Abstract
Importance
Although hospitals vary markedly in survival for their patients with in-hospital cardiac arrest, specific resuscitation practices that distinguish sites with higher cardiac arrest survival remain unknown.
Objective
To identify resuscitation practices associated with higher rates of in-hospital cardiac arrest survival.
Design, Setting, and Participants
Nationwide survey of resuscitation practices at adult hospitals participating in the Get With The Guidelines (GWTG)-Resuscitation registry and with ≥ 20 adult in-hospital cardiac arrest cases between 2012 and 2013.
Main Outcomes and Measures
Risk-standardized survival rates for cardiac arrest were calculated at each hospital, and these were then used to categorize hospitals into quintiles of performance. The association between resuscitation practices and quintiles of survival was evaluated using hierarchical proportional odds logistic regression models.
Results
Overall, 150 of 192 eligible hospitals (78.1%) completed the study survey and 131 facilities with ≥ 20 cases comprised the final study cohort. Risk-standardized survival rates after in-hospital cardiac arrest varied substantially (median: 23.7%; range: 9.2% to 37.5%). Several resuscitation practices were associated with survival on bivariate analysis, although only three were significant after multivariable adjustment: tracking interruptions in chest compressions (adjusted OR for being in a higher survival quintile category, 2.71 [95% CI: 1.24, 5.93]; P=0.01); reviewing cardiac arrest cases monthly or quarterly (adjusted OR for being in a higher survival quintile category, 8.55 [1.79, 40.0] for monthly and 6.85 [1.49, 31.3] for quarterly; P=0.03); and adequate resuscitation training (adjusted OR, 3.23 [1.21, 8.33]; P=0.02).
Conclusions and Relevance
Using survey information from acute care hospitals participating in a national quality improvement registry, we identified three resuscitation strategies associated with higher hospital rates of survival for patients with in-hospital cardiac arrest. These strategies can form the foundation for best practices for resuscitation care at hospitals, given the high incidence and variation in survival for in-hospital cardiac arrest.
Introduction
In-hospital cardiac arrest occurs in approximately 200,000 patients annually in the U.S.1 Despite a poor prognosis, survival for this condition varies by 3-fold across hospitals, from 11% to 35%.2 Recently, the Institute of Medicine issued a call to action on increasing our understanding of resuscitation practices in order to prompt renewed efforts for implementation research.3 Although several strategies, including bystander delivery of cardiopulmonary resuscitation and therapeutic hypothermia have been linked to better outcomes for out-of-hospital cardiac arrest, resuscitation practices associated with higher survival for in-hospital cardiac arrest remain undefined. Use of feedback devices to optimize cardiopulmonary resuscitation quality4 and immediate debriefing of team members after resuscitation5 have been described in single-center studies, but neither has been shown to be associated with overall survival. Determining which resuscitation practices distinguish hospitals with high survival rates for in-hospital cardiac arrest remains a critical next step to advancing care in these high-risk patients.6
The emergence of the Get With The Guidelines (GWTG)-Resuscitation registry has recently enabled several multi-center investigations of in-hospital cardiac arrest. However, resuscitation practices within hospitals have been infrequently characterized even within GWTG-Resuscitation, and the association of resuscitation practices with in-hospital cardiac arrest survival has not been previously examined in any data source. Accordingly, within GWTG-Resuscitation, we performed facility-level surveys to assess resuscitation practices among currently enrolled hospitals. We leveraged recently developed statistical methods to adjust for patient case-mix and examined the association of hospitals’ resuscitation practices with risk-standardized in-hospital cardiac survival rates. Our goal was to identify resuscitation practices associated with better performance, as these approaches may be potentially shared across facilities to improve overall outcomes.
Methods
Study Population
GWTG-Resuscitation is a large, prospective, national quality-improvement registry of in-hospital cardiac arrest and is sponsored by the American Heart Association. Its design has been described in detail previously.7 In brief, trained quality-improvement hospital personnel identify all patients without do-not-resuscitate orders with a cardiac arrest (defined as absence of a palpable central pulse, apnea, and unresponsiveness) who undergo cardiopulmonary resuscitation. Cases are identified by multiple methods, including centralized collection of cardiac arrest flow sheets, reviews of hospital paging system logs, and routine checks of code carts, pharmacy tracer drug records, and hospital billing charges for resuscitation medications.7 The registry uses standardized Utstein-style definitions for all patient variables and outcomes to facilitate uniform reporting across hospitals.8, 9 In addition, data accuracy is ensured by rigorous certification of hospital staff and use of standardized software with data checks for completeness and accuracy.
As in-hospital cardiac arrest survival has improved over the past decade,10 we restricted our study population to 204 hospitals within GWTG-Resuscitation who were (1) active within the registry during November 2014 (when the survey was initiated) and (2) entered cases between January 1, 2012 and December 31, 2013 (Supplementary Appendix eFigure 1). We excluded pediatric hospitals (n = 12), as well as pediatric cases in hospitals with both pediatric and adult patients. Among the remaining 192 hospitals that were contacted to complete the study survey, 42 did not respond, yielding a completion rate of 78.1%. Hospitals that did not respond had similar characteristics and survival rates for in-hospital cardiac arrest as hospitals that completed the survey (Supplementary Appendix eTable 1). Finally, among 150 hospitals which completed the study survey, we excluded 19 hospitals with fewer than 20 cardiac arrests (total of 145 cardiac arrest cases) during the 2-year study period. Our final study cohort comprised 17,613 adult patients at 131 hospitals.
Measures and Data Collection
In November of 2014, we surveyed resuscitation practices among actively participating hospitals within GWTG-Resuscitation over a 6-month period of time. Liaisons within each hospital connected to GWTG-Resuscitation served as the primary recipient of the survey. The survey was developed based on clinical expertise in our team, outside experts, and the scientific leadership within GWTG-Resuscitation (Supplementary Appendix eFigure 2). The survey included 45 items concerning 22 key resuscitation strategies, using multiple-choice questions for each item. Prior to its implementation period, the survey was field-tested by pilot hospital sites for clarity and comprehensiveness.
Resuscitation practices in the survey covered a variety of hospital strategies related to the prevention (e.g., use of rapid response teams, standardized risk scores for appropriate hospital unit assignment of admitted patients, patient to nurse ratio), treatment (e.g., use of mock codes, intra-arrest monitoring devices of cardiopulmonary resuscitation quality), and review (e.g., immediate debriefing after an acute resuscitation, formal reviews of cardiac arrest cases and quality of care measures [survival rates, defibrillation time]) of in-hospital cardiac arrests. Questions on hospital culture included items about administrative leadership, quality improvement, safety, and perceived barriers at one’s hospital.
Statistical Analysis
The primary outcome for this study was hospital rates of survival to hospital discharge. For each hospital, we first computed risk-standardized survival rates to hospital discharge for in-hospital cardiac arrest using previously validated methodology.2 Briefly, this published model considered a total of 26 variables to predict survival to discharge after in-hospital cardiac arrest. Using multivariable hierarchical logistic regression, an initial model of 18 predictors was derived with a c-statistic of 0.738. Further model reduction yielded a final parsimonious model (c-statistics of 0.734) of 9 predictors (age; initial cardiac arrest rhythm; hospital location of arrest; hypotension, sepsis, metastatic or hematologic malignancy, and hepatic insufficiency within 24 hours of cardiac arrest; and treatment with mechanical ventilation or need for intravenous vasopressors preceding cardiac arrest). For this study, we re-constructed a hierarchical logistic regression model with our study cohort using these 9 final predictors to predict survival to hospital discharge. Using the hospital-specific estimates (i.e., random intercepts) derived from this hierarchical model, a risk-standardized survival rate for each hospital was determined.2
Summary statistics were then used to describe the distribution of hospital rates of risk-standardized survival for in-hospital cardiac arrest in the cohort. To highlight best resuscitation practices at sites with the highest survival rates and to facilitate clinical interpretability of study findings, the hospital sample was divided into quintiles of risk-standardized in-hospital cardiac arrest survival. We then categorized the quintiles into three groups to simplify reporting: top quintile, middle three quintiles, and bottom quintile. Characteristics of hospitals and patients were then compared across the 3 groups.
For each of the hospital strategies and culture items, we determined the number and percentage of hospitals in each response category. To evaluate the association of specific resuscitation practices and hospital culture with hospital rates of risk-standardized survival for in-hospital cardiac arrest, hierarchical logistic regression models were used, which account for clustering of patients within hospitals.11, 12 For initial bivariate comparisons, we constructed a separate model for each hospital strategy and factor, as well as hospital case volume. We then constructed a multivariable hierarchical proportional odds logistic regression model, which included those independent variables that had a bivariate association with hospital rates of risk standardized survival (P<0.10). A proportional odds model was used as it could examine the association between resuscitation practices and a hospital’s likelihood of having risk-standardized survival rates in the next highest quintile category. For instance, a hospital strategy with an odds ratio of 1.50 would indicate that hospitals employing that strategy had 50% greater odds of being in the top hospital survival quintile as compared with hospitals in the middle quintiles and of being in the middle quintiles as compared with the bottom quintile.
All study analyses were performed with SAS 9.2 (SAS Institute, Cary, NC) and R version 2.10.0.13 The hierarchical models were fitted with the use of the GLIMMIX macro in SAS and evaluated at a 2-sided significance level of 0.05. Dr. Chan had full access to the data and takes responsibility for its integrity. All authors have read and agree to the manuscript as written. The institutional review board of the Mid America Heart Institute approved the study protocol.
Results
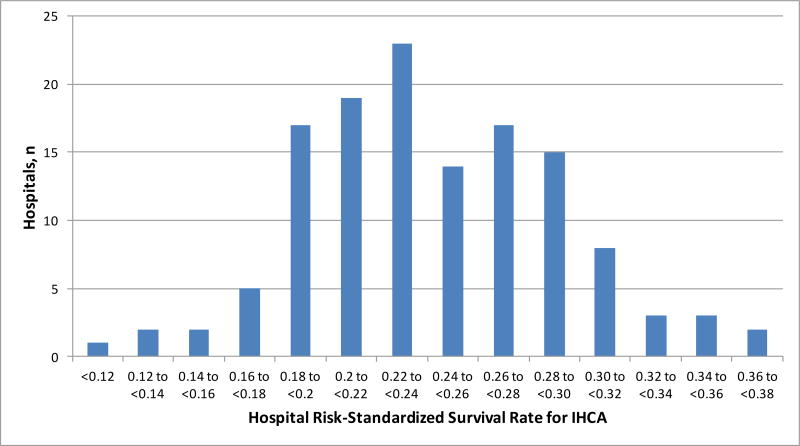
Across 131 hospitals, risk-standardized rates of survival for in-hospital cardiac arrest varied substantially, ranging from 9.2% to 37.5% (median of 23.7%, inter-quartile range [IQR]: 20.6% to 27.7%) (Figure 1). To quantify the extent of variation in survival, the adjusted median odds ratio was 1.47 (95% CI: 1.41, 1.57), which suggests that patients with identical covariates had, on average, a 47% difference in odds of surviving to hospital discharge at two different randomly selected hospitals.
Figure 1. Distribution of Risk-Standardized Survival Rates for In-Hospital Cardiac Arrest Among Study Hospitals.
Abbreviation: IHCA, in-hospital cardiac arrest
The median risk-standardized survival rate for hospitals in the top quintile, middle three quintiles, and bottom quintile was 30.9% (IQR: 29.1% to 32.8%), 23.6% (IQR: 21.9% to 26.3%), and 19.0% (IQR: 15.4% to 19.5%), respectively. Hospitals in the top quintile were more likely to be academic hospitals, but there were no differences in bed number, geographical location, or rural status between the 3 hospital categories (Table 1). In general, patient factors were relatively similar between hospitals in the top, middle three, and bottom quintiles. Hospitals in the top quintile did have a lower proportion of cardiac arrest patients with black race and pulseless electrical activity as the initial cardiac arrest rhythm, but were also more likely to have patients with hypotension prior to cardiac arrest.
Table 1. Characteristics of Study Hospitals, Stratified by Quintile Category of Risk-Standardized Survival*.
| Lowest Survival Quintile 1 (n = 26) |
Middle Survival Quintiles 2 to 4 (n = 78) |
Highest Survival Quintile 5 (n = 27) |
P value | |
|---|---|---|---|---|
| HOSPITAL CHARACTERISTICS | ||||
| Bed number, n (%) | 0.09 | |||
| <200 | 0.0% | 27.3% | 21.7% | |
| 200 to 499 | 75.0% | 49.1% | 43.5% | |
| ≥ 500 | 25.0% | 23.6% | 34.8% | |
| Academic status, n (%) | 0.04 | |||
| Major teaching hospital | 18.8% | 27.3% | 47.8% | |
| Minor teaching hospital | 62.5% | 32.7% | 17,4% | |
| Non-teaching hospital | 18.8% | 40.0% | 34.8% | |
| Rural hospital, n (%) | 6.3% | 9.1% | 8.7% | 0.97 |
| Geographical location, n (%) | 0.17 | |||
| North Mid-Atlantic | 18.8% | 16.4% | 26.1% | |
| South Mid-Atlantic | 25.0% | 25.5% | 17.4% | |
| North Central | 25.0% | 12.7% | 26.1% | |
| South Central | 31.3% | 18.2% | 8.7% | |
| Mountain Pacific | 0.0% | 27.3% | 21.7% | |
| Cardiac Arrest Case Volume, Median (IQR) | 117 (73, 186) | 84 (40, 172) | 122 (66, 241) | 0.24 |
|
| ||||
| DEMOGRAPHICS | ||||
| Age | 65.3 ± 4.9 | 66.6 ± 4.4 | 65.2 ± 3.5 | 0.23 |
| Male Sex, % | 58.8% ± 6.8% | 60.0% ± 9.6% | 60.2% ± 4.3% | 0.78 |
| Black Race, % | 33.2% ± 23.2% | 18.1% ± 17.8% | 14.4% ± 15.2% | <0.001 |
| PRE-EXISTING CONDITIONS, % | ||||
| Hypotension | 10.4% ± 9.9% | 19.9% ± 15.3% | 28.3% ± 17.3% | <0.001 |
| Sepsis | 13.2% ± 10.8% | 15.5% ± 9.3% | 17.8% ± 9.3% | 0.21 |
| Metastatic Malignancy | 9.2% ± 4.6% | 11.2% ± 7.0% | 10.9% ± 7.1% | 0.43 |
| HepaticInsufficiency | 5.1% ± 4.7% | 6.6% ± 4.4% | 7.7% ± 5.6% | 0.15 |
| ARREST CHARACTERISTICS, % | ||||
| Initial Cardiac Arrest Rhythm | ||||
| Pulseless Electrical Activity | 37.0% ± 14.7% | 29.9% ± 9.9% | 26.5% ± 8.1% | 0.001 |
| Asystole | 47.5% ± 11.8% | 52.8% ± 10.1% | 51.2% ± 10.9% | 0.09 |
| Ventricular Fibrillation | 9.6% ± 5.6% | 10.0% ± 4.9% | 12.6% ± 5.2% | 0.053 |
| Pulseless Ventricular Tachycardia | 6.0% ± 3.2% | 7.3% ± 4.1% | 9.7% ± 7.3% | 0.02 |
| Hospital Location | ||||
| ICU | 51.7% ± 11.9% | 48.4% ± 12.1% | 44.1% ± 14.3% | 0.09 |
| Monitored unit | 13.7% ± 9.0% | 13.8% ± 10.6% | 14.1% ± 9.1% | 0.99 |
| Non-monitored unit | 14.2% ± 8.8% | 17.4% ± 11.9% | 15.7% ± 9.5% | 0.61 |
| Emergency room | 12.3% ± 12.5% | 11.6% ± 10.8% | 17.2% ± 15.5% | 0.12 |
| Procedural or surgical area | 6.1% ± 3.7% | 6.6% ± 4.4% | 7.2% ± 4.5% | 0.52 |
| Other | 2.0% ± 2.0% | 2.2% ± 2.8% | 1.9% ± 1.9% | 0.76 |
| INTERVENTIONS IN PLACE PRIOR TO ARREST, % | ||||
| Mechanical ventilation | 32.2% ± 15.5% | 30.2% ± 13.6% | 35.7% ± 13.3% | 0.22 |
| Intravenous Vasopressors | 20.3% ± 13.6% | 21.0% ± 10.1% | 23.4% ± 8.2% | 0.52 |
For age, the mean of the mean age at each hospital is reported for each quintile group. Otherwise, for other patient variables, rates represent the mean (± standard deviation) prevalence rate among hospitals in each quintile group.
Abbreviations: IQR, inter-quartile range
Several hospital resuscitation practices had statistically significant bivariate (unadjusted) associations with risk-standardized survival rates for in-hospital cardiac arrest (Table 2). Compared with hospitals in the middle quintiles or the bottom quintile, hospitals in the top quintile were more likely to have cardiac arrests reviewed sooner after their occurrence, track defibrillation times, track interruptions in chest compressions, conduct immediate debriefing after an acute resuscitation, have a dedicated intensive care specialist at all times in their intensive care units, and report adequate resuscitation training. In contrast, hospitals in the bottom survival quintile were much more likely to cite a lack of a resuscitation champion as a moderate or severe barrier at their facility. Notably, a number of other resuscitation strategies had no significant association with in-hospital cardiac arrest survival. This included review of cardiac arrests in routine morbidity and mortality conferences, conduct of mock codes, presence of a rapid response team, use of dedicated cardiac arrest resuscitation teams, allowance for nurses not certified in Acute Cardiac Life Support to defibrillate patients prior to resuscitation team arrival, frequency of hypothermia treatment, patient to nurse ratio, and use of intra-arrest devices for enhancing cardiopulmonary resuscitation quality, such as a metronome, audio-visual feedback, and mechanical devices.
Table 2. Unadjusted Associations Between Hospital Strategies and Factors with Risk-Standardized Survival for In-Hospital Cardiac Arrest.
| Risk Standardized Survival Rate Groups | ||||
|---|---|---|---|---|
| Lowest Survival Quintile (Q1) n = 26 |
Middle Survival Quintiles (Q2-Q4) n = 78 |
Highest Survival Quintile (Q5) n = 27 |
P for trend |
|
|
STRATEGIES TO PREVENT IHCA
| ||||
| Does your hospital use a risk score for bed type placement on admission? | 5 (19.2%) | 9 (11.7%) | 7 (29.2%) | 0.13 |
| Not answered | 1 | 3 | ||
| Does your hospital discuss code status with all admitted patients? | 17 (68.0%) | 47 (61.0%) | 17 (65.4%) | 0.95 |
| Not answered | 1 | 1 | 1 | |
| Does your hospital have a rapid response team? | 19 (73.1%) | 68 (87.2%) | 23 (85.2%) | 0.51 |
| Does your hospital use root cause analysis to examine IHCAs? | 16 (64.0%) | 48 (62.3%) | 19 (70.4%) | 0.51 |
| Not answered | 1 | 1 | ||
| What is your hospital's patient to nurse ratio on general medical/surgical floors? | 0.33 | |||
| 4 or fewer patients per nurse | 4 (15.4%) | 15 (19.5%) | 5 (20.0%) | |
| 5 patients per nurse | 11 (42.3%) | 38 (49.4%) | 14 (56.0%) | |
| 6 or more patients per nurse | 11 (42.3%) | 24 (31.2%) | 6 (24.0%) | |
| Not answered | 1 | 2 | ||
|
| ||||
| STRATEGIES TO TREAT IHCA | ||||
|
| ||||
| What Committee collects and reviews IHCA data? | 0.66 | |||
| Dedicated hospital resuscitation committee | 16 (64.0%) | 57 (75.0%) | 20 (74.1%) | |
| General quality improvement committee | 2 (8.0%) | 8 (10.5%) | 2 (7.4%) | |
| Other | 7 (28.0%) | 11 (14.5%) | 5 (18.5%) | |
| Not answered | 1 | 2 | ||
| How often are IHCAs reviewed? | 0.19 | |||
| At least monthly | 11 (44.0%) | 40 (52.6%) | 15 (55.6%) | |
| Quarterly | 9 (36.0%) | 29 (38.2%) | 11 (40.7%) | |
| Semi-annually or annually | 4 (16.0%) | 4 (5.3%) | 0 (0.0%) | |
| Not reviewed | 1 (4.0%) | 3 (3.9%) | 1 (3.7%) | |
| Not answered | 1 | 2 | ||
| Does your hospital track its survival rate for IHCA | 18 (75.0%) | 61 (81.3%) | 21 (77.8%) | 0.94 |
| Not answered | 2 | 3 | ||
| Does your hospital track its times to defibrillation? | 17 (68.0%) | 55 (72.4%) | 24 (88.9%) | 0.04 |
| Not answered | 1 | 2 | ||
| Does your hospital track interruptions to chest compressions? | 6 (24.0%) | 25 (33.3%) | 14 (51.9%) | 0.03 |
| Not answered | 1 | 3 | ||
| Are IHCA events discussed at Morbidity and Mortality conferences? | 8 (32.0%) | 23 (31.5%) | 10 (40.0%) | 0.45 |
| Not answered | 1 | 5 | 2 | |
| Does your hospital conduct mock codes? | 24 (96.0%) | 67 (87.0%) | 24 (88.9%) | 0.69 |
| Not answered | 1 | 1 | ||
| Is there a residency training program at your hospital? | 15 (57.7%) | 40 (51.9%) | 13 (48.1%) | 0.54 |
| Not answered | 1 | |||
| How often are code carts checked? | 0.82 | |||
| Every shift | 11 (42.3%) | 30 (38.5%) | 7 (25.9%) | |
| Daily | 12 (46.2%) | 47 (60.3%) | 20 (74.1%) | |
| Weekly | 1 (3.8%) | 0 (0.0%) | 0 (0.0%) | |
| Other | 2 (7.7%) | 1 (1.3%) | 0 (0.0%) | |
| Does your hospital use a dedicated Code Blue team? | 19 (73.1%) | 59 (75.6%) | 20 (74.1%) | 0.98 |
| Does your hospital routinely use devices for CPR? | ||||
| None used routinely | 15 (57.7%) | 42 (53.8%) | 12 (44.4%) | 0.31 |
| Yes | ||||
| Metronome | 0 (0.0%) | 5 (6.4%) | 2 (7.4%) | 0.39 |
| CPR device with audio and/or visual feedback | 3 (11.5%) | 12 (15.4%) | 6 (22.2%) | 0.28 |
| Capnography (continuous end-expiratory carbon dioxide values) | 11 (42.3%) | 25 (32.1%) | 15 (55.6%) | 0.10 |
| Mechanical CPR device (e.g. Autopulse, LUCAS) | 2 (7.7%) | 9 (11.5%) | 2 (7.4%) | 0.76 |
| How often code debriefing performed | 0.03 | |||
| Always (100% of the time) | 0 (0.0%) | 5 (6.5%) | 1 (3.7%) | |
| Frequently (50% to 99% of the time) | 6 (24.0%) | 18 (23.4%) | 10 (37.0%) | |
| Occasionally (10% to 49% of the time) | 7 (28.0%) | 17 (22.1%) | 10 (37.0%) | |
| Rarely (1% to 9% of the time) | 10 (40.0%) | 27 (35.1%) | 6 (22.2%) | |
| Never (0% of the time) | 2 (8.0%) | 10 (13.0%) | 0 (0.0%) | |
| Not answered | 1 | 1 | ||
|
| ||||
| POST-RESUSCITATION CARE STRATEGIES | ||||
|
| ||||
| How often is hypothermia begun in comatose patients with ROSC? | 0.31 | |||
| Always (100% of the time) | 2 (8.0%) | 8 (10.5%) | 4 (15.4%) | |
| Frequently (50% to 99% of the time) | 7 (28.0%) | 22 (28.9%) | 7 (26.9%) | |
| Occasionally (10% to 49% of the time) | 6 (24.0%) | 18 (23.7%) | 8 (30.8%) | |
| Rarely (1% to 9% of the time) | 9 (36.0%) | 18 (23.7%) | 5 (19.2%) | |
| Never (0% of the time) | 0 (0.0%) | 2 (2.6%) | 1 (3.8%) | |
| Therapeutic hypothermia not available at my hospital | 1 (4.0%) | 8 (10.5%) | 1 (3.8%) | |
| Not answered | 1 | 2 | 1 | |
| Does your hospital have board eligible physicians available 24/7 in ICUs? | 13 (50.0%) | 33 (44.6%) | 20 (76.9%) | 0.01 |
| Not answered | 4 | 1 | ||
| What type of ICU model does your hospital employ? | 0.95 | |||
| Closed unit | 9 (34.6%) | 18 (25.0%) | 7 (28.0%) | |
| Open unit with mandatory consult for intensive care specialist | 7 (26.9%) | 31 (43.1%) | 10 (40.0%) | |
| Open unit with multiple physicians or teams | 10 (38.5%) | 23 (31.9%) | 8 (32.0%) | |
| Not answered | 6 | 2 | ||
|
| ||||
| HOSPITAL CULTURE, LEADERSHIP, AND SAFETY | ||||
|
| ||||
| Barriers to resuscitation quality | ||||
| Lack of direct feedback - not/weak barrier | 14 (53.8%) | 45 (59.2%) | 17 (63.0%) | 0.55 |
| Not answered | 2 | |||
| Adequate resuscitation training (not a barrier or only mild barrier) | 19 (73.1%) | 62 (81.6%) | 24 (92.3%) | 0.06 |
| Not answered | 2 | 1 | ||
| Outdated/insufficient equipment- not/weak barrier | 22 (84.6%) | 63 (84.0%) | 25 (96.2%) | 0.13 |
| Not answered | 3 | 1 | ||
| Lack of support from senior administration - not/weak barrier | 24 (92.3%) | 65 (86.7%) | 24 (92.3%) | 0.72 |
| Not answered | 3 | 1 | ||
| Lack of an appropriate resuscitation champion- not/weak barrier | 17 (65.4%) | 58 (76.3%) | 24 (92.3%) | 0.02 |
| Not answered | 2 | 1 | ||
| Current institution culture- not/weak barrier | 20 (76.9%) | 60 (80.0%) | 23 (88.5%) | 0.26 |
| Not answered | 3 | 1 | ||
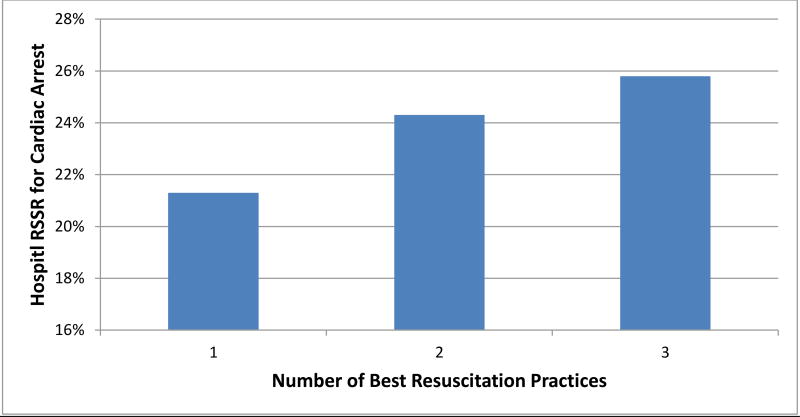
After multivariable adjustment, three resuscitation practices were independently associated with hospital rates of risk-standardized survival. Although fewer than 35% of hospitals routinely monitored for interruptions of chest compressions during an acute resuscitation, it was performed in more than half of the hospitals in the top survival quintile. As a result, hospitals that tracked interruptions in chest compressions had a more than 2-fold greater odds of being in a higher survival quintile category than hospitals that did not track cardiopulmonary resuscitation quality (adjusted odds ratio, 2.71 [95% CI: 1.24, 5.93]; P=0.01). Moreover, hospitals that reviewed their cardiac arrest cases monthly or quarterly had a more than 6-fold odds of being in a higher survival quintile category than hospitals that reviewed them less frequently than once quarterly (adjusted ORs of 8.55 [1.79, 40.0] for monthly review and 6.85 [1.49, 31.3] for quarterly review; P=03) (Table 3). Hospitals in which staff cited resuscitation training as adequate (i.e., not a barrier at all or only a weak barrier) had a greater than 3-fold odds of being in a higher survival quintile category compared with those where it was considered a moderate or severe barrier (OR, 3.23 [1.21, 8.33]=0.02). Notably, no new hospital practices were identified as significant predictors when we repeated the analyses with hospital risk-standardized survival rates modeled as a continuous variable rather than as quintile groups. Finally, risk standardized survival rates for hospitals implementing 1, 2, or all 3 of these strategies (all hospitals implemented at least one strategy) were 21.3% ± 5.5%, 24.3% ± 5.3%, and 25.8% ± 4.2%, respectively (Figure 2).
Table 3. Adjusted Associations Between Hospital Factors and Risk-Standardized Survival Rates for In-Hospital Cardiac Arrest.
The proportional odds model examines the association between resuscitation practices and a hospital’s likelihood of having risk-standardized survival rates in the next highest quintile category. For instance, a hospital strategy with an odds ratio of 1.50 would indicate that hospitals employing that strategy had 50% greater odds of being in the top hospital survival quintile as compared with hospitals in the middle quintiles and of being in the middle quintiles as compared with the bottom quintile.
| Hospital Resuscitation Strategy or Factor | Adjusted Odds Ratio (95% CI) |
P value |
|---|---|---|
| Frequency of review of in-hospital cardiac arrest cases | ||
| Less than once quarterly | Reference | 0.03 |
| At least once monthly | 8.55 ( 1.79, 40.0) | |
| At least once quarterly | 6.85 (1.49, 31.3) | |
| Monitoring for interruptions of chest compressions | 2.71 (1.24, 5.93) | 0.01 |
| Adequate resuscitation training at one’s hospital (not a barrier or only mild barrier) | 3.23 (1.21, 8.33) | 0.02 |
| Monitoring of times to defibrillation | 1.89 (0.74, 4.83) | 0.18 |
| Frequency of immediate code debriefing | ||
| Not at all or <10% of all resuscitations | Reference | 0.65 |
| 10% to 49% of all resuscitation | 1.19 (0.44, 3.23) | |
| 50% to 100% of all resuscitation | 1.56 (0.61, 4.00) | |
| Presence of intensive care specialist in hospital ICUs at all times | 1.84 (0.84, 4.00) | 0.13 |
| Lack of resuscitation champion is a moderate to severe barrier at one's hospital | 0.56 (0.21, 1.49) | 0.25 |
Abbreviations: ICU, intensive care unit
Figure 2. Risk Standardized Survival Rates (RSSRs) for Hospitals Employing 1, 2, or all 3 Resuscitation Practices.
Discussion
Using data from acute care hospitals in the U.S. participating in a national registry, we identified three hospital resuscitation practices that were associated with higher hospital rates of survival for patients with in-hospital cardiac arrest. These strategies included frequent review of cardiac arrest cases, monitoring for interruptions of chest compressions during acute cardiopulmonary resuscitation, and staff’s global assessment of the adequacy of resuscitation training at their site. Other factors that have been suggested as potential innovations in resuscitation care, such as immediate debriefing after cardiopulmonary resuscitation, simulation training (‘mock codes’), dedicated resuscitation teams, use of intra-resuscitation monitoring devices, allowing non-critical care nursing staff to defibrillate patients, and patient to nurse ratio, were not associated with hospital rates of survival although the confidence intervals around some of these resuscitation practices were wide. Since risk-standardized survival rates varied substantially, our results provide initial insights into which resuscitation practices may distinguish hospitals with higher rates of survival for in-hospital cardiac arrest.
The emergence of GWTG-Resuscitation over the past 15 years has facilitated numerous studies describing the epidemiology and outcomes of in-hospital cardiac arrest.14–17 Beside these patient-level studies, several studies also have described site-level variation in survival.2, 18 Yet, the factors that distinguish top-performing hospitals in cardiac arrest survival from other hospitals were not defined in these studies since information linking resuscitation practices to outcomes has been difficult to obtain. Consequently, identification of best resuscitation practices has been recognized as the critical next step in in-hospital resuscitation research.6 To date, few studies have collected information on hospital resuscitation practices,19, 20 and none have evaluated the association between these practices and in-hospital cardiac arrest survival. By collecting information on hospital strategies for resuscitation care, we were able to extend the findings of prior studies and identify several hospital practices associated with higher cardiac arrest survival.
Although it makes intuitive sense that more frequent cardiac arrest review could be associated with higher hospital survival for in-hospital cardiac arrest, this relationship has not been previously assessed or quantified. In this study, nearly all hospitals in the highest survival quintile reviewed their in-hospital cardiac arrest cases at least once quarterly, and many on a monthly basis. In contrast, 1 in 6 hospitals in the lowest survival quintile reviewed their cardiac arrest cases infrequently, although these represented fewer than 10% of hospitals in the study sample. The process of cardiac arrest case review can identify gaps in resuscitation care and lead to quality improvement efforts to address these gaps. More frequent case review likely increases the efficiency of this feedback cycle and allows for more informative discussions when the cardiac arrest event is relatively recent.
Another strategy we identified—monitoring for interruptions of chest compressions during an acute resuscitation—was employed by fewer than 35% of hospitals, but by more than half of the hospitals in the top survival quintile. Studies in out-of-hospital cardiac arrest have highlighted the importance of minimizing interruptions in chest compressions during resuscitation care, and recent changes in advanced cardiac life support training reflect this emphasis.21 For in-hospital cardiac arrest, a prior study found that use of automated external defibrillators was not beneficial and potentially harmful, presumably because of longer periods of interruptions of chest compressions with deployment of the automated external defibrillator.22 Further study may be warranted to determine which method of providing feedback for interruptions of chest compressions may be most effective, but our findings suggest that the opportunity to improve may be great as nearly two-thirds of hospitals currently do not monitor this aspect of cardiopulmonary resuscitation quality.
Organizational factors and training have been cited as critical to performance in other conditions, such as door-to-balloon time for ST-segment elevation myocardial infarction.23, 24 In this study, we found hospitals in which staff cited adequate resuscitation training had higher cardiac arrest survival. Although we did not evaluate which specific aspects of resuscitation training and preparation optimize the delivery of acute cardiopulmonary resuscitation and post-resuscitation care, our findings highlight that a quick survey of staff perception of adequacy of resuscitation training may be an important routine screen by hospital leadership in identifying gaps in their staff’s preparedness and comfort in treating patients with in-hospital cardiac arrest.
Our study should be interpreted in the context of the several considerations. Our study may have been underpowered to evaluate some of the hospitals strategies. For instance, in the multivariable model, immediate debriefing after resuscitation was not significantly associated with hospital survival. However, hospitals which conducted immediate debriefing in at least half of their in-hospital cardiac arrests had an adjusted OR of 1.56, and there was a suggestion of a dose-response curve (see Table 3). Moreover, although we found that the requirement of a dedicated specialist physician 24 hours a day 7 days a week in intensive care units was associated with higher hospital rates of survival on bivariate analysis (with 77% of hospitals in the top quintile employing this strategy as compared to 50% or less in the other two hospital categories), this strategy was no longer significantly associated with better survival after multivariable adjustment but had a large estimate of effect (OR of 1.82) and a P-value of 0.12. Further study of several of these resuscitation practices in a larger hospital sample may be warranted to look for their targeted impact on outcomes.
In addition, although three hospital strategies were identified, further prospective studies are needed to demonstrate that their dissemination is associated with improved hospital survival, especially in hospitals in the lower quintiles. Development of tools to improve the frequency and content of cardiac arrest case reviews, facilitate monitoring for interruptions of chest compressions, and enhance resuscitation training among hospital staff, will be critically important to validate these best practices, as we demonstrated associations but not causality, and these practices may be markers of other aspects of resuscitation care. Moreover, as any dissemination strategy to introduce a new behavior involves disruption of existing behaviors, confirmation of the benefits of each of these strategies will be critical.
Our study had other key limitations that affect its interpretation. First, the survey data were reported by a single respondent in collaboration with other staff at the hospital, and the reported policies and practices were not independently confirmed. However, survey respondents were liaisons to the GWTG-Resuscitation registry and were therefore among the most likely individuals to evaluate their institution’s resuscitations practices. Moreover, inaccurate responses would be expected to be non-differential and bias findings toward the null, reinforcing the validity of our positive associations. Second, our study population was limited to hospitals participating in GWTG-Resuscitation and our findings may not apply to non-participating hospitals. Specifically, the prevalence of some resuscitation strategies may be lower in non-participating hospitals and the prevalence of perceived resuscitation barriers may be higher, although GWTG-Resuscitation does represent a diverse set of U.S. hospitals with a broad spectrum of hospital risk-standardized survival rates. Third, although the estimates of effect for monthly and quarterly cardiac arrest case reviews were statistically significant, the wide confidence intervals suggest imprecision on the strength of that association. Finally, some strategies may be important in specific institutions but not necessarily across the full sample due to contextual effects unique to that hospital; therefore, our results should not inhibit innovations that may be effective in particular settings.
In conclusion, using survey information from acute care hospitals participating in a national quality improvement registry, we identified three resuscitation strategies associated with higher hospital rates of survival for patients with in-hospital cardiac arrest. These strategies can form the foundation for best practices for resuscitation care at hospitals, given the high incidence and variation in survival for in-hospital cardiac arrest.
Supplementary Material
Acknowledgments
Funding/Support:
Drs. Chan (K23HL102224 and 1R01HL123980) and Nallamothu (1R01HL123980) are supported by grants from National Heart Lung and Blood Institute.
GWTG-Resuscitation is sponsored by the American Heart Association, which had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The manuscript is reviewed and approved by the GWTG-Resuscitation research and publications committee prior to journal submission.
Footnotes
Disclosures: None of the authors have any financial disclosures or conflicts of interest to disclose
Authorship: Dr. Chan had full access to all of the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Chan, Nallamothu
Acquisition, analysis, or interpretation of data: Chan, Krein, Tang, Iwashyna, Harrod, Kennedy, Lehrich, Kronick, Nallamothu
Drafting of the manuscript: Chan, Nallamothu
Critical revision of the manuscript for important intellectual content: Chan, Krein, Tang, Iwashyna, Harrod, Kennedy, Lehrich, Kronick, Nallamothu
Statistical analysis: Tang
Obtained funding: Chan, Nallamothu
Administrative, technical, or material support: Chan, Krein, Harrod, Kennedy, Lehrich, Nallamothu
Study supervision: Chan, Nallamothu
References
- 1.Merchant RM, Yang L, Becker LB, et al. Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med. 2011;39:2401–2406. doi: 10.1097/CCM.0b013e3182257459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chan PS, Berg RA, Spertus JA, et al. Risk-standardizing survival for in-hospital cardiac arrest to facilitate hospital comparisons. J Am Coll Cardiol. 2013;62:601–609. doi: 10.1016/j.jacc.2013.05.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strategies to Improve Cardiac Arrest Survivial: A Time to Act. Institute of Medicine; Washington, D.C.: 2015. [Google Scholar]
- 4.Kirkbright S, Finn J, Tohira H, Bremner A, Jacobs I, Celenza A. Audiovisual feedback device use by health care professionals during CPR: a systematic review and meta-analysis of randomised and non-randomised trials. Resuscitation. 2014;85:460–471. doi: 10.1016/j.resuscitation.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 5.Edelson DP, Litzinger B, Arora V, et al. Improving in-hospital cardiac arrest process and outcomes with performance debriefing. Arch Intern Med. 2008;168:1063–1069. doi: 10.1001/archinte.168.10.1063. [DOI] [PubMed] [Google Scholar]
- 6.Chan PS, Nallamothu BK. Improving outcomes following in-hospital cardiac arrest: life after death. JAMA. 2012;307:1917–1918. doi: 10.1001/jama.2012.3504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 8.Cummins RO, Chamberlain D, Hazinski MF, et al. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital 'Utsteinstyle' American Heart Association. Circulation. 1997;95:2213–2239. doi: 10.1161/01.cir.95.8.2213. [DOI] [PubMed] [Google Scholar]
- 9.Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110:3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 10.Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS. Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2012;367:1912–1920. doi: 10.1056/NEJMoa1109148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldstein H. Multilevel Statistical Models. London and New York: Edward Arnold; Wiley; 1995. [Google Scholar]
- 12.Goldstein H. Multilevel Statistical Models. 3. London: 2003. Free 2nd Edition: http://www.ats.ucla.edu/stat/examples/msm_goldstein/goldstein.pdf: Arnold Publishers. [Google Scholar]
- 13.R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing V; Austria: 2008. URL http://www.R-project.org. [Google Scholar]
- 14.Chan PS, Krumholz HM, Nichol G, Nallamothu BK. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358:9–17. doi: 10.1056/NEJMoa0706467. [DOI] [PubMed] [Google Scholar]
- 15.Chan PS, Nichol G, Krumholz HM, et al. Racial differences in survival after in-hospital cardiac arrest. JAMA. 2009;302:1195–1201. doi: 10.1001/jama.2009.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Girotra S, Chan PS. Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2013;368:680–681. doi: 10.1056/NEJMc1215155. [DOI] [PubMed] [Google Scholar]
- 17.Goldberger ZD, Chan PS, Cooke CR, Hayward RA, Krumholz HM, Nallamothu BK. Duration of resuscitation efforts and survival after in-hospital cardiac arrest - Authors' reply. Lancet. 2013;381:447. doi: 10.1016/S0140-6736(13)60241-X. [DOI] [PubMed] [Google Scholar]
- 18.Merchant RM, Berg RA, Yang L, Becker LB, Groeneveld PW, Chan PS. Hospital variation in survival after in-hospital cardiac arrest. J Am Heart Assoc. 2014;3:e000400. doi: 10.1161/JAHA.113.000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Finn JC, Jacobs IG. Cardiac arrest resuscitation policies and practices: a survey of Australian hospitals. The Medical journal of Australia. 2003;179:470–474. [PubMed] [Google Scholar]
- 20.Edelson DP, Yuen TC, Mancini ME, et al. Hospital cardiac arrest resuscitation practice in the United States: a nationally representative survey. J Hosp Med. 2014;9:353–357. doi: 10.1002/jhm.2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meaney PA, Bobrow BJ, Mancini ME, et al. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation. 2013;128:417–435. doi: 10.1161/CIR.0b013e31829d8654. [DOI] [PubMed] [Google Scholar]
- 22.Chan PS, Krumholz HM, Spertus JA, et al. Automated external defibrillators and survival after in-hospital cardiac arrest. JAMA. 2010;304:2129–2136. doi: 10.1001/jama.2010.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bradley EH, Curry LA, Spatz ES, et al. Hospital strategies for reducing risk-standardized mortality rates in acute myocardial infarction. Ann Intern Med. 2012;156:618–626. doi: 10.1059/0003-4819-156-9-201205010-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bradley EH, Curry LA, Webster TR, et al. Achieving rapid door-to-balloon times: how top hospitals improve complex clinical systems. Circulation. 2006;113:1079–1085. doi: 10.1161/CIRCULATIONAHA.105.590133. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.