scholar]
- 28.Connell CM, D’Augelli AR. Social support and human development: Issues in theory, research, and practice. J Community Health. 1988;13:104–14. doi: 10.1007/BF01364205. [DOI] [PubMed] [Google Scholar]
- 29.Schradle SB, Dougher MJ. Social support as a mediator of stress: Theoretical and empirical isssues. Clinical Psychology Review. 1985;5:641–61. [Google Scholar]
- 30.Helgeson VS. Social support and quality of life. Qual Life Res. 2003;12(Suppl 1):25–31. doi: 10.1023/a:1023509117524. [DOI] [PubMed] [Google Scholar]
- 31.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98:310–57. [PubMed] [Google Scholar]
- 32.Wilcox BL. Social support, life stress, and psychological adjustment: A test of the buffering hypothesis. Am J Community Psychol. 1981;9:371–86. doi: 10.1007/BF00918169. [DOI] [PubMed] [Google Scholar]
- 33.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 34.Bennett JA. Mediator and moderator variables in nursing research: Conceptual and statistical differences. Res Nurs Health. 2000;23:415–20. doi: 10.1002/1098-240x(200010)23:5<415::aid-nur8>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 35.Fu C, Leoutsakos JM, Underwood C. An examination of resilience cross-culturally in child and adolescent survivors of the 2008 China earthquake using the Connor-Davidson Resilience Scale (CD-RISC) J Affect Disord. 2014;155:149–53. doi: 10.1016/j.jad.2013.10.041. [DOI] [PubMed] [Google Scholar]
- 36.Li CC, Chen ML, Chang TC, et al. Social support buffers the effect of self-esteem on quality of life of early-stage cervical cancer survivors in Taiwan. Eur J Oncol Nurs. 2015;19:486–94. doi: 10.1016/j.ejon.2015.02.008. [DOI] [PubMed] [Google Scholar]
- 37.Wan C, Zhang D, Yang Z, et al. Validation of the simplified Chinese version of the FACT-B for measuring quality of life for patients with breast cancer. Breast Cancer Res Treat. 2007;106:413–18. doi: 10.1007/s10549-007-9511-1. [DOI] [PubMed] [Google Scholar]
- 38.Rao D, Chen WT, Pearson CR, et al. Social support mediates the relationship between HIV stigma and depression/quality of life among people living with HIV in Beijing, China. Int J STD AIDS. 2012;23(7):481–84. doi: 10.1258/ijsa.2009.009428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Manning-Walsh J. Social support as a mediator between symptom distress and quality of life in women with breast cancer. J Obstet Gynecol Neonatal Nurs. 2005;34(4):482–93. doi: 10.1177/0884217505278310. [DOI] [PubMed] [Google Scholar]
- 40.Lopez-Tarruella S, Martin M. Recent advances in systemic therapy: Advances in adjuvant systemic chemotherapy of early breast cancer. Breast Cancer Res. 2009;11(2):204. doi: 10.1186/bcr2226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Min JA, Yoon S, Lee CU, et al. Psychological resilience contributes to low emotional distress in cancer patients. Support Care Cancer. 2013;21:2469–76. doi: 10.1007/s00520-013-1807-6. [DOI] [PubMed] [Google Scholar]
- 42.Pieters HC. “I’m Still Here”: Resilience among older survivors of breast cancer”. Cancer Nurs. 2016;39:E20–28. doi: 10.1097/NCC.0000000000000248. [DOI] [PubMed] [Google Scholar]
- 43.Stewart DE, Yuen T. A systematic review of resilience in the physically ill. Psychosomatics. 2011;52:199–209. doi: 10.1016/j.psym.2011.01.036. [DOI] [PubMed] [Google Scholar]
- 44.Schury K, Zimmermann J, Umlauft M, et al. Childhood maltreatment, postnatal distress and the protective role of social support. Child Abuse Negl. 2017;67:228–39. doi: 10.1016/j.chiabu.2017.02.021. [DOI] [PubMed] [Google Scholar]
- 45.Wood SK, Bhatnagar S. Resilience to the effects of social stress: Evidence from clinical and preclinical studies on the role of coping strategies. Neurobiol Stress. 2015;1:164–73. doi: 10.1016/j.ynstr.2014.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lin J, Guo Q, Ye X, et al. The effect of social support and coping style on depression in patients with continuous ambulatory peritoneal dialysis in southern China. Int Urol Nephrol. 2013;45:527–35. doi: 10.1007/s11255-012-0309-7. [DOI] [PubMed] [Google Scholar]
- 47.Shively CA, Clarkson TB, Kaplan JR. Social deprivation and coronary artery atherosclerosis in female cynomolgus monkeys. Atherosclerosis. 1989;77:69–76. doi: 10.1016/0021-9150(89)90011-7. [DOI] [PubMed] [Google Scholar]
- 48.Charney DS. Psychobiological mechanism of resilience and vulnerability: Implications for successful adaptation to extreme stress. Am J Psychiatry. 2004;161:195–216. doi: 10.1176/appi.ajp.161.2.195. [DOI] [PubMed] [Google Scholar]
- 49.Bartz JA, Hollander E. The neuroscience of affiliation: Forging links between basic and clinical research on neuropeptides and social behavior. Horm Behav. 2006;50:518–28. doi: 10.1016/j.yhbeh.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 50.Ozbay F, Fitterling H, Charney D, Southwick S. Social support and resilience to stress across the life span: a neurobiologic framework. Curr Psychiatry Rep. 2008;10:304–10. doi: 10.1007/s11920-008-0049-7. [DOI] [PubMed] [Google Scholar]
- 51.Ozbay F, Johnson DC, Dimoulas E, et al. Social support and resilience to stress: From neurobiology to clinical practice. Psychiatry (Edgmont) 2007;4:35–40. [PMC free article] [PubMed] [Google Scholar]
- 52.Hosein Souri TH. Relationship between resilience, optimism and psychological well-being in students of medicine. Procedia – Social and Behavioral Sciences. 2011;30:1541–44. [Google Scholar]
- 53.Wright LJ, Zautra AJ, Going S. Adaptation to early knee osteoarthritis: the role of risk, resilience, and disease severity on pain and physical functioning. Ann Behav Med. 2008;36:70–80. doi: 10.1007/s12160-008-9048-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


