Endovascular aneurysm repair (EVAR) has become the predominant operative repair for abdominal aortic aneurysms (AAA). Almost 75 per cent of the 45,000 AAA repairs annually are performed by an endovascular method. EVAR decreases perioperative mortality compared with an open repair; however, EVAR has increased risk of complications postoperatively. Because endoleaks are common (33% within two years),1 appropriate surveillance of these patients is important. Current guidelines recommend surveillance with 1-month and 12-month CT scanning, and an additional 6-month imaging if an endoleak is identified at 1 month. After 12 months, annual screening with CT or color duplex ultrasound (if no endoleak is found) is sufficient.2
Despite acceptance of these guidelines, many institutions have reported poor compliance (15–57%) among patients after EVAR.3, 4 Unfortunately, the causes for low adherence to follow-up is unclear. We hypothesized that travel distance, travel time, and patient income may predict which patients are at risk of poor compliance after EVAR. Finally, we evaluated the impact of surveillance compliance on patient morbidity and mortality. To identify potential solutions for these patients, we also queried whether these patients were able to attend appointments with other providers at our hospital over these time points.
After obtaining Institutional Review Board approval, we retrospectively identified all patients who received EVAR for infrarenal AAA from June 2009 to June 2013 at Emory University Hospital. Institutional electronic medical records (EMRs) were used to obtain all follow-up and patient data. Patients undergoing EVAR included those with both asymptomatic and symptomatic presentations, including rupture. Exclusion criteria included being treated for iliac artery aneurysm(s) and/or undergoing concomitant renal/mesenteric artery stenting.
Morbidity and mortality analysis was performed on all patients. Follow-up analysis was only conducted on patients surviving until their 12-month visit. Standard protocol included follow-up appointments at 1-, 6-, and 12-month postoperative clinic visits. Patient follow-up was divided into groups—complete follow-up, no follow-up, or limited follow-up (missing ≥1 time point). Nonvascular visits were also captured in our EMR. Travel distance and time were calculated using patients’ home addresses to the vascular clinic (Google Maps). Patient incomes were estimated from the average and median income of patients’ zip code. Secondary outcomes investigated included length of stay, discharge to home, overall survival, and perioperative complications.
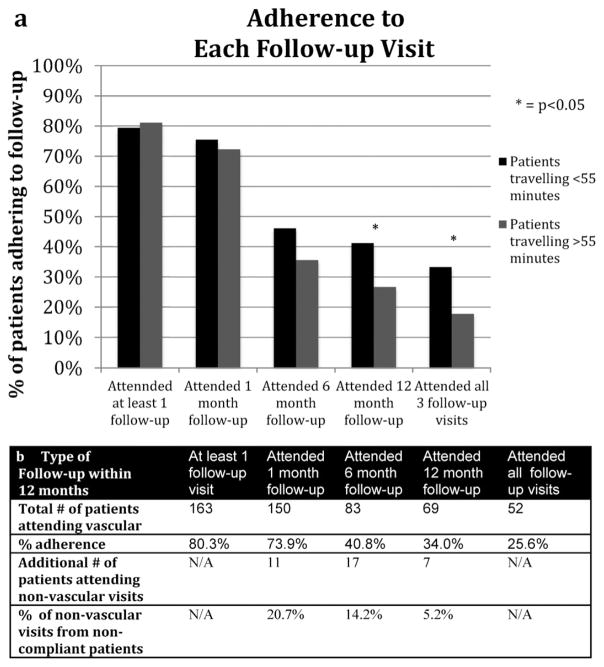
A total of 225 patients underwent standard EVAR who met inclusion criteria between June 2009 and June 2013. Twenty-two patients (10%) had mortality within one year leaving 203 patients to be included in follow-up analysis. A total of 173 patients (85%) had any follow-up with our vascular service, and 31 patients (15.3%) had no follow-up at our institution during this time period. Although 141 patients (70%) had limited follow-up, only 62 patients (19%) had complete follow-up compliance (Fig. 1A). Thirty-one patients (15%) were seen at our institution by various nonvascular surgeons during this time period with 14 patients being seen by our cardiology physicians (Fig. 1B).
Fig. 1.
(A) Adherence to various appointments based on patient traveling time. (B) Adherence to follow-up appointments based on type of provider.
The average and median distance traveled by patients were 77 miles and 45 miles, respectively, and the estimated time of their travel was a mean of 83 minutes and a median time of 55 minutes. Patients with incomplete follow-up had increased travel time compared with patients who had complete follow-up (90.3 vs 68.6 minutes; P = 0.049). In addition, patients below the median travel time had worse follow-up adherence (Table 1). As expected, those with better follow-up surveillance also had improved rates of CT scans when segregated by median travel time <55 minutes (45%) versus >55 minutes (29%) (P = 0.016). The median average income of all patients was calculated at $63,946. There were no differences in adherence rates for patients above and below the median income (79.8 vs 79.6%, P = 0.97). The top quartile versus bottom quartile of patients by income was also not significantly different (74.5 vs 78.0%, P = 0.68). Finally, travel time did not impact overall mortality [12.9 vs 9.1% (P = 0.396) for patients above or below the median travel time].
Table 1.
Comparison of Patients with Complete versus Incomplete Follow-up after EVAR
| All Patients (% or SD) (n = 225) | Complete Follow-up (% or SD) (n = 62) | No or Limited Follow-up (% or SD) (n = 141) | P value | |
|---|---|---|---|---|
| Age (years) | 73.3(8.0) | 73.3(7.4) | 73.1(8.2) | 0.856 |
| Male | 173(76.9%) | 49(79.0%) | 107(75.9% | 0.625 |
| Endoleak | 58(25.8%) | 19(30.6%) | 32(22.7%) | 0.229 |
| Rupture | 27(12.0%) | 5.00(8.1%) | 9.00(6.4%) | 0.663 |
| Major complications | 23(10.2%) | 1(1.6%) | 13(9.2%) | 0.049 |
| Discharged home | 206(91.6%) | 62(100%) | 131(92.9%) | 0.032 |
| Days to DC | 2.84(4.98) | 1.97(1.2) | 3.02(5.8) | 0.161 |
| Distance (miles) | 74.2(82.0) | 60.6(80.1) | 83.6(85.7) | 0.068 |
| Distance >100 miles | 44(19.6%) | 9(14.5%) | 32(22.7%) | 0.181 |
| Travel time (minutes) | 81.4(72.4) | 68.6(70.4) | 90.3(75.2) | 0.049 |
| Late mortality | 25(11.1%) | 7(11.3%) | 18(12.8%) | 0.768 |
We have identified travel time, but not travel distance or median income, as a predictor of poor compliance after EVAR. Because about 20 to 30 per cent of EVAR patients have problems identified during surveillance and approximately half of these patients undergo intervention, adherence to protocol surveillance is an important and possibly modifiable patient safety issue.1 However, adherence to follow-up is poor in our study, prior studies, and in larger reviews. Whereas other studies have attempted to understand what affects these poor rates of compliance, some of the identified factors are not modifiable, i.e., advanced age, chronic diseases, and Medicaid eligibility.3 Attempts to evaluate the effect of travel on follow-up adherence are still under investigation.3, 4
Emory University is uniquely situated in Atlanta, a large city with sprawling suburbs with traffic delays. Therefore, our clinic is particularly well suited to investigate the drivers of travel burden. Still, there are important limitations to this work. We understand that we do not capture those who had their follow-up outside of our institution (i.e., with referring physicians). Furthermore, patients were not surveyed as to why they did not follow up. This limitation is complicated as patients who do not follow up may be less likely to return such a survey, which would bias the survey instrument and limit interpretation.
We found that many of these patients who failed to follow up with vascular surgeons were seen by other providers within our system. Owing to the poor rates of follow-up, the Vascular Quality Initiative has placed EVAR with associated follow-up compliance as one of its quality improvement projects. Institutionally, Emory has an ongoing quality improvement initiative to address the poor adherence that we have seen. A large portion of no follow-up patients were seen with their primary cardiologist (47%). Although adjusting travel time and distance for patients is not feasible, coordination of care is crucial to combat this barrier. We propose that intelligent messaging within the EMR could improve surveillance compliance. Improved scheduling may allow for appointments with vascular surgeons and other specialties to fall on the same day. In addition, although clinic visits are important, appropriate imaging could be obtained without a visit to a vascular surgeon. Scheduling of outpatient imaging at local imaging centers may allow for review of EVAR for complications.
We have identified travel time as a significant factor in patient compliance and a driver of travel burden. EMR systems that enable other physicians within the system to assist in improving compliance may be able to limit the number of patients with no follow-up after EVAR. Further integration or documentation of what patients are being followed outside the system by referring physicians is key to knowing for sure how many of these patients are noncompliant with follow-up recommendations. We suggest integrating such information into the medical record as part of quality reporting.
Acknowledgments
Funding: KO8HL119592; SVS Foundation/American College of Surgeons Mentored Clinical Scientist Research Career Development Award; Emory Department of Surgery.
Contributor Information
Andrew D. Morris, Emory University Hospital, Department of Surgery, Division of Vascular Surgery, Atlanta, Georgia
Joshua E. Preiss, Emory University Hospital, Department of Surgery, Division of Vascular Surgery, Atlanta, Georgia
Samuel Ogbuchi, Morehouse School of Medicine, Atlanta, Georgia
Shipra Arya, Emory University Hospital, Department of Surgery, Division of Vascular Surgery, Atlanta, Georgia. Atlanta Veteran Affairs Medical Center, Division of Vascular Surgery, Decatur, Georgia
Yazan Duwayri, Emory University Hospital, Department of Surgery, Division of Vascular Surgery, Atlanta, Georgia
Thomas F. Dodson, Emory University Hospital, Department of Surgery, Division of Vascular Surgery, Atlanta, Georgia
William D. Jordan, Emory University Hospital, Department of Surgery, Division of Vascular Surgery, Atlanta, Georgia
Luke P. Brewster, Emory University Hospital, Department of Surgery, Division of Vascular Surgery, Atlanta, Georgia. Atlanta Veteran Affairs Medical Center, Division of Vascular Surgery, Decatur, Georgia
References
- 1.Lal BK, Zhou W, Li Z, et al. Predictors and outcomes of endoleaks in the veterans affairs open versus endovascular repair (OVER) trial of abdominal aortic aneurysms. J Vasc Surg. 2015;62:1394–404. doi: 10.1016/j.jvs.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 2.Chaikof EL, Brewster DC, Dalman RL, et al. SVS practice guidelines for the care of patients with an abdominal aortic aneurysm: Executive summary. J Vasc Surg. 2009;50:880–96. doi: 10.1016/j.jvs.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 3.Schanzer A, Messina LM, Ghosh K, et al. Follow-up compliance after endovascular abdominal aortic aneurysm repair in Medicare beneficiaries. J Vasc Surg. 2015;61(1):16–22. e11. doi: 10.1016/j.jvs.2014.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sarangarm D, Knepper J, Marek J, et al. Post-endovascular aneurysm repair patient outcomes and follow-up are not adversely impacted by long travel distance to tertiary vascular surgery centers. Ann Vasc Surg. 2010;24:1075–81. doi: 10.1016/j.avsg.2010.05.009. [DOI] [PubMed] [Google Scholar]