Abstract
Physicians have an important role addressing the obesity epidemic. Lack of adequate teaching to provide weight management counseling (WMC) is cited as a reason for limited treatment. National guidelines have not been translated into an evidence-supported, competency-based curriculum in medical schools. Weight Management Counseling in Medical Schools: A Randomized Controlled Trial (MSWeight) is designed to determine if a multi-modal theoretically-guided WMC educational intervention improves observed counseling skills and secondarily improve perceived skills and self-efficacy among medical students compared to traditional education (TE). Eight U.S. medical schools were pair-matched and randomized in a group randomized controlled trial to evaluate whether a multi-modal education (MME) intervention compared to traditional education (TE) improves observed WMC skills. The MME intervention includes innovative components in years 1–3: a structured web-course; a role play exercise, WebPatientEncounter, and an enhanced outpatient internal medicine or family medicine clerkship. This evidence-supported curriculum uses the 5As framework to guide treatment and incorporates patient-centered counseling to engage the patient. The primary outcome is a comparison of scores on an Objective Structured Clinical Examination (OSCE) WMC case among third year medical students. The secondary outcome compares changes in scores of medical students from their first to third year on an assessment of perceived WMC skills and self-efficacy.
MSWeight is the first RCT in medical schools to evaluate whether interventions integrated into the curriculum improve medical students’ WMC skills. If this educational approach for teaching WMC is effective, feasible and acceptable it can affect how medical schools integrate WMC teaching into their curriculum.
Keywords: Weight management counseling, 5As, patient-centered counseling, medical education, group randomized controlled trial, medical schools
1.0 INTRODUCTION
Obesity has reached epidemic proportions and is one of the most compelling health problems facing Americans. Slightly more than 70% of U.S. adults have overweight or obesity, [1] placing them at increased risk for diabetes, heart disease, and cancer [2]. National surveys demonstrate that only 20–40% of adult patients with obesity receive weight management counseling (WMC) from a physician [3–6]. This results in missed opportunities to engage patients in weight management, diet, and physical activity promotion, [3] ultimately increasing their risk of morbidity and premature mortality. Given that physicians can effectively assist patients with weight management, [7–15] the U.S. Preventive Services Task Force recommends that physicians “screen all adult patients for obesity and offer intensive counseling and behavioral interventions to promote weight loss for adults” [16].
Physicians, however, lack adequate education in WMC [6, 17, 18] and report low perception of their skills or self-efficacy regarding their ability to perform WMC [19, 20]. The 1985 report from the National Academy of Sciences recommends at least 25 – 30 hours of nutrition education in medical school [21]. A recent survey of U.S. medical schools found that the average required hours of nutrition were 20.4 in 2000 and 19.0 in 2012; [22, 23] however only about one-third of surveyed schools achieve the recommended minimum hours [22]. A larger gap exists for skills-based practice for WMC with only 2% of the schools in the noted survey reporting patient assessment and counseling [22].
The most prominent organization of medical schools, the Association of American Medical Colleges (AAMC), seeks to address the noted deficit by recommending that WMC be strongly emphasized within the medical school curriculum [24]. They have developed curriculum guidelines providing competencies and learning objectives related to the biologic, population health, and clinical training aspects of WMC. These guidelines [16, 25] have not been translated into an evidence-supported, competency-based curriculum [24, 26]. To help close the gap we have developed a WMC curriculum for counseling adults, “MSWeight” (Medical Students learning Weight management counseling skills). We are evaluating its efficacy compared to traditional medical education on students’ WMC skills and their perception of their skills in a group randomized controlled trial. This pair-matched RCT is similar in design to our prior study, MSQuit (Randomized Controlled Trial (RCT) for Smoking Cessation in 10 Medical Schools-5R01 CA136888) [27].
This research is the first of its kind to develop and evaluate the effect of a WMC medical school curriculum intervention on fostering WMC skills acquisition in a multi-site RCT. If efficacious, MSWeight can have an important public and clinical health impact by providing foundational education to enable physicians-in-training to help patients who have overweight or obesity achieve a healthier weight. This research is timely and critical for addressing the obesity epidemic.
2.0 METHODS
2.1 Study Design
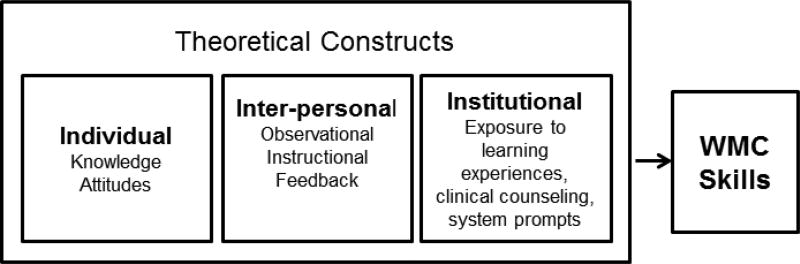
MSWeight is a multi-modal educational intervention (MME) guided by Social Cognitive Theory, [28] Gagne’s Conditions of Learning,[29] and Socio-Ecological Theory [30]. An eight-school pair-matched group RCT design is used to compare MME to traditional medical education (TE) for the primary and secondary outcomes. The primary outcome of observed WMC skills is measured by an Objective Structured Clinical Examination (OSCE), the standard method for observing and evaluating medical student skills at all U.S. medical schools [31]. WMC OSCE scores will be compared between MME and TE schools for the graduating class of 2020 measured during the students’ core clerkship rotation (either Family Medicine or out-patient Internal Medicine). The secondary outcome of student perceived WMC skills and self-efficacy in delivering WMC is measured by changes in scores for medical students from their first year to during their core clerkship rotation. In addition to our primary aim of comparing efficacy of MME to TE for teaching WMC, we will address the potential influence of individual, interpersonal and institutional factors on observed student WMC skills and student perceived WMC skills. The noted constructs are included in our three guiding theories [28, 29, 30] (see Figure 1). We also will evaluate the feasibility and acceptability of implementing the MME across medical schools. If the MME approach improves students’ WMC skills and is acceptable to students, faculty and school administration, then it can support integration of national recommendations for training future physicians in WMC.
Figure 1. Theoretical Constructs that Potentially Influence WMC Skills.
Theoretical constructs represent the constructs that are applicable to individual, interpersonal and institutional levels.
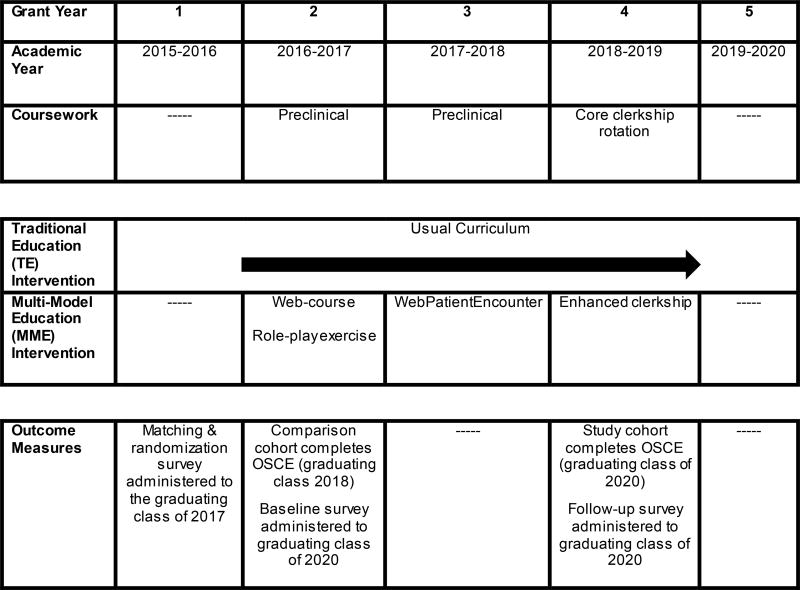
It employs a nested cross-sectional study design to compare OSCE scores between MME and TE schools. The MME curriculum developed and modeled from previous on-line tested instruction [32] includes: 1) an evidence-supported and competency-based web-course; 2) a role play exercise guided by a WMC OSCE-based checklist; 3) novel use of standardized WebPatientEncounter [33] technology to provide practice and structured feedback to students on their WMC skills; and 4) an enhanced Family Medicine or outpatient Internal Medicine clerkship that provides WMC skill building experiences. A web-based patient encounter is an innovative addition that was not used in the MSQuit intervention and was added to potentially increase the impact of the intervention on WMC skills. This combination of the web-course, role play exercise, WebPatientEncounter, and preceptor facilitated teaching during an enhanced clerkship provides repeated exposure to the WMC curriculum during the first three years of medical school. The curriculum is intended to provide a structured and reinforcing foundation for helping medical students build and practice WMC skills, and to build confidence in their skills and self-efficacy [28] (i.e. belief in their ability to perform WMC) for implementing WMC (see Figure 2 for the Study Timeline).
Figure 2. Study Timeline.
OSCE=objective structured clinical exam; Pre-clinical=medical student academic year 1and year 2; Core clerkship rotation=occurs after pre-clinical coursework is completed (2nd or 3rd year of medical school); RCT=randomized controlled trial; MME=multimodal education; TE=traditional education; CD=clerkship directors; SP=standardized patient.
To capture school pre-intervention OSCE scores, a comparison cohort of students (graduating class of 2018) at each school who are not part of the intervention will complete the OSCE (see Figure 2). The study cohort is comprised of students from the graduating class of 2020. MME students will have completed the enhanced clerkship activities during their core clerkship rotations. The study cohort (MME and TE) OSCEs will be administered after completion of the same pre-determined clerkship. To determine the impact of the intervention on our secondary outcomes, perceived WMC skills and self-efficacy for delivering WMC, students in the eight schools in the Class of 2020 will complete a 16 item suvey assessing their perceived WMC skills and an additional item assessing their WMC self-efficacy as first year students (i.e. “Baseline Survey”) and after their core clerkship rotation and following their WMC OSCE (“Follow-up Survey”). (See Table 1).
Table.1.
Study Measures -
| Year | 2015–2016 | 2016–2017 | 2018–2019 | |
|---|---|---|---|---|
| Objective Measure: OSCE |
------ | Comparison cohort completes the OSCE class of 2018 |
Study cohort completes the OSCE class of 2020 |
|
| Self-Report Measures: Student Surveys |
Matching and Randomization Survey administered to the class of 2017 |
Baseline Survey administered to the class of 2020 |
Follow Up Survey administered to the class of 2020 |
|
| WMC perceived skills | X | X | X | |
| Self-efficacy to deliver WMC | X | X | X | |
| Attitudes about PD-WMC | X | X | X | |
| Obesity Bias [34] | X | X | X | |
| Intention to Treat | ------ | X | X | |
| Perception of Impact on Patient Motivation | X | ------ | X | |
| Prior experiences in WMC | X | ------ | X | |
| Personal Health Habits | X | X | X | |
OSCE=Objective standardized clinical exam; WMC=weight management counseling; PD=physician delivered.
Evaluation of the feasibility and acceptability of implementing the MME intervention is measured through interviews with each MME school study PI or designee, participation rates (feasibility) and satisfaction scores (acceptability) for each intervention component.
2.2 Participants and Randomization
Eight medical schools are participating in the MSWeight RCT. Six of the eight schools previously participated in the NCI-funded trial, MSQuit [27]. The two remaining schools were recruited through networks with colleagues. Schools are from each U.S. region (e.g. North, South, West, Midwest) and met the following criteria at the time of recruitment: 1) includes a Family Medicine or out-patient Internal Medicine clerkship; and 2) is willing and able to offer a WMC OSCE for students following the completion of a core clerkship, the Family or out-patient Internal Medicine Clerkship rotation, or as part of a cumulative OSCE. The University of Massachusetts Medical School coordinates the study. MSWeight was submitted and determined to be exempt at the University of Massachusetts Medical School and by each participating medical school’s Institutional Review Board.
Prior to randomization, the eight schools were surveyed about the presence of curricula and number of hours addressing behavior change and WMC in medical school years 1 through 3. In addition, a Matching and Randomization Survey was administered to the Class of 2017 for both TE and MME schools, during their core clerkship rotations (See Table 1 for measures and when they were administered).
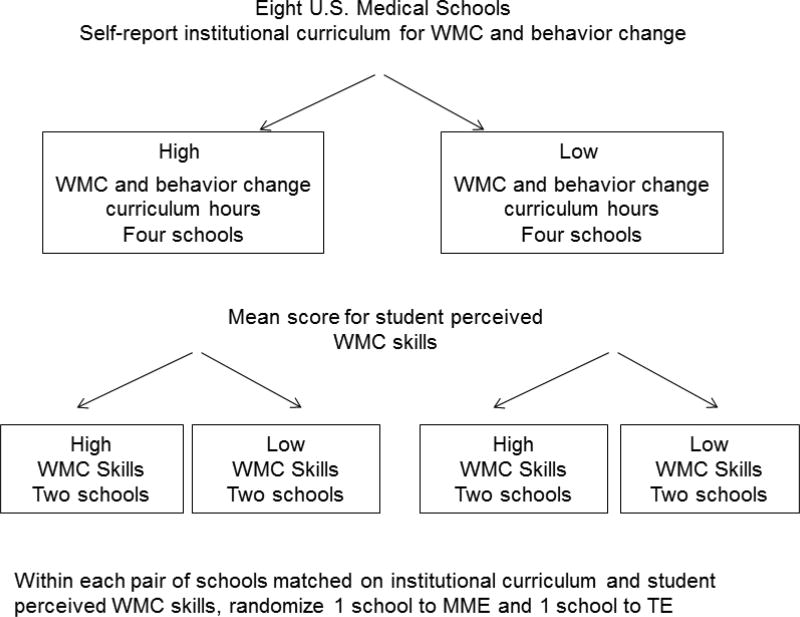
The survey was designed to include questions built on content and format used in previous research [35]. Measures include student demographics, attitudes, and questions to assess perceived skills for WMC (16 items; responses 1=not at all skilled, to 5=very skilled) and self-efficacy for delivering WMC (1 item; responses 1=strongly disagree to 4=strongly agree). The survey was pilot tested for ease of understanding with medical students from the University of Massachusetts Medical School and site PIs. Results from the pilot test were used to refine the final self-administered survey. Schools were stratified into high (four schools) or low (four schools) WMC and behavior change curriculum hours based upon reports from the school faculty or PI. Within each institutional curriculum stratum, the four schools were then rank ordered based on school mean score for student perceived WMC skills from the Matching and Randomization Survey. This resulted in four strata with two schools each. These pair matched schools were randomly assigned to either MME or TE. Randomization was accomplished using a random number generator (See Figure 3).
Figure 3. Randomization Schema.
WMC = weight management counseling
MME = multi-modal education
TE = traditional education
Following randomization first year students from the study cohort (class of 2020 students) at the eight schools were informed that their medical school was participating in a study to test the effectiveness of different teaching methods to facilitate medical student skill development in WMC. By completing the survey the student is agreeing to take part in the research study. Each medical school PI obtained the current roster of the class of 2020 from its Office of Student Affairs or the registrar. For sites with multiple campuses the school selected the medical students at the campus who would be able to complete the study OSCE and take part in the intervention if randomized to the MME. Altogether, from the eight medical schools combined, 1307 medical students in the class of 2020 will be eligible to participate in the study.
2.3 Medical School Education Arms
2.3.1 Traditional Education (TE) Comparison Arm
The TE arm represents “usual care” and includes the current content and mode for WMC teaching weight management among schools randomized to TE. Modes of learning mainly include WMC lectures interspersed among basic science and behavior change classes, with some use of small group discussions or communication skill-building exercises and clinical experiences for health behaviors.
2.3.2 Multi-Modal Education (MME) Intervention Arm
The MME intervention targets student individual factors (WMC knowledge, obesity bias, WMC observed skills, and WMC perceived skills and self-efficacy), interpersonal factors between faculty and student (modeling and provision of WMC feedback), and institutional factors (exposure to WMC curriculum, including clinical experiences) to support WMC skill building for medical students. The MME intervention is modeled on the protocol we have used for diet, alcohol, and smoking behavior change interventions, using patient-centered counseling integrated into the 5As framework (Ask, Advise, Assess, Assist, and Arrange) [36–38] as well as incorporating content from the obesity guidelines noted in Section 2.3.2 [25]. The MME is designed to give students repeated and sequential exposure to WMC curricula over the course of the first three years of medical school.
2.3.2.1 Web-Course “MSWeight: Building Weight Management Counseling Skills”
Our team of experts in behavioral health, medical practice and nutrition reviewed existing online courses such as New Lifestyle [39] and Nutrition in Medicine [40] for teaching WMC. Other selected resources include the American Heart Association/American College of Cardiology/The Obesity Society Clinical Guidelines for the Management of Overweight and Obesity in Adults, [41] Center for Disease Control and Prevention, [1] American College of Sports Medicine’s Exercise is Medicine®, [42] the U.S. Department of Health and Human Services’ Physical Activity Guidelines, [43] the American Heart Association’s Fitness Basics, [44] and the 2015–2020 Dietary Guidelines for Americans [45]. Using these resources as a guide the team selected key goals for the web-based didactic component of the intervention. The web-course includes 14 modules that range from epidemiology of overweight/obesity and the role of the physician in WMC to providing tools that physicians can use to partner with patients to make dietary and physical activity behavior changes. Since obesity bias is prevalent in society and can be present during a medical student-physician-patient interaction [34], the web-course incorporated content to raise awareness about obesity bias and increase knowledge for effectively counseling patients with obesity.
To facilitate the web-course completion, the course is self-paced. Each module is designed to be completed by students in approximately 15 minutes with an overall time commitment of 4 hours. Medical education deans and course directors agreed to include the course in the first year curriculum and to record course completion among their students. At the end of the web-course, students will complete a short quiz. Upon completion of the quiz students will receive a certificate of completion. The web-course is promoted as a prerequisite for the role play exercise.
2.3.2.2 Role Play Exercise
The goal of the role play exercise is to provide students with hands-on practice conducting WMC. The one-hour session is facilitated by school faculty instructors and includes a brief video demonstration of a physician-patient encounter for WMC that incorporates the 5As framework followed by a brief discussion of the video and WMC challenges such as initiating the conversation about weight management and goal setting. Subsequent to the discussion, students break into dyads and practice two physician-patient encounters.
2.3.2.3 WebPatientEncounter
The WebPatientEncounter [33] is an innovative addition to the intervention that provides students with WMC skills practice during the second year. In this intervention, students interact with a standardized patient (SP) with obesity in a formative WebPatientEncounter, using a video-conferencing system developed and administered by investigators at Drexel University College of Medicine - in alignment with our OSCE checklist. It provides a two-way video that can be recorded and stored. After a 15-minute encounter the SPs (hired and trained by Drexel University) guide the student through our structured OSCE WMC behavior checklist, noting behaviors and communication skills the student successfully implemented and those the student could have employed for a more effective encounter. The SP provides feedback by playing back relevant parts of the encounter to show the student what they did. Students can access their interview for continued reflection. Total time with the SP is 40 minutes; staff at Drexel University along with staff at each MME institution schedule student/SP meetings.
2.3.2.4 Enhanced Clerkship and Faculty Development
Clinical preceptors are in the position to teach, model, provide practice opportunities, give constructive feedback to students during the clerkship experience, and can have a positive impact on students’ clinical skills development [46, 47]. In MSQuit, we involved academic detailers to conduct the faculty development. Such educational outreach has demonstrated effectiveness for teaching physicians various intervention skills [36, 38, 48–52]. However, the educational level, experience, and skill level of the academic detailers varies between schools. We were concerned that academic detailers [27, 52] are not on the front line with preceptors or medical students and may not adequately teach them WMC. For the current study, the clerkship director (CD) delivers the intervention because the CD is on the front line with faculty and students. Clinical faculty also play a major role in student education, precepting students during their core clerkship rotations. For this reason the clerkship directors in this study work with the UMass team to develop preceptor faculty development materials, designing the educational session to be brief, 30 minutes, to enhance preceptor engagement.
Clerkship directors facilitate the group educational session for the preceptors. Preceptors are strongly encouraged to: (1) conduct WMC with their patients for students to observe, as modeling is an effective training technique, [53] and (2) actively observe students with patients and give critical feedback related to their WMC skills. The clerkship directors' educational program for preceptors includes principles of patient engagement and use of the 5As and patient-centered counseling for WMC. For preceptors who are not on-site, a recorded session is sent out electronically. Preceptors and medical students receive pocket guides to reinforce intervention concepts. Through use of a checklist, preceptors and medical students verify that the medical student was observed and given feedback on their WMC skills. The checklist is forwarded to the study coordinator at the site. Materials are provided in multiple formats including one easy to access by smartphone.
2.4 Intervention Implementation and Fidelity
To maximize implementation of the MME intervention, site PIs are encouraged to tailor implementation of the intervention to their institution’s unique characteristics and needs within their organizational and educational context. While the curriculum content is standardized across schools, each school has flexibility to choose the specific course in which the educational intervention is to be implemented and when to implement it (e.g. during the Doctoring and Clinical Skills course). Schools are provided with guidelines for implementation timing so that students across schools receive the intervention within a common and specific timeframe. These guidelines are as follows: 1) the web-course is implemented when medical students in our intervention study cohort are in their first year; 2) the role play is implemented after the web-course during the study cohort students are in their first year of medical school; 3) the WebPatientEncounter takes place during the second year after the role play exercise and prior to the clerkship; and 4) the clerkship director/preceptor teaching experience takes place prior to the study cohort entering the outpatient internal or family medicine clerkship rotation.
To maximize intervention fidelity specific steps are implemented. First, we ensure that all MME site PIs and key staff for a particular intervention have a role in its refinement. They or their designee (e.g. whoever implemented the intervention component) are therefore familiar with the intervention content, goals, and objectives. Next, our team made sure the content and structure of the intervention components (e.g. role play exercise, enhanced clerkship) were standardized and semi-guided with written instructions and examples of discussion points provided for faculty instructors. The web-course is directly implemented by the UMass team remotely as it requires student login and registration to ensure participation. The UMass team facilitates standardized orientations for each intervention component. Finally, conference calls with MME faculty are held monthly and individually as needed to address challenges in real time and to enhance fidelity to program implementation.
3.0 MEASURES
3.1 Primary Outcome: Observed Weight Management Counseling Skill
OSCEs for assessing clinical skills consist of a series of stations (cases) intended to simulate a component of a clinical encounter [31]. This rigorous assessment was used to evaluate medical students’ tobacco dependence treatment skills in our prior trial [54] and will be used in the MSWeight trial. As noted in Section 2.1, for the primary outcome we will compare MME school and TE school scores on the WMC OSCE using a nested cross-sectional design. As with MSQuit [27] the OSCE will be used to objectively measure skills among medical students who have completed their core clerkship.
Student scores on the WMC OSCE are determined by an OSCE checklist consisting of 23 items assessing WMC skills integrating 5As behaviors (15 items) and patient-centered counseling skills (8 items). The WMC skill items integrated into the 5As framework were based on the 2013 Guideline for the Management of Overweight and Obesity in Adults published by The Obesity Society and American College of Cardiology/American Heart Association [25]. The communication skill items were developed based on patient-centered counseling models and guidelines. Examples of 5As items include: “Asked permission to discuss diet and physical activity history and current behaviors” (Ask); “Advised that weight loss is recommended based on the patient’s personal health information (e.g. BMI and risk factors)” (Advise); “Assessed the patient’s level of readiness to make lifestyle changes to achieve weight loss” (Assess); “Assisted the patient by discussing behavior change strategies that will help achieve their goals” (Assist); and “Recommended or referred the patient to weight management resources in the clinic or in the community and scheduled a follow up appointment” (Arrange follow-up). An example of communication skills items include “Used a majority of open-ended questions during the encounter”. The OSCE checklist was refined based on application of the checklist to videotaped encounters and reviewed and approved by behavioral health and weight management experts, practicing clinicians and medical students prior to finalizing.
The 8 Patient-Centered items are scored 0–2 (max = 16) and the 15 5A items are scored Yes/No (max = 15), for a maximum score of 31 for each OSCE. The final scores will be computed as total points earned. One coder will score each OSCE tape. To check for consistency a 'gold standard' coder and supervisor will code 10% of the completed checklist for each coder. This verification process will be conducted on an ongoing basis to detect and correct any discrepancies. This method is consistent with scoring in the MSQuit where consistency was very high [54]. Although students are not expected to complete all 23 checklist behaviors, higher overall scores may be indicative of better WMC performance. Similar to MSQuit, we anticipate that the 8 patient-centered items also will be used to create a separate outcome from the total OSCE score indicating number of completed behaviors.
All WMC OSCEs are videotaped and blinded. Trained coders will score them. The coders will not be members of the research team and will be blinded to school and its intervention assignment (MME or TE). Coders will complete a series of trainings and follow-up booster trainings led by our research team and will have several opportunities to practice coding WMC OSCE performances from a pool of practice UMass students.
3.1.1 WMC OSCE Case Refinement and Checklist Development
We adapted a WMC-specific OSCE case that has been used previously as a teaching tool within a medical school curriculum. The OSCE case was reviewed and refined with input from each school’s site PI, clinical skills course director, and SP trainer. The OSCE checklist was developed using the WMC perceived skills and patient-centered counseling items from the baseline survey, and refined through a process of co-investigators, clinicians, and weight management experts reviewing four SP WMC OSCE videotapes and coding the tapes using the checklist. Once the checklist was revised and refined it was reviewed by the PI and the investigative team, practicing physicians, and medical students. The checklist was finalized when consensus was reached.
3.1.2 Standardized Patient Training
As in MSQuit [27] our research team trained each school’s SP trainer in the details of the case through a series of half-day trainings. Trainers were then responsible to train the SPs at their school. The number of SPs at each school is dependent upon the number of concurrent sessions scheduled. An expert SP trainer reviewed a training video for each SP and the school’s trainer coached the SP with any corrections required (see ref [55] for discussion of this training).
3.2 Secondary Outcomes: Self-Reported WMC Skill and Self-Efficacy
For our secondary outcomes, student perceived WMC skills and self-efficacy, students in both MME and TE schools complete surveys at baseline (“Baseline Survey”) and follow-up (“Follow-up Survey”, post intervention). The baseline and follow-up surveys include 15 items to assess perceived skills in WMC using patient-centered counseling and integrating the 5As framework. Students are asked to rate their skill level in carrying out each of the WMC steps with patients (1=Not at all skilled to 5=Very skilled). Examples of items are similar to the OSCE items in the primary outcome (section 3.1). The total score is the average among WMC skills using patient-centered counseling and integrating the 5As framework. The secondary outcome of student perceived WMC skills is calculated as the average of the ratings across these items. A separate, single item global self-efficacy question was included in the baseline and follow-up survey: “I feel confident in providing weight management counseling for my patients with overweight and obesity”, (1=Strongly disagree to 5=Strongly agree) to assess self-efficacy in conducting WMC with patients.
3.3 Other Outcomes of Interest: Proposed Mediators
Several intrapersonal, interpersonal, and organizational variables are hypothesized as mediators and are measured for students in MME and TE schools through the matching and randomization and the follow-up surveys. Intrapersonal mediators include perceived WMC skills and self-efficacy (as described above) and include the frequency of instructional and observational experiences in WMC received by students. In the noted surveys the core clerkship medical students are asked the number of times that they have been instructed how to do WMC. Students also report how frequently they observed a physician or preceptor perform WMC 5As behaviors with a patient with obesity or overweight. Finally, organizational mediators are assessed in the baseline and follow-up surveys, including counseling prompts, reminders, or clinic/system changes.
3.4 Process Evaluations: Feasibility and Acceptability of the MME
Feasibility and acceptability data will be gathered on MME conference calls, debriefing with PIs and other key personnel about implementation of each component, and through student and preceptor evaluations. The research team at each medical school document feasibility, that is, participation rates for student intervention components and faculty development. Acceptability data are collected via satisfaction surveys students complete after each MME component. Finally, we will determine curriculum and institutional changes at both TE and MME schools that may affect student training in WMC. In order to capture institutional curricula changes over time, we will assess school curricula on nutrition, WMC, and behavior change after completion of the intervention using the same approach that we used for matching and randomization prior to intervention initiation.
3.5 Sample Size and Power Calculation
Our primary outcome is WMC skills measured by the study cohort post-intervention OSCE score. Adjusting for school-specific mean baseline OSCE score, the detectable MME-TE mean difference is given by Δ = [2(σm2 ϴm + mσg2 ϴg) (tα/2 + tβ)2 / mg]1/2 where σm2 and σg2 indicate school and intervention group components of total variance of OSCE score=σy2, respectively; ϴm and ϴg reflect reductions in those variance components from covariate adjustment; m=number of students per school and g=number of schools per condition; and tc indicates a critical value with right tail probability c from a t-distribution with degrees of freedom=2(g−1) [55, 56]. To be conservative, we take ϴm=1. ϴg = 1 – R2y.x where R2y.x=proportion of outcome variance explained by baseline school mean, estimated as the square of the over-time correlation. Also, σg2 = σy2 × intra-class (intra-school) correlation (ICC) and σm2 =σy2 × (1−ICC). Using values from our prior randomized clinical trial of MME versus TE for tobacco counseling as a guide, [57] the observed over-time correlation in school means = 0.87 and ICC=0.12. Standardizing the outcome (σy2=1), and taking m=125, two-sided hypothesis testing with 0.05 Type I error rate, 80% power, and g=4 schools per condition, the projected detectable MME-TE difference in mean OSCE score=0.42 standard deviations; this difference is in line with the prior study’s observed between-group difference of 0.35 standard deviations, and we anticipate a larger difference in MSWeight given the more intensive intervention. Power for the secondary outcome, perceived WMC skills, will be higher than for the primary outcome given the anticipated positive correlation over time for both individual students and schools. The ICC indicates within-school correlation of OSCE scores from students in the same school. We have used results from MSQuit [57] as a guide for anticipated magnitude of the intervention effect given that the components of the intervention are similar in both studies.
3.6 Data Management and Data Analysis Plan
3.6.1 Data management, confidentiality, and blinding
Each eligible student is assigned an ID by school personnel which is used in all study data files; no study investigators outside the school have access to student identifying information that can be linked to their ID. All study data are entered into REDCap (Research Electronic Data Capture), a secure web-based application for research studies, either directly by students (survey data) or by study personnel. OSCE scoring will be conducted by coders blinded to school and randomization arm.
3.6.2 Data analysis plan
Analyses of the primary outcome will compare post-intervention MME and TE schools’ WMC OSCE scores, adjusting for pre-intervention scores. To account for the nested cross-sectional design, with students measured at two time points in the same schools – pre-intervention = Comparison Cohort students (class of 2018), post-intervention = Study Cohort students (class of 2020)– we will use a two-stage mixed model analysis of covariance (ANCOVA) [55, 56]. In the first stage, 16 (8 schools × 2 time points) mean scores will be estimated from an ANCOVA for student-level WMC OSCE scores as a function of school, time point, and their interaction. In the second stage, the eight post-intervention school-mean scores will be regressed on intervention assignment and the corresponding pre-intervention school mean. This approach adjusts for any MME-TE differences in baseline school mean WMC OSCE scores while accounting for within-school correlation. The secondary outcome, perceived WMC skills, will be measured twice in the same study cohort students, both pre- and post-intervention, allowing the assessment of change within individual students. Depending on the distribution of this outcome, MME-TE differences post-intervention will be estimated using linear mixed models (continuous) or random effects logistic regression (categorical), adjusting for the student’s own pre-intervention report and treating school as a random effect to account for within-school clustering. The latter models will adjust for relevant student-level covariates, such as gender, age, and planned specialty.
3.7 Ethics and Dissemination
Site PIs obtained school approval to participate in the research (both MME and TE schools) and to incorporate WMC MME intervention components into the existing medical student curriculum (MME schools only) well in advance of project implementation. All surveys, OSCE scores, and MME evaluation component data will be de-identified before being given to the UMass Coordinating Center research team, who will manage databases and analyses.
All IRBs noted that completing surveys was voluntary. Three of the eight IRBs required a consent information sheet, not requiring documentation of written consent. One IRB required a consent information sheet noting that participation in the intervention was voluntary. Two of the three medical schools included language about releasing their de-identified videotaped OSCE to the research team noting that the research team would code the OSCE. Data sharing and the timely release of sharing the final research data are essential. The dissemination plan includes publications, presentations at and distribution to organizations to which our project members currently belong. We will use NCI’s Cancer Control Planet that we have used previously for distribution of all project materials in other projects led by current investigators. The plan includes sharing the use of research tools, such as project surveys and OSCEs, curricula materials such as web-based training and enhanced clerkship materials, and results from surveys collected in multiple years of the study. Our findings will be highly relevant to individuals in medical education and obesity behavior change fields.
4.0 DISCUSSION
Guidelines for the treatment of obesity recommend intensive behavioral counseling [16, 25]. The US Preventive Services Task Force recommends that physicians screen and offer intensive behavioral counseling to patients with obesity; [16] and the Centers for Medicare and Medicaid Services (CMS) approved covering intensive behavioral counseling by primary care physicians using the 5As model [58]. Although research is limited, WMC delivered by a variety of trained interventionists in the primary care setting is recommended and is consistently associated with patient weight loss [59–61]. However, WMC training is limited and not standardized across medical schools [6, 22, 26]. Learning is optimal when knowledge is acquired and experience occurs early, skills are reinforced consistently, and teaching is integrated into all aspects of a curriculum [29, 62–67]. Therefore, early exposure to WMC through didactic sessions, skill building exercises, and preceptor modeling, observation, and opportunities to practice WMC with patients and receive feedback from preceptors has great potential to benefit medical students. Additionally, the opportunity to methodically learn behavioral skills such as WMC may be most beneficial when trainees can observe, be observed, and receive immediate critical feedback from preceptors during medical school.
The MSWeight study is the first group randomized controlled trial that seeks to establish whether a MME intervention compared to TE methods will influence medical student WMC skills and self-efficacy. It has many strengths in design and outcome implications. The MME intervention incorporates components of a known effective web-course [39] and the role play exercise. It also includes the novel use of the WebPatientEncounter [33] and methods to train clerkship directors and preceptors to provide instruction in WMC. The MME intervention is grounded in learning theory, implemented early in the medical school curriculum, and integrated throughout a student’s medical school experience. Finally, because the MME intervention was developed with the goal of possible and eventual national medical school dissemination, the curriculum was refined through input from medical students, medical school administrators, medical faculty, education specialists and WMC specialists. In addition the MME was designed to be delivered in a standardized manner yet allow for flexibility to tailor the MME components to a school’s specific curriculum.
One other notable strength of this research is its use of scores from observed WMC OSCEs for its primary outcome. This rigorous method of evaluation reduces potential student and school-level biases as independent and blinded coders code the OSCE videotapes in the current study in order to objectively evaluate WMC skills. Prior research has shown that medical students evaluate their experience positively with health behavior change trained SPs, [68] and that SPs are trained in a variety of health behavior change cases. However, little research, if any, has objectively used a weight management-specific case and OSCE scores to measure intervention impact on student WMC skills. If feasible to implement, our OSCE WMC case may be used for additional training purposes or could be used for required undergraduate medical student standardized evaluation (e.g. Clinical Skills Exam (CSE) of USMLE Step 2) [69].
Potential limitations of the current study include the need for flexibility in implementation given the challenges associated with implementing a multi-modal intervention across multiple medical schools with varying school resources, institutional policies, prior WMC curricula, and community obesity rates. Through our process evaluation we will be able to better understand some of the contextual factors affecting implementation. Real world medical education is changing at a very fast pace, continuously allowing for more flexibility and options for students and our pragmatic approach reflects these trends. Although we have matched for school-level differences in student perceived WMC skills, differences in the ability to feasibly implement the study across medical schools exist. For example, school-related policies that allow faculty to make curriculum components graded or required versus optional differ among institutions and potentially can affect student participation rates and study outcomes. Schools also may differ in the number of faculty who have interest or expertise in WMC which also may affect school-level outcomes.
In summary, a WMC intervention that can effectively help physicians-in-training, their clerkship directors and their preceptors learn WMC skills could make an important contribution to medical education, clinical medicine and population health.
Acknowledgments
We acknowledge all school site PIs, research coordinators, evaluators, directors of standardized patients, medical directors of clinical education and simulation center, research assistants, support staff, participating medical students, course directors, clerkship directors, preceptors and our weight bias consultant who have and will implement and participate in the study.
Funding: This work is supported by the National Institutes of Health, National Cancer Institute, 5R01CA194787.
Role of the Funding Source: The funding source has had no involvement in the conduct of the research or preparation of the article.
Abbreviations/Definitions
- 5As
Ask, Assess, Advise, Assist, Arrange
- MME
Multi-modal education
- TE
Traditional education
- OSCE
Objective Structured Clinical Examination
- Pre-clinical coursework
occurs prior to core clerkship rotations and timing varies by school
- Core clerkship rotation
occurs after pre-clinical coursework is completed (2nd or 3rd year of medical school)
- SP
Standardized patient
- WMC
Weight Management Counseling
- RCT
Randomized Controlled Trial
- MSQuit Medical Students
Medical Students Helping Patients Quit Tobacco
- MSWeight
Medical Students Learning Weight Management Counseling Skills
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competing interests
The authors declare that they have no competing interests with this study.
Author Contributions
JO conceived the study and developed the protocol with RH, LC and AG. JO led the writing of the first draft of the paper, with contributions from KA, LC, MB, SC, LP, BO, DJ and AG. All authors contributed to editing and redrafting, and have read and approved the manuscript for submission.
References
- 1.Centers for Disease Control and Prevention. Division of Nutrition PA, and Obesity, National Center for Chronic Disease Prevention and Health Promotion. [updated September 1, 2016];Overweight & Obesity, Data & Statistics. 2016 cited 2016 December 14. Available from: https://www.cdc.gov/obesity/data/adult.html.
- 2.National Institutes of Health. The practical guide. In: Initiative NOE, editor. Identification, evaluation, and treatment of overweight and obesity in adults. Washington, DC: 2000. [Google Scholar]
- 3.Galuska DA, Will JC, Serdula MK, Ford ES. Are health care professionals advising obese patients to lose weight? Journal of the American Medical Association. 1999 Oct 27;282(16):1576–1578. doi: 10.1001/jama.282.16.1576. [DOI] [PubMed] [Google Scholar]
- 4.Ahmed NU, Delgado M, Saxena A. Trends and disparities in the prevalence of physicians' counseling on diet and nutrition among the U.S. adult population, 2000–2011. Preventive Medicine. 2016;89:70–75. doi: 10.1016/j.ypmed.2016.05.014. [DOI] [PubMed] [Google Scholar]
- 5.Abid A, Galuska D, Khan LK, Gillespie C, Ford ES, Serdula MK. Are healthcare professionals advising obese patients to lose weight? A trend analysis. MedGenMed. 2005 Oct 12;7(4):10. Epub 2006/04/15. [PubMed] [Google Scholar]
- 6.Vitolins MZ, Crandall S, Miller D, Ip E, Marion G, Spangler JG. Obesity Educational Interventions in U.S. Medical Schools: A systematic Review and Identified Gaps. Teaching and Learning in Medicine: An International Journal. 2012;24(3):267–272. doi: 10.1080/10401334.2012.692286. Epub 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ockene IS, Hebert JR, Ockene JK, Saperia GM, Stanek E, Nicolosi RJ, Merriam PA, Hurley TG. Effect of physician-delivered nutrition counseling training and an office-support program on saturated fat intake, weight, and serum lipid measurements in a hyperlipidemic population: Worcester Area Trial for Counseling in Hyperlipidemia (WATCH) Arch Intern Med. 1999 Apr 12;159(7):725–731. doi: 10.1001/archinte.159.7.725. [DOI] [PubMed] [Google Scholar]
- 8.U.S. Preventive Services Task Force. Screening for obesity in adults: recommendations and rationale. Ann Intern Med. 2003 Dec 2;139(11):930–932. doi: 10.7326/0003-4819-139-11-200312020-00012. [DOI] [PubMed] [Google Scholar]
- 9.Jay M, Gillespie C, Schlair S, Kalet A. Physicians' use of 5As in counseling obese patients: is the quality of counseling associated with patients' motivation and intention to lose weight? BMC Health Serv Res. 2010;10:159. doi: 10.1186/1472-6963-10-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tsai AG, Wadden TA. Treatment of obesity in primary care practice in the United States: a systematic review. J Gen Intern Med. 2009 Sep;24(9):1073–1079. doi: 10.1007/s11606-009-1042-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ockene IS, Hebert JR, Ockene JK, Merriam PA, Hurley TG, Saperia GM. Effect of training and a structured office practice on physician-delivered nutrition counseling: the Worcester-Area Trial for Counseling in Hyperlipidemia (WATCH) Am. J. Prev. Med. 1996 Jul-Aug;12(4):252–258. [PubMed] [Google Scholar]
- 12.Wadden TA, Volger S, Sarwer DB, Vetter ML, Tsai AG, Berkowitz RI, Kumanyika S, Schmitz KH, Diewald LK, Barg R, Chittams J, Moore RH. A two-year randomized trial of obesity treatment in primary care practice. N Engl J Med. 2011 Nov 24;365(21):1969–1979. doi: 10.1056/NEJMoa1109220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haas WC, Moore JB, Kaplan M, Lazorick S. Outcomes from a medical weight loss program: primary care clinics versus weight loss clinics. Am J Med. 2012 Jun;125(6):603, e607–611. doi: 10.1016/j.amjmed.2011.07.039. [DOI] [PubMed] [Google Scholar]
- 14.Tsai AG, Wadden TA, Rogers MA, Day SC, Moore RH, Islam BJ. A primary care intervention for weight loss: results of a randomized controlled pilot study. Obesity (Silver Spring) 2010 Aug;18(8):1614–1618. doi: 10.1038/oby.2009.457. [DOI] [PubMed] [Google Scholar]
- 15.Rose SA, Poynter PS, Anderson JW, Noar SM, Conigliaro J. Physician weight loss advice and patient weight loss behavior change: a literature review and meta-analysis of survey data. Int J Obes (Lond) 2013 Jan;37(1):118–128. doi: 10.1038/ijo.2012.24. [DOI] [PubMed] [Google Scholar]
- 16.U.S. Preventive Services Task Force. Screening for and Management of Obesity in Adults: U.S. Preventive Services Task Force Recommendation Statement. 2012 Jun AHRQ Publication No. 11-05159-EF-2. [Google Scholar]
- 17.Block JP, DeSalvo KB, Fisher WP. Are physicians equipped to address the obesity epidemic? Knowledge and attitudes of internal medicine residents. Prev Med. 2003 Jun;36(6):669–675. doi: 10.1016/s0091-7435(03)00055-0. [DOI] [PubMed] [Google Scholar]
- 18.Forman-Hoffman V, Little A, Wahls T. Barriers to obesity management: a pilot study of primary care clinicians. BMC Fam Pract. 2006;7:35. doi: 10.1186/1471-2296-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kristeller JL, Hoerr RA. Physician attitudes toward managing obesity: differences among six specialty groups. Prev Med. 1997 Jul-Aug;26(4):542–549. doi: 10.1006/pmed.1997.0171. [DOI] [PubMed] [Google Scholar]
- 20.Davis NJ, Shishodia H, Taqui B, Dumfeh C, Wylie-Rosett J. Resident physician attitudes and competence about obesity treatment: need for improved education. Med Educ Online. 2008;13:5. doi: 10.3885/meo.2008.Res00257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Research Council Committee on Nutrition in Medical Education. Nutrition Education in U.S. Medical Schools. Washington, DC.: National Academies Press (US). Copyright (c) National Academy of Sciences; 1985. [Google Scholar]
- 22.Adams KM, Butsch WS, Kohlmeier M. The State of Nutrition Education at US Medical Schools. Journal of Biomedical Education. 2015:7. doi: 10.1155/2015/357627. Epub 01/11/2015. [DOI] [Google Scholar]
- 23.Adams KM, Kohlmeier M, Zeisel SH. Nutrition education in U.S. medical schools: latest update of a national survey. Acad Med. 2010 Sep;85(9):1537–1542. doi: 10.1097/ACM.0b013e3181eab71b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Association of American Medical Colleges (AAMC) Report VIII Contemporary Issues in Medicine: The Prevention and Treatment of Overweight and Obesity; Medical School Objectives Project. Washington, DC: Association of American Medical Colleges (AAMC); 2007. Aug, Report No.: VIII. [Google Scholar]
- 25.Jensen MD, Ryan DH, Apovian CM, Loria CM, Ard JD, Millen BE, Comuzzie AG, Nonas CA, Donato KA, Pi-Sunyer FX, Hu FB, Stevens J, Hubbard VS, Stevens VJ, Jakicic JM, Wadden TA, Kushner RF, Wolfe BM, Yanovski SZ. AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2013 Nov 7; doi: 10.1016/j.jacc.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 26.Chisholm A, Hart J, Mann KV, Harkness E, Peters S. Preparing medical students to facilitate lifestyle changes with obese patients: a systematic review of the literature. Acad Med. 2012 Jul;87(7):912–923. doi: 10.1097/ACM.0b013e3182580648. [DOI] [PubMed] [Google Scholar]
- 27.Hayes RB, Geller A, Churchill L, Jolicoeur D, Murray DM, Shoben A, David SP, Adams M, Okuyemi K, Fauver R, Gross R, Leone F, Xiao R, Waugh J, Crawford S, Ockene JK. Teaching tobacco dependence treatment and counseling skills during medical school: Rationale and design of the Medical Students helping patients Quit tobacco (MSQuit) group randomized controlled trial. Contemp Clin Trials. 2014 Mar;37(2):284–293. doi: 10.1016/j.cct.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice-Hall; 1977. [Google Scholar]
- 29.Gagne RM. The conditions of learning. 4. New York: Holt, Rinehart & Winston; 1985. [Google Scholar]
- 30.Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot. 1996;10:282–298. doi: 10.4278/0890-1171-10.4.282. [DOI] [PubMed] [Google Scholar]
- 31.Mazor K, Ockene J, Rogers H, Carlin M, Quirk M. The Relationship between Checklist Scores on a Communication OSCE and Analogue Patients’ Perceptions of Communication. Advances in Health Sciences Education. 2005;10:37–51. doi: 10.1007/s10459-004-1790-2. [DOI] [PubMed] [Google Scholar]
- 32.Geller AC, Hayes RB, Leone F, Churchill LC, Leung K, Reed G, Jolicoeur D, Okuliar C, Adams M, Murray DM, Liu Q, Waugh J, David S, Ockene JK. Tobacco dependence treatment teaching by medical school clerkship preceptors: survey responses from more than 1,000 US medical students. Prev Med. 2013 Aug;57(2):81–86. doi: 10.1016/j.ypmed.2013.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Drexel University College of Medicine. WebPatientEncounter. [updated November 12, 2014];2014 cited 2017 February 14. Available from: https://webcampus.drexelmed.edu/webosce/
- 34.Ip EH, Marshall S, Vitolins M, Crandall SJ, Davis S, Miller D, Kronner D, Vaden K, Spangler J. Measuring medical student attitudes and beliefs regarding patients who are obese. Acad Med. 2013 Feb;88(2):282–289. doi: 10.1097/ACM.0b013e31827c028d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Geller AC, Brooks DR, Powers CA, Brooks KR, Rigotti NA, Bognar B, McIntosh S, Zapka J. Tobacco cessation and prevention practices reported by second and fourth year students as US medical schools. J Gen Intern Med. 2008;23(7):1071–1076. doi: 10.1007/s11606-008-0526-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ockene JK, Ockene IS, Quirk ME, Hebert JR, Saperia GM, Luippold RS, Merriam PA, Ellis S. Physician training for patient-centered nutrition counseling in a lipid intervention trial. Prev Med. 1995;24:563–570. doi: 10.1006/pmed.1995.1090. [DOI] [PubMed] [Google Scholar]
- 37.Ockene JK, Wheeler EV, Adams A, Hurley TG, Hebert J. Provider training for patient-centered alcohol counseling in a primary care setting. Arch Intern Med. 1997;157:2334–2341. [PubMed] [Google Scholar]
- 38.Ockene JK, Quirk M, Goldberg RJ, Kristeller J, Donnelly G, Kalan KL, Gould B, Greene H, Harrison-Atlas R, Pease J, Pickens S, Williams J. A residents' training program for the development of smoking intervention skills. Arch Int Med. 1988;148:1039–1045. [PubMed] [Google Scholar]
- 39.Miller D, Crandall S, Davis S, Ip E, Jamback G, Burns C, Kronner D, Marion G, Spangler J, Vaden K, Vernon J, Vitolins M. NEW Lifestyle: A downloadable teaching and learning program for Nutrition, Exercise, and Weight management. MedEdPORTAL. 2012;8:9256. Available from: Access www.mededportal.org/publication/9256. [Google Scholar]
- 40.Adams KM, Kohlmeier M, Powell M, Zeisel SH. Nutrition in medicine: nutrition education for medical students and residents. Nutr Clin Pract. 2010 Oct;25(5):471–480. doi: 10.1177/0884533610379606. Epub 2010/10/22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, Hu FB, Hubbard VS, Jakicic JM, Kushner RF, Loria CM, Millen BE, Nonas CA, Pi-Sunyer FX, Stevens J, Stevens VJ, Wadden TA, Wolfe BM, Yanovski SZ, Jordan HS, Kendall KA, Lux LJ, Mentor-Marcel R, Morgan LC, Trisolini MG, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC, Jr, Tomaselli GF, American College of Cardiology/American Heart Association Task Force on Practice G. Obesity S. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014 Jun 24;129(25 Suppl 2):S102–138. doi: 10.1161/01.cir.0000437739.71477.ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.American College of Sports Medicine. Exercise is Medicine 2017. cited 2017 February 14. Available from: http://www.exerciseismedicine.org/
- 43.U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans. cited 2017 February 14. Available from: https://health.gov/paguidelines/
- 44.American Heart Association. Healthy Living, Physical Activity Fitness Basics: American Heart Association. 2017 cited 2016. http://www.heart.org/HEARTORG/HealthyLiving/PhysicalActivity/FitnessBasics/Fitness-Basics_UCM_462340_SubHomePage.jsp.
- 45.U.S. Department of Health and Human Services. Dietary Guidelines for Americans: U.S. Department of Agriculture and U.S. Department of Health and Human Services. [updated February 14, 2017];2015 cited 2017 February 14. Available from: https://health.gov/dietaryguidelines/
- 46.Furney SL, Orsini AN, Orsetti KE, Stern DT, Gruppen LD, Irby DM. Teaching the one-minute preceptor. A randomized controlled trial. J Gen Intern Med. 2001 Sep;16(9):620–624. doi: 10.1046/j.1525-1497.2001.016009620.x. Epub 2001/09/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Neher JO, Stevens NG. The one-minute preceptor: shaping the teaching conversation. Fam Med. 2003 Jun;35(6):391–393. Epub 2003/06/24. [PubMed] [Google Scholar]
- 48.Goldstein MG, Niaura R, Willey C, Kazura A, Rakowski W, DePue J, Park E. An academic detailing intervention to disseminate physician-delivered smoking cessation counseling: smoking cessation outcomes of the Physicians Counseling Smokers Project. Prev Med. 2003 Feb;36(2):185–196. doi: 10.1016/s0091-7435(02)00018-x. Epub 2003/02/20. [DOI] [PubMed] [Google Scholar]
- 49.Gorin SS, Ashford AR, Lantigua R, Hossain A, Desai M, Troxel A, Gemson D. Effectiveness of academic detailing on breast cancer screening among primary care physicians in an underserved community. J Am Board Fam Med. 2006 Mar-Apr;19(2):110–121. doi: 10.3122/jabfm.19.2.110. Epub 2006/03/04. [DOI] [PubMed] [Google Scholar]
- 50.Ockene JK, Zapka JG. Physician-based smoking intervention: a rededication to a five-step strategy to smoking research. Addict Behav. 1997 Nov-Dec;22(6):835–848. doi: 10.1016/s0306-4603(97)00065-8. [DOI] [PubMed] [Google Scholar]
- 51.Seager JM, Howell-Jones RS, Dunstan FD, Lewis MA, Richmond S, Thomas DW. A randomised controlled trial of clinical outreach education to rationalise antibiotic prescribing for acute dental pain in the primary care setting. Br Dent J. 2006 Aug 26;201(4):217–222. doi: 10.1038/sj.bdj.4813879. discussion 216. Epub 2006/08/12. [DOI] [PubMed] [Google Scholar]
- 52.Soumerai SB, Avorn J. Principles of educational outreach ('academic detailing') to improve clinical decision making. Jama. 1990 Jan 26;263(4):549–556. Epub 1990/01/26. [PubMed] [Google Scholar]
- 53.Schmidt S, Rice A, Kolasa K. Teaching by example: educating medical students through a weight management experience. Fam Med. 2013 Sep;45(8):572–575. [PubMed] [Google Scholar]
- 54.Mazor K, Jolicoeur D, Hayes R, Geller A, Churchill L, Ockene J. Assessing Medical Students’ Tobacco Dependence Treatment Skills Using a Detailed Behavioral Checklist. Teaching and Learning in Medicine. 2015;27(3):292–298. doi: 10.1080/10401334.2015.1044660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Murray DM. Design and analysis of community trials: Lessons from the Minnesota Heart Health Program. Am J Epidemiol. 1995;142(6):569–575. doi: 10.1093/oxfordjournals.aje.a117677. [DOI] [PubMed] [Google Scholar]
- 56.Murray DM, Hannan PJ, Wolfinger RD, Baker WL, Dwyer JH. Analysis of data from group-randomized trials with repeat observations on the same groups. Stat Med. 1998 Jul 30;17(14):1581–1600. doi: 10.1002/(sici)1097-0258(19980730)17:14<1581::aid-sim864>3.0.co;2-n. Epub 1998/08/12. [DOI] [PubMed] [Google Scholar]
- 57.Ockene JK, Hayes RB, Churchill LC, Crawford SL, Jolicoeur DG, Murray DM, Shoben AB, David SP, Ferguson KJ, Huggett KN, Adams M, Okuliar CA, Gross RL, Bass PF, 3rd, Greenberg RB, Leone FT, Okuyemi KS, Rudy DW, Waugh JB, Geller AC. Teaching Medical Students to Help Patients Quit Smoking: Outcomes of a 10-School Randomized Controlled Trial. J Gen Intern Med. 2016 Feb;31(2):172–181. doi: 10.1007/s11606-015-3508-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Centers for Medicare and Medicaid Services. Decision memo for intensive behavioral therapy for obesity 2011. Available from: http://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?&NcaName=Intensive%20Behavioral%20Therapy%20for%20Obesity&bc=ACAAAAAAIAAA&NCAId=253&.
- 59.Wadden TA, Butryn ML, Hong PS, Tsai AG. Behavioral treatment of obesity in patients encountered in primary care settings: a systematic review. JAMA. 2014 Nov 5;312(17):1779–1791. doi: 10.1001/jama.2014.14173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Carvajal R, Wadden TA, Tsai AG, Peck K, Moran CH. Managing obesity in primary care practice: a narrative review. Ann N Y Acad Sci. 2013 Apr;1281:191–206. doi: 10.1111/nyas.12004. Epub 2013/01/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schlair S, Moore S, McMacken M, Jay M. How to Deliver High-Quality Obesity Counseling in Primary Care Using the 5As Framework. JCOM. 2012;19(5):221–229. [Google Scholar]
- 62.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 63.Baranowski T, Perry PJ, Parcel GS. Health Behavior and Health Education: Theory, Research and Practice. 3. San Francisco: Wiley & Sons; 2002. How individuals, environments, and health behavior interact. [Google Scholar]
- 64.Brookfield SD. New directions for continuing education. San Francisco: Jossey-Bass; 1985. Self-directed learning from theory to practice. [Google Scholar]
- 65.Knowles MS. The modern practice of adult education: from pedagogy to androgogy. New York: Adult Education Company; 1980. [Google Scholar]
- 66.Lave J, Wenger E. Situated learning: legitimate peripheral participation. Cambridge: University of Cambridge Press; 1991. [Google Scholar]
- 67.Torre DM, Daley BJ, Sebastian JL, Elnicki DM. Overview of current learning theories for medical educators. Am J Med. 2006 Oct;119(10):903–907. doi: 10.1016/j.amjmed.2006.06.037. [DOI] [PubMed] [Google Scholar]
- 68.Wagenschutz H, Ross P, Purkiss J, Yang J, Middlemas S, Lypson M. Standardized Patient Instructor (SPI) interactions are a viable way to teach medical students about health behavior counseling. Patient Educ Couns. 2011 Aug;84(2):271–274. doi: 10.1016/j.pec.2010.07.047. [DOI] [PubMed] [Google Scholar]
- 69.Alvin MD. The USMLE Step 2 CS: Time for a change. Med Teach. 2016 Aug;38(8):854–856. doi: 10.3109/0142159X.2016.1147539. [DOI] [PubMed] [Google Scholar]