Abstract
Background
Patients undergoing coronary artery bypass grafting (CABG) must often see multiple providers dispersed across many care locations. To test whether “teamwork” (assessed with the bipartite clustering coefficient) among these physicians is a determinant of surgical outcomes, we examined national Medicare data from patients undergoing CABG.
Methods and Results
Among Medicare beneficiaries who underwent CABG between 2008 and 2011, we mapped relationships between all physicians who treated them during their surgical episodes, including both surgeons and nonsurgeons. After aggregating across CABG episodes in a year to construct the physician social networks serving each health system, we then assessed the level of physician teamwork in these networks with the bipartite clustering coefficient. Finally, we fit a series of multivariable regression models to evaluate associations between a health system’s teamwork level and its 60-day surgical outcomes. We observed substantial variation in the level of teamwork between health systems performing CABG (standard deviation for the bipartite clustering coefficient was 0.09). While health systems with high and low teamwork levels treated beneficiaries with comparable comorbidity scores, these health systems differed over several sociocultural and healthcare capacity factors (e.g., physician staff size, surgical caseload). After controlling for these differences, health systems with higher teamwork levels had significantly lower 60-day rates of emergency department visit, readmission, and mortality.
Conclusions
Health systems with physicians who tend to work together in tightly knit groups during CABG episodes realize better surgical outcomes. As such, delivery system reforms focused on building teamwork may have positive effects on surgical care.
Keywords: coronary artery bypass graft surgery, health outcomes, health services research, team-based care
Journal Subject Terms: Cardiovascular Surgery, Quality and Outcomes, Health Services
Surgical outcomes after coronary artery bypass grafting (CABG) vary significantly across hospitals in the United States (U.S.), even after adjusting for case-mix differences.1,2 To reduce variability in CABG outcomes, numerous quality improvement initiatives have been launched, including national and regional collaboratives,3,4 clinical pathways,5,6 and pay-for-performance programs.7,8 Despite some encouraging results, unwarranted variation in CABG outcomes persists. Critics suggest that part of the problem relates to the one-dimensional nature of these initiatives, which primarily target cardiac surgeons’ activities in the operating room and immediately following surgery.
However, there is growing recognition that CABG is not an “individual game” but rather a “team sport,” involving multiple physicians who work together before, during, and after surgery. Frequent interactions between these physician teammates around shared patients may influence their collective performance.9,10 Specifically, as the number of their interactions increases, physician teammates will build trust and familiarity, be more likely to anticipate each other’s practice patterns, and establish preferred ways of communication. Such enhanced teamwork could have salutary effects on CABG outcomes, particularly downstream ones beyond the early perioperative period.
In this context, we analyzed national data from Medicare beneficiaries who underwent CABG. We used network analytical tools, in particular the bipartite clustering coefficient, to characterize the level of teamwork among cardiac surgeons and nonsurgeons in the health systems where these procedures were performed. We then compared surgical outcomes across health systems, stratifying by their teamwork level. Findings from our study serve to inform hospitals and health system leaders about the possible effects of healthcare reforms designed to foster physician team building—most notably the patient-centered medical home, bundled payments, and accountable care organizations (ACOs)—on surgical outcomes.
Methods
Data source and study population
We began by identifying all beneficiaries age 66 and older in the Medicare Provider Analysis and Review (MedPAR) file who underwent CABG in U.S. hospitals between January 1, 2008 and December 30, 2011. Several considerations make CABG attractive for the purposes of our study. First, CABG is commonly performed on older adults, and the procedure always requires inpatient admission, helping to ensure its reliable identification in Medicare claims. Second, outcomes for CABG vary widely across health systems for reasons not attributable to differences in clinical risk. Third, the complexity of CABG typically demands the attention of multiple providers. As a result, relationships between primary care physicians (PCPs), noninvasive and interventional cardiologists, and cardiac surgeons may be especially important for shaping outcomes.
To ensure complete claims data, we required that beneficiaries had continuous enrollment in fee-for-service Medicare Parts A and B for a total of six months prior to and extending 60 days after their admission for surgery for inclusion in our sample. After identifying all beneficiaries who met these criteria, we then used the MedPAR file to determine the hospitals where their CABG was performed. These hospitals serve formally and informally as anchors for outpatient clinics and other facilities that constitute local health systems.
Mapping the physician teams that serve the health systems where beneficiaries are treated
Next, we identified all physicians who participated in the care of these beneficiaries during their surgical episodes through paid claims in the Carrier, MedPAR, and Outpatient files. We designated each beneficiary’s treating surgeon as the surgeon who billed for cardiac surgery services closest to the surgery date (available in the MedPAR file). To determine each beneficiary’s primary care physician (PCP), we used the plurality algorithm described by Pham and colleagues.11 To find care provided by other medical and surgical specialists, we constructed a time window that began 30 days prior to and extended 60 days after the index admission. We excluded claims submitted by physicians who do not participate in direct patient care (e.g., radiology) and those who have limited roles in perioperative management (e.g., pathology).
We then aggregated across all CABG episodes at a given anchor hospital by calendar year, to construct CABG-specific, bipartite physician social networks. Briefly, networks are collections of points (or nodes) connected together in series of lines (called ties).12 In social networks, the nodes represent individuals or groups of individuals within a particular social environment, and each tie connecting them denotes an interaction. For our bipartite networks, there were two sets of nodes (physicians and beneficiaries), and the ties connected one set of nodes to the other. We used these networks to represent the physician teams that serve each health system where beneficiaries are treated.
Characterizing the level of physician teamwork in a health system
To characterize the level of physician teamwork in a given health system, we calculated the bipartite clustering coefficient for its associated physician social network. The method for determining the bipartite clustering coefficient is shown schematically in Figure 1. Mathematically, the coefficient was measured as 4* (M/S), where S is the number of physician pairs sharing a single patient (or more) common and M is the number of physician pairs sharing at multiple patients in common.13,14 We multiplied the ratio of M/S by four because each M contains four S configurations. The number of M relationships indicates the extent to which physicians re-partner with one another in the care of multiple patients.
Figure 1.
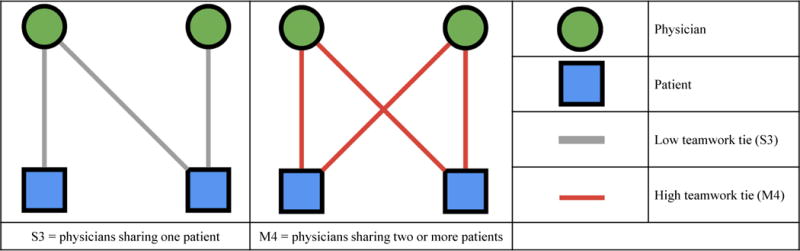
Measuring a physician referral network’s level of teamwork. We computed our measure of teamwork, the bipartite clustering coefficient, by counting, for each hospital network, the total number of pairs of physicians who share a single patient (or more) in common, denoted S (see the left panel in the figure), and the total number of pairs of physicians who share multiple patients in common, denoted M (see the middle panel in the figure). After obtaining these values, we calculated the measure as M/S. We multiply the final value by four because there are four S configurations for every M configuration.
The bipartite clustering coefficient summarizes the tendency for physicians in the network to assemble into dense, tightly-interconnected groups (or cliques) around shared patients.12 In bipartite networks like ours, if the bipartite clustering coefficient is high, then many of the L relationships—connections formed when physicians share in the care of only one patient—are redundant, and therefore they reinforce existing relationships between physicians. The measure ranges from 0 to 1. Values closer to 1 indicate higher levels of clustering in the physician social network.
Clustering has long been used in the social sciences to explore the role of coordination, communication, and trust in teams.15–17 Social network theory suggests that highly clustered networks are more effective as information conduits because they improve the ability of collaborating physicians to share information and develop innovative protocols for treatment.18,19 To the extent that clustering promotes these different forms of teamwork, we hypothesized that it may also lead to improved surgical outcomes.
Assessing surgical outcomes
Our primary outcome measures were 60-day rates of emergency department (ED) visit, readmission, and mortality—all three of which are plausibly influenced by physician teamwork. We considered an ED visit, readmission, or death as having occurred if a patient was discharged alive from the acute care hospital where he underwent surgery, and he was subsequently seen in the ED, readmitted at any acute care hospital, or died within 60 days from the date of discharge. We excluded from the readmission definition patients who were transferred to another hospital or to a rehabilitation facility at the time of initial discharge. We aggregated all outcomes for individual patients to the health system level to calculate rates per 1,000 discharges.
Statistical analysis
For all analyses, our unit of analysis was the health system-year. In our initial analytic step, we used one-way analysis of variance to make comparisons between health systems stratified by their physician teamwork level. For these comparisons, we broke our observations (hospital X years) into three equal groups. The clustering coefficient values were [0, 0.200] for the low group (n=1,514), [0.201, 0.273] for the moderate group (n=1,513), and [0.274, 0.714] for the high group (n=1,513). Specifically, we compared the communities [defined using hospital service area (HSA) boundaries20] served by each health system over a range of sociocultural (total resident population, total black population, total Hispanic population, proportion of residents living below federal poverty line, proportion of residents with a bachelor’s degree, proportion of residents living in a rural area) and healthcare capacity factors (number of acute care hospital beds per 1,000 residents, number of PCPs per 100,000 residents, number of medical specialists per 100,000 residents, number of surgeons per 100,000 residents).
In addition, we evaluated differences between anchor hospitals where CABG was performed in health systems with low versus high teamwork levels. Specific hospital factors examined included the number of CABG patients treated, the number of physicians providing care around the CABG episode, the proportion of CABG patients from outside the Core-Based Statistical Area in which the hospital was located, and the mean Charlson score for the hospital’s CABG patients.21 We also used data from the American Hospital Association Annual Survey to compare anchor hospitals with regards to their academic status.22
We then estimated a series of multivariable regression models to assess whether surgical outcomes (60-day ED visit, readmission, and mortality) varied significantly by a health system’s teamwork level. We used a random-effects negative binomial specification to model care teamwork, treating the health system’s bipartite clustering coefficient as a continuous predictor. In our random intercept models, we included random effects for health system. We adjusted our models for the hospital- and HSA-level factors described above, as well as for the number of physicians in the network. All models had year fixed effects (i.e., a categorical variable for year was included in each model; the reference year was 2008).
Finally, we performed several sensitivity analyses to test the robustness of our findings. To determine whether our results were influenced by differences in case severity between health systems, we reran our models controlling for the proportion of a health system’s CABG procedures that were performed during an urgent or emergent admission. Given that early mortality after CABG may be a marker for more severe cardiac disease, we repeated our analyses controlling for the proportion of beneficiaries undergoing CABG in a health system that survived more three days post-procedure. To examine the effects of shortening or lengthening the claims window used to measure our outcomes of interest, we also fit separate models based on 30- and 90-day follow-up periods, respectively.
We performed all analyses using Stata SE Version 13.1. All tests were two-tailed, and the probability of Type 1 error was set at 0.05. The Health Sciences Institutional Review Board of the University of Michigan approved this study.
Results
In total, we examined 251,630 Medicare beneficiaries who underwent CABG during the study period. Over the course of their surgical episodes, these beneficiaries were cared for by 466,243 physicians practicing in 1,186 health systems. The level of teamwork for CABG varied substantially across these health systems. Specifically, the minimum observed value for a health system’s bipartite clustering coefficient was 0 (where no physicians shared multiple patients), and the maximum observed value was 0.71 (where many physicians shared multiple patients).
As an example, Figure 2 shows two physician referral networks at health systems in Texas with higher and lower levels of teamwork for CABG based on 2011 data. Despite being only 90 miles apart and having similar patient and physician counts, there are visually striking differences between the two with regards to their patterns of ties and, hence, clustering. For example, physicians in Fort Worth share relatively few patients with their colleagues, as indicated by the large number of gray-colored ties in the corresponding network diagram (Figure 2, left panel). With a bipartite clustering coefficient of 0.097, the Fort Worth health system has a relatively low level of teamwork for CABG and the network appears to be fragmented with a highly decentralized structure. By contrast, the network diagram for Waco (Figure 2, right panel) is highly interconnected around a dense core of physicians who share many patients (as indicated by the many red colored ties). A bipartite clustering coefficient of 0.428 suggests a high level of teamwork through referral relationships around patients undergoing CABG in this health system.
Figure 2.
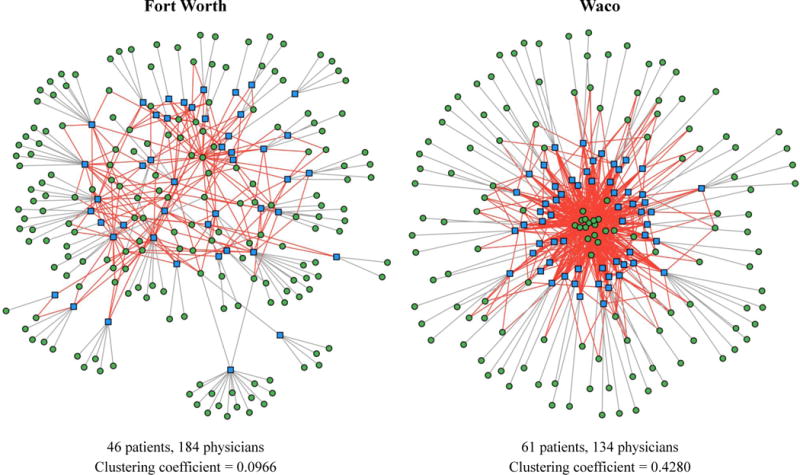
Illustrative example of two health systems in Texas where CABG procedures were performed, based on 2011 data. The network diagrams above demonstrate the wide variation in teamwork levels among sample hospitals. The left hand side shows a hospital in Fort Worth, Texas, where physicians rarely share more than one patient in common, as indicated by the low density of red ties (which correspond to the M component of our bipartite clustering coefficient) and the overall sparseness of the network. The right hand side, by contrast, shows a hospital in Waco, Texas, where teamwork is much more common. The network diagram shows a high density of red ties, indicating many shared patients among physicians. These many overlapping ties have the effect of bringing members of the network close together, as seen in the center of the diagram. Notice that both hospitals have a similar number of patients and physicians, and differences in teamwork levels are not attributable to simple differences in network size.
Local health systems and teamwork levels
Compared to health systems with high teamwork levels for CABG, those with low levels served communities with higher proportions of black and Hispanic residents (Table 1, P<0.001 for each comparison). Their communities were, on average, less rural, and they had a higher proportion of college-educated residents (P<0.001 for each comparison). With regards to healthcare capacity, health systems with low teamwork levels for CABG tended to have more PCPs and medical specialists but fewer acute care beds and surgeons per capita (P<0.001 for each comparison).
Table 1.
Comparisons between communities served by health systems with low, moderate, and high levels of physician teamwork (2011 data).
| Low | Moderate | High | |||||
|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Mean | SE | P-Value | |
| Regional sociocultural factors | |||||||
| Total resident population (in thousands, log) | 13.65 | 1.08 | 13.16 | 1.11 | 12.75 | 1.05 | 0.00 |
| Proportion of residents living below federal poverty line (mean)* | 0.13 | 0.05 | 0.14 | 0.04 | 0.14 | 0.05 | 0.06 |
| Proportion of residents with a bachelor’s degree (mean)* | 0.18 | 0.05 | 0.17 | 0.05 | 0.16 | 0.05 | 0.00 |
| Proportion of residents living in a rural area (mean)* | 0.24 | 0.19 | 0.26 | 0.20 | 0.31 | 0.23 | 0.00 |
| Total black population (in thousands, log) | 11.26 | 1.86 | 10.62 | 1.88 | 10.09 | 1.91 | 0.00 |
| Total Hispanic population (in thousands, log) | 11.45 | 1.73 | 10.76 | 1.79 | 10.16 | 1.74 | 0.00 |
| Regional healthcare capacity factors | |||||||
| No. of acute care hospital beds per 1,000 residents (mean) | 2.29 | 0.58 | 2.39 | 0.63 | 2.44 | 0.70 | 0.00 |
| No. of PCPs per 100,000 residents (mean) | 69.41 | 17.03 | 67.20 | 16.38 | 66.16 | 15.16 | 0.02 |
| No. of medical specialists per 100,000 residents (mean) | 48.74 | 14.76 | 45.79 | 13.83 | 42.69 | 11.62 | 0.00 |
| No. of surgeons per 100,000 residents (mean) | 37.60 | 9.03 | 37.73 | 9.23 | 38.52 | 8.46 | 0.31 |
Estimated using levels found in patients’ home ZIP codes
Abbreviations: CBSA, core-based statistical area; No., number; PCP, primary care physician; SE, standard error
Characteristics of the hospitals within these local health systems where CABG procedures were performed are displayed in Table 2. Generally speaking, the level of comorbid illness for patients undergoing CABG was comparable between hospitals. However, hospitals in health systems with low levels of teamwork for CABG were more likely to have an academic affiliation (P<0.001). In addition, they had larger physician staffs, treated more cardiac patients, and received more surgical referrals from outside their immediate geographic area (P<0.001 for each comparison) than those hospitals in health systems with high teamwork levels for CABG.
Table 2.
Comparisons between anchor hospitals of health systems with low, moderate, and high levels of physician teamwork (2011 data).
| Low | Moderate | High | P-Value | ||||
|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Mean | SE | ||
| Anchor hospital characteristics | |||||||
| No. of CABG patients (mean) | 63.65 | 57.30 | 42.28 | 31.00 | 27.23 | 22.38 | 0.00 |
| No. of physicians caring for CABG (mean) | 238.77 | 224.94 | 151.34 | 95.10 | 90.16 | 58.54 | 0.00 |
| Proportion of CABG patients from outside the CBSA (mean) | 0.55 | 0.26 | 0.52 | 0.23 | 0.44 | 0.24 | 0.00 |
| Mean Charlson score for CABG patients | 2.31 | 0.61 | 2.39 | 0.56 | 2.36 | 0.65 | 0.22 |
| Academic status | 0.63 | 0.48 | 0.53 | 0.50 | 0.44 | 0.50 | 0.00 |
Abbreviations: CABG, coronary artery bypass grafting; CBSA, core-based statistical area; SE, standard error
Teamwork level and CABG outcomes
After accounting for the above differences between health systems, we found that higher levels of teamwork were associated with significantly improved CABG outcomes (full model results are displayed in Table 3 and the Supplementary Table). Adjusted rates of ED visit, readmission, and mortality stratified by a health system’s teamwork level for CABG, are displayed in Figure 3. Health systems with physician teams that worked together frequently around CABG episodes achieved ED visit, readmission, and mortality rates, which were 24.6%, 24.4%, and 28.4% lower, respectively, than those of health systems with low teamwork levels. Put differently, initiatives seeking to foster physician teamwork in health systems with low to moderate levels at baseline have the potential to reduce the number of ED visits, readmissions, and deaths following CABG by 71.4, 53.7, and 16.8 per 1,000 discharges each year, respectively. These findings were robust across sensitivity analyses (Table 3 and the Supplementary Table).
Table 3.
Regression Results—CABG 60-Day Mortality.
| Mortality | |||||
|---|---|---|---|---|---|
| Main Model | 30-Day Window | 90-Day Window | Emergent Surgery | Survival >3 Days | |
| Patient variables | |||||
| Proportion of patients from outside the CBSA | 0.05 (0.09) | 0.05 (0.10) | 0.11 (0.09) | 0.05 (0.09) | 0.05 (0.09) |
| Charlson score (mean) | 0.07+ (0.04) | 0.06 (0.04) | 0.07+ (0.04) | 0.07+ (0.04) | 0.07+ (0.04) |
| Proportion surviving >3 days post-surgery | 0.02 (0.33) | ||||
| Proportion requiring emergent surgery | -0.02 (0.08) | ||||
| Proportion living below federal poverty line (mean)† | −2.24*** (0.57) | −2.40*** (0.61) | −2.55*** (0.55) | −2.25*** (0.57) | −2.24*** (0.57) |
| Proportion with a bachelor’s degree (mean)† | −1.92*** (0.56) | −2.06*** (0.60) | −1.95*** (0.54) | −1.92*** (0.56) | −1.92*** (0.56) |
| Proportion living in a rural area (mean)† | 0.36** (0.13) | 0.49*** (0.14) | 0.31* (0.12) | 0.36** (0.13) | 0.36** (0.13) |
| Hospital variables | |||||
| Number of patients | 0.01*** (0.00) | 0.01*** (0.00) | 0.01*** (0.00) | 0.01*** (0.00) | 0.01*** (0.00) |
| Number of physicians | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) |
| Academic hospital | 0.02 (0.04) | 0.02 (0.04) | 0.02 (0.03) | 0.02 (0.04) | 0.02 (0.04) |
| Total resident population (in thousands, log) | −0.04 (0.04) | −0.03 (0.05) | −0.02 (0.04) | −0.04 (0.04) | −0.04 (0.04) |
| Total black population (in thousands, log) | 0.05* (0.02) | 0.04* (0.02) | 0.05** (0.02) | 0.05* (0.02) | 0.05* (0.02) |
| Total Hispanic population (in thousands, log) | −0.01 (0.02) | 0.00 (0.02) | −0.02 (0.02) | −0.01 (0.02) | −0.01 (0.02) |
| Acute care hospital beds per 1,000 residents | 0.00 (0.03) | 0.00 (0.04) | 0.01 (0.03) | 0.00 (0.03) | 0.00 (0.03) |
| PCPs per 100,000 residents | 0.00 (0.00) | 0.00 (0.00) | −0.00+ (0.00) | 0.00 (0.00) | 0.00 (0.00) |
| Medical specialists per 100,000 residents | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) |
| Surgeons per 100,000 residents | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) |
| Network variables | |||||
| Teamwork | −1.78*** (0.24) | −1.71*** (0.26) | −1.77*** (0.24) | −1.78*** (0.24) | −1.78*** (0.24) |
| Other variables | |||||
| Year = 2009 | −0.16*** (0.03) | −0.17*** (0.03) | −0.18*** (0.03) | −0.16*** (0.03) | −0.16*** (0.03) |
| Year = 2010 | −0.25*** (0.03) | −0.27*** (0.03) | −0.27*** (0.03) | −0.25*** (0.03) | −0.25*** (0.03) |
| Imputed | −2.14*** (0.41) | −1.89*** (0.41) | −2.24*** (0.41) | −2.14*** (0.41) | −2.14*** (0.41) |
| Constant | 3.24*** (0.46) | 3.43*** (0.55) | 3.15*** (0.44) | 3.25*** (0.46) | 3.24*** (0.46) |
| Observations (Hospitals X Year) | 3339.00 | 3339.00 | 3339.00 | 3339.00 | 3339.00 |
| Hospitals | 1141.00 | 1141.00 | 1141.00 | 1141.00 | 1141.00 |
| Log likelihood | −6524.3 | −9703 | −6814.4 | −6524.3 | −6524.3 |
Standard errors in parentheses
p<0.1,
p<0.05,
p<0.01,
p<0.001
Estimated using levels found in patients’ home zip codes
Abbreviations: CABG, coronary artery bypass grafting; CBSA, core-based statistical area; PCP, primary care physician
Figure 3.
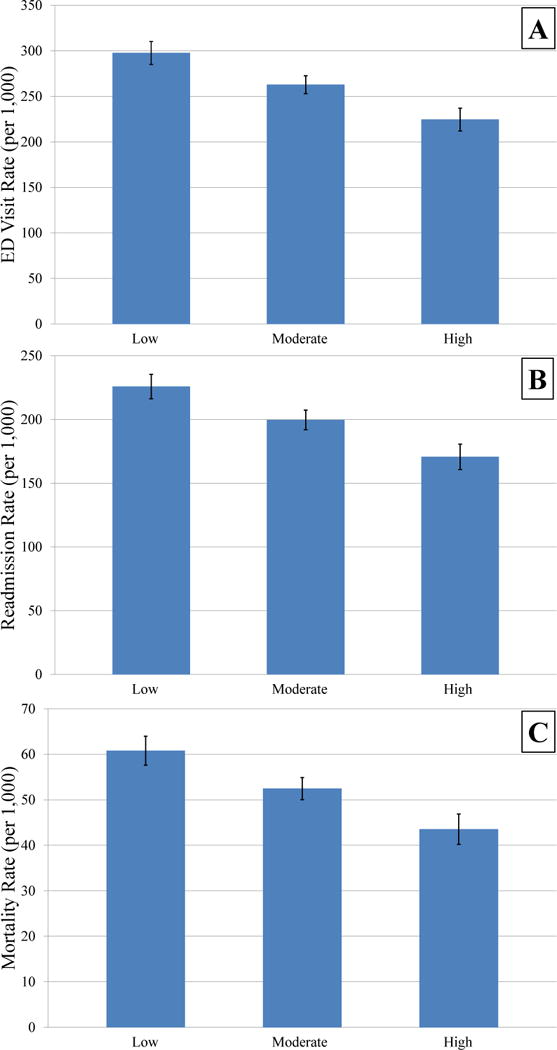
Adjusted rates (per 1,000) of readmission (A), ED visit (B), and mortality (C) stratified by the level of teamwork for CABG in a health system. All models were adjusted for potential hospital- (the number of CABG patients treated, the number of physicians providing care around the CABG episode, the proportion of CABG patients from outside the Core-Based Statistical Area, the hospital’s academic status) and HSA-level confounders (total resident population, total black population, total Hispanic population, proportion of residents living below federal poverty line, proportion of residents with a bachelor’s degree, proportion of residents living in a rural area, number of acute care hospital beds per 1,000 residents, number of PCPs per 100,000 residents, number of medical specialists per 100,000 residents, number of surgeons per 100,000 residents), as well as dummies for calendar year.
To understand the value of our teamwork measure on the model fit, we used a likelihood ratio test. The results from this test were significant for each outcome (readmissions: chi-square=74.24, P<0.001; ED visits: chi-square=77.47, P<0.001; mortality: chi-square=53.05, P<0.001), suggesting that adding the bipartite clustering coefficient to the model improved its fit. We also examined the substantive importance of the measure by comparing it to other variables that should have an important influence on surgical outcomes. For example, we found that a 25% increase in the average Charlson score at a hospital was associated with an increase of approximately one readmission per 1,000 CABG procedures. A similar 25% increase in the level of education in the community served by hospital (as indicated by the proportion of residents with a bachelor’s degree) is associated with a decrease in readmissions of approximately 21 per 1,000 CABG procedures. By comparison, a 25% increase in the bipartite clustering coefficient (our measure of teamwork) is associated with an approximate decrease in readmissions of 17 per 1,000 CABG procedures.
Discussion
In the Medicare population, we observed substantial variability in the level of physician teamwork (as measured by the bipartite clustering coefficient) around CABG across health systems. Those health systems with lower teamwork levels tended to be larger academic medical centers that received a higher proportion of surgical referrals from outside their immediate area. Health systems in which surgeons and nonsurgeons worked together in tightly knit groups during CABG episodes achieved lower 60-day ED visit, readmission, and mortality rates following the index hospitalization, even after adjusting for a variety of regional- and hospital-level factors. Taken together, the benefits of planned delivery system reforms focused on team building are likely to extend to surgical care.
To date, most studies examining the relationship between physician teamwork and clinical health outcomes have looked at the care of patients with chronic medical conditions.23,24 Although findings from these studies are, no doubt, important, their relevance to surgical patients, like those undergoing CABG, is unclear. Few would expect teamwork among physicians to have a measurable impact on operative complications, which are major drivers of health services utilization in the post-discharge period.25 However, major surgery like CABG can also exacerbate existing comorbidities and even cause new organ system complications, for which timely recognition and information exchange between the surgeon, medical consultants, and PCP may play an important role in reducing subsequent ED visits, readmissions, and even death. Our study lends support to this possibility.
Our study must be considered in the context of several limitations. First and foremost, the interactions between physicians that we identified were not directly observed but rather inferred through shared patients based on medical claims. As such, informal consultation without billing (i.e., curbsiding), which is common in academic centers where specialty fellows often provide after-hours care without in-person “staffing,” is not captured with our analysis. However, health services researchers are increasingly using sources of administrative data to construct physician social networks like the ones that we describe,26–28 and our approach has been validated in prior work. For example, to determine whether relationships ascertained from medical claims correspond with actual professional relationships, physicians affiliated with a large academic and community physicians’ organization were recently surveyed about their referral and advice relationships with physician colleagues.29 Relationships assessed by this survey were then compared with those identified by Medicare claims. Up to 82% of claims-based relationships were recognized by survey respondents, suggesting that administrative data can be used to predict the existence of meaningful relationships between physicians.
Second, while we adjusted for differences between hospitals and the healthcare markets that they served in our modeling approach, we must acknowledge the possibility of residual confounding. For instance, there are important technical issues around CABG procedures (e.g., small vessel caliber, the presence of aortic calcification, the degree of left ventricular dysfunction), which can affect post-surgical outcomes, but are not captured in medical claims. Insofar as omitted variables exist, our estimates on the effects of physician teamwork could be biased. However, given the observed effect size, any omitted variable would have to be highly correlated with both our exposure and outcomes to negate our findings, which is less likely.
We also acknowledge that some tightly-knit groups of physicians may care for a disproportionate share of remote referrals. Because of their willingness to support providers who are external to their natural networks, these groups could appear to have lower teamwork levels than they would otherwise. To account for this possibility, we controlled for the proportion of patient undergoing CABG in a health system from outside its Core-Based Statistical Area. While anesthesiologists who work in the intensive care setting can influence perioperative outcomes, we excluded them from our physician social networks because we cannot cleanly distinguish their care from that of those who deliver anesthesia services in the operating room. In addition, our analysis was based entirely on older Medicare beneficiaries undergoing CABG, and it is possible that a health system’s teamwork level differs for younger patients and those subjected to other cardiac procedures. That being said, the Centers for Medicare &Medicaid Services (CMS) are spearheading many of the planned reforms to bolster teamwork. Thus, our findings will be of interest to clinicians, hospital leaders, and policymakers regardless of their generalizability. Finally, as it is true with all observational studies, we cannot determine causality with these data, only association.
Limitations notwithstanding, our work has important policy implications. Under the current delivery system, physicians are responsible for only one aspect of a relevant set of medical decisions. Consequently, they may fail to see the full clinical picture for a given patient, lack the power to take all the appropriate actions given what they know, or even have affirmative incentives to shift costs onto others. To address this care fragmentation, policymakers have launched a variety of reforms that emphasize care coordination —most notably the patient-centered medical home, bundled payments, and ACOs.
At the core of these reforms are the social levers like shared accountability and collective incentives, the explicit intent of which is to encourage physicians to have stronger relationships with each other and build better social networks. The only way to understand the potential value of this approach is through network analysis. Along these lines, our study is one of the first to explore whether modifiable attributes of physician social networks that operate within health systems are associated with performance—and we are aware of only one other analysis in the specific setting of operative procedures.30 The implications of this are potentially powerful for cardiac surgery where the development of heart teams has helped in perioperative decision-making but may also be extended to the postoperative period.31
In summary, we observed that Medicare beneficiaries who underwent CABG in health systems where physicians worked together frequently had fewer postoperative ED visits, readmissions, and deaths. Our findings suggest that the way in which surgeons and nonsurgeons collaborate in their patients’ care could be manipulated in an effort to improve surgical outcomes. Indeed, programs being rolled out by CMS and other payers are already incorporating such “social innovations.32” Thus, further research is needed synthesizing both quantitative analyses (such as our own) of referral patterns and qualitative analyses of physician information-sharing in order to better understand the contexts that shape physician teams.
Supplementary Material
What is Known
Coronary artery bypass grafting (CABG) is a “team sport,” involving multiple physicians who work together before, during, and after surgery.
Frequent interactions between these physician teammates around shared patients may influence their collective performance.
What the Study Adds
In the Medicare population, substantial variability exists in the level of physician teamwork (as measured by the bipartite clustering coefficient) around CABG episodes across health systems.
Health systems in which surgeons and nonsurgeons work together in tightly knit groups during CABG episodes achieve lower emergency department visit, readmission, and mortality rates following the index hospitalization, even after adjusting for a variety of regional- and hospital-level factors.
Acknowledgments
Funding Sources: This study was funded, in part, by the Agency for Healthcare Research and Quality (grant 1K08HS020927-01A1; Dr. Hollingsworth).
Footnotes
Conflict of Interest Disclosures: None.
References
- 1.Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, Welch HG, Wennberg DE. Hospital volume and surgical mortality in the United States. New Engl J Med. 2002;346:1128–37. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 2.Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in Hospital Mortality Associated with Inpatient Surgery. New Engl J Med. 2009;361:1368–75. doi: 10.1056/NEJMsa0903048. [DOI] [PubMed] [Google Scholar]
- 3.Klein LW, Edwards FH, DeLong ER, Ritzenthaler L, Dangas GD, Weintraub WS. ASCERT: The American College of Cardiology Foundation-The Society of Thoracic Surgeons Collaboration on the Comparative Effectiveness of Revascularization Strategies. JACC-Cardiovasc Inte. 2010;3:124–6. doi: 10.1016/j.jcin.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Connor GT, Plume SK, Olmstead EM, Morton JR, Maloney CT, Nugent WC, Hernandez F, Jr, Clough R, Leavitt BJ, Coffin LH, Marrin CA, Wennberg D, Birkmeyer JD, Charlesworth DC, Malendka DJ, Quinton HB, Kasper JF. A regional intervention to improve the hospital mortality associated with coronary artery bypass graft surgery. JAMA. 1996;275:841–6. [PubMed] [Google Scholar]
- 5.Anderson B, Higgins L, Rozmus C. Critical pathways: Application to selected patient outcomes following coronary artery bypass graft. Appl Nurs Res. 1999;12:168–74. doi: 10.1016/s0897-1897(99)80213-4. [DOI] [PubMed] [Google Scholar]
- 6.Rumble SJ, Jernigan MH, Rudisill PT. Determining the effectiveness of critical pathways for coronary artery bypass graft patients: retrospective comparison of readmission rates. J Nurs Care Qual. 1996;11:34–40. doi: 10.1097/00001786-199612000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Shih T, Nicholas LH, Thumma JR, Birkmeyer JD, Dimick JB. Does Pay-for-Performance Improve Surgical Outcomes? An Evaluation of Phase 2 of the Premier Hospital Quality Incentive Demonstration. Ann Surg. 2014;259:677–81. doi: 10.1097/SLA.0000000000000425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jha AK, Joynt KE, Orav EJ, Epstein AM. The long-term effect of Premier Pay for Performance on patient outcomes. New Engl J Med. 2012;366:1606–15. doi: 10.1056/NEJMsa1112351. [DOI] [PubMed] [Google Scholar]
- 9.Bodenheimer T, Ghorob A, Willard-Grace R, Grumbach K. The 10 building blocks of high-performing primary care. Ann Fam Med. 2014;12:166–71. doi: 10.1370/afm.1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carrier E, Gourevitch MN, Shah NR. Medical homes challenges in translating theory into practice. Med Care. 2009;47:714–22. doi: 10.1097/MLR.0b013e3181a469b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pham HH, Schrag D, O’Malley AS, Wu B, Bach PB. Care patterns in Medicare and their implications for pay for performance. New Engl J Med. 2007;356:1130–9. doi: 10.1056/NEJMsa063979. [DOI] [PubMed] [Google Scholar]
- 12.Newman M. Networks: An Introduction. New York City: Oxford University Press Inc; 2010. [Google Scholar]
- 13.Robins G, Alexander M. Small worlds among interlocking directors: Network structure and distance in bipartite graphs. Comput Math Organ Theory. 2004;10:69–94. [Google Scholar]
- 14.Latapy M, Magnien C, Del Vecchio N. Basic notions for the analysis of large two-mode networks. Soc Networks. 2008;30:31–48. [Google Scholar]
- 15.Aldrich HE, Kim PH. Small Worlds, Infinite Possibilities? How Social Networks Affect Entrepreneurial Team Formation and Search. Strateg Entrep J. 2007;1:147–65. [Google Scholar]
- 16.Fewell JH, Armbruster D, Ingraham J, Petersen A, Waters JS. Basketball Teams as Strategic Networks. Plos One. 2012;7(11):1–9. doi: 10.1371/journal.pone.0047445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Uzzi B, Spiro J. Collaboration and creativity: The small world problem. Am J Sociol. 2005;111:447–504. [Google Scholar]
- 18.Margolis P, Halfon N. Innovation networks - A strategy to transform primary health care. JAMA. 2009;302:1461–2. doi: 10.1001/jama.2009.1428. [DOI] [PubMed] [Google Scholar]
- 19.Zappa P. The network structure of knowledge sharing among physicians. Qual Quant. 2011;45:1109–26. [Google Scholar]
- 20.The Darmouth Atlas of Health Care. at Available at: http://www.dartmouthatlas.org/ Accessed on December 3, 2015.
- 21.Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53:1258–67. doi: 10.1016/s0895-4356(00)00256-0. [DOI] [PubMed] [Google Scholar]
- 22.Kralovec PD, Mullner R. The American Hospital Association’s Annual Survey of Hospitals: Continuity and change. Health Serv Res. 1981;16:351–5. [PMC free article] [PubMed] [Google Scholar]
- 23.Casalino LP, Pesko MF, Ryan AM, Nyweide DJ, Iwashyna TJ, Sun X, Mendelsohn J, Moody J. Physician networks and ambulatory care-sensitive admissions. Med Care. 2015;53:534–41. doi: 10.1097/MLR.0000000000000365. [DOI] [PubMed] [Google Scholar]
- 24.Landon BE, Onnela JP, Keating NL, Barnett ML, Paul S, O’Malley AJ, Keegan T, Christakis NA. Using administrative data to identify naturally occurring networks of physicians. Med Care. 2013;51:715–21. doi: 10.1097/MLR.0b013e3182977991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Merkow RP, Ju MH, Chung JW, Hall BL, Cohen ME, Williams MV, Tsai TC, Ko CY, Bilimoria KY. Underlying reasons associated with hospital readmission following surgery in the United States. JAMA. 2015;313:483–95. doi: 10.1001/jama.2014.18614. [DOI] [PubMed] [Google Scholar]
- 26.Barnett ML, Christakis NA, O’Malley J, Onnela JP, Keating NL, Landon BE. Physician patient-sharing networks and the cost and intensity of care in US hospitals. Med Care. 2012;50:152–60. doi: 10.1097/MLR.0b013e31822dcef7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pollack CE, Weissman G, Bekelman J, Liao K, Armstrong K. Physician social networks and variation in prostate cancer treatment in three cities. Health Serv Res. 2012;47:380–403. doi: 10.1111/j.1475-6773.2011.01331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Landon BE, Keating NL, Barnett ML, Onnela JP, Paul S, O’Malley AJ, Keegan T, Christakis NA. Variation in patient-sharing networks of physicians across the United States. JAMA. 2012;308:265–73. doi: 10.1001/jama.2012.7615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barnett ML, Landon BE, O’Malley AJ, Keating NL, Christakis NA. Mapping physician networks with self-reported and administrative data. Health Serv Res. 2011;46:1592–609. doi: 10.1111/j.1475-6773.2011.01262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pollack CE, Wang H, Bekelman JE, Weissman G, Epstein AJ, Liao K, Dugoff EH, Armstrong K. Physician social networks and variation in rates of complications after radical prostatectomy. Value Health. 2014;17:611–8. doi: 10.1016/j.jval.2014.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Holmes DR, Rich JB, Zoghbi WA, Mack MJ. The heart team of cardiovascular care. J Am Coll Cardiol. 2013;61:903–7. doi: 10.1016/j.jacc.2012.08.1034. [DOI] [PubMed] [Google Scholar]
- 32.Lewis VA, Fisher ES. Social networks in health care - So much to learn. JAMA. 2012;308:294–6. doi: 10.1001/jama.2012.7476. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


