Abstract
Objective
Patients with non-ischaemic systolic heart failure (HF) and idiopathic dilated cardiomyopathy (DCM) are a heterogenous group with varied morbidity and mortality. Prognostication in this group is challenging. We performed a systematic review and meta-analysis to examine the significance of the presence of contractile reserve as assessed via stress imaging on mortality and hospitalisation.
Methods
A search for studies that non-invasively assessed contractile reserve in patients with DCM or non-ischaemic HF with reduced ejection fraction, stress imaging with follow-up data comparing outcomes. A range of imaging modalities and stressors were included. We examined primary endpoints of mortality and secondary endpoints of combined cardiovascular events including HF progression or hospitalisation. Our analysis compared endpoints in patients with contractile reserve and those without it.
Results
Nine prospective cohort studies were identified describing a total of 787 patients. These studies are methodologically but not statistically heterogenous (I2 = 31%). Using a random effect model, the presence of contractile reserve was associated with a significantly lower risk of mortality and cardiovascular events odds ratios of 0.20 (CI 0.11, 0.39) (P < 0.00001) and 0.13 (CI 0.04, 0.40) (P = 0.0004), respectively.
Conclusion
Regardless of stressor and imaging modality and despite the significant methodological heterogeneity within the current data (imaging techniques and parameters), patients with non-ischaemic cardiomyopathy and reduced EF who demonstrate contractile reserve have a lower mortality, and lower events/hospitalisations. The presence of contractile reserve therefore offers a potential positive prognostic indicator when managing these patients.
Keywords: dilated cardiomyopathy, prognosis, stress echocardiography, contractile reserve
Introduction
Systolic heart failure (HF) is a heterogenous disease with a varied prognosis which can be poor despite best modern medical therapy (1). An accurate assessment of prognosis allows patients to receive better counselling before embarking on complex therapies including devices and referral for transplantation as well as providing appropriate end-of-life care with an appropriate timescale.
The ability to identify high-risk patients at initial assessment allows appropriately targeted specialist care and more intensive follow-up for those at high risk of admission and disease progression.
The current European Society of Cardiology guidelines do not provide a consensus on the best approach to prognostication in this patient group; however, they acknowledge that there should be a multimodality approach (2). Although several prognostic HF models exist and may help predict cardiac mortality in patients with HF, they are less useful for prediction of hospitalisations and a recent meta-analysis and meta-regression study of 117 prognostic models revealed only a moderate accuracy of models predicting mortality (3). Stress echocardiography plays a role in the assessment of a range of cardiac disease as evidenced by current European guidelines (4) but its place in the non-ischaemic systolic HF group is less clear and is not currently used regularly in clinical practice. Whilst useful in defining the presence of systolic HF, echocardiography-defined bands of severity (mild/moderate/severe) provide little incremental prognostic discrimination. NYHA class and EF severity (5, 6, 7) are associated with adverse outcomes but have significant limitations with respect to their long-term prognostic power (8).
The use of stress echocardiography to assess contractile reserve has shown promise as a prognostic indicator in the assessment of systolic HF (9) and specifically in the idiopathic dilated cardiomyopathy (DCM) subgroup (10). Current data describing the assessment of contractile reserve are highly varied and the generalisability of studies is limited by small cohort numbers and differing indices of contractile reserve.
‘Contractile reserve’ refers to the difference between myocardial contractility at rest compared to stress either through physiological means with exercise or pharmacological means such as the beta-adrenergic effects of dobutamine. Dipyridamole is predominantly vasodilatory causing increased coronary flow through inhibition of cellular re-uptake of adenosine. This increase in coronary perfusion may promote a rise in cardiac contractility through the Gregg phenomenon (11). Additionally, adenosine accumulation may exert direct sympathomimetic chemoreceptor activity stimulating cardiac contractility (12). The assessment of contractile reserve gives an indication of cardiac reserve i.e. the maximum amount by which cardiac output can be increased from a state of rest. Dobutamine stress assessment of contractile reserve may give an indication of beta-adrenergic receptor sensitivity and/or density in the myocardium of patients with DCM with mild or no symptoms (13).
Assessment of the presence of contractile reserve with non-invasive imaging techniques relies upon reliable and reproducible methods with clear parameters. These indices include an assessment of change in systolic function or LV dimensions with stress. Commonly used echocardiographic parameters include assessment of change in LV ejection fraction, wall motion score index (WMSI), LV dimensions and more recently LV global strain in the form of global circumferential and longitudinal strain % change. Radionuclide methods tend to use change in ejection fraction.
The objective of this systematic review and meta-analysis was to describe the current literature and to determine, with a higher degree of precision, whether reduced or absent contractile reserve in patients with non-ischaemic systolic HF predicts future events.
Methods
Search strategy
A literature search was performed using PubMed, Embase, Ovid, Google Scholar and the Cochrane Library for studies published between 1990 and 2016 in all languages. The PRISMA guidelines were adhered to for our meta-analysis. Authors of studies that were not published in English were contacted by email to request English versions. Authors of studies were also contacted by email to request clarification of data as required. Review articles relevant to this subject and their reference lists were also reviewed. Where the study subject was relevant but published data were inadequate for this meta-analysis, authors were emailed for clarification of unpublished data; we received 1 response with no additional data provided.
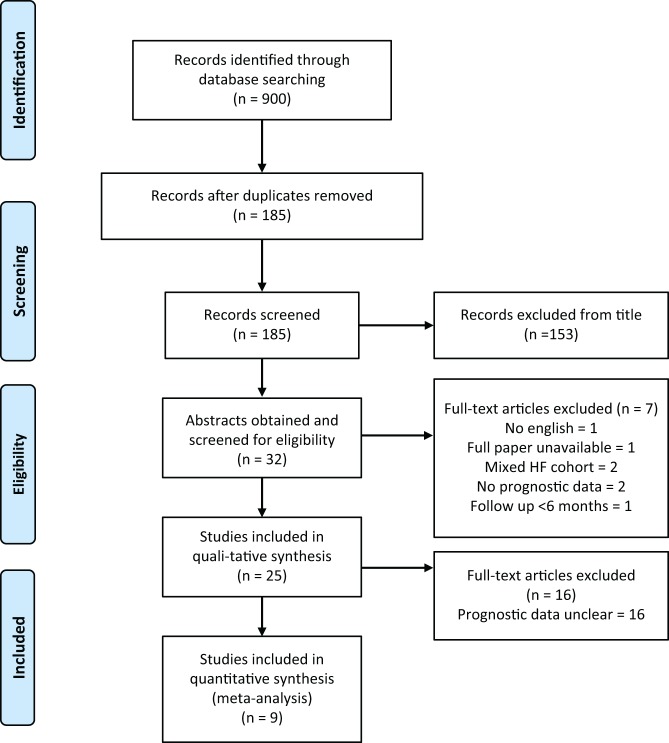
The following search criteria were used: ‘systolic HF and contractile reserve prognosis’; ‘DCM and contractile reserve’. Figure 1 illustrates our search strategy following the PRISMA guidelines (14).
Figure 1.
Search strategy following the PRISMA guidelines (14).
Inclusion and exclusion criteria
Articles were included in this meta-analysis if they involved any of the following:
Studies investigating the presence of contractile reserve in patients with non-ischaemic systolic HF and/or idiopathic DCM.
Imaging modalities included were transthoracic echocardiography with stress agents including dobutamine, exercise, dipyridamole or adenosine and radionuclide angiography.
Studies showing prognostic data with mortality or combined endpoints of cardiovascular events.
The following exclusion criteria were used: studies <20 patients, follow-up period of <12 months and prognostic data without clear comparison of contractile reserve. Studies were compared to ensure that the populations had not overlapped.
The studies were unmatched in terms of population demographics and represented the heterogenous patient population with non-ischaemic systolic HF. The clinical definitions for patients with DCM and exclusion methods for ischaemic heart disease were compared, and these often referred to now outdated WHO definitions from 1995 (15). The imaging modalities, indices recorded and methodology of stress were also compared in addition to baseline patient characteristics.
Outcomes
The primary outcome was total mortality. Secondary outcomes were combined cardiovascular and cardiac events including hospitalisation from decompensated HF and cardiac transplantation. The following variables were also assessed: methodology of contractile reserve assessment and criteria for presence of contractile reserve.
Statistical analysis
For each study, odds ratios (ORs) and confidence intervals (CIs) were calculated, both for primary and secondary outcomes. Because of methodological heterogeneity in the included studies, a random effect model was used to calculate the summary statistics and their 95% CIs. Statistical heterogeneity was assessed using with the chi-squared test. Data analysis was performed using Review Manager Version 5.3 (The Cochrane Collaboration, Update Software, Oxford, United Kingdom). Statistical support was provided by Paul Bassett, Statistical Consultant.
Results
Initial search results yielded 900, and following exclusion of duplicates, there were 185 potential studies for analysis; of these, 153 studies or review articles were excluded from their title as they did not assess the relevant patient group or clinical question. One relevant study had no available English translation, 2 included patients with mixed HF including ischaemic heart disease, 2 had no prognostic data and 1 paper had a follow-up period of <6 months. Twenty-five full-text articles were then requested and screened. Of these, 16 were then excluded due to lack of clarity regarding their prognostic data or comparison of patients with and without contractile reserve.
The total number of patients included in the remaining 9 studies was 787. Of these, 7 studies addressed the primary outcome of mortality, involving 580 patients. Pinamonti 2004 and Ramahi 2001 assessed transplant-free survival as the primary outcome; all others used cardiac or all-cause mortality as their primary outcome. Assessment of secondary outcomes of HF progression or hospitalisation was performed in 2 studies (11, 27) with 175 patients; these have been included in a separate analysis. These studies did not have significant statistical heterogeneity (I2 = 31%).
Assessment of contractile reserve in response to stressors (dobutamine/exercise/dipyridamole) was assessed most commonly using change in WMSI, used in 6 studies. The change in WMSI considered significant for the presence of contractile reserve varied from 0.15 to 0.44, with ≥0.25 being used in 3 studies. The 3 studies not using WMSI all assessed change in LV EF with a range of 2–10% used as significant for contractile reserve.
Table 1 displays relevant patient and study characteristics. There was a significant male predominance in all studies, 574 males (73%) with a relatively young patient population with mean age across all studies in the range of 45–62 years. All but one of the included studies has defined their patients’ resting LV EF in their inclusion criteria. In 5 studies, all patients have severe LV systolic dysfunction with an LV EF of <35%, a total of 489 patients. Three studies include patients with LV EF <40%, 226 patients. One study includes a range of LV systolic impairment from 20 to 50%, 71 patients.
Table 1.
Study characteristics and patient demographics.
| Paper details | Imaging and stress modality | Patient cohort | Cohort size | Contractile reserve criteria | DCM criteria used | Outcomes/endpoints assessed | Follow-up period |
|---|---|---|---|---|---|---|---|
| Stipac et al. (20) | High-dose dobutamine stress echocardiography – 5–40 µg/kg/min | 38 consecutive patients with DCM (31 men, mean age 50 +/− 10, LV EF 18.1% +/− 7, NYHA I–III) | 38 | Change in WMSI >0.19, EF increase of >2% | LVEDV >60 mm, LV EF <35%, (ETOH, IHD, arrhythmia, toxins, myocarditis, valvular heart disease, AF excluded) | Cardiac mortality | 60 months |
| Pratali et al. (10) | High-dose dobutamine stress echo (up to 40 µg/kg/min) | 186 patients with DCM (131 men, mean age 56 +/− 12 years, LV EF 25% +/− 7, NYHA I–IV) | 186 | Change in WMSI >0.44 | LV EF <35%, no coronary disease at angiogram | Cardiac mortality | 15 +/− 3 months |
| Pratali et al. (21) | Dipyridamole and dobutamine stress echocardiography. High-dose DSE 5-40 µg/kg/min | 87 patients with DCM (63 males, mean age 54 +/− 12, LV EF 23.7% +/− 8.2, NYHA 2.34 +/− 0.6) | 87 | Change in WMSI ≥ 0.25 | LV EF <35%, no coronary disease at angio within 5 years | All-cause mortality | 52 months (range 6–72) |
| Pinamonti et al. (22) | Dobutamine stress echo, 5–30 µg/kg/min | 51 patients with DCM, (33 males, 67%; mean age 45 +/−13, LV EF 24% +/− 6, NYHA 2.06 +/− 0.81) | 51 | Change in LV EF >10% and peak LVEF 40% | LV EF <40%, coronary angiogram and biopsy to exclude IHD/myocarditis | Transplant-free survival. Cardiac mortality or transplantation primary endpoints. Secondary endpoints include NYHA class and LVEF | 34 +/− 16 months |
| Pratali et al. (23) | Dipyridamole stress echo | 116 patients with DCM, (99 males, mean age 58 +/−12, LV EF 27.4% +/− 6.8, NYHA 2.5 +/− 0.6) | 116 | Change in WMSI ≥ 0.15 | Global LVSD, EF <35%, no IHD at angio within 5 years | Cardiac death free survival | 60 months |
| Parthenakis et al. (24) | Low dose dobutamine stress echo (5, 10, 15 µg/kg/min) | 43 consecutive patients with DCM (33 males, mean age 60.8 +/− 9.6, LV EF 31.9% +/− 7.2, NYHA II–III) | 43 | Change in WMSI >25% | Non-ischaemic DCM, not clearly defined | Cardiac mortality and re-hospitalisation for HF decompensation | 45 +/− 22 months |
| Ramahi et al. (25) | Low dose dobutamine equilibrium radionuclide ventriculography at 10 µg/kg/min | 62 patients with HFREF, non-ischaemic, (42 males, mean age 48 +/− 11, LV EF 20% +/− 6, NYHA 2.6 +/− 0.6) | 62 | Change in LVEF ≥ 8% | Severe LVSD, EF <30%, coronary disease excluded by angiography | All-cause mortality before cardiac transplantation | 25 +/− 15 months |
| Nagaoka et al. (26) | Exercise stress radionuclide angiography | 71 patients (52 men, 19 women) mean age 54. NYHA 1–II, LV EF 20– 50% | 71 | Change in LVEF ≥5% | Ischaemic CM excluded at angiography, AF, specific heart muscle disease, toxins and inherited conditions excluded | Cardiac mortality | 60 months |
| Rigo et al. (27) | Dipyridamole stress echo (0.84 mg/kg in 10 mins) | 132 patients with DCM, 90 males, age 62+/− 11. LVEF <40% (mean 32% +/− 7), angiographically normal coronaries & NYHA <or = III | 132 | Change in WMSI >0.25 | LV EF <40%, no history of coronary heart disease and angiographically normal coronary arteries at angiography before enrolment | All-cause mortality, cardiac mortality & development or progression of HF | 40 months |
DCM, dilated cardiomyopathy; LV EF, left ventricular ejection fraction; LVSD, LV systolic dysfunction; NYHA, New York Heart Association; WMSI, wall motion score index.
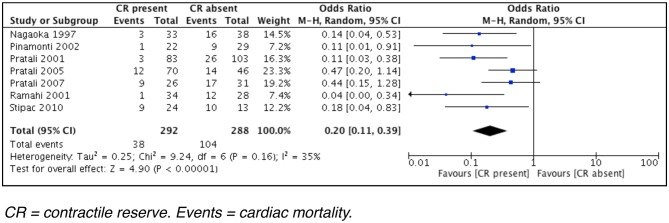
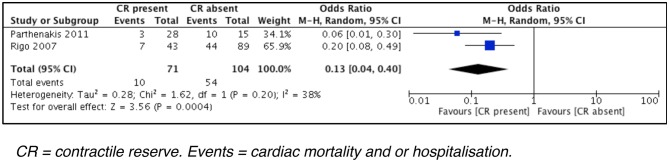
The presence of contractile reserve was associated with significantly lower mortality (Fig. 2), OR of 0.20 (CI 0.11, 0.39) (P = <0.0001). The presence of contractile reserve was also associated with significantly lower combined cardiovascular events (mortality and hospitalisation with HF) (Fig. 3), OR 0.13 (CI 0.04, 0.40) (P = 0.0004).
Figure 2.
Forest plot of primary outcome data (cardiac mortality).
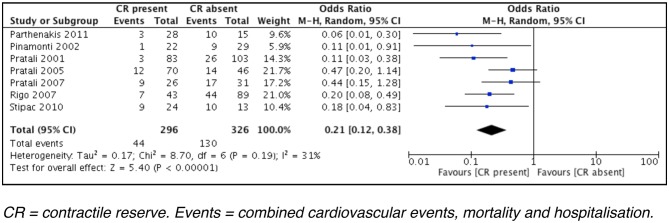
Figure 3.
Forest plot of secondary outcome data (combined cardiovascular events).
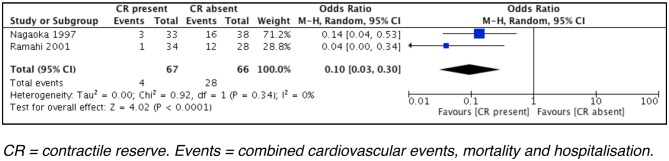
Comparing studies using imaging modalities of radionuclide angiography (Fig. 4; 2 studies, 165 patients) and echocardiography (Fig. 5; 7 studies, 796 patients) for LV function assessment, results demonstrate that either modality shows similar combined outcomes: OR of 0.10 (CI 0.03, 0.30) (P < 0.0001) for radionuclide angiography and an OR of 0.21 (CI 0.12, 0.38) (P < 0.00001) for echocardiography.
Figure 4.
Studies using radionuclide angiography (combined primary and secondary outcomes).
Figure 5.
Studies using echocardiography (combined primary and secondary outcomes).
Comparing studies using stressors of dobutamine (6 studies, 436 patients), dipyridamole (2 studies, 248 patients) and exercise (1 study, 71 patients) shows similar combined outcomes: OR of 0.14 (CI 0.07, 0.29 (P < 0.00001) for dobutamine, OR of 0.31 (CI 0.13, 0.72) (P < 0.007) for dipyridamole and OR of 0.14 (CI 0.04, 0.53) (P = 0.004) for exercise.
Discussion
This study confirms that in patients with non-ischaemic cardiomyopathy and significantly reduced EF, the presence of contractile reserve regardless of stressor (dobutamine/dipyridamole/exercise), or whether measured by echocardiography or nuclear methods, is associated with mortality that is 80% lower and similarly lowers event and hospitalisation rates.
There has long been a description of a significant incremental benefit in the use of contractile reserve during prognostic assessment of this patient group; however, limitations to the data set and particularly the heterogeneity of methods have precluded its routine incorporation into clinical practice. Incremental prognostic benefit of the presence of CR has been demonstrated compared to cardiopulmonary exercise testing (CPET) (23). CR assessment is of particular value when patients have limited ambulation or have equivocal CPET results.
This effect may not simply be confined to the LV; data (excluded from this meta-analysis) by Matsumoto and coworkers (16) have suggested that both LV and RV contractile reserves are independent parameters associated with cardiovascular events and produced an incremental prognostic value compared with clinical and baseline echocardiographic parameters. In a combined model, predictions based on clinical and baseline echocardiographic parameters were improved by the addition of LV contractile reserve parameters (change in global strain and EF) and further improved by adding RV contractile reserve (RV-free wall).
A subanalysis comparing the characteristics of resting vs stress LV systolic function is not possible with currently available data; as such, we cannot make a statistical assessment of the incremental value of contractile reserve. Current predictive models based around EF are recognised to be limited, so an incremental improvement can be safely assumed. This is also backed up by two studies (22, 23) that patients with the presence of contractile reserve are those with lower NYHA class and higher resting LV EF with a suggestion of significant incremental value in prognostic assessment with positive contractile reserve.
In the Pratali 2005 study, 71 patients (61%) were considered as responders (change in WMSI > 0.15) and 45 (39%) were classified as non-responders (change in WMSI < 0.15). Responders showed lower NYHA class (P = 0.03) and less severe left ventricular dysfunction (P = 0.02). LV EF 28.6 +/− 6.6 and NYHA 2.35 +/− 0.6 in responders vs LV EF 25.6 +/− 6.8 and NYHA 2.62 +/− 0.7 in non-responders. In the Pinamonti 2002 study, 22 (43%) patients were considered responders and 29 (57%) non-responders (change in LV EF >10% and peak LV EF 40%). Those with contractile reserve also had significantly higher resting LV EF (P = 0.046) and lower NYHA class (P = 0.0028). Although these are statistically significant differences, the absolute numbers of LV EF are all within the severe category <35% and the differences in LV EF % are small, given observer variability and accuracy of imaging modalities.
Deformation imaging is becoming increasingly important particularly to describe the long-axis function of the heart. Tissue Doppler Imaging and strain are both powerful additive tools in the echocardiographic assessment of LV systolic function. The use of these parameters in the assessment of contractile reserve may allow greater reproducibility and accuracy, adding to the prognostic usefulness of this test (17). We have previously described a strong positive prognostic effect of contractile reserve measured by S’ from spectral Tissue Doppler Imaging with exercise stress in patients with systolic HF (18).
A recent study (19) has compared the change in the systolic strain rate assessed by echocardiography and the change in maximum first derivative of LV pressure (LV dP/dtmax) derived from simultaneous left heart catheterisation as indices of contractility under stress with dobutamine. They also found a significant correlation between the percentage change in systolic strain rate and the percentage change in LV dP/dtmax. This study was performed in both normal controls and patients with DCM with results indicating a clear role for echocardiographic measurement of strain as a valid method for contractile reserve assessment.
Study limitations and areas for further research
The obvious and wide heterogeneity of the individual study methodologies represents the major limitation of this study. These studies do not have standardised inclusion criteria and, although broadly similar, do not share precise definitions for DCM. There is also significant heterogeneity in the follow-up of each study which will undoubtedly impact the total event rates over time with fewer events occurring in studies with shorter periods of follow-up. Likewise, the definitions of contractile reserve were fixed by the individual study investigators. The methodologies used to define a significant cutoff for the presence of CR are varied and often not clearly described. There is an acknowledgement of the continuous nature of this parameter and the need to avoid observer variability.
Nine studies use change in WMSI as their assessment of contractile reserve. This has been shown to be feasible and reproducible in several prior studies. Of these 6 studies, 3 use CR definition of change in WMSI > 0.25, the other 3 studies use different values (0.15–0.44). Other studies use change in LV EF as a marker of contractile reserve with differing values from 2% to 10%.
The majority of studies use stress echocardiography as their imaging modality of choices for assessment of CR. The stress agents used vary with dobutamine, dipyridamole and exercise being used; Rigo and c use both pharmacological stress agents as a form of comparison and conclude that there is clinical equivalence in ischaemia detection. It is less easy to understand how vasodilators induce a useful haemodynamic stress; however, there was no difference in effect size. There is however considerable heterogeneity in the data with regard to stressor dose used. Dose response to stressors could not be determined. The heterogeneity of follow-up data and small cohort sizes do not allow ‘time to event’ prognostication; however, absence of CR is demonstrated to be a marker of increased cardiovascular risk.
Conclusions
Patients with non-ischaemic systolic HF and absent contractile reserve die sooner than those with confirmed contractile reserve. The presence of contractile reserve is associated with statistically significant lower mortality, OR 0.2 (CI 0.11, 0.39) (P < 0.00001). It does not matter how the patients are assessed (echocardiography or nuclear radionuclide imaging) nor by which agent or method they are stressed. Impaired contractile reserve also demonstrates increased risk for a range of secondary endpoints, particularly hospitalisation which is critical in planning care needs.
The heterogeneity in these studies, which vary widely, suggests the need to develop agreed international standards for assessment of contractile reserve, which could be used in a suitably powered prospective study designed to develop a better prognostic model than that currently offered by resting data collection. It is intuitively clear that documenting the heart’s ability to augment its function in relation to demand will offer more information than that acquired in the resting state. This study confirms this and demonstrates that augmentation powerfully predicts prognosis and cardiac events in patients with DCM and non-ischaemic systolic HF.
Declaration of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding
This work did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
References
- 1.Meta-analysis Global Group in Chronic Heart Failure (MAGGIC). The survival of patients with heart failure with preserved or reduced left ventricular ejection fraction: an individual patient data meta-analysis. European Heart Journal 2012. 33 1750–1757. ( 10.1093/eurheartj/ehr254) [DOI] [PubMed] [Google Scholar]
- 2.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. European Journal of Heart Failure 2016. 18 891–975. ( 10.1002/ejhf.592) [DOI] [PubMed] [Google Scholar]
- 3.Ouwerkerk W, Voors AA, Zwinderman AH. Factors influencing the predictive power of models for predicting mortality and/or heart failure hospitalization in patients with heart failure. JACC Heart Failure 2014. 2 429–436. ( 10.1016/j.jchf.2014.04.006) [DOI] [PubMed] [Google Scholar]
- 4.Sicari R, Nihoyannopoulos P, Evangelista A, Kasprzak J, Lancellotti P, Poldermans D, Voigt JU, Zamorano JL. & European Association of Echocardiography. Stress echocardiography expert consensus statement: European Association of Echocardiography (EAE) (a registered branch of the ESC). European Journal of Echocardiography 2008. 9 415–437. ( 10.1093/ejechocard/jen175) [DOI] [PubMed] [Google Scholar]
- 5.Sugrue DD, Rodeheffer RJ, Codd MB, Ballard DJ, Fuster V, Gersh BJ. The clinical course of idiopathic dilated cardiomyopathy. A population-based study. Annals of Internal Medicine 1992. 117 117–123. [DOI] [PubMed] [Google Scholar]
- 6.Ciaccheri M, Castelli G, Nannini M, Santoro G, Troiani V, Di Lenarda A, Miani D, Sinagra G, Mestroni L, Risoli A, et al. The prognostic assessment of dilated cardiomyopathy: a follow-up of 138 patients. Giornale Italiano Di Cardiologia 1990. 20 645–650. [PubMed] [Google Scholar]
- 7.Hofmann T, Meinertz T, Kasper W, Geibel A, Zehender M, Hohnloser S, Stienen U, Treese N, Just H. Mode of death in idiopathic dilated cardiomyopathy: a multivariate analysis of prognostic determinants. American Heart Journal 1988. 116 1455–1463. ( 10.1016/0002-8703(88)90728-4) [DOI] [PubMed] [Google Scholar]
- 8.Parakh K1, Kittleson MM, Heidecker B, Wittstein IS, Judge DP, Champion HC, Barouch LA, Baughman KL, Russell SD, Kasper EK, et al. The variable natural history of idiopathic dilated cardiomyopathy. Israel Medical Association Journal 2012. 14 666–671. [PubMed] [Google Scholar]
- 9.Marmor A, Schneeweiss A. Prognostic value of non-invasively obtained left ventricular contractile reserve in patients with severe heart failure. JACC: Journal of the American College of Cardiology 1997. 29 422–428. ( 10.1016/S0735-1097(96)00493-7) [DOI] [PubMed] [Google Scholar]
- 10.Pratali L, Picano E, Otasevic P, Vigna C, Palinkas A, Cortigiani L, Dodi C, Bojic D, Varga A, Csanady M, et al. Prognostic significance of the dobutamine echocardiography test in idiopathic dilated cardiomyopathy. American Journal of Cardiology 2001. 88 1374–1378. ( 10.1016/S0002-9149(01)02116-6) [DOI] [PubMed] [Google Scholar]
- 11.Gregg DE. Effect of coronary perfusion pressure or coronary flow on oxygen usage of the myocardium. Circulation Research 1963. 13 497e500. [DOI] [PubMed] [Google Scholar]
- 12.Biaggioni I, Olafsson B, Robertson RM, Hollister AS, Robertson D. Cardiovascular and respiratory effects of adenosine in conscious man. Evidence for chemo- receptor activation. Circulation Research 1987. 61 779e86. [DOI] [PubMed] [Google Scholar]
- 13.Kobayashi M1, Izawa H, Cheng XW, Asano H, Hirashiki A, Unno K, Ohshima S, Yamada T, Murase Y, Kato TS, et al. Dobutamine stress testing as a diagnostic tool for evaluation of myocardial contractile reserve in asymptomatic or mildly symptomatic patients with dilated cardiomyopathy. JACC: Cardiovascular Imaging 2008. 1 718–726. ( 10.1016/j.jcmg.2008.04.012) [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG. & The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Medicine 2009. 6 e1000097 ( 10.1371/journal.pmed.1000097) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Richardson P, McKenna W, Bristow M, Maisch B, Mautner B, O’Connell J, Olsen E, Thiene G, Goodwin J, Gyarfas I, et al. Report of the 1995 World Health Organization/International Society and Federation of Cardiology Task Force on the definition and classification of cardiomyopathies. Circulation 1996 93 841–842. ( 10.1161/01.CIR.93.5.841) [DOI] [PubMed] [Google Scholar]
- 16.Matsumoto K, Tanaka H, Kaneko A, Ryo K, Fukuda Y, Tatsumi K, Kawai H, Hirata K. Contractile reserve assessed by three-dimensional global circumferential strain as a predictor of cardiovascular events in patients with idiopathic dilated cardiomyopathy. Journal of the American Society of Echocardiography 2012. 25 1299–1308. ( 10.1016/j.echo.2012.09.018) [DOI] [PubMed] [Google Scholar]
- 17.Matsumoto K, Tanaka H, Onishi A, Motoji Y, Tatsumi K, Sawa T, Miyoshi T, Imanishi J, Mochizuki Y, Hirata K. Bi-ventricular contractile reserve offers an incremental prognostic value for patients with dilated cardiomyopathy. European Heart Journal: Cardiovascular Imaging 2015. 16 1213–1223. ( 10.1093/ehjci/jev069) [DOI] [PubMed] [Google Scholar]
- 18.van Zalen J, Patel NR J, Podd S, Raju P, McIntosh R, Brickley G, Beale L, Sturridge LP, Lloyd GWL. Prognostic importance of tissue velocity imaging during exercise echocardiography in patients with systolic heart failure. Echo Research and Practice 2015. 2 19–27. ( 10.1530/ERP-14-0074) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Minoshima M, Noda A, Kobayashi M, Miyata S, Hirashiki A, Okumura T, Izawa H, Ishii H, Kondo T, Murohara T. Endomyocardial radial strain rate imaging during dobutamine stress echocardiography for the evaluation of contractile reserve in patients with dilated cardiomyopathy. Journal of Clinical Ultrasound 2016 44 555–560. ( 10.1002/jcu.22376) [DOI] [PubMed] [Google Scholar]
- 20.Stipac AV, Otasevic P, Popovic ZB, Cvorovic V, Putnikovic B, Stankovic I, Nesković AN. Prognostic significance of contractile reserve assessed by dobutamine-induced changes of Tei index in patients with idiopathic dilated cardiomyopathy. European Journal of Echocardiography 2010. 11 264–270. ( 10.1093/ejechocard/jep208) [DOI] [PubMed] [Google Scholar]
- 21.Pratali L, Otasevic P, Neskovic A, Molinaro S, Picano E. Prognostic value of pharmacologic stress echocardiography in patients with idiopathic dilated cardiomyopathy: a prospective, head-to-head comparison between dipyridamole and dobutamine test. Journal of Cardiac Failure 2007. 13 836–842. ( 10.1016/j.cardfail.2007.07.011) [DOI] [PubMed] [Google Scholar]
- 22.Pinamonti B, Perkan A, Di Lenarda A, Gregori D, Sinagra G. Dobutamine echocardiography in idiopathic dilated cardiomyopathy: clinical and prognostic implications. European Journal of Heart Failure 2002. 4 49–61. ( 10.1016/S1388-9842(01)00208-2) [DOI] [PubMed] [Google Scholar]
- 23.Pratali L, Otasevic P, Rigo F, Gherardi S, Neskovic A, Picano E. The additive prognostic value of restrictive pattern and dipyridamole-induced contractile reserve in idiopathic dilated cardiomyopathy. European Journal of Heart Failure 2005. 7 844–851. ( 10.1016/j.ejheart.2004.10.010) [DOI] [PubMed] [Google Scholar]
- 24.Parthenakis F, Patrianakos A, Nyktari E, Arfanakis D, Zacharis E, Vardas P. Prognostic value of NT-pro BNP, left ventricular inotropic reserve and cardiopulmonary exercise test in patients with non-ischemic dilated cardiomyopathy. International Journal of Cardiology 2011. 147 326–328. ( 10.1016/j.ijcard.2010.12.079) [DOI] [PubMed] [Google Scholar]
- 25.Ramahi TM, Longo MD, Cadariu AR, Rohlfs K, Slade M, Carolan S, Vallejo E, Wackers FJ. Dobutamine-induced augmentation of left ventricular ejection fraction predicts survival of heart failure patients with severe non-ischaemic cardiomyopathy. European Heart Journal 2001. 22 849–856. ( 10.1053/euhj.2001.2654) [DOI] [PubMed] [Google Scholar]
- 26.Nagaoka H, Isobe N, Kubota S, Iizuka T, Imai S, Suzuki T, Nagai R. Myocardial contractile reserve as prognostic determinant in patients with idiopathic dilated cardiomyopathy without overt heart failure. Chest 1997. 111 344–350. ( 10.1378/chest.111.2.344) [DOI] [PubMed] [Google Scholar]
- 27.Rigo F, Gherardi S, Galderisi M, Sicari R, Picano E. The independent prognostic value of contractile and coronary flow reserve determined by dipyridamole stress echocardiography in patients with idiopathic dilated cardiomyopathy. American Journal of Cardiology 2007. 99 1154–1158. ( 10.1016/j.amjcard.2006.11.049) [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a