Abstract
Objectives
A randomized controlled study was conducted with 422 homeless, stimulant-using G/B men and 29 transgender women (N=451) to assess two community-based interventions to reduce substance abuse and improve health: (a) a nurse case-managed program combined with contingency management (NCM + CM) versus (b) standard education plus contingency management (SE + CM).
Study Design
Hypotheses tested included: a) completion of hepatitis A/B vaccination series; b) reduction in stimulant use; and c) reduction in number of sexual partners.
Methods
A deconstructive cost analysis approach was utilized to capture direct costs associated with the delivery of both interventions. Based on an analysis of activity logs and staff interviews, specific activities and the time required to complete each were analyzed as follows: a) NCM + CM only; b) SE + CM only; c) Time to administer/record vaccines; and d) Time to receive and record CM visits. Cost comparison of the interventions included only staffing costs and direct cash expenditures.
Results
The study outcomes showed significant over time reductions in all measures of drug use and multiple sex partners, compared to baseline, although no significant between-group differences were detected. Cost analysis favored the simpler SE + CM intervention over the more labor-intensive NCM + CM approach. Because of the high levels of staffing required for the NCM relative to SE, costs associated with it was significantly higher.
Conclusions
Findings suggest that while both intervention strategies were equally effective in achieving desired health outcomes, the brief SE + CM appeared less expensive to deliver.
Keywords: Community Participatory Research, Gay, Homelessness, Substance Use/Abuse
Introduction
Homeless gay and bisexual (G/B) men and transgender women (GBT hereafter) represent a highly vulnerable population in the United States (US) because of their unstable living arrangements, unprotected sexual behaviors, and engagement in drug use.1–3 It is estimated that 30–45% of GBT young adults may be homeless.4 In one study among homeless men who have sex with men (MSM; N=20), 25% have reported engaging in unprotected receptive anal intercourse, less than a quarter (20%) reported unprotected insertive anal intercourse, 15% reported unprotected vaginal intercourse and over half (65%) reported a positive urine drug test.1 GBT populations in the US have unique risk factors for homelessness which include running away from their families and/or the foster care system due to experiencing stigma related to their sexual orientation4, 5 or early abuse in the home.6
Once on the streets, challenges to meet necessities lead many to engage in street currency (e.g., survival sex).2, 3 As a result, one of the main public health concerns for this group is the risk of contracting hepatitis B Virus (HBV), a disease which is vaccine-preventable.7, 8 Yet, the rate of infection remains high, resulting in high costs in treating hepatitis-related liver diseases.
According to Centers for Disease Control and Prevention,9 the leading causes of HBV infections among adults in the US include homosexual activity, injection drug use (IDU), and having two or more sexual partners. The presence of other behavioral and health problems such as alcohol abuse, non-injection drug use, or HIV/AIDS often contribute to the aggravation of the liver disease.10, 11
There are many barriers to improve health care services to these “hidden” populations in the US.12, 13 In recent years, however, researchers and service providers have begun to investigate different strategies to overcome these barriers and reach out to these populations. For instance, two strategies which have been explored in reducing drug use among G/B men include contingency management (CM) and cognitive behavioral therapy (CBT).14–17 CM often includes different forms of incentives such as vouchers, goods, or services that are intended to reinforce positive behavior, and has been found to be effective in reducing substance abuse.18 CM was also found to be more effective in reducing methamphetamine use and protected receptive anal intercourse among G/B men in comparison to CBT.16 After a 24-week intervention with substance-dependent homeless MSM, Reback et al.14 revealed that participants in CM provided significant more urine sample that were free of stimulant metabolites than the control group.
Nyamathi and colleagues have also been investigating various nurse-led community intervention programs that tailor to the needs of the homeless population who are often involved in drug use and at risk for HBV. These programs included nurse-peer teams which were designed to incorporate protective strategies, improve coping, provide linkages with community resources.19, 20 and increase the hepatitis vaccination completion rates and knowledge levels.21, 22
The main purpose of the present study was to conduct a cost analysis of two community-based intervention strategies: (a) nurse case management plus contingency management (NCM + CM); and (b) the standard education plus contingency management (SE + CM) designed to: a) complete HAV/HBV vaccination; b) reduce stimulant use; and c) reduce number of sexual partners at four- and eight-month evaluation post intervention. For this paper, the goal was to calculate costs associated with the delivery of each intervention model relative to their respective treatment outcomes. We hypothesized that greater personal attention through nurse case management, coupled with contingency management, i.e., NCM+CM, compared to SE+CM, would also lead to higher costs in service delivery for the anticipated intervention outcomes.
Methods
Design
This study was based on the results of a randomized controlled trial (RCT) conducted with gay and bisexual men and transgender women to assess of the impact of two community-based intervention strategies on the following intervention outcomes: a) completion of HAV/HBV vaccination; b) reduction in stimulant use; and c) reduction in number of sexual partners at four- and eight-month evaluation post intervention. In this paper, costs associated with the delivery of each intervention model relative to their respective treatment outcomes were calculated. This study was approved by UCLA’s and Friend’s Research Institute’s Institutional Review Boards (IRB) and registered with the Clinical Trials protocol registration system: NCT00926146.
Sample and Setting
Our study targeted non-heterosexual populations, which are typically neglected in mainstream public health programs. The resulting sample included 451 homeless, stimulant-using G/B men and transgender women. The purpose of this study was to explore how historically discriminated and neglected populations may respond to rather mainstream public health interventions.
Eligibility criteria included: a) age 18–46; b) self-reported being homeless; c) G/B man or transgender woman; d) used stimulants within the previous three months (confirmed by urinalysis or by hair analysis if the urine screening could not detect a stimulant metabolite); and e) no self-reported participation in drug treatment in the last 30 days. Exclusion criteria included: a) monolingual speakers of languages other than English or Spanish; and b) persons judged to be cognitively impaired by the research staff. This was assessed by asking the individual to repeat critical aspects of the design and procedures of the study as reported during the consenting process.
In our study, 997 individuals were assessed for eligibility. Ninety-one declined to participate in the study. In total, 455 were excluded from the study because they were not between 18 to 46 years old (n=120), not gay or bisexual (n=90), not male to female transgender (n=29), had a negative hair sample (n=86), reported no stimulant use within last 3 months (n=63), not homeless (n=23), and other reasons (n=44). Homelessness was defined as not having a regular place to live, but instead had to stay in a shelter, abandoned building, all-night theater, car, outdoors, or other such places. The community site in which the research was conducted was located in a sex-work district in West Hollywood, California, and provided drop in services for this this gay and bisexual population.
Procedures
Following IRB clearances, trained research staff posted flyers announcing the study in West Hollywood, and presented information regarding the nature of the study to potential participants. Based on the flyer posting, location at the community research site and times when the research staff were at the research site was provided. Interested persons then met the research staff privately at the research site to receive more detailed information. Thereafter, written informed consent was obtained by the Project Director or approved designee in a private room at the research site followed by a question and answer session. Once the participant provided informed consent, a two-minute screening was administered by trained staff to assess eligibility for the study.
If participants were eligible for the study, a blood sample was tested for HBV and HCV, and a rapid HIV test was conducted. Research staff asked participants to return to receive results provided by the study nurse. Upon this return visit that occurred within 7–10 days, a second informed consent was administered followed by a baseline assessment. A total of 451 stimulant-using (methamphetamine, amphetamine, and cocaine) participants were enrolled in the study.
In this RCT design, eligible participants were randomly assigned by computer assignment to two community-based intervention conditions: a) NCM + CM; or b) SE + CM. Among the 451 enrolled, 227 were randomized to NCM + CM and 224 to SE + CM programs by using URN randomization23, stratifying on age (18 vs. 29 vs. 30–46), ethnicity (white vs. non-White) and HBV status (negative vs. positive). The NCM + CM intervention consisted of eight 20-minute case management meetings, delivered by a nurse in a private space at the study site, and eight hepatitis-focused health education sessions over a 16 week period, delivered by a trained peer health educator in a similar private area at the study site. The NCM sessions were delivered one-on-one and focused on the relationship between drug use and unprotected sexual behaviors, HIV, HBV, and HCV. The importance of completing the HAV/HBV Twinrix vaccine was also encouraged. Moreover, the nurse provided counseling to enrolled participants with a focus on positive emotional support and personal empowerment.
The eight hepatitis-focused health education sessions were delivered by trained peer community educator staff, each 20 minutes in length with typically 4–5 participants, and emphasized the promotion of strategies to reduce risk of hepatitis and HIV. Those assigned to the SE + CM group received a 20-minute standard health education provided by a health educator that focused on the importance of condom use and other means of protection against HIV, HBV, and HCV, including the importance of completing the HAV/HBV vaccination. Nearly two-thirds of the NCM + CM participants (144/227 [63 %]) completed all eight NCM sessions, while 148/227 (65 %) completed all eight hepatitis-focused health education sessions. Almost all SE + CM participants (222/224 [99 %]) completed the brief education session.
Assessments at 4- and 8- month follow-ups included a questionnaire and drug urine analysis. The 4-month follow-up was limited to a 2-month period, while the 8-month follow-up was conducted over several months to find participants who were difficult to locate. Participants received $10 to complete the screening questionnaire, $20 to complete the baseline questionnaire, and $30 and $35 to complete the 4- and 8-month evaluations.
Contingency Management (CM) program
The same CM reinforcement and payout schedule was provided to participants in both programs in which a progressive contingency schedule24 was provided wherein participants received a $2.50 voucher for the first urine sample that was negative for stimulant metabolites, with an incremental increase of $1.25 for each subsequent negative urine sample for stimulant metabolites. Three-weekly urine samples were required each week for the 16 weeks on Tuesdays, Thursdays, and Saturdays. Stimulant-free urines added voucher points that could be redeemed for merchandise selected by the participant. When positive tests for a stimulant metabolite was revealed, or for participants who did not submit a urine sample, voucher points were not accumulated and their subsequent voucher value was reduced to the initial $2.50. However, a rapid reset procedure enabled participants to return to their pre-positive test result after three clean urine test results. The maximum value that participants could earn for all urines that tested negative was $444.
Measures and Cost Elements
Sociodemographic factors
The participants self-reported their gender identity and sexual orientation on the screener and the baseline questionnaire.
Vaccination
The HAV/HBV Twinrix vaccine were offered free of charge to all study participants regardless of group assignment. Moreover, the importance of completing the vaccine series was encouraged in both interventions. The cost of each vaccine was $44; each participant would receive a maximum of three vaccines, plus a booster, thus, the total maximum cost for the series was $176 per participant if they were eligible to be vaccinated. As we later acknowledged in the limitation section towards the end, our direct cost accounting method obviously left out many other cost-relevant items, such as in-kind contributions, voluntary services, shared costs in public facilities, and subsidized services. These costs items were important for cost analysis. However, our treatment setting and partnering agencies were unable to provide such accounting information or adequate specifics that would allow us to attach dollar values for cost analysis. It should be noted that not all study participants were eligible for vaccination. Only participants not carrying hepatitis surface antibodies were eligible for vaccination.
Drug use based on urinalysis drug
In addition to the CM intervention that included the provision of urine specimens three times a week for 12 weeks, urine specimens were requested as well at the 4- and 8-month follow-up evaluations to assess recent stimulant use (i.e., methamphetamine, amphetamine, and cocaine) via radio immune assays. The temperature strip on the test cup ensured that the sample is at body temperature and not a substitute to avoid any manipulation by the participant. A 5-panel FDA-approved urine test cup (Phamatech, Inc.) was used in this study. The test cup screened for metabolites of the following drugs: Amphetamines (1000 ng/mL), Cocaine (300 ng/mL), Methamphetamines/MDMA (500 ng/mL), Opiates (2000 ng/mL), and THC (50 ng/mL). The test kit cost $3.15 each and was paid for by the NIH grant. The cost of administering urinalysis by the project staff was included in the staff time.
Number of sexual partners
This study relied on self-reports by study participants on the number of sexual partners at baseline, and then at 4- and 8-month follow-up periods. Multiple sexual partners was assessed by asking how many different men in total have you had sex with in the past 30 days, including your primary partner if you have one. Responses were coded as 0 (0–1 partner) or 1 (2 or more partners).
Cost data elements
Our accounting strategy was to capture two main groups of expenses: a) actual cash expenditures, either used to procure incentives such as gift cards or bus tokens, or paid directly to participants; and b) salaries and benefits of the staff who were directly involved in the delivery of the services. These expenditures are what we call “direct costs”, services and activities that were monetarized and recorded somewhere.
Staff salary and benefits cost calculation
While relatively straightforward in payroll records, the actual allocation of the intervention staff costs (hence cost of personnel) was based on the differential amounts of time spent on specific activities. Staffing cost consisted of salaries and fringe benefits. Depending on their job classification, e.g., registered nurse, program manager, licensed vocational nurse, peer educators, their salary and benefits varied. The presence of nurse case management was the only major difference between the staffing between the two intervention conditions. Subjects from both intervention conditions were received and followed up by the same site staff, with the exception of the nurse case management component, which only occurred to the NCM+CM group.
In this staffing cost calculation exercise, we used a deconstruction method to break down the amount of time the staff spent on all key clinical activities, and then applied the overall personnel costs proportional to these accounted times.25 In other words, these specific clinical activities thus became the anchoring events used to account for the total amount of personnel costs. Based on an analysis of activity logs and staff interviews, specific activities and the time required to complete each of them were as follows:
Nurse case management (NCM + CM only): maximum of 8 sessions, and 20 minutes each for a total of 160 minutes;
Standard group education (SE + CM only): maximum of 1 session for 20 minutes;
Time to administer/record vaccines: maximum of 4 and 10 minutes each; and
Time to receive and record CM visits: maximum of 36 visits, and 10 minutes each or a total of 360 minutes.
This time also included activities such as scheduling for interventions, reminder calls, making copies, and other miscellaneous office chores. We lumped these activities into this one broad category.
Results
Sample Demographics
A total of 451 stimulant-using (methamphetamine, amphetamine, and cocaine) participants were enrolled in the study. Total sample size completing the 4-month evaluation was 352 (79%) while 398 (90%) completed the 8-month follow-up interview. Due to the shorter observation time, slightly fewer participants were located at the 4-month timeframe than the 8-month period, which allowed additional time to track down the enrolled participants for the 2nd follow-up interview.
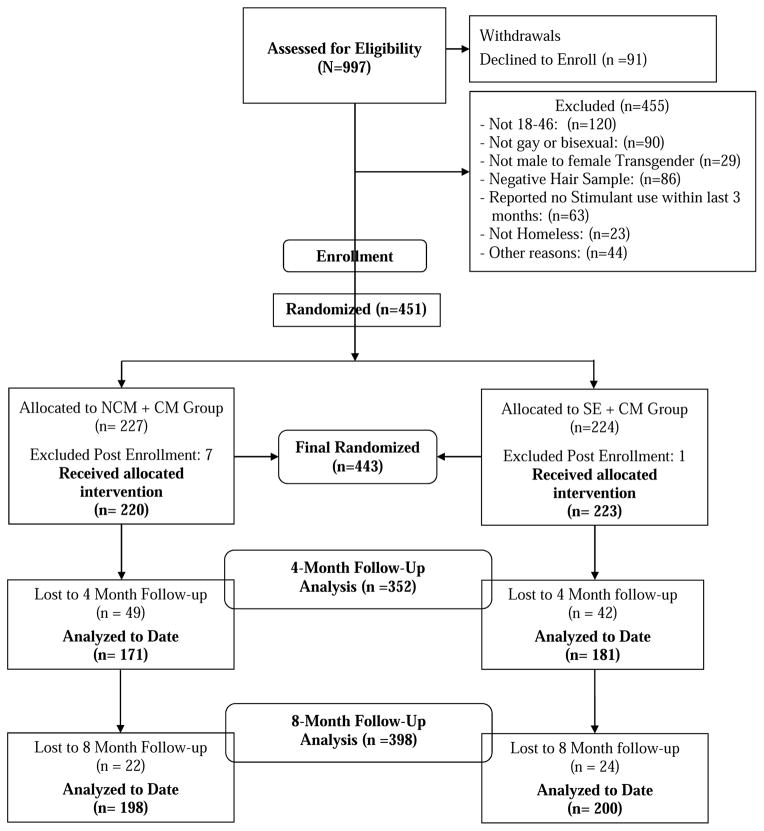
To ensure that the randomized assignment procedure worked properly, a series of tests of equivalence were carried out between the two groups on all socio-demographic characteristics and urinalysis test results assessed using chi-square tests (categorical variables) and t and Wilcoxon two-sample tests (continuous variables). No significant differences were detected between the two groups, except for marginally significant variations in time of being homeless (p=.04) and stay in shelters (p=.06). These differences were controlled at baseline. CONSORT diagram is depicted in Figure 1.
Figure 1.
CONSORT flow Diagram
As shown in Table 1, participants were predominantly African American/black and Caucasian/white, with fewer Hispanics/Latinos and persons of other race/ethnicities. Both groups of participants had very similar ages (Mean = 34.31 years of age) and levels of education (Mean = 12.17 years). About one in four reported having a partner. Over half (60.5%) spent at least a week in the prior month living on the street.
Table 1.
Sample Characteristics by Intervention (N = 451)
| Baseline Measure | NCMa+CMb | SE+CMb | Total | Pc | ||
|---|---|---|---|---|---|---|
| n = 227 | n = 224 | n = 451 | ||||
|
| ||||||
| n | % | N | % | % | ||
| Race/ethnicity | 0.61 | |||||
| African American/black | 82 | 36.12 | 86 | 38.39 | 37.25 | |
| Caucasian/white | 80 | 35.24 | 79 | 35.27 | 35.25 | |
| Hispanic/Latino | 30 | 13.22 | 35 | 15.63 | 14.41 | |
| Mixed | 21 | 9.25 | 13 | 5.80 | 7.54 | |
| Other | 14 | 6.17 | 11 | 4.91 | 5.54 | |
| Age (Mean, SD) | 34.04 | 8.1 | 34.57 | 8.3 | 34.31 | 0.58 |
| Education (Mean, SD) | 12.06 | 2.3 | 12.27 | 2.2 | 12.17 | 0.42 |
| Partnered | 62 | 27.31 | 50 | 22.32 | 24.83 | .22 |
| On Street ≥ 1 wkd | 148 | 65.20 | 125 | 55.80 | 60.53 | .04 |
| In shelter ≥ 1 wkd | 24 | 10.57 | 37 | 16.52 | 13.53 | .06 |
| Positive for HBV | 122 | 53.74 | 105 | 46.88 | 50.33 | .14 |
| Positive for HIV | 38 | 16.96 | 34 | 15.60 | 16.29 | .70 |
| Drug Dependence: | ||||||
| Methamphetamine | 200 | 91.74 | 191 | 87.21 | 89.47 | .12 |
| Cocaine | 130 | 59.63 | 123 | 56.16 | 57.89 | .46 |
| Amphetamines | 84 | 38.53 | 77 | 35.16 | 36.84 | .47 |
| Ever injected drugs: | .47 | |||||
| Yes, past 30 days | 73 | 32.16 | 76 | 33.93 | 33.04 | |
NCM = nurse case management.
CM = case management.
Two-sample t or Wilcoxon test.
The month before baseline.
Close to 90% of the participants used methamphetamine; and 33% of the participants injected drugs in the month prior to the baseline interview. Over half (50.3%) were positive for HBV while fewer than one third (30.2%) were positive for HCV. Slightly over 16% were found to be HIV positive. Injection drug use (IDU) in the past month was reported by one-third (33%) of the participants.
Key Outcomes
Table 2 shows the rate of vaccination, stimulant use, and multiple sexual partners. On all three key outcome measures, both intervention strategies seemed to produce sizeable impacts. Following the baseline interviews, 170 were found eligible for vaccination. Of those, about 85% of these eligible participants in both groups completed the three-dose series during the intervention periods. Neither statistically significant nor substantive differences were found in the breakdowns of either the number of participants or vaccines received between the two groups. On the measure of illicit drug use, sizeable reductions were achieved across both intervention strategies between baseline and subsequent two time points (i.e., 4- and 8-months). For instance, UA results showed that while more than 70% of both groups tested positive for methamphetamine use at baseline, less than 30% were positive at 8-months. While more than 38% of the participants in both groups reported having sex with multiple partners at baseline, the percentage decreased to 17.28% for the NCM + CM participants and 21.59% for the SE + CM participants at the 8-months.
Table 2.
Vaccination, Drug Use and Sexual Partners at 8 Months
| Baseline | 4 Months | 8 months | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| N | % | N | % | N | % | Pb | |
| Vaccines Received | |||||||
| NCM + CM (n=78)a | N/A | N/A | 67 | 85.9 | |||
| SE + CM (n=92)a | N/A | N/A | 78 | 84.8 | |||
| Drug Use (Urine Testc): | |||||||
| Cocaine | |||||||
| NCM + CM (n=135) | 43 | 31.85 | 8 | 5.93 | 14 | 10.37 | .001 |
| SE + CM (n=141) | 47 | 33.33 | 11 | 7.80 | 10 | 7.09 | .001 |
| Methamphetamine | |||||||
| NCM + CM (n=135) | 99 | 73.33 | 28 | 20.74 | 33 | 24.44 | .001 |
| SE + CM (n=141) | 102 | 72.34 | 40 | 28.37 | 42 | 29.79 | .001 |
| Amphetamine | |||||||
| NCM + CM (n=135) | 67 | 49.63 | 24 | 17.78 | 29 | 21.48 | .001 |
| SE + CM (n=141) | 69 | 48.74 | 33 | 23.40 | 35 | 24.82 | .001 |
| Multiple Sexual Partners (2or more based on Self Reports) | |||||||
| NCM + CM (n=162) | 63 | 38.89 | 37 | 22.84 | 28 | 17.28 | .001 |
| SE + CM (n=176) | 67 | 38.07 | 35 | 19.89 | 38 | 21.59 | .001 |
Notes:
Participants eligible for vaccination;
For change over time based on log-linear modeling chi-square test;
subjects who provided urine samples at all three time points.
Cash Expenditures Related to Intervention Activities
For all the CM cash payment and the cost of acquiring vaccines, the total amount of cash expenditures for the entire study sample was $111,062 (M=$246.26; SD=$175.86), ranging from a low of $30.00 to the maximum of $715 per study subject. The amount of direct cash (or cash equivalent) spent on program activities were about the same for both groups of participants with neither statistical nor substantive significant differences.
An independent-samples t-test was conducted to compare the NCM + CM and SE + CM participants on the following variables: number of vaccines received, cost for vaccines used, assessment cash payment at intake, locator update cash payment, cash incentives for referrals, number of contingency visits, CM cash payout. No significant differences were detected between the two groups on all outcome variables, except for CM incentive payout. There was a marginally significant difference on CM cash payout between the NCM + CM participants (M=$96.17; SD=$130.33) and SE + CM participants (M=$119.93; SD=$148.61); t=1.81, p < .10 (two-tailed). On average, SE + CM participants made more CM visits (M=15.36; SD=12.92) than NCM + CM participants (M=13.67; SD=12.12). When all cash expenditures were summed up, our t-test (two-tailed) revealed significant difference between the NCM + CM participants (M=$229.56; SD=161.27) and the SE + CM participants (M=$263.18; SD=188.36) with t=2.04 and p< .05, indicating that the SE + CM participants had a higher participation in the CM-specified activities.
Accounting Staff Salaries and Benefits
Detailed accounting was carried out on actual salary figures, associated benefits, and the level of time commitment (i.e., full time equivalence or FTE) of the staff directly involved in the intervention activities. For the entire four years of intervention, most personnel costs were incurred in Year 2 and 3, during which slightly more than three full-time staff were directly involved in the delivery of the services. Salary and fringe benefit figures were obtained directly from the human resource department overseeing the financial operation of the study, thus reflecting the different levels of salary packages, benefits, and other compensations associated with each staff member’s HR classification.
The total actual salaries and benefits of $456,028 were distributed in proportion to the amount of time spent on all key clinical activities or anchoring events as discussed earlier. Table 3 shows that in sum NCM + CM participants consumed a total of 85,975 minutes of staff time (with M= 378.74; and SD=207.62) for their activities. In comparison, SE + CM participants consumed a total of 41,520 minutes of staff time (with M=185.36; and SD=133.33). It was clear that the NCM + CM program consumed approximately twice the amount of staff time as the SE + CM participants, or a ratio of 2.04 to 1.
Table 3.
Staff Time (in Minutes) Spent on Study Activities
| Group A (N=227) | Group B (N=224) | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Range | Mean | Std. Dev. | Sum | Mean | Std. Dev. | Sum | |
| Nurse-led Education Sessions | 0~8 | 6.17 | 2.67 | 1,400 | -- | -- | -- |
| Total Nurse-Led Education Minutes | 0~160 | 123.35 | 53.44 | 28,000 | -- | -- | -- |
| Total Nurse Case Management Minutes | 0~160 | 108.44 | 50.99 | 24,615 | -- | -- | -- |
| Control Group Education (minutes) | 0~20 | -- | -- | -- | 20.00 | .000 | 4,480 |
| Number of Vaccines Received+ | 1~4 | 2.97 | .82 | 232 | 2.86 | .82 | 263 |
| Time to Administer/Record Vaccinations (Minutes) | 10~40 | 29.74 | 8.21 | 2,320 | 28.59 | 8.20 | 2,630 |
| Number of Contingency Management (CM) Visits | 0~36 | 13.67 | 12.12 | 3,104 | 15.36 | 12.92 | 3,441 |
| Time to Receive/Record CM Visits (Minutes) | 0~360 | 136.74 | 121.17 | 31,040 | 153.61 | 129.15 | 34,410 |
| Total Minutes Spent on Study Participants* | 10~695 | 378.74 | 207.62 | 85,975 | 185.36 | 133.33 | 41,520 |
Notes: +78 NCM + CM participants and 92 SE + CM participants received vaccinations.
t=11.75; p< .000 (two-tailed).
Cost Comparison of the Two Interventions
As shown in Table 4, for the entire project over the four years in operation, a total of $111,062 in cash expenditures was spent on activities for both groups and another $456,028 on salaries and benefits for the staff. Within these two grand totals, $52,110 was spent on NCM + CM in cash expenditures and $58,952 for SE + CM. Based on the allocation of time proportionate to the time spent on key intervention activities, NCM + CM accounted for $306,182.58 of the wages and benefits spent on the staff, while SE + CM accounted for $149,845.42. On an annualized basis (i.e., by smoothing the fluctuations over the four years), the average cash expenditure per participant for NCM + CM was $57.39 compared to $65.79 per participant in SE + CM. However, the average wages and benefits were $337.21 per participant in the NCM + CM versus $167.24 in the SE + CM.
Table 4.
Cost Summary
| NCM + CM | SE + CM | |||
|---|---|---|---|---|
|
| ||||
| 4-Year Total | Per Participant | 4-Year Total | Per Participant | |
| Cash Expenditures 3 | $52,110.00 | $229.56 | $58,952.00 | $263.18 |
| Personnel | $306,182.58 | $1,348.82 | $149,845.42 | $668.95 |
| Total | $358,292.58 | $1,578.38 | $208,797.42 | $932.13 |
Because vaccination is a major public health strategy focused on reducing infectious diseases, the rate of vaccination among high-risk populations can be perceived as a major health care saving measure in public policy. According to the Hepatitis B Foundation, of all approved chronic HBV therapies, the cost of treatment (i.e., Lamivudine) starts from the lowest of $2,918 (adjusted to 2012 dollars) a year per patient to the highest of $28,214 (adjusted to 2012 dollars) a year for Interferon alfa-2b (30–35 million IU) (Hepatitis B foundation, undated). By contrast, the SE + CM program cost only $233 a year per participant, or $394 per participant for the more intensive NCM + CM. In either case, the cost of administering these two intervention modalities as designed and deployed in this study was far less expensive in terms of achieving desired vaccination and behavioral outcomes. Moreover, our cost analysis suggests that the less labor intensive SE + CM program may be as effective as the more intensive intervention.
Discussion
Homeless GBT persons are at increased risk of infectious diseases, and as a “hidden” population, they face barriers to accessing healthcare services. The prevalence of chronic HBV infection in the US is estimated to be between 0.8 to 1.4 million.26 Chesson et al.27 estimated that the direct medical cost of outpatient treatment for symptomatic acute HBV infection to be $272 per occurrence and the cost of hospitalization for symptomatic HBV infection is $8,080 per occurrence. For chronic HBV infection, direct cost of treatment is estimated to be $59,308.27 If a liver transplant is needed, the cost would rise to $163,438.28 The total charges by hospitalization (exclusive of physician charges) for HBV in the U.S. increased from $357 million in 1990 to $1.5 billion in 2003; it then plateaued at $1.3 billion.29 Therefore any community-based strategies in delivering healthcare services to this “hidden” population can help us understand better how to reach these GBT persons, and perhaps reduce their risk of catching infectious diseases such as HAV/HBV.
In this paper, we analyzed the operational cost of two community-based intervention strategies that focused on completion of the HAV/HBV vaccination series, reducing stimulant use and the multiple sexual partners. Outcomes from both community-based interventions appeared to support the value of both culturally sensitive and community-tailored behavioral intervention programs as implemented in this study, irrespective of the treatment modality. Both treatment approaches produced equivalent reduction in all key outcome indicators. Since averting HBV infections is very valuable, a small decrease in drug use and number of partners may be worth the efforts, whichever the intervention might be.
Findings from this study suggest that, for this particular population, an initial contact and recruitment interactions were perhaps an effective method of introducing them to the healthcare and vaccination services. Those receptive to the idea of vaccines and relevant knowledge from the brief health education would be amenable to behavioral changes, provided there are concrete financial incentives to keep them engaged for a period of time. Those non-responsive participants would probably require different intervention strategies.
The simpler, less expensive approach in the SE + CM intervention can also improve efficiency in an urban environment, such as Los Angeles, where multiple community-based intervention agencies can be deployed to reach the many pockets of hard-to-reach populations who may engage in high risk behaviors and have limited access to routine healthcare services. In such urban contexts, a brief public health education session coupled with CM may be sufficient to deliver the same level of quality service and achieve similar outcomes as the more labor and staff-intensive NCM + CM strategy.
Limitations
This study is not without its limitations; therefore, findings must be interpreted with caution. First, one shortcoming of the design was the absence of an intervention modality without the contingency management. Both interventions had the identical CM component, which perhaps was the single most important factor contributing to the similar treatment outcomes. Without a reference group that differed from both SE + CM and NCM + CM, we were unable to tease out the influence of CM.
Second, although the vaccines used in this study were provided free of charge to all program participants, such a practice may have limited generalizability in social contexts where public funding may be lacking.
Third, there are several complementary approaches to perform an economic evaluation of healthcare interventions (e.g., cost-effectiveness analysis, cost-utility analysis, benefit-cost analysis).30 Some researchers consider the value of all resources used in providing a treatment program, which includes in-kind contributions, subsidized resources, and voluntary services.31 Such indirect and intangible sources that may benefit a community health program include shared facilities and utilities, in-kind contributions, and volunteer time.30 It may be conceptually desirable to include both direct and indirect costs associated with the implementation of a program; however, such a valuation scheme demands a careful documentation of every source that has benefitted a program and be converted into dollar values. Our collaborating community agency simply did not keep records of any such services nor indirect costs that may be converted into cash values. As a result, we were only able to capture direct costs associated with the interventions under evaluation.
Fourth, one of our main outcome variables was self-reported multiple sexual partners, however, out interview instrument did not explore further on the characteristics of the sexual encounters/partners. Without greater details on the nature of these sexual partners, the use of “multiple sexual partners” was a crude and imprecise way to gauge exposure to potential infectious disease.
Fifth, our study was targeting gay, bisexual and transgender populations, who are often neglected in mainstream community-based public health programs. In total, 29 transgender women were part of our sample. We decided not to separate our sample into finer subgroups, such as transgender women, gay men, and bisexual men, because our proposed study was interested in exploring how these historically discriminated and neglected populations may respond to mainstream public health interventions. Future research should explore how subpopulations of different sexual orientations may respond variedly to mainstream public health programs, which are designed mostly by heterosexuals for heterosexuals.
Finally, our study and most background literature cited in this paper were from the US. Therefore findings from this study may not be generalizable to any other countries.
Conclusions
While our nurse-led case management and standard care were deployed according to the random assignment procedure, we were unable to implement a no-incentive component into this study. In this study, we found that while significant improvement in key outcomes was detected over the two time points in data collection, no significant differences were found between the two treatment conditions. For instance, a high rate of vaccination (about 85% among all eligible participants in both groups) was achieved. Such a high vaccination rate may be attributed to a combination of CM and the fact the study site was conveniently located in the community facility frequented by the target population. However, our current study design was inadequate to pinpoint the main cause for the observed outcome.
This was because our study was carried in a community-based treatment center, and it was impractical to withhold cash incentives from control subjects while encouraging all subjects to participate in the baseline intake and subsequent series of vaccination. As a result, we applied the same CM reward system to both the treatment and control groups, thus creating a situation where both groups had an identical overlap in intervention modality, i.e., cash incentives. In other words, for practical and ethical considerations, we were unable to present two very different treatment modalities to the two assigned conditions.
Although we observed a drop in all outcome measures across both groups, we were unable to tease out what might have contributed to the treatment outcomes. In the light of the fact that CM has been found to be effective in encouraging treatment participation in many clinical settings as reviewed in the literature, we speculate that it was the CM that was the most effective component or at least assume its effects were constant in both across intervention models. Future research should explore ways, where permitted for ethical considerations, to remove the CM component or drastically alter the incentive structure to create significantly different reward systems. On the other hand, one may also speculate that both NCM and SE were equally effective in producing the observed outcomes, while holding the CM factor constant. Our current student design was unable to answer this question.
Further study or further analysis may also be warranted to extend beyond the intended RCT design, as reported here in this paper. Instead, for exploratory purposes, the entire sample can be put through multivariate regression analyses to establish the profiles and mediating covariates that may have played varied roles in influencing the outcomes and pinpoint when/for whom a more labor-intensive intervention may work better. In adhering to our original design, our analysis did not go beyond a strict RCT comparison. Future analysis may go beyond the scope of an RCT design to provide different treatment and nuanced examination of the two different treatment protocols. For example, one can follow the mediation model to examine how responding differed across groups among individuals who had lower participation in CM-specific activities. Furthermore, future study can take into account of intermediating covariates, such as reductions in substance use (or use of one specific substance) may lead to increased participation in vaccination.
Highlights.
Compared two programs on reduction of drug use among gay, bisexual men and transgender women
Cost analysis approach was utilized to capture direct costs associated with the delivery of both programs
Cost analysis favored the simpler program over the more labor-intensive approach.
Footnotes
Author Disclosures
This study was funded by the National Institute on Drug Abuse, Grant No. R01DA016147.
This study is registered with the Clinical Trials protocol registration system: NCT00926146
Financial Disclosures: None
Ethical Review Board Disclosure: Approval to conduct research with human subjects was obtained from the respective institutional review boards
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Reback CJ, Kamien JB, Amass L. Characteristics and HIV risk behaviors of homeless, substance-using men who have sex with men. Addict Behav. 2007;32:647–54. doi: 10.1016/j.addbeh.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 2.Whitbeck LB, Chen X, Hoyt DR, Tyler KA, Johnson KD. Mental disorder, subsistence strategies, and victimization among gay, lesbian, and bisexual homeless and runaway adolescents. J Sex research. 2004;41:329–42. doi: 10.1080/00224490409552240. [DOI] [PubMed] [Google Scholar]
- 3.Tyler KA. A comparison of risk factors for sexual victimization among gay, lesbian, bisexual, and heterosexual homeless young adults. Violence Vict. 2008;23:586–602. doi: 10.1891/0886-6708.23.5.586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Durso LE, Gates GJ. Serving Our Youth: Findings from a National Survey of Service Providers Working with Lesbian, Gay, Bisexual, and Transgendered Youth who are Homeless or At Risk of Becoming Homeless. Los Angeles: The Williams Institute with True Colors Fund and The Palette Fund; 2012. [Google Scholar]
- 5.Keuroghlian AS, Shtasel D, Bassuk EL. Out on the street: a public health and policy agenda for lesbian, gay, bisexual, and transgender youth who are homeless. Am J Orthopsychiatry. 2014;84:66–72. doi: 10.1037/h0098852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rew L, Whittaker TA, Taylor-Seehafer MA, Smith LR. Sexual health risks and protective resources in gay, lesbian, bisexual, and heterosexual homeless youth. J Spec Pediatr Nurs. 2005;10:11–9. doi: 10.1111/j.1088-145x.2005.00003.x. [DOI] [PubMed] [Google Scholar]
- 7.Alter MJ. Protecting future generations through immunization against hepatitis B. Ann Intern Med. 2001;135:835–6. doi: 10.7326/0003-4819-135-9-200111060-00013. [DOI] [PubMed] [Google Scholar]
- 8.Mast EE, Margolis HS, Fiore AE, Brink EW, Goldstein ST, Wang SA, et al. A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP) part 1: immunization of infants, children, and adolescents. MMWR Recomm Rep. 2005;54:1–31. [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention; Hepatitis DoV, editor. Viral Hepatitis Surveillance. Atlanta, GA: National Center for HIV/AIDS, Viral Hepatitis, STD & TB Prevention; 2011. [Google Scholar]
- 10.Vaccine Preventable Illness: Hepatitis B. Saint Paul, MN: 2013. Immunization Action Coalition. [Google Scholar]
- 11.Zuckerman AJ. In: Chapter 70 Hepatitis Viruses. SB, editor. Galveston, TX: University of Texas Medical Branch; 1996. [PubMed] [Google Scholar]
- 12.Spicer SS. Healthcare needs of the transgender homeless population. Journal of Gay & Lesbian Mental Health. 2010;14:320–39. [Google Scholar]
- 13.Lim FA, Brown DV, Jr, Justin Kim SM. CE: Addressing Health Care Disparities in the Lesbian, Gay, Bisexual, and Transgender Population: A Review of Best Practices. Am J Nurs. 2014;114:24–34. doi: 10.1097/01.NAJ.0000450423.89759.36. [DOI] [PubMed] [Google Scholar]
- 14.Reback CJ, Peck JA, Dierst-Davies R, Nuno M, Kamien JB, Amass L. Contingency management among homeless, out-of-treatment men who have sex with men. J Subst Abuse Treat. 2010;39:255–63. doi: 10.1016/j.jsat.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Menza TW, Jameson DR, Hughes JP, Colfax GN, Shoptaw S, Golden MR. Contingency management to reduce methamphetamine use and sexual risk among men who have sex with men: a randomized controlled trial. BMC Public Health. 2010;10:774. doi: 10.1186/1471-2458-10-774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shoptaw S, Reback CJ, Peck JA, Yang X, Rotheram-Fuller E, Larkins S, et al. Behavioral treatment approaches for methamphetamine dependence and HIV-related sexual risk behaviors among urban gay and bisexual men. Drug Alcohol Depend. 2005;78:125–34. doi: 10.1016/j.drugalcdep.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 17.Shoptaw S, Reback CJ, Larkins S, Wang PC, Rotheram-Fuller E, Dang J, et al. Outcomes using two tailored behavioral treatments for substance abuse in urban gay and bisexual men. J Subst Abuse Treat. 2008;35:285–93. doi: 10.1016/j.jsat.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 18.Secades-Villa R, Garcia-Fernandez G, Pena-Suarez E, Garcia-Rodriguez O, Sanchez-Hervas E, Fernandez-Hermida JR. Contingency management is effective across cocaine-dependent outpatients with different socioeconomic status. J Subst Abuse Treat. 2013;44:349–54. doi: 10.1016/j.jsat.2012.08.018. [DOI] [PubMed] [Google Scholar]
- 19.Nyamathi AM, Marlow E, Branson C, Marfisee M, Nandy K. Hepatitis A/B vaccine completion among homeless adults with history of incarceration. J Forensic Nurs. 2012;8:13–22. doi: 10.1111/j.1939-3938.2011.01123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nyamathi A, Dixon EL, Wiley D, Christiani A, Lowe A. Hepatitis C virus infection among homeless men referred from a community clinic. West J Nurs Res. 2006;28:475–88. doi: 10.1177/0193945906286620. [DOI] [PubMed] [Google Scholar]
- 21.Nyamathi A, Liu Y, Marfisee M, Shoptaw S, Gregerson P, Saab S, et al. Effects of a nurse-managed program on hepatitis A and B vaccine completion among homeless adults. Nurs Res. 2009;58:13–22. doi: 10.1097/NNR.0b013e3181902b93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nyamathi A, Branson C, Kennedy B, Salem B, Khalilifard F, Marfisee M, Getzoff D, Leake B. Impact of nursing interventions on decreasing substances among homeless youth. Am J Addictions. 2012;21:558–65. doi: 10.1111/j.1521-0391.2012.00288.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. J Stud Alcohol Suppl. 1994;12:70–5. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- 24.Higgins ST, Budney AJ, Bickel WK, Foerg FE, Donham R, Badger GJ. Incentives improve outcome in outpatient behavioral treatment of cocaine dependence. Arch Gen Psychiatry. 1994;51:568–76. doi: 10.1001/archpsyc.1994.03950070060011. [DOI] [PubMed] [Google Scholar]
- 25.Zhang SX, Roberts ELR, McCollister KE. An economic analysis of the in-prison therapeutic community model on prison management costs. J Criminal Justice. 2009;37:388–95. [Google Scholar]
- 26.Wilkins T, Zimmerman D, Schade RR. Hepatitis B: diagnosis and treatment. Am Fam Physician. 2010;81:965–72. [PubMed] [Google Scholar]
- 27.Chesson HW, Blandford JM, Gift TL, Tao G, Irwin KL. The estimated direct medical cost of sexually transmitted diseases among American youth, 2000. Perspect Sex Reprod Health. 2004;36:11–9. doi: 10.1363/psrh.36.11.04. [DOI] [PubMed] [Google Scholar]
- 28.van der Hilst CS, Ijtsma AJ, Slooff MJ, Tenvergert EM. Cost of liver transplantation: a systematic review and meta-analysis comparing the United States with other OECD countries. Med Care Res Rev. 2009;66:3–22. doi: 10.1177/1077558708324299. [DOI] [PubMed] [Google Scholar]
- 29.Kim WR. Epidemiology of hepatitis B in the United States. Hepatology. 2009;49:S28–34. doi: 10.1002/hep.22975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McCollister KE, French MT, Inciardi JA, Butzin CA, Martin SS, Hooper RM. Post-release substance abuse treatment for criminal offenders: A cost effectiveness analysis. J Quantitative Criminology. 2003;19:389–407. [Google Scholar]
- 31.Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-effectiveness in health and medicine. Oxford, UK: Oxford University Press; 1996. [Google Scholar]