Abstract
Social-emotional information processing (SEIP) was assessed in individuals with current DSM-5 Intermittent Explosive Disorder (IED: n = 100) and in healthy (n = 100) and psychiatric (n = 100) controls using a recently developed and validated self-rated questionnaire. SEIP vignettes depicted both direct aggressive and relationally aggressive scenarios of a socially ambiguous nature and were followed by questions assessing subjects' reactions and judgments about the vignettes. IED subjects differed from both healthy and psychiatric controls in all SEIP components. While hostile attribution was highly related to history of aggression, it was also directly correlated with negative emotional response. Further analysis revealed that this component, as well as response valuation and response efficiency, rather than hostile attribution, best explained history of aggressive behavior. A reformulated SEIP model, including self-reported history of childhood trauma, found that negative emotional response and response efficiency were the critical correlates for history of aggressive behavior. Psychosocial interventions of aggressive behavior in IED subjects may do well to include elements that work to reduce the emotional response to social threat and that work to restructure social cognition so that the tendency towards overt, or relationally, aggressive responding is reduced.
Keywords: Social emotional information processing, Hostile attribution, Negative emotion, Aggression
1. Introduction
Intermittent Explosive Disorder (IED), as operationalized in DSM-5, is a disorder of impulsive aggression (Coccaro, 2011). Recent epidemiological surveys reveal that IED is relatively common with the largest such study estimating the lifetime prevalence of DSM-5 IED at about 3.5% (Coccaro et al., in press), a lifetime prevalence rate greater than that of schizophrenia and bipolar disorder combined. In addition, IED aggregates in first-degree relations (Coccaro, 2010), is associated with reductions in indices of serotonin function (Coccaro et al., 2010), as well as abnormalities in indices of other neurotransmitter function (Coccaro et al., 1998, 2012a; 2012b, 2013; Lee et al., 2009), and responds to both psychopharmacologic (Coccaro et al., 2009a) and cognitive-behavioral intervention (McCloskey et al., 2008). Improved understanding of cognitive-emotional processes involved in aggression is needed to advance the scope of treatment approaches.
1.1. Social information processing (SIP) in aggression
Our biopsychosocial model of impulsive aggression posits that central neurotransmitters set the threshold at which one will “explode” in response to social threat, with other factors contributing to how this threshold is reached in each “here and now” moment of social interactions (Coccaro et al., 2011). These other factors include, but are not limited to, a dysfunction in social information processing (SIP) where SIP represents a series of cognitive – and emotional – steps individuals take in social situations when they respond to the actions of others towards them.
Models of SIP, first introduced over fifty years ago, seek to explain selected social behaviors such as decision making and problem solving (e.g., Abelson, 1968; Simon, 1969; Wyer, 1974). Later, a number of information processing models were developed to account for individual differences in aggressive behaviors (e.g., Crick and Dodge, 1994; Dodge, 1980; Huesmann, 1982, 1988, 1998). These models have focused on two broad sets of processes underlying aggressive behavior. First, encoding and interpretation of cues (e.g., attribution of intent, including hostile attribution) and, second, response assessment, response choice, and enactment (e.g., evaluation of the likelihood that each alternative will produce the desired outcomes) which Fontaine et al., 2008 has referred to as “response evaluation and decision making”.
Hostile attribution (HA) is the tendency to interpret the intent of others as “hostile” when in ambiguous interactions (Milich and Dodge, 1984). HA has been identified as a key etiologic element in the development and maintenance of aggressive behaviors (Orobio de Castro et al., 2002). “Aggressive” individuals are reported to attribute hostile intent more often than their “non-aggressive” counterparts (e.g., Fontaine and Dodge, 2006) and several studies report a positive relationship of HA with aggressive behavior (e.g., Bailey and Ostrov, 2008; Crick, 1995; Dodge, 1980; Dodge and Somberg, 1987; Feldman and Dodge, 1987; Hubbard et al., 2001; Orobio de Castro et al., 2002).
Relationships between HA and aggression have been examined primarily in samples of children or adolescents (Orobio de Castro et al., 2002 for review). In the past decade, the results of only a small number of studies in adults have been published (i.e., Bailey and Ostrov, 2008; Barefoot et al., 1989; Basquill et al., 2004; Epps and Kendall, 1995; MacBrayer et al., 2003; Matthews and Norris, 2002; Miller and Lynam, 2006), mostly in college students or in adults with mild mental retardation. Accordingly, the role for HA in aggression in adults with IED remains largely unexplored.
Cognitive variables beyond HA such as response assessment, outcome expectation, and response decision making, following an ambiguous social interaction, have been examined only recently, and most frequently, in children/adolescents (Fontaine et al., 2002, 2010). Response assessment involves evaluation of the “pros and cons” of different types of behavioral responses that the individual may choose in the context of socially ambiguous situations. Typically, individuals choose from socially appropriate, overtly aggressive, or relationally aggressive, responses. Outcome expectation is the consideration of what outcome may be expected if one chooses to enact one response or another. Response efficiency refers to the assessment of how easy it is for the individual to display a given response in a social interaction. Assessment of such factors can be readily added following controlled exposure to ambiguous social interactions.
Current SIP models of aggression have begun to go beyond cognition and are now examining the role of emotion and how the two are interrelated (Loeber and Coie, 2001). Both HA and emotion reactions to social threat are closely related components of SIP (Crick and Dodge, 1994; Guerra and Huesmann, 2004; Lemerise and Arsenio, 2000). Specifically, the presence of HA typically leads to a negative emotional response, suggesting that negative emotional response may mediate the relationship between HA and aggression (Coccaro et al., 2009b, 2016). Not surprisingly, negative emotions are positively associated with both aggressive behaviors (e.g., Arsenio et al., 2000; Cornell et al., 1999; Deater-Deckard et al., 2010; Eisenberg et al., 2009) and HA (Lemerise and Maulden, 2010) and are likely to be important in influencing response and outcome evaluation (Harper et al., 2010). That said, previous studies have not taken an integrative perspective of HA and negative emotional responding by examining the simultaneous effects of these two processes on aggression.
1.2. The role of childhood trauma/maltreatment in SIP models of aggression
Another key factor related to aggressive behavior appears is history of childhood trauma which consistently correlates with aggressive behavior later in childhood (Singer et al., 2013) and adolescence (Song et al., 1998). The relationship between childhood trauma and later aggressive behavior has also been found in adult subjects with prominent histories of impulsive aggressive behavior (Fanning et al., 2014). This relationship is mediated by hostile attribution (Dodge et al., 1990), a finding that has been replicated in subsequent studies including one of our own in a population-based sample of adults (Coccaro et al., 2009b). While the mechanism underlying this observation is unknown, experimental maltreatment of rodent pups has been shown to lead to heightened stress responses due to a failure to turn off genes regulating stress response (Zhang et al., 2013). This suggests that epigenetic changes associated with childhood trauma/maltreatment may affect social-emotional processing circuits. Accordingly, assessment for history of childhood trauma/maltreatment is a critical variable to include in studies of SIP and aggression.
1.3. The present study
Over the past decade, the authors developed a social and emotional information processing questionnaire (SEIP-Q) assessment in which both psychometric properties as well as patient-control differences in adult healthy volunteer and impulsive aggressive individuals were evaluated (Coccaro et al., 2016). The present work reports on a large number of patient and control subjects and is the first study in adult psychiatric participants to examine several aspects of SEIP simultaneously, including cognitive and emotional processing variables. Based on our previous data, and that of work in children and adolescents discussed above, we had three aims: Aim I: Examine how SEIP-Q variables differ among impulsively aggressive, psychiatric control, and healthy control, subjects. Aim II: Investigate the relationships between SEIP-Q variables and history of aggressive behavior, including testing how SEIP-Q variables explain variance in the relationship between HA and aggression. Aim III: Examine how SEIP-Q variables explain variance in the relationship between hostile attribution and aggression and between history of childhood trauma/maltreatment and aggression in later life.
2. Methods
2.1. Subjects
300 adult participants, with and without syndromal (formerly Axis I) or personality (formerly Axis II) disorders, were included in this study. This sample does not overlap with participants previously reported in our prior publications (Coccaro et al., 2009b, 2016). All study participants were systematically evaluated for impulsive aggressive and other personality-related behaviors. Subjects were recruited from clinical settings and through public service announcements seeking out individuals who: a) reported psychosocial difficulties related to one or more DSM-5 diagnoses (Psychiatric Controls: PC or Intermittent Explosive Disorder: IED) or, b) had little evidence of psychopathology (Healthy Controls: HC). All participants provided written informed consent and the study was approved by the Institutional Review Board (IRB). Potential participants with a life history of bipolar disorder, schizophrenia (or other psychotic disorder), or mental retardation, as were potential participants with a current substance use disorder, were excluded from this study.
2.2. Diagnostic assessment
Syndromal and personality disorder diagnoses were made by DSM-5 criteria (American Psychiatric Association, 2013). Diagnoses were made using information from: (a) the Structured Clinical Interview for DSM Diagnoses (SCID-I; First et al., 1997) and the Structured Interview for the Diagnosis of DSM Personality Disorder (SIDP; Pfohl et al., 1997); (b) clinical interview by a research psychiatrist; and, (c) review of all other available clinical data. The research diagnostic interviews were conducted by individuals with a masters or doctorate degree in Clinical Psychology after a rigorous training program including lectures on DSM diagnoses and rating systems, videos of expert raters conducting SCID/SIDP interviews, and practice interviews/ratings until the raters were deemed reliable with the trainer. This process resulted in good to excellent inter-rater reliabilities (mean kappa of 0.84 ± 0.05; range: 0.79 to 0.93) across anxiety, mood, substance use, impulse control, and personality disorders. Final DSM-5 diagnoses were assigned by team best-estimate consensus procedures involving research psychiatrists and clinical psychologists as previously described (Coccaro et al., 2012c). The various psychiatric diagnoses for all participants are listed in Table 1. For participants with any psychiatric diagnosis (n = 200), most (74.5%) reported: a) history of formal psychiatric evaluation and/or treatment (62.0%) or, b) history of behavioral disturbance during which the study participant, or others, thought they should have sought mental health services but did not (13.5%).
Table 1.
DSM-5 diagnoses in the sample.
| HC (N = 100) | PC (N = 100) | IED (N = 100) | |
|---|---|---|---|
| Current Syndromal Disorders: | |||
| Any Depressive Mood Disorder | 0 | 13 | 23 |
| Any Anxiety Disorder | 0 | 11 | 26 |
| Obsessive-Compulsive Disorders | 0 | 1 | 4 |
| Stress and Trauma Disorders | 0 | 7 | 17 |
| Eating Disorders | 0 | 3 | 6 |
| Somatoform Disorders | 0 | 1 | 1 |
| Non-IED Impulse Control Disorders | 0 | 0 | 0 |
| Lifetime Syndromal Disorders: | |||
| Any Depressive Mood Disorder | 0 | 41 | 70* |
| Any Anxiety Disorder | 0 | 15 | 33 |
| Any Substance Use Disordera | 0 | 41 | 47 |
| Obsessive-Compulsive Disorders | 0 | 4 | 6 |
| Stress and Trauma Disorders | 0 | 14 | 31 |
| Eating Disorders | 0 | 10 | 10 |
| Somatoform Disorders | 0 | 1 | 1 |
| Non-IED Impulse Control Disorders | 0 | 0 | 3 |
| Personality Disorders: | |||
| Any Personality Disorder | 0 | 57 | 94* |
| Any Specific Personality Disorder | 0 | 32 | 65* |
| Cluster A | 0 | 4 | 14 |
| Cluster B | 0 | 18 | 47* |
| Cluster C | 0 | 18 | 34 |
| PD-NOS | 0 | 25 | 29 |
p < 0.05 between PC and IED subjects (after adjusting for multiple comparisons).
Defined by DSM-5 as in sustained remission from a substance use disorder.
2.3. Measures
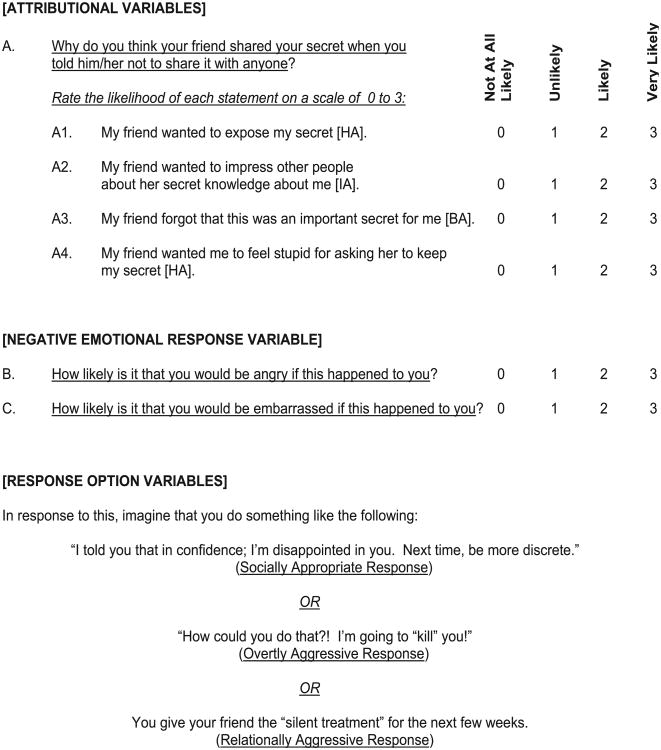
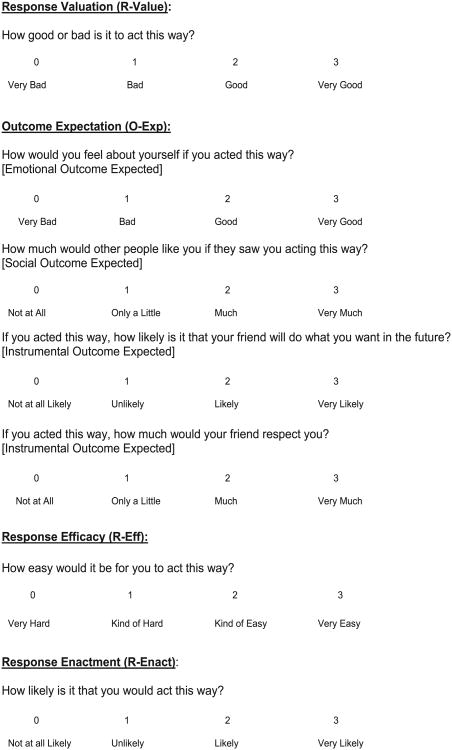
2.3.1. Social-emotional information processing questionnaire (SEIP-Q; Appendix)
The full SEIP-Q assesses attribution bias, emotional response, response valuation, outcome expectancy, response efficiency, and response enactment to socially ambiguous situations in which an adverse action is directed at “Person A” by “Person B”; subjects are asked to identify with “Person A”. Adverse actions were designed to fall into two categories: a) direct aggression (e.g., being “hit” by someone) and relational aggression (e.g., being “rejected” by someone). Each vignette is followed by four Likert-scaled questions that assessed direct hostile intent (e.g., “This person wanted to physically/emotionally hurt me”), indirect hostile intent (e.g., “This person wanted to make me look bad”), instrumental non-hostile intent (e.g., “This person wanted to win the match”), and neutral or benign intent (e.g., “This person did this by accident”). These attribution items were followed by two items designed to reflect Negative Emotional Response (NER; i.e., “How likely is it that you would be angry if this happened to you?” and “How likely is it that you would be upset with yourself if this happened to you?”). The SEIP-Q then assesses the desirability of three possible behavioral responses to each vignette: (a) socially appropriate response, (b) direct aggressive response and, (c) relationally aggressive response. Following each of these potential responses are seven items assessing response evaluation and decision making (RED) variables: “Response Valuation” (R-Value: e.g., “How good is it to act this way?”), “Outcome Expectation” (O-Exp: e.g., “If you acted this way, how would you feel about yourself?; How likely is it you will get what you want?; How likely is it that others will like you?, How likely is it that others will respect you?”), “Response Efficacy (R-Eff; e.g., “How easy is it for you to act this way?”). A final item, assessing the likelihood of choosing the proposed response, “Response Enactment” (R-Enact) was also obtained but not used in the hierarchical models testing relationships with history of actual aggressive events and with history of childhood trauma); see Appendix for example. All Likert-scaled ratings ranged from 0 (e.g., “Not At All Likely”) to 3 (e.g., “Very Likely”). RED variables were calculated for each of three response scenarios and were first examined as an overall RED variable for each scenario and then as the four separate components making up the overall RED variable. For ease of interpretation, individual SEIP-Q scores represent each variable as an averaged score on the same 0–3 scale. We have previously reported on the psychometrics of the attributional and emotional SEIP variables (Coccaro et al., 2009b) and of the response evaluation and decision making SEIP variables (Coccaro et al., 2016) with internal consistency and test-retest reliability in the good-to-excellent range.
2.4. Other measures
2.4.1. Overt aggressive and related behaviors
Overt aggressive behavior was quantified with the Aggression scale from the Life History of Aggression assessment [LHA; (Coccaro et al., 1997). LHA Aggression contains five items related to the actual lifetime frequency of temper tantrums, general fighting, specific physical assault, specific property assault, and verbal assault and has high internal consistency, excellent inter-rater reliability, and good test-retest reliability. Non-aggressive antisocial behavior was assessed with the Callous/Unemotional (Part 1) scale of the Psychopathic Checklist-Screening Version (PCL-SV; Hart et al., 2003). State level of depression was assessed using the Beck Depression Inventory-II (BDI-II; Beck and Brown, 1996).
2.4.2. Self-reported history of childhood trauma
Self-reported history childhood trauma was assessed using the Childhood Trauma Questionnaire (CTQ), a 28-item questionnaire assessing self-reported history of emotional abuse, physical abuse, emotional neglect, physical neglect, and sexual abuse in childhood. The CTQ has good internal, and test-retest, reliability (Bernstein and Fink, 1998). The total CTQ score was used in this study.
2.5. Statistical analysis
Differences between HC, PC, and IED subjects were tested using one-way ANCOVA/MANCOVA, or Chi-square statistics. Subsequently, Pearson correlation and multiple regression analyses were conducted to examine how different processes of SEIP-Q relate to each other. Finally, several hierarchical multiple regression models were analyzed to explore whether how the variables of the SEIP-Q explain variance in the relationship between hostile attribution and aggression and how SEIP-Q variables explain variance in the relationship between childhood trauma and aggression. All statistical tests were two-tailed using an alpha value of 0.05 and were conducted using SPSS 22.
3. Results
3.1. Sample characteristics
HC, PC, and IED participants differed in age, race, and in socio-economic class score (SES), but not sex. The age difference was due to a modestly greater age among IED and PC compared with HC participants; racial differences were due to fewer African-Americans among HC, compared with PC/IED subjects; SES score differences were due to lower scores among PC/IED, compared with HC, participants. Accordingly, we added each of these variables as covariates for all subsequent analyses. As expected, HC, PC, and IED participants differed in all behavioral measures of focus in this study. The direction of these differences was in the order of IED participants having higher (i.e., more pathologic) scores compared with PC participants who had higher scores compared with HC participants (Table 2).
Table 2.
Descriptive statistics of study variables.
| HC (N = 100) | PC (N = 100) | IED (N = 100) | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Mean | SD | Mean | SD | Mean | SD | |
| Demographic statistics | ||||||
| Gender (% males) | 50 | 42 | 40 | |||
| % White | 69 | 66 | 53 | |||
| % African American | 15 | 23 | 31 | |||
| % Other | 16 | 11 | 16 | |||
| Age | 33.4 | 12.9 | 36.2 | 11.7 | 37.3 | 10.9 |
| SES | 46.6 | 11.2 | 39.7a | 14.0 | 37.3b | 13.8 |
| Global and behavioral measures | ||||||
| Global assessment of function (GAF) | 84.7a | 5.7 | 65.2a | 11.2 | 55.1b | 8.8 |
| Life history of aggression (LHA) | 4.8a | 3.3 | 8.6a | 4.5 | 18.2b | 4.3 |
| Callous/unemotional psychopathy (PCL-SV) | 0.4a | 0.9 | 1.5b | 1.8 | 2.8c | 2.7 |
| BDI depression (BDI-II) | 4.4 | 11.6 | 9.9a | 10.9 | 15.4b | 11.1 |
| Childhood trauma history (CTQ) | 26.4 | 7.0 | 38.2a | 14.6 | 46.8b | 17.6 |
Note. Gobal GAF = Global Assessment of Function. EPQ = Eysenck Personality Questionnaires. LHA = Life History of Aggression. Between-group differences in each variable were examined using one-way ANOVAs or chi-square tests; groups with different superscripts are significantly different from each other.
HC significantly different from PC
PC significantly different from IED
IED significantly different from PC and HC.
3.2. Aim I: group differences in SEIP-Q variables
3.2.1. Attributional and emotional response variables
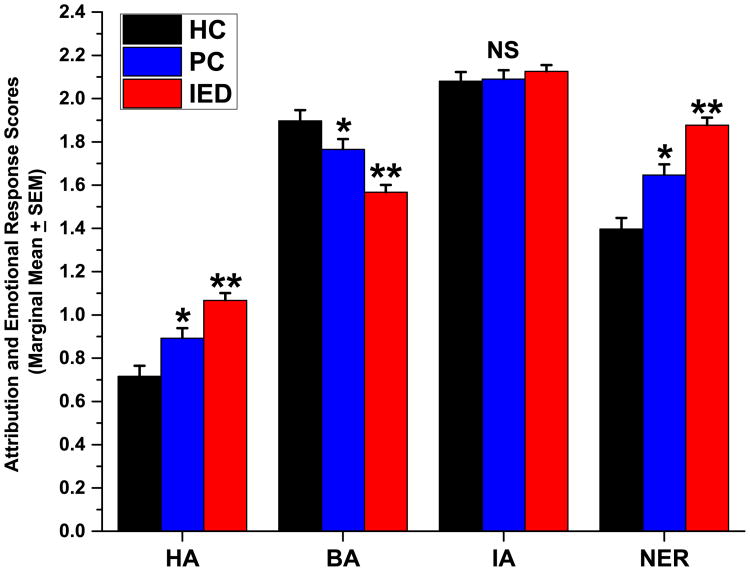
MANCOVA (covariates: age, sex, race, ses, and PCL-SV Part 1; dependent variables: HA, BA, IA, and NER) and follow-up ANCOVA analyses revealed significant between-group differences. Levels of HA, Benign Attribution (BA), and NER, but not levels of Instrumental Attribution (IA), differed significantly between IED and HC/PC participants (Fig. 1).
Fig. 1.
Marginal means (±SEM) from MANCOVA for Hostile Attribution (HA), Benign Attribution (BA), Instrumental Attribution (IA), and Negative Emotional Response (NER) scores. * Indicates post hoc p < 0.05 from HC participants; ** indicates post-hoc p < 0.05 from both HC and PC participants.
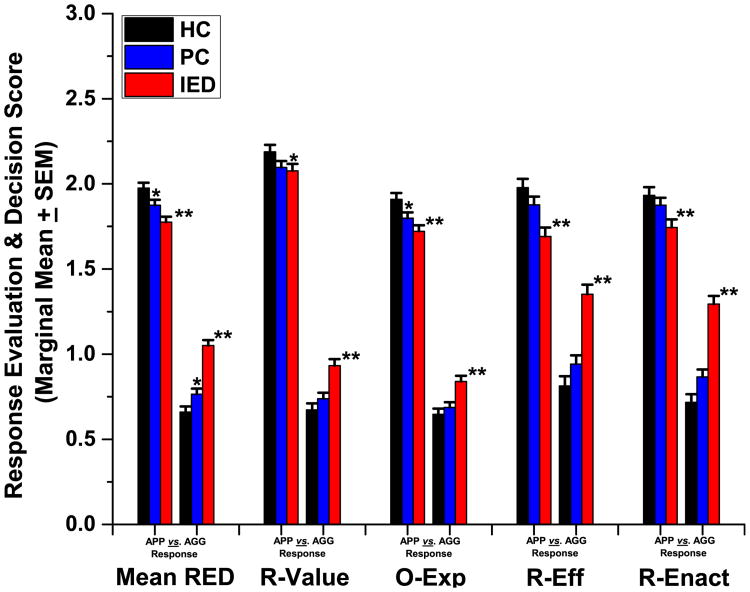
3.2.2. Response evaluation and decision SEIP variables
Overall, participants rated socially appropriate responses more favorably than aggressive responses to socially ambiguous stimuli (Appropriate Responses: 1.87 ± 0.33 vs. Aggressive Responses: 0.82 ± 0.38, paired t299 = 31.66, p < 0.001). Within the set of RED variables, IED participants reported reduced efficacy (R-Eff) for, and reduced likelihood of, carrying out (R-Enact) socially appropriate responses to ambiguous social threat compared to HC or PC participants. IED participants also differed from HC, but not PC, participants for Outcome-Expectancy (O-Exp) scores. As expected, IED participants expected more favorable outcomes for aggressive responses, be they overtly aggressive, or relationally, aggressive in nature, and less favorable outcomes for appropriate responses compared with HC participants (Fig. 2).
Fig. 2.
Marginal means (±SEM) from MANCOVA for Socially Appropriate (APP) compared with Aggressive (AGG) responses for Mean RED score (Mean RED), Response Valuation (R-Value), Outcome Expectancy (O-Exp), Response Efficacy (R-Eff) and Response Enactment (R-Enact) scores. * Indicates post-hoc p < 0.05 from HC participants; ** indicates post-hoc p < 0.05 from both HC and PC participants.
3.3. Aim II: nature of relationship between SEIP-Q variables and history of overt aggressive behavior
LHA Aggression represents a quantitative measure of actual aggressive events. As such, LHA is an ecologically valid index of aggression and appropriately used to investigate the role of SEIP variables in individual differences in aggressive behavior. As expected, each of the key SEIP variables correlated with LHA Aggression, including the RED variables for aggressive responses, correlated with LHA Aggression (i.e., HA: r = 0.32, NER: r = 0.40, mean RED score: r = 0.46; R-Value: r = 0.35, O-Exp: r = 0.31, R-Eff: r = 0.49; all ps < 0.001; n.b., R-Enact was not used in this analysis as it is conceptually very similar to LHA Aggression). Next, a hierarchical multiple regression analysis was performed to determine the unique relationships of these variables to LHA Aggression scores. HA and the relevant covariates were entered on Step 1; NER was added at Step 2; and mean RED score at Step 3. As expected, HA was positively associated with LHA aggression at Step 1). However, the addition of NER at Step 2 eliminated the relationship between LHA Aggression and HA and established a moderately strong relationship between LHA Aggression and NER. Adding mean RED score at Step 3 revealed a significant relationship between LHA Aggression and mean RED score and a continuing significant relationship with NER. Substituting R-Value, O-Exp, and R-Eff scores (for mean RED score) in the last step of the model revealed that, of these RED variables, only R-Eff displayed a significant relationship with LHA Aggression (β = 0.362, p < 0.001) (Table 3).
Table 3.
Regression models predicting life history of aggression with. Hostile attribution, negative emotional response with response evaluation and decision variables for aggressive responses.
| Variables entered | Model F | Model p | R2 | Δ R2 | F change | B | SE | b | p | |
|---|---|---|---|---|---|---|---|---|---|---|
| Step 1 model | (Covariates) | 8.69 | <0.001 | 0.129 | ||||||
| HA | 4.358 | 0.850 | 0.300 | <0.001 | ||||||
| Step 2 model | (Covariates) | 13.29 | <0.001 | 0.214 | 0.085 | 2–31.72 (p < 0.001) | ||||
| HA | 0.670 | 1.029 | 0.046 | 0.516 | ||||||
| NER | 5.119 | 0.909 | 0.394 | <0.001 | ||||||
| Step 3 model | (Covariates) | 15.91 | <0.001 | 0.276 | 0.062 | 0–25.08 (p < 0.001) | ||||
| HA | −0.994 | 1.044 | −0.068 | 0.342 | ||||||
| NER | 3.984 | 0.903 | 0.307 | <0.001 | ||||||
| RED | 5.680 | 1.134 | 0.320 | <0.001 |
3.4. Aim III: revised SEIP model of aggression including history ofearly life trauma in the Appendix
HA has been reported to mediate the relationship between early life history of trauma and aggression (Crick and Dodge, 1996). In the current sample HA and CTQ each correlated significantly with LHA Aggression (HA with CTQ: r = 0.30, HA with LHA: r = 0.32, CTQ with LHA: r = 0.53; each p < 0.001). Accordingly, we conducted a similar hierarchical multiple regression analysis to that described above, this time including CTQ as a predictor variable. CTQ scores (and relevant covariates) were entered at Step 1, HA at Step 2, NER at Step 3, mean RED score at Step 4. CTQ was significantly associated with LHA Aggression with a relatively large beta value at Step 1. The addition of HA, at Step 2, was associated with a small, but significant, relationship between HA and LHA Aggression and a small reduction in beta value for CTQ and LHA Aggression. The addition of NER at Step 3 was also associated with a significant relationship to LHA Aggression, but a substantial reduction in beta value and loss of statistical significance for HA, and a modest reduction in beta value for CTQ and LHA Aggression. In the final step, adding mean RED score for aggressive responses revealed a significant relationship between LHA Aggression and mean RED score and continuing significant relationships between LHA Aggression with CTQ and NER. Substituting R-Value, O-EXP, and R-Eff scores (for mean RED score) in the last step of the model revealed that, of these RED variables, only R-Eff displayed a significant relationship with LHA Aggression (β = 0.242, p < 0.001); Table 4.
Table 4.
Regression models predicting life history of aggression with childhood trauma questionnaire, hostile Attribution, and negative emotional response with response evaluation and decision variables for aggressive responses.
| Variables entered | Model F | Model p | R2 | Δ R2 | F change | B | SE | b | p | |
|---|---|---|---|---|---|---|---|---|---|---|
| Step 1 Model | (With Covariates) | 24.52 | <0.001 | 0.294 | ||||||
| CTQ | 0.224 | 0 0.022 | 0.520 | <0.001 | ||||||
| Step 2 Model | (Covariates) | 22.91 | <0.001 | 0.319 | 0.025 | 2–10.79 (p = 0.001) | ||||
| CTQ | 0.205 | 0.023 | 0.475 | <0.001 | ||||||
| HA | 2.517 | 0.766 | 0.173 | <0.001 | ||||||
| Step 3 Model | (Covariates) | 23.62 | <0.001 | 0.362 | 0.042 | 0–19.30 (p < 0.001) | ||||
| CTQ | 0.184 | 1–0.022 | 0.427 | <0.001 | ||||||
| HA | 0.047 | 0.932 | 0.003 | <0.962 | ||||||
| NER | 3.685 | 0.839 | 0.284 | <0.001 | ||||||
| Step 4 Model | (Covariates) | 24.26 | <0.001 | 0.400 | 0.039 | 6–18.70 (p < 0.001) | ||||
| CTQ | 0.171 | 1–0.022 | 0.396 | <0.001 | ||||||
| HA | −1.231 | 0–0.952 | −0.085 | <0.197 | ||||||
| NER | 2.888 | 0.835 | 0.222 | 0.001 | ||||||
| RED | 4.518 | 1–1.045 | 0.254 | <0.001 |
4. Discussion
In this study, IED study participants displayed elevated Hostile Attribution (HA) and Negative Emotional Response (NER) in response to vignettes depicting ambiguous, agonistic, social interactions, in comparison with both heathy and psychiatric controls. Specifically, HA and NER scores were both higher in IED participants compared with PC subjects who had higher scores on these variables compared with HC subjects; an inverse pattern was observed for Benign Attribution (BA) scores. Instrumental Attribution (IA) scores were not different across the groups despite the large between-group differences in life history of aggression. This was observed in our earlier study (Coccaro et al., 2009b). Accordingly, these attribution/emotional response variables appear to be dimensionally related to aggressive behavior.
Additionally, IED participants predicted less favorable outcomes for socially appropriate responses, and had lower self-efficacy for carrying out these responses, and reported they were less likely to carry out these responses than healthy participants. Despite the fact that most aggressive outbursts occurring in those with IED are not-premeditated, and are not done to achieve some tangible goal, IED participants still tend to justify their aggressive actions to themselves, consistent with their response patterns on the SEIP-Q. Thus, these data help support a cognitive psychotherapeutic approach with IED subjects to include specific cognitive restructuring aimed at reducing beliefs that such behaviors are “justifiable”, promote realistic expectations about outcomes, and enhance self-efficacy for carry out appropriate (as opposed to aggressive) responses.
Other novel findings include the nature of the relationship between SEIP-Q variables and aggression in the context of history of actual aggressive events (LHA Aggression) and in the context of history of childhood trauma (CTQ). For the first, we report that negative emotional response to ambiguous social stimuli is the strongest correlate of aggression history followed by efficacy of response. This is consistent with a recent study reporting that negative emotions (i.e., anger) influence aggressive children to focus on outcome (Harper et al., 2010). Our study did not find a role for outcome expectancy, overall, but we did find that IED participants had higher scores for SEIP variables related to instrumental, emotional, and social outcome. For the second, after all key SEIP variables are considered, only CTQ, NER, and R-Eff appear to be associated with LHA Aggression. This finding suggests, first, that NER accounts for the relationship between HA and life history of aggression and, second, that negative emotional response to ambiguous social stimuli and an individual's positive view of aggressive actions, are the prime correlates of actual aggressive behavior in the real world. This latter finding is partly consistent with that of Fontaine et al., 2010 who reported that response evaluation variables mediate the relationship between HA and antisocial behavior in school-aged children. In that study, a composite of all response evaluation and decision making variables fully mediated the relationship between HA and antisocial behavior across three time points. In this study, we broke down the individual components of response evaluation and decision making and found that not all components are relevant to aggressive behavior when all are considered simultaneously. While aggressive behavior is related to antisocial behavior, the two are not synonymous, and antisocial behavior includes non-overtly aggressive behaviors. Moreover, to reduce the potential influence of non-overtly aggressive antisocial behaviors, all analyses included callous/unemotional psychopathic traits as a covariate. Thus, these data represent relationships between SEIP and a more narrowly defined construct of aggressive behavior.
Previous studies have reported that HA mediates the relationship between childhood trauma and aggression (e.g, Dodge, et al., 1990). However, when included in statistical models, NER and R-Eff accounted for a significant portion of the variance in the LHA aggression scores while HA accounted for none. Overall, this suggests that the role of all SEIP variables, especially NER and R-Eff (and possibly R-Value), are needed to explain the development and/or maintenance of aggressive behavior. If so, psychosocial interventions of aggressive behavior may do well to include elements that work to reduce the emotional response to social threat so that aggressive behavior is reduced. Some, but not all, of these elements were included in a recent psychosocial intervention of aggression in IED. This trial, conducted in a modest number of study participants, included relaxation and coping skills training, but not empathy training, did find significant reductions in state aggression along with a reduction in hostile automatic thoughts (McCloskey et al., 2008). While effective, the number of IED participants reaching remission was less than 30%, suggesting that additional psychosocial elements may be needed to enhance the efficacy of this treatment approach.
Evidence supporting a link between social cognition and emotion has been accumulating over the past decade and subsequent empirical research has also supported a connection between emotional processing and hostile attribution bias as well as the possible relevance of newer SEIP variables related to response evaluation and outcome expectancy (Fontaine and Dodge, 2006). The notion that negative emotion may be critical to the development and maintenance of aggression is further supported by reports demonstrating that IED study participants produce significantly more errors in identifying expressions of facial emotions than controls (Best et al., 2002). In addition, the labeling of neutral faces as “angry” (proxy for hostile attribution) was correlated with history of childhood trauma in the IED participants in this study (unpublished data). Subsequent work reports that individuals with IED display a greater fMRI BOLD response to anger faces in the amygdala compared with controls (Coccaro et al., 2007; McCloskey et al., 2016) suggesting that non-verbal emotional cues related to possible threat in social situations may lead to aggressive actions through imbalances in cortico-limbic circuits (Coccaro et al., 2011), especially when those individuals have other neurobiologic abnormalities related to behavioral inhibition. This latter finding is in contrast to aggressive individuals high in callous/unemotional traits in whom fMRI BOLD responses to emotional stimuli in the amygdala is blunted compared with controls (Dolan and Fullam, 2009; Finger et al., 2011; Harenski et al., 2010; White et al., 2012). Accordingly, it is important to consider the presence of this form of psychopathy in future studies. Finally, this work sets the stage for the clinical neuroscience investigation of brain regions involved in SEIP in human subjects in which brief video clips, described by the SEIP-Q vignettes used this study, are presented to subjects during fMRI scanning.
Strengths of this study include the use of an assessment, based on established theoretical constructs, with good to excellent psychometric properties; a well characterized, clinically relevant, adult participant group; and relevant variables related to aggression and other behaviors and constructs.
Limitations include the fact that the study was cross-sectional in nature, participants were not primarily recruited from treatment settings, and that there was no control group characterized by non-impulsive aggression or a control group containing other disorders in which impulsive aggression may be observed. First, a longitudinal assessment of these data would be helpful in testing whether the variables in question can predict future impulsive aggressive events. That said, these data are consistent with previous data collected longitudinally (Pettit et al., 2010). Second, while study participants with a psychiatric history were not primarily recruited from treatment settings, nearly 75% had history of formal treatment for psychiatric disorder or of behavioral disturbance that should have been assessed by mental health professionals. Thus, most of the psychiatric participants in this study should be similar to those drawn from a treatment setting. Third, our psychiatric control group controlled for aggression and for psychiatric comorbidities in our IED participants but not for different types of aggression (e.g., impulsive vs. premeditated) or for other disorders in which aggression, impulsive or otherwise, may be seen. Studies including these types of study participants will be needed in the future in order to determine if there are higher-order interactions influencing any two-way associations that may exist.
5. Conclusions
First, social information processing biases that have been linked to aggressive behavior in childhood and adolescence continue to operate in adulthood. Accordingly, these biases should be targets for treatment intervention in adults with recurrent, problematic, impulsive aggressive behavior. Second, emotional processes are a key component of social cognition and aggression as previously suggested (Fontaine et al., 2010). Third, variables related to response evaluation and decision making are important in the development and maintenance of aggression.
Acknowledgments
This work was supported in part by grants from the National Institute of Mental Health:
RO1 MH104673 and R21 MH63262 (Dr. Coccaro) and from the Pritzker-Pucker Foundation.
Appendix
Sample SEIP Vignette
You tell a friend something personal and ask your friend not to discuss it with anyone else. However, a couple of weeks later, you find out that a lot of people know about it. You ask your friend why s/he told other people and your friend says, “Well, I don't know, it just came up and I didn't think it was a big deal.”
Footnotes
Contributors: Emil F. Coccaro, M.D
Jennifer R. Fanning, Ph.D
Sarah K. Keedy, Ph.D.
Royce Lee, M.D
Conflict of interest statement: Dr. Coccaro reports being on the Scientific Advisory Board of Azevan Pharmaceuticals, Inc. and being a current recipient of a grant award from the NIMH. Dr. Lee reports being a past recipient of a research grant from Azevan Pharmaceuticals, Inc. Drs. Fanning and Keedy report no conflicts of interest regarding this work.
References
- Abelson RP. Simulation of social behavior. In: Lindzey G, Aronson E, editors. Handbook of Social Psychology II. Addison-Wesley; Reading, MA: 1968. pp. 274–356. [Google Scholar]
- Arsenio WF, Cooperman S, Lover A. Affective predictors of preschoolers' aggression and peer acceptance: direct and indirect effects. Dev Psychol. 2000;36:438–448. [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders Fifth Edition. fifth. American Psychiatric Association Press; Washington, D.C: 2013. [Google Scholar]
- Bailey C, Ostrov J. Differentiating forms and functions of aggression in emerging adults: associations with hostile attribution biases and normative beliefs. J Youth Adolesc. 2008;37:713–722. [Google Scholar]
- Barefoot JC, Dodge KA, Peterson BL, Dahlstrom WG, Williams RB. The Cook–Medley hostility scale: item content and ability to predict survival. Psychosom Med. 1989;51:46–57. doi: 10.1097/00006842-198901000-00005. [DOI] [PubMed] [Google Scholar]
- Basquill M, Nezu C, Nezu A, Klein T. Aggression-related hostility bias and social problem-solving deficits in adult males with mental retardation. Am J Ment Retard. 2004;109:255–263. doi: 10.1352/0895-8017(2004)109<255:AHBASP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Beck AT, Brown GK. Beck Depression Inventory-II (BDI-II) The Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Bernstein DP, Fink L. Manual for the Childhood Trauma Questionnaire. The Psychological Corporation; New York: 1998. [Google Scholar]
- Best M, Williams JM, Coccaro EF. Evidence for a dysfunctional prefrontal circuit in patients with an impulsive aggressive disorder. Proc Natl Acad Sci U S A. 2002;99:8448–8453. doi: 10.1073/pnas.112604099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccaro EF. A family history study of intermittent explosive disorder. J Psychiatr Res. 2010;44:1101–1105. doi: 10.1016/j.jpsychires.2010.04.006. [DOI] [PubMed] [Google Scholar]
- Coccaro EF. Intermittent explosive disorder: development of integrated research criteria for Diagnostic and Statistical Manual of Mental Disorders. Compr Psychiatry. (fifth) 2011;52:119–125. doi: 10.1016/j.comppsych.2010.05.006. [DOI] [PubMed] [Google Scholar]
- Coccaro EF, Sripada CS, Yanowitch RN, Phan KL. Corticolimbic function in impulsive aggressive behavior. Biol Psychiatry. 2011;69:1153–1159. doi: 10.1016/j.biopsych.2011.02.032. [DOI] [PubMed] [Google Scholar]
- Coccaro EF, Berman ME, Kavoussi RJ. Assessment of life history of aggression: development and psychometric characteristics. Psychiatry Res. 1997;73:147–157. doi: 10.1016/s0165-1781(97)00119-4. [DOI] [PubMed] [Google Scholar]
- Coccaro EF, Fanning J, Lee R. Intermittent explosive disorder and substance use disorder: analysis of the national comorbidity study - replication sample. J Clin Psychiatry. 2016 doi: 10.4088/JCP.15m10306. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccaro EF, Fanning J, Lee R. Development of a social emotional information processing assessment for adults (SEIP-Q) Aggress Behav. 2016 Jun 20; doi: 10.1002/ab.21661. E-Pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccaro EF, Kavoussi RJ, Hauger RL, Cooper TB, Ferris CF. Cerebrospinal fluid vasopressin levels: correlates with aggression and serotonin function in personality-disordered subjects. Arch Gen Psychiatry. 1998;55:708–714. doi: 10.1001/archpsyc.55.8.708. [DOI] [PubMed] [Google Scholar]
- Coccaro EF, Lee R, Kavoussi RJ. A double-blind, randomized, placebo-controlled trial of fluoxetine in patients with intermittent explosive disorder. J Clin Psychiatry. 2009a;70:653–662. doi: 10.4088/JCP.08m04150. [DOI] [PubMed] [Google Scholar]
- Coccaro EF, Lee R, Kavoussi RJ. Aggression, suicidality, and intermittent explosive disorder: serotonergic correlates in personality disorder and healthy control subjects. Neuropsychopharmacology. 2010;35:435–444. doi: 10.1038/npp.2009.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccaro EF, Lee R, Liu T, Mathe AA. CSF NPY correlates with aggression in human subjects. Biol Psychiatry. 2012a;72:997–1003. doi: 10.1016/j.biopsych.2012.07.029. [DOI] [PubMed] [Google Scholar]
- Coccaro EF, Lee R, Owens MJ, Kinkead B, Nemeroff CB. Cerebrospinal fluid substance P-Like immunoreactivity correlates with aggression in personality disordered subjects. Biol Psychiatry. 2012b;72:238–243. doi: 10.1016/j.biopsych.2012.02.023. [DOI] [PubMed] [Google Scholar]
- Coccaro EF, Lee R, Vezina P. Cerebrospinal fluid glutamate concentration correlates with impulsive aggression in human subjects. J Psychiatr Res. 2013;47:1247–1253. doi: 10.1016/j.jpsychires.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccaro EF, McCloskey MS, Fitzgerald DA, Phan KL. Amygdala and orbitofrontal reactivity to social threat in individuals with impulsive aggression. Biol Psychiatry. 2007;62:168–178. doi: 10.1016/j.biopsych.2006.08.024. [DOI] [PubMed] [Google Scholar]
- Coccaro EF, Nayyer H, McCloskey MS. Personality disorder-not otherwise specified evidence of validity and consideration for DSM-5. Compr Psychiatry. 2012c;53:907–914. doi: 10.1016/j.comppsych.2012.03.007. [DOI] [PubMed] [Google Scholar]
- Coccaro EF, Noblett KL, McCloskey MS. Attributional and emotional responses to socially ambiguous cues: validation of a new assessment of social/emotional information processing in healthy adults and impulsive aggressive patients. J Psychiatr Res. 2009b;43:915–925. doi: 10.1016/j.jpsychires.2009.01.012. [DOI] [PubMed] [Google Scholar]
- Cornell DG, Peterson CS, Richards H. Anger as a predictor of aggression among incarcerated adolescents. J Consult Clin Psychol. 1999;67:108–115. doi: 10.1037//0022-006x.67.1.108. [DOI] [PubMed] [Google Scholar]
- Crick N. Relational aggression: the role of intent attributions, feelings of distress, and provocation type. Dev Psychopathol. 1995;7:313–322. [Google Scholar]
- Crick N, Dodge K. A review and reformulation of social information-processing mechanisms in children's social adjustment. Psychol Bull. 1994;115:74–1101. [Google Scholar]
- Crick N, Dodge K. Social information-processing mechanisms in reactive and proactive aggression. Child Dev. 1996;67:993–1002. [PubMed] [Google Scholar]
- Deater-Deckard K, Beekman C, Wang Z, Kim J, Petrill S, Thompson L, DeThorne L. Approach/positive anticipation, frustration/anger, and overt aggression in childhood. J Pers. 2010;78:991–1010. doi: 10.1111/j.1467-6494.2010.00640.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge K. Social cognition and children's aggressive behavior. Child Dev. 1980;51:162–170. [PubMed] [Google Scholar]
- Dodge K, Somberg D. Hostile attributional biases among aggressive boys are exacerbated under conditions of threats to the self. Child Dev. 1987;58:213–224. doi: 10.1111/j.1467-8624.1987.tb03501.x. [DOI] [PubMed] [Google Scholar]
- Dodge KA, Bates JE, Pettit GS. Mechanisms in the cycle of violence. Science. 1990;250(4988):1678–1683. doi: 10.1126/science.2270481. [DOI] [PubMed] [Google Scholar]
- Dolan MC, Fullam RS. Psychopathy and functional magnetic resonance imaging blood oxygenation level-dependent responses to emotional faces in violent patients with schizophrenia. Biol Psychiatry. 2009;66:570–577. doi: 10.1016/j.biopsych.2009.03.019. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Valiente C, Spinrad TL, Cumberland A, Liew J, Reiser M, Losoya SH. Longitudinal relations of children's effortful control, impulsivity, and negative emotionality to their externalizing, internalizing, and co-occurring behavior problems. Dev Psychol. 2009;45:988–1008. doi: 10.1037/a0016213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epps J, Kendall PC. Hostile attributional bias in adults. Cogn Ther Res. 1995;19:159–178. [Google Scholar]
- Fanning JR, Meyerhoff JJ, Lee R, Coccaro EF. History of childhood maltreatment in intermittent explosive disorder and suicidal behavior. J Psychiatr Res. 2014;56:10–17. doi: 10.1016/j.jpsychires.2014.04.012. [DOI] [PubMed] [Google Scholar]
- Feldman E, Dodge K. Social information processing and sociometric status: sex, age, and situational effects. J Abnorm Child Psychol. 1987;15:211–227. doi: 10.1007/BF00916350. [DOI] [PubMed] [Google Scholar]
- Finger EC, Marsh AA, Blair KS, Reid ME, Sims C, Ng P, Blair RJ. Disrupted reinforcement signaling in the orbitofrontal cortex and caudate in youths with conduct disorder or oppositional defiant disorder and a high level of psychopathic traits. Am J Psychiatry. 2011;168:152–162. doi: 10.1176/appi.ajp.2010.10010129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) Psychiatric Institute Biometrics Research; New York: 1997. [Google Scholar]
- Fontaine R, Dodge K. Real-time decision making and aggressive behavior in youth: a heuristic model of response evaluation and decision (RED) Aggress Behav. 2006;32:604–624. doi: 10.1002/ab.20150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontaine RG, Burks VS, Dodge KA. Response decision processes and externalizing behavior problems in adolescents. Dev Psychopathol. 2002;14:107–122. doi: 10.1017/s0954579402001062. [DOI] [PubMed] [Google Scholar]
- Fontaine RG, Tanha M, Yang C, Dodge KA, Bates JE, Pettit GS. Does response evaluation and decision (RED) mediate the relation between hostile attributional style and antisocial behavior in adolescence? J Abnorm Child Psychol. 2010;38:615–626. doi: 10.1007/s10802-010-9397-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontaine RG, Yang C, Dodge KA, Bates JE, Pettit GS. Testing an individual systems model of response evaluation and decision (RED) and antisocial behavior across adolescence. Child Dev. 2008;79:462–475. doi: 10.1111/j.1467-8624.2007.01136.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerra NG, Huesmann LR. A cognitive-ecological model of aggression. Rev Int Psychol Soc. 2004;2:177–204. [Google Scholar]
- Harenski CL, Harenski KA, Shane MS, Kiehl KA. Aberrant neural processing of moral violations in criminal psychopaths. J Abnorm Psychol. 2010;119:863–874. doi: 10.1037/a0020979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper BD, Lemerise EA, Caverly SL. The effect of induced mood on children's social information processing: goal clarification and response decision. J Abnorm Child Psychol. 2010;38:575–586. doi: 10.1007/s10802-009-9356-7. [DOI] [PubMed] [Google Scholar]
- Hart SD, Cox DN, Hare RD. Hare Psychopathy Checklist: Screening Version (PCL-SV) MHS; Toronto, Ontario, Canada: 2003. [Google Scholar]
- Hubbard J, Dodge K, Cillessen A, Coie J, Schwartz D. The dyadic nature of social information processing in boys' reactive and proactive aggression. J Person Soc Psychol. 2001;80:268–280. doi: 10.1037/0022-3514.80.2.268. [DOI] [PubMed] [Google Scholar]
- Huesmann LR. Information processing models of behavior. In: Hirschberg N, Humphreys L, editors. Multivariate Applications in the Social Sciences. Lawrence Erlbaum Associates; Hillsdale, NJ: 1982. pp. 261–288. [Google Scholar]
- Huesmann LR. An information processing model for the development of aggression. Aggress Behav. 1988;14:13–24. [Google Scholar]
- Huesmann LR. The role of social information processing and cognitive schema in the acquisition and maintenance of habitual aggressive behavior. In: Geen R, Donnerstein E, editors. Human Aggression. Academic Press; San Diego, CA: 1998. pp. 73–109. 1998. [Google Scholar]
- Lee R, Ferris C, Van de Kar LD, Coccaro EF. Cerebrospinal fluid oxytocin, life history of aggression, and personality disorder. Psychoneuroendocrinology. 2009;34(10):1567–1573. doi: 10.1016/j.psyneuen.2009.06.002. [DOI] [PubMed] [Google Scholar]
- Lemerise E, Arsenio W. An integrated model of emotion processes and cognition in social information processing. Child Dev. 2000;71:107–118. doi: 10.1111/1467-8624.00124. [DOI] [PubMed] [Google Scholar]
- Lemerise E, Maulden J. Emotions and social information processing: implication for understanding aggressive (and non-aggressive) children. In: Arsenio W, Lemerise E, editors. Emotions, Aggression, and Moral Development: Bridging Development and Psychopathology. American Psychological Association; Washington, DC: 2010. pp. 157–176. [Google Scholar]
- Loeber R, Coie J. Continuities and discontinuities of development, with particular emphasis on emotional and cognitive components of disruptive behaviour. In: Hill J, Maughan B, editors. Conduct Disorders in Childhood and Adolescence. Cambridge University Press; New York: 2001. pp. 379–407. [Google Scholar]
- MacBrayer EK, Milich R, Hundley M. Attributional biases in aggressive children and their mothers. J Abnorm Psychol. 2003;112:698–708. doi: 10.1037/0021-843X.112.4.598. [DOI] [PubMed] [Google Scholar]
- Matthews B, Norris F. When is believing ‘seeing’? Hostile attribution bias as a function of self-reported aggression. J Appl Soc Psychol. 2002;32:1–32. [Google Scholar]
- McCloskey MS, Noblett KL, Deffenbacher JL, Gollan JK, Coccaro EF. Cognitive-behavioral therapy for intermittent explosive disorder: a pilot randomized clinical trial. J Consult Clin Psychol. 2008;76(5):876–886. doi: 10.1037/0022-006X.76.5.876. [DOI] [PubMed] [Google Scholar]
- McCloskey MS, Phan KL, Angstadt A, Fettich KC, Keedy S, Coccaro EF. Amygdala hyperactivation to angry faces in intermittent explosive disorder. J Psychiatr Res. 2016;79:34–41. doi: 10.1016/j.jpsychires.2016.04.006. [DOI] [PubMed] [Google Scholar]
- Milich R, Dodge KA. Social information processing in child psychiatric populations. J Abnorm Child Psychol. 1984;12:471–490. doi: 10.1007/BF00910660. [DOI] [PubMed] [Google Scholar]
- Miller J, Lynam D. Reactive and proactive aggression: similarities and differences. Pers Indiv Diff. 2006;41:1469–1480. [Google Scholar]
- Orobio de Castro B, Veerman J, Koops W, Bosch J, Monshouwer H. Hostile attribution of intent and aggressive behavior: a meta-analysis. Child Dev. 2002;73(3):916–934. doi: 10.1111/1467-8624.00447. [DOI] [PubMed] [Google Scholar]
- Pettit GS, Lansford JE, Malone PS, Dodge KA, Bates JE. Domain specificity in relationship history, social-information processing, and violent behavior in early adulthood. J Pers Soc Psychol. 2010;98(2):190–200. doi: 10.1037/a0017991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfohl B, Blum N, Zimmerman M University of Iowa. Dept. of, P. Structured Interview for DSM-IV Personality Disorder. American Psychiatric Press; Washington D.C: 1997. [Google Scholar]
- Simon HA. The Sciences of the Artificial. MIT Press; Cambridge, MA: 1969. [Google Scholar]
- Singer MI, Miller DB, Guo S, Flannery DJ, Frierson T. Contributors to violent behavior among elementary and middle school children. Pediatrics. 2013;104:878–886. doi: 10.1542/peds.104.4.878. [DOI] [PubMed] [Google Scholar]
- Song LY, Singer MI, Anglin TM. Violence exposure and emotional trauma as contributors to adolescents' violent behaviors. Archives Pediatr Adolesc Med. 1998;152:531–536. doi: 10.1001/archpedi.152.6.531. [DOI] [PubMed] [Google Scholar]
- White SF, Marsh AA, Fowler KA, Schechter JC, Adalio C, Pope K, Blair RJ. Reduced amygdala response in youths with disruptive behavior disorders and psychopathic traits: decreased emotional response versus increased top-down attention to nonemotional features. Am J Psychiatr. 2012;169:750–758. doi: 10.1176/appi.ajp.2012.11081270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyer RS., Jr . Cognitive Organization and Change: an Information-processing Approach. Lawrence Erlbaum Associates; Potomac, MD: 1974. [Google Scholar]
- Zhang TY, Labonte B, Wen XL, Turecki G, Meaney MJ. Epigenetic mechanisms for the early environmental regulation of hippocampal glucocorticoid receptor gene expression in rodents and humans. Neuro-psychopharmacology. 2013;38:111–123. doi: 10.1038/npp.2012.149. [DOI] [PMC free article] [PubMed] [Google Scholar]