Abstract
OBJECTIVE
To update national population-level pregnancy-related mortality estimates and examine characteristics and causes of pregnancy-related deaths in the United States during 2011–2013.
METHODS
We conducted an observational study using population-based data from the Pregnancy Mortality Surveillance System to calculate pregnancy-related mortality ratios by year, age group, and race–ethnicity groups. We explored 10 cause-of-death categories by pregnancy outcome during 2011–2013 and compared their distribution with those in our earlier reports since 1987.
RESULTS
The 2011–2013 pregnancy-related mortality ratio was 17.0 deaths per 100,000 live births. Pregnancy-related mortality ratios increased with maternal age, and racial–ethnic disparities persisted with non-Hispanic black women having a 3.4 times higher mortality ratio than non-Hispanic white women. Among causes of pregnancy-related deaths, the following groups contributed more than 10%: cardiovascular conditions ranked first (15.5%) followed by other medical conditions often reflecting pre-existing illnesses (14.5%), infection (12.7%), hemorrhage (11.4%), and cardiomyopathy (11.0%). Relative to the most recent report of Pregnancy Mortality Surveillance System data for 2006–2010, the distribution of cause-of-death categories did not change considerably. However, compared with serial reports before 2006–2010, the contribution of hemorrhage, hypertensive disorders of pregnancy, and anesthesia complications declined, whereas that of cardiovascular and other medical conditions increased (population-level percentage comparison).
CONCLUSION
The pregnancy-related mortality ratio and the distribution of the main causes of pregnancy-related mortality have been relatively stable in recent years.
The risk of death during and shortly after pregnancy from pregnancy-related causes has not declined in the United States for more than 25 years.1 Data from the Centers for Disease Control and Prevention’s (CDC) Pregnancy Mortality Surveillance System show that the pregnancy-related mortality ratio has increased from approximately 10 deaths per 100,000 live births in the early 1990s to 16 deaths per 100,000 live births for the aggregate period 2006–2010.2 The same data document important, persistent racial–ethnic disparities in pregnancy-related mortality for greater than 20 years and suggest a continuing increasing contribution of chronic diseases, particularly cardiovascular disease, to mortality.2 Reasons for the reported increase in pregnancy-related mortality are not entirely clear, although improvements in the identification of these events—use of data linkages and of a pregnancy question (ie, checkbox) on the 2003 U.S. standard death certificate—were shown to have an important contribution (Creanga AA, Callaghan WM. Recent increases in the U.S. maternal mortality rate: disentangling trends from measurement issues [letter]. Obstet Gynecol 2017;129:206–7).3,4
To provide the most recent national, population-level information regarding overall pregnancy-related mortality, causes of death, and populations at risk, we examine pregnancy-related mortality in the United States between 2011 and 2013, thus updating our previously published reports of aggregated 1987–2010 Pregnancy Mortality Surveillance System data.1,5–7
MATERIALS AND METHODS
We conducted an observational study using 2011–2013 data from the CDC’s Pregnancy Mortality Surveillance System. Fifty-two reporting areas (ie, 50 U.S. states, New York City, and Washington, DC) voluntarily submit to the CDC’s Division of Reproductive Health deidentified copies of death certificates for females 12–55 years who died during or within 1 year of pregnancy from any cause; when available, linked birth or fetal death certificates are also sent. Additional sources of information for the Pregnancy Mortality Surveillance System include computerized searches of Lexis Nexis, reports by public health agencies, including state-based maternal mortality review committees, professional organizations, and individual health care providers. A clinically trained medical epidemiologist (C.S.) reviews all the information available for each death, determines the relationship between death and pregnancy, and the underlying cause of death. All information is reviewed again by a committee composed of the original reviewer and independent reviewers (A.A.C., W.M.C.) after initial data entry and cause-of-death determination to increase the consistency in ascertainment. A pregnancy-related death is defined as the death of a woman during or within 1 year of pregnancy that was caused by a pregnancy complication, a chain of events initiated by pregnancy, or the aggravation of an unrelated condition by the physiologic effects of pregnancy.1 The temporal association between the pregnancy status and death is ascertained with one or more of the following: the pregnancy checkbox on the death certificate indicating the woman was pregnant at the time of death or describing the interval between the end of a pregnancy and death; words or codes indicating a pregnancy on the death certificate; notes indicating the duration of complications causing or events leading to death on the death certificate; or availability of a birth or fetal death certificate within 1 year of the woman’s death. The causal association between the pregnancy status and death is based on the clinical cause of death, the interval between the end of pregnancy and death, and the pathophysiology of pregnancy complications. Deaths attributable to a medical condition exacerbated by but not unique to pregnancy are not considered pregnancy-related if the temporal association between the pregnant status and death is known solely from a pregnancy checkbox stating “pregnant within a year”; if the checkbox states “pregnant within 42 days” or “pregnant within 90 days,” the death may be considered pregnancy-related or not depending on the cause of death and the pathophysiologic relationship between the cause and pregnancy.
Coding for the Pregnancy Mortality Surveillance System is based on a system developed in 1986 by the American College of Obstetricians and Gynecologists and the CDC Maternal Mortality Study Group. A 10-group cause-of-death classification including hemorrhage, infection, amniotic fluid embolism, thrombotic pulmonary or other embolism, hypertensive disorders of pregnancy, anesthesia complications, cerebrovascular accidents, cardiomyopathy, cardiovascular disease, and other noncardiovascular medical conditions is used for cause-of-death reporting. For each pregnancy-related death, the Pregnancy Mortality Surveillance System database includes the pregnancy outcome, associated medical conditions, and demographic and obstetric variables available in vital records.
For this analysis, maternal age was categorized as 19 or younger, 20–24, 25–29, 30–34, 35–39, or 40 years or older; race–ethnicity was categorized as non-Hispanic white, non-Hispanic black, Hispanic, or other; nativity or country of birth was categorized as U.S.- or foreign-born; maternal education was categorized as less than 12, 12, or greater than 12 completed years; marital status was categorized as married or living together or unmarried; pregnancy outcomes were grouped as undelivered, induced or spontaneous abortion, live birth, stillbirth, ectopic pregnancy, molar pregnancy, or unknown; and timing of death was categorized as: before delivery, day of delivery (0 days), 1–6, 7–41, 42–182, or 183–364 days postpartum. Data on race and ethnicity were missing for five women; in these women, race–ethnicity was assigned according to the predominant racial–ethnic group for the birthing population of women in the state where the woman died during the year of her death. Gestational trophoblast disease was the recorded pregnancy outcome for only one death during the period; in line with our previous Pregnancy Mortality Surveillance System report,2 for analysis purposes, we included this case in the undelivered category. Information on whether the woman was obese may be noted on death certificates as a contributing cause of death or may be obtained by calculating the prepregnancy body mass index {BMI, calculated as weight [kg]/[height (m)]2} using the woman’s height and prepregnancy weight recorded on the birth certificate; a woman with a BMI greater than 30 was considered obese.8
We calculated pregnancy-related mortality ratios (number of pregnancy-related deaths per 100,000 live births) for the 2011–2013 period by year and age group for the four race–ethnicity groups of interest. Denominator data (ie, live births) are from National Center for Health Statistics births reports.9–11 Analysis of cause-of-death data involved two steps: we first examined causes of pregnancy-related death by pregnancy outcome during 2011–2013 and then calculated proportionate maternal mortality (ie, specific cause of death as a percentage of all pregnancy-related deaths) to explore changes in causes of pregnancy-related deaths since 1987 using previously published Pregnancy Mortality Surveillance System data. All analyses, including χ2 or Fisher exact tests, used to compare women’s sociodemographic by racial–ethnic groups were conducted using STATA 14. Pregnancy Mortality Surveillance System data do not include any personal identifiers; thus, the CDC’s institutional review board deemed the study as research not involving human subjects.
RESULTS
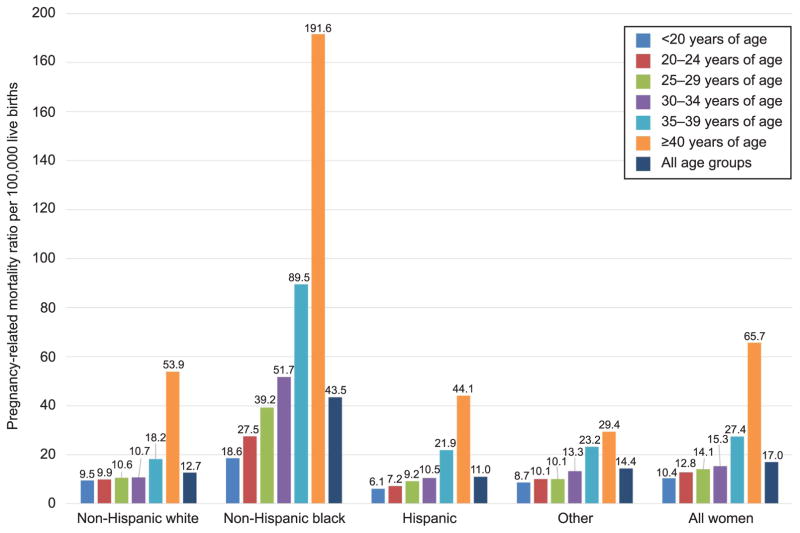
Data for 5,259 potential pregnancy-related deaths occurring between 2011 and 2013 were received by the CDC. Of these, 2,009 were found to be pregnancy-related (meeting both temporal and causal relationships with pregnancy), 3,131 were pregnancy-associated but not pregnancy-related (meeting only the temporal, not the causal relationship with pregnancy), and 62 were not pregnancy-associated (occurring more than 1 year after the end of pregnancy); for 57 women, neither the temporal nor the causal relationship between the death and pregnancy was met. This report is restricted to the 2,009 pregnancy-related deaths occurring in the United States during 2011–2013. Annual population-level pregnancy-related mortality ratios were 17.8 deaths per 100,000 live births in 2011, 15.9 deaths per 100,000 live births in 2012, and 17.3 deaths per 100,000 live births in 2013; the corresponding ratio for the 2011–2013 period was 17.0 deaths per 100,000 live births (Fig. 1).
Figure 1.
Population-level pregnancy-related mortality ratios by age, race–ethnicity, and overall for 2011–2013. Results are population-level and can be compared as absolute values.
Creanga. Pregnancy-Related Mortality in the United States. Obstet Gynecol 2017.
Forty percent of all pregnancy-related deaths during the period were among non-Hispanic white women, 37.9% among non-Hispanic black women, and 14.9% among Hispanic women, with few year-to-year differences (Table 1). For the 3-year period, specific race–ethnicity pregnancy-related mortality ratios were 12.7, 43.5, 11.0, and 14.4 deaths per 100,000 live births for non-Hispanic white, non-Hispanic black, Hispanic, and women of other races, respectively (Fig. 1). The ratio of the pregnancy-related mortality ratios between non-Hispanic black and non-Hispanic white women during 2011–2013 was 3.4 with an annual range between 3.2 (in 2013) and 3.6 (in 2012). Of all pregnancy-related deaths, 16.1% of deaths were in foreign-born women. More than half of Hispanic women (53.9%) and women of other races (55.5%) dying from pregnancy complications during this period were foreign-born compared with only 3.1% of non-Hispanic white and 8.2% of non-Hispanic black women.
Table 1.
Pregnancy-Related Deaths by Year and Women’s Sociodemographic Characteristics: United States, 2011–2013
| Characteristic | Race–Ethnicity
|
||||
|---|---|---|---|---|---|
| Non-Hispanic White (n=812) | Non-Hispanic Black (n=761) | Hispanic (n=299) | Other (n=137) | All Women (N=2,009) | |
| Maternal age (y) | |||||
| 19 or younger | 34 (4.2) | 40 (5.3) | 19 (6.4) | 3 (2.2) | 96 (4.8) |
| 20–24 | 132 (16.3) | 154 (20.2) | 52 (17.4) | 13 (9.5) | 351 (17.5) |
| 25–29 | 205 (25.3) | 177 (20.2) | 68 (22.7) | 26 (19.0) | 476 (23.7) |
| 30–34 | 195 (24.0) | 168 (22.1) | 61 (20.4) | 42 (30.7) | 466 (23.2) |
| 35–39 | 144 (17.7) | 139 (18.3) | 66 (22.1) | 40 (29.2) | 389 (19.4) |
| 40 or older | 102 (12.6) | 83 (10.9) | 33 (11.0) | 13 (9.5) | 231 (11.5) |
| Maternal education (y) | |||||
| Less than 12 | 128 (15.8) | 132 (17.4) | 95 (31.8) | 17 (12.4) | 372 (18.5) |
| 12 | 273 (33.6) | 275 (36.1) | 75 (25.1) | 37 (27.0) | 660 (32.9) |
| Greater than 12 | 343 (42.2) | 282 (37.1) | 73 (24.4) | 77 (56.2) | 775 (56.2) |
| Missing | 68 (8.4) | 72 (9.5) | 56 (18.7) | 6 (4.4) | 6 (4.4) |
| Marital status | |||||
| Married | 453 (55.8) | 207 (27.2) | 156 (52.2) | 94 (68.6) | 910 (45.3) |
| Unmarried | 353 (43.5) | 529 (69.5) | 141 (47.2) | 43 (31.4) | 1,066 (53.1) |
| Missing | 6 (0.7) | 25 (3.3) | 2 (0.7) | 0 (0.0) | 33 (1.6) |
| Foreign-born status | 25 (3.1) | 62 (8.2) | 161 (53.9) | 76 (55.5) | 324 (16.1) |
| Obesity recorded* | 148 (18.2) | 142 (18.7) | 37 (12.4) | 13 (9.5) | 340 (16.9) |
| Pregnancy outcome† | |||||
| Undelivered | 229 (28.2) | 212 (27.9) | 67 (22.4) | 24 (17.5) | 532 (26.5) |
| Abortion | 14 (1.7) | 17 (2.2) | 13 (4.4) | 4 (2.9) | 48 (2.4) |
| Live birth | 434 (53.5) | 398 (52.3) | 162 (54.2) | 84 (61.3) | 1,078 (53.7) |
| Stillbirth | 45 (5.5) | 31 (4.1) | 15 (5.0) | 7 (5.1) | 98 (4.9) |
| Ectopic | 20 (2.5) | 22 (2.9) | 8 (2.7) | 4 (2.9) | 54 (2.7) |
| Missing | 70 (8.6) | 81 (0.6) | 34 (11.4) | 14 (10.2) | 199 (9.9) |
All comparisons are statistically significant at P<.05 based on χ2 or Fisher exact tests.
Data are n (%).
On maternal death certificate, fetal death certificate, or live birth certificate.
The total number of live births during 2011–2013 was 11,838,612.
Three in 10 (30.9%) women who died from pregnancy-related conditions during the study period were older than 35 years of age (Table 1). Pregnancy-related mortality ratios increased with maternal age for all women, but, within age groups, non-Hispanic black women 40 years of age and older had the highest risk of dying from pregnancy complications (192 deaths per 100,000 live births; Fig. 1). Over the 2011–2013 period, the risk ratio for death among non-Hispanic black compared with non-Hispanic white women was lowest among teenagers (2:1), increased continuously with age reaching its peak among women in their 30s (4.8:1), and was slightly lower for women 40 years or older (3.6:1).
Among women who died from pregnancy-related conditions, a significantly higher proportion of Hispanic than non-Hispanic women had less than 12 years of education and a significantly lower proportion of non-Hispanic black women than women in any other race group were married (both P<.05; Table 1). Notably, approximately 18% of non-Hispanic white and black women were obese compared with 12.4% of Hispanic and 9.5% of other race women (Table 1). Of the 766 women with pregnancy-related deaths for whom the onset of prenatal care was known, 65 (8.5%) had not received any prenatal care and 188 (24.5%) started pre-natal care in their second or third trimester (data not shown).
Pregnancy outcomes were known for approximately 90% of pregnancy-related deaths (Table 1). Slightly more than one fourth (26.5%) of women were undelivered, more than half (53.7%) had a live birth, 4.9% a stillbirth, 2.7% an ectopic pregnancy, and 2.4% an induced or spontaneous abortion; one woman in our series was reported to have died after gestational trophoblastic disease. The timing of death in relation to the end of the pregnancy was known for 86.8% (n=1,743) of all women with pregnancy-related deaths during the 2011–2013 period (data not shown). Among these women, 532 (30.5%) died before delivery, 293 (16.8%) on the day of delivery or pregnancy termination, 317 (18.2%) between 1 and 6 days postpartum, and 372 (21.3%) between 7 and 41 days postpartum; only 229 (13.2%) died on or after 42 days postpartum. This latter proportion ranged between 7.4% among Hispanic and 14.6% among non-Hispanic black women.
Of the 10 groups of causes of death, the following contributed more than 10% of all pregnancy-related deaths during the period of study: cardiovascular conditions ranked first (15.5%) followed by other noncardiovascular medical conditions (14.5%), infection (12.7%), hemorrhage (11.4%), and cardiomyopathy (11.0%); the other groups of causes of death contributed between 0.2% and 9.2% (Table 2). Of note, cardiovascular conditions, cardiomyopathy, and other medical conditions contributed 40.9% and 46.8% of pregnancy-related deaths among non-Hispanic white and black women, respectively, but only 25.5% among women of other races and 31.3% among Hispanic women. Conversely, 39.5% of pregnancy-related deaths among Hispanic and 48.9% among other race women were attributable to hemorrhage, infection, and hypertensive disorders of pregnancy (data not shown).
Table 2.
Causes of Pregnancy-Related Death by Outcome of Pregnancy: United States, 2011–2013
| Cause of Death | Pregnancy Outcome
|
||||||
|---|---|---|---|---|---|---|---|
| Live birth | Stillbirth | Ectopic | Abortion | Undelivered | Unknown | Total | |
| Hemorrhage | 112 (10.4) | 21 (21.4) | 51 (94.4) | 6 (12.5) | 19 (3.6) | 19 (9.6) | 228 (11.4) |
| Ruptured ectopic | 1 | 0 | 51 | 0 | 2 | 0 | 54 |
| Uterine rupture or laceration | 11 | 9 | 0 | 3 | 2 | 3 | 28 |
| Abruptio placenta | 15 | 3 | 0 | 0 | 5 | 3 | 26 |
| Placenta previa | 5 | 0 | 0 | 0 | 1 | 0 | 6 |
| Placenta accrete, increta, or percreta | 10 | 3 | 0 | 0 | 3 | 3 | 19 |
| Retained products of conception | 3 | 0 | 0 | 0 | 1 | 0 | 4 |
| Atony or other uterine bleeding | 38 | 3 | 0 | 2 | 0 | 6 | 49 |
| Other or unspecified | 29 | 3 | 0 | 1 | 5 | 4 | 42 |
| Thrombotic pulmonary embolism* | 102 (9.5) | 2 (2.0) | 0 (0.0) | 4 (8.3) | 65 (12.2) | 11 (5.5) | 184 (9.2) |
| Amniotic pulmonary embolism | 86 (8.0) | 5 (5.1) | 0 (0.0) | 1 (2.1) | 8 (1.5) | 11 (5.5) | 111 (5.5) |
| Hypertensive disorders | 109 (10.1) | 12 (12.2) | 0 (0.0) | 1 (2.1) | 16 (3.0) | 10 (5.0) | 148 (7.4) |
| Preeclampsia | 63 | 8 | 0 | 0 | 6 | 7 | 84 |
| Eclampsia | 46 | 4 | 0 | 1 | 10 | 3 | 64 |
| Infection | 118 (11.0) | 16 (16.3) | 0 (0.0) | 19 (39.6) | 73 (13.8) | 29 (14.6) | 255 (12.7) |
| Chorioamnionitis | 4 | 1 | 0 | 2 | 1 | 2 | 10 |
| Genital tract | 1 | 0 | 0 | 0 | 0 | 0 | 1 |
| Sepsis | 66 | 6 | 0 | 11 | 27 | 15 | 125 |
| Other or unspecified | 47 | 9 | 0 | 6 | 45 | 12 | 119 |
| Anesthesia complications | 1 (0.1) | 0 (0.0) | 1 (1.9) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 3 (0.2) |
| Cardiomyopathy | 144 (13.4) | 6 (6.1) | 0 (0.0) | 2 (4.2) | 31 (5.8) | 38 (19.1) | 221 (11.0) |
| Cerebrovascular accident | 83 (7.7) | 3 (3.1) | 1 (1.9) | 0 (0.0) | 29 (5.5) | 17 (8.5) | 133 (6.6) |
| Cardiovascular conditions | 166 (15.4) | 9 (9.2) | 1 (1.9) | 4 (8.3) | 109 (20.5) | 23 (11.6) | 312 (15.5) |
| Noncardiovascular conditions | 103 (9.6) | 20 (20.4) | 0 (0.0) | 6 (12.5) | 132 (24.9) | 31 (15.6) | 292 (14.5) |
| Unknown | 54 (5.0) | 4 (4.1) | 0 (0.0) | 4 (8.3) | 50 (9.4) | 10 (5.0) | 122 (6.1) |
| Total | 1,078 (100) | 98 (100) | 54 (100) | 48 (100) | 532 (100) | 199 (100) | 2,009 (100) |
Data are n (%) or n.
Five “other” embolisms are included among the 184 thrombotic pulmonary embolisms.
The most common causes of death varied by pregnancy outcome. Among deaths after a live birth, thromboembolism, cardiomyopathy, and other cardiovascular conditions were the three most common causes of death, whereas hemorrhage, other noncardiovascular medical conditions, and infection were most commonly found with deaths after a stillbirth. Because 42 days postpartum represents the cutoff for the World Health Organization’s definition of maternal death12 as opposed to 1 year in our definition of pregnancy-related death, we used our data with known information on timing of death to examine which causes of death would be more likely under-counted using the former definition. Among the 1,743 women with a known interval between the end of pregnancy and death, 1,514 (86.9%) died during pregnancy or within 42 days of the end of pregnancy. Almost all pregnancy-related deaths from hemorrhage, hypertensive disorders of pregnancy, and amniotic fluid embolism occurred within 42 days postpartum (98.7%, 96.8%, and 100.0%, respectively). However, a considerable proportion of deaths attributable to the remaining cause-of-death groups occurred after 42 days—9.9% of deaths attributable to each thrombotic pulmonary embolism and infection, 17.0% of cerebrovascular accident deaths, 20.5% of cardiovascular condition deaths, 32.0% of other noncardiovascular medical condition deaths, and 55.2% of cardiomyopathy deaths.
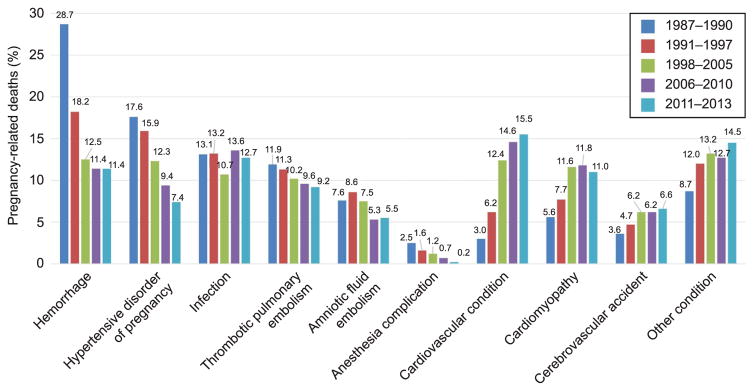
We compared proportionate maternal mortality (ie, percentage of all pregnancy-related deaths) by cause of death for five time periods: 1987–1990, 1991–1997, 1998–2005, 2006–2010, and 2011–2013, corresponding to previously published reports of Pregnancy Mortality Surveillance System data (Fig. 2). Relative to the 2006–2010 data, proportionate mortality by cause of death did not change considerably at the population level in 2011–2013, yet compared with data before the 2006–2010 period, at the population level, the contribution of hemorrhage, hypertensive disorders of pregnancy, and anesthesia complications declined, whereas that of cardiovascular, cerebrovascular accidents, and other medical conditions increased.
Figure 2.
Population-level, cause-specific proportionate pregnancy-related mortality for 1987–1990, 1991–1997, 1998–2005, 2006–2010, and 2011–2013. Results are population-level and can be compared as absolute values.
Creanga. Pregnancy-Related Mortality in the United States. Obstet Gynecol 2017.
DISCUSSION
This analysis used national, population-level data to examine 2011–2013 pregnancy-related deaths in the United States. The pregnancy-related mortality ratio exhibited relative stability with 16–17 deaths per 100,000 live births since 2008.1 The observed leveling of the trend may be the result of most states having adopted the new versions of death certificates including the pregnancy checkbox.3 During 2011–2013, less than 15% of births were to women 35 years or older,9–11 but 30% of pregnancy-related deaths were in this age group. Increasingly more pregnant women in the United States have chronic health conditions13–15 and are overweight or obese16,17; these conditions put pregnant women, especially those 40 years of age and older, at higher risk of adverse outcomes.1,2 Among 2011–2013 pregnancy-related deaths, 16.9% were in women for which prepregnancy obesity was recorded on vital statistics. We report obesity information given our higher confidence in the quality of this information in vital statistics data17,18 and the increasing attention from professional organizations on the management of obese pregnant women.8 Obesity information may be missing in our data, especially so for woman who died undelivered (no birth certificate). However, with one in six deaths in women whom we know were obese before pregnancy, there is need for health care providers to carefully consider the specific needs of pregnant obese women.
As per earlier Pregnancy Mortality Surveillance System reports,5,6 the contribution of traditional causes of pregnancy-related mortality (hemorrhage, hypertensive disorders of pregnancy, thromboembolism) continued to decline, whereas that of cardiovascular and other medical conditions increased. For both 2006–2010 and 2011–2013 periods in our reports, cardiovascular conditions, including cardiomyopathy, were responsible for approximately 26% of all pregnancy-related deaths.2 This proportion translates to a cardiovascular-specific pregnancy-related mortality ratio of 4.2 deaths per 100,000 live births in 2006–20101 and 4.8 deaths per 100,000 live births during 2011–2013. By comparison, although cardiovascular conditions were also the main cause of maternal mortality in the United Kingdom during the 2012–2014 period, the cardiovascular-specific maternal mortality ratio was 2 per 100,000 live births.19 Addressing cardiovascular disease in pregnancy requires early identification of disease, ideally before pregnancy, and continuous, risk-appropriate specialist care and follow-up throughout the pregnancy. Notable differences from the preceding Pregnancy Mortality Surveillance System report2 are the decline in proportionate mortality from hypertensive disorders of pregnancy (9.4% in 2006–2010 compared with 7.4% in 2011–2013) and infection (13.6% during 2006–2010 compared with 12.7% in 2011–2013). The latter is the result of fewer influenza-related deaths in 2011–2013 than 2006–2010 when the 2009 H1N1 pandemic disproportionally affected pregnant women.20,21
Racial–ethnic disparities in pregnancy-related mortality persisted during 2011–2013—non-Hispanic black women had a 3.4 times higher risk of dying from pregnancy complications than non-Hispanic white women. Our data also showed that half of Hispanic and other race women who died from pregnancy complications were foreign-born. These findings highlight the need to better understand how social determinants of health and barriers to risk-appropriate care can be addressed to promote optimal outcomes for all women.
Pregnancy Mortality Surveillance System data have limitations. Because pregnancy-related deaths are relatively rare events, their identification may still be incomplete. On the other hand, in our review of Pregnancy Mortality Surveillance System data in recent years, we have observed the marking of the pregnancy checkbox among women older than 45 years even in the absence of documentation of pregnancy status on death certificates. Although this may indicate a group of women with very high-risk pregnancies, the possibility of misclassification of deaths, also noted by others,22 cannot be excluded. Linkages of maternal death and birth or fetal death certificate data can be done regularly by states in an effort to validate the checkbox information to the extent possible. Even if the Pregnancy Mortality Surveillance System is the most comprehensive source of national maternal mortality data and its 10-category cause-of-death system is more granular than International Classification of Diseases, 10th Revision codes, it contains limited information for understanding modifiable contributors to pregnancy-related mortality. With more than half of U.S. states now having functional maternal mortality review committees, state-level data and reports of maternal mortality can be used in tandem with the Pregnancy Mortality Surveillance System data to provide specific, data-driven recommendations to prevent future maternal deaths. Although not all maternal deaths are preventable, obstetricians should be familiar with current levels and causes of pregnancy-related deaths in the United States. Collaborative efforts such as those between the California Department of Public Health and the California Maternal Quality Care Collaborative demonstrate the promise that reviewing maternal deaths for the purpose of taking action can reduce the risk of women dying from complications of pregnancy.23 Reviews of severe maternal morbidity can complement the information obtained from maternal mortality reviews and improve our understanding of factors leading to adverse maternal events.24
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Each author has indicated that he or she has met the journal’s requirements for authorship.
References
- 1.Centers for Disease Control and Prevention. Pregnancy-related mortality surveillance. Available at: http://www.cdc.gov/reproductivehealth/MaternalInfantHealth/PMSS.html. Retrieved December 21, 2016.
- 2.Creanga AA, Berg CJ, Syverson C, Seed K, Bruce C, Callaghan WM. Pregnancy-related mortality in the United States, 2006–2010. Obstet Gynecol. 2015;125:5–12. doi: 10.1097/AOG.0000000000000564. [DOI] [PubMed] [Google Scholar]
- 3.MacDorman MF, Declercq E, Cabral H, Morton C. Recent increases in the U.S. maternal mortality rate: disentangling trends from measurement issues. Obstet Gynecol. 2016;128:447–55. doi: 10.1097/AOG.0000000000001556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Joseph KS, Lisonkova S, Muraca GM, Razaz N, Sabr Y, Mehrabadi A, et al. Factors underlying the temporal increase in maternal mortality in the United States. Obstet Gynecol. 2017;129:91–100. doi: 10.1097/AOG.0000000000001810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berg CJ, Atrash HK, Koonin LM, Tucker M. Pregnancy-related mortality in the United States, 1987–1990. Obstet Gynecol. 1996;88:161–7. doi: 10.1016/0029-7844(96)00135-4. [DOI] [PubMed] [Google Scholar]
- 6.Berg CJ, Chang J, Callaghan WM, Whitehead SJ. Pregnancy-related mortality in the United States, 1991–1997. Obstet Gynecol. 2003;101:289–96. doi: 10.1016/s0029-7844(02)02587-5. [DOI] [PubMed] [Google Scholar]
- 7.Berg CJ, Callaghan WM, Syverson C, Henderson Z. Pregnancy-related mortality in the United States, 1998–2005. Obstet Gynecol. 2010;116:1302–9. doi: 10.1097/AOG.0b013e3181fdfb11. [DOI] [PubMed] [Google Scholar]
- 8.Weight gain during pregnancy. Committee Opinion No. 548. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2013;121:210–2. doi: 10.1097/01.aog.0000425668.87506.4c. [DOI] [PubMed] [Google Scholar]
- 9.Martin JA, Hamilton BE, Ventura SJ, Osterman MJ, Mathews TJ. Births: final data for 2011. Natl Vital Stat Rep. 2013;62:1–69.72. [PubMed] [Google Scholar]
- 10.Martin JA, Hamilton BE, Osterman MJ, Curtin SC, Matthews TJ. Births: final data for 2012. Natl Vital Stat Rep. 2013;62:1–68. [PubMed] [Google Scholar]
- 11.Martin JA, Hamilton BE, Osterman MJ, Curtin SC, Matthews TJ. Births: final data for 2013. Natl Vital Stat Rep. 2015;64:1–65. [PubMed] [Google Scholar]
- 12.Trends in maternal mortality: 1990 to 2015. WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division; Available at: http://apps.who.int/iris/bitstream/10665/194254/1/9789241565141_eng.pdf. Retrieved December 21, 2016. [Google Scholar]
- 13.Kuklina EV, Ayala C, Callaghan WM. Hypertensive disorders and severe obstetric morbidity in the United States: 1998–2006. Obstet Gynecol. 2009;113:1299–306. doi: 10.1097/AOG.0b013e3181a45b25. [DOI] [PubMed] [Google Scholar]
- 14.Albrecht SS, Kuklina EV, Bansil P, Jamieson DJ, Whiteman MK, Kourtis AP, et al. Diabetes trends among delivery hospitalizations in the U.S. 1994–2004. Diabetes Care. 2010;33:768–73. doi: 10.2337/dc09-1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuklina EV, Callaghan WM. Chronic heart disease and severe obstetric morbidity among hospitalizations for pregnancy in the USA: 1995–2006. BJOG. 2011;118:345–52. doi: 10.1111/j.1471-0528.2010.02743.x. [DOI] [PubMed] [Google Scholar]
- 16.Hinkle SN, Sharma AJ, Kim SY, Park S, Dalenius K, Brindley PL, et al. Prepregnancy obesity trends among low-income women, United States, 1999–2008. Matern Child Health J. 2012;16:1339–48. doi: 10.1007/s10995-011-0898-2. [DOI] [PubMed] [Google Scholar]
- 17.Deputy NP, Sharma AJ, Kim SY. Gestational weight gain—United States, 2012 and 2013. MMWR Morb Mortal Wkly Rep. 2015;64:1215–20. doi: 10.15585/mmwr.mm6443a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deputy NP, Sharma AJ, Kim SY, Hinkle SN. Prevalence and characteristics associated with gestational weight gain adequacy. Obstet Gynecol. 2015;125:773–81. doi: 10.1097/AOG.0000000000000739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Knight M, Nair M, Tuffnell D, Kenyon S, Shakespeare J, Brocklehurst P, et al., editors. Saving lives, improving mothers’ care—surveillance of maternal deaths in the UK 2012–14 and lessons learned to inform maternity care from the UK and Ireland confidential enquiries into maternal deaths and morbidity 2009–14. Oxford (United Kingdom): National Perinatal Epidemiology Unit, University of Oxford; 2016. [Google Scholar]
- 20.Callaghan WM, Creanga AA, Jamieson DJ. Pregnancy-related mortality resulting from influenza in the United States during the 2009–2010 pandemic. Obstet Gynecol. 2015;126:486–90. doi: 10.1097/AOG.0000000000000996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Siston AM, Rasmussen SA, Honein MA, Fry AM, Seib K, Callaghan WM, et al. Pandemic 2009 influenza A(H1N1) virus illness among pregnant women in the United States. JAMA. 2010;303:1517–25. doi: 10.1001/jama.2010.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.MacDorman MF, Declercq E, Thoma ME. Trends in maternal mortality by sociodemographic characteristics and cause of death in 27 states and the District of Columbia. Obstet Gynecol. 2017;129:811–818. doi: 10.1097/AOG.0000000000001968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.MCAH Bulletin. California maternal mortality rates. Available at: https://archive.cdph.ca.gov/data/statistics/Documents/2013MaternalMortalityRates-CA%20and%20US.pdf. Retrieved December 21, 2016.
- 24.Kilpatrick SJ, Berg C, Bernstein P, Bingham D, Delgado A, Callaghan WM, et al. Standardized severe maternal morbidity review: rationale and process. Obstet Gynecol. 2014;124:361–6. doi: 10.1097/AOG.0000000000000397. [DOI] [PMC free article] [PubMed] [Google Scholar]