Abstract
Introduction
Missed opportunities and barriers to vaccination limit progress toward achieving high immunization coverage and other global immunization goals. Little is known about vaccination practices contributing to missed opportunities and barriers among private healthcare providers in Africa.
Methods
Service Provision Assessments (SPA) of representative samples of health facilities in four African countries (Kenya, Tanzania, Senegal, Malawi) in 2010-2015 were used to describe missed opportunities and barriers for vaccination in public, private for-profit, private not-for-profit and faith-based facilities. Data included vaccination practices, observations during sick child and antenatal visits, and exit interviews following sick child visits.
Results
Data from 3,219 health facilities, 11,613 sick child visits and 8,698 antenatal visits were included. A smaller proportion of for-profit facilities offered child vaccination services (country range, 25-37%) than did public facilities (range, 90-96%). The proportion of facilities offering pentavalent vaccine (diphtheria, pertussis, tetanus, hepatitis B and Haemophilus influenza type b antigens) daily ranged 0-77% across countries and facility types. Less than 33% of for-profit facilities in any country offered measles vaccination daily. A minority of public or private providers assessed the child’s vaccination status during a sick child visit (range by country and facility type, 14-44%), or offered tetanus toxoid during antenatal visits (range, 19-51%). Very few providers discussed the importance of newborn vaccination.
Conclusion
Substantial missed opportunities for, and barriers to, vaccination were identified across this representative sample of health facilities in four African countries. Strategies are needed to ensure that private and public providers implement practices to minimize barriers and missed opportunities for vaccination.
Keywords: Immunization, vaccination, Africa, Service Provision Assessment survey
Introduction
In many low and middle-income countries (LMICs), immunization services are provided solely through government-funded public providers, but recent evidence indicates the private health sector may also play an important role in immunization service provision [1]. The Global Vaccine Action Plan 2011-2020 (GVAP) proposes increased private sector involvement in community demand and related vaccination coverage improvement strategies to “ensure strong immunization systems are an integral part of a well-functioning health system” [2].
Little is known about the characteristics of private sector delivery of immunization services in LMICs, including how private and public sector practices differ along lines of service quality and adherence to national immunization policies [1]. The current limited evidence indicate private healthcare providers have lower levels of knowledge about immunization and service quality compared to public sector providers [1, 3, 4]; however only one published study from Africa is currently available [4].
The GVAP calls on all countries to reach ≥ 90% national coverage and ≥ 80% coverage in every district for all vaccines in the country’s national immunization schedule by 2020 [2]. Global coverage, as measured by the third dose of diphtheria-tetanus-pertussis vaccine (DTP3), has remained stagnant at 85% since 2010 [5]. Of particular concern is the World Health Organization (WHO) African Region, which had the lowest DTP3 coverage (76%) of all WHO regions in 2015.
Minimizing missed opportunities for vaccination (MOV) is one important strategy to reach and sustain ≥ 90% coverage. MOV occur when an individual presents for any health service and is not provided all vaccinations for which they are eligible. Every preventive and curative health service encounter is an opportunity to vaccinate an eligible individual. MOV are common; a 2014 review in LMICs concluded that MOV occurred in 32%–46% of public health service encounters [6]. Recent assessments in Africa reported high MOV prevalence, ranging from 43% to 57%, and documented multiple reasons for an MOV [7, 8], including healthcare providers not checking a child’s vaccination eligibility during a sick child visit, false contraindications for vaccination, and hesitancy to open multi-dose vaccine vials. Given this evidence, in 2016 the WHO Strategic Advisory Group of Experts on Immunization endorsed a global strategy to identify and reduce MOV prevalence worldwide [8, 9].
Strategies for reducing MOV include screening for vaccination status during visits to health facilities for mild illness, ensuring children receive all recommended vaccinations during a single visit, and using facility-based child vaccination registers to help track when individuals are due for vaccination [10]. Both private and public health sectors could play important roles in implementing MOV reduction strategies. Although MOV have been examined in the public sector, little is known about MOV in the private health sector.
Health sector surveys such as Service Provision Assessment (SPA) surveys provide an opportunity for insight into MOV across private and public sectors. SPA surveys are conducted every 3-7 years in LMICs to assess availability, delivery, and quality of services in a representative sample of health facilities. This paper assesses potential barriers and MOV in public and private (for-profit, not-for-profit and faith-based) health facilities in four African countries that conducted SPA surveys during 2010-2015: Kenya, Tanzania, Senegal and Malawi.
Methods
SPA surveys collect information on facility-based health services in developing countries using service readiness indicators developed by WHO and the United States Agency for International Development (USAID) [11, 12]. Ten health services and topics are assessed in SPA surveys. We used data from two components of SPA surveys: 1) facility inventory assessments (at all sampled health facilities), and 2) sick child and antenatal care visit observations and exit interviews (from among all sampled health facilities where visits were occurring on the day the inventory assessment occurred). We assessed potential barriers to services, including service availability, fees, and satisfaction with care. We also assessed MOV during sick child visits when recommended childhood vaccinations should be provided to eligible children, and during antenatal care visits when tetanus toxoid (TT) should be provided to eligible pregnant women.
SPA survey methodology
Typically, SPA surveys collect data from a nationally representative sample of 400-700 formal sector health facilities [12]. In Kenya, Tanzania, and Senegal, the sample of health facilities is designed to be representative at the national and regional levels by type of facility and by the different operating authorities. In Malawi, a census of all formal-sector health facilities was conducted.
Generally, SPA surveys include 10-15 survey teams, each comprised of 3-4 surveyors. During the facility visit, the facility manager, person in-charge of the facility, or the most senior health worker is interviewed using the facility inventory questionnaire to obtain information on availability of health services, resources for these services and procedures followed for providing these services.
Surveyors also observe client-provider consultations for a single day using standardized observation protocols for antenatal care, curative care for sick children, and other services [12, 13]. SPA surveys do not include observations or exit interviews following well child or immunization visits. Surveyors attempt to select two new antenatal clients for every follow-up client. Only children under five years of age who present with an illness (as opposed to an injury or an eye or skin infection only) are selected. Where many eligible clients are present, the surveyors select no more than five clients per provider and no more than 15 clients for a particular service in any health facility [14-16].
Service observations are coupled with exit interviews using standardized questionnaires to document the client’s experience with the services received. For sick child visits, the child’s caregiver (usually a parent) participates in the exit interview. The surveyor reads a list of common topics associated with client dissatisfaction, asking if each topic posed a major or minor problem, or no problem during the visit.
Definitions
Health facility type was defined by operating authority categories used in SPA surveys: 1) public; 2) private for-profit (for-profit), 3) private not-for-profit/non-governmental organization (not-for-profit); and 4) private mission/faith-based organization (faith-based). In Tanzania, parastatal facilities were categorized as private not-for-profit facilities per Tanzania Ministry of Health definitions [17].
Data inclusion criteria
SPA surveys conducted during 2010-2015 in African countries (Kenya, Tanzania, Senegal and Malawi) were included in the analyses, using facility-level (inventory) and individual-level (observation protocol and client exit interview) questionnaire data [14-16, 18]. All facilities interviewed in the SPA surveys were included in our facility-based analyses unless they offered only inpatient services or stand-alone voluntary counseling and testing or used different inventory questionnaires for a specific facility type, such as “health huts” in Senegal (community-based outreach site run by community health workers). Multiple client exit interviews and observation protocols were conducted at the surveyed facilities. All sick child exit interviews and observations and antenatal observations from the sampled facilities were included unless clients refused.
In the Kenya SPA (2010) survey, 703 facilities were randomly sampled from a master list of 6,192 facilities; due to non-response, 695 facilities were included in the final dataset [14]. For the Tanzania SPA (2014-15) survey, of 7,102 verified health facilities, 1,200 were sampled and 1,188 were included in the final dataset [16]. Senegal conducts a continuous SPA survey each year covering various health service areas. Facility-level data from the 2012-13 survey were analyzed; of 3,084 health facilities, 458 were sampled and 438 successfully interviewed [18]. Observations and exit interviews for sick child visits in Senegal were available from facilities surveyed in 2012-13; antenatal care observation data were available for 2014 from a different set of facilities. Analyses accounted for weights to account for the probability of selection of facilities within defined strata (region, facility type (e.g. clinic, hospital) and operating authority), and adjusted for non-response [12]. The Malawi SPA (2013-14) survey was designed as a census of all 1,060 formal-sector health facilities in the country; 977 were included in the final dataset. The Malawi data were weighted for non-response [15].
Data analysis
For Kenya, Tanzania, and Senegal, sample strata were created by crossing region and facility type. When a single unit stratum was present, adjacent strata from the same region were collapsed to calculate sampling errors. This was done separately for facility- and individual-level analyses since some facilities did not have any individual-level observations, resulting in a greater number of single unit strata than at the facility level. At the individual-level, facility was treated as the primary sampling unit. Since Malawi conducted a census of facilities, facility-level observations were not stratified. Individual-level observations were stratified by facility.
Each individual-level sick child observation and exit interview was merged with the inventory questionnaire data for the facility at which that observation was conducted. For questions regarding TT receipt or counseling about newborn vaccination, each antenatal care observation was merged with the inventory questionnaire data for the facility at which that observation was conducted.
For availability of vaccination services, supply of immunization cards, and service fees, data from the facility inventory questionnaire were used. Pentavalent vaccine (combination vaccine with diphtheria, pertussis, tetanus, hepatitis B and Haemophilus influenza type b antigens) was used as a proxy for general vaccination service delivery. Daily vaccination was defined as provision of vaccination at least 20 days per month. For assessment of caregiver perception of service quality and satisfaction, data from the sick child exit interviews were used. For measured wait times, data from sick child visit observations were used. Percentages were not calculated for facility types within a country if there were ≤ 5 facilities or interviews within that facility type.
To assess MOV among children, we used data from observed sick child visits to assess if the provider reviewed child’s health card, and assessed immunization status (i.e., if provider looked at the child’s health card either before beginning the consultation, or while collecting information from the caretaker, or while examining the child). We used data from the provider’s response when asked “Did you vaccinate the child during this visit or refer the child for vaccination today other than vitamin A supplementation? If no: Why not?”, to assess if the provider reported vaccinating or referring the child for vaccination or the reason for not doing so. To assess MOV among pregnant women we used data from observed antenatal visits to assess if the provider administered or prescribed TT vaccination and provided counseling about the importance of newborn vaccination.
We used the survey command in STATA 12, with the provided survey weights from the SPA survey dataset for our analyses, accounting for stratification and clustering as described above. We calculated weighted proportions for each indicator of interest across all facilities in each country and by facility type. We conducted chi-square tests to assess whether the frequency of an indicator significantly differed across the four facility types, and t-tests for pairwise analyses comparing public facilities with each of the other three facility types when the chi-square test indicated overall significance. We used a p-value threshold of ≤ 0.05 to assess statistical significance. For Malawi facility-level indicators only, no statistical tests of significance were conducted since the total number of facilities per strata were not available to calculate a finite population correction to ensure a proper estimate of variance for each indicator.
Results
The study included data from 3,219 surveyed facilities in the four countries (Table 1). In Kenya, 5 facilities were excluded because they offered only inpatient services or stand-alone voluntary counseling and testing. In Senegal, 74 “health hut” facility types were excluded because different inventory questionnaires were used for those facilities. With the exception of Tanzania, the majority of the private facilities were for-profit facilities.
Table 1.
Characteristics of health facilities with Service Provision Assessment (SPA) surveys, by facility type, in Kenya 2010), Tanzania (2014-2015), Senegal (2012-2013, 2014), and Malawi (2013-2014)
| Country | Facility indicator | Public N (%) |
Private for-profit N (%) |
Private not-for-profit/NGO N (%) |
Mission/faith based N (%) |
Total N (%) |
|---|---|---|---|---|---|---|
| Kenya | Total facilities surveyed | 345 (50) | 215 (34) | 38 (3) | 92 (13) | 690 |
| Facilities providing sick child care | 334 (98) | 196 (94) | 21 (87) | 87 (98) | 638 (96) | |
| Facilities providing antenatal care | 320 (88) | 140 (46) | 17 (77) | 81 (88) | 560 (81) | |
| Sick child visit observations | 1452 | 260 | 57 | 247 | 2016 (5205) | |
| Antenatal visit observations | 1030 | 151 | 25 | 206 | 1412 (3965) | |
| Tanzania2 | Total facilities surveyed | 780 (72) | 184 (14) | 20 (2) | 204 (12) | 1188 |
| Facilities providing sick child care | 776 (100) | 161 (91) | 18 (71) | 199 (97) | 1154 (98) | |
| Facilities providing antenatal care | 754 (96) | 80 (36) | 12 (17) | 185 (81) | 1031 (85) | |
| Sick child visit observations | 3723 | 364 | 50 | 824 | 4961 (10155) | |
| Antenatal visit observations | 2906 | 249 | 34 | 818 | 4007 (8155) | |
| Senegal | Total facilities surveyed3 | 305 (83) | 43 (12) | 1 (0) | 15 (5) | 364 |
| Facilities providing sick child care3 | 298 (98) | 28 (64) | 1 (100) | 15 (100) | 342 (94) | |
| Facilities providing antenatal care4 | 290 (99) | 29 (73) | 11 (87) | 19 (100) | 349 (96) | |
| Sick child visit observations3 | 1118 | 102 | 4 | 83 | 1307 (3285) | |
| Antenatal visit observations4 | 1096 | 44 | 35 | 36 | 1211 (3005) | |
| Malawi | Total facilities surveyed | 478 (48) | 275 (29) | 57 (6) | 167 (17) | 977 |
| Facilities providing sick child care | 457 (95) | 249 (90) | 49 (86) | 165 (99) | 920 (94) | |
| Facilities providing antenatal care | 408 (85) | 72 (26) | 10 (17) | 153 (91) | 643 (65) | |
| Sick child visit observations | 2173 | 461 | 94 | 601 | 3329 (7485) | |
| Antenatal visit observations | 1487 | 72 | 18 | 491 | 2068 (4125) | |
| Overall | Total facilities surveyed | 1908 | 717 | 116 | 478 | 3219 |
| Total sick child visit observations | 8466 | 1187 | 205 | 1755 | 11613 | |
| Total antenatal care observations | 6519 | 516 | 112 | 1551 | 8698 |
Senegal SPA survey collects subset of data annually instead of all data in one year; sick child data available for 2012-2013; antenatal care data available for 2014.
Tanzania categorized operating authority as public, private for-profit, parastatal, or mission/faith-based. Parastatal facility data shown in private not-for-profit column.
Refers to facilities/observations included in the 2012-2013 SPA survey.
Refers to facilities/observations included in the 2014 SPA survey.
Number of facilities within country where these observations occurred.
Most facilities in the four countries provided sick child and antenatal care; a lower proportion of for-profit and not-for-profit facilities than public facilities provided antenatal care (Table 1). We included data from 11,613 sick child visit observations and interviews, and 8,698 antenatal visit observations. There were 31 refusals for sick child interviews in Kenya, 1 in Tanzania, none in Senegal and 112 in Malawi. For antenatal interviews, there were 33 refusals in Kenya, 3 in Tanzania, none in Senegal and 37 in Malawi. Most but not all of the facilities that provided sick child or antenatal care contributed sick child or antenatal observations (Table 1).
Potential barriers to immunization services
Availability of immunization services and immunization cards
In all countries, higher proportions of public (country range, 91%-96%) facilities offered childhood immunization services than did for-profit (country range, 25%-37%) facilities (Table 2). In Tanzania, a higher proportion of public facilities offered childhood immunization services than did all three other facility types. The proportion of facilities offering pentavalent vaccine daily ( ≥ 20 days/month) varied from none to 77% across countries and facility types (Table 2). In Kenya, a higher proportion of public facilities offered pentavalent vaccine daily, compared to other facility types.
Table 2.
Characteristics of immunization services at facilities, by facility type - Service Provision Assessment (SPA) surveys in Kenya (2010), Tanzania (2014-2015), Senegal (2012-2013), and Malawi (2013-2014)
| Public % | Private for-profit % (p value)1 | Private not-for-profit/NGO % (p value)1 | Mission/Faith-based % (p value)1 | p value2 | |
|---|---|---|---|---|---|
| Facility characteristic | Kenya (N=690) | ||||
| Offers immunization service | 91 | 37 (<0.01) | 75 (0.08) | 80 (0.18) | <0.01 |
| Offers daily (≥20 days/month) pentavalent vaccination | 64 | 37 (<0.01) | 37 (0.03) | 47 (0.02) | <0.01 |
| Offers daily measles vaccination | 51 | 23 (<0.01) | 35 (0.16) | 29 (<0.01) | <0.01 |
| Health cards available3 | 92 | 87 | 87 | 89 | 0.74 |
| Client fee for immunization service | 20 | 75 (<0.01) | 43 (0.18) | 81 (<0.01) | <0.01 |
| Tanzania4(N=1188) | |||||
| Offers immunization service | 95 | 27 (<0.01) | 16 (<0.01) | 79 (<0.01) | <0.01 |
| Offers daily (≥20 days/month) pentavalent vaccination | 69 | 63 | 69 | 77 | 0.41 |
| Offers daily measles vaccination | 24 | 11 | 20 | 28 | 0.42 |
| Health cards available3 | 87 | 91 | 87 | 76 | 0.07 |
| Client fee for immunization service | 1 | 1 | 0 | 3 | 0.48 |
| Senegal5(N=364) | |||||
| Offers immunization service | 93 | 30 (<0.01) | - | 79 (0.22) | <0.01 |
| Offers daily (≥20 days/month) pentavalent vaccination | 40 | 44 (0.78) | - | 0 (<0.01) | 0.02 |
| Offers daily measles vaccination | 5 | 33 (0.22) | - | 0 (<0.01) | <0.01 |
| Health cards available3 | 89 | 86 | - | 87 | 0.93 |
| Client fee for immunization service | 36 | 34 | - | 12 | 0.27 |
| Malawi6(N=977) | |||||
| Offers immunization service | 96 | 25 | 33 | 95 | - |
| Offers daily (≥20 days/month) pentavalent vaccination | 43 | 13 | 26 | 46 | - |
| Offers daily measles vaccination | 40 | 8 | 21 | 41 | - |
| Health cards available3 | 57 | 46 | 42 | 58 | - |
| Client fee for immunization service | 0 | 7 | 5 | 3 | - |
p value (t-test) for pairwise difference in proportion compared to public facilities; test done only among those indicators where the overall chi-square test result indicated a significant difference between any facility types.
Chi square p-values for differences across all facility types.
Of facilities offering immunization services.
Tanzania categorized operating authority as public, private-for-profit, parastatal, or mission/faith-based. Parastatal facility data shown in private not-for-profit column.
Percentages not calculated for private not-for-profit category because only 1 private not-for-profit facility surveyed in Senegal.
No facility level statistical tests done for Malawi due to census design.
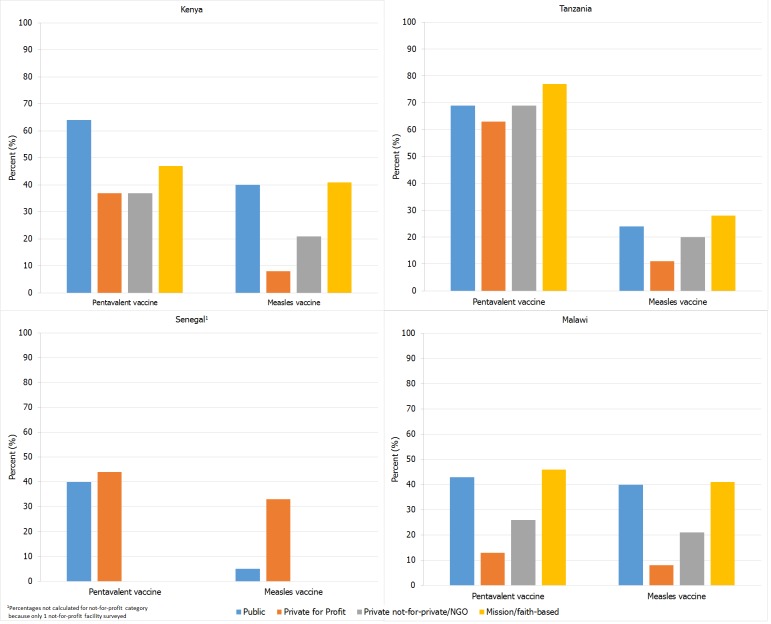
Among for-profit facilities, 8%-33% (country range) offered measles vaccine daily compared to 13%-63% that offered pentavalent vaccine daily (Table 2, Figure 1). A majority of each facility type in each country had a supply of blank immunization cards except for those in Malawi where only about half of all facilities (facility type range, 42%-58%) had blank immunization cards available (Table 2).
Figure 1.
Proportion of facilities offering pentavalent and measles vaccines on a daily (≥20 days/month) basis, by facility type – Service Provision Assessment surveys in Kenya (2010), Tanzania (2014-2015), Senegal (2012-2013), and Malawi (2013-2014)
Fees for immunization services
The proportion of facilities that reported charging fees for immunization visits varied among countries. In Tanzania and Malawi, few facilities of any operating authority type (facility type range, 0%-3% for Tanzania, 0%-7% for Malawi) charged fees for immunization visits (Table 2). In Kenya, a higher proportion of for-profit (75%) and faith-based private facilities (81%) reported that they charged fees for immunization visits than did public facilities. However, a substantial proportion of public facilities in both Kenya (20%) and Senegal (36%) charged fees for immunization visits. In Kenya, additional questions were asked about why fees were charged: of the public facilities in Kenya that charged fees for immunization services, 66% charged for the immunization card, 26% for vaccine administration and 13% for vaccine.
Missed opportunities for vaccination
During sick child visits
The proportion of providers who were observed reviewing the child health card for any reason during a sick child visit varied widely by country and facility type (Table 3). A lower proportion of providers in for-profit facilities in Tanzania (21%) and Malawi (67%) than in public facilities in Tanzania (42%) and Malawi (76%) reviewed the child health card. In Malawi a higher proportion of providers in not-for-profit (82%) and faith-based facilities (84%) than in public facilities (76%) reviewed the card. Specific assessment of the child’s immunization status was less commonly observed; a minority of providers in all countries and all facility types did so (Table 3). In Malawi, a lower proportion of public providers assessed vaccination status compared to for-profit, not-for-profit and faith-based providers.
Table 3.
Service characteristics observed during sick child visit or antenatal visit, by facility type - Service Provision Assessment (SPA) surveys in Kenya (2010),Tanzania (2014-2015), Senegal1 (2012-2013, 2014), and Malawi (2013-2014)
| Public % (p value)2 | Private for- profit % (p value)2 | Private not-for-profit/NGO % (p value)2 | Mission/Faith-based % (p value)2 | p value3 | |
|---|---|---|---|---|---|
| Kenya | |||||
| Sick child visit (N=2016) | |||||
| Provider reviewed child health card6 | 80 | 66 | 81 | 69 | 0.29 |
| Provider assessed immunization status6 | 44 | 32 | 34 | 34 | 0.37 |
| Vaccination administered7 | 7 | 3 (0.03) | 39 (0.06) | 7 (0.88) | <0.01 |
| Child referred for vaccination7 | 4 | 2 | 2 | 2 | 0.51 |
| Child “not due”/Fully immunized7 | 68 | 69 | 44 | 58 | 0.24 |
| Not immunization day7 | 2 | 3 | 2 | 4 | 0.60 |
| No immunization check7 | 17 | 19 | 11 | 26 | 0.40 |
| Antenatal visit (N=1412) | |||||
| TT administered/prescribed6 | 51 | 42 | 45 | 48 | 0.55 |
| Newborn vaccination discussed6 | 13 | 3 | 15 | 23 | 0.11 |
| Tanzania 4 | |||||
| Sick child visit (N=4961) | |||||
| Provider reviewed child health card6 | 42 | 21 (<0.01) | 21 (0.19) | 38 (0.39) | <0.01 |
| Provider assessed immunization status6 | 25 | 18 | 15 | 23 | 0.36 |
| Vaccination administered7 | 3 | 0 | 2 | 2 | 0.20 |
| Child referred for vaccination7 | 0 | 1 | 0 | 0 | 0.90 |
| Child “not due”/Fully immunized7 | 61 | 65 | 58 | 59 | 0.69 |
| Not immunization day7 | 21 | 11 | 23 | 22 | 0.07 |
| No immunization check7 | 13 | 9 | 16 | 16 | 0.35 |
| Antenatal visit (N=4007) | |||||
| TT administered/prescribed6 | 36 | 38 | 19 | 35 | 0.75 |
| Newborn vaccination discussed6 | 3 | 2 | 0 | 3 | 0.95 |
| Senegal | |||||
| Sick child visit5 (N=1307) | |||||
| Provider reviewed child health card6 | 14 | 33 (0.08) | - | 41 (<0.01) | <0.01 |
| Provider assessed immunization status6 | 27 | 18 | - | 17 | 0.16 |
| Vaccination administered7 | 4 | 6 | - | 1 | 0.47 |
| Child referred for vaccination7 | 1 | 0 | - | 0 | 0.63 |
| Child “not due”/Fully immunized7 | 27 | 14 (<0.01) | - | 7 (<0.01) | <0.01 |
| Not immunization day7 | 18 | 19 | - | 22 | 0.70 |
| No immunization check7 | 49 | 60 | - | 70 | 0.06 |
| Antenatal visit (N=1211) | |||||
| TT administered/prescribed6 | 33 | 47 | 24 | 37 | 0.27 |
| Newborn vaccination discussed6 | 0 | 0 | 0 | 3 | 0.48 |
| Malawi | |||||
| Sick child visit (N=3329) | |||||
| Provider reviewed child health card6 | 76 | 67 (<0.01) | 82 (<0.01) | 84 (<0.01) | <0.01 |
| Provider assessed immunization status6 | 14 | 22 (<0.01) | 30 (<0.01) | 23 (<0.01) | <0.01 |
| Vaccination administered7 | 2 | 1 (<0.01) | 7 (0.10) | 2 (0.89) | <0.01 |
| Child referred for vaccination7 | 2 | 1 | 2 | 1 | 0.66 |
| Child “not due”/Fully immunized7 | 61 | 57 (0.02) | 49 (0.02) | 62 (0.64) | 0.02 |
| Not immunization day7 | 6 | 5 (0.05) | 16 (<0.01) | 10 (<0.01) | <0.01 |
| No immunization check7 | 28 | 35 (<0.01) | 17 (<0.01) | 25 (0.04) | <0.01 |
| Antenatal visit (N=2068) | |||||
| TT administered/prescribed6 | 26 | 24 (0.66) | 50 (0.03) | 38 (<0.01) | <0.01 |
| Newborn vaccination discussed6 | 2 | 2 (0.96) | 26 (<0.01) | 3 (0.04) | <0.01 |
Senegal SPA collects subset of data annually; sick child data available for 2012-2013; antenatal care data available for 2014.
p value (t-test) for pairwise difference in proportion compared to public facilities; test done only among those indicators where the overall chi-square test result indicated a significant difference between any facility types.
Chi square p-value for differences across facility types.
Tanzania categorized operating authority as public, private for profit, parastatal, or mission/faith-based. Parastatal facility data shown in private not-for-profit column.
Percentages not calculated because <5 (n=4) sick child interviews in private not-for-profit facilities in Senegal.
Observed by surveyor
Reported by provider
During sick child visits, few providers reported administering vaccinations or referring the child for vaccination (Table 3). Rather, providers indicated that the child was not due for vaccination, that they had not checked the child’s vaccination status, or that the sick child visit occurred on a non-immunization day.
During antenatal care visits
In each country, ≤ 51% of providers in any facility type administered or prescribed TT to pregnant women (Table 3). Overall, very few providers, in public or private facilities, discussed the importance of newborn vaccination with the pregnant woman (country range, 0-15%).
Health facility services and caregiver satisfaction
Wait times
Compared to other facility types, observed mean and median wait times for sick child visits were the shortest in for-profit facilities in each country except Senegal. For example, median wait times were 15, 30 and 10 minutes in for-profit facilities, compared to 30, 60, and 80 minutes in public facilities in Kenya, Tanzania and Malawi respectively (data not shown). In Kenya and Malawi, approximately 25% of caregivers visiting public facilities reported that wait times were a major problem, the highest proportion among the facility types (Table 4).
Table 4.
Caregivers’ satisfaction with sick child services, by facility type - Service Provision Assessment (SPA) surveys in Kenya (2010), Tanzania (2014-2015), Senegal (2012-2013), and Malawi (2013-2014)
| Caregiver responses | Public % (p value)2 | Private for profit % (p value)2 | Private not-for-profit/NGO1 % (p value)2 | Mission/Faith-based % (p value)2 | p value3 |
|---|---|---|---|---|---|
| Kenya (N=2016) | |||||
| Reported major problems | |||||
| Wait time | 28 | 12 (<0.01) | 10 (<0.01) | 13 (<0.01) | <0.01 |
| Availability of medicine | 21 | 2 (<0.01) | 32 (0.48) | 1 (<0.01) | <0.01 |
| Hours of service | 9 | 8 | 10 | 2 | 0.29 |
| Days of service | 6 | 2 | 11 | 2 | 0.10 |
| Facility cleanliness | 2 | 1 | 1 | 1 | 0.14 |
| Provider attitude | 2 | 0 | 1 | 0 | 0.35 |
| Very satisfied with services | 74 | 76 | 82 | 76 | 0.79 |
| Not satisfied with services | 3 | 0 (<0.01) | 3 (0.26) | 0 (<0.01) | <0.01 |
| Facility visited not closest to home | 14 | 34 (<0.01) | 7 (0.09) | 37 (<0.01) | <0.01 |
| Tanzania (N=4961) | |||||
| Reported major problems | |||||
| Wait time | 16 | 11 | 19 | 17 | 0.53 |
| Availability of medicine | 20 | 5 (<0.01) | 16 (0.66) | 7 (<0.01) | <0.01 |
| Hours of service | 6 | 3 | 2 | 2 | 0.09 |
| Days of service | 3 | 1 | 1 | 1 | 0.06 |
| Facility cleanliness | 5 | 2 (0.02) | 1 (<0.01) | 1 (<0.01) | <0.01 |
| Provider attitude | 2 | 1 | 1 | 2 | 0.77 |
| Very satisfied with services | 74 | 74 | 82 | 75 | 0.85 |
| Not satisfied with services | 6 | 3 | 0 | 4 | 0.41 |
| Facility visited not closest to home | 11 | 39 (<0.01) | 29 (0.09) | 31 (<0.01) | <0.01 |
| Senegal 4(N=1307) | |||||
| Reported major problems | |||||
| Wait time | 15 | 33 | - | 20 | 0.16 |
| Availability of medicine | 10 | 10 | - | 3 | 0.23 |
| Hours of service | 6 | 11 | - | 9 | 0.62 |
| Days of service | 3 | 0 (<0.01) | - | 11 (0.08) | <0.01 |
| Facility cleanliness | 3 | 0 | - | 0 | 0.61 |
| Provider attitude | 1 | 6 | - | 2 | 0.18 |
| Very satisfied with services | 82 | 89 | - | 74 | 0.08 |
| Not satisfied with services | 0 | 0 | - | 0 | 0.90 |
| Facility visited not closest to home | 18 | 65 (<0.01) | - | 54 (<0.01) | <0.01 |
| Malawi (N=3329) | |||||
| Reported major problems | |||||
| Wait time | 25 | 8 (<0.01) | 10 (<0.01) | 15 (<0.01) | <0.01 |
| Availability of medicine | 16 | 5 (<0.01) | 2 (<0.01) | 4 (<0.01) | <0.01 |
| Hours of service | 14 | 2 (<0.01) | 2 (<0.01) | 6 (<0.01) | <0.01 |
| Days of service | 8 | 2 (<0.01) | 7 (0.47) | 3 (<0.01) | <0.01 |
| Facility cleanliness | 5 | 1 (<0.01) | 2 (0.05) | 1 (<0.01) | <0.01 |
| Provider attitude | 5 | 1 (<0.01) | 2 (0.07) | 2 (<0.01) | <0.01 |
| Very satisfied with services | 81 | 81 | 83 | 82 | 0.90 |
| Not satisfied with services | 6 | 3 (<0.01) | 1 (<0.01) | 3 (<0.01) | <0.01 |
| Facility visited not closest to home | 10 | 36 (<0.01) | 28 (<0.01) | 24 (<0.01) | <0.01 |
Tanzania categorized managing authority as public, private for profit, parastatal, or mission/faith-based. Parastatal facility data shown in private not-for-profit column.
p value (t-test) for pairwise difference in proportion compared to public facilities; test done only among those indicators where the overall chi-square test result indicated a significant difference between any facility types.
Chi square p-value for differences across operating authority types
Percentages not calculated because <5 (n=4) sick child interviews in private not-for-profit facilities in Senegal.
Other services
In Kenya, Tanzania and Malawi, a higher proportion of caregivers at public facilities reported major problems with availability of medicine compared to caregivers at for-profit or faith-based facilities (Table 4). Only a small proportion of caregivers (<5%) in any country reported major problems with facility cleanliness or provider attitude, regardless of facility type (Table 4). However, in Tanzania and Malawi, caregivers at public facilities more often reported problems with facility cleanliness compared to caregivers at other facility types; caregivers at Malawi public facilities reported problems with provider attitude more than in other facility types. The proportion of caregivers reporting a major problem with hours or days of service delivery was low (<14%) in all facility types in all four countries; in Malawi problems with hours or days of service reported by caregivers were higher in public facilities than in for-profit or faith-based facilities.
Caregiver satisfaction
The majority (facility type range, 74%-83%) of clients in each country reported being very satisfied with services, regardless of facility type. The proportion of caregivers not satisfied with services was low (<6% in all countries and facility types), but in Kenya and Malawi it was higher in public facilities than in for-profit or faith-based facilities. A notable proportion of caregivers sought sick child services at a facility other than the one closest to their home. Of those, more sought care at for-profit facilities (country range, 34-65%) or faith-based facilities (country range, 24%-54%), compared to public facilities. The most common reasons for not visiting the facility closest to their residence included the closer facility being too expensive (country range 5%-20%), having a bad reputation (country range, 4-19%), or having no medication (country range, 3%-21%), or the caregiver received a referral to the farther clinic (country range, 5%-21%).
Discussion
This study was the first to use SPA surveys to compare factors related to vaccination barriers and MOV across public and private health facilities. Data were drawn from nationally representative surveys, whose large sample sizes improve generalizability of results. The high facility response rates (99%) and the use of standardized questionnaires across countries enabled transnational comparisons. We observed differences in barriers to vaccination by facility type, including less availability of child immunization services in for-profit compared to public facilities in all countries, a higher proportion of for-profit facilities charging fees than public facilities in Kenya, and higher proportions of caregivers reporting problems with wait times and unsatisfactory care in public facilities than in for-profit facilities in Kenya and Malawi. We identified common missed opportunities across facility types, including infrequent vaccination screening and vaccine administration during sick child visits, and infrequent TT administration and counseling about newborn vaccination during antenatal care visits. This study helps to fill a knowledge gap about vaccination practices in the private sector and identifies potential opportunities to increase access to and utilization of immunization services across all facility types.
Fees for immunizations, whether official or informal, create an important barrier to vaccinations [19], and their existence is particularly concerning in public facilities. Although user fees were uncommon in Tanzania and Malawi, a substantial proportion of public facilities charged fees in Kenya and Senegal. Understanding how and why public facilities charge user fees for immunization services is an important future step for addressing how to remove this barrier to vaccination. Of the four countries in this study, only the Kenya data included information on specific fees charged for immunization services. More information from additional countries is needed.
Wait times were reported as a major problem across all types of facilities in all four countries. Long wait times are often cited as a barrier to health care seeking [19, 20]. Private facilities were found to have shorter wait times, but also were more likely to charge fees and many offered immunization services at limited times or not at all.
Despite problems that caregivers reported with services they received, the majority, across all facility types, reported satisfaction with services, similar to findings from other studies that reported relatively high levels of client satisfaction with the quality of primary health care services received [21, 22]. Clients are more likely to adhere to recommended care if they are satisfied with the quality of services [23]. Thus concerted efforts are needed to ensure that immunization services are of high quality and acceptable to clients. Monitoring for key barriers such as user fees and long wait times would enable these issues to be addressed in a timely manner to maintain client satisfaction.
A significant proportion of providers across countries and facility types did not screen sick children for eligible vaccinations, and vaccination was uncommon during sick child visits. Immunization histories of the sick children and their illness severity are unknown, so it is not possible to ascertain the proportion of children eligible for vaccination who were not screened. A recent study in Dominican Republic [24] found that 53% of children visiting health facilities for illness and eligible for vaccination had MOV, compared to 40% of children visiting for vaccination. A review of 57 studies of MOV [6] found a pooled MOV prevalence among children of 32.2%; the most common reasons for MOV related to health care provider practices, of which not reviewing immunization cards or vaccination history were the most common.
Additionally, we identified a potential MOV specific to measles vaccination; the majority of surveyed facilities, particularly for-profit facilities, reported providing measles vaccination less frequently than pentavalent vaccination. This practice may stem from the requirement that a measles vaccine vial be discarded within six hours of being opened, unlike pentavalent vaccine which can be stored for later use. Providers may be reluctant to open a multi-dose measles vaccine vial when only a few children present for vaccination; instead the child is told to return on a special measles vaccination day [25, 26]. Turning away a child creates an MOV, with uncertainty that the child will return, particularly if the caregiver has to travel far to the facility. Availability of measles vaccines containing fewer doses, for example five-dose vials, may contribute to reducing MOVs caused by reluctance to open a ten-dose measles vaccine vial for a few children.
Pregnant women receiving antenatal care often did not receive TT. Thus, most providers missed an important opportunity to protect neonates from tetanus at birth. TT vaccination contributes significantly to the elimination of neonatal tetanus. Across all facility types, there is a need to educate or re-orient providers on the importance of TT for pregnant women. Antenatal visits also provide an opportunity to increase awareness about newborn immunization, yet our results indicate such education rarely occurred. It is important for policy makers and service providers to make use of the opportunity that antenatal visits offer to improve maternal and child health. Further, an additional MOV for TT vaccination for women exists when women bringing their infants for routine immunization or sick child visits are not screened and vaccinated as indicated.
Limitations
Some facilities did not provide sick child or antenatal care on the day of the surveys, so observations and exit interviews were not conducted there. The characteristics of these facilities are unknown. However, of facilities that provided sick child or antenatal care, the majority contributed sick child observations (85%) or antenatal care observations (74%), likely minimizing potential bias. Variations in country context relative to health systems (including private provider practices) and health care seeking behavior may complicate country comparisons and limit generalizability to other LMICs.
We used exit interviews following sick child visits to assess caregiver perceptions of care. Assessments following immunization visits may have yielded more specific information about provider immunization practices, but were not available in SPA surveys. The method of conducting exit interviews at the health facility may predispose clients to give socially desirable answers, resulting in higher reported satisfaction, but the addition of structured observation may mitigate some of this potential bias. Our analysis focused on generating hypotheses for future studies and was not intended to assess causal associations. To do so would require study designs incorporating collection and analysis of applicable covariate data alongside exposure and outcome data. Not all countries participate in SPA surveys and they are infrequent, limiting broader analysis of SPA survey data.
Conclusion
Despite substantial progress in increasing the number of children vaccinated worldwide, over a third of all countries have not yet met the Global Vaccine Action Plan 2011–2020 target of 90% national DTP3 coverage [5]. We found potential barriers and missed opportunities for vaccination in public and private (for-profit, not-for-profit, and faith-based) health facilities in four sub-Saharan African countries. Several barriers and missed opportunities for vaccination were more prevalent in private facilities than in other facility types. Potential interventions include those that address needs for training and guidance; structural and systems changes such as policies for vaccination screening and removal of fees; and specific interventions to engage the private sector in delivery of high quality vaccination services. Reducing measles vaccine vial size may contribute significantly to reducing measles MOVs given the concerns of vaccine wastage which, in most cases, lead to health facilities having special days for measles vaccinations. In some countries, working through professional societies may provide opportunities to incorporate immunization training into professional development standards and to communicate vaccination policies. Minimizing missed opportunities and barriers to vaccination in both public and private health sectors can help to improve immunization coverage to meet development goals.
What is known about this topic
The African region has the lowest immunization coverage of all WHO regions (76% DPT3 coverage in 2015);
Reducing missed opportunities for and barriers to vaccination can improve immunization coverage and reduce immunity gaps;
There is limited information about immunization practices in private health facilities; very few studies have compared immunization practices in public and private facilities in low and middle income countries.
What this study adds
Service provider assessments provide useful large-scale and representative information about immunization in both public and private health facilities, and enabled identification of substantial missed opportunities and barriers to vaccination in four African countries;
A smaller proportion of for-profit health facilities than public facilities in four African countries offer childhood immunization services. Less than a third of for-profit facilities offered measles vaccination daily;
A minority of public and private providers in four African countries assessed immunization status of children during sick child visits, offered tetanus toxoid vaccine to pregnant women, or discussed the importance of newborn vaccination during antenatal visits.
Competing interests
The authors declare no competing interest.
Acknowledgments
The authors acknowledge and appreciate the feedback of CDC staff members who reviewed and provided comments on this manuscript, including Kathleen Wannemuehler, Laura Conklin, Abigail Shefer, and Kimberley Fox. The authors also appreciate the SPA survey teams who collected the data in Kenya, Tanzania, Senegal and Malawi. Funding: This work was supported by funds from the Centers for Disease Control and Prevention.
Authors’ contributions
Olorunsaiye C: concept development, data analysis, interpretation of results, manuscript writing. Langhamer M: data analysis, interpretation of results, manuscript writing. Wallace A: concept development, interpretation of results, manuscript writing. Watkins M: concept development, interpretation of results, manuscript writing. All authors have read and agreed to the final version of the manuscript.
Disclaimer
The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Levin A, Kaddar M. Role of the private sector in the provision of immunization services in low-and middle-income countries. Health Policy Plan. 2011 Jul;26(Suppl 1):i4–12. doi: 10.1093/heapol/czr037. [DOI] [PubMed] [Google Scholar]
- 2.Global vaccine action plan 2011-2020 . World Health Organization. 2013. [Google Scholar]
- 3.Wagner Z, Szilagyi PG, Sood N. Comparative performance of public and private sector delivery of BCG vaccination: Evidence from Sub-Saharan Africa. Vaccine. 2014 Jul 31;32(35):4522–8. doi: 10.1016/j.vaccine.2014.06.020. [DOI] [PubMed] [Google Scholar]
- 4.Oluoha C, Umeh C, Ahaneku H. Assessing the contributions of private health facilities in a pioneer private-public partnership in childhood immunization in Nigeria. Journal of Public Health in Africa. 2014:5. doi: 10.4081/jphia.2014.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Casey RM. Global Routine Vaccination Coverage, 201 MMWR Morbidity and Mortality Weekly Report. 2016. p. 6. [DOI] [PubMed] [Google Scholar]
- 6.Sridhar S, Maleq N, Guillermet E, Colombini A, Gessner BD. A systematic literature review of missed opportunities for immunization in low-and middle-income countries. Vaccine. 2014;32:6870–9. doi: 10.1016/j.vaccine.2014.10.063. [DOI] [PubMed] [Google Scholar]
- 7.Restrepo-Méndez MC, Barros AJ, Wong KL, et al. Missed opportunities in full immunization coverage: findings from low-and lower-middle-income countries. Global health action. 2016:9. doi: 10.3402/gha.v9.30963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organisation Meeting of the Strategic Advisory Group of Experts on immunization, April 2016– conclusions and recommendations. Wkly Epidemiol Rec. 2016 May 27;91(21):266–84. [PubMed] [Google Scholar]
- 9.Planning Guide to Reduce Missed Opportunities for Vaccination (MOV) Accessed 20 Feb 2017.
- 10.Velandia-González M, Trumbo SP, Díaz-Ortega JL, et al. Lessons learned from the development of a new methodology to assess missed opportunities for vaccination in Latin America and the Caribbean. BMC international health and human rights. 2015;15:1. doi: 10.1186/s12914-015-0043-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Service availability and readiness assessment (SARA) an annual monitoring system for service delivery: reference manual. [Google Scholar]
- 12.Service Provision Assessment survey Overview Accessed 20 Feb 2017.
- 13.Pregnancy, childbirth, postpartum, and newborn care . a guide for essential practice. World Health Organization. 2003. [PubMed] [Google Scholar]
- 14.Kenya service provision assessment survey 2010 . Nairobi: National Coordinating Agency for Population and Development, Ministry of Medical Services, Ministry of Public Health and Sanitation, Kenya National Bureau of Statistics, and ICF Macro. ICF International; 2011. [Google Scholar]
- 15.Malawi Service Provision Assessement Survey 2013-2014 Accessed 20 Feb 2017.
- 16.Tanzania Service Provision Assessment Survey (TSPA) 2014-15 Accessed 20 Feb 2017.
- 17.Tanzania Private Health Sector Assessment . USAID, ed: International Finance Corporation - World Bank. 2013. [Google Scholar]
- 18.Sénégal - Enquête Continue sur la Prestation des Services de Soins de Santé (ECPSS) 2014 Accessed 20 Feb 2017.
- 19.Favin M, Steinglass R, Fields R, Banerjee K, Sawhney M. Why children are not vaccinated: a review of the grey literature. International Health. 2012;4:229–38. doi: 10.1016/j.inhe.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 20.Assefa F, Mosse A. Assessment of Clients’ satisfaction with health service deliveries at jimma university specialized hospital. Ethiopian Journal of Health Sciences. 2011 Jul;21(2):101–9. doi: 10.4314/ejhs.v21i2.69050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Uzochukwu B, Onwujekwe O, Akpala C. Community satisfaction with the quality of maternal and child health services in southeast Nigeria. East African Medical Journal. East Afr Med J. 2004 Jun;81(6):293–9. doi: 10.4314/eamj.v81i6.9178. [DOI] [PubMed] [Google Scholar]
- 22.Ogaji DS, Giles S, Daker-White G, Bower P. Systematic review of patients’ views on the quality of primary health care in sub-Saharan Africa. SAGE Open Medicine. 2015;3:2050312115608338. doi: 10.1177/2050312115608338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baltussen R, Yé Y, Haddad S, Sauerborn RS. Perceived quality of care of primary health care services in Burkina Faso. Health Policy and Planning. 2002 Mar;17(1):42–8. doi: 10.1093/heapol/17.1.42. [DOI] [PubMed] [Google Scholar]
- 24.Garib Z, Vargas AL, Trumbo SP, et al. Missed Opportunities for Vaccination in the Dominican Republic: Results of an Operational Investigation. Biomed Res Int. 2016;2016:4721836. doi: 10.1155/2016/4721836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Drain PK, Nelson CM, Lloyd JS. Single-dose versus multi-dose vaccine vials for immunization programmes in developing countries. Bulletin of the World Health Organization. 2003;81(10):726–31. [PMC free article] [PubMed] [Google Scholar]
- 26.Byberg S, Fisker A, Rodrigues A, et al. Household experience and costs of seeking measles vaccination in rural Guinea-Bissau. Tropical medicine and International Health. 2016 doi: 10.1111/tmi.12793. [DOI] [PubMed] [Google Scholar]