Abstract
AIM
To evaluate the influence of the titanium nitride (TiN) coating on the results of a total knee arthroplasty (TKA).
METHODS
A total of 910 patients (338 men; 572 woman), with a mean age of 65 (range 36-94) undergoing 1031 primary TKAs were assessed. Clinical evaluation and patient-reported outcomes were gathered one year after surgery. The questionnaires included the Knee injury and Osteoarthritis Outcome Score (KOOS)-Dutch version, Visual Analogue Scale (VAS) pain scores in rest and during active knee movement, VAS-satisfaction scores, and EQ-5D-3L health scores. This was aimed to assess the overall knee function and patient satisfaction, and to enable us to make a gross comparison to other TKAs.
RESULTS
At a mean follow-up of 46 mo (range 1-92) the overall implant survival was 97.7% and 95.1% for any operative reason related to the implant. Twenty-three knees (2.2%) required revision surgery. Arthrofibrosis was the most common indication for a re-operation. The clinical evaluation and patient-reported outcomes revealed good to excellent patient satisfaction and function of the arthroplasty. The median postoperative VAS-pain scores on a scale of 0-100, at one year after surgery were 1 in rest and 2 during movement.
CONCLUSION
The TiN coated, mobile bearing TKA results are excellent and similar to those of other widely used TKA designs. Residual pain of the knee remains a concern and the TiN coating in combination with the mobile bearing does not seem to be the simple solution to this problem. Future research will have to show that the coating gives a better survival than the cobalt chrome version.
Keywords: Total knee arthroplasty, Titanium nitride coating, Mobile bearing, Pain, Satisfaction and survival
Core tip: The titanium nitride coated, mobile bearing total knee arthroplasty (TKA) results are excellent and similar to those of other widely used TKA designs.
INTRODUCTION
Total knee arthroplasty (TKA) is the golden standard treatment for treating patients with end stage Osteoarthritis, and although very successful, approximately 10% of patients experience residual pain[1]. In the last 20-30 years much research have been done and many theories have been proposed to explain this residual pain. Today most TKA manufacturers use approximately the same design, but small differences in the used materials and coatings, make each arthroplasty unique. Each small change to a well renowned arthroplasty system needs to be evaluated.
Although fixed bearing designs have revealed a high degree of clinical success over the past decades, implant loosening and polyethylene wear were regularly causes for failure[2,3]. In the 1970’s, Buechel and Pappas introduced the (LCS-system) mobile bearing in TKAs, hereby trying to reduce polyethylene contact stress and therefore wear[4]. Although the mobile bearing achieves excellent results, literature is not clear whether a mobile bearing is better than a fixed bearing TKA. Some studies show a difference, yet others show no significant differences between fixed- and mobile bearing TKAs[5-9]. Today most femur and tibia components used, are made of cobalt-chromium-molybdenum (CoCrMo) alloy[10].
Titanium nitride (TiN) is a ceramic, which is regularly used as a coating to enhance other materials with the properties of TiN. This coating is administered to a wide variety of implants used in cardiac-, neurologic-, dental- and orthopaedic surgery[11-13]. Beneficial properties of TiN include hardness, more scratch resistant, a smoother surface, less adhesion to polyethylene and a more wettable surface[10,14-16]. The TiN coating is thought to reduce the wear of Polyethylene and the potential for wear debris induced osteolysis, which today is still a considerable cause for revision surgery[2,3]. Furthermore In vitro studies have shown that Cobalt en Chrome ions can induce an inflammatory response, thus induce pain and swelling[10]. Adding the TiN coating to the CoCrMo TKA system, is thought to reduce the release of Cobalt and Chrome ions[10].
The primary goal is to report if the TiN coating in a mobile bearing TKA has any influence on the clinical outcome, patient satisfaction and the mid term implant survival of the TKA. This TiN TKA has been used in several clinics the last decade. Yet, little is published or reported about the clinical outcome and survival[10,14,15].
MATERIALS AND METHODS
All patients that had received a primary ACS® (Implantcast, Buxtehude, Germany) TiN mobile bearing TKA, between February 2007 and April 2012 in our clinic, were included in this study. The data for all included patients was collected up until October 2014, by utilizing the clinics’ database and by contacting patients if any necessary data was missing. No patients were excluded on the basis of the severity of their disease or deformity of the knee. Patient sex, age, BMI, ASA-class (American Society of Anaesthesiology), arthroplasty side, component sizing and use of posterior stabilised components were gathered as baseline patient characteristics. Informed consent was obtained from all individual participants included in this study.
The Primary endpoints were defined as true revisions, defined as exchange of the tibial and/or femoral component, and secondary resurfacing of the patella. Secondary endpoints were defined as “revision for any reason” and included also open and arthroscopic arthrolysis, exchange of the polyethylene liner, and realignment of the patella. All patients were asked to complete a questionnaire at 1 year following primary TKA. The questionnaire included the Knee injury and Osteoarthritis Outcome Score (KOOS)-Dutch version[17], Visual Analogue Scale (VAS) pain scores in rest and during active knee movement, VAS-satisfaction scores, and EQ-5D-3L health scores. This was aimed to assess the overall knee function and patient satisfaction, and to enable us to make a gross comparison to other TKAs.
Operative technique
Three orthopaedic surgeons within the same orthopedic clinic performed all TKAs, with osteoarthritis being the most common indication for surgery. Patients underwent either a general- or spinal-anaesthetic and all patients received a locally infiltrated anaesthetic (LIA) at the end of surgery. All patients received perioperative antibiotic prophylaxis for 24 h. A straight longitudinal incision was made to expose the knee joint. A surgical tourniquet was used during all TKAs. All prostheses were fixed using bone cement. Postoperative thrombo-profylaxis was administered in the form of daily subcutaneous injections with Low Molecular Weight Heparin (LMWH) and use of a Trombo Embolism Deterrent (TED) stocking during 4 wk after surgery. Physical therapy was prescribed generally starting two weeks after surgery.
Statistical analysis
Survival analyses were performed using the Kaplan-Meier methods and cumulative survival rates were calculated with 95%CI for both true revision and revision for any reason as endpoints. Patients who died with the implant intact or who were lost to follow up were identified from patient files, and the follow-up time for these patients was censored at the date of death or last clinical or telephone based contact. Multivariate Cox regression analysis was performed to assess the association between potential risk factors (age, BMI, ASA, component sizing and indication) and revision. The KOOS, VAS-pain and satisfaction, and EQ-5D scores are described as medians with accompanying interquartile ranges (IRQ). Comparisons between the revision and non-revision group were performed by use of Mann Whitney U-tests. Statistical analysis was performed with the use of SPSS 24.0 (Armonk, NY: IBM Corp). A P-value < 0.05 was considered statistically significant.
RESULTS
A total of 910 patients with 1031 Primary ACS arthroplasties, performed by 3 orthopaedic surgeons, were identified from the database. This included 338 male (37.1%) and 572 female (62.9%) patients, with a mean age of 65.4 years (range 36-94) at time of surgery.
The arthroplasties were performed in 52.7% (n = 543) on the right side, and in 47.3% (n = 488) on the left. A total of 121 patients had received bilateral arthroplasty between 2007 and 2012. Mean BMI was 28.7 (range 20.4-47.3). 26.3% of patients had an ASA-score of 1, 67.8% had an ASA-score of 2 and 5.9% had an ASA-score of 3.
Clinical outcomes at 1 year after surgery
A total of 671 patients (65%) had filled out the questionnaires at one year after primary TKA (Table 1). The KOOS measured at 1 year after surgery showed generally good levels of function during activities of daily life (ADL), pain, and symptoms with a median scores of 89 (IQR: 70-97), 92 (IQR: 72-100), 86 (IQR: 71-93), respectively. The domains “sport/rec” and “QoL” had median values of 40 (IQR: 15-70) and 69 (IQR: 50-88), respectively. In all but the “sports and recreational function” subscale of the KOOS, patients without required revision surgery scored significant higher scores (P-value < 0.01) then the revision group (Table 1).
Table 1.
Comparisons of clinical outcomes 1 year after primary total knee arthroplasty (medians with interquartile ranges)
| Arthroplasty in situ (n = 663) | Revised (n = 8) | P value | |
| KOOS-pain | 92 (72; 100) | 64 (42; 72) | < 0.01 |
| KOOS-sympt | 86 (71; 93) | 68 (56; 78) | < 0.01 |
| KOOS-adl | 89 (70; 97) | 59 (51; 75) | < 0.01 |
| KOOS-sport | 40 (15; 70) | 33 (6; 65) | 0.56 |
| KOOS-qol | 69 (50; 88) | 38 (38; 55) | < 0.01 |
| VAS-pain (rest) | 1 (0; 7) | 8 (1; 61) | 0.06 |
| VAS-pain (activity) | 2 (0; 13) | 18 (3; 40) | 0.03 |
| VAS-satisfaction | 91 (70; 100) | 45 (14; 38) | < 0.01 |
| EQ-5D | 0.84 (0.78; 1.0) | 0.76 (0.35; 0.78) | < 0.01 |
| EQ-5D-VAS | 80 (70; 90) | 71 (50; 89) | 0.26 |
KOOS: Knee injury and osteoarthritis outcome score; VAS: Visual analogue scale.
The median postoperative VAS-pain scores on a scale of 0-100, at one year after surgery were 1 in rest and 2 during movement of the joint in the non-revision group. The patients that required a revision operation scored significantly higher VAS scores during activity (P = 0.03).
Overall patient satisfaction levels were good, revealing a median VAS-satisfaction score of 91 (IQR: 70-100) out of 100 in the non-revised, vs 45 (IQR: 14-38) out of 100 in the revision group at one year following primary surgery. This difference was statistically significant (P < 0.01).
At one year after surgery patients reported high levels of health-related quality of life. There was a significant difference (P < 0.01) in the EQ-5D scores between the revised and non-revised TKA scores, with the revision group showing lower scores corresponding with a lower quality of life (Table 1).
Component sizing
Table 2 shows the overall use of arthroplasty sizes utilised in this study. Size 4 femoral and tibial components were the most frequently implanted (both 38%) with a 10 mm thick liner (53%). Twelve female knee replacements were done using a Gender-specific, also known as a Slim-variety, arthroplasty. In 18 cases, use of a Posterior Stabilised (PS) femoral component with matching PS-liner was deemed necessary to acquire a peri-operative stable knee joint. All but two TKAs were primarily implanted without a patellar component. In these two cases peri-operative patellar tracking was suboptimal due to heavy wear and severe deformation of the patella and/or trochlea. The size of the components was not significantly associated with revision rates for component exchange as well as revisions for any reason (0.22 < P < 0.72).
Table 2.
Implant component sizing (n = 1031)
| Component size femur | n (%) | Component size tibia | n (%) | Size liner | n (%) |
| 2 | 5 (0.5) | 3 | 57 (5.6) | 10 | 545 (53) |
| 3 | 257 (25.0) | 4 | 386 (37.6) | 12.5 | 394 (38.2) |
| 4 | 390 (37.9) | 5 | 287 (27.9) | 15 | 80 (7.8) |
| 5 | 280 (27.2) | 6 | 221 (21.5) | 17.5 | 8 (0.8) |
| 6 | 97 (7.4) | 7 | 76 (7.4) | 20 | 2 (0.2) |
| Missing | 2 | Missing | 4 | Missing | 2 |
Survival analysis
The mean follow-up period of all 1031 patients was 46 mo, ranging from 1 to 92 mo. Overall arthroplasty survival for component exchange was 97.7% (95%CI: 97.2-98.2) and 95.1% (95%CI: 94.4-95.8) for revision for any reason. Seventeen patients (18 TKAs) had died due to causes unrelated to knee surgery after a mean follow-up of 30.1 mo (range: 9 to 56) (Figure 1).
Figure 1.
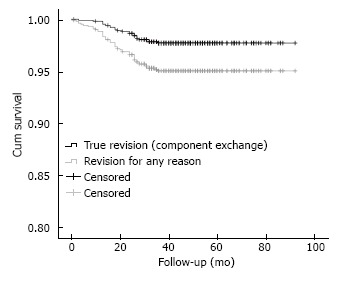
Kaplan-Meier survival curves of the ACS total knee arthroplasty for both True revision (component exchange and revision for any reason).
A total of 23 (2.2%) TKAs required revision surgery of at least one component of the TKA or addition of a patellar button. All revisions were performed within the first three years postoperatively. Mean time to revision was 21 mo (range: 3 to 36). Revision of six tibial components was performed due to malpositioning at primary surgery, two of which also required addition of a patellar button. In five cases revision was required following a traumatic event, resulting in periprosthetic bone fractures, and muscle-/ligament tears. One of which, revision of the femoral component was necessary at 27 mo, after a fracture of the femur was caused during manipulation under narcosis, at five months after primary TKA. Revision surgery was performed on 2 patients due to infection of the TKA. Revision surgery of the total joint was performed in two stages with addition of antibiotic treatment. These treatments proved successful as the revised TKAs are still implanted.
Isolated Patellofemoral (PF) pain occurred in four patients after TKA and required addition of a patellar component. Two patients had PF pain accompanied by non-traumatic instability and required polyethylene exchange along with the addition of a patellar component. One patient reported PF pain and instability after a traumatic event for which PE exchange and addition of a patellar component was performed. Arthrofibrosis combined with PF pain was seen in four patients. In these cases addition of a patellar component was done along with an arthrolysis and in three cases removal of the liner was necessary to release the posterior capsule. An implantation of a patellar component was necessary to improve patellar tracking along the trochlea.
Revision for other reasons in terms open and arthroscopic arthrolysis, exchange of the polyethylene liner, and realignment of the patella, was performed in an additional 27 patients (2.6%), resulting in a total amount of 50 revisions for any reason (4.8%) with a mean time to revision of 18 mo (range 1 to 36). Of these 27 procedures, seventeen knees (34% of all revisions for any reason) required an open release for which the PE needed to be removed, eight knees (16%) required an open arthrolysis without PE exchange, one knee (2%) was arthroscopically released and in one knee (2%) an arthroscopic lavage was done, followed by antibiotic treatment due to an infection of the knee.
Five patients required open arthrolysis with exchange of the polyethylene liner. In three of these cases no clear improvement of the ROM was achieved by a manipulation under anaesthesia (MUA). One patient suffered from periarticular ossifications (PAO’s), which were excised at 13 mo after surgery and therefore required polyethylene exchange. In one case, the patient had complaints of a large fabella for which removal of the PE was needed to gain access for excision. Five patients suffered from joint instability after a traumatic event, and four patients had complaints of instability following primary surgery without any clear trauma. One early infection (within 1 mo) was treated with arthroscopic lavage followed by an additional treatment. Of the eight TKAs that received an open procedure without PE exchange, seven patients underwent arthrolysis for arthrofibrosis, of which two cases required additional realignment of the patella without implantation of a patellar button. One patient had complaints of a Corpus Liberum (CL) that required removal. On inspection, there was no visible damage caused by the CL.
In one case amputation of the lower limb was necessary within the first month after surgery, due to a rupture of a pseudo-aneurysm. This lead to a compartment syndrome, which was detected too late due to an epidural anaesthesia.
MUA was performed in 33 knees (3.2%) at a mean follow up time of 4.1 (range 1-8) mo. In three cases MUA was followed by an open release, for which PE exchange was also necessary and in one case by component exchange. All TKAs that required MUA suffered from arthrofibrosis that limited the functional Range of Motion (ROM) of 90 degrees of flexion or full extension. Patient age, gender, BMI and ASA-class were not significantly associated with true revision as well as revision for any reason (0.38 < P < 0.99).
DISCUSSION
In this large retrospective review of a TiN coated mobile bearing TKA, good to excellent scores were achieved and a very low pain scores. A median postoperative VAS pain scores in a scale of 0-100, at one year after surgery were 1 in rest and 2 during movement of the joint. The median reported KOOS-pain scores were 92. These reported pain scores seem to be comparable with the reported VAS-pain scores reported by Moon et al[18] of 1.4 (in de “Buechel and Pappas” total knee group) and 1.8 (in the “NexGen-LPS” total knee group). Therefore the results of the TiN coated mobile bearing TKA concur with the results of the CoCrMo mobile bearing TKA, and are not superior or inferior to the CoCrMo mobile bearing TKA[18,19].
It was suggested in the literature, that the TiN coating could protect the synovium of the knee for the release of Co and Cr ions[10]. In vitro studies have shown that Co en Cr ions can induce an inflammatory response, thus induce pain and swelling[10]. Van Hove et al[10] compared the TiN coating to a CoCrMo mobile bearing TKA and found no difference in postoperative pain scores or inflammation between the two groups. So the hypothesis that the TiN coating could make a difference in the direct post operative period, does not seem to be the case, our results are comparable to the CoCrMo mobile bearing TKA.
Another reason for our group to use the mobile bearing TKA is the low number of patients with anterior knee pain or PF pain after a TKA. Resurfacing or nor resurfacing the patella during primary TKA still remains controversial[1,20]. Anterior knee pain after TKA could have multiple causes and is not solely caused by not resurfacing the patella during primary surgery. In our series all but two TKAs in this study were implanted without the use of a patellar component. Later 10 Patients (1.0%) suffered from PF pain and required a secondary resurfacing of the patella. Thus in our series, more than 1000 knees were not resurfaced with a patella, this may further support the theory that resurfacing of the patella is not strictly necessary in primary mobile bearing TKA[20-22]. There are some limitations in this study with regard to this dilemma. We did not specifically ask questions regarding PF pain or quantify that amount of pain. Although the completed questionnaires can give some insight in the overall knee function and pain scores, they do not isolate PF pain. We only have data on PF pain if this resulted in the secondary resurfacing of the patella.
Patient satisfaction were good, revealing a median VAS-satisfaction score of 91 (IQR 70-100) out of 100 in the non-revised, vs 45 (IQR: 14-38) out of 100 in the revision group at one year following primary surgery. This difference was statistically significant (P < 0.01). At one year after surgery patients reported high levels of health-related quality of life. There was a significant difference (P < 0.01) in the EQ-5D scores between the revised and non-revised TKA scores, with the revision group showing lower scores corresponding with a lower quality of life. The impact of a revision or secondary operation can be revealed in this way.
The TiN coating of the CoCrMo TKA could be beneficial to patients with a metal allergy, especially those with a known nickel sensitivity[23]. This precludes them from receiving a CoCrMo alloyed arthroplasty. Due to the increase in the number of TKAs performed annually; the amount of patients with a painful well-implanted TKA is also thought to increase. If a patient is known with a metal allergy, it is advised to perform an anallergic implant, like the TiN coated implants.
MUA was performed in 33 (3.2%) cases, and this is in unison with the widely reported prevalence of 1.3%-12%[8]. For all but 3 patients in our study, a single MUA followed by intensive physical therapy was sufficient to improve ROM to a functional level of > 90 degrees of flexion and full extension. An additional open release was necessary in the above-mentioned three patients following MUA to regain a functional ROM.
The TiN coating is thought to reduce the wear of Polyethylene and the potential for wear debris induced osteolysis, which today is still a considerable cause for revision surgery[2,3]. This is thought to be due to the beneficial properties of TiN coating, they include: The hardness, more scratch resistant, a smoother surface, less adhesion to polyethylene and a more wettable surface[10,14-16]. In this series a survival of 97.7% at a mean follow-up period of 46 mo was found. This is comparable to the survivorship of other TKAs. The survival of conventional knee arthroplasties, using fixed bearing implants, ranges from 90%-95% of > 10 years[18]. Beuchel et al[19] reported a 20 year survival of the LCS cemented rotating platform TKA of 97.7%. Jordan et al[24] reported survivorship of 94.8% at 8 years of the meniscal-bearing TKA. All retrieved polyethylene liners were inspected for wear during revision surgery. There were no reports of significant wear of the retrieved liners. The mean revision period of 21 mo is however, arguably too short to reveal high levels, if any, of polyethylene wear. Whether or not the addition of a TiN coating of a mobile bearing TKA reduces polyethylene wear and thus enhance the survival of the arthroplasty needs to be further investigated in the upcoming years.
Results of this study should be interpreted taking into account the limitations inherent to retrospective studies. Additionally, the response rate of completed questionnaires was 65%. This percentage might be susceptible to selection bias. A limitation of our study is due to lack of pre-operative pain scores, it is however not possible to quantify the improvement of patient reported pain after TKA.
In conclusion the ACS TiN mobile bearing TKA is a reliable arthroplasty yielding good to excellent clinical results, with a high level of function and low revision rates at a mean follow-up of 46 mo after surgery. Based on the outcomes of this study, the use of the ACS TiN coated, mobile bearing TKA appears to be justified and will be used as our primary TKA. Further research is necessary to investigate long-term survival of the arthroplasty and whether or not the addition of the TiN coating is beneficial for polyethylene wear.
ARTICLE HIGHLIGHTS
Research background
Evaluate the influence of the titanium nitride (TiN) coating on the results of a total knee arthroplasty (TKA).
Research motivation
Very little is known about the influence of the TiN coating on the results of a TKA.
Research objectives
Evaluate the overall clinical outcome, evaluating pain and patient satisfaction and the mid-term implant survival.
Research methods
A total of 910 patients (338 men; 572 woman), with a mean age of 65 (range 36-94) undergoing 1031 primary TKAs were assessed. Clinical evaluation and patient-reported outcomes were gathered one year after surgery. The questionnaires included the Knee injury and Osteoarthritis Outcome Score (KOOS)-Dutch version, Visual Analogue Scale (VAS) pain scores in rest and during active knee movement, VAS-satisfaction scores, and EQ-5D-3L health scores. This was aimed to assess the overall knee function and patient satisfaction, and to enable us to make a gross comparison to other TKAs.
Research results
At a mean follow-up of 46 mo (range 1-92) the overall implant survival was 97.7% and 95.1% for any operative reason related to the implant. Twenty-three knees (2.2%) required revision surgery. Arthrofibrosis was the most common indication for a re-operation. The clinical evaluation and patient-reported outcomes revealed good to excellent patient satisfaction and function of the arthroplasty. The median postoperative VAS-pain scores on a scale of 0-100, at one year after surgery were 1 in rest and 2 during movement.
Research conclusion
The TiN coated, mobile bearing TKA results are excellent and similar to those of other widely used TKA designs. Residual pain of the knee remains a concern and the TiN coating in combination with the mobile bearing does not seem to be the simple solution to this problem. Future research will have to show that the coating gives a better survival than the cobalt chrome version.
ACKNOWLEDGMENTS
We would like to thank Drs. Karin van Dorp, Paulien van Kampen, Hellen Welling, Nienke Bruijn, Dirk Jan de Jong and his team of physiotherapist for their help in performing this study.
Footnotes
Institutional review board statement: This was not necessary seeing that is a retrospective case series.
Informed consent statement: All the patients included in the study gave an informed consent.
Conflict-of-interest statement: No potential conflicts of interest. No financial support.
Data sharing statement: The authors are willing to share the data of the present study.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: The Netherlands
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
Peer-review started: August 7, 2017
First decision: September 4, 2017
Article in press: November 10, 2017
P- Reviewer: Chen YK, Cui Q, Hooper GJ, Li JM S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
Contributor Information
Stefan J M Breugem, Orthopedium, Orthopedic Clinic, Delft 2616 LS, The Netherlands.
Jeroen Linnartz, Orthopedium, Orthopedic Clinic, Delft 2616 LS, The Netherlands.
Inger Sierevelt, Slotervaart Hospital, Amsterdam 1066 EC, The Netherlands.
Jon D Bruijn, Orthopedium, Orthopedic Clinic, Delft 2616 LS, The Netherlands.
Marcel J M Driessen, Orthopedium, Orthopedic Clinic, Delft 2616 LS, The Netherlands.
References
- 1.Breugem SJ, Haverkamp D. Anterior knee pain after a total knee arthroplasty: What can cause this pain? World J Orthop. 2014;5:163–170. doi: 10.5312/wjo.v5.i3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hooper G, Rothwell A, Frampton C. The low contact stress mobile-bearing total knee replacement: a prospective study with a minimum follow-up of ten years. J Bone Joint Surg Br. 2009;91:58–63. doi: 10.1302/0301-620X.91B1.20484. [DOI] [PubMed] [Google Scholar]
- 3.Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010;468:45–51. doi: 10.1007/s11999-009-0945-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haider H, Garvin K. Rotating platform versus fixed-bearing total knees: an in vitro study of wear. Clin Orthop Relat Res. 2008;466:2677–2685. doi: 10.1007/s11999-008-0463-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vogt JC, Saarbach C. LCS mobile-bearing total knee replacement. A 10-year’s follow-up study. Orthop Traumatol Surg Res. 2009;95:177–182. doi: 10.1016/j.otsr.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 6.Kim TK. CORR Insights®: Rotating-platform TKA no different from fixed-bearing TKA regarding survivorship or performance: a meta-analysis. Clin Orthop Relat Res. 2014;472:2194–2196. doi: 10.1007/s11999-014-3584-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Callaghan JJ. Mobile-bearing knee replacement: clinical results: a review of the literature. Clin Orthop Relat Res. 2001;(392):221–225. doi: 10.1097/00003086-200111000-00027. [DOI] [PubMed] [Google Scholar]
- 8.Parvizi J, Tarity TD, Steinbeck MJ, Politi RG, Joshi A, Purtill JJ, Sharkey PF. Management of stiffness following total knee arthroplasty. J Bone Joint Surg Am. 2006;88 Suppl 4:175–181. doi: 10.2106/JBJS.F.00608. [DOI] [PubMed] [Google Scholar]
- 9.Huang CH, Liau JJ, Cheng CK. Fixed or mobile-bearing total knee arthroplasty. J Orthop Surg Res. 2007;2:1. doi: 10.1186/1749-799X-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Hove RP, Brohet RM, van Royen BJ, Nolte PA. No clinical benefit of titanium nitride coating in cementless mobile-bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23:1833–1840. doi: 10.1007/s00167-014-3359-9. [DOI] [PubMed] [Google Scholar]
- 11.Sin DC, Kei HL, Miao X. Surface coatings for ventricular assist devices. Expert Rev Med Devices. 2009;6:51–60. doi: 10.1586/17434440.6.1.51. [DOI] [PubMed] [Google Scholar]
- 12.Cogan SF. Neural stimulation and recording electrodes. Annu Rev Biomed Eng. 2008;10:275–309. doi: 10.1146/annurev.bioeng.10.061807.160518. [DOI] [PubMed] [Google Scholar]
- 13.Mezger PR, Creugers NH. Titanium nitride coatings in clinical dentistry. J Dent. 1992;20:342–344. doi: 10.1016/0300-5712(92)90021-4. [DOI] [PubMed] [Google Scholar]
- 14.van Hove RP, Sierevelt IN, van Royen BJ, Nolte PA. Titanium-Nitride Coating of Orthopaedic Implants: A Review of the Literature. Biomed Res Int. 2015;2015:485975. doi: 10.1155/2015/485975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mohammed A, Metcalfe A, Woodnutt D. Medium-term outcome of titanium nitride, mobile bearing total knee replacement. Acta Orthop Belg. 2014;80:269–275. [PubMed] [Google Scholar]
- 16.Galetz MC, Seiferth SH, Theile B, Glatzel U. Potential for adhesive wear in friction couples of UHMWPE running against oxidized zirconium, titanium nitride coatings, and cobalt-chromium alloys. J Biomed Mater Res B Appl Biomater. 2010;93:468–475. doi: 10.1002/jbm.b.31604. [DOI] [PubMed] [Google Scholar]
- 17.de Groot IB, Favejee MM, Reijman M, Verhaar JA, Terwee CB. The Dutch version of the Knee Injury and Osteoarthritis Outcome Score: a validation study. Health Qual Life Outcomes. 2008;6:16. doi: 10.1186/1477-7525-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moon KH, Hong SH, Hong TH. Total knee replacement arthroplasty with Buechel and Pappas knee: minimum 2-year follow-up. Clin Orthop Surg. 2015;7:62–68. doi: 10.4055/cios.2015.7.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buechel FF Sr, Buechel FF Jr, Pappas MJ, D’Alessio J. Twenty-year evaluation of meniscal bearing and rotating platform knee replacements. Clin Orthop Relat Res. 2001;388:41–50. doi: 10.1097/00003086-200107000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Fu Y, Wang G, Fu Q. Patellar resurfacing in total knee arthroplasty for osteoarthritis: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2011;19:1460–1466. doi: 10.1007/s00167-010-1365-0. [DOI] [PubMed] [Google Scholar]
- 21.Johnson TC, Tatman PJ, Mehle S, Gioe TJ. Revision surgery for patellofemoral problems: should we always resurface? Clin Orthop Relat Res. 2012;470:211–219. doi: 10.1007/s11999-011-2036-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wyatt MC, Frampton C, Horne JG, Devane P. Mobile- versus fixed-bearing modern total knee replacements- which is the more patella-friendly design?: The 11-year New Zealand Joint Registry study. Bone Joint Res. 2013;2:129–131. doi: 10.1302/2046-3758.27.2000159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Faschingbauer M, Renner L, Boettner F. Allergy in Total Knee Replacement. Does It Exist?: Review Article. HSS J. 2017;13:12–19. doi: 10.1007/s11420-016-9514-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jordan LR, Olivo JL, Voorhorst PE. Survivorship analysis of cementless meniscal bearing total knee arthroplasty. Clin Orthop Relat Res. 1997;338:119–123. doi: 10.1097/00003086-199705000-00018. [DOI] [PubMed] [Google Scholar]


