Abstract
Background
Sphenopalatine ganglion is the largest collection of neurons in the calvarium outside of the brain. Over the past century, it has been a target for interventional treatment of head and facial pain due to its ease of access. Block, radiofrequency ablation, and neurostimulation have all been applied to treat a myriad of painful syndromes. Despite the routine use of these interventions, the literature supporting their use has not been systematically summarized. This systematic review aims to collect and summarize the level of evidence supporting the use of sphenopalatine ganglion block, radiofrequency ablation and neurostimulation.
Methods
Medline, Google Scholar, and the Cochrane Central Register of Controlled Trials (CENTRAL) databases were reviewed for studies on sphenopalatine ganglion block, radiofrequency ablation and neurostimulation. Studies included in this review were compiled and analyzed for their treated medical conditions, study design, outcomes and procedural details. Studies were graded using Oxford Center for Evidence-Based Medicine for level of evidence. Based on the level of evidence, grades of recommendations are provided for each intervention and its associated medical conditions.
Results
Eighty-three publications were included in this review, of which 60 were studies on sphenopalatine ganglion block, 15 were on radiofrequency ablation, and 8 were on neurostimulation. Of all the studies, 23 have evidence level above case series. Of the 23 studies, 19 were on sphenopalatine ganglion block, 1 study on radiofrequency ablation, and 3 studies on neurostimulation. The rest of the available literature was case reports and case series. The strongest evidence lies in using sphenopalatine ganglion block, radiofrequency ablation and neurostimulation for cluster headache. Sphenopalatine ganglion block also has evidence in treating trigeminal neuralgia, migraines, reducing the needs of analgesics after endoscopic sinus surgery and reducing pain associated with nasal packing removal after nasal operations.
Conclusions
Overall, sphenopalatine ganglion is a promising target for treating cluster headache using blocks, radiofrequency ablation and neurostimulation. Sphenopalatine ganglion block also has some evidence supporting its use in a few other conditions. However, most of the controlled studies were small and without replications. Further controlled studies are warranted to replicate and expand on these previous findings.
Electronic supplementary material
The online version of this article (10.1186/s10194-017-0826-y) contains supplementary material, which is available to authorized users.
Keywords: Sphenopalatine ganglion, Block, Radiofrequency ablation, Neurostimulation, Nerve stimulation, Neuromodulation
Review
The sphenopalatine ganglion (SPG) is also known as pterygopalatine ganglion, nasal ganglion or Meckel’s ganglion. It is the largest and most superior ganglion of sensory, sympathetic and parasympathetic nervous system. It has the largest collection of neurons in the calvarium outside of the brain. It is also the only ganglion having access to the outside environment through the nasal mucosa. SPG gives rise to greater and lesser palatine nerves, nasopalatine nerve, superior, inferior and posterior lateral nasal branches, as well as the pharyngeal branch of the maxillary nerve. There are also orbital branches reaching the lacrimal gland.
Because of its proximity to multiple important neuroanatomic structures in pain perception, SPG has been postulated to be involved in facial pain and headaches for over a century. For headache, SPG is thought to play a central role in the generation of trigeminal autonomic cephalalgia (TAC). TAC is a broad term that encompasses cluster headache, paroxysmal hemicrania, and short-lasting unilateral neuralgiform headache attack with conjunctival injection and tearing (SUNCT). It is typically distributed in the trigeminal distribution with ipsilateral cranial autonomic features. TAC is characterized by parasympathetic (lacrimation, rhinorrhea, nasal congestion and edema) activation and sympathetic dysfunction (ptosis and miosis). These clinical features can be explained by the activation of the sympathetic and parasympathetic pathways within SPG [1]. The disruption of this pathway by SPG blockade is thought to be central to relieving the headache produced by TAC. For face and neck neuralgias, connections of SPG with facial nerve, lesser occipital nerve and cutaneous cervical nerves are thought to be the mechanism [1]. Irritation of the SPG can also cause orbital, periorbital and mandibular symptoms through its connection with the ciliary and otic ganglions and reflex otalgia by its connection with the tympanic plexus. Connections of SPG with the vagus nerve may produce visceral symptoms in dysfunctional states [1]. SPG may also play an important role in vasodilation to protect the brain against ischemia from stroke or migraine with aura. This mechanism is thought to be through the postganglionic parasympathetic fibers, which are connected to the vascular beds of the cerebral hemisphere [2]. Because the upper cervical roots are connected to the superior cervical ganglion through the sympathetic trunk, which is connected to the deep petrosal nerve then to the SPG, SPG blockade is thought to be able to relieve pain from the head, face, neck and upper back [1]. This is the rationale for using SPG block in treating any head, face, neck pain refractory to conventional treatment. Through the inhibition of the sympathetic trunk, SPG block was also thought to be useful in treating generalized muscle pain including fibromyalgia and low back pain [3]. For postdural puncture headache, the pain mechanism is thought to be secondary to cerebrospinal fluid leak that exceeds the production rate, causing traction on the meninges and parasympathetic mediated reflex vasodilatation of the meningeal vessels. SPG blockade is thought to work through blocking the parasympathetic flow to the cerebral vasculature, allowing the cerebral vessels to return to normal diameter, thus relieving the headache [4].
Although the mechanism by which pain is produced from SPG is not well-characterized, SPG has been the treatment target ranging from cluster headache to low back pain. Three main types of interventions are currently available: chemical nerve block/lysis, radiofrequency ablation and neurostimulation. Some of these interventions are commonly performed in interventional pain clinics for treatment of headache resistant to conservative measures. Despite their use, the level of evidence for using SPG interventions varies widely across a myriad of conditions.
In this systematic review, we sought to systematically collect the evidence supporting the use of these SPG interventions in treating various painful conditions. We also summarized the level of evidence for each condition and intervention.
Methods
Protocol
This systematic review applies the guidelines issued in the latest Preferred Reporting Items for Systematic Reviews and Meta-Analysis (Additional file 1: PRISMA).
Information sources
The electronic databases of PubMed (https://www.ncbi.nlm.nih.gov/pubmed/), Cochrane Central Register of Controlled Trials (CENTRAL, www.cochranelibrary.com), Google Scholar (https://scholar.google.com/) were searched to identify relevant articles. Additionally, references within eligible papers were screened for additional articles.
Literature search strategy
The search was conducted in May 2017. The search strategy was based on the Population, Intervention, Comparator, Outcome (PICO) framework and was conducted to find studies on sphenopalatine ganglion block, radiofrequency ablation and neurostimulation. Population (P) was defined as patients suffering from any medical condition; intervention (I) was limited to sphenopalatine ganglion block, sphenopalatine radiofrequency ablation, and sphenopalatine ganglion neurostimulation; patients receiving interventions were compared (C) to preintervention status, patients without treatment or healthy controls; the outcome (O) needed to either qualitatively or quantitatively measure the reduction in disease severity with intervention. The complete entered search strategy in PubMed was: “(sphenopalatine) AND ganglion) AND block” for sphenopalatine ganglion block; “(sphenopalatine) AND ganglion) AND radiofrequency” for radiofrequency ablation; and (sphenopalatine AND ganglion AND neurostimulation) OR (sphenopalatine AND ganglion AND neuromodulation).
Eligibility criteria and study selection
To be included in this review, studies had to meet the following criteria: 1. The study sample was human. 2. Interventions must be SPG block, SPG radiofrequency ablation or SPG neurostimulation. 3. Articles had to be written in English. 4. Full-Text articles had to be available. 5. Conference abstracts and reviews were excluded.
Data items and collection
The following items were compiled in the evidence tables for SPG block (Table 2-12): first author, year of publication, medical condition treated, approach, imaging modality, medication used for the procedure, number of cases, study design and outcome. For radiofrequency ablation, the following additional items were collected: radiofrequency ablation temperature, type of radiofrequency ablation, parameter used and how to identify the correct position of the radiofrequency cannula/probe. For neurostimulation, the following additional items were collected: type of stimulator, type of stimulation and how to identify the correct position.
Table 2.
Studies with evidence level above case series in SPG block, radiofrequency ablation and neurostimulation
| Evidence level above case series | ||||||||
|---|---|---|---|---|---|---|---|---|
| Author | Year | Medical problems | Approach | Imaging | Medication | Number of cases | Study design | Outcome |
| SPG Block | ||||||||
| Berger et al. [32] | 1986 | Low back pain | Cotton tip applicator and transnasal needle | None | Cocaine or lidocaine | 7 cases with cocaine, 7 cases with lidocaine, 7 controls | Case-control | No statistical significance between cases and controls |
| Slade et al. [51] | 1986 | Tear secretion with topical anesthesia | Needle injection, through the greater palatine foramen | None | 2% lidocaine | 10 | Case-control (using self as control) | Tear secretion significantly reduced by 73% (p < 0.001) |
| Henneberger et al. [36] | 1988 | Nicotine addiction | Cotton tipped applicator, transnasal approach | None | Bupivacaine, cocaine or saline | 6 with bupivacaine, 5 with cocaine, 6 with saline | Double-blind placebo-controlled | Significantly fewer symptoms of discomfort for patients in the anesthetic treatment groups than placebo group |
| Silverman et al. [37] | 1993 | Experimentally induced pain (submaximal effort tourniquet test) | Cotton tipped applicator | None | 20% lidocaine and epinephrine | 16 healthy volunteers | Double-blind, cross-over study | No significant difference between experimental and placebo group. |
| Scudds et al. [3] | 1995 | Chronic muscle pain syndrome | Cotton tipped applicator, transnasal approach | None | 4% lidocaine | 42 with fibromyalgia, 19 with myofascial pain syndrome | Double-blind randomized controlled | No statistical significance between 4% lidocaine and placebo |
| Janzen et al. [30] | 1997 | Myofascial pain syndrome and fibromyalgia | Nasal spray | None | 4% lidocaine | 42 with fibromyalgia, 19 with myofascial pain syndrome | Double-blind, placebo-controlled | No statistical significance between 4% lidocaine and placebo |
| Ferrante et al. [31] | 1998 | Myofascial pain syndrome of the head, neck and shoulders | NA | None | 4% lidocaine | 13 cases, 7 controls | Double-blind, placebo-controlled, crossover design | No statistical significance |
| Costa et al. [6] | 2000 | Cluster headache (nitroglycerin induced) | Cotton tipped applicator, transnasal approach | None | 10% cocaine or 10% lidocaine | 6 episodic CH, 9 chronic CH | Double-blind, placebo-controlled, | All patients with induced pain responded to cocaine after 31.3 min and lidocaine after 37 min |
| Hwang et al. [23] | 2003 | Removal of nasal packing after nasal operation | Needle injection into the greater palatine canal | None | 1% lidocaine | 11 | Case-control | Injection side had significantly lower pain than the control side |
| Kanai et al. [11] | 2006 | Second division trigeminal neuralgia | Nasal spray | None | Lidocaine | 25 | Randomized control | Significantly decreased pain with intranasal lidocaine spray |
| Ahmed et al. [18] | 2007 | Sinonasal surgery intraoperative isofluorane consumption, hypotensive agents used, postoperative pain | Bilateral SPG block, injected between the middle and inferior turbinates | None | 0.5% lidocaine and epinephrine. | 15 cases, 15 controls | Randomized-controlled | Significantly reduced intraoperative isofluorane consumption and esmolol use, postoperative tramadol use and postoperative pain. |
| Ali et al. [20] | 2010 | Endoscopic trans-nasal resection of pituitary adenoma, anesthetic, vasodilator and analgesic sparing effect | Bilateral SPG block, injected between the middle and inferior turbinates | None | 1.5% lidocaine and epinephrine | 15 cases and 15 controls | Randomized-controlled | Significantly reduced in sevoflurane and nitroglycerine consumption, emergence time, postoperative pain and need of meperidine analgesia. |
| Cho et al. [17] | 2011 | Endoscopic sinus surgery postoperative analgesia efficacy | Transoral, through the greater palatine foramen | None | 0.25% bupivacaine with epinephrine | 60 | Double-blind randomized, placebo-controlled | Pain not significantly different from control |
| Kesimci et al. [22] | 2012 | Endoscopic sinus surgery postoperative analgesia efficacy | Bilateral SPG block, injected between the middle and inferior turbinates | None | 0.5% bupivacaine or 0.5% levobupivacaine | 45 | Double-blind randomized, placebo-controlled | Postoperative pain significantly reduced, also significantly few patients requiringadditional analgesics in the postoperative 24 h. |
| Demaria et al. [21] | 2012 | Endoscopic sinus surgery postoperative analgesia efficacy | Bilateral SPG block, palatal approach | None | 2% lidocaine and 1% tetracaine | 70 | Double-blind randomized, placebo-controlled | Patients were discharged sooner than the control group. The block group also required less total fentanyl in the recovery room. |
| Cady et al. [15] | 2015 | Chronic migraine | Tx360 | None | 0.5% bupivacaine | 38 | Double blind, placebo control | Significantly decreased headache at 24 h |
| Cady et al. [16] | 2015 | Chronic migraine | Repetitive block (twice a week) with Tx360 | None | 0.5% bupivacaine | 38 | Double blind, placebo control | No statistical difference at 1 month and 6 months between treatment and control groups. |
| Schaffer et al. [34] | 2015 | Acute anterior or global headache | Tx360 device | None | 0.5% bupivacaine | 93 | Randomized placebo-controlled | No statistically significant difference |
| Al-Qudah et al. [19] | 2015 | Endoscopic sinus surgery postoperative analgesia efficacy | Applied to the SPG region | None | 2% lidocaine and epinephrine | 60 (30 cases, 30 controls) | Double-blind, placebo controlled | Significant pain reduction in the SPG block group |
| Narouze et al. [38] | 2009 | Chronic cluster headache | Infrazygomatic approach | Fluoroscopy | NA | 15 | Prospective cohort | Mean attack intensity, mean attack frequency, pain disability index significant reduced at 1 year follow-up (P < 0.0005, P < 0.0003, P < 0.002, respectively) |
| SPG Neurostimulation | ||||||||
| Schoenen et al. [41] | 2013 | Cluster headache | ATI SPG stimulator positioned on the lateral-posterior maxilla medial to the zygoma. Customized, mean frequency 120.4 Hz, mean pulse width 389.7 us, mean intensity 1.6 mA | CT | – | 28 cases, with 3 randomized settings. | Randomized controlled | Pain relief achieved in 67.1% of full stimulation-treated attacks compared to 7.4% of sham-treated attacks. P < 0.0001 |
| Jurgens et al. [42] | 2016 | Cluster headache | Neurostimulator, described in Schoenen et al. [41] | CT | – | 33 cases | Cohort study. Long-term follow-up from [41] | 61% of patients were either acute responder (>50% relief from moderate or greater pain) or frequency responder (>50% in attack frequency) at 24 months |
| Barloese et al. [43] | 2016 | Cluster headache | Neurostimulator, described in Schoenen et al. [41] | CT | – | 33 cases | Cohort study. Long-term follow-up from [41] | 30% experienced at least 1 episode of complete attack remission (attack-free period exceeding 1 month) |
Table 12.
Studies of SPG blocks for other syndromes
| Other syndromes | ||||||||
|---|---|---|---|---|---|---|---|---|
| Author | Year | Medical problems | Approach | Imaging | Medication | Number of cases | Study design | Outcome |
| Byrd et al. [73] | 1930 | “Remote dysfunctions” | Cotton tipped applicator, transnasal approach | None | 50% butyn | Over 2000 cases | Case series | Remote dysfunctions were arrested |
| Sparer et al. [74] | 1935 | Recurrent convulsive seizures associated with nasal pathology | Needle injection | None | Mixture of alcohol and novocaine | 3 | Case series | Cessation of seizures |
| Ruskin et al. [29] | 1946 | Muscle spasms and arthritic pain | Unknown | None | cocaine, novocaine or nupercaine | 68 | Case series | Pain partially or completely relieved with SPGB and intramuscular injections of ironyl and calcium ascorbate |
| Amster et al. [28] | 1948 | 4 migraine, 2 acute torticollis, 12 painful spastic shoulder, 2 intercostal neuritis, 3 herpes zosters, 4 persistent hiccups, 5 ureteral colic, 3 dysmenorrhea, 7 peripheral painful vascular spasm, 61 lumbosacral and sacroiliac pain | Cotton tipped applicator, transnasal approach | None | Nupercaine, pontocaine, monocaine | 103 | Case series | Relief of pain and spasm in 90% of cases |
| Ruskin et al. [75] | 1949 | Arthritic pain | Unknown | None | Unknown | 30 | Case series | Pain partially or completely relieved with SPGB and iron salt of the adenylic nucleotide |
| Slade et al. [51] | 1986 | Tear secretion with topical anesthesia | Needle injection, through the greater palatine foramen | None | 2% lidocaine | 10 | Case-control (using self as control) | Tear secretion significantly reduced by 73% (p < 0.001) |
| Henneberger et al. [36] | 1988 | Nicotine addiction | Cotton tipped applicator, transnasal approach | None | Bupivacaine, cocaine or saline | 6 with bupivacaine, 5 with cocaine, 6 with saline | Double-blind placebo-controlled | Significantly fewer symptoms of discomfort for patients in the anesthetic treatment groups than the placebo group |
| Silverman et al. [37] | 1993 | Experimentally induced pain (submaximal effort tourniquet test) | Cotton tipped applicator | None | 20% lidocaine and epinephrine | 16 healthy volunteers | Double-blind, cross-over study | No significant difference between experimental and placebo groups |
| Quevedo et al. [76] | 2005 | Complex regional pain syndrome involving the lower extremity | Cotton tip applicator, transnasal | None | 4% tetracaine | 2 | Case series | 50% pain reduction |
| Triantafyllidi et al. [77] | 2016 | Hypertension | Cotton tip applicator, transnasal | None | 2% lidocaine | 22 | Cohort study | Systolic blood pressure significantly decreased by 24 hrs and by 21-30 days |
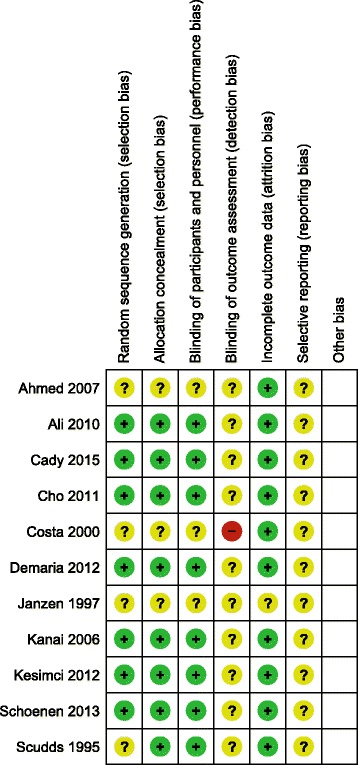
Risk of bias assessment
The quality of randomized-controlled studies was assessed using the 7-item criteria in Review Manager Software version 5.35 provided by the Cochrane Collaboration [5]. The 7-item criteria contained: (1) random sequence generation; (2) allocation concealment; (3) blinding of participants and personnel; (4) blinding of outcome assessment; (5) incomplete outcome data; (6) selective reporting and (7) other bias.
Analysis of evidence and recommendations
Level of evidence was graded based on Oxford Center for Evidence-based Medicine (1a: Systematic review of randomized-controlled trials. 1b: Individual randomized-controlled trials with narrow confidence interval. 2a: Systematic review of homogenous cohort studies. 2b: Individual cohort studies and low quality randomized-controlled trial. 3a: Systematic review of homogenous case-control studies. 3b: Individual case-control study. 4. Case series and poor-quality cohort and case-control studies. 5. Expert opinion. Grade of recommendation: A: Consistent level 1 studies. B: Consistent level 2 or 3 studies or extrapolations from level 1 studies. C: Level 4 studies or extrapolations from level 2 or 3 studies. D: Level 5 evidence or troublingly inconsistent or inconclusive studies of any level. Risk of bias in individual studies and across studies were not systematically assessed as most studies included in this review were case reports and case series.
Results
Overall summary
The result of the search process is provided in Fig. 1. 60 articles were included for SPG block, 15 articles for SPG radiofrequency ablation, and 8 articles for SPG neurostimulation.
Fig. 1.
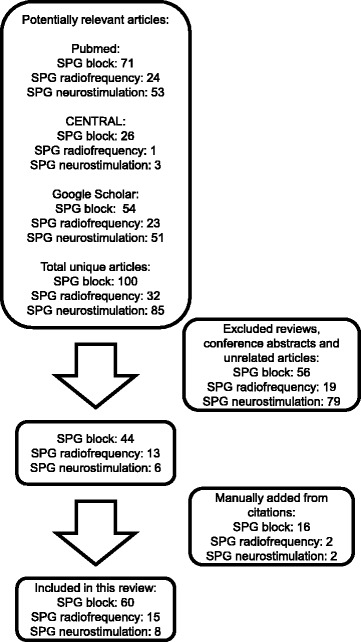
Overview of the systematic review process
The evidence levels and grades of recommendation for SPG block, radiofrequency ablation and neurostimulation are summarized in Table 1. Any study with evidence level above case series is included in Table 2. Risk of bias of randomized-controlled studies is summarized in Fig. 2. Most randomized-controlled studies included in this review have adequate randomization and blinding of participants and personnel.
Table 1.
Summary of evidence level and grade of recommendation for SPG block, radiofrequency ablation and neurostimulation
| Medical condition | Application/ Medication used in controlled studies | Number of controlled studies | Highest level of evidence | Grade of recommendation |
|---|---|---|---|---|
| SPG block | ||||
| Cluster headache | Cotton swab/cocaine or lidocaine | 1 | 2b | B |
| Second-division trigeminal neuralgia | Lidocaine spray | 1 | 2b | B |
| Reducing the needs of analgesics after endoscopic sinus surgery | Needle injection, transnasal and palatal approach/lidocaine,bupivacaine, levobupivacaine, tetracaine | 6 | 1b | B |
| Reducing the pain associated with nasal packing removal after nasal operation | Needle injection, infrazygomatic approach/lidocaine | 1 | 3b | B |
| Migraine | Tx360 device/ bupivicane | 1 | 2b | B |
| Postdural puncture headache, sphenopalatine maxillary neuralgia, facial neuralgia, sympathetic neuralgia, post-traumatic atypical facial pain, atypical odontalgia, pain from midline granuloma, herpetic keratitis, hemifacial headache,paroxysmal hemicrania, nasal pain, hemicrania continua, trigeminal neuropathy, cancer pain, seizures associated nasal pathology, arthritic pain and muscle spasm, intercostal neuritis, persistent hiccups, ureteral colic, dysmenorrhea, peripheral painful vascular spasm, complex regional pain syndrome and hypertension | Various protocols | 0 | 4 | C |
| Myofascial pain | Cotton-tipped applicator, nasal spray/lidocaine | 2 | 2b | Not recommended |
| SPG radiofrequency ablation | ||||
| Cluster headache | Infrazygomatic approach/80 °C, 60s ×2 | 0 (1 cohort study) | 2b | B |
| Sluder’s neuralgia, posttraumatic headache, chronic head and face pain, atypical trigeminal neuralgia, atypical facial pain, chronic facial pain secondary to cavernous sinus meningioma, trigeminal neuralgia, SPG neuralgia due to herpes zoster | Various protocols | 0 | 4 | C |
| SPG neurostimulation | ||||
| Cluster headache | Customized to each patient, mean frequency 120.4 ± 15.5 Hz, pulse width 389.7 ± 75.4 μs, intensity 1.6 ± 0.8 mA | 1 | 1b | B |
| Idiopathic facial pain, migraine | Various protocols | 0 | 4 | C |
Fig. 2.
Risk of bias summary of randomized-controlled studies
In the following sections, we will summarize the level of evidence and grades of recommendations by the type of SPG interventions and associated medical conditions.
Sphenopalatine ganglion block
Sixty articles were included for sphenopalatine ganglion block. Of the 60 studies, 11 were small randomized-controlled studies, and 1 was retrospective case-control study. The rest of the literature included case reports and case series. The type of blocking agent varied across studies, but they could be broadly put into three categories: cocaine, voltage-gated sodium channel blocker (local anesthetics), and a combination of voltage-gated sodium channel blocker and steroids. Voltage-gated sodium channel blocker is the most commonly used agent.
Cluster headache
There were nine articles on chronic cluster headaches collected through our literature search (see Table 3). One was a small double-blind placebo-controlled study (level 2b), six were case series and two were case reports (level 4, see Table 3). Costa et al. [6] reported a double-blind, placebo-controlled study using 15 cases of episodic and chronic cluster headaches. Cluster headache was induced with nitroglycerin, and SPG was treated with 10% solution of cocaine hydrochloride (1 ml, mean amount of application of 40-50 mg), 10% lidocaine (1 ml) or saline using a cotton swab previously immersed in these solutions. The cotton swab was placed in the region corresponding to the sphenopalatine fossa under anterior rhinoscopy. This was done in both the symptomatic and the non-symptomatic sides for 5 min. Patients treated with cocaine and lidocaine reported relief in 31.3 min in the cocaine group and 37 min for lidocaine group, compared to 59.3 min in the saline group. The side effect was mainly the unpleasant taste of lidocaine. This study was limited by its small number of participants, the acutely induced cluster headache from nitroglycerin, and its measure on only short-term outcome.
Table 3.
Studies of SPG block for cluster headache
| Cluster headache | ||||||||
|---|---|---|---|---|---|---|---|---|
| Author | Year | Medical problems | Approach | Imaging | Medication | Number of cases | Study design | Outcome |
| Devoghel et al. [52] | 1981 | Cluster headache | Needle injection. Supra-zygomatic approach | None | Pure alcohol | 120 | Case series | 85.8% had complete relief |
| Barre et al. [7] | 1982 | Cluster headache | Cotton swab. Applied to sphenopalatine foramen. Self-application if responded to treatment | None | 50 mg of cocaine flakes, then 10% and 5% cocaine solution | 11 | Case series | 10 out of 11 had 50-100% abortion rate in spontaneous headache |
| Kittrelle et al. [8] | 1985 | Cluster headache | Lidocaine directly dropped into the nostrils | None | 4% lidocaine | 5 | Case series | 4 of 5 patients obtained relief of nitrate-induced cluster headaches |
| Costa et al. [6] | 2000 | Cluster headache (nitroglycerin induced) | Cotton tipped applicator, transnasal approach | None | 10% cocaine or 10% lidocaine | 6 episodic CH, 9 chronic CH | Double-blind, placebo-controlled, | All patients with induced pain responded to cocaine after 31.3 min and lidocaine after 37 min |
| Felisati et al. [9] | 2006 | Chronic cluster headache | Endoscopic needle injection that approaches the pterygopalatine fossa by way of the lateral nasal wall | None | Triamcinolone acetonide, 1% bupivacaine and 2% mepivacaine with adrenaline | 21 | Case series | 11 out of 21 have improvement in symptoms |
| Yang et al. [53] | 2006 | Chronic cluster headache | Transnasal needle | Fluoroscopy | 0.2% Ropivacaine and triamcinolone | 1 | Case report | 60% pain relief |
| Pipolo et al. [10] | 2010 | Drug-resistant chronic cluster headache | Needle into the inferior portion of the sphenopalatine foramen (transnasal endoscopic technique-prasanna 1993 | None | 40 mg triamcinolone acetonide, 1% bupivacaine, 2% mepivacaine with adrenaline | 15 | Case series | 55% experience complete subsidence of CH symptoms |
| Zarembinski et al. [54] | 2014 | Drug-resistant chronic cluster headache, with Jacob’s disease | Sphenopalatine ganglion block via mandibular notch, then radiofrequency oblation. | Fluoroscopy, CT | 0.25% bupivacaine and 10 mg/ml dexamethasone | 1 | Case report | Pain significantly improved. |
| Kastler et al. [55] | 2014 | Cluster headache (14), persistent idiopathic facial pain (10), and other types of facial pain (18) | Infrazygomatic approach | CT | Absolute alcohol | 14 | Case series | 76.5% of patients have 50% pain relief at 1 month |
Other case reports/series using cocaine and local anesthetics as blocking agents generally reported good immediate outcomes for aborting acute cluster headache. One study using cocaine reported 10 out of 11 patients receiving 50-100% relief from spontaneous cluster headache [7], another study using lidocaine reported four out of five patients receiving relief from nitrate-induced cluster headache [8]. Because of the short-term relief from cocaine and lidocaine, steroid has been tried to prolong the relief provided by SPG block. In one case series, combination of triamcinolone, bupivacaine, mepivacaine and epinephrine helped improve severity and frequency of cluster headaches in 11 out of 21 patients [9]. The same cocktail helped 55% of the 15 treated patients in another case series [10].
In summary, SPG block has moderate evidence in treating cluster headache. The overall grade of recommendation is B for SPG block on cluster headache. The strongest evidence lies in aborting nitroglycerin-induced cluster headache using local application of cocaine or lidocaine with cotton swab through the transnasal approach. The side effect was mainly the unpleasant taste of lidocaine. Addition of steroid may provide longer relief, but the evidence remains weak (Grade C recommendation).
Trigeminal neuralgia
There were four articles on SPG block for trigeminal neuralgia through our literature search. One was a randomized-controlled study (level 2b), two were case series and one case report (level 4, see Table 4). Kanai et al. performed a randomized-controlled study with 25 participants with refractory second-division trigeminal neuralgia [11]. In this study, twenty-five patients with second-division trigeminal neuralgia were randomized to receive two sprays (0.2 ml) of either lidocaine 8% or saline placebo in the affected nostril using a metered-dose spray. The paroxysmal pain triggered by touching or moving face was assessed. Intranasal lidocaine 8% spray significantly decreased the paroxysmal pain for an average of 4.3 h. The side effects were limited to local irritation with burning, stinging or numbness of the nose and eye, and bitter taste and numbness of the throat. One case series [12] and one case report [13] reported immediate pain relief from nerve blocks with lidocaine and bupivacaine. One case series used a combination of dexamethasone and ropivacaine with the Tx360 applicator, which resulted in short-term pain relief [14]. Multiple blocks over time seemed to provide longer pain relief but it was restricted to isolated cases.
Table 4.
Studies of SPG block for trigeminal neuralgia
| Trigeminal neuralgia | ||||||||
|---|---|---|---|---|---|---|---|---|
| Author | Year | Medical problems | Approach | Imaging | Medication | Number of cases | Study design | Outcome |
| Peterson et al. [12] | 1995 | Trigeminal neuralgia | Cotton tip applicator | None | 4% lidocaine | 2 | Case series | Pain free |
| Manahan et al. [13] | 1996 | Trigeminal neuralgia | NA | None | Bupivacaine | 1 | Case report | Pain free |
| Kanai et al. [11] | 2006 | Second division trigeminal neuralgia | Nasal spray | None | Lidocaine | 25 | Randomized control | Significantly decreased pain with intranasal lidocaine spray |
| Candido et al. [14] | 2013 | Trigeminal neuralgia, chronic migraine headache, post-herpetic neuralgia | Tx360 Nasal applicator, transnasal | None | 0.5% ropivacaine and 2 mg dexamethasone | 3 | Case series | Satisfactory |
In summary, the overall grade of recommendation is B for SPG block on trigeminal neuralgia. The strongest evidence lies in treating with 8% lidocaine nasal spray in the affected nostril. The analgesia is effective but temporary (4.3 h). It is well-tolerated with side effects limited to local irritations. Addition of steroid and use of the Tx360 applicator may be useful but there has not been a controlled study.
Migraine
There was one small double-blind, placebo-controlled study and one long-term follow-up of the same study (level 2b), two case series and one case report (level 4, see Table 5). Cady et al. [15] reported a randomized-controlled study using the Tx360 device and bupivacaine to acutely treat chronic migraines with repetitive SPG blockade. 38 subjects with chronic migraines were included in the final analysis. Participants received a series of 12 SPG blocks with either 0.3 cm3 of 0.5% bupivacaine or saline delivered with the Tx360® through each nostril, over a 6-week period (2 SPG blocks/week). SPG block was found to be effective in reducing the severity of migraines up to 24 h. However, repetitive blocks did not provide any statistically significant relief at 1-month or 6-month follow-ups [16]. The most common side effects were mouth numbness, lacrimation, and bad taste, but there was no statistical difference in frequency of side effects between the bupivacaine and saline groups.
Table 5.
Studies of SPG block for migraine
| Migraine | ||||||||
|---|---|---|---|---|---|---|---|---|
| Author | Year | Medical problems | Approach | Imaging | Medication | Number of cases | Study design | Outcome |
| Amster et al. [28] | 1948 | Migraine | Cotton tipped applicator, transnasal approach | None | Nupercaine, pontocaine, monocaine | 4 | Case series | Relief of pain and spasm in 90% of cases |
| Maizels et al. [56] | 1999 | Migraine with aura | Self-administered intranasal 4% lidocaine | None | 4% lidocaine | 1 | Case report | Most headaches were successfully aborted for 15 months |
| Yarnitsky et al. [57] | 2003 | Migraine | Cotton tip applicator | None | 2% lidocaine | 32 | Case series | Significant reduction in pain score during migraine |
| Cady et al. [15] | 2015 | Chronic migraine | Tx360 | None | 0.5% bupivacaine | 38 | Double blind, placebo control | Significantly decreased headache at 24 h |
| Cady et al. [16] | 2015 | Chronic migraine | Tx360 | None | 0.5% bupivacaine | 38 | Double blind, placebo control | No statistical difference at 1 month and 6 months between treatment and control groups. |
Given the positive randomized-controlled study, grade of recommendation is B for short term treatment of chronic migraines using 0.5% bupivacaine with the Tx360 device®. It should be noted that the effect is only present for 24 h. and it is not suitable for patients seeking relief greater than 24 h.
Postoperative pain of the head and face
There were six randomized-controlled studies, one case-control study and one case series falling under this category (Table 6).
Table 6.
Studies of SPG blocks for operative pain of the head and face
| Operative Pain of the head and neck | ||||||||
|---|---|---|---|---|---|---|---|---|
| Author | Year | Medical problems | Approach | Imaging | Medication | Number of cases | Study design | Outcome |
| Robiony et al. [24] | 1998 | Skeletal transverse discrepancy of the maxilla | Transcutaneous truncal anesthesia of the maxillary nerve in association with transmucosal anesthesia of the sphenopalatine ganglion | None | Prilocaine carbocaine cream | 12 | Case series | Total anesthesia of the maxillary area facilitated the operations and appreciably reduced amount of postoperative pain |
| Hwang et al. [23] | 2003 | Removal of nasal packing after nasal operation | Needle injection into the greater palatine canal | None | 1% lidocaine | 11 | Case-control | Injection side had significantly lower pain than the control side |
| Ahmed et al. [18] | 2007 | Endoscopic sinonasal surgery intraoperative isofluorane consumption, hypotensive agents used, postoperative pain | Bilateral SPG block, injected between the middle and inferior turbinates | None | 0.5% lidocaine and epinephrine. | 15 cases, 15 controls | Randomized-controlled | Significantly reduced intraoperative isofluorane consumption and esmolol use, postoperative tramadol use and postoperative pain. |
| Ali et al. [20] | 2010 | Endoscopic trans-nasal resection of pituitary adenoma, anesthetic, vasodilator and analgesic sparing effect | Bilateral SPG block, injected between the middle and inferior turbinates | None | 1.5% lidocaine and epinephrine | 15 cases and 15 controls | Randomized-controlled | Significantly reduced in sevoflurane and nitroglycerine consumption, emergence time, postoperative pain and need of meperidine analgesia. |
| Kesimci et al. [22] | 2012 | Endoscopic sinus surgery postoperative analgesia efficacy | Bilateral SPG block, injected between the middle and inferior turbinates | None | 0.5% bupivacaine or 0.5% levobupivacaine | 45 | Double-blind randomized, placebo-controlled | Postoperative pain significantly reduced, also significantly few patients requiring additional analgesics in the postoperative 24 h. |
| Demaria et al. [21] | 2012 | Endoscopic sinus surgery postoperative analgesia efficacy | Bilateral SPG block, palatal approach | None | 2% lidocaine and 1% tetracaine | 70 | Double-blind randomized, placebo-controlled | Patients were discharged sooner than the control group. The block group also required less total fentanyl in the recovery room. |
| Al-Qudah et al. [19] | 2015 | Endoscopic sinus surgery postoperative analgesia efficacy | Applied to the SPG region | None | 2% lidocaine and epinephrine | 60 (30 cases, 30 controls) | Double-blind, placebo controlled | Significant pain reduction in the SPG block group |
Six randomized-controlled studies examined the efficacy of SPG blockade in reducing the needs of analgesics after endoscopic sinus surgery (level 2b). One study by Cho et al. [17] did not show significant difference between SPG block and placebo, but five additional randomized-controlled studies showed significant reduction in the need of post-operative analgesics in the group treated with SPG block [18–22]. The five positive studies used 0.5% lidocaine with epinephrine [18], 1.5% lidocaine with epinephrine [22], 0.5% bupivacaine or 0.5% levobupivacaine [22], 2% lidocaine and 1% tetracaine [21]. The SPG block was applied using injections, bilaterally through the transnasal or palatal approach. There was no difference in complications between the treatment and placebo group.
Hwang et al. [23] reported a case-control study to assess the efficacy of SPG block in reducing the pain associated with nasal packing removal after nasal operation (level 3b). 1% lidocaine was injected into the greater palatine canal ipsilaterally using infrazygomatic approach. Participants reported significantly lower pain on the side of the nose that received SPG block compared to the control side.
Robiony et al. [24] reported one case series (level 4) on the effectiveness of combined maxillary transcutaneous nerve block and SPG block in reducing postoperative pain for surgical correction of skeletal transverse discrepancy of the maxilla.
Given five positive double-blind placebo-controlled studies and one negative study, the grade of recommendation is B for SPG block in improving postoperative analgesia efficacy after endoscopic sinus surgery. Each study blocked SPG with injection of different local anesthetics using different approaches. In 5 studies, SPG block was consistently found to be effective in reducing the need of analgesics after endoscopic sinus surgery. A combination with maxillary transcutaneous nerve block may be also helpful but further systematic study is necessary to evaluate its efficacy. Grade of recommendation is also B for reducing pain associated with nasal packing removal after nasal surgery, using lidocaine injection through the infrazygomatic approach.
Head and neck cancer pain
Three case reports and series were found (level 4 evidence, Table 7). One study was SPG block and two on SPG neurolysis with phenol. The largest case series was by Varghese et al. [25], who reported 22 cases of successful treatment with 6% phenol used via nasal endoscopy, as a neurolytic sphenopalatine ganglion block, for pain caused by advanced head and neck cancer. The overall grade of recommendation is C for any of these painful conditions.
Table 7.
Studies of SPG block for cancer pain
| Head and neck cancer pain | ||||||||
|---|---|---|---|---|---|---|---|---|
| Author | Year | Medical problems | Approach | Imaging | Medication | Number of cases | Study design | Outcome |
| Prasanna et al. [58] | 1993 | Pain from carcinoma of the tongue and floor of the mouth | Nasal sinuscope | None | 0.25% bupivacaine | 10 | Case series | Immediate pain relief |
| Varghese et al. [25] | 2001 | Pain due to advanced head and neck cancer | Endoscopic needle injection | None | 6% phenol | 22 | Case series | 17 out of 22 patients had significant pain relief |
| Varghese el al. [59] | 2002 | Pain due to advanced head and neck cancer | Transnasal through the sphenopalatine foramen | None | 6% phenol | 1 | Case report | Significant pain relief |
Postherpetic neuralgia
A total of three case reports and series were found through our search process (level 4 evidence, Table 8). All three articles reported successful treatment of postherpetic neuralgia with SPG block using local anesthetics. One study reported successful treatment of postherpetic neuralgia involving the ophthalmic division of the trigeminal nerve, by SPG block under direct visualization through nasal endoscopy [26]. Another article reported success in treating sinus arrest in postherpetic neuralgia by SPG block through trans-nasal approach utilizing cotton tipped applicators [27], and one study reported successful treatment of herpes zoster within a heterogeneous case series [28]. The overall grade of recommendation is C.
Table 8.
Studies of SPG block on postherpetic neuralgia
| Postherpetic neuralgia | ||||||||
|---|---|---|---|---|---|---|---|---|
| Author | Year | Medical problems | Approach | Imaging | Medication | Number of cases | Study design | Outcome |
| Prasanna et al. [26] | 1993 | Postherpetic neuralgia involving the ophthalmic division of the trigeminal nerve | Combination of stellate ganglion and sphenopalatine ganglion block, cotton tip applicator | None | Lidocaine and bupivacaine | 1 | Case report | Pain free |
| Saberski et al. [27] | 1999 | Sinus arrest in postherpetic neuralgia | Cotton tipped applicator, transnasal approach | None | 20% lidocaine | 1 | Case report | No paroxysmal pain or sinus pauses immediately after block |
| Amster et al. [28] | 1948 | Herpes zoster | Cotton tipped applicator, transnasal approach | None | Nupercaine, pontocaine, monocaine | 3 | Case series | Relief of pain and spasm in 90% of cases |
Musculoskeletal pain
There were two negative randomized-controlled study on head, neck and shoulder myofascial pain. There were also a small case-control study on low back pain, a small randomized-controlled study on chronic muscle pain syndrome and two large case series in our literature search (Table 9).
Table 9.
Studies of SPG block for musculoskeletal pain
| Musculoskeletal pain | ||||||||
|---|---|---|---|---|---|---|---|---|
| Author | Year | Medical problems | Approach | Imaging | Medication | Number of cases | Study design | Outcome |
| Amster et al. [28] | 1948 | Lumbosacral and sacroiliac pain | Cotton tipped applicator, transnasal approach | None | Nupercaine, pontocaine, monocaine | 61 | Case series | Relief of pain and spasm in 90% of cases |
| Ruskin et al. [29] | 1946 | Lumbo-sacral spasm | Unknown | None | Cocaine, novocaine or nupercaine | 36 | Case series | Pain partially or completely relieved with SPGB and intramuscular injections of ironyl and calcium ascorbate |
| Berger et al. [32] | 1986 | Low back pain | Cotton tip applicator and transnasal needle | None | Cocaine or lidocaine | 7 cases with cocaine, 7 cases with lidocaine, 7 controls | Case-control | No statistical significance between cases and controls |
| Scudds et al. [3] | 1995 | Chronic muscle pain syndrome | Cotton tipped applicator, transnasal approach | None | 4% lidocaine | 42 with fibromyalgia, 19 with myofascial pain syndrome | Double-blind randomized controlled | No statistical significance between 4% lidocaine and placebo |
| Janzen et al. [30] | 1997 | Myofascial pain syndrome and fibromyalgia | Nasal spray | None | 4% lidocaine | 42 with fibromyalgia, 19 with myofascial pain syndrome | Double-blind, placebo-controlled | No statistical significance between 4% lidocaine and placebo |
| Ferrante et al. [31] | 1998 | Myofascial pain syndrome of the head, neck and shoulders | NA | None | 4% lidocaine | 13 cases, 7 controls | Double-blind, placebo-controlled, crossover design | No statistical significance |
Successful treatment of lumbosacral pain with SPG block was initially reported in two large case series in the 1940s [28, 29]. However, further randomized-controlled studies dismissed these findings. Scudds et al. [3] reported a randomized-controlled study applying SPG block (cotton-tipped pledgelets with 4% lidocaine) to 42 participants with fibromyalgia and 19 participants with myofascial pain syndrome. He reported no statistical difference between treatment and placebo group in pain intensity, headache frequency, sensitivity to pressure, anxiety, depression, and sleep quality. Janzen et al. [30] reported a similar randomized-controlled study by applying SPG block with lidocaine spray. Forty-two participants with fibromyalgia and 19 with myofascial pain syndrome were included in his study. He again found not difference between the treatment and placebo group. Ferrante et al. [31] reported a randomized-controlled study with 13 cases of head, neck and shoulder myofascial pain and 7 healthy controls. He also showed no significant effect with SPG block. On low back pain, Berger et al. [32] reported a case-control study with 21 patients randomized to cocaine, lidocaine and saline. He did not find significant differences in outcomes. Given the negative randomized-controlled studies, it is not recommended to use SPG block on musculoskeletal pain.
Postdural puncture headache
There were two case series and one case report (level 4) reporting successful treatment of postdural puncture headache (Table 10). No higher-level studies were available. Cohen et al. [33] reported the largest case series of 32 cases with postdural puncture headache. In the series, 69% of the patients treated with transnasal SPG block were saved from epidural blood patch. The overall grade of recommendation is C for SPG block on postdural puncture headache.
Table 10.
Studies of SPG blocks for postdural puncture headache
| Postdural puncture headache | ||||||||
|---|---|---|---|---|---|---|---|---|
| Author | Year | Medical problems | Approach | Imaging | Medication | Number of cases | Study design | Outcome |
| Cohen et al. [60] | 2014 | Postdural puncture headache | Cotton-tip applicator | None | 5% lidocaine | 32 | Case series | 69% of the patients were saved from epidural blood patch |
| Kent et al. [4] | 2015 | Postdural puncture headache | Cotton-tip applicator | None | 2% lidocaine | 3 | Case series | 1 patient had relief, 2 had to get epidural blood patch. |
| Cardoso et al. [61] | 2017 | Postdural puncture headache | Cotton-tip applicator | None | 0.5% Levobupivacaine | 1 | Case report | Symptoms relieved by 5 min. |
Other pain syndromes of the head and face
Pain syndromes involving the head and face not belonging to any category mentioned above are summarized in Table 11. There was a negative randomized-controlled study using Tx360 device treating acute anterior and global headache [34]. There were also multiple case reports and series on the effectiveness of SPG in controlling various types of head and facial pain. Local anesthetics and steroids have been used for SPG block, while phenol and alcohol have been used for SPG neurolysis. They have been successfully used in Sluder’s neuralgia, sphenopalatine maxillary neuralgia, facial neuralgia, sympathetic neuralgia, post-traumatic atypical facial pain, atypical odontalgia, pain from midline granuloma, herpetic keratitis, hemifacial headache, paroxysmal hemicrania, nasal pain, hemicrania continua and trigeminal neuropathy. The largest case series was provided by Rodman et al. [35], documenting 147 patients with various types of nasal pain and headache. He reported that 81.3% of the patients had pain relief after receiving SPG block with a mixture of bupivacaine and triamcinolone. Schaffer et al. [34] reported a randomized placebo-controlled study using Tx360 device to treat acute anterior or global headache. A total of 93 participants were recruited in the study, but the study showed no statistical significance between the treatment and control groups. Because of the result, we do not recommend SPG block for anterior or global headache. The overall grade of recommendation is C for other types of head and facial pain, including Sluder’s neuralgia, sphenopalatine maxillary neuralgia, facial neuralgia, sympathetic neuralgia, post-traumatic atypical facial pain, atypical odontalgia, pain from midline granuloma, herpetic keratitis, hemifacial headache, paroxysmal hemicrania, nasal pain, hemicrania continua and trigeminal neuropathy.
Table 11.
Studies of SPG blocks for other pain syndromes of the head and face
| Pain syndromes of the head and face | ||||||||
|---|---|---|---|---|---|---|---|---|
| Author | Year | Medical problems | Approach | Imaging | Medication | Number of cases | Study design | Outcome |
| Ruskin et al. [62] | 1925 | SP maxillary neuralgia, SP facial neuralgia, SP sympathetic neuralgia, SPG cell neuralgia | Needle injection. | None | 20% Cocaine, 10% silver nitrate, 70% alcohol | 7 | Case series | Improvements or complete relief |
| Stechison et al. [63] | 1994 | Post-traumatic atypical facial pain syndrome | Needle injection. Transfacial transpterygomaxillary access to foramen rotundum SPG and maxillary nerve | CT | First stage: 0.5% bupivacaine, Second stage: 98% ethyl alcohol and 0.5% bupivacaine in 2:1 ratio | 5 | Case series | 3 had alcohol neurotomy and pain free at 5, 8 and 12 months. 2 responded poorly to first stage blockade and did not have alcohol neurotomy. |
| Peterson et al. [12] | 1995 | Atypical odontalgia | Cotton tip, self-application | None | 4% lidocaine | 1 | Case report | Pain free |
| Saade et al. [64] | 1996 | Pain from midline granuloma | Self-administered SPG block | None | Lidocaine | 1 | Case report | Significant pain relief |
| Puig et al. [65] | 1998 | Sluder’s neuralgia | Cotton tip applicator and transnasal needle | None | 88% phenol | 8 | Case series | 90% decrease in head and face pain for 9.5-month duration |
| Windsor et al. [66] | 2004 | Herpetic keratitis | Transnasal cotton tip applicator | None | Tetracaine, adrenalin and 10% cocaine] | 1 | Case report | Effect of block lasts for a month. Requires months blocks |
| Obah et al. [67] | 2006 | Hemifacial and headache | Transnasal | None | 4% lidocaine | 1 | Case report | 80% reduction in pain intensity |
| Cohen et al. [33] | 2009 | Postdural puncture headache | Cotton tip applicator | None | Lignocaine | 13 | Case series | 11 out of 13 had immediate relief of headache |
| Morelli et al. [68] | 2010 | Paroxysmal hemicrania resistant to multiple therapies | Endoscopic needle injection into the nasal mucous membrane immediately behind and over the inferior portion of the sphenopalatine foramen and into the fossa | None | Triamcinolone acetonide, 1% bupivacaine, 2% mepivacaine with adrenalin | 1 | Case report | Reduction in frequency and intensity of pain |
| Rodman et al. [35] | 2012 | Nasal pain or headache | Endoscopic needle injection | None | 0.5% bupivacaine and triamcinolone acetonide | 147 | Case series | 81.3% of patients have improvement |
| Grant et al. [69] | 2014 | Tension headache in pregnant woman | Cotton tip applicator | None | 4% lidocaine | 1 | Case report | BID block for a total of 7 blocks, pain free after |
| Kastler et al. [55] | 2014 | Cluster headache (14), persistent idiopathic facial pain (10), and other types of facial pain (18) | Infrazygomatic approach | CT | Absolute alcohol | 28 | Case series | 85.7% of patient with persistent idiopathic facial pain and 40% of other types of facial pain had 50% pain relief at 1 month |
| Androulakis et al. [70] | 2016 | Hemicrania continua | Tx360 device | None | Repetitive 0.5% bupivacaine | 1 | Case report | Significant improvement in headache by 14 week |
| Malec-Milewska et al. [71] | 2015 | Trigeminal neuropathy | Zygomatic approach | Fluoroscopy | 65% ethanol with lidocaine | 20 | Case series | Significant pain relief |
| Schaffer [34] | 2015 | Acute anterior or global headache | Tx360 device | None | 0.5% bupivacaine | 93 | Randomized placebo-controlled | No statistically significant difference |
| Sussman et al. [72] | 2016 | Chronic posttraumatic headache after sport-related concussion | Cotton-tip applicator | None | 2% lidocaine and 0.5% bupivacaine | 1 | Case report | Symptom free at 6-month follow-up |
Other syndromes
SPG block has been used for a myriad of other conditions not involved in painful syndromes of the head and face. These conditions include seizures associated nasal pathology, arthritic pain and muscle spasm, intercostal neuritis, persistent hiccups, ureteral colic, dysmenorrhea, peripheral painful vascular spasm, complex regional pain syndrome and hypertension (Table 12). Most of these studies reported significant improvement, but none of them had evidence level above case series. There was one randomized-controlled study in assessing the efficacy of SPG block in treating nicotine addiction, but the result was negative [36]. One small double-blind cross-over study examined whether SPG block reduces experimentally induced pain using submaximal effort tourniquet test, but the SPG block failed to make a difference in pain perception [37].
Overall, the grade of recommendation for any of these syndrome remains at C. SPG block is not recommended for nicotine addiction due to the negative randomized study.
Summary for SPG block
Grade of recommendation of using SPG block is B for cluster headache, second-division trigeminal neuralgia, migraine, reducing the pain associated with nasal packing removal after nasal operation and for reducing the needs of analgesics after endoscopic sinus surgery. Out of these conditions, SPG block has the best evidence in reducing the needs of analgesics after endoscopic sinus surgery, as there are six randomized-controlled studies. It should be noted that the recommendation for cluster headache, second-division trigeminal neuralgia and migraine are each based on one small study, and it is only meant for acute treatment. There is no positive controlled study warranting chronic treatment with SPG block. For other pain syndromes, grade of recommendations is C due to the lack of positive controlled studies. These syndromes include postdural puncture headache, sphenopalatine maxillary neuralgia, facial neuralgia, sympathetic neuralgia, post-traumatic atypical facial pain, atypical odontalgia, pain from midline granuloma, herpetic keratitis, hemifacial headache, paroxysmal hemicrania, nasal pain, hemicrania continua, trigeminal neuropathy, cancer pain, seizures associated nasal pathology, arthritic pain and muscle spasm, intercostal neuritis, persistent hiccups, ureteral colic, dysmenorrhea, peripheral painful vascular spasm, complex regional pain syndrome and hypertension. Use of SPG block for myofascial pain, including fibromyalgia and head, neck, shoulder myofascial pain and low back pain, is not recommended due to several negative randomized-controlled studies.
Radiofrequency ablation
Fifteen studies were included on the topic of SPG radiofrequency ablation. One study was a small but positive prospective cohort study for cluster headaches, while the other 14 studies were case reports and case series. There were no controlled studies.
Cluster headache
There was one prospective cohort study and eight case reports/series on the treatment of cluster headache. Three case reports were on pulsed radiofrequency and six on continuous radiofrequency ablation (Table 13). Narouze et al. [38] performed a prospective cohort study of 15 cases of chronic cluster headaches treated with radiofrequency ablation using infrazygomatic approach under fluoroscopy guidance. A total of 0.5 mL of lidocaine 2% was injected and 2 radiofrequency lesions were carried out at 80 °C for 60 s each. After the ablation, 0.5 mL of bupivacaine 0.5% and 5 mg of triamcinolone were injected. He reported statistically improved attack intensity, frequency and pain disability index up to 18 months (level 2b). As for side effects: 50% (7/15) reported temporary paresthesias in the upper gums and cheek that lasted for 3-6 weeks with complete resolution. In only one patient, a coin-like area of permanent anesthesia over the cheek persisted. Sanders et al. [39] reported the largest case series of 66 cluster headache patients treated with radiofrequency ablation after 12 to 70 months. He reported complete relief in 60.7% of patients with episodic cluster headache, and in 30% of patients with chronic cluster headache. Of the 66 treated patients, eight patients experienced temporary postoperative epistaxis and 11 patients exhibited cheek hematomas. A partial radiofrequency lesion of the maxillary nerve was inadvertently made in four patients. Nine patients complained of hypoesthesia of the palate, which disappeared in all patients within 3 months.
Table 13.
Studies of SPG radiofrequency ablation on cluster headache
| Cluster headache | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| First author | Year | Medical problem | Approach | Imaging | Temperature (°C) | Type of RFA | Parameter | How to identify right spot | Study design | Number of cases | Outcome |
| Sanders et al. [39] | 1997 | Cluster headache | Infrazygomatic approach | Fluoroscopy | 70 | High frequency | 50 Hz, 0.2-1 V | Paresthesia in the palate | Case-only | 66 | 60.7% of episodic cluster headache patients received complete relief, 30% in chronic cluster headache patients achieved complete relief |
| Narouze et al. [38] | 2009 | Chronic cluster headache | Infrazygomatic approach | Fluoroscopy | 80 | Unknown | 50 Hz at <0.5 V to produce deep paresthesia behind the root of the nose | . | Prospective cohort | 15 | Mean attack intensity, mean attack frequency, pain disability index significant reduced at 1 year follow-up (P < 0.0005, P < 0.0003, P < 0.002, respectively) |
| Chua et al. [78] | 2011 | Cluster headaches | Infrazygomatic approach | Fluoroscopy | 42 | Pulsed | 50 Hz, 0.5-0.7 V | Paresthesia at the root of the nose | Case series | 3 | Two had excellent relief, one had partial relief by 2 months |
| Oomen et al. [79] | 2012 | Atypical facial pain, cluster headache, Sluder’s neuralgia, Sluder’s neuropathy | Infrazygomatic approach | Fluoroscopy | 80 | Unknown | 50 Hz | Paresthesia in the nose and not in the area of the maxillary nerve | Case series | 3 | Adequate pain reduction: 4/4 in atypical facial pain, 2/3 in cluster headache, 1/2 in Sluder’s neuralgia, 2/2 in Sluder’s neuropathy, 1/1 in posttraumatic neuropathy, 0/1 in post-herpetic neuralgia, 0/1 in SUNCT (60% showed considerable pain relief after a single procedure). |
| Zarembinski et al. [54] | 2014 | Drug-resistant chronic cluster headache, with Jacob’s disease | Initially sphenopalatine ganglion block, then radiofrequency. | Fluoroscopy, CT | Unknown | Unknown | Unknown | NA | Case report | 1 | Pain significantly improved. |
| Fang et al. [80] | 2015 | Cluster headache | Infrazygomatic approach | CT | 42 | Pulsed | Unknown | 0.1-0.3 V to induce paresthesia of the nasal root | Case series | 16 | 11 episodic and 1 chronic cluster headache patients had complete relief by 6.3 days. 2 episodic and 2 chronic cluster headache patients had no relief. |
| Bendersky et al. [81] | 2015 | Cluster headache | Infrazygomatic approach | Fluoroscopy | 42 | Pulsed | 45 V, 2 Hz, pulse width 20 ms | Paresthesia at the roof of the nose | Case series | 3 | 2 patients had no relief, 1 had relief until 1 month. Continue RFA gave relief to all three patients. |
| Dharmavaram et al. [82] | 2016 | Cluster headache | Lateral approach | Fluoroscopy | 80 | Continuous | Unknown | paresthesia at the root of the nose was obtained at 0.3 V | Case report | 1 | Pain free for 2 months |
| Loomba et al. [83] | 2016 | Cluster headache | Infrazygomatic approach | CT | 80 | Continuous | 50 Hz | <0.3 V to induce paresthesia of the nasal root | Case report | 1 | Near complete resolution at 6 months |
The grade of recommendation is B for treating cluster headache with radiofrequency ablation because of the positive cohort study.
Other head and facial pain
There were Seven case reports/series on various head and facial pain other than cluster headaches (all level 4, Table 14). These included Sluder’s neuralgia, posttraumatic headache, chronic head and facial pain, atypical trigeminal neuralgia, atypical facial pain, chronic facial pain secondary to cavernous sinus meningioma, trigeminal neuralgia and SPG neuralgia due to herpes zoster. Akbas et al. [40] reported a 27-case series with various types of head and facial pain. In 35% of the cases, pain was completely relieved, while 42% had moderate relief and 23% had no relief with the SPG radiofrequency ablation. Because there were only case reports and case series available, the grade recommendation is C for any of these conditions.
Table 14.
Studies of SPG radiofrequency ablation on head and facial pain
| First author | Year | Medical problem | Approach | Imaging | Temperature (°C) | Type of RFA | How to identify the right spot | Study design | Number of cases | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| Salar et al. [50] | 1987 | Sluder’s neuralgia | Lateral extraoral approach | Fluoroscopy | 60 and 65 | Continuous | 0.2-0.3 V, paresthesia in the distribution of the maxillary nerve | Case series | 7 | Disappearance of the typical pain attacks, lacrimation and nasal secretion, however, a slight, deep-seated troublesome sensation persisted |
| Shah et al. [84] | 2004 | Posttraumatic headache | Infrazygomatic approach | Fluoroscopy | 42 | Pulsed | 50 Hz and 0.5 V produced tingling sensation at the root of the nose | Case report | 1 | Pain reduced from 10/10 to 1/10 |
| Bayer et al. [85] | 2005 | Chronic head and face pain | Infrazygomatic approach | Fluoroscopy | 42 | Pulsed | 50 Hz up to 1 V, paresthesia elicited at the roof of the nose, motor stimulation performed at 2 Hz to rule out trigeminal contact, which results in rhythmic mandibular contraction | Case series | 30 | 21% had complete pain relief, 65% had moderate pain relief, 14% had no pain relief. |
| Nguyen et al. [86] | 2010 | Atypical trigeminal neuralgia | Coronoid approach | Fluoroscopy | 42 | Pulsed | 50 Hz with 1 ms pulse duration, 0.6 V | Case report | 1 | Symptom-free after 2 yrs. |
| Oomen et al. [79] | 2012 | Atypical facial pain, cluster headache, Sluder’s neuralgia, Sluder’s neuropathy | Infrazygomatic approach | Fluoroscopy | 80 | Unknown | 50 Hz, paresthesia in the nose and not in the area of the maxillary nerve | Case series | 4 atypical facial pain, 2 Sluder’s neuralgia, 2 Sluder’s neuropathy, 1 post-traumatic neuropathy of infraorbital nerve, 1 postherpetic neuralgia, 1 SUNCT | Adequate pain reduction: 4/4 in atypical facial pain, 2/3 in cluster headache, 1/2 in Sluder’s neuralgia, 2/2 in Sluder’s neuropathy, 1/1 in posttraumatic neuropathy, 0/1 in post-herpetic neuralgia, 0/1 in SUNCT (60% showed considerable pain relief after a single procedure). |
| Elahi et al. [87] | 2014 | Facial pain secondary to cavernous sinus meningioma removal | Infrazygomatic approach | Fluoroscopy | 80 | Continuous | 50 Hz, paresthesia in the nasolabial midline region | Case report | 1 | Satisfactory pain relief at 12 months |
| Akbas et al. [40] | 2016 | Atypical facial pain, SPG neuralgia due to herpes zoster, atypical Trigeminal neuralgia | Infrazygomatic approach | Fluoroscopy | 42 | Continuous | Paresthesia at the roof of the nose at 0.5–0.7 V. To rule out trigeminal contact, motor stimulation at a frequency of 2 Hz was applied | Case series | 27 | Pain relief not achieved in 23%, completely relieved in 35% and moderately relieved in 42% of patients |
Summary for SPG radiofrequency ablation
Grade of recommendation is B for applying SPG radiofrequency ablation to intractable cluster headache. The protocol used in the cohort study took infrazygomatic approach under fluoroscopy and two radiofrequency ablations were carried out at 80 °C for 60 s. However, there is not yet a randomized-controlled study to test its efficacy. Grade of recommendation is C for other head and facial pain, including Sluder’s neuralgia, posttraumatic headache, atypical trigeminal neuralgia, atypical facial pain, chronic facial pain secondary to cavernous sinus meningioma, trigeminal neuralgia and SPG neuralgia due to herpes zoster.
Sphenopalatine ganglion neurostimulation
Eight studies were included for SPG neurostimulation. There was one randomized-controlled study with two long-term follow-ups of the same study and five case report/case series on sphenopalatine ganglion neurostimulation (Table 15).
Table 15.
Studies of SPG neurostimulation
| Neurostimulation | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| First author | Year | Medical problem | Stimulator | Approach | Imaging | Types of stimulation | How to identify the right spot | Study design | Number of cases | Outcome |
| Tepper et al. [45] | 2009 | Intractable migraine | Medtronic model 3625 or 3628 | Infrazygomatic approach | Fluoroscopy | Customized, average amplitude, 1.2 V, pulse rate 67 Hz, pulse width 462 μs | Paresthesia with stimulation at the back of the nose and deep in the back of the soft palate | Case only | 11 | 2 pain-free, 3 had pain reduction, 5 had no response, 1 was not stimulated |
| Ansarinia et al. [44] | 2010 | Cluster headache | Medtronic model 3625 | Pterygopalatine fossa | Fluoroscopy | Customized, average amplitude, 1.7 V, frequency 88 Hz, pulse width 294 μs | paresthesia with stimulation in the posterior nasopharynx and root of the nose | Case only | 6 | Total 18 CH attacks, complete resolution with SPG stimulation in 11 attacks, partial in 3, no relief in 4. |
| Schoenen et al. [41] | 2013 | Cluster headache | ATI SPG stimulator | Pterygopalatine fossa proximate to the sphenopalatine ganglion | CT | Customized, mean frequency 120.4 Hz, mean pulse width 389.7 μs, mean intensity 1.6 mA | X-ray | Randomized controlled | 28 cases, with 3 randomized settings. | Pain relief achieved in 67.1% of full stimulation-treated attacks compared to 7.4% of sham-treated attacks. P < 0.0001 |
| Elahi et al. [47] | 2015 | Idiopathic right facial pain | Medtronic model 3378 | The pterygopalatine fossa | Fluoroscopy | 0.5 mV, pulse width 250 – 450 μs, and 40 – 80 Hz | X-ray | Case report | 1 | 2/10 pain on 6-month follow-up |
| Meng et al. [88] | 2016 | Cluster headache | Medtronic model 3487A | Pterygopalatine fossa | Fluoroscopy | Bilateral stimulation, right 0-, 1+, 130 Hz, 120 μs, 0.7 V; left 8-, 9+, 130 Hz, 120 μs, 0.8 V | X-ray | Case report | 1 | Headache frequency reduced to once a week, pain level 1/10 at 4 months |
| William et al. [46] | 2016 | Idiopathic facial pain, supraorbital neuropathy, hemicrania continua, facial anesthesia dolorosa, occipital neuropathy | Medtronic Subcompact Octrode | SPG | Fluoroscopy | Unknown | X-ray | Case series | 5 | 80% reported sustained facial pain at mean follow-up of 9.6 months. |
| Jurgens et al. [42] | 2016 | Cluster headache | Neurostimulator, described in [41] | Pterylopalatine fossa | CT | Customized, applied as soon as the patient feels cluster headache attacks | X-ray | Cohort study. Long-term follow-up from [41] | 33 cases | 61% of patients were either acute responder (>50% relief from moderate or greater pain) or frequency responder (>50% in attack frequency) at 24 months |
| Barloese et al. [43] | 2016 | Cluster headache | Neurostimulator, described in [41] | Pterylopalatine fossa | CT | Customized, applied as soon as the patient feels cluster headache attacks | X-ray | Cohort study. Long-term follow-up from [41] | 33 cases | 30% experienced at least 1 episode of complete attack remission (attack-free period exceeding 1 month). |
Cluster headache
There was one randomized-controlled study with two long-term follow-ups of the same study, and two case reports/series on cluster headache. Schoenen et al. [41] reported a randomized-controlled trial using SPG neurostimulator for patients with refractory cluster headaches. Twenty-eight patients underwent SPG stimulator implantation and stimulations were applied at the onset of cluster headache. The study employed a protocol that randomly inserted a placebo when treatment was initiated by the patient for a cluster headache attack. Three settings were delivered in a randomized fashion (1:1:1): full stimulation (i.e. customized stimulation parameters established during the therapy titration period), sub-perception stimulation, and sham stimulation. A total of 566 cluster headaches were treated, and pain relief was achieved in 67.1% of patients receiving full stimulation compared to 7.4% receiving sham treatment (P < 0.0001). Pain relief using sub-perception stimulation was not significantly different from sham stimulation (P = 0.96). Acute rescue medication was used in 31% of cluster headache attacks in patients receiving full stimulation, compared to 77.4% treated with sham stimulation (P < 0.0001) and 78.4% with sub-perception stimulation (P < 0.0001). In terms of side effect, most patients (81%) experienced transient, mild to moderate loss of sensation within distinct maxillary nerve regions; 65% of events resolved within 3 months. Jurgens et al. [42] reported a cohort study from the subjects who volunteered to be followed for 24 months from the study by Schoenen et al. In this study, 61% of patients were either acute responder (>50% relief from moderate or greater pain) or frequency responder (>50% in attack frequency) at 24 months. Barloese et al. [9] analyzed participants who experienced remission from the same dataset. 30% of participants were found to have at least 1 episode of complete attack remission in the 24-month period. Ansarinia et al. [44] reported a case series of 6 patients. Out of the 18 attacks recorded, there were 11 attacks receiving complete relief from the stimulations, 3 getting partial relief and 4 without relief.
With the positive randomized-controlled trial, the grade of recommendation is B for using SPG neurostimulation on cluster headache. Given the positive effect from these studies, further trials are encouraged.
Migraine headache
There was one case series of 11 cases on SPG neurostimulation in acutely treating intractable migraine headaches [45]. In this study, 11 patients with a history of migraine headache for a mean of 20 years were studied. Spontaneous and induced migraine headaches were acutely treated with SPG neurostimulation. Out of the 11 treated, two patients were pain-free, three had some pain reduction, while five had no response. Because of the largely negative response, there is currently not enough evidence for treating intractable migraine with SPG neurostimulation.
Other head and facial pain
There was one case series and one case report on other types of head and facial pain. William et al. [46] reported a case series on idiopathic facial pain, supraorbital neuropathy, hemicrania continua, facial anesthesia dolorosa and occipital neuropathy. SPG neurostimulation was combined with trigeminal or peripheral stimulation. 80% of the patients reviewed reported sustained relief in facial pain. It is unclear whether SPG stimulation alone would provide the same relief in these cases. Elahi et al. [47] reported a single case of SPG neurostimulation for idiopathic facial pain with good success.
Given the sparse literature, the grade of recommendation is C for SPG neurostimulation in idiopathic facial pain and D for SPG stimulation combined with trigeminal/peripheral stimulation in supraorbital neuropathy, hemicrania continua, facial anesthesia dolorosa and occipital neuropathy.
Summary for SPG neurostimulation
Grade of recommendation is B for applying SPG neurostimulation to cluster headache and C for idiopathic facial pain. There may be a role of combined SPG and trigeminal or peripheral neurostimulation in isolated cases. Due to its invasive nature, SPG neurostimulation warrants further investigations with more high quality, large-scale studies.
Discussion
Sphenopalatine ganglion block
Sphenopalatine ganglion block has been used for over a century. In 1908, Sluder first proposed that inflammation in the posterior ethmoid and sphenoid sinuses may be involved in unilateral facial pain associated with tearing, congestion and rhinorrhea. He also claimed to have successfully treated facial neuralgia, asthma, earache and lower-half headache. Over time, the term Sluder’s neuralgia has varied definitions across the medical literature. Its characteristics mostly resemble cluster headache and it has been suggested that the term Sluder’s neuralgia be discarded [48]. However, an analysis suggested that cluster headache and Sluder’s neuralgia may be two different entities [49]. This review kept Sluder’s neuralgia and cluster headaches as two distinct type of headaches because of the differences. Since Sluder’s first publication, SPG block has been reported to be used successfully in treating multiple pain syndromes, including cluster headaches, trigeminal neuralgia, migraine, postherpetic neuralgia and atypical facial pain. It was also used for treating intractable cancer pain of the head and face as well as facial pain management after endoscopic sinus surgery. However, for most pain syndromes the evidence for using SPG nerve block remains at case report and case series level. There were a few small yet positive randomized-controlled studies in nitroglycerin-induced cluster headache, second-division trigeminal neuralgia, migraine, reducing the pain associated with nasal packing removal after nasal operation and for reducing the needs of analgesics after endoscopic sinus surgery. It should be emphasized that the evidence for treating these conditions with SPG block is based on very few small studies. The exception lies in reducing the needs of analgesics after endoscopic sinus surgery, which is backed by five randomized-controlled studies. It should be also noted that long-term treatment may not be beneficial, as demonstrated by the chronic repetitive block study in migraine by Cady et al. [16]. When SPG block is offered as a treatment option, patients should be informed of such caveats.
Blocking strategies
Several techniques exist for SPG blockade. Four types of applications exist: cotton-tip applicator, Tx360 device, nasal spray and needle injections. Three main types of approaches exist: transnasal, transoral and infrazygomatic approaches. Cotton-tip applicator, Tx360 device and nasal spray can only be applied through the transnasal approach. Needle injection, on the other hand, can be performed in any approach. Applied local anesthetics included lidocaine, bupivacaine, ropivacaine, levobupivacine, mepivacaine, novocaine, nupercaine, pontocaine, monocaine, tetracaine, and prilocaine, with varying concentrations, but lidocaine and bupivacaine were by far the most common. Other medications include cocaine, ethanol and phenol. Co-medications included epinephrine, triamcinolone and dexamethasone. Some studies used fluoroscopy or CT to guide needle placement. Unfortunately, there are no head-to-head trials comparing the efficacy among different blocking strategies. The recommendations made in this article are based on strategies used in the positive controlled studies.
Side effects
Side effects from SPG blockade is typically local. Potential side effects are numbness and stinging at the root of the nose and palate, numbness or lacrimation of ipsilateral eye, and bitter taste and numbness of the throat. With needle injection techniques, there is also the risk of bleeding, infection and epistaxis.
Sphenopalatine ganglion radiofrequency ablation
The use of radiofrequency on sphenopalatine ganglion was first reported by Salar et al. [50] for treating Sluder’s neuralgia. Since the first report, there were multiple case reports on using SPG radiofrequency ablation in treating head and facial pain. About half of the reports focused on treating cluster headaches, but it has also been successfully used on patients with post-traumatic headache, atypical trigeminal neuralgia and anesthesia dolorosa after cavernous meningioma surgery. However, most of the literature today remains at the case report and case series level. There was only one small prospective cohort study on the effectiveness of SPG radiofrequency ablation. Well-controlled studies are yet to be performed to confirm the validity of this therapeutic modality in treating headache and facial pain.
Compared to the short-lived effect of SPG block, SPG radiofrequency ablation tend to be long lasting. Narouze et al. [38] reported statistically improved attack intensity, frequency and pain disability index up to 18 months in patients who underwent SPG radiofrequency ablation. As a comparison, Costa et al. [6] only reported shorter cluster headache duration with SPG block, and Cady et al. reported only up to 24 h of relief in chronic migraine [15] while no difference was found at 1 and 6 months with repetitive SPG block [16].
Ablation strategies
Most radiofrequency ablation of SPG were carried out with the infrazygomatic approach. The most commonly used temperature is 80 °C for thermal ablation, and 42 °C for pulsed ablation. There is unfortunately no head-to-head comparison between the two types of ablations. All studies confirmed the position of RF cannula/probe by applying low voltage sensory stimulation (between 0.2-0.1 V) while patients felt paresthesia or tingling sensation at the root of the nose. The only study with evidence level above case series was a cohort study on patients with chronic cluster headache [38]. In this positive study, the authors applied 2 rounds of thermal ablation at 80 °C for 60 s each. Pre- and post-ablation medications were also given (pre: 0.5 ml of 2% lidocaine; post: 0.5 ml of 0.5% bupivacaine and 5 mg of triamcinolone).
Side effects
Based on the study by Narouze et al. [38], about 50% (7/15) reported temporary paresthesias in the upper gums and cheek that lasted for 3-6 weeks with complete resolution. Rare permanent small zone of hypoesthesia over the cheek could also happen. In the large case series by Sanders et al. [39], of the 66 treated patients, eight patients experienced temporary postoperative epistaxis and 11 patients exhibited cheek hematomas. A partial radiofrequency lesion of the maxillary nerve was inadvertently made in four patients. Nine patients complained of hypoesthesia of the palate, which disappeared in all patients within 3 months.
Sphenopalatine ganglion neurostimulation
Neurostimulation has emerged in recent years as a potential therapeutic modality for headaches and facial pain. Even though number of studies on SPG neurostimulation has not been abundant, the overall quality of the studies has been high. The study by Shoenen et al. [41] was the only randomized-controlled study in using SPG neurostimulation to treat chronic cluster headache. Despite the small number of participants, the effectiveness is demonstrated by the large effect size and highly significant P value. The two long-term follow-up articles continued to support the effectiveness of such intervention [42, 43]. These three studies combined is the strongest piece evidence to date, suggesting that SPG neurostimulation is effective in treating cluster headache. There were other isolated case reports on the successful application of SPG neurostimulation to other pain syndromes, but higher level of evidence is lacking.
Stimulation strategies
Stimulation settings vary widely across study subjects, stimulator models and studies. In the controlled study by Schoenen et al. [41], the mean frequency was 120.4 ± 15.5 Hz, mean pulse width 389.7 ± 75.4 μs with mean intensity 1.6 ± 0.8 mA during full stimulation. These numbers are for references only, and the stimulation setting should be individualized based on responses.
Side effects
In Schoenen’s controlled study [41], the most common acute side effects are sensory disturbances (81%), pain (38%), swelling (22%). Other side effects included tooth pain (16%), trismus (16%), headache (9%), dry eye (9%), and hematoma (9%). Across all 32 patients, five device- or procedure-related serious adverse events occurred. The most common serious adverse events are due to erroneous lead placements and lead migration to adjacent nerves.
Limitations
There are several limitations in our review. Firstly, articles could have been missed because only Pubmed, CENTRAL and Google Scholar were used. Second, most of the studies included in this review were case studies and case reports. By nature of these kinds of studies, publication bias will be skewed toward positive outcomes. Thirdly, due to the paucity of controlled studies, meta-analysis could not be adequately performed to create a quantitative analysis. Despite these limitations, this study was the first to systematically summarize SPG interventions. As more controlled studies become available, meta-analysis will be possible and thus providing better level of evidence in this developing field.
Conclusions
SPG has been the target for treating pain syndrome in the head and face for over a hundred years. The strongest evidence lies in using SPG block, radiofrequency ablation and neurostimulation on cluster headache. Sphenopalatine ganglion block also has good evidence in treating trigeminal neuralgia, migraines, reducing the needs of analgesics after endoscopic sinus surgery and reducing pain associated with nasal packing removal after nasal operations. Large-scale, double-blinded, randomized-controlled studies are warranted in establishing these techniques in treating cluster headache and other head and facial pain.
Acknowledgements
Not applicable.
Funding
No funding was received for this manuscript.
Availability of data and materials
Not applicable.
Abbreviations
- SPG
Sphenopalatine ganglion
- TAC
Trigeminal autonomic cephalalgia
Additional file
PRISMA checklist. (DOC 64 kb)
Authors’ contributions
KWDH designed the study, managed the literature searches and summaries of previous related work and wrote the first draft of the manuscript. RP and SK critically reviewed the study manuscript and provided revisions for intellectual content. All authors read and approved the final manuscript.
Authors’ information
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s10194-017-0826-y) contains supplementary material, which is available to authorized users.
Contributor Information
Kwo Wei David Ho, Email: KwoWei.Ho@neurology.ufl.edu.
Rene Przkora, Email: RPrzkora@anest.ufl.edu.
Sanjeev Kumar, Email: SKumar@anest.ufl.edu.
References
- 1.Piagkou M, Demesticha T, Troupis T, Vlasis K, Skandalakis P, Makri A, Mazarakis A, Lappas D, Piagkos G, Johnson EO. The pterygopalatine ganglion and its role in various pain syndromes: from anatomy to clinical practice. Pain Pract. 2012;12(5):399–412. doi: 10.1111/j.1533-2500.2011.00507.x. [DOI] [PubMed] [Google Scholar]
- 2.Oluigbo CO, Makonnen G, Narouze S, Rezai AR. Sphenopalatine ganglion interventions: technical aspects and application. Prog Neurol Surg. 2011;24:171–179. doi: 10.1159/000323049. [DOI] [PubMed] [Google Scholar]
- 3.Scudds RA, Janzen V, Delaney G, Heck C, McCain GA, Russell AL, Teasell RW, Varkey G, Woodbury MG. The use of topical 4% lidocaine in spheno-palatine ganglion blocks for the treatment of chronic muscle pain syndromes: a randomized, controlled trial. Pain. 1995;62(1):69–77. doi: 10.1016/0304-3959(94)00232-4. [DOI] [PubMed] [Google Scholar]
- 4.Kent S, Mehaffey G. Transnasal sphenopalatine ganglion block for the treatment of postdural puncture headache in the ED. Am J Emerg Med. 2015;33(11):1714.e1711–1714.e1712. doi: 10.1016/j.ajem.2015.03.024. [DOI] [PubMed] [Google Scholar]
- 5.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Group CBM. Group CSM The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Costa A, Pucci E, Antonaci F, Sances G, Granella F, Broich G, Nappi G. The effect of intranasal cocaine and lidocaine on nitroglycerin-induced attacks in cluster headache. Cephalalgia. 2000;20(2):85–91. doi: 10.1046/j.1468-2982.2000.00026.x. [DOI] [PubMed] [Google Scholar]
- 7.Barre F. Cocaine as an abortive agent in cluster headache. Headache: J Head Face Pain. 1982;22(2):69–73. doi: 10.1111/j.1526-4610.1982.hed2202069.x. [DOI] [PubMed] [Google Scholar]
- 8.Kittrelle JP, Grouse DS, Seybold ME. Cluster headache: local anesthetic abortive agents. Arch Neurol. 1985;42(5):496. doi: 10.1001/archneur.1985.04060050098017. [DOI] [PubMed] [Google Scholar]
- 9.Felisati G, Arnone F, Lozza P, Leone M, Curone M, Bussone G. Sphenopalatine endoscopic ganglion block: a revision of a traditional technique for cluster headache. Laryngoscope. 2006;116(8):1447–1450. doi: 10.1097/01.mlg.0000227997.48020.44. [DOI] [PubMed] [Google Scholar]
- 10.Pipolo C, Bussone G, Leone M, Lozza P, Felisati G. Sphenopalatine endoscopic ganglion block in cluster headache: a reevaluation of the procedure after 5 years. Neurol Sci. 2010;31(Suppl 1):S197–S199. doi: 10.1007/s10072-010-0325-2. [DOI] [PubMed] [Google Scholar]
- 11.Kanai A, Suzuki A, Kobayashi M, Hoka S. Intranasal lidocaine 8% spray for second-division trigeminal neuralgia. Br J Anaesth. 2006;97(4):559–563. doi: 10.1093/bja/ael180. [DOI] [PubMed] [Google Scholar]
- 12.Peterson JN, Schames J, Schames M, King E. Sphenopalatine ganglion block: a safe and easy method for the management of orofacial pain. Cranio. 1995;13(3):177–181. doi: 10.1080/08869634.1995.11678065. [DOI] [PubMed] [Google Scholar]
- 13.Manahan AP, Malesker MA, Malone PM. Sphenopalatine ganglion block relieves symptoms of trigeminal neuralgia: a case report. Nebr Med J. 1996;81(9):306–309. [PubMed] [Google Scholar]
- 14.Candido KD, Massey ST, Sauer R, Darabad RR, Knezevic NN. A novel revision to the classical transnasal topical sphenopalatine ganglion block for the treatment of headache and facial pain. Pain Physician. 2013;16(6):E769–E778. [PubMed] [Google Scholar]
- 15.Cady R, Saper J, Dexter K, Manley HR. A double-blind, placebo-controlled study of repetitive transnasal sphenopalatine ganglion blockade with tx360(®) as acute treatment for chronic migraine. Headache. 2015;55(1):101–116. doi: 10.1111/head.12458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cady RK, Saper J, Dexter K, Cady RJ, Manley HR. Long-term efficacy of a double-blind, placebo-controlled, randomized study for repetitive sphenopalatine blockade with bupivacaine vs. saline with the Tx360 device for treatment of chronic migraine. Headache. 2015;55(4):529–542. doi: 10.1111/head.12546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cho DY, Drover DR, Nekhendzy V, Butwick AJ, Collins J, Hwang PH. The effectiveness of preemptive sphenopalatine ganglion block on postoperative pain and functional outcomes after functional endoscopic sinus surgery. Int Forum Allergy Rhinol. 2011;1(3):212–218. doi: 10.1002/alr.20040. [DOI] [PubMed] [Google Scholar]
- 18.Ahmed H, Abu-Zaid E. Role of intraoperative endoscopic sphenopalatine ganglion block in sinonasal surgery. J Med Sci. 2007;7:1297–1303. doi: 10.3923/jms.2007.1297.1303. [DOI] [Google Scholar]
- 19.Al-Qudah M. Endoscopic sphenopalatine ganglion blockade efficacy in pain control after endoscopic sinus surgery. Int Forum Allergy Rhinol. 2016;6(3):334–338. doi: 10.1002/alr.21644. [DOI] [PubMed] [Google Scholar]
- 20.Ali AR, Sakr SA, Rahman ASM. Bilateral sphenopalatine ganglion block as adjuvant to general anaesthesia during endoscopic trans-nasal resection of pituitary adenoma. Egypt J Anaesth. 2010;26(4):273–280. doi: 10.1016/j.egja.2010.05.002. [DOI] [Google Scholar]
- 21.DeMaria S, Govindaraj S, Chinosorvatana N, Kang S, Levine AI. Bilateral sphenopalatine ganglion blockade improves postoperative analgesia after endoscopic sinus surgery. Am J Rhinol Allergy. 2012;26(1):e23–e27. doi: 10.2500/ajra.2012.26.3709. [DOI] [PubMed] [Google Scholar]
- 22.Kesimci E, Öztürk L, Bercin S, Kırış M, Eldem A, Kanbak O. Role of sphenopalatine ganglion block for postoperative analgesia after functional endoscopic sinus surgery. Eur Arch Otorhinolaryngol. 2012;269(1):165–169. doi: 10.1007/s00405-011-1702-z. [DOI] [PubMed] [Google Scholar]
- 23.Hwang JH, Liu CM, Liu TC, Hsu MC. Sphenopalatine ganglion block before removal of nasal packing. Laryngoscope. 2003;113(8):1423–1424. doi: 10.1097/00005537-200308000-00030. [DOI] [PubMed] [Google Scholar]
- 24.Robiony M, Demitri V, Costa F, Politi M, Cugini U. Truncal anaesthesia of the maxillary nerve for outpatient surgically assisted rapid maxillary expansion. Br J Oral Maxillofac Surg. 1998;36(5):389–391. doi: 10.1016/S0266-4356(98)90653-2. [DOI] [PubMed] [Google Scholar]
- 25.Varghese BT, Koshy RC. Endoscopic transnasal neurolytic sphenopalatine ganglion block for head and neck cancer pain. J Laryngol Otol. 2001;115(5):385–387. doi: 10.1258/0022215011907938. [DOI] [PubMed] [Google Scholar]
- 26.Prasanna A, Murthy PS. Combined stellate ganglion and sphenopalatine ganglion block in acute herpes infection. Clin J Pain. 1993;9(2):135–137. doi: 10.1097/00002508-199306000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Saberski L, Ahmad M, Wiske P. Sphenopalatine ganglion block for treatment of sinus arrest in postherpetic neuralgia. Headache. 1999;39(1):42–44. doi: 10.1046/j.1526-4610.1999.3901042.x. [DOI] [PubMed] [Google Scholar]
- 28.Amster J. Sphenopalatine ganglion block for the relief of painful vascular and muscular spasm with special reference to lumbosacral pain. N Y State J Med. 1948;48(22):2475. [PubMed] [Google Scholar]
- 29.Ruskin SL. The control of muscle spasm and arthritic pain through sympathetic block at the nasal ganglion and the use of the adenylic nucleotide. Am J Dig Dis. 1946;13(10):311–320. doi: 10.1007/BF03003575. [DOI] [PubMed] [Google Scholar]
- 30.Janzen VD, Scudds R. Sphenopalatine blocks in the treatment of pain in fibromyalgia and myofascial pain syndrome. Laryngoscope. 1997;107(10):1420–1422. doi: 10.1097/00005537-199710000-00023. [DOI] [PubMed] [Google Scholar]
- 31.Ferrante FM, Kaufman AG, Dunbar SA, Cain CF, Cherukuri S. Sphenopalatine ganglion block for the treatment of myofascial pain of the head, neck, and shoulders. Reg Anesth Pain Med. 1998;23(1):30–36. doi: 10.1016/s1098-7339(98)90108-0. [DOI] [PubMed] [Google Scholar]
- 32.Berger JJ, Pyles ST, Saga-Rumley SA. Does topical anesthesia of the sphenopalatine ganglion with cocaine or lidocaine relieve low back pain? Anesth Analg. 1986;65(6):700–702. doi: 10.1213/00000539-198606000-00025. [DOI] [PubMed] [Google Scholar]
- 33.Cohen S, Sakr A, Katyal S, Chopra D. Sphenopalatine ganglion block for postdural puncture headache. Anaesthesia. 2009;64(5):574–575. doi: 10.1111/j.1365-2044.2009.05925.x. [DOI] [PubMed] [Google Scholar]
- 34.Schaffer JT, Hunter BR, Ball KM, Weaver CS. Noninvasive sphenopalatine ganglion block for acute headache in the emergency department: a randomized placebo-controlled trial. Ann Emerg Med. 2015;65(5):503–510. doi: 10.1016/j.annemergmed.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 35.Rodman R, Dutton J. Endoscopic neural blockade for rhinogenic headache and facial pain: 2011 update. Int Forum Allergy Rhinol. 2012;2(4):325–330. doi: 10.1002/alr.21035. [DOI] [PubMed] [Google Scholar]
- 36.Henneberger JT, Menk EJ, Middaugh RE, Finstuen K. Sphenopalatine ganglion blocks for the treatment of nicotine addiction. South Med J. 1988;81(7):832–836. doi: 10.1097/00007611-198807000-00007. [DOI] [PubMed] [Google Scholar]
- 37.Silverman DG, Spencer RF, Kitahata LM, O'Connor TZ. Lack of effect of sphenopalatine ganglion block with intranasal lidocaine on submaximal effort tourniquet test pain. Reg Anesth. 1993;18(6):356–360. [PubMed] [Google Scholar]
- 38.Narouze S, Kapural L, Casanova J, Mekhail N. Sphenopalatine ganglion radiofrequency ablation for the management of chronic cluster headache. Headache: J Head Face Pain. 2009;49(4):571–577. doi: 10.1111/j.1526-4610.2008.01226.x. [DOI] [PubMed] [Google Scholar]
- 39.Sanders M, Zuurmond WW. Efficacy of sphenopalatine ganglion blockade in 66 patients suffering from cluster headache: a 12- to 70-month follow-up evaluation. J Neurosurg. 1997;87(6):876–880. doi: 10.3171/jns.1997.87.6.0876. [DOI] [PubMed] [Google Scholar]
- 40.Akbas M, Gunduz E, Sanli S, Yegin A. Sphenopalatine ganglion pulsed radiofrequency treatment in patients suffering from chronic face and head pain. Braz J Anesthesiol. 2016;66(1):50–54. doi: 10.1016/j.bjan.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 41.Schoenen J, Jensen RH, Lantéri-Minet M, Láinez MJ, Gaul C, Goodman AM, Caparso A, May A (2013) Stimulation of the sphenopalatine ganglion (SPG) for cluster headache treatment. Pathway CH-1: a randomized, sham-controlled study. Cephalalgia 0333102412473667 [DOI] [PMC free article] [PubMed]
- 42.Jürgens TP, Barloese M, May A, Láinez JM, Schoenen J, Gaul C, Goodman AM, Caparso A, Jensen RH (2016) Long-term effectiveness of sphenopalatine ganglion stimulation for cluster headache. Cephalalgia. 10.1177/0333102416649092 [DOI] [PMC free article] [PubMed]
- 43.Barloese MC, Jürgens TP, May A, Lainez JM, Schoenen J, Gaul C, Goodman AM, Caparso A, Jensen RH. Cluster headache attack remission with sphenopalatine ganglion stimulation: experiences in chronic cluster headache patients through 24 months. J Headache Pain. 2016;17(1):67. doi: 10.1186/s10194-016-0658-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ansarinia M, Rezai A, Tepper SJ, Steiner CP, Stump J, Stanton-Hicks M, Machado A, Narouze S. Electrical stimulation of sphenopalatine ganglion for acute treatment of cluster headaches. Headache: J Head Face Pain. 2010;50(7):1164–1174. doi: 10.1111/j.1526-4610.2010.01661.x. [DOI] [PubMed] [Google Scholar]
- 45.Tepper SJ, Rezai A, Narouze S, Steiner C, Mohajer P, Ansarinia M. Acute treatment of intractable migraine with sphenopalatine ganglion electrical stimulation. Headache. 2009;49(7):983–989. doi: 10.1111/j.1526-4610.2009.01451.x. [DOI] [PubMed] [Google Scholar]
- 46.William A, Azad TD, Brecher E, Cherry T, Bernstein I, Bruce DM, Rohrer S, Smith Z, William M, Sabelman E, Heit G, Pezeshkian P, Sedrak M. Trigeminal and sphenopalatine ganglion stimulation for intractable craniofacial pain--case series and literature review. Acta Neurochir. 2016;158(3):513–520. doi: 10.1007/s00701-015-2695-y. [DOI] [PubMed] [Google Scholar]
- 47.Elahi F, Reddy CG. Sphenopalatine ganglion electrical nerve stimulation implant for intractable facial pain. Pain Physician. 2015;18(3):E403–E409. [PubMed] [Google Scholar]
- 48.Ahamed SH, Jones NS. What is Sluder's neuralgia? J Laryngol Otol. 2003;117(6):437–443. doi: 10.1258/002221503321892253. [DOI] [PubMed] [Google Scholar]
- 49.Oomen KP, van Wijck AJ, Hordijk GJ, de Ru JA. Sluder's neuralgia: a trigeminal autonomic cephalalgia? Cephalalgia. 2010;30(3):360–364. doi: 10.1111/j.1468-2982.2009.01919.x. [DOI] [PubMed] [Google Scholar]
- 50.Salar G, Ori C, Iob I, Fiore D. Percutaneous thermocoagulation for sphenopalatine ganglion neuralgia. Acta Neurochir. 1987;84(1):24–28. doi: 10.1007/BF01456346. [DOI] [PubMed] [Google Scholar]
- 51.Slade SG, Linberg JV, Immediata AR. Control of lacrimal secretion after sphenopalatine ganglion block. Ophthal Plast Reconstr Surg. 1986;2(2):65–70. doi: 10.1097/00002341-198601050-00002. [DOI] [PubMed] [Google Scholar]
- 52.Devoghel JC. Cluster headache and sphenopalatine block. Acta Anaesthesiol Belg. 1981;32(1):101–107. [PubMed] [Google Scholar]
- 53.Yang IY, Oraee S. A novel approach to transnasal sphenopalatine ganglion injection. Pain Physician. 2006;9(2):131–134. [PubMed] [Google Scholar]
- 54.Zarembinski C, Graff-Radford S. An unusual challenge in performing sphenopalatine ganglion block with enlarged coronoid process: Jacob's disease. Pain Med. 2014;15(2):329–332. doi: 10.1111/pme.12302. [DOI] [PubMed] [Google Scholar]
- 55.Kastler A, Cadel G, Comte A, Gory G, Piccand V, Tavernier L, Kastler B. Alcohol percutaneous neurolysis of the sphenopalatine ganglion in the management of refractory cranio-facial pain. Neuroradiology. 2014;56(7):589–596. doi: 10.1007/s00234-014-1354-y. [DOI] [PubMed] [Google Scholar]
- 56.Maizels M. Intranasal lidocaine to prevent headache following migraine aura. Headache. 1999;39(6):439–442. doi: 10.1046/j.1526-4610.1999.3906439.x. [DOI] [PubMed] [Google Scholar]
- 57.Yarnitsky D, Goor-Aryeh I, Bajwa ZH, Ransil BI, Cutrer FM, Sottile A, Burstein R. 2003 Wolff award: possible parasympathetic contributions to peripheral and central sensitization during migraine. Headache: J Head Face Pain. 2003;43(7):704–714. doi: 10.1046/j.1526-4610.2003.03127.x. [DOI] [PubMed] [Google Scholar]
- 58.Prasanna A, Murthy PS. Sphenopalatine ganglion block and pain of cancer. J Pain Symptom Manag. 1993;8(3):125. doi: 10.1016/0885-3924(93)90139-M. [DOI] [PubMed] [Google Scholar]
- 59.Varghese BT, Koshy RC, Sebastian P, Joseph E. Combined sphenopalatine ganglion and mandibular nerve, neurolytic block for pain due to advanced head and neck cancer. Palliat Med. 2002;16(5):447–448. doi: 10.1191/0269216302pm549xx. [DOI] [PubMed] [Google Scholar]
- 60.Cohen S, Ramos D, Grubb W, Mellender S, Mohiuddin A, Chiricolo A. Sphenopalatine ganglion block: a safer alternative to epidural blood patch for postdural puncture headache. Reg Anesth Pain Med. 2014;39(6):563. doi: 10.1097/AAP.0000000000000172. [DOI] [PubMed] [Google Scholar]
- 61.Cardoso JM, Sá M, Graça R, Reis H, Almeida L, Pinheiro C, Machado D. Sphenopalatine ganglion block for postdural puncture headache in ambulatory setting. Rev Bras Anestesiol. 2017;67(3):311–313. doi: 10.1016/j.bjan.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 62.Ruskin SL. Contributions to the study of the spheno-palatine ganglion. Laryngoscope. 1925;35(2):87–108. doi: 10.1288/00005537-192502000-00001. [DOI] [Google Scholar]
- 63.Stechison MT, Brogan M. Transfacial transpterygomaxillary access to foramen rotundum, sphenopalatine ganglion, and the maxillary nerve in the management of atypical facial pain. Skull Basenn. 1994;4(1):15–20. doi: 10.1055/s-2008-1058983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Saade E, Paige GB. Patient-administered sphenopalatine ganglion block. Reg Anesth. 1996;21(1):68–70. [PubMed] [Google Scholar]
- 65.Puig CM, Driscoll CL, Kern EB. Sluder's sphenopalatine ganglion neuralgia--treatment with 88% phenol. Am J Rhinol. 1998;12(2):113–118. doi: 10.2500/105065898781390253. [DOI] [PubMed] [Google Scholar]
- 66.Windsor RE, Jahnke S. Sphenopalatine ganglion blockade: a review and proposed modification of the transnasal technique. Pain Physician. 2004;7(2):283–286. [PubMed] [Google Scholar]
- 67.Obah C, Fine PG. Intranasal sphenopalatine ganglion block: minimally invasive pharmacotherapy for refractory facial and headache pain. J Pain Palliat Care Pharmacother. 2006;20(3):57–59. [PubMed] [Google Scholar]
- 68.Morelli N, Mancuso M, Felisati G, Lozza P, Maccari A, Cafforio G, Gori S, Murri L, Guidetti D. Does sphenopalatine endoscopic ganglion block have an effect in paroxysmal hemicrania? A case report. Cephalalgia. 2010;30(3):365–367. doi: 10.1111/j.1468-2982.2009.01882.x. [DOI] [PubMed] [Google Scholar]
- 69.Grant GJ, Schechter D, Redai I, Lax J. Transnasal topical sphenopalatine ganglion block to treat tension headache in a pregnant patient. Int J Obstet Anesth. 2014;23(3):292–293. doi: 10.1016/j.ijoa.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 70.Androulakis XM, Krebs KA, Ashkenazi A. Hemicrania continua may respond to repetitive sphenopalatine ganglion block: a case report. Headache. 2016;56(3):573–579. doi: 10.1111/head.12783. [DOI] [PubMed] [Google Scholar]
- 71.Malec-Milewska M, Horosz B, Kosson D, Sekowska A, Kucia H. The effectiveness of neurolytic block of sphenopalatine ganglion using zygomatic approach for the management of trigeminal neuropathy. Neurol Neurochir Pol. 2015;49(6):389–394. doi: 10.1016/j.pjnns.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 72.Sussman WI, Mautner K, Mason RA, Bonecutter K, Shealy AK (2016) Sphenopalatine ganglion block for Management of Refractory Chronic Posttraumatic Headaches after a sport-related concussion. Clin J Sport Med. 10.1097/JSM.0000000000000325 [DOI] [PubMed]
- 73.Byrd H, Byrd W. Sphenopalatine phenomena: present status of knowledge. Arch Intern Med. 1930;46(6):1026–1038. doi: 10.1001/archinte.1930.00140180127013. [DOI] [Google Scholar]
- 74.Sparer W. Cessation of convulsive seizures following injection of alcohol into spheno-palatine ganglia. Three Cases The Laryngoscope. 1935;45(11):886–890. [Google Scholar]
- 75.Ruskin SL. A newer concept of arthritis and the treatment of arthritic pain and deformity by sympathetic block at the sphenopalatien (nasal) ganglion and the use of the iron salt of the adenylic nucleotide. Am J Dig Dis. 1949;16(11):386–401. doi: 10.1007/BF03002723. [DOI] [PubMed] [Google Scholar]
- 76.Quevedo JP, Purgavie K, Platt H, Strax TE. Complex regional pain syndrome involving the lower extremity: a report of 2 cases of sphenopalatine block as a treatment option. Arch Phys Med Rehabil. 2005;86(2):335–337. doi: 10.1016/j.apmr.2004.04.033. [DOI] [PubMed] [Google Scholar]
- 77.Triantafyllidi H, Arvaniti C, Palaiodimos L, Vlachos S, Schoinas A, Batistaki C, Kostopanagiotou G, Lekakis J. Infiltration of the sphenopalatine ganglion decreases blood pressure in newly diagnosed and never treated patients with essential hypertension. Int J Cardiol. 2016;223:345–351. doi: 10.1016/j.ijcard.2016.08.230. [DOI] [PubMed] [Google Scholar]
- 78.Chua NH, Vissers KC, Wilder-Smith OH. Quantitative sensory testing may predict response to sphenopalatine ganglion pulsed radiofrequency treatment in cluster headaches: a case series. Pain Pract. 2011;11(5):439–445. doi: 10.1111/j.1533-2500.2010.00445.x. [DOI] [PubMed] [Google Scholar]
- 79.Oomen KP, van Wijck AJ, Hordijk GJ, de Ru JA. Effects of radiofrequency thermocoagulation of the sphenopalatine ganglion on headache and facial pain: correlation with diagnosis. J Orofac Pain. 2012;26(1):59–64. [PubMed] [Google Scholar]
- 80.Fang L, Jingjing L, Ying S, Lan M, Tao W, Nan J. Computerized tomography-guided sphenopalatine ganglion pulsed radiofrequency treatment in 16 patients with refractory cluster headaches: twelve- to 30-month follow-up evaluations. Cephalalgia. 2016;36(2):106–112. doi: 10.1177/0333102415580113. [DOI] [PubMed] [Google Scholar]
- 81.Bendersky DC, Hem SM, Yampolsky CG. Unsuccessful pulsed radiofrequency of the sphenopalatine ganglion in patients with chronic cluster headache and subsequent successful thermocoagulation. Pain Pract. 2015;15(5):E40–E45. doi: 10.1111/papr.12288. [DOI] [PubMed] [Google Scholar]
- 82.Dharmavaram SKA, Palanisamy V, Raju SK (2016) Conventional radiofrequency ablation of sphenopalatine ganglion for the treatment of cluster headache. Indian J Pain 30
- 83.Loomba V, Upadhyay A, Kaveeshvar H. Radiofrequency ablation of the Sphenopalatine ganglion using cone beam computed tomography for intractable cluster headache. Pain Physician. 2016;19(7):E1093–E1096. [PubMed] [Google Scholar]
- 84.Shah RV, Racz GB. Long-term relief of posttraumatic headache by sphenopalatine ganglion pulsed radiofrequency lesioning: a case report. Arch Phys Med Rehabil. 2004;85(6):1013–1016. doi: 10.1016/j.apmr.2003.07.017. [DOI] [PubMed] [Google Scholar]
- 85.Bayer E, Racz GB, Miles D, Heavner J. Sphenopalatine ganglion pulsed radiofrequency treatment in 30 patients suffering from chronic face and head pain. Pain Pract. 2005;5(3):223–227. doi: 10.1111/j.1533-2500.2005.05314.x. [DOI] [PubMed] [Google Scholar]
- 86.Nguyen M, Wilkes D. Pulsed radiofrequency V2 treatment and intranasal sphenopalatine ganglion block: a combination therapy for atypical trigeminal neuralgia. Pain Pract. 2010;10(4):370–374. doi: 10.1111/j.1533-2500.2010.00382.x. [DOI] [PubMed] [Google Scholar]
- 87.Elahi F, Ho KWD. Case report in neurological medicine. 2014. Successful Management of Refractory headache and facial pain due to cavernous sinus Meningioma with Sphenopalatine ganglion radiofrequency. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Meng DW, Zhang JG, Zheng Z, Wang X, Luo F, Zhang K. Chronic bilateral Sphenopalatine ganglion stimulation for intractable bilateral chronic cluster headache: a case report. Pain Physician. 2016;19(4):E637–E642. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


