Periventricular leukomalacia (PVL), a white matter injury (WMI) affecting the premature infant's brain is commonly associated with cerebral palsy (CP). Among premature infants < 1,500 g, approximately 7,000 develop CP yearly and 20,000–30,000 exhibit major cognitive deficits yearly (Volpe, 2009). PVL results from hypoxia-ischemia (HI) with or without infection and is characterized by white matter necrotic lesions, hypomyelination, microglial activation, astrogliosis, and neuronal death. Risk factors for the development of PVL include: prematurity associated with immature cerebrovascular development, HI insults with lack of appropriate auto-regulation of cerebral blood flow, free radical production, energy deprivation, intrauterine infection and chorioamnionitis. Affected infants show definitive signs of cerebral palsy such as spastic diplegia, seizures, developmental delay, visual and hearing impairment, scoliosis and incontinence by 6–9 months of age. PVL can also occur in term infants with certain congenital cyanotic heart disease which will not be our focus here (Volpe, 2001).
Timing of PVL and developmental sequelae: PVL is most common between 23–30 weeks gestation. After 24 weeks, there is axon and dendrite formation, differentiation synaptogenesis, myelination and synaptic pruning and development of circuitry. This developmental process persists up to 2 years after birth. Therefore, any injury in this stage will lead to developmental disturbance (Volpe, 2009).
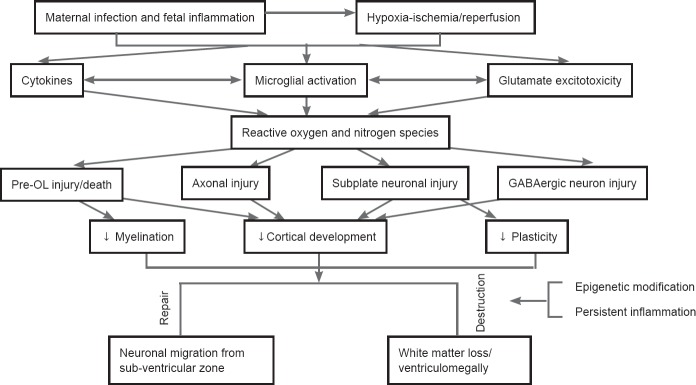
Etiology of PVL: There are two major etiologies of PVL: HI and infection/inflammation causing a fetal inflammatory response. Many factors play a pivotal role in the pathogenesis of PVL and increase preterm neonate susceptibility to develop HI, including arterial end and border zones in the periventricular white matter, pressure-passive circulation without autoregulation and the susceptibility of premyelinating oligodendrocytes (pre-OLs) to both reactive oxidative (ROS) and nitrative stress (RNS) and excitotoxicity caused by accumulation of injurious extracellular glutamate (Rumajogee et al., 2016). Preterm infants have deficient antioxidant system and have increased expression of glutamate receptors and glutamate transporter as compared to full term infants. HI leads to decreased glutamate uptake by the neurons and astrocytes. The accumulation of extracellular glutamate, reversal of glutamate transporter function in astrocytes and oligodendrocytes (OLs) and the lack of reuptake further potentiates glutamate excitotoxicity (Fern et al, 2001). Reperfusion of ischemic tissues is associated with microvascular and endothelial injury, production of more ROS and RNS and triggers more inflammatory response. Infection and/or systemic inflammation, which are seen in neonates born with chorioamnionitis and/or umbilical cord vasculitis, induce a systemic increase in pro-inflammatory cytokines. In these cases, brain injury is caused by sustained inflammatory response rather than passage of microbes, proven by lack of granulocytes in the brain.
Types of WMI: WMI is the broader category and is divided into PVL and diffuse white matter gliosis without focal necrosis (no leukomalacia) as indicated by neuropathological studies. PVL is further divided neuropathologically into 3 categories based on severity: focal necrosis cystic (> 5 mm), focal necrosis non cystic (2–3 mm) and diffuse microscopic necrosis (Volpe, 2017). Due to advances in medical management and care of preterm infants, focal lesions are rarely seen. Focal lesions involve necrosis of all tissue causing cavitary lesions surrounded by astrogliosis and microgliosis, and loss of neuronal axons. Anatomically, focal lesions occur along the distribution of the end zones of the long penetrating arteries. The diffuse type of PVL with microscopic necrosis is caused by a decrease in white matter thickness leading to ventriculomegaly. Diffuse type is also associated with astrogliosis and microgliosis. Anatomically, diffuse lesions occur in the distributions of the border zones between the long penetrating arteries and the end zones of the short penetrating arteries. Both types of lesions have an increase in pro-inflammatory cytokines mainly tumor necrosis factor-α, interleukin-1β, interleukin 6, interleukin-8 and interleukin-9 (Volpe, 2009).
Diagnosis and management of WMI: PVL can be diagnosed by US and MRI. US can easily diagnose focal cystic, occasionally diagnose non cystic lesions while maybe unable to detect diffuse lesions. High resolution MRI together with diffuse tensor imaging (DTI) can easily diagnose diffuse PVL. They can even diagnose the mildest form of WMI which is diffuse white matter gliosis caused by astrogliosis and microgliosis. No current therapy can reverse or ameliorate PVL. Only preventative measures are available as antenatal steroids, treating hypotension, hypocarbia and infections. Supportive therapy including early intervention, physical, occupational therapy and access to tertiary centers for the management of disabilities is of utmost importance. Life expectancy is variable ranging from only a few months to a full life expectancy. This is dependent on number of key disabilities and their severity, as well as mobility, feeding, respiratory and cognitive functioning.
Spread of WMI: WMI in infants with PVL can be wide spread to the periventricular, subcortical and callosal white matters, and internal capsule. Corpus callosum containing commissural myelinated fibers is impaired in PVL. Injury to the corticospinal tracts in PVL leads to motor deficits, including CP. Axonal injury is frequently seen as axons are susceptible to HI and due to failure of axonal ensheathment by the pre-OL. Injury to the grey matter areas like thalamus and basal ganglia can also be seen. Selective subplate neuronal injury/death, leads to abnormal cortical development and impaired plasticity. Late migrating GABAergic neurons undergo apoptosis in response to HI leading to a decrease in subcortical and upper cortical neurons (Volpe, 2009).
Microglial role: Microglia plays a key role during brain development, involving apoptosis, synaptic pruning, vascularization, axonal development, and myelination. In utero, microglial number peaks in the white matter in the third trimester. Microglia activation causes the release of pro-inflammatory cytokines and free radicals leading to pre-OLs loss and maturation arrest. Pre-OLs are vulnerable to free radical, whereas the mature OLs are more resistant. Free radicals are both a cause and a result of inflammation. Iron is a main source of free radicals. There is active acquisition of iron during OL differentiation. This mechanism explains why PVL is commonly seen with intraventricular hemorrhage (IVH) (Tahraoui et al., 2001).
Regeneration after WMI: It is believed that persistent inflammation and possibly epigenetic modifications including phosphorylation, ubiquitination and acetylation of histones and methylation of DNA and RNA can last for years after the initial injury. These modifications cause added injury, prevent regeneration and affect plasticity. On the other hand, neuronal replenishment in the cerebral white matter in PVL has been shown in animal models evidenced by increased migration of immature neurons from the sub-ventricular zone (SVZ) to distant sites of injury with neurogenesis persisting for months after the initial insult. In human autopsy brains, doublecortin (DCX); a marker of post mitotic migrating neurons; was significantly increased in PVL cases compared to controls. It is believed that neuronal progenitors in the human SVZ respond to injury by differentiation and migration outward but without proliferation (Haynes et al., 2011).
Modeling PVL: Currently, there is no available treatment for this devastating injury. All animal models must show a convincing relevance to human lesion. There are 3 main categories of animal models than can induce PVL: Antenatal or postnatal HI surgery, induction of systemic inflammatory response through administration of bacteria or LPS and lastly using N-methyl-D-aspartate (NMDA) and non-NMDA receptor agonists causing excitotoxicity (Choi et al., 2011).
HI model of PVL: Rice-Vannucci HI model (in which 7-day-old rat pups undergo unilateral ligation of the common carotid artery followed by exposure to 8% oxygen) is a model of HI which contributed significantly to studying brain injury in neonates. Many modifications to this model have been made to produce selective grey or white matter injury to HI model in the term and the preterm infant. Our HI injury mouse model (which involves temporary bilateral carotid artery ligation at postnatal day (P) 5 followed by 20 minutes of hypoxia 8%, (P5 corresponds to gestational age (GA) 24–30 for white matter maturation), that mimics human PVL in several important ways, including hind or lower limb paresis, incoordination and initial failure to thrive due to lack of adequate feeding. Our model also mimics human PVL histologically in the form of ventriculomegaly due to white matter loss from decreased OLs numbers as well as OLs maturational arrest. We showed; in our model; a significant astrogliosis and microgliosis in the periventricular white matter similar to human PVL pathological changes. At the molecular level, we showed in our model that activation of nuclear factor kappa B pathway; along with a significant increase of pro-inflammatory cytokines; leads to an increase in the number of activated microglia (M1 phenotype) and a reduction of repair microglia (M2 phenotype). Nitric oxide produced by activated microglia causes direct injury to the pre-OLs along with brain hypoperfusion (Zaghloul et al., 2017). Ability to use this HI mouse model in transgenic animals can lead to a deeper understanding of the pathophysiology of PVL and provide numerous preventive/therapeutic options which are enhanced by the long term survival of this model.
Conclusion: PVL is a complex combination of destructive and developmental disturbances (Figure 1). Pre-OL injury appears to be the first step in PVL. Currently, MRI/fMRI is successfully used to delineate the extent of the injury and predict the prognosis. Clinically relevant models will enable us to test and provide promising preventive/therapeutic strategies in rodents which eventually can be tested in our neonates with a goal to improve outcome and decrease or alleviate the morbidity of this devastating disease.
Figure 1.
Mechanism of injury and repair in periventricular leukomalacia.
pre-OL: Premyelinating oligodendrocyte.
This work was supported by Lilling Family Neonatal Research Lab, Feinstein Institute for Medical Research.
Footnotes
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
References
- 1.Choi EK, Park D, Kim TK, Lee SH, Bae DK, Yang G, Yang YH, Kyung J, Kim D, Lee WR, Suh JG, Jeong ES, Kim SU, Kim YB. Animal models of periventricular leukomalacia. Lab Anim Res. 2011;27:77–84. doi: 10.5625/lar.2011.27.2.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fern R. Ischemia: astrocytes show their sensitive side. Prog Brain Res. 2001;132:405–411. doi: 10.1016/S0079-6123(01)32091-5. [DOI] [PubMed] [Google Scholar]
- 3.Haynes RL, Xu G, Folkerth RD, Trachtenberg FL, Volpe JJ, Kinney HC. Potential neuronal repair in cerebral white matter injury in the human neonate. Pediatr Res. 2011;69:62–67. doi: 10.1203/PDR.0b013e3181ff3792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rumajogee P, Bregman T, Miller SP, Yager JY, Fehlings MG. Rodent hypoxia-ischemia models for cerebral palsy research: a systematic review. Front Neurol. 2016;7:57. doi: 10.3389/fneur.2016.00057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tahraoui SL, Marret S, Bodénant C, Leroux P, Dommergues MA, Evrard P, Gressens P. Central role of microglia in neonatal excitotoxic lesions of the murine periventricular white matter. Brain Pathol. 2001;11:56–71. doi: 10.1111/j.1750-3639.2001.tb00381.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Volpe JJ. Neurobiology of periventricular leukomalacia in the premature infant. Pediatr Res. 2001;50:553–562. doi: 10.1203/00006450-200111000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Volpe JJ. The encephalopathy of prematurity--brain injury and impaired brain development inextricably intertwined. Semin Pediatr Neurol. 2009;16:167–178. doi: 10.1016/j.spen.2009.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Volpe JJ. Confusions in nomenclature: “periventricular leukomalacia” and “white matter injury”-identical, distinct, or overlapping? Pediatr Neurol. 2017;73:3–6. doi: 10.1016/j.pediatrneurol.2017.05.013. [DOI] [PubMed] [Google Scholar]
- 9.Zaghloul N, Patel H, Ahmed MN. A model of Periventricular Leukomalacia (PVL) in neonate mice with histopathological and neurodevelopmental outcomes mimicking human PVL in neonates. PLoS One. 2017;12:e0175438. doi: 10.1371/journal.pone.0175438. [DOI] [PMC free article] [PubMed] [Google Scholar]