Abstract
Objective
Examine the impact of age on baseline eating disorder symptoms/risk factors and on the effects of completing three variants of an eating disorder prevention program.
Method
680 women (60% White) were randomized to clinician-led Body Project groups, peer-led Body Project groups, an Internet-based version of the Body Project (eBodyProject), or educational video control condition. Participants, who were on average 22.2 years old (SD = 7.1, range 17-64, median = 19), were assessed at pretest, posttest, and 6-month follow-up.
Results
Two of the seven baseline variables were significantly associated with age, indicating that older age was associated with lower reported dieting (r = −.12) and better psychosocial functioning (r = −.13). Interactions indicated that age moderated the intervention effects, such that group-based programs were superior to the Internet-delivered version in terms of eating disorder symptom reductions for women up to age 20, whereas the Internet-delivered program were superior to group-based interventions, particularly in terms of BMI reduction, for women over approximately age 25. None of the four tests examining whether age moderated the effects of delivering Body Project groups by mental health clinicians versus undergraduate peer educators were significant.
Conclusions
Results suggest that group-based versions of the Body Project should be implemented with young women up to the age of 20, as they produce larger eating disorder symptom reductions, whereas the Internet version of the Body Project should be implemented with women aged 25 or older, as it produces superior weight loss/gain prevention effects.
Keywords: Eating disorders, prevention, age, moderation, obesity
Eating disorders are often considered to primarily affect young women. Few studies have examined the phenomenology of eating disorders among women after young adulthood and even less is known regarding the degree to which eating disorder prevention programs that are effective with young women also help older women. Although prospective studies indicate that late adolescence/early adulthood is the peak period of eating disorder onset [1; 2], these conditions do emerge later for some individuals. Based on retrospective data, Hudson and colleagues [3] found that anorexia nervosa had the earliest mean age of onset (18.9 years), followed by bulimia nervosa (19.7 years), and binge eating disorder (25.4 years). Regarding the range of onset ages, the interquartile ranges (i.e., average onset age for 25% to 75%) were 16.0–22.0 for anorexia nervosa, 14.0–22.0 for bulimia nervosa, and 17.0–32.0 for binge eating disorder. Examining the cumulative age of onset curves, rates of anorexia nervosa plateaued near age 26, bulimia nervosa near age 47, and binge eating disorder after age 70. Thus, these conditions tend to develop in late adolescence/early adulthood but impact women across the age range.
The goals of the present study are to examine the impact of age at the start of a prevention intervention on baseline levels of eating disorder risk factors and symptoms and whether age moderates the effects of three variants of the Body Project [4], an empirically supported eating disorder selective prevention program for young women with body dissatisfaction [5]. Data come from a randomized trial that is evaluating the relative effectiveness of clinician-led Body Project groups, undergraduate peer educator-led Body Project groups, and an Internet-delivered version of the program (called eBody Project), compared to an educational video control condition, with participants recruited from three colleges. We conducted this trial with female students and staff because rates of eating disorders are significantly higher among women than men [3], there are over 10 million US female college students [6], and colleges typically have an existing infrastructure for delivering prevention programs. We did not place an upper limit on the age of participants and allowed graduate students and staff who worked at the university to enroll. The sample had a mean age of 22.2 but ranged from 17 to 64 years of age, of which 20% were 25 or older, the commonly used definition for nontraditional-age college students [e.g., 7]. In a report analyzing initial outcomes on four variables (thin-ideal internalization, body dissatisfaction, negative affect, and eating disorder symptoms) with the entire sample [4], participants in clinician-led and peer-led Body Project groups, relative to video controls, showed similar reductions in the continuous outcome measures at both post-intervention (M d = .54 and .52, respectively; all 4 outcomes for each contrast p < .001) and 6-month follow-up (d = .33 and .35, respectively; all 4 outcomes p < .05 for clinician-led vs. video and 3 of 4 contrasts significant for peer-led vs. video); effects for the Internet-delivered eBody Project intervention relative to video control were approximately 50% smaller (d = .33 at post and .16 at 6-month follow-up; all 4 contrasts p < .05 at post, 2 of 4 significant at follow-up).
The current study examined two primary questions: (1) whether age is associated with different levels of current risk factors, current eating disorder symptoms, and body mass index (BMI) at baseline, and (2) whether age moderates the acute effects of prevention interventions on the clinically significant outcomes of eating disorder risk symptoms and BMI.
Regarding the first aim of baseline age differences, because the beauty ideal is centered around youth, it could be that body image concerns, eating disorder risk factors and symptoms increase with age. Surveys find that middle-aged women (defined as 35–55 years of age), report high rates of eating disorder symptoms, dieting, and body dissatisfaction, especially among those with higher body mass (BMI) values [8; 9; 10]. Some evidence suggests that body dissatisfaction does not show significant declines until women are past 70 [11]. Knowing whether women of different ages markedly vary on initial risk factors or symptom status might influence the focus of eating disorder prevention efforts.
Regarding the second aim of age moderation of intervention effects, the majority of eating disorder prevention programs have targeted adolescents and children [12], although a handful of prevention programs have been evaluated with middle-aged women, including a cognitive-behavioral group intervention aimed at improving body image and disordered eating behaviors in women 30–60 years of age with body dissatisfaction [13]; a program aimed at reducing body image concern and dieting behaviors among chronic female dieters (mean age = 44) [14]; and a 1-day Acceptance and Commitment Therapy (ACT) workshop focused on body dissatisfaction and disordered eating attitudes for women 18–65 years of age (mean = 43) with body dissatisfaction [15]. Although it is very encouraging that such programs are being developed and appear to produce positive effects in initial evaluations, no one to our knowledge has examined whether age significantly moderates the effectiveness of eating disorder prevention programs. Establishing that an intervention is helpful for women across a wide age span, rather than having to tailor programs for specific age groups, could facilitate implementation efforts. Conversely, if some versions of the Body Project are more effective for younger women whereas other versions are more effective for older women, we could better match individuals to the format most beneficial to them. The present trial affords a unique opportunity to examine these questions because it is the largest randomized trial to evaluate the Body Project program to date and contains participants of the broadest age range.
Method
Participants and Procedure
Participants were 680 women (M age = 22.2, SD = 7.1; M BMI [kg/m2] = 25.5, SD = 5.6) recruited from three universities in Oregon and Texas. The sample was 60% European American, 17% Latina, 14% Asian, 5% African American, 3% American Indian/Alaska Native, 1% Native Hawaiian/Pacific Islander. Participants were recruited between March 2013 – April 2015 using mass emails and flyers. Interested women were directed to a webpage to confirm that they had body dissatisfaction (inclusion criterion) and to complete the Eating Disorder Diagnostic Scale (EDDS) [16]; those with probable DSM-IV [17] anorexia nervosa, bulimia nervosa, and binge eating disorder were excluded. Eligible participants were randomly assigned to clinician-led Body Project groups (n = 173), undergraduate peer-led Body Project groups (n = 162), the eBody Project (n = 184), or an educational video condition (n = 161). Participants completed assessments at pretest, posttest, and 6-month follow-up conducted by female assessors masked to condition.
The Body Project consisted of 4 weekly 1-hour group sessions with 5–9 participants delivered by either clinicians or undergraduate peer educators using a scripted manual [see 18 for details regarding session content]. Teams of two facilitators delivered the intervention, with 19 clinician leaders and 17 peer leaders who were recruited from mental health clinics and the college peer leader program, respectively. The eBody Project is an Internet-based version of this intervention that includes 6 40-minute modules involving user-driven self-education activities and games designed to parallel the group program [see 19 for details]. Participants in the educational video condition were asked to view Dying to Be Thin [20], a 55-min documentary on eating disorders, body dissatisfaction, and body acceptance that was provided to them at no cost. Additional details regarding the study are provided in Stice et al. [4].
Measures
Thin-ideal internalization
The Thin-Ideal Internalization Scale [4] assessed agreement with 8 statements representing facets of the beauty ideal (“Slim women are more attractive”), which are rated on a 5-point scale. The measure showed an average α = .75 across assessments in the present trial. An earlier version of the measure, which shared most items, had shown 2-week test-retest reliability (r = .80), predictive validity for bulimic symptom onset, and sensitivity to detecting intervention effects [5].
Body dissatisfaction
Items from the Satisfaction and Dissatisfaction with Body Parts Scale [21] assessed satisfaction with 9 body parts rated on a 6-point scale. It has shown internal consistency (α = .94), 3-week test-retest reliability (r = .90), predictive validity for bulimic symptom onset, and sensitivity to intervention effects [5]; average α = .86.
Dieting
The 10-item Dutch Restrained Eating Scale (DRES) [22] assessed the frequency of dieting behaviors rated on a 5-point scale. It has shown internal consistency (α = .95), 2-week test-retest reliability (r = .82), convergent validity with self-reported caloric intake (but not objectively measured caloric intake), predictive validity for bulimic symptom onset, and sensitivity to intervention effects [5; 22]; average α = .91.
Negative affect
Negative affect was assessed with the sadness, guilt, and fear/anxiety subscales from the Positive Affect and Negative Affect Scale-Revised (PANAS-X) [23]. Participants reported the extent to which they had felt 20 negative emotional states, each rated on a 5-point scale. This scale has shown internal consistency (α = .95), 3-week test-retest reliability (r = .78), convergent validity, and predictive validity for bulimic symptom onset [24; 23]; average α = .94.
Psychosocial functioning
Psychosocial functioning in the family, peer, school, and work spheres, which has been found to be a highly significant risk factor for all eating disorders [25] was assessed with 17 items adapted from the Social Adjustment Scale (SAS) [26] rated on a 5-point scale. The adapted items have shown internal consistency (α = .77), 1-week test-retest reliability (r = .83), and sensitivity to intervention effects in multiple prevention trials [24; 5]; average α = .74.
Eating disorder symptoms
The semi-structured Eating Disorder Diagnostic Interview (EDDI) [27] assessed DSM-IV eating disorder symptoms. Items assessing symptoms in the past month were summed to form a composite of current symptoms; lifetime retrospective data were not collected regarding age of symptom onset at pretest. This composite has shown internal consistency (α = .92), inter-rater agreement (ICC r = .93), 1-week test-retest reliability (ICC r = .95), predictive validity, and sensitivity to detecting intervention effects [28; 27]. The symptoms composite showed internal consistency (average α = .70), inter-rater agreement (ICC = .96), and 1-week test-retest reliability (ICC = .96).
Body mass index (BMI)
After removing shoes and coats, height was measured to the nearest millimeter using stadiometers and weight was assessed to the nearest 0.1 kg using digital scales. Two measures of each were obtained and averaged. BMI correlates with direct measures of body fat such as dual energy x-ray absorptiometry (r = .80 – .90) and health measures such as blood pressure, adverse lipoprotein profiles, and diabetes mellitus [29].
Statistical Methods
Pearson correlations were used to examine the relations between age with the five baseline risk factors and two current symptom indices. We then examined whether age moderated intervention effects for the eating disorder symptoms composite score and BMI, both of which were assessed at pretest, posttest, and 6-month post-intervention follow-up. Random effect linear growth models were computed from posttest and 6-month follow-up data. The main effect of condition is a test of differences at posttest and the condition × time interaction (coded as months since posttest) is a test of whether intervention groups showed different trajectories during the 6-month follow-up. To test moderation, mean centered age was entered as a moderator along with age × condition, and age × condition × time, interaction terms. Three orthogonal contrasts from the four-level condition variable (1 = clinician-led, 2 = peer-led, 3 = eBody Project, 4 = video control) were tested: (1) active intervention (clinician-led, peer-led, eBody Project) vs. video control (n = 519 vs. 161, respectively) with contrast codes 1/3, 1/3, 1/3, −1, (2) group intervention (clinician-led, peer-led) vs. eBody Project Internet-based intervention (n = 335 vs. 184, respectively) with contrast codes 1/2, 1/2, −1, 0, and (3) clinician-led vs. peer-led groups (n = 173 vs. 162, respectively) with contrast codes 1, −1, 0, 0. A significant age × condition interaction would indicate differential posttest scores for a contrast as a function of age. A significant age × condition × time interaction would indicate differential change in trajectories for a contrast as a function of age. This trial used a partially nested design but previous analyses [4] indicated no significant variability attributable to groups in the partially clustered models, so we did not control for nesting in the two group-based conditions in this report. Site was investigated as a moderator of intervention effects, but were non-significant and thus, we ignored effects of site for these analyses. Missing data were imputed using IVEWare [30] with imputed data in 20 data sets analyzed separately; model parameters and standard errors were combined following Rubin [31].
Results
Preliminary Analyses
Three participants (0.4%) failed to provide age information and were not included in analyses. Of the remaining 677 cases the average age was 22.2 years (SD = 7.1, minimum = 17, maximum = 64, median = 19). There were no missing data at baseline but attrition was 10% at posttest (missing eating disorder symptom and interviewer-assessed BMI data = 9% and 11%, respectively) and 16% at 6-month (missing eating disorder symptom and interviewer-assessed BMI data = 11% and 22%, respectively). Attrition at posttest was associated with age (t[675] = 2.18, p = .031) with older women more likely to provide posttest data compared to younger women, but age was not associated with attrition at 6-month follow-up (p = .829). Age was not significantly associated with study condition or rates of ancillary health treatment during study enrollment (all p’s > .114). The average age of clinician facilitators was 33.8 years (SD = 10.1, range = 24–55 years) vs. 20.9 years for peer facilitators (SD = 0.9, range = 19–22 years); t-value = 5.86, p < .001. Participants were randomly assigned to condition regardless of age (i.e., no stratification) and age was not associated with condition assignment [4], as would be expected from random assignment; the number of female participants over age 24 in each of the 44 groups ranged from 0 – 7 (M = 1.7, SD = 2.3).
Association of Age with Baseline Eating Disorder Risk Factors and Symptom Measures
Correlations of the participant age with baseline levels of the eating disorder risk factors and symptom measures are shown in Table 1. Two of the seven baseline variables were significantly associated with participant age: dieting (r = −.119) and psychosocial functioning (r = −.132); these associations indicated that older age was associated with lower reported dieting and better psychosocial adjustment. Both of these effects were small (r effects: trivial < .10, small = .10 - .29, medium = .30 - .49, large ≥ .50).
Table 1.
Correlations of Age with Baseline Variables.
| Baseline Variable | Correlation r | p-value |
|---|---|---|
| Thin-ideal internalization | −.033 | .389 |
| Body dissatisfaction | .066 | .085 |
| Dieting | −.119 | .002 |
| Negative affect | −.058 | .132 |
| Psychosocial functioning | −.132 | .001 |
| Eating disorder symptoms composite | .053 | .170 |
| BMI | .067 | .082 |
Degree to which Age Moderates Intervention Effects
We next examined whether age moderated prevention effects on the two outcomes. Results of the tests of moderation in Table 2 show that four of the twelve interactions were significant. Age moderated both the condition effect (p = .006) and the condition × time effect (p = .016) for eating disorder symptoms in the group versus Internet contrast (Contrast 2); age moderated the condition × time effect (p = .041) for BMI in the active versus control contrast (Contrast 1); and age moderated the condition × time effect (p = .021) for BMI in the group versus Internet contrast (Contrast 2).
Table 2.
Test of Age Moderation Effects for Three Planned Contrasts.
| Age × Condition
|
Age × Condition × Time
|
||||
|---|---|---|---|---|---|
| Outcome | Contrast | T-value | p-value | T-value | p-value |
| Eating disorder symptoms | Active vs. control | 1.04 | .299 | 1.27 | .203 |
| Group vs. individual | 2.76 | .006 | 2.40 | .016 | |
| Clinician vs. peer | 1.31 | .189 | 0.01 | .993 | |
|
| |||||
| BMI | Active vs. control | 0.16 | .872 | 2.04 | .041 |
| Group vs. individual | 0.09 | .928 | 2.31 | .021 | |
| Clinician vs. peer | −0.36 | .720 | 0.15 | .882 | |
Graphical displays of the regions of significance were used to interpret significant moderating effects. In Figure 1a the vertical axis shows the difference between the group versus Internet intervention contrast at posttest (Age × Condition Contrast 2) on eating disorder symptom scores and the horizontal axis shows the range of participant ages in the study. The heavy line depicts the mean difference estimate. The two thin outer lines show the 95% confidence interval around the mean difference. Values of the age in which the mean difference in eating disorder symptom scores value of zero is not contained in the confidence interval represent significant change. Three patterns as a function of age are evident in Figure 1a: (1) women from approximately ages 17 to 20 (~63% of the sample) experienced significantly greater posttest reductions in eating disorder symptoms if they received the group interventions rather than eBody Project; (2) posttest eating disorder symptom reductions for women from approximately ages 20 to 40 (~31% of the sample) did not differ between the group interventions and eBody Project; and (3) women 40 and older (~ 6% of the sample) experienced significantly greater posttest reductions in eating disorder symptoms in the eBody Project condition compared to the group interventions. Figure 1b shows the degree of change from posttest to 6-month follow-up (Age × Condition × Time Contrast 2) in eating disorder symptoms for women who received group interventions relative to women in the eBody Project. For women who were approximately 31 years of age and or older (~ 7% of the sample), those who received one of the group interventions showed greater reductions in eating disorder symptoms over follow-up compared to women who had received the eBody Project.
Figure 1.
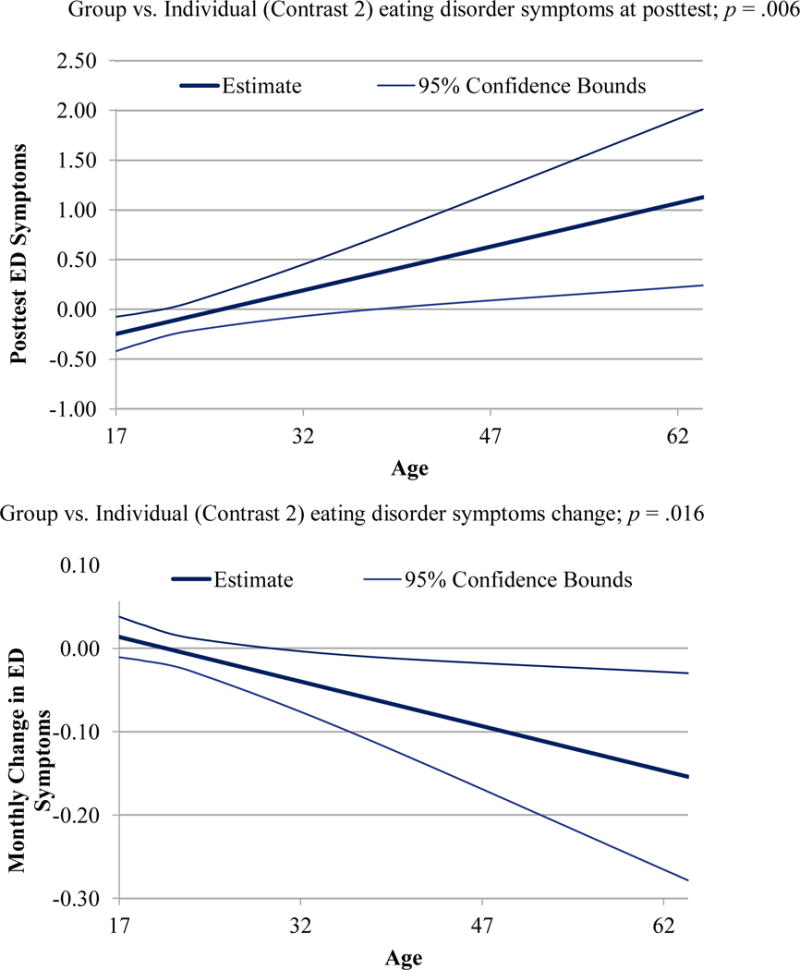
a and b Regions of Significance for Posttest Eating Disorder (ED) Symptom Scores and Change in ED Symptom Scores for Group versus Individual Programs
Note: To facilitate interpretation the ages shown on the horizontal axis were converted from mean centered to observed ages.
Age moderation effects for BMI are shown in Figure 2. Figure 2a shows significantly less BMI gainfrom posttest to 6-month follow-up (Age × Condition × Time Contrast 1) for women who received any of the three active interventions relative to women in the educational video control, which emerged at approximately age 37 and older (~ 5% of the sample). Lastly, Figure 2b shows significantly more BMI gain from posttest to 6-month follow-up (Age × Condition × Time Contrast 2) for women who received one of the group interventions relative to women in the eBody Project, which emerged at approximately age 25 and older (~ 17% of the sample). To interpret the magnitude of effects for the four interactions with age, Table 3 contains the effect size (Cohen’s d, small = .20 - .49) for four set age groups.
Figure 2.
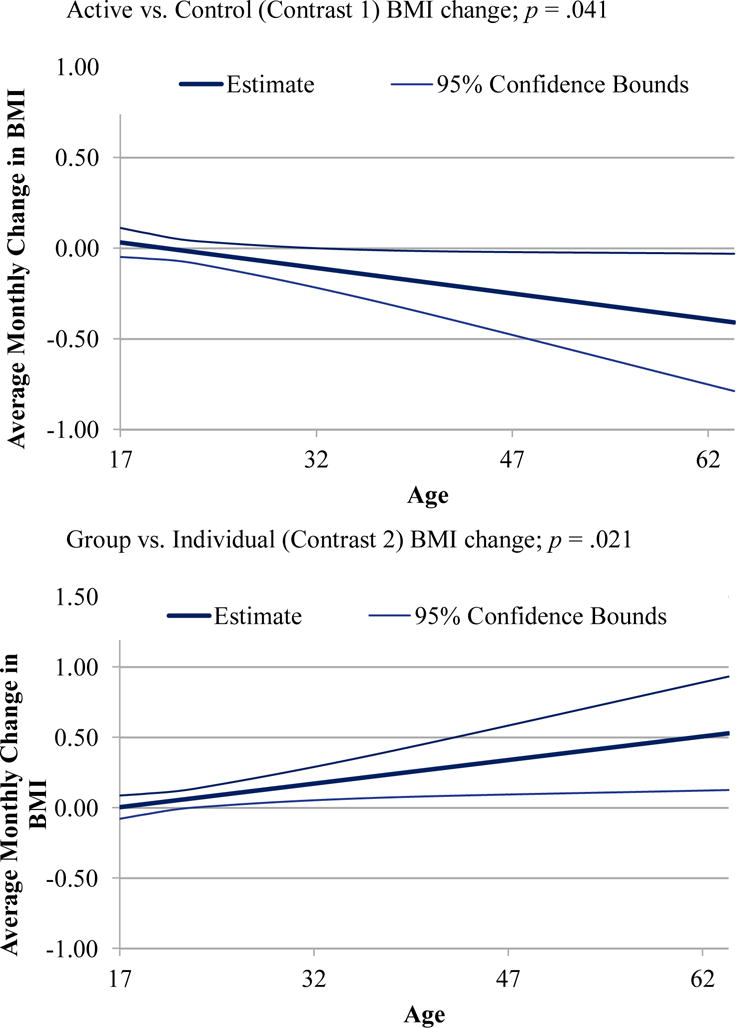
a and b Regions of Significance for Change in Body Mass Index (BMI) Scores for Active versus Video Control Programs and Group versus Individual Programs
Note: To facilitate interpretation the ages shown on the horizontal axis were converted from mean centered to observed ages.
Table 3.
Effect Size Estimates (d) for Significant Age Moderation Effects.
| Outcome | ES for Contrast | Age group | |||
|---|---|---|---|---|---|
| 17–19.9 | 20–24.9 | 25–29.9 | 30+ | ||
| (n = 344) | (n = 201) | (n = 73) | (n = 59) | ||
| Eating disorder symptoms | Group vs. eBody Project (A×C) | −.21 | −.18 | −.36 | .53 |
| Group vs. eBody Project (A×C×T) | .01 | −.03 | .17 | −.71 | |
|
| |||||
| BMI | Active vs. video control (A×C×T) | .02 | .01 | −.02 | −.22 |
| Group vs. eBody Project (A×C×T) | −.01 | .13 | −.07 | .44 | |
Note. Sample sizes (n) refer to number of the total sample in each age group, not contrast specific sample sizes. Effects sizes for age × condition (A×C) interactions are Cohen’s d and computed as group difference in the outcome at posttest divided by the pretest pooled standard deviation and age × condition × time (A×C×T) effect sizes are equivalent to Cohen’s d and). Pooled standard deviations were computed separately within each age group.
Discussion
The goals of this report were to examine age differences on baseline levels of eating disorder risk factors and symptoms and the degree to which age moderates response to three variants of an evidence-based selective prevention program. Overall, the differences that were significant were small in magnitude or, with one exception, applied to fairly small subsets of the entire sample, which suggests that participants across the examined age range were fairly similar at the start of the program and generally responded similarly to the prevention interventions. The generally focused nature of the significant findings is encouraging in terms of enhancing the feasibility of implementing these program as broadly as possible.
Regarding significant age effects on the participants’ characteristics when they started the trial, two differences were found indicating that the older participants had lower rates of dieting and better psychosocial adjustment, both of which were small effects. In other studies examining large samples of adult women over a broader age range, rates of reported dieting tend to decrease slightly with age [e.g., 60% among US women under the age of 55 reported weight control behaviors in the previous year compared to 50% of women 55 or older; 32]. It was encouraging that age was not found to be significantly associated with baseline levels of body dissatisfaction (the variable used to determine risk status and study inclusion), thin-ideal internalization (the primary target of the Body Project intervention), eating disorder symptoms (the primary outcome), or body mass, which could have influenced the other risk factors, if significant.
The second aim was to examine the impact of age on the magnitude of preventive effects on eating disorders symptoms and BMI. In the series of three planned orthogonal contrasts, moderation effects of age on the overall effectiveness of prevention efforts regardless of format relative to an educational video (i.e., Contrast 1) were significant for one outcome over follow-up and moderation effects of age on the effectiveness of in-person delivered Body Project group interventions relative to the stand-alone Internet-based eBody Project format (i.e., Contrast 2) were significant for both outcomes over follow-up in addition to one outcome at posttest. None of the four tests examining whether age moderated the effects of delivering the group-based Body Project by mental health clinicians versus undergraduate peer educators (i.e., Contrast 3) were significant, suggesting that older and younger group members did not markedly differ in their response to Body Project groups led by professional mental health clinicians or well-trained undergraduate peer educators.
The first moderation effect consisted of a significant Age × Condition interaction for eating disorder symptoms for group-based versus Internet prevention (Contrast 2), which indicated an intervention difference at posttest. Computing the 95% confidence interval for this effect across the age span suggested that, compared to those in the eBody Project, women between the ages of 17 and 20 in the two group-based conditions tended to have lower eating disorder symptom scores at the end of the intervention. This effect, which was small in magnitude, applied to almost two-thirds of the sample. Figure 1a also suggested that the effect was reversed for women who were approximately 40 years of age or older (roughly 6% of the sample); for this subset, those in group-based programs actually had higher eating disorder symptoms at posttest compared to women in eBody Project. This finding at posttest may have been mitigated by the second moderation effect (i.e., the significant Condition × Time × Age effect for Contrast 2), which suggested that women who were approximately 31 years of age or older in the two group-based conditions experienced greater eating disorder reductions over follow-up relative to women in the eBody Project condition. It is not surprising that these symptom effects were stronger in group interventions, as qualitative data from Body Project participants indicated that the group setting was perceived as one of the most valuable aspects of the program [33]; the positive effect of group-based delivery appeared to be most potent for the youngest participants.
The other two significant moderation effects consisted of Age × Condition × Time interactions for BMI in Contrasts 1 and 2, which indicated an intervention difference from posttest to 6-month follow-up; both effects were small in magnitude. Regarding the contrast of active prevention efforts relative to the educational video control, women in one of the three active conditions who were approximately 37 years of age or older (roughly 5% of the sample) experienced significantly lower BMI values over time relative to women of that age in the video control. Contrast 2 suggested that the potential weight reduction effects were specific to the eBody Project, starting with women who were approximately 25 years of age or older (which comprised 17% of the study sample). We have previously found the eBody Project produced weight gain prevention effects for the total sample out to 2-years post-intervention relative to educational brochure and video control conditions [M d = −.73; 34] and the Body Project resulted in lower obesity onset by 1-year follow-up relative to assessment control [3% vs. 12% onset; 35].
The results suggest that older women in particular benefitted from the eBody Project Internet-delivered format of prevention in terms of both eating disorder symptoms and BMI reductions. This pattern of effects did not appear to be due to older participants being more compliant with the self-directed method of intervention (e.g., eBody Project participants who were 30 years of age completed on average 3.3 modules compared to a mean of 4.2 modules for women who were at the mean of 22 years old). While it is encouraging that the eBody Project was not problematic for the older women, it should be noted again that the majority of our “older participants” were in their twenties, recruited from university settings, and generally well-educated. It is possible that women who were older than the traditionally aged college student may have preferred the privacy afforded by the Internet version of the program, potentially because there was less of a social comparison with younger participants who better conformed to the youthful beauty ideal.
Overall, the moderation effect that applied to the largest proportion of our sample (approximately 63%) suggested that eating disorder symptom reduction effects were significantly greater in either clinician- or peer educator-led group-based interventions as compared to the individually delivered eBody Project for women up to age 20; this effect is the strongest “treatment matching” recommendation offered by the present results. The second strongest recommendation for matching individuals to a specific treatment consisted of the recommendation for eBody Project over the group-delivered versions, particularly in terms of BMI reductions, for women over approximately age 25. These recommendations reflect qualitative moderation effects (i.e., different variants of the Body Project intervention are recommended at different ages) as opposed to a quantitative moderation effect, in which the same intervention would be made to all ages although the anticipated effect would differ in magnitude [36]. The findings for Aim 2 are useful in that they suggest post college-age women can benefit from Body Project groups, which has not been previously examined, and may especially benefit from the eBody Project, and that both formats of these interventions might work well in settings where women could easily be recruited across a wide age range (e.g., in the workplace).
Study limitations should be noted. First, although this was our largest study of eating disorder prevention programs, we did not have a large number of older women across the upper age levels; thus, we cannot comment with confidence on the effectiveness of the Body Project or eBody Project for middle-aged or older women specifically. Second, we focused on current presence or absence of both eating disorder risk factors and symptoms at baseline; we did not collect lifetime retrospective data to know how long those indices of eating pathology had been present. Our focus in this study was to evaluate the effectiveness of the three versions of the Body Project and examine variables that impact those outcomes rather than to contribute to knowledge regarding the etiology of eating disorders. Third, 60% of the sample was White and generally well-educated, which limits generalizability to other race/ethnicity and socioeconomic groups. Fourth, statistical power to detect moderation effects is often substantially lower than detecting main effects [37] and we did not apply a Bonferroni experiment-wide correction for the number of conducted tests. If we had, none of age moderation tests would have been considered significant (p = .05/12 = .004), although the two baseline age differences would have remained significant.
Future research directions include replicating the age differences (and non-differences) reported herein and, if replicated, understand what factors account for these effects and how they might influence the delivery of prevention efforts for women across the age span. In addition, future research needs to examine the effectiveness of various modalities of the Body Project with more diverse samples and in settings other than colleges and high schools. Although the Body Project group-based intervention has produced similar intervention effects for a variety of ethnic groups in the U.S. and is effective in other countries [38], it is important to continue evaluating the impact of age on this prevention program with a broader range of women of different ages, races, ethnicities, and cultures. This focus may be most relevant for evaluating the scalability of the eBody Project, given positive results for Internet-delivery in the present report.
Acknowledgments
This study was supported by grant (HD071900-01A1) from the National Institute of Child Health & Human Development.
We thank Julie Pope and Amber Borcyk for their work on this project and the participants who made this study possible.
Footnotes
Disclosure of Conflicts
The authors do not have any financial conflicts of interest to disclose.
References
- 1.Lewinsohn PM, Striegel-Moore RH, Seeley JP. The epidemiology and natural course of eating disorders in young women from adolescence to young adulthood. J Am Acad Child Adolesc Psychiatry. 2000;39:1284–1292. doi: 10.1097/00004583-200010000-00016. [DOI] [PubMed] [Google Scholar]
- 2.Stice E, Marti CN, Rohde P. Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. J Abnorm Pschol. 2013;122(2):445. doi: 10.1037/a0030679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stice E, Rohde P, Shaw H, Gau JM. Implementation trial of clinician-led, peer-led, and Internet-delivered dissonance-based eating disorder prevention programs. Manuscript submitted for publication. 2016 [Google Scholar]
- 5.Stice E, Marti C, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: Long-term effects from a randomized efficacy trial. J Consult Clin Psych. 2008;76:329–340. doi: 10.1037/0022-006X.76.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.U.S. Department of Education. Digest of Educational Statistics, 2007. National Center for Education Statistics. 2008 [Google Scholar]
- 7.Bean JP, Metzner BS. A conceptual model of nontraditional undergraduate student attrition. Rev Educ Res. 1985;55:485–540. [Google Scholar]
- 8.Gagne D, Von Holle A, Brownley K, Runfola C, Hofmeier S, Branch K, Bulik C. Eating disorder symptoms and weight and shape concerns in a large web-based convenience sample of women ages 50 and above: Results of the Gender and Body image study. Int J Eat Disord. 2012;45:832–44. doi: 10.1002/eat.22030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marcus M, Bromberger J, Wei H, Brown C, Kravitz H. Prevalence and selected correlates of eating disorder symptoms among a multiethnic community sample of midlife women. Ann Behav Med. 2007;33:269–77. doi: 10.1007/BF02879909. [DOI] [PubMed] [Google Scholar]
- 10.McLean S, Paxton S, Wertheim E. Factors associated with body dissatisfaction and disordered eating in women in midlife. Int J Eat Disord. 2010;43:527–36. doi: 10.1002/eat.20737. [DOI] [PubMed] [Google Scholar]
- 11.Tiggemann M. Body image across the adult lifespan: Stability and change. Body Image. 2004;1:29–41. doi: 10.1016/S1740-1445(03)00002-0. [DOI] [PubMed] [Google Scholar]
- 12.Stice E, Shaw H, Marti CN. A meta-analytic review of eating disorder prevention programs: Encouraging findings. Annu Rev Clin Psychol. 2007;3:207–231. doi: 10.1146/annurev.clinpsy.3.022806.091447. [DOI] [PubMed] [Google Scholar]
- 13.McLean SA, Paxton SJ, Wertheim EH. A body image and disordered eating intervention for women in midlife: A randomized controlled trial. J Consult Clin Psych. 2011;79:751. doi: 10.1037/a0026094. [DOI] [PubMed] [Google Scholar]
- 14.Higgins LC, Gray W. Changing the body image concern and eating behaviour of chronic dieters: the effects of a psychoeducational intervention. Psychol Health. 1998;13:1045–1060. [Google Scholar]
- 15.Pearson AN, Follette VM, Hayes SC. A pilot study of acceptance and commitment therapy as a workshop intervention for body dissatisfaction and disordered eating attitudes. Cogn Behav Pract. 2012;19:181–197. [Google Scholar]
- 16.Stice E, Fisher M, Martinez E. Eating disorder diagnostic scale: Additional evidence of reliability and validity. Psychol Assessment. 2004;16:60–71. doi: 10.1037/1040-3590.16.1.60. [DOI] [PubMed] [Google Scholar]
- 17.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 2000. text rev. [Google Scholar]
- 18.Stice E, Butryn M, Rohde P, Shaw H, Marti N. An effectiveness trial of a new enhanced dissonance eating disorder prevention program among female college students. Behav Res Ther. 2013;51:862–871. doi: 10.1016/j.brat.2013.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stice E, Rohde P, Durant S, Shaw H. A preliminary trial of a prototype Internet dissonance-based eating disorder prevention program for young women with body image concerns. J Consult Clin Psych. 2012;80:907–916. doi: 10.1037/a0028016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Video WGBH. Twin Cities Public Television. Saint Paul, MN: WGBH Educational Foundation; 2000. Dying to be thin [DVD] [Google Scholar]
- 21.Berscheid E, Walster E, Bohrnstedt G. The happy American body: A survey report. Psychol Today. 1973;7:119–131. [Google Scholar]
- 22.van Strien T, Frijters JE, Van Staveren WA, Defares PB, Deurenberg P. The predictive validity of the Dutch Restrained Eating Scale. Int J Eat Disord. 1986;5:747–755. [Google Scholar]
- 23.Watson D, Clark LA. Affects separable and inseparable: On the hierarchical arrangement of the negative affects. J Pers Soc Psychol. 1992;62:489–505. [Google Scholar]
- 24.Stice E, Shaw H, Burton E, Wade E. Dissonance and healthy weight eating disorder prevention programs: A randomized efficacy trial. J Consult Clin Psych. 2006;74:263–275. doi: 10.1037/0022-006X.74.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stice E, Gau JM, Rohde P, Shaw H. Risk factors that predict future onset of each DSM-5 eating disorder: Predictive specificity in high-risk adolescent females. J Abnorm Psychol. doi: 10.1037/abn0000219. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weissman M, Bothwell S. Assessment of social adjustment by patient self-report. Arch Gen Psychiatry. 1976;33:1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- 27.Stice E, Rohde P, Gau J, Shaw H. An effectiveness trial of a dissonance-based eating disorder prevention program for high-risk adolescent girls. J Consult Clin Psych. 2009;77:825–834. doi: 10.1037/a0016132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burton E, Stice E. Evaluation of a healthy-weight treatment program for bulimia nervosa: A preliminary randomized trial. Behav Res Ther. 2006;44(12):1727–1738. doi: 10.1016/j.brat.2005.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pietrobelli A, Faith M, Allison D, Gallagher D, Chiumello G, Heymsfield S. Body mass index as a measure of adiposity among children and adolescents: A validation study. J Pediatr. 1998;132:204–210. doi: 10.1016/s0022-3476(98)70433-0. [DOI] [PubMed] [Google Scholar]
- 30.Raghunathan T, Solenberger P, Van Hoewyk J. IVEware: imputation and variance estimation software University of Michigan. Ann Arbor, MI: Institute for Social Research; 2016. [Google Scholar]
- 31.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley & Sons, Inc; 1987. [Google Scholar]
- 32.Yaemsiri S, Slining MM, Agarwal SK. Perceived weight status, overweight diagnosis, and weight control among US adults: The NHANES 2003–2008 Study. Int J Obes (Lond) 2011;35:1063–1070. doi: 10.1038/ijo.2010.229. [DOI] [PubMed] [Google Scholar]
- 33.Shaw H, Rohde P, Stice E. Participant feedback from peer-led, clinician-led, and Internet-delivered eating disorder prevention interventions. Int J Eat Disord. 2016;49:1087–1092. doi: 10.1002/eat.22605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stice E, Durant S, Rohde P, Shaw H. Effects of a prototype internet dissonance-based eating disorder prevention program at 1- and 2-year follow-up. Health Psychol. 2014;33:1558–1567. doi: 10.1037/hea0000090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stice E, Shaw H, Burton E, Wade E. Dissonance and Healthy Weight Eating Disorder Prevention Programs: A Randomized Efficacy Trial. J Consult Clin Psychol. 2006;74(2):263–275. doi: 10.1037/0022-006X.74.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 37.Brown CH, Sloboda Z, Faggiano F, Teasdale B, Keller F, Burkhart G, et al. Methods for synthesizing findings on moderation effects across multiple randomized trials. Prev Sci. 2013;14(2):144–156. doi: 10.1007/s11121-011-0207-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stice E, Rohde P, Shaw H. The Body Project: A Dissonance-Based Eating Disorder Prevention Program (updated edition) New York: Oxford University Press; 2012. [Google Scholar]


