Abstract
Background
There is a consensus that cancer care should go beyond physical care as cancer patients and their family caregivers experience psychological burden, financial difficulty, as well as social relation issues. The current study aimed to investigate the moderating impact of social support on depression and anxiety of cancer patients and their family caregivers.
Methods
Gastric cancer patients and their family caregivers who visited a university medical center in Seoul were approached for participation in the study. Fifty-two pairs of adult patients and caregivers participated in the study. Along with demographic information and the physical condition of the patients, such as pre-operation cancer stage and the type of gastrectomy, social support, depression, and anxiety were measured for patients and caregivers, respectively.
Results
In the first round of analysis, patients’ depression was associated with age, while patients’ anxiety was related to income. On the other hand, caregivers’ depression was not associated with patients’ health and living arrangement. In the second round of analysis to examine the moderating effect of social support, patients’ income and social support were related to depression and anxiety, but the interaction of income and social support was only observed for anxiety. For caregivers, no interaction effects were found. Social support decreased the negative effects of low income status on the patients.
Conclusion
While the income of the families with cancer cannot be adjusted in the short-term, their experience of social support can be managed by a proper support system. Diverse implications in medical settings are discussed.
Introduction
Cancer has been a leading cause of death across continents. 14 million new cases and 8.2 million deaths were related to cancer worldwide [1]. Five-year disease free survival varies by type of cancer, with an estimated rate of 74.4% for gastric cancer in South Korea (2010~2014) [2]. Given the increase in survival for cancer patients, psychosocial factors can have a significant impact on patients as well as their caregivers. Since the introduction of psycho-oncology as a field of specialty in providing care for cancer patients, it has become more common to assess the psychosocial factors that govern the quality of life of cancer patients. A systematic review notes that social support can have an effect on a number of different health indexes including cardiovascular, endocrine, and immune function [3], and more specifically with disease progression among breast cancer patients [4].
Cancer patients with relatively good prognosis, however, might lose attention and support from those in their social network. This can leave the family caregivers as the sole source of support during the long process of treatment and survivorship. Caregivers of cancer patients are reported to experience physical and psychological difficulties and are vulnerable to developing depression due to the stressors related to caregiving [5–7].
In this regard, the current study aimed to investigate the moderating role of social support on psychological well-being of both cancer patients and family caregivers.
Materials and methods
Procedures
The Institutional Review Board of the research site, a university medical center in Seoul, South Korea, approved the study (IRB Number 4-2014-0861). The opportunity for research participation was advertised in the gastric cancer division of its cancer center. Adult gastric cancer patients who were 18 or older and able to communicate in both oral and written Korean language were recruited. In addition, patients were recruited at least one month after surgery; by that point in time patients start experiencing minimal pain and physical strength to the degree that they can perform daily activities with almost no difficulty, including eating regular foods. Patients who expressed their interest in the study met with the research nurse to complete the informed consent. Then the patient was administered the survey in a quiet room. It took about 20–35 minutes to complete the cross-sectional survey.
In order to recruit family caregivers, the family members who accompanied the patients to the clinic were included. Caregivers who were 18 or older and had no barrier to communicate in Korean were recruited. When the caregiver expressed their interest, the research nurse administered the survey after gaining the informed consent. Each participant of the dyads completed the survey individually in a quiet space in the medical center. Fifty-two dyads of adult patients and family caregivers, 104 persons in total, participated in the study. There were no withdrawals during the course of the survey. All individuals who volunteered to participate completed the survey.
Measurements
Basic information
Demographic variables, including age, gender, marital status, education, religion, income, and living arrangement, were included in the patient and family caregiver questionnaires. These factors have been examined in previous studies of predictors of anxiety and/or depression among cancer patients [5–9]. To measure the physical condition of patients, pre-operation cancer stage and the type of gastrectomy were retrieved from the patients’ medical records, with the patients’ consent, by the medical doctor in the research team.
Social support
Duke-UNC Functional Social Support Questionnaire [10] was used to measure the perceived degree of social support. Participants were asked to rate the levels of 8 different types of support they received. Items of support include “people care what happened to me,” “love and affection,” “chances to talk to someone about problems at work or with my housework,” and “chances to talk to someone I trust about my personal and family problems”.
Depression and anxiety
The Hospital Anxiety and Depression Scale (HADS from below) was employed to measure the depression and anxiety of the participants [11]. Seven out of 14 items reflect depression; the other 7 items indicate anxiety. Total score of each subscale was used for depression (0 to 21) and anxiety (0 to 21) respectively in the analyses.
Analysis
Hierarchical multiple regression analyses were conducted to test the shared variance among the variables of interest. In the first round of analysis, we aimed to identify the significant predictors of depression and anxiety out of patients’ age, income, living arrangement, type of surgery, and cancer stage. In Model II, patients’ and caregivers’ social support were entered as predictors to see the effects on depression and anxiety of patients and caregivers, respectively.
The predictors shown to have significant main effects in the first round of analysis were selected to be entered in the second round of analysis to see the interaction effect with social support. In Model I, age and income were entered as predictors; in Model II, patients’ social support was entered as a predictor of patients’ depression and anxiety; and in Model III, the product terms of social support with age and income, respectively, were entered as predictors to investigate the moderating effect of social support.
Results and discussion
As Table 1 shows, there were more male patients than female patients. Only 4 percent of the participants lived alone. More than two thirds of the participants finished at least high school. Most of the patients (82.7%) had partial gastrectomy as treatment. Regarding the caregivers, only thirty-six or thirty-seven out of fifty-two participants provided the information on their gender, age, and relation to the patient.
Table 1. Characteristics of the participants.
| Items | N | Percent | |
|---|---|---|---|
| <Patients> | |||
| Gender | Male | 30 | 57.7 |
| Female | 22 | 42.3 | |
| Age | Mean | 54.3 | |
| SD | 12.1 | ||
| Income (USD/month) |
Mean | 3000 | |
| SD | 1700 | ||
| Living arrangement | Alone | 2 | 4.1 |
| With spouse | 14 | 28.6 | |
| With spouse and children | 24 | 49.0 | |
| With spouse and parents | 3 | 6.1 | |
| With spouse, children, and parents | 6 | 12.2 | |
| Education | No schooling | 1 | 1.9 |
| Primary school | 3 | 5.8 | |
| Middle school | 7 | 13.5 | |
| High school | 22 | 42.3 | |
| College/University | 18 | 34.6 | |
| Post-graduate | 1 | 1.9 | |
| Cancer stage | Stage 1 | 35 | 67.3 |
| Stage 2 | 8 | 15.4 | |
| Stage 3 | 9 | 17.3 | |
| Type of surgery | Partial gastrectomy | 43 | 82.7 |
| Total gastrectomy | 9 | 17.3 | |
| <Caregivers> | |||
| Gender | Male | 10 | 27.8 |
| Female | 26 | 72.2 | |
| Age | Mean | 45.0 | |
| SD | 12.8 | ||
| Relation to the patient | Spouse | 21 | 56.8 |
| Daughter | 5 | 13.5 | |
| Son | 4 | 10.8 | |
| Daughter-in-law | 3 | 8.1 | |
| Others | 4 | 10.8 | |
In the first round of analysis, Model I showed marginally significant effect of patients’ income on patients’ anxiety (Table 2). On the other hand, no predictors related to patients’ health or living status explained caregivers’ depression and anxiety in Model I (Table 3). However, when social support was entered in Model II, patients’ age had marginally significant effect on patients’ depression; patients’ income had significant predictability of patients’ anxiety. Also patients’ social support predicted patients’ anxiety, whereas caregivers’ social support explained both depression and anxiety of caregivers (Tables 2 and 3). In other words, there was no dyadic effect: patients’ social support neither predicted caregivers’ outcomes, nor did caregivers’ social support predict patients’ outcomes.
Table 2. Predictors of patient’s depression and anxiety.
|
Predictors |
Patient’s Depression | |||
| Model I (n = 50) | Model II (n = 50) | |||
| β (SE) | p value | β (SE) | p value | |
| Age | .387 (.267) | .157 | .525 (.257) | .056 |
| Income | -.498 (.019) | .101 | -.427 (.018) | .141 |
| Living arrangement | .125 (4.488) | .697 | .205 (4.230) | .502 |
| Kinds of surgery | -.219 (5.905) | .344 | -.139 (6.660) | .592 |
| Cancer stage | -.100 (3.108) | .668 | -.125 (2.907) | .569 |
| Patient’s social support | -.389 (.387) | .183 | ||
| Caregiver’s social support | -.083 (.444) | .783 | ||
|
Predictors |
Patient’s Anxiety | |||
| Model I (n = 48) | Model II (n = 48) | |||
| β (SE) | p value | β (SE) | p value | |
| Age | .021 (.108) | .937 | .273 (.079) | .170 |
| Income | -.523 (.007) | .069 | -.444 (.005) | .037 |
| Living arrangement | .160 (1.446) | .592 | .404 (1.049) | .078 |
| Kinds of surgery | -.373 (2.309) | .105 | -.244 (1.905) | .195 |
| Cancer stage | -.024 (1.207) | .918 | -.085 (.850) | .600 |
| Patient’s social support | -.688 (.114) | .005 | ||
| Caregiver’s social support | -.050 (.137) | .831 | ||
Table 3. Predictors of Caregiver’s depression and anxiety.
|
Predictors |
Caregiver’s Depression | |||
| Model I (n = 43) | Model II (n = 43) | |||
| β (SE) | p value | β (SE) | p value | |
| Age | .144 (.217) | .566 | .207 (.202) | .379 |
| Income | -.408 (.014) | .122 | -.323 (.012) | .173 |
| Living arrangement | .106 (2.925) | .709 | .246 (2.699) | .354 |
| Kinds of surgery | .000 (4.418) | .999 | -.166 (4.151) | .407 |
| Cancer stage | .246 (2.400) | .261 | .133 (2.171) | .497 |
| Patient’s social support | .245 (.246) | .271 | ||
| Caregiver’s social support | -.618 (.293) | .017 | ||
|
Predictors |
Caregiver’s Anxiety | |||
| Model I (n = 39) | Model II (n = 39) | |||
| β (SE) | p value | β (SE) | p value | |
| Age | .178 (.088) | .465 | .304 (.077) | .163 |
| Income | -.332 (.006) | .188 | -.217 (.005) | .305 |
| Living arrangement | .034 (1.190) | .901 | .227 (1.030) | .346 |
| Kinds of surgery | .291 (1.797) | .165 | .140 (1.584) | .442 |
| Cancer stage | .152 (.976) | .467 | .034 (.829) | .849 |
| Patient’s social support | .082 (.094) | .680 | ||
| Caregiver’s social support | -.634 (.112) | .008 | ||
We proceeded to investigate the main effects of age, income, and social support, as well as their interaction effects. In the second round of hierarchical multiple regression analyses, patients’ depression was explained by patients’ income and patients’ anxiety was explained by income, social support, and their interaction (Table 4). For caregivers’ outcomes, no predictors related to patients’ status or caregivers’ social support had significant predicting power (Table 5).
Table 4. Moderating effects of social support on patients’ depression and anxiety.
|
Predictors |
Patient’s Depression | |||||
| Model I (n = 50) | Model II (n = 50) | Model III (n = 50) | ||||
| β (SE) | p value | β (SE) | p value | β (SE) | p value | |
| Age | .105 (.149) | .534 | .122 (.141) | .449 | -.649(.900) | .526 |
| Income | -.394 (.009) | .026 | -.342 (.008) | .041 | -2.105 (.049) | .038 |
| Patient’s social support | -.337 (.227) | .042 | -1.625 (1.733) | .189 | ||
| Age*Social support | 1.067 (.027) | .463 | ||||
| Income*Social support | 1.925 (.002) | .074 | ||||
|
Predictors |
Patient’s Anxiety | |||||
| Model I (n = 48) | Model II (n = 48) | Model III (n = 48) | ||||
| β (SE) | p value | β (SE) | p value | |||
| Age | -.197 (.052) | .232 | -.217 (.042) | .106 | -1.445 (.244) | .067 |
| Income | -.409 (.003) | .016 | -.290 (.003) | .037 | -2.439 (.014) | .002 |
| Patient’s social support | -.566 (.069) | .000 | -2.432 (.475) | .010 | ||
| Age*Social support | 1.607 (.007) | .117 | ||||
| Income*Social support | 2.397 (.000) | .005 | ||||
Table 5. Moderating effects of social support on Caregivers’ depression and anxiety.
|
Predictors |
Caregiver’s Depression | |||||
| Model I (n = 43) | Model II (n = 43) | Model III (n = 43) | ||||
| β (SE) | p value | β (SE) | p value | β (SE) | p value | |
| Age | .114 (.144) | .531 | .068 (.140) | .698 | -.183 (.699) | .836 |
| Income | -.552 (.010) | .006 | -.400 (.011) | .052 | -.777 (.038) | .258 |
| Caregiver’s social support | -.335 (.253) | .102 | -.766 (1.281) | .450 | ||
| Age*Social support | .353 (.022) | .764 | ||||
| Income*Social support | .481 (.001) | .558 | ||||
|
Predictors |
Caregiver’s Anxiety | |||||
| Model I (n = 39) | Model II (n = 39) | Model III (n = 39) | ||||
| β (SE) | p value | β (SE) | p value | |||
| Age | .236 (.055) | .173 | .181 (.051) | .254 | 1.101 (.243) | .153 |
| Income | -.589 (.004) | .002 | -.407 (.004) | .027 | -.675 (.013) | .248 |
| Caregiver’s social support | -.401 (.092) | .031 | .476 (.446) | .579 | ||
| Age*Social support | -1.247 (.008) | .222 | ||||
| Income*Social support | .336 (.000) | .630 | ||||
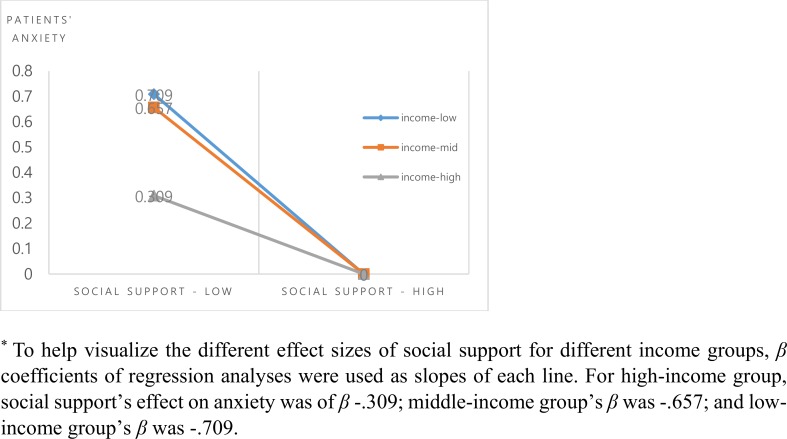
The interaction effect of patients’ income and social support on patients’ anxiety was found (Fig 1). When the participants were grouped into three different income groups (low, middle, and high tertiles), the effect of social support was highest for the low-income group, followed by the middle-income group and high-income group. In other words, the impact of social support was higher for those in low-income group than for those in the high-income group.
Fig 1. Patients’ social support and anxiety by income group.
Conclusions
Summary of results
In sum, the predictors that explained patients’ depression and anxiety were different from those that explained caregivers’ depression and anxiety. There were tendencies that older patients and patients with less income felt more depressed; and that patients with less income and patients with less social support felt more anxious. For caregivers, only caregivers’ social support explained their depression and anxiety: caregivers with less social support felt more depressed and anxious.
With respect to the interaction effect of social support and patients’ status, only patients’ anxiety was significantly explained by the interaction of patients’ income and their social support (for patients’ depression the interaction was marginally significant). More specifically, patients with less income was influenced more strongly by their social support or the lack thereof. By the same token, patients with more social support could be influenced less strongly by their income or the lack thereof.
Implications
It is well documented that people in low income households have higher likelihood to experience depression and anxiety, generally speaking [12–13]. For cancer patients, who are vulnerable to external stimuli because of their medical condition, in particular, the lack of monetary resources can pose a serious stress. By the same token, any support provided for the families struck by cancer can be helpful, and, as a matter of fact, it was stated so by cancer patients and caregivers alike [14].
On the other hand, management of financial status of all families in a society might need plans on a larger scheme. While cancer patients go through psychological hardships, along with the physical pain and difficulties, social support provided by their family and friends can have rather direct effects. Social support can buffer the psychological burden of the lack of monetary resources in the treatment process. Notwithstanding the positive effects that social support can have, cancer patients and caregivers are reluctant to seek support from others because of the perceived stigma related to cancer [14]. Therefore, education of family members and community members about cancer and its psychological impact could enhance positive communication and promote the natural flow of social support, which in turn can help reduce patients’ anxiety and depression [15].
Similarly, methods to educate medical professionals to provide support to their patients could potentially promote the well-being of everyone involved as well. Even though we know that discussions about the illness, prognosis, plausible treatment plans between patient and the medical team enhance the psychological well-being of cancer patients [16], it is typically not enacted in the education curriculum for medical professionals. Learning how to talk to cancer patients and their family caregivers supportively should be essential in medical settings, particularly where the burden of cancer is high.
Limitations and suggestions
With a set of 52 patient and caregiver dyads, it is hard to generalize the findings to other populations. The small number of participants might account for the lack of consistent results with other literature. For example, Given and colleagues’ study identified the most vulnerable family caregivers of cancer patients, according to their gender, age, employment status, and relationship to the patient [17]. However, the current study did not yield similar results, possibly due to limited statistical power.
Also the dataset was composed of gastric cancer only. Results cannot be generalized to other types of cancer, particularly if the prognosis is not as good, as in the case of lung or pancreatic cancer. For types of cancer that have lower survival rates, one of the biggest sources of concern for both patients and caregivers is the anxiety about relapse [14]. Furthermore, the dataset consisted of patients doing fairly well clinically. Thus the results might not be applicable to those with advanced cancer or in palliative care. Therefore, it is recommended to include various types of cancer, along with various stages of cancer, in the future studies.
Conclusions
Despite limitations, the current study provides insight on the moderating role of social support when it comes to the effect of income on patient’s anxiety. Cancer patients will benefit from social support to overcome their anxiety related to the medical condition, more so with those of low income than of high income. This provides perspective for the efforts to mobilize resources to support cancer patients.
Supporting information
(SAV)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by Samsung Medical Center grant (SMO1160041 & SMO1151341). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Stewart BW & Wild CP. World Cancer Report. World Health Organization, 2014.
- 2.National Cancer Information Center of Korea. Survival rate by cancer type. Retrieved in January 2017 from http://www.cancer.go.kr/mbs/cancer/subview.jsp?id=cancer_040302000000.
- 3.Uchino BN. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. J Behav Med, 2006; 29(4): 377–387. doi: 10.1007/s10865-006-9056-5 [DOI] [PubMed] [Google Scholar]
- 4.Nausheen B, Gidron Y, Peveler R, Moss-Morris R. Social support and cancer progression: A systematic review. J Psychosom Res, 2009; 67(5): 403–415. doi: 10.1016/j.jpsychores.2008.12.012 [DOI] [PubMed] [Google Scholar]
- 5.Gaston-Johansson F, Lachica EM, Fall-Dickson JM, Kennedy MJ. Psychological distress, fatigue, burden of care, and quality of life in primary caregivers of patients with breast cancer undergoing autologous bone marrow transplantation. Oncol Nurs For, 2004; 31(6): 1161–1169. [DOI] [PubMed] [Google Scholar]
- 6.Glajchen M. The emerging role and needs of family caregivers in cancer care. J Support Oncol, 2004; 2(2): 145–155. [PubMed] [Google Scholar]
- 7.Haley WE. Family caregivers of elderly patients with cancer: Understanding and minimizing the burden of care. J Support Oncol, 2003; 1(2): 25–29. [PubMed] [Google Scholar]
- 8.Lloyd GG, Parker AC, Ludlam CA, McGuire RJ. Emotional impact of diagnosis and early treatment of lymphomas. J Psychosom Res, 1984; 28: 157–62. [DOI] [PubMed] [Google Scholar]
- 9.Pettingale KW, Burgess C, Greer S. Psychological response to cancer diagnosis-I. Correlations with prognostic variables. J Psychosom Res, 1987; 32: 255–61. [DOI] [PubMed] [Google Scholar]
- 10.Broadhead W. E., Gehlbach S. H., de Gruy F. V., & Kaplan B. H. The Duke-UNC functional social support questionnaire: Measurement of social support in family medicine patients. Med Care, 1988; 26(7): 709–723. [DOI] [PubMed] [Google Scholar]
- 11.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiat Scand, 1983; 67(6): 361–370. [DOI] [PubMed] [Google Scholar]
- 12.Melchior M, Chastang J-F, Walburg V, Arseneult L, Galera C, Fombonne E. Family income and youths’ symptoms of depression and anxiety: A longitudinal study of the French GAZEL youth cohort. Depress Anxiety, 2010; 27(12): 1095–1103. doi: 10.1002/da.20761 [DOI] [PubMed] [Google Scholar]
- 13.Sareen J, Afifi TO, McMillan KA, Asmundson GJG. Relationship between household income and mental disorders. Arch Gen Psychiat, 2011; 68(4): 419–427. doi: 10.1001/archgenpsychiatry.2011.15 [DOI] [PubMed] [Google Scholar]
- 14.Jeong A, An JY, Park JH, Park K. What cancer means to the patients and their primary caregivers in the family-accounted Korean context: A dyadic interpretation. Psycho-Oncology, in press. [DOI] [PubMed] [Google Scholar]
- 15.Jeong A, Shin DW, Kim SY, Yang HK, Park JH. Avoidance of cancer communication, perceived social support, and anxiety and depression among patients with cancer. Psycho-Oncology, 2016; 25(11): 1301–1307. doi: 10.1002/pon.4060 [DOI] [PubMed] [Google Scholar]
- 16.Otani K, Uchitomi Y. Psychology of cancer patients and their mental care. Nihon Jibiinkoka Gakkai Kaiho, 2010; 113(2): 45–52. [DOI] [PubMed] [Google Scholar]
- 17.Given B, Wyatt G, Given C, Gift A, Sherwood P, DeVoss D, et al. Burden and depression among caregivers of patients with cancer at the end-of-life. Oncol Nurs For, 2005; 31(6): 1105–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(SAV)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.