Abstract
Aims
Women are less likely than men to receive brief intervention (BI) for unhealthy alcohol use. In 2007, the U.S. Veterans Health Administration (VA) used a national performance measure to implement BI. Although AUDIT-C scores ≥3 for women and ≥4 for men optimize sensitivity and specificity for identifying unhealthy alcohol use, VA’s performance measure required BI only among a targeted subgroup defined by a non-gender-specific score threshold (AUDIT-C≥5). This may have influenced gender differences in receipt of BI among those optimally eligible for BI. Therefore, we evaluate differences in proportions of women and men offered BI before and after BI implementation.
Methods
National secondary chart review data (7/06-6/10) identified all outpatients with unhealthy alcohol use for whom BI would be indicated (AUDIT-C ≥3 women, ≥4 men). Logistic regression, including a time-by-gender interaction, estimated the prevalence and 95% confidence interval (CI) of BI for women and men pre- and post-implementation.
Findings
Among patients optimally eligible for BI (n=51,272, 8,206 women and 43,066 men), the prevalence of BI increased more steeply for men than women after implementation (interaction p-value <0.0001). Pre-implementation rates of BI were 21% (95% CI, 18-24) for women and 26% (95% CI, 24-29) for men, and post-implementation rates were 32% (95% CI, 30-34) for women and 47% (95% CI, 45-49) for men.
Conclusions
Healthcare systems implementing BI with performance measures may wish to consider that specifying a single alcohol screening threshold for men and women may increase gender differences in receipt of BI among patients likely to benefit.
Keywords: Alcohol, Brief intervention, Women, Gender, Alcohol Use Disorders, Disparities
1. INTRODUCTION
Brief intervention for primary care patients with unhealthy alcohol use identified by population-based alcohol screening reduces drinking (Jonas et al., 2012), is widely recommended (U.S. Preventive Services Task Force, 2004), and considered a top prevention priority (Maciosek et al., 2006). Despite strong recommendations for its use and rigorous tests of diverse implementation strategies, implementing brief intervention into care has proven challenging (Nilsen, Aalto, Bendtsen, & Seppa, 2006; Williams et al., 2011). However, the U.S. Veterans Health Administration (VA) has had success implementing first population-based alcohol screening and then brief intervention for screen-positive patients using national performance measures linked to financial incentives for network directors (Bradley et al., 2006; Lapham et al., 2012; Williams et al., 2014). These successes have highlighted performance measurement as a potentially successful implementation strategy (Williams et al., 2011) and the VA as a leader in implementation (Moyer & Finney, 2010).
In recent years, both in and outside of the U.S., national guidelines (National Health Service, 2010) and/or policies (Bendtsen et al., 2016; Centers for Medicare and Medicaid Services, 2011; HealthCare.gov, 2013a, 2013b) have incentivized implementation of brief intervention. Thus, healthcare systems are increasingly implementing this clinical service. In this context, the performance measure used by the VA may be replicated in other systems. Indeed, in collaboration with the Centers for Medicare & Medicaid Services, the Joint Commission developed a brief intervention quality measure similar to VA’s that is recommended as a common national hospital performance measure (The Joint Commission, 2016). Thus, understanding intended and unintended consequences of VA’s performance measure may optimize implementation of brief intervention across systems.
One important aspect to understand when evaluating implementation efforts is “reach,” which includes both the extent to which the target population for the intervention receives it and the extent to which the intervention is received equitably across sub-populations of the eligible population (Fitzgerald, Angus, Emslie, Shipton, & Bauld, 2016; Glasgow, McKay, Piette, & Reynolds, 2001; Glasgow, Vogt, & Boles, 1999). Historically, while randomized controlled trials of brief intervention suggest similar efficacy among women and men with unhealthy alcohol use (Fleming, Barry, Manwell, Johnson, & London, 1997; Fleming et al., 2000; Gebara, Bhona, Ronzani, Lourenco, & Noto, 2013; E. Kaner et al., 2013; Manwell, Fleming, Mundt, Stauffacher, & Barry, 2000), women have been less likely than men to receive brief interventions in practice (Bertakis & Azari, 2007; Burman et al., 2004; E. F. S. Kaner, Heather, Brodie, Lock, & McAvoy, 2001; Volk, Steinbauer, & Cantor, 1996). These differences have been hypothesized to result from increased stigma regarding alcohol use for and about women and the historically higher —but now increasingly equal (Slade et al., 2016)— prevalence of alcohol use disorders among men than women (Weisner & Schmidt, 1992).
Performance measurement is promoted as a means for incentivizing quality care via transparency and feedback (Austin, McGlynn, & Pronovost, 2016), and, because it can standardize practice, performance measurement also holds promise for reducing healthcare disparities (Institute of Medicine, 2006). However, the ability of performance measurement to realize these goals will depend on the extent to which measures are valid and well-specified (Pearson et al., 2002; Saitz, 2010) and the extent to which they do not result in unintended consequences (Austin et al., 2016; Chassin, Loeb, Schmaltz, & Wachter, 2010).
It is unknown whether and how VA’s performance measure for brief intervention influenced gender differences in receipt of brief intervention. The performance measure used by VA to implement brief intervention targets only a sub-population of the larger population of optimally eligible patients. Specifically, although AUDIT-C scores ≥3 for women and ≥4 for men optimize sensitivity and specificity for identifying unhealthy alcohol use (Bradley et al., 2003; Bradley et al., 2007; Bush, Kivlahan, McDonell, Fihn, & Bradley, 1998), VA’s performance measure requires documentation of brief intervention for all patients with AUDIT-C scores ≥5. While the decision to use a single cut-point was made to minimize the clinical burden of false-positive screens (Lapham et al., 2012), it could have inadvertently increased gender differences in receipt of brief intervention among patients likely to benefit.
Thus, among the total population of optimally eligible patients with unhealthy alcohol use, as well as among subpopulations of patients who were and were not targeted by VA’s implementation, we describe the proportion of women and men who were offered brief intervention both before and after implementation and evaluate whether gender differences in receipt of brief intervention changed in relation to implementation of brief intervention with a performance measure.
2. MATERIALS AND METHODS
2.1 Data Source and Study Sample
This national cross-sectional study used secondary chart review data collected by a VHA independent contractor, West Virginia Medical Institute (WVMI), through the External Peer Review Program (EPRP) 7/1/2006 – 11/30/2010. Each month, EPRP randomly samples both inpatients and outpatients at every VA medical center for standardized record review to monitor facility-level adherence to national performance measures and other recommended care. In order to monitor gender- and disease-specific care, EPRP oversamples patients with specific chronic diseases and women ages 20-69. Outpatients eligible for each month’s EPRP sample include those with an outpatient visit in the month preceding medical record review and another outpatient visit 13-24 months prior to the date of record review to establish VA care engagement. Patients included in the current fiscal year’s EPRP sampling are not eligible. Demographic and diagnostic information were obtained from the VA’s National Patient Care Databases (NPCD) and Patient Treatment Files (PTF). The study, including waivers of both informed consent and HIPAA authorization, was approved by the VA Puget Sound IRB.
Patients were included in the total study sample if they screened positive on their first documented AUDIT-C at optimal screening thresholds for unhealthy alcohol use (≥3 points for women and ≥4 points for men) (Bradley et al., 2003; Bush et al., 1998) and had at least 30 days between alcohol screening and chart abstraction to allow time for documentation of brief intervention. Two non-overlapping sub-samples of the total study sample were defined based on whether they were targeted by implementation. The first—patients not targeted by VA’s performance measure—included patients who screened positive for mild unhealthy alcohol use (women with AUDIT –C scores of 3-4 and men with AUDIT-C scores of 4) but were not targeted by the performance measure. The second—patients targeted by VHA’s performance measure—included patients with AUDIT-C scores ≥ 5, the denominator of VHA’s brief intervention performance measure.
2.2 Measures
Documented brief intervention was defined as (1) advice to abstain from drinking or drink within recommended limits and/or (2) feedback linking alcohol use to the patient’s specific or general health documented in the electronic medical record. These elements of brief intervention are consistent with those offered in randomized controlled trials of its efficacy (Whitlock, Polen, Green, Orleans, & Klein, 2004), and documentation of these elements is required to meet VA’s performance measure(Williams et al., 2014) and often facilitated with electronic clinical decision support (Williams et al., 2016). Gender was based on administrative documentation of male or female sex.
In preparation for the brief intervention performance measure, EPRP started monitoring receipt of brief intervention on 7/1/06, and VA’s performance measure for brief intervention was announced on 10/1/07 (Williams et al., 2014). Patients were categorized into 2 groups based on whether their positive alcohol screen occurred before (7/1/2006 – 9/30/2007) or after (10/1/2007 - 11/30-2010) implementation of the performance measure. While brief intervention was expected to be low prior to the performance measure, it was expected to be occurring at a non-zero rate simply as a result of having implemented alcohol screening.
Demographic and clinical characteristics were also ascertained. Demographic characteristics included age, race/ethnicity, marital status, and eligibility for VA coverage. AUDIT-C scores were categorized into alcohol use risk groups (3-4, 5, 6-7, 8-9, and 10-12), as higher scores reflect greater problem severity (Rubinsky, Dawson, Williams, Kivlahan, & Bradley, 2013). Other measures of alcohol use severity, other substance use and comorbid conditions were measured based on documentation of International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) diagnoses in the year prior to alcohol screening (L. J. Chavez, E. C. Williams, G. T. Lapham, & K. A. Bradley, 2012b; Deyo, Cherkin, & Ciol, 1992; Rubinsky et al., 2013).
2.3 Analyses
Characteristics were described and compared across gender using chi-square tests of independence in the total sample and the two population subsamples. To assess whether gender differences in receipt of brief interventions changed over time in association with implementation of the brief intervention performance measure, logistic regression models estimated the prevalence and 95% confidence interval (CI) of documented brief intervention for women and men. Regression models were conducted separately in all three samples (the total study sample, and both sub-samples); each model included a multiplicative time-by-gender interaction. Cluster-robust standard errors were estimated in order to address correlation of outcomes at the level of the facility. Models were otherwise unadjusted. Among each of the 3 study samples, post-estimation Wald-tests tested for gender differences in the prevalence of documented brief intervention before and after the performance measure. All analyses were conducted using Stata v11 (StataCorp., 2007).
3. RESULTS
Among 71,673 women and 319,171 men included in EPRPs electronic medical record chart reviews, 11% (n=8,206) women and 13% (n=43,066) men screened positive for unhealthy alcohol use (AUDIT-C ≥ 3 women and ≥ 4 men), making brief interventions appropriate. Among women for whom brief intervention was indicated (AUDIT-C ≥3), 5,462 (67%) were not targeted by the performance measure (AUDIT-C =3 or 4) and 2,744 (33%) were targeted by the performance measure (AUDIT-C ≥5). In contrast, among men for whom brief intervention was indicated (AUDIT-C ≥4), 18,202 (42%) were not targeted by the performance measure (AUDIT-C =4), and 24,863 (58%) were targeted by the performance measure (AUDIT-C ≥5).
Overall, the sample was consistent with other VA samples with unhealthy alcohol use (Williams et al., 2017)—generally older (>50 years) and non-Hispanic white with substantial mental health, substance use, and medical comorbidity (Table 1). Most characteristics differed across gender in the total sample, as well as among patients targeted and not targeted by the performance measure (Table 1). Rates of mental health, alcohol use and other substance use disorders, and medical comorbidities were generally higher among both women and men targeted by the performance measure than those not targeted and higher among women than men (e.g., for women and men, respectively, the prevalence of alcohol use disorders was 13% and 15% among those not targeted and 50% and 47% among those targeted).
Table 1.
Demographic and clinical characteristics of female and male Veteran outpatients who screened positive for unhealthy alcohol use: overall and among those targeted and not targeted by VA’s performance measure for brief intervention.
| Total Sample of Patients with Unhealthy Alcohol Use Indicated for Brief Intervention (BI) (AUDIT-C ≥3 women, ≥4 men) |
Patients with Unhealthy Alcohol Use not Targeted by VA’s Performance Measure for BI (AUDIT-C 3-4 women/4 men) |
Patients with Unhealthy Alcohol Use Targeted by VA’s Performance Measure for BI (AUDIT-C ≥ 5) |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||
| (n=51,272) | (n=23,665) | (n =27,607) | |||||||||||||
|
| |||||||||||||||
| Women (8,206) |
Men (43,066) |
Women (5,462) |
Men (18,203) |
Women (2,744) |
Men (24,863) |
||||||||||
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | ||||
| Age | * | * | * | ||||||||||||
| <25 | 178 | (2) | 304 | (1) | 109 | (2) | 67 | (0) | 69 | (3) | 237 | (1) | |||
| 25–34 | 1,372 | (17) | 2,228 | (5) | 909 | (17) | 603 | (3) | 463 | (17) | 1,625 | (7) | |||
| 35–49 | 3,073 | (37) | 5,315 | (12) | 1,899 | (35) | 1,406 | (8) | 1,174 | (43) | 3,909 | (16) | |||
| 50–64 | 3,210 | (39) | 21,972 | (51) | 2,224 | (41) | 7,863 | (43) | 986 | (36) | 14,109 | (57) | |||
| >=65 | 373 | (5) | 13,247 | (31) | 321 | (6) | 8,264 | (45) | 52 | (2) | 4,983 | (20) | |||
| Race | * | * | * | ||||||||||||
| Hispanic | 505 | (6) | 2,376 | (6) | 323 | (6) | 808 | (4) | 182 | (7) | 1,568 | (6) | |||
| Non-Hispanic Black | 51 | (1) | 767 | (2) | 29 | (1) | 249 | (1) | 22 | (1) | 518 | (2) | |||
| Non-Hispanic White | 1,394 | (17) | 10,107 | (24) | 924 | (17) | 4,470 | (25) | 470 | (17) | 5,637 | (23) | |||
| Other/Unknown | 6,256 | (76) | 29,816 | (69) | 4,186 | (77) | 12,676 | (70) | 2,070 | (75) | 17,140 | (69) | |||
| Married | 2,228 | (27) | 20,265 | (47) | * | 1,617 | (30) | 10,271 | (56) | * | 611 | (22) | 9,994 | (40) | * |
| Exempt from Mandatory VA Co-payment | 6,720 | (82) | 31,808 | (74) | * | 4,457 | (82) | 12,651 | (70) | * | 2,263 | (83) | 19,157 | (77) | * |
| Tobacco use (past year) | 3,967 | (48) | 19,908 | (46) | * | 2,254 | (41) | 6,016 | (33) | * | 1,713 | (62) | 13,892 | (56) | * |
| Any Mental Health Diagnosis | 5,630 | (69) | 21,382 | (50) | * | 3,452 | (63) | 7,082 | (39) | * | 2,178 | (79) | 14,300 | (58) | * |
| Count of Medical Diagnoses | * | * | * | ||||||||||||
| One | 1,203 | (15) | 8,219 | (19) | 762 | (14) | 3,379 | (19) | 441 | (16) | 4,840 | (20) | |||
| Two or More | 850 | (10) | 13,661 | (32) | 611 | (11) | 6,653 | (37) | 239 | (9) | 7,008 | (28) | |||
| AUDIT-C Category | * | ** | |||||||||||||
| AUDIT-C 3–4(W)/4(M) | 5,462 | (67) | 18,203 | (42) | 5,462 | (100) | 18,203 | (100) | 0 | (0) | 0 | (0) | |||
| AUDIT-C 5 | 799 | (10) | 6,826 | (16) | 0 | (0) | 0 | (0) | 799 | (29) | 6,826 | (28) | |||
| AUDIT-C 6–7 | 871 | (11) | 7,367 | (17) | 0 | (0) | 0 | (0) | 871 | (32) | 7,367 | (30) | |||
| AUDIT-C 8–9 | 504 | (6) | 4,955 | (12) | 0 | (0) | 0 | (0) | 504 | (18) | 4,955 | (20) | |||
| AUDIT-C 10–12 | 570 | (7) | 5,715 | (13) | 0 | (0) | 0 | (0) | 570 | (21) | 5,715 | (23) | |||
| Problem Substance Use* | 2,310 | (28) | 15,427 | (36) | * | 868 | (16) | 3,072 | (17) | 1,442 | (53) | 12,355 | (50) | ** | |
| Any Substance use Treatment | 998 | (12) | 5,916 | (14) | * | 305 | (6) | 871 | (5) | ** | 693 | (25) | 5,045 | (20) | * |
| Alcohol Use Disorders | 2,067 | (25) | 14,387 | (33) | * | 709 | (13) | 2,688 | (15) | ** | 1,358 | (50) | 11,699 | (47) | ** |
| Alcohol-Related Medical Diagnoses | 361 | (4) | 2,740 | (6) | * | 79 | (1) | 307 | (2) | 282 | (10) | 2,433 | (10) | ||
| Any non-Alcohol SUD Diagnosis | 811 | (10) | 4,536 | (11) | 314 | (6) | 862 | (5) | ** | 497 | (18) | 3,674 | (15) | * | |
chi-square test of independence comparing patient characteristics between men and women significant at p<0.001
chi-square test of independence comparing patient characteristics between men and women significant at p<0.05
In the total study sample, the estimated prevalence of brief intervention was 21% (95% CI, 18-24%) for women and 26% (24-29%) for men pre-implementation, and 32% (30-34%) for women and 47% (45-49%) for men, post- implementation (Figure 1). There were significant differences in receipt of brief intervention across gender both before (p<0.001) and after (p<0.001) the performance measure, and there was a significant time by gender interaction (p=0.0001) such that brief intervention increased for men more steeply than for women after implementation (Figure 1).
Figure 1.
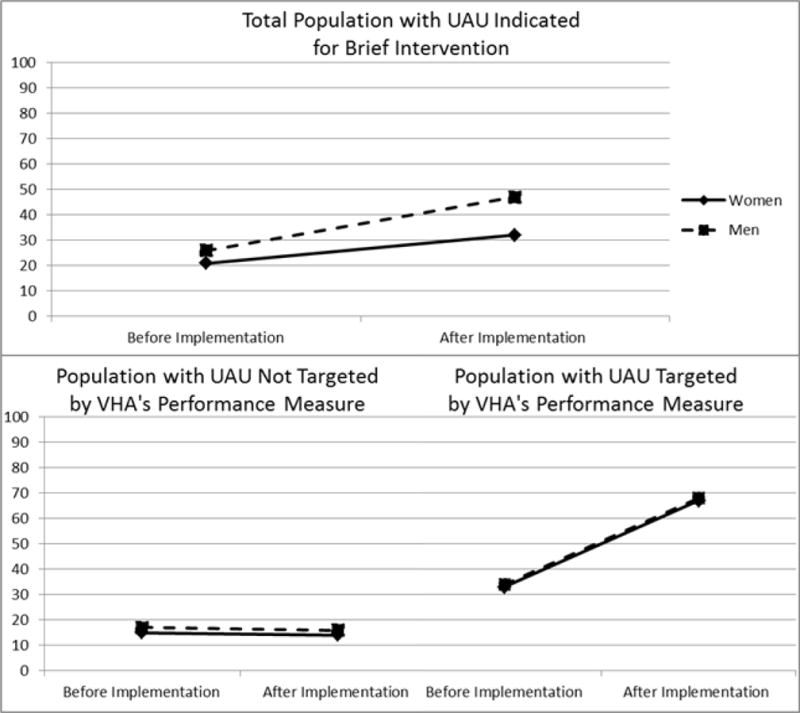
Estimated prevalence and 95% Confidence Interval (CI) of receipt of brief intervention (BI) for women and men before and after implementation of VA’s performance measure for BI: Among the total population with unhealthy alcohol use (UAU) optimally eligible for BI, as well as sub-populations targeted and not targeted by VA’s performance measure for BI.
The time by gender interaction was removed after stratification into subgroups of patients not-targeted by the performance measure (interaction p=0.25) and those targeted (interaction p=0.08). Among the subgroup not targeted by the performance measure, gender differences existed in the prevalence of brief intervention before (p=0.0038) and after (p=0.0042) the performance measure but prevalences were similar across time for both genders: 15% (95% CI 12-18%) for women and 17% (95% CI 14-21%) for men pre- and 14% (12-16%) for women and 16% (95% CI 14-19%) post-implementation. Among the subgroup targeted by the performance measure, there was a steep increase in documented brief intervention among all patients after implementation (from 34% to 68%) with no significant differences in brief intervention across gender before (p=0.1543) or after (p=0.16) implementation: 33% (30-36%) women and 34% (31-27%) men and 67% (65-69%) women and 68% (67-70%) men receiving brief intervention pre- and post-implementation, respectively.
4. DISCUSSION
This study described gender differences in receipt of brief intervention before and after implementation of a national performance measure for brief intervention in the VA and evaluated changes in receipt of brief intervention associated with implementation. Rates of brief intervention increased for both genders among patients targeted by VA’s performance measure and stayed stable among those not targeted. However, among all patients for whom brief intervention would have been appropriate, a smaller proportion of women than men had documented brief intervention both before and after the performance measure, and the gender difference in receipt of brief intervention increased 3-fold after implementation.
Findings revealed unintended consequences of implementation of the brief intervention performance measure in this large national healthcare system and raised questions regarding use of a single screening threshold for women and men to identify the targeted population. Specifically, as a result of the single screening threshold, the population targeted by implementation was not balanced across gender—only 33% of women compared to 58% of men with unhealthy alcohol use were targeted. While performance measurement has been hypothesized to reduce healthcare disparities (Institute of Medicine, 2003), the specifications of a performance measure will determine the extent to which differences in care receipt across subgroups are influenced. In this instance—the alcohol screening thresholds used to define the target population resulted in disproportionate targeting of women and men. Therefore, recommended care increased across genders in those targeted (an intended consequence), but gender differences in receipt of brief intervention in those optimally eligible increased substantially after implementation (an unintended consequence). Of note, although there was a significant time by gender interaction for the population as a whole, this interaction was eliminated by stratification into targeted and not-targeted groups suggesting that the gender differences were due to the differential targeting of the performance measure, not from implementation of the measure in a gender-discrepant manner.
Findings also suggest several unintended and potentially adverse consequences of VA’s performance measure on clinical care for women with unhealthy alcohol use. First, findings from this study suggest that VA’s performance measure for brief intervention does not incentivize its receipt for more than two-thirds of women who screen positive for unhealthy alcohol use. Though these women screen positive at low-levels of severity (AUDIT-C scores of 3 or 4), a previous study among female veterans found that women screening positive at these levels are at increased risk for poor alcohol-related consequences (e.g., blackouts) and self-reported symptoms of alcohol use disorders relative to low-level drinkers (L. J. Chavez, E. C. Williams, G. Lapham, & K. A. Bradley, 2012a). Thus, VA’s performance measure targeting patients with scores of 5 or more is likely missing an opportunity to intervene with a number of women who have already experienced alcohol-related problems. Similarly, the present study identified a greater prevalence of alcohol use disorders and specialty addictions treatment among women than men among patients targeted by the performance measure, indicating that the severity of alcohol use among those targeted by the performance measure may have been higher for women than men. This is consistent with previous studies demonstrating higher likelihood of alcohol use disorders and alcohol-related consequences among women than men at equivalent AUDIT-C scores (Rubinsky et al., 2013; Rubinsky, Kivlahan, Volk, Maynard, & Bradley, 2010). While data from randomized controlled trials that included women suggest similar efficacy of brief intervention among women and men with unhealthy alcohol use (Fleming et al., 1997; Fleming et al., 2000; Gebara et al., 2013; E. Kaner et al., 2013; Manwell et al., 2000), the efficacy of brief intervention may not extend to patients with the most severe alcohol use (Jonas et al., 2012). Thus, implementation efforts that inadvertently target women with greater severity than men may ultimately be associated with gender differences in response to brief intervention and alcohol-related outcomes.
Results of this study may be informative to healthcare systems implementing brief intervention. Because other healthcare systems may use similar performance measures for implementation, as was the case with the Joint Commission (The Joint Commission, 2016), it will be important for systems to consider potential unintended consequences of performance measures and their specifications, especially when selecting screening thresholds to identify target populations for whom care is incentivized. However, selection of an alcohol screening threshold for which follow-up care should be expected in a high-volume large healthcare system is not simple; consideration of influences on gender differences in care should be weighed against implications of adding workload. The choice of a screening threshold for a particular setting depends on the performance characteristics of the screen (sensitivity and specificity for unhealthy alcohol use) but also on the population prevalence of unhealthy alcohol use and the costs of false-positive screening relative to the benefits of true-positive screening (Bradley et al., 2003; Bradley et al., 2007). The benefits of true-positive alcohol screening include the benefits of brief intervention, as well as identifying patients who may benefit from more intensive interventions (Bradley & Williams, 2010). While unhealthy alcohol use is less common among women than men (Chavez et al., 2012b; Hawkins, Lapham, Kivlahan, & Bradley, 2010; Nolen-Hoeksema, 2004), women have increased morbidity and mortality compared to men who drink equivalent amounts (Bradley, Badrinath, Bush, Boyd-Wickizer, & Anawalt, 1998; Chavez et al., 2012b; Harris, Bradley, Bowe, Henderson, & Moos, 2010; Holman & English, 1996; Lembke, Bradley, Henderson, Moos, & Harris, 2011; Nolen-Hoeksema, 2004). Therefore, providing brief interventions to women may be at least as important as doing so for men. However, the costs associated with assessing and offering follow-up care to false-positive patients (e.g. opportunity costs, possible psychological detriment to patient) may be substantial.
This study has several limitations. First, alcohol screening results used to identify study samples were clinically documented, which may have resulted in mis-categorization (Bradley et al., 2011). Further, this study was observational; changes over time in gender differences may have been due to historical trends rather than VHA’s performance measure. Finally, this study evaluated associations between gender and receipt of brief intervention and does not address the quality of brief interventions received. Because other studies have identified quality concerns with brief interventions delivered clinically in VA (Williams et al., 2016; Williams et al., 2014), the clinical significance of this study’s findings may be limited.
Despite limitations, this study found that gender differences in receipt of brief intervention increased 3-fold after implementation of a brief intervention performance measure. This is likely because the majority of women (67%) versus slightly less than half of men (42%) screened positive for unhealthy alcohol use at levels not targeted by the performance measure. As healthcare systems use performance measures to implement brief intervention, they may wish to consider that specification of a single alcohol screening threshold for both men and women may increase gender differences in receipt of brief intervention.
Acknowledgments
The authors gratefully acknowledge both Jennifer Jenkins and Stacey Rittmueller, MPH for project administration and Stacey for editing early drafts of the manuscript.
SOURCES OF SUPPORT
Data for this study were provided by the VA Office of Analytics and Business Intelligence. This work was supported by the VA Substance Use Disorders Quality Enhancement Research Initiative (QLP 59-047; Williams PI). Dr. Williams is supported by a Career Development Award from VA HSR&D (CDA 12-276), and Dr. Bradley is supported by a mid-career mentorship award from NIAAA (K24-AA022128). Views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs, the University of Washington, or Kaiser Permanente Washington Health Research Institute.
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs, the University of Washington, Kaiser Permanente Washington Health Research Institute, or Ohio State University. This study, including a HIPAA waiver of written consent, was approved by Institutional Review Board at VA Puget Sound.
Footnotes
CONTRIBUTORS
All authors contributed to the article. ECW served as the principal investigator of the study, guiding all aspects of study design, analysis, interpretation, and preparation of the manuscript prior to submission and serving as the lead author of the manuscript. KAB served as senior investigator and senior author guiding analytic design and interpretation throughout the study; ECW and GTL conducted all data analyses; ADR contributed to data management and analysis; LJC and DB contributed to study design and interpretation. All authors contributed to study design and interpretation reviewed and contributed to iterative drafts of the manuscript prior to submission.
COMPETING INTERESTS
All authors declare no potential competing interests
References
- Austin JM, McGlynn EA, Pronovost PJ. Fostering Transparency in Outcomes, Quality, Safety, and Costs. The Journal of the American Medical Association. 2016;316(16):1661–1662. doi: 10.1001/jama.2016.14039. [DOI] [PubMed] [Google Scholar]
- Bendtsen P, Mussener U, Karlsson N, Lopez-Pelayo H, Palacio-Vieira J, Colom J, Anderson P. Implementing referral to an electronic alcohol brief advice website in primary healthcare: results from the ODHIN implementation trial. BMJ Open. 2016;6(6):e010271. doi: 10.1136/bmjopen-2015-010271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertakis KD, Azari R. Determinants of physician discussion regarding tobacco and alcohol abuse. Journal of Health Communication. 2007;12(6):513–525. doi: 10.1080/10810730701508187. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Badrinath S, Bush K, Boyd-Wickizer J, Anawalt B. Medical risks for women who drink alcohol. Journal of General Internal Medicine. 1998;13(9):627–639. doi: 10.1046/j.1525-1497.1998.cr187.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley KA, Bush KR, Epler AJ, Dobie DJ, Davis TM, Sporleder JL, Kivlahan DR. Two brief alcohol-screening tests from the Alcohol Use Disorders Identification Test (AUDIT): validation in a female Veterans Affairs patient population. Archives of Internal Medicine. 2003;163(7):821–829. doi: 10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcoholism, Clinical and Experimental Research. 2007;31(7):1208–1217. doi: 10.1111/j.1530-0277.2007.00403.x. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Lapham GT, Hawkins EJ, Achtmeyer CE, Williams EC, Thomas RM, Kivlahan DR. Quality concerns with routine alcohol screening in VA clinical settings. Journal of General Internal Medicine. 2011;26(3):299–306. doi: 10.1007/s11606-010-1509-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley KA, Williams EC. What Can General Medical Providers Do for Hospitalized Patients with Alcohol Dependence After Discharge? Journal of General Internal Medicine. 2010;25(10):1000–1002. doi: 10.1007/s11606-010-1441-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley KA, Williams EC, Achtmeyer CE, Volpp B, Collins BJ, Kivlahan DR. Implementation of evidence-based alcohol screening in the Veterans Health Administration. American Journal of Managed Care. 2006;12(10):597–606. [PubMed] [Google Scholar]
- Burman ML, Kivlahan DR, Buchbinder MB, Broglio K, Zhou XH, Merrill JO, Bradley KA. Alcohol-related advice for VA primary care patients: who gets it, who gives it? Journal of Studies on Alcohol. 2004;65(5):621–630. doi: 10.15288/jsa.2004.65.621. [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Archives of Internal Medicine. 1998;158(16):1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. Decision Memo for Screening and Behavioral Counseling Interventions in Primary Care to Reduce Alcohol Misuse (CAG-00427N) 2011 Retrieved from Available from: http://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=249#_ftn29. Accessed March 8, 2012:
- Chassin MR, Loeb JM, Schmaltz SP, Wachter RM. Accountability measures–using measurement to promote quality improvement. New England Journal of Medicine. 2010;363(7):683–688. doi: 10.1056/NEJMsb1002320. doi:NEJMsb1002320 [pii] 10.1056/NEJMsb1002320. [DOI] [PubMed] [Google Scholar]
- Chavez LJ, Williams EC, Lapham G, Bradley KA. Association between alcohol screening scores and alcohol-related risks among female veterans affairs patients. Journal of Studies on Alcohol and Drugs. 2012a;73(3):391–400. doi: 10.15288/jsad.2012.73.391. [DOI] [PubMed] [Google Scholar]
- Chavez LJ, Williams EC, Lapham GT, Bradley KA. Association between alcohol screening scores and alcohol-related risks among female Veterans Affairs patients. Journal of Studies on Alcohol and Drugs. 2012b;73(3):391–400. doi: 10.15288/jsad.2012.73.391. [DOI] [PubMed] [Google Scholar]
- Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of Clinical Epidemiology. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- Fitzgerald N, Angus K, Emslie C, Shipton D, Bauld L. Gender differences in the impact of population-level alcohol policy interventions: evidence synthesis of systematic reviews. Addiction. 2016 doi: 10.1111/add.13452. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/27177685. [DOI] [PubMed]
- Fleming MF, Barry KL, Manwell LB, Johnson K, London R. Brief physician advice for problem alcohol drinkers: a randomized controlled trial in community-based primary care practices. The Journal of the American Medical Association. 1997;277(13):1039–1045. [PubMed] [Google Scholar]
- Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, Barry KL. Benefit-cost analysis of brief physician advice with problem drinkers in primary care settings. Medical Care. 2000;38(1):7–18. doi: 10.1097/00005650-200001000-00003. [DOI] [PubMed] [Google Scholar]
- Gebara CF, Bhona FM, Ronzani TM, Lourenco LM, Noto AR. Brief intervention and decrease of alcohol consumption among women: a systematic review. Substance Abuse Treatment, Prevention, and Policy. 2013;8:31. doi: 10.1186/1747-597X-8-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, McKay HG, Piette JD, Reynolds KD. The RE-AIM framework for evaluating interventions: what can it tell us about approaches to chronic illness management? Patient Education and Counseling. 2001;44(2):119–127. doi: 10.1016/s0738-3991(00)00186-5. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. American Journal of Public Health. 1999;89(9):1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris AH, Bradley KA, Bowe T, Henderson P, Moos R. Associations between AUDIT-C and mortality vary by age and sex. Population Health Management. 2010;13(5):263–268. doi: 10.1089/pop.2009.0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins EJ, Lapham GT, Kivlahan DR, Bradley KA. Recognition and management of alcohol misuse in OEF/OIF and other veterans in the VA: a cross-sectional study. Drug and Alcohol Dependence. 2010;109(1-3):147–153. doi: 10.1016/j.drugalcdep.2009.12.025. doi:S0376-8716(10)00027-X [pii] 10.1016/j.drugalcdep.2009.12.025. [DOI] [PubMed] [Google Scholar]
- HealthCare.gov. What are my preventive care benefits? 2013a https://www.healthcare.gov/what-are-my-preventive-care-benefits/ Retrieved from.
- HealthCare.gov. What does marketplace health insurance cover? 2013b https://www.healthcare.gov/what-does-marketplace-health-insurance-cover/. Retrieved from.
- Holman CD, English DR. Ought low alcohol intake to be promoted for health reasons? Journal of the Royal Society of Medicine. 1996;89(3):123–129. doi: 10.1177/014107689608900303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. 2003 Retrieved from Washington, D.C.: [PubMed] [Google Scholar]
- Institute of Medicine. Performance Measurement: Accelerating Improvement. Washington, DC: The National Academies Press; 2006. Achieving a National System for Performance Measurement and Reporting; pp. 63–82. [Google Scholar]
- Jonas DE, Garbutt JC, Amick HR, Brown JM, Brownley KA, Council CL, Harris RP. Behavioral counseling after screening for alcohol misuse in primary care: a systematic review and meta-analysis for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2012;157(9):645–654. doi: 10.7326/0003-4819-157-9-201211060-00544. [DOI] [PubMed] [Google Scholar]
- Kaner E, Bland M, Cassidy P, Coulton S, Dale V, Deluca P, Drummond C. Effectiveness of screening and brief alcohol intervention in primary care (SIPS trial): pragmatic cluster randomised controlled trial. British Medical Journal. 2013;346:e8501. doi: 10.1136/bmj.e8501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaner EFS, Heather N, Brodie J, Lock CA, McAvoy BR. Patient and practitioner characteristics predict brief alcohol intervention in primary care. British Journal of General Practice. 2001;51(471):822–827. [PMC free article] [PubMed] [Google Scholar]
- Lapham GT, Achtmeyer CE, Williams EC, Hawkins EJ, Kivlahan DR, Bradley KA. Increased documented brief alcohol interventions with a performance measure and electronic decision support. Medical Care. 2012;50(2):179–187. doi: 10.1097/MLR.0b013e3181e35743. [DOI] [PubMed] [Google Scholar]
- Lembke A, Bradley KA, Henderson P, Moos R, Harris AH. Alcohol screening scores and the risk of new-onset gastrointestinal illness or related hospitalization. Journal of General Internal Medicine. 2011;26(7):777–782. doi: 10.1007/s11606-011-1688-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maciosek MV, Coffield AB, Edwards NM, Flottemesch TJ, Goodman MJ, Solberg LI. Priorities among effective clinical preventive services results of a systematic review and analysis. American Journal of Preventive Medicine. 2006;31(1):52–61. doi: 10.1016/j.amepre.2006.03.012. (see erratum page 458 Volume 432, Number 455) [DOI] [PubMed] [Google Scholar]
- Manwell LB, Fleming MF, Mundt MP, Stauffacher EA, Barry KL. Treatment of problem alcohol use in women of childbearing age: results of a brief intervention trial. Alcoholism, Clinical and Experimental Research. 2000;24(10):1517–1524. [PubMed] [Google Scholar]
- Moyer A, Finney JW. Meeting the challenges for research and practice for brief alcohol intervention. Addiction. 2010;105(6):963–964. doi: 10.1111/j.1360-0443.2010.02907.x. discussion 964-965. [DOI] [PubMed] [Google Scholar]
- National Health Service. National Institute for Health and Clinical Excellence: Alcohol-use disorders:preventing harmful drinking. NICE public health guidance 24. 2010 https://www.nice.org.uk/guidance/ph24. Retrieved from http://www.nice.org.uk/guidance/PH24.
- Nilsen P, Aalto M, Bendtsen P, Seppa K. Effectiveness of strategies to implement brief alcohol intervention in primary healthcare. A systematic review. Scandinavian Journal of Primary Health Care. 2006;24(1):5–15. doi: 10.1080/02813430500475282. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in risk factors and consequences for alcohol use and problems. Clinical Psychology Review. 2004;24(8):981–1010. doi: 10.1016/j.cpr.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Pearson ML, Ganz PA, McGuigan K, Malin JR, Adams J, Kahn KL. The case identification challenge in measuring quality of cancer care. Journal of Clinical Oncology. 2002;20(21):4353–4360. doi: 10.1200/JCO.2002.05.527. [DOI] [PubMed] [Google Scholar]
- Rubinsky AD, Dawson DA, Williams EC, Kivlahan DR, Bradley KA. AUDIT-C scores as a scaled marker of mean daily drinking, alcohol use disorder severity, and probability of alcohol dependence in a U.S. general population sample of drinkers. Alcoholism, Clinical and Experimental Research. 2013;37(8):1380–1390. doi: 10.1111/acer.12092. [DOI] [PubMed] [Google Scholar]
- Rubinsky AD, Kivlahan DR, Volk RJ, Maynard C, Bradley KA. Estimating risk of alcohol dependence using alcohol screening scores. Drug and Alcohol Dependence. 2010;108(1-2):29–36. doi: 10.1016/j.drugalcdep.2009.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitz R. Candidate performance measures for screening for, assessing, and treating unhealthy substance use in hospitals: advocacy or evidence-based practice? Annals of Internal Medicine. 2010;153(1):40–43. doi: 10.7326/0003-4819-153-1-201007060-00008. doi:153/1/40 [pii] 10.1059/0003-4819-153-1-201007060-00008. [DOI] [PubMed] [Google Scholar]
- Slade T, Chapman C, Swift W, Keyes K, Tonks Z, Teesson M. Birth cohort trends in the global epidemiology of alcohol use and alcohol-related harms in men and women: systematic review and metaregression. BMJ Open. 2016;6(10):e011827. doi: 10.1136/bmjopen-2016-011827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release Special Edition 10.1. College Station TX: Stata Corporation; 2007. [Google Scholar]
- The Joint Commission. Specifications Manual for National Hospital Inpatient Quality Measures. 2016 http://www.jointcommission.org/assets/1/6/Substance_Use_Measures_List.doc.pdf, accessed 4/29/17. Retrieved from.
- U.S. Preventive Services Task Force. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: Recommendation statement. Annals of Internal Medicine. 2004;140:554–556. doi: 10.7326/0003-4819-140-7-200404060-00016. [DOI] [PubMed] [Google Scholar]
- Volk RJ, Steinbauer JR, Cantor SB. Patient factors influencing variation in the use of preventive interventions for alcohol abuse by primary care physicians. Journal of Studies on Alcohol. 1996;57(2):203–209. doi: 10.15288/jsa.1996.57.203. [DOI] [PubMed] [Google Scholar]
- Weisner C, Schmidt L. Gender disparities in treatment for alcohol problems. The Journal of the American Medical Association. 1992;268(14):1872–1876. [PubMed] [Google Scholar]
- Whitlock EP, Polen MR, Green CA, Orleans T, Klein J. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2004;140(7):557–568. doi: 10.7326/0003-4819-140-7-200404060-00017. [DOI] [PubMed] [Google Scholar]
- Williams EC, Achtmeyer CE, Young JP, Rittmueller SE, Ludman EJ, Lapham GT, Bradley KA. Local implementation of alcohol screening and brief intervention at five Veterans Health Administration primary care clinics: perspectives of clinical and administrative staff. Journal of Substance Abuse Treatment. 2016;60:27–35. doi: 10.1016/j.jsat.2015.07.011. [DOI] [PubMed] [Google Scholar]
- Williams EC, Johnson ML, Lapham GT, Caldeiro RM, Chew L, Fletcher GS, Bradley KA. Strategies to implement alcohol screening and brief intervention in primary care settings: a structured literature review. Psychology of Addictive Behaviors. 2011;25(2):206–214. doi: 10.1037/a0022102. [DOI] [PubMed] [Google Scholar]
- Williams EC, Lapham GT, Shortreed SM, Rubinsky AD, Bobb JF, Bensley KM, Bradley KA. Among patients with unhealthy alcohol use, those with HIV are less likely than those without to receive evidence-based alcohol-related care: A national VA study. Drug and Alcohol Dependence. 2017;174:113–120. doi: 10.1016/j.drugalcdep.2017.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams EC, Rubinsky AD, Chavez LJ, Lapham GT, Rittmueller SE, Achtmeyer CE, Bradley KA. An early evaluation of implementation of brief intervention for unhealthy alcohol use in the US Veterans Health Administration. Addiction. 2014;109(9):1472–1481. doi: 10.1111/add.12600. [DOI] [PMC free article] [PubMed] [Google Scholar]


