Abstract
A comparative in vivo pharmacokinetic (PK) study of tilmicosin (TIL) was conducted in 6 crossbred healthy pigs and 6 crossbred pigs infected with Haemophilus (H.) parasuis following oral administration of a single 40 mg/kg dose. The infected model was established by intranasal inoculation and confirmed by clinical signs, blood biochemistry, and microscopic examinations. Plasma TIL concentrations were determined by a validated high-performance liquid chromatography method with ultraviolet detection at 285 nm. PK parameters were calculated by using WinNonlin software. After TIL administration, the main PK parameters of TIL in healthy and H. parasuis-infected pigs were as follows: Area under the concentration-time curve, maximal drug concentration, half-life of the absorption phase, half-life of the distribution phase, and half-life of the elimination phase were 34.86 ± 9.69 vs. 28.73 ± 6.18 µg · h/mL, 1.77 ± 0.33 vs. 1.67 ± 0.28 µg/mL, 2.27 ± 0.45 vs. 2.24 ± 0.44 h, 5.35 ± 1.40 vs. 4.61 ± 0.35 h, and 43.53 ± 8.17 vs. 42.05 ± 9.36 h, respectively. These results of this exploratory study suggest that there were no significant differences between the PK profiles of TIL in the healthy and H. parasuis-infected pigs.
Keywords: Haemophilus parasuis, high pressure liquid chromatography, infected pigs, pharmacokinetics, tilmicosin
Introduction
Tilmicosin (TIL) is a semi-synthetic macrolide antibiotic widely used in veterinary medicine. It is a 16-member macrolide prepared by chemical modification of desmycosin [30]. The antimicrobial activity of TIL is reportedly better than that of tylosin [2]. TIL has a mechanism for inhibiting the protein synthesis of susceptible bacteria by combining simultaneously with the 50S subunits in the ribosome to block transpeptidation and/or mRNA displacement [12]. TIL preparations in previous reports include injection [8], food premix [19], and solid lipid nanoparticles [9]. Due to its antibacterial potency and pharmacokinetic (PK) features, TIL has the potential to become a valuable antibiotic in the treatment of pulmonary infectious diseases in the pig farming industry.
The efficacy of TIL is attributed to its low inhibitory concentration, broad antimicrobial spectrum, large distribution volume, long elimination half-life, and other pharmacodynamic characteristics [7,19]. The potent activities of TIL against Haemophilus (H.) parasuis isolated from pigs have been reported by several groups. A study by Zhang et al. [30] has showed that 100% of H. parasuis wild-type isolates were covered when the epidemiologic cutoff value was 16 µg/mL. For 97 isolates of H. parasuis cultured from Australian pigs, the minimal inhibitory concentration (MIC) was between 1 and 4 µg/mL, and the MIC50 and MIC90 were 2 and 4 µg/mL, respectively [5]. For 52 H. parasuis isolates from pigs in Denmark, the MIC of 49 strains was 2 µg/mL, but 4 µg/mL for the remaining 3 strains [1]. For 110 Chinese clinical H. parasuis isolates, the MIC50 and MIC90 were 1 and 2 µg/mL [31]. DeRosa et al. [6] also reported that the TIL MIC90 was ≤ 0.125 µg/mL for H. parasuis isolates that were collected by Colorado Animal Research Enterprises from swine diagnosed with clinical disease.
Understanding and employing PK principles can increase the probability of therapeutic success and reduce the occurrence of adverse drug effects in the body. The PK features of TIL have already been studied in many species, including broiler chickens [23], equine [4], swine [25], goats [22], and rats [18]; however, PK investigations of TIL in infected animals are quite few. The PK profiles of a drug can be influenced by the pathophysiological changes during an infection, and PK parameters in infected animals are more close to the clinical conditions [15,24]. As previously reported, physiological and biochemical differences such as body temperature, plasma protein binding ratio, blood pressure, anemia, and liver function in healthy and diseased animals can result in changes to a drug's PK profile and parameters [28]. Thus, the purpose of this study was to describe TIL kinetics in both healthy and infected pigs. To that end, we compared TIL PK profiles and parameters between healthy and infected crossbred pigs.
Materials and Methods
Materials
Nicotinamide adenine dinucleotide (NAD) and fetal calf serum were obtained from Guangzhou Ruite Biological Technology (China). Tryptic soy broth (TSB) and tryptose soya agar (TSA) were bought from Qingdao Hope Bio-Technology (China). TIL was obtained from Zhejiang Guobang Pharmaceutical Factory (China). Ammonium formate and formic acid were purchased from Aladdin Biological Engineering Technology & Services (China). Acetonitrile (liquid chromatography grade) was provided by TEDIA (USA). The water for high pressure liquid chromatography (HPLC) was prepared with a Milli-Q system (Millipore, USA). Other chemicals and reagents not specified in the text were of analytical grade or equivalent.
Animals
Sixteen healthy castrated crossbred (Duroc × Large White × Landrace) pigs with initial live weight of 16 ± 2 kg, 5 weeks of age, and of equal sex were purchased from the experimental station of Tarim University (Xinjiang, China). Six pigs (healthy group) were utilized for determination of healthy PK profiles and 6 pigs (infected group) were used to investigate infected PK profiles. By recording clinical signs of another 4 pigs (1 infected pig and 1 healthy pig for microscopic examination; 2 more healthy pigs were used as negative controls) we validated the disease model. Before the experiment, all pigs were housed in laboratory animal rooms of Tarim University's Animal Teaching Hospital for one week to acclimatize. During the acclimatization periods, the pigs were kept on basal feed twice daily with water available ad libitum around the clock without drugs and contaminants. The environmental temperature and relative humidity were maintained at 15℃–20℃ and 80%–90%, respectively. After final sampling, all pigs were immediately euthanized. All experimental protocols concerning the handling of pigs were in accordance with the requirements of the experimental animal ethics guidelines of the Ethics Committee at Animal Science Academy of Xinjiang Uygur Autonomous Region. All efforts were made to minimize the suffering of the animals.
Experimental model for H. parasuis-induced disease
Challenge strain
H. parasuis (serotype 5) was donated from the Key Laboratory of Tarim Animal Husbandry Science and Technology of Xinjiang Production & Construction Corps and identified by performing polymerase chain reaction (PCR) assessment before being used in the present study. To minimize the effects of in vitro procedures on virulence, the isolate was passaged twice in vitro and stored at −70℃.
Challenge preparation
H. parasuis were streaked from glycerol-frozen stocks onto TSA (containing 5% fetal calf serum and 10 µg/mL NAD) plates and incubated at 37℃ for 48 h in an atmosphere containing 5% CO2. A single bacterial colony from the fresh plates was inoculated in TSB (containing 5% fetal calf plasma and 10 µg/mL NAD) and grown at 37℃ in a shaking incubator at 773.5 × g to the logarithmic growth phase [20]. Just prior to the inoculation of pigs, the amplified bacteria were diluted with sterile phosphate-buffered saline (PBS; 0.1 M, pH = 7.4, prewarmed to 37℃) to 3–5 mL containing approximately 2 × 109 CFU/mL (CFU, colony-forming unit) for use as the final bacterial inoculum.
Experimental design
In this experiment, the pigs were inoculated intranasally to obtain 6 experimental models for H parasuis-induced disease [27]. Healthy pigs and infected pigs were housed separately in isolation rooms. Seven healthy pigs were inoculated with 3–5 mL of the challenge inoculum in each nostril to provide a total inoculum dose of approximately 2 × 109 CFU/mL. Three healthy pigs were inoculated with 5 mL of sterile PBS in each nostril. Clinical signs including appetite, walk willing, breathing, and psychiatric status were monitored and rectal temperatures were obtained and recorded three times daily. Gross lesions were recorded and samples were obtained for bacterial isolation and microscopic examination [29] to monitor the pneumonic lung. In addition, blood samples (2 mL) taken from the anterior vena cava were collected from pigs immediately prior to inoculation and 72 h post-inoculation. Samples were analyzed with a semiautomatic biochemical analyzer (UV-VIS2; bioMérieux, France) to monitor liver and renal functions [16].
Microscopic examination
Histopathological changes in lung were observed by optical microscope (BX41, Olympus, Japan) to validate the disease model. One pig from the healthy group and 1 pig from the infected group were euthanized at 72 h post-inoculation to collect lung secretions and tissues. Samples were fixed in 10% neutral-buffered formalin, embedded in paraffin, sectioned at 5 µm, and stained with hematoxylin and eosin (H&E).
PK study
Clinical signs and rectal temperatures were recorded immediately prior to inoculation and at 36 h after the inoculation. Both healthy and infected groups were administrated TIL (suspended in a 5% sodium carboxymethylcellulose solution) by oral gavage in a single 40 mg/kg dose. This dose was based on the clinical outcome from a 400 mg/kg feed (about 40 mg/kg body weight) treatment of H. parasuis in pigs [17]. At different times (0, 0.5, 0.75, 1, 2, 3, 4, 6, 8, 12, 24, 36, 48, 72, and 96 h) after TIL administration, blood samples (2 mL) were taken from anterior vena cava. The TIL levels in the plasma were determined by performing HPLC. The plasma drug concentration and time data were analyzed based on non-compartmental PKs by using WinNonlin software (ver. 5.2.1; Pharsight, USA).
HPLC assay
TIL was quantified by using a Waters 2695 series HPLC and a Waters 2587 UV detector set at a wavelength of 285 nm (Waters, USA). Chromatographic separation was achieved with an analytical ZORBAX SB C18 column (250 mm × 4.6 mm, inside diameter 5 µm; Agilent Technology, USA) at room temperature. The mobile phase consisted of 5 mM ammonium formate with added 0.1% formic acid (phase A) and acetonitrile (phase B) (73:27, v/v). The flow rate and injection volume of the drugs was 1 mL/min and 20 µL, respectively.
The TIL in pig plasma was extracted by mixing 0.5 mL plasma with 2.5 mL dichloromethane twice under oscillation conditions for 5 min to allow complete mixing and was followed by centrifugation (SiGMA 3K15; Sigma, Germany) at 46,412 × g for 10 min. After centrifugation, the supernatant was evaporated and resuspended in 0.5 mL of the mobile phase, and 20 µL was taken for HPLC analysis after filtration through a 0.22 µm polyvinylidene difluoride filter (Chucheng, China). The plasma TIL concentration was linear over the range of 0.02 –10 µg/mL with a correlation coefficient of 0.999. The limit of quantification (LOQ) was 0.05 µg/mL and the intra-day variation for the three different plasma concentrations (0.02, 0.5 and 5 µg/mL) were 2.37%, 2.89%, and 3.45%, respectively, while inter-day variation were 1.62%, 2.11%, and 2.39%, respectively. Recoveries from plasma for the three TIL concentrations (0.02, 0.5 and 5 µg/mL) were 93.25%, 95.33% and 97.65%, respectively.
Statistical analysis
GraphPad Prism 5.0 software (GraphPad Software, USA) was used to perform the statistical analyses, including data processing and graphical representations. In each case, a two-tailed t-test was used to assess the significance of differences in PK parameter values between the healthy and infected pigs. A p value of 0.05 was regarded as significant.
Results
Macro characteristics of inoculated pigs
The pigs from the inoculation group did not exhibit any significant clinical consequences or elevations in rectal temperatures at 12 h post-inoculation. Thereafter, the inoculated pigs successively manifested prospective signs, including reduction of movement, diminished appetite, crouching posture, dyspnea, and cough. At approximately 16 h post-inoculation, they were slightly lethargic and had mildly elevated rectal temperature. At 36 h after inoculation, a significantly elevated rectal temperature (average, 41.8℃; p < 0.05 when compared with normal rectal temperature) was detected. When forced to move they were non-weight bearing on one limb. Additional clinical observations included mucopurulent nasal discharge, swollen joints, and lateral recumbency prior to 48 h post-inoculation. In contrast, all control pigs remained clinically normal throughout the experiment. After euthanasia at 72 h post-inoculation, necropsy revealed inflammation on the pleural surface of the lung and peritoneal surfaces of the liver, spleen, and small intestine.
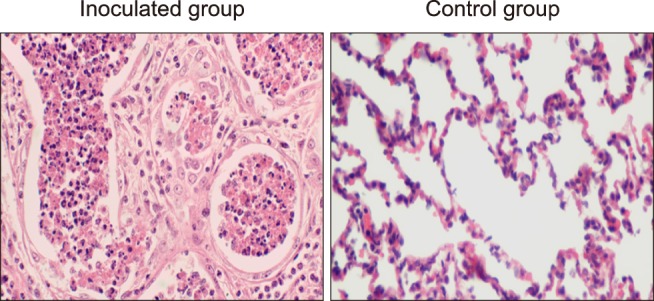
Micro characteristics of inoculated pigs
Microscopic lesions in the lung were investigated in the inoculated and control pigs at 48 h post-inoculation. Histopathologic alterations in the lung of infected pig mainly included swelling, degeneration, necrosis, and obscure lobular boundaries. As shown in Fig. 1, scattered interlobular septa were distended by serous exudate; as well, there were moderate numbers of neutrophils, exfoliated epithelial cells, and macrophages, and interlobular lymphatics were dilated and contained scant eosinophilic material. Moreover, there were focally extensive areas in which alveolar lumens contained variable numbers of neutrophils and macrophages, and there were scant amounts of fibrin in adjacent lobules. Within these areas, alveolar septal capillaries were congested, and occasional bronchioles contained low numbers of neutrophils. In contrast, no observable pathological changes were found in lung tissues of control pigs.
Fig. 1. Histopathological image of pig lung at 48 h after intranasal inoculation with Haemophilus parasuis (left) or sterilized saline (right). H&E stain. 400×.
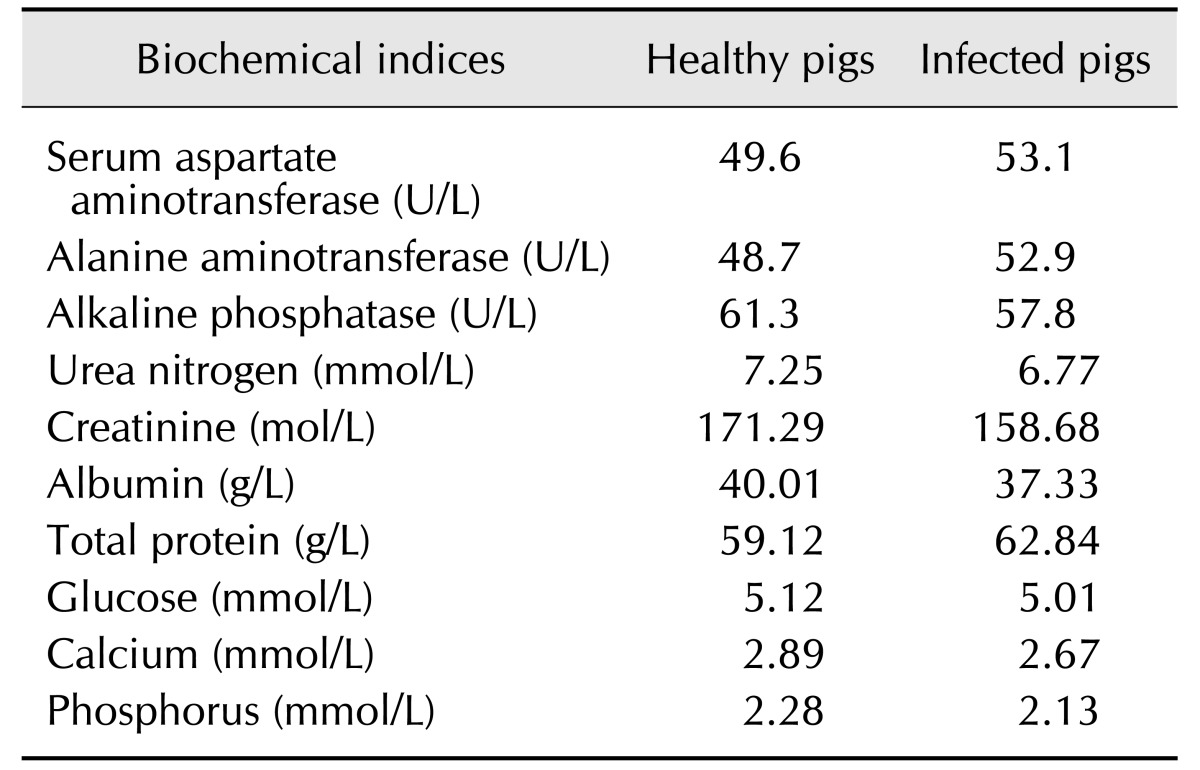
Serum or blood biochemical analysis
As shown in Table 1, the concentrations of alkaline phosphatase, urea nitrogen, creatinine, glucose, calcium, phosphorus, and albumin in plasma were lower in inoculated pigs that in healthy pigs. In contrast, the levels of total protein, plasma aspartate aminotransferase, and alanine aminotransferase had increased. Regardless, the serum/blood biochemical statistical analysis did not detect significant differences in serum or blood characteristics between healthy and infected pigs (two-tailed t-test, p > 0.05).
Table 1. Differences in biochemical indices in serum or blood between healthy pigs and Haemophilus parasuis-infected pigs.
No significant differences detected between healthy and infected groups (two-tailed t-test, p > 0.05).
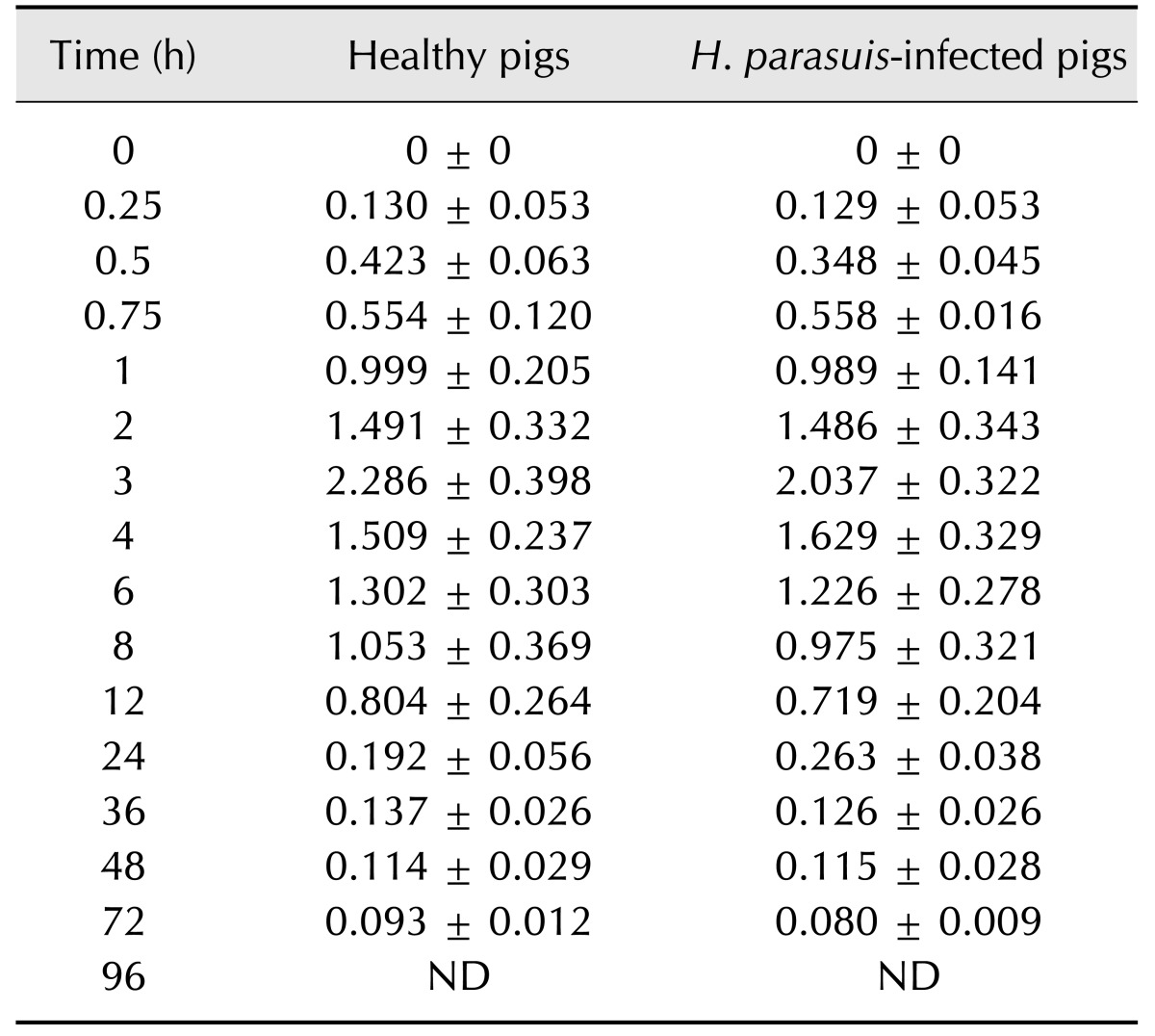
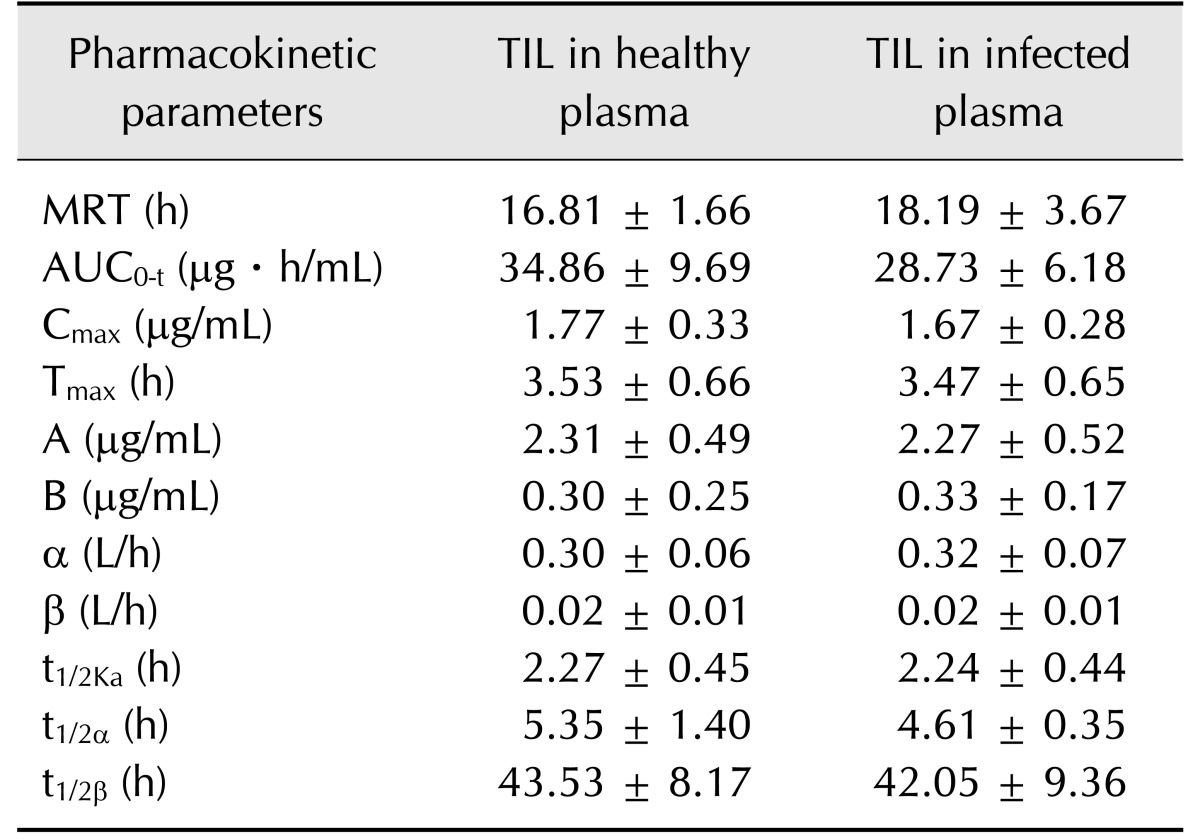
PKs
Blood samples obtained at all post-treatment times were analyzed. Based on a quantification limit of 0.05 µg/mL, the plasma drug concentration-time profiles of TIL following oral administration of a single dose of 40 mg/kg in healthy pigs and pigs infected with H. parasuis are illustrated in Table 2 and Fig. 2. The TIL in healthy pig plasma swiftly reached a peak concentration of 1.77 ± 0.33 µg/mL at 3.53 ± 0.66 h postadministration, after which the concentration decreased slowly and became sustained at 0.093 ± 0.012 µg/mL for 72 h, based on a quantification limit of 0.05 µg/mL. The TIL in plasma of infected pigs reached a peak concentration of 1.67 ± 0.28 µg/mL at 3.47 ± 0.65 h post-administration and then declined to below the detectable limit at 72 h post-administration. The main PK parameters of TIL in healthy pigs and infected pigs are summarized in Table 3. There were no statistically significant differences detected among the PK parameter values between healthy and infected pigs.
Table 2. Concentrations (mg/mL) of tilmicosin in serum at various times following oral administration of a single dose of 40 mg/kg body weight in healthy and Haemophilus parasuis-infected pigs.
Values presented are means ± SD (n = 6). ND, not determined.
Fig. 2. Semi-logarithmic plot of tilmicosin (TIL) concentration following oral administration of a single dose of 40 mg/kg body weight in healthy pigs and pigs infected with Haemophilus parasuis. Drugs concentrations are presented as means ± SD (n = 6).
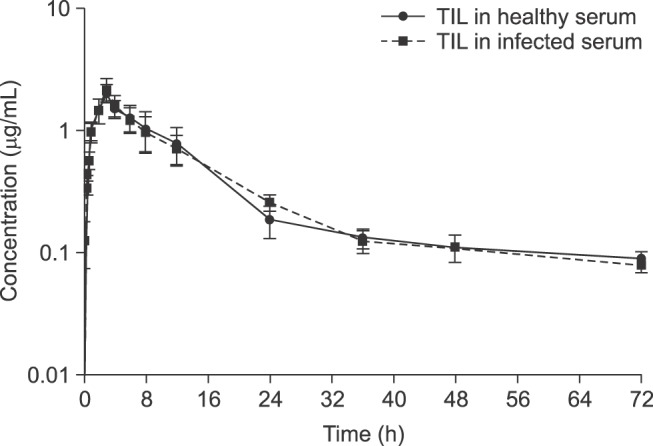
Table 3. Pharmacokinetic parameters of tilmicosin (TIL) in plasma following oral administration of a single dose of 40 mg/kg body weight in healthy and Haemophilus parasuis-infected pigs.
Values presented are means ± SD (n = 6). No significant differences between healthy and infected groups (two-tailed t-test, p > 0.05). MRT, mean residence time; AUC0-t, area under the concentration-time curve; Cmax, maximal drug concentration; Tmax, time to reach Cmax A, intercept for the distribution phase; B, intercept for the elimination phase; α, distribution rate constant (the distribution phase represents the drug being distributed out of a deep compartment into the blood); β, Elimination rate constant; t1/2Ka, half-life of the absorption phase; t1/2α, half-life of the distribution phase; t1/2β, half-life of the elimination phase.
Discussion
H. parasuis is a Gram-negative, opportunistic pathogen of pig, and it is one of the main causes of porcine respiratory disease complex in the world and is responsible for cases of fibrinous polyserositis, arthritis, dyspnea, and intense heat stress in young pigs [10]. Incidences of H. parasuis infection have reached 10% to 15% and mortality rates due to H. parasuis can be as high as 10% [21], which results in great economic loss in industrial intensive pig breeding around the world [14,30]. TIL has been widely used as a medicated premix for control of H. parasuis; however, there are only rare cases reporting PK parameters related to TIL in livestock and poultry, and no PK data have been reported related to TIL in pigs with pathogenic organisms and respiratory tract infections. Previous research has shown that the drug PK parameters in infected animals are more close to the clinical conditions and the results of that research has been helpful in designing and optimizing dosage regimens [3,24]. Moreover, it has provided reference data for use in the formulation of new dosage preparations for poorly soluble drugs such as TIL. Therefore, the current study on the PK features of TIL in both healthy pigs and in pigs experimentally infected with H. parasuis has practical value.
In this study, 5-week-old castrated crossbred (Duroc × Large white × Landrace) pigs were inoculated intranasally with an inoculum containing 2 × 109 CFU of H. parasuis to establish an experimental model of H. parasuis-induced disease. The in vivo challenge method was supported by previous study into experimental reproduction of H. parasuis infection in pig; study that included clinical, bacteriological, and morphological results [27]. In the present study, following H. parasuis inoculation, the pigs manifested typical symptoms of bacterial pneumonia, including reduction of movement, diminished appetite, crouching posture, dyspnea, and cough, and those signs were very consistent with clinically observed symptoms. In contrast, all control pigs remained clinically normal throughout the experiment. In addition, microscopic lesions observed in microphotographs confirmed that an experimental model of H. parasuis-induced disease was successfully established. However, the biochemical indices in the blood of healthy and infected pigs did not show significant differences. The similarity in test values may be explained by considering that blood biochemical indices in the body are dynamically balanced, whether the pigs were infected by H. parasuis or not. This suggestion is consistent with the results of a study into PKs related to florfenicol treatment in pigs experimentally infected with Actinobacillus pleuropneumoniae [16] and another showing the PK-modulated effects of Spirulina platensis against TIL-induced cardiotoxicity in mice [11].
The PK results obtained in this study indicated that TIL plasma concentration versus time generated after a single oral administration of TIL were best fitted by a two-compartment open model. When administering TIL orally, the absorption and distribution phases occur simultaneously. In the distribution phase, TIL is distributed out of a deep compartment into the blood, where it is subsequently eliminated. The half-lives of the absorption phase of TIL in healthy pigs and in pigs experimentally infected with H. parasuis after oral administration of a single 40 mg/kg dose were 2.27 ± 0.45 h vs. 2.24 ± 0.44 h, while the half-lives of the distribution phase were 5.35 ± 1.40 h vs. 4.61 ± 0.35 h, those of the elimination phase were 43.53 ± 8.17 h vs. 42.05 ± 9.36 h, and the area under the concentration-time curve values were 34.86 ± 9.69 µg·h/mL vs. 28.73 ± 6.18 µg·h/mL, respectively. Those results indicate that TIL is quickly absorbed and slowly eliminated after oral administration in both healthy pigs and in pigs experimentally infected with H. parasuis; moreover, there were no significant differences in the PK profiles of TIL in plasma.
At present, TIL is widely used in the animal food industry for prophylactic and therapeutic purposes due to its antibacterial potency and PK features. However, there are few studies reporting on the PKs of TIL after oral administration to animals. Shen et al. [25] previously determined TIL concentrations in the plasma of swine after oral administration levels of 20 and 40 mg/kg. In that study, blood samples were obtained from a jugular vein immediately before and at 10, 20, and 30 min and 1, 2, 3, 4, 6, 8, 12, 24, 36, 48, 72, 96 and 120 h after TIL administration. In that study, the absorption half-lives were 1.49 ± 0.23 and 1.64 ± 0.40 h, the distribution half-lives were 2.96 ± 0.58 and 3.20 ± 0.76 h, elimination half-lives were 25.26 ± 8.25 and 20.69 ± 5.07 h, peak concentration were 1.19 ± 0.30 and 2.03 ± 0.28 µg/mL after oral administration of TIL base at doses of 20 and 40 mg/kg, respectively. Keles et al. [13] investigated the PK features and tissue concentration of TIL in fowl, after oral administration of a single dose of TIL (50 mg/kg), and the mean maximum concentration of TIL in the lungs was 6.2 times greater than that observed in plasma. The total systemic clearance (CL) was 1.33 L/h. In addition, TIL was eliminated more slowly from the lungs (mean half-life, 75.74 h) than from plasma (30.18 h) in fowl. Clark et al. [4] investigated the disposition of TIL in horse after subcutaneous administration of a single dose of 10 mg/kg. In that study, the TIL concentration reached a maximal drug concentration (Cmax) of approximately 0.20 µg/mL in the plasma of the horses, and the TIL concentration in plasma persisted, exhibiting a mean residence time (MRT) of 19 h. Maximum tissue residue concentrations of TIL measured in equine lung, kidney, liver, and muscle tissues were 2.78, 4.88, 1.40, and 0.88 µg/g, respectively. The MRT of TIL in those tissues was approximately 27 h.
In this investigation, the Cmax detected in infected plasma after oral administration of TIL at a single dose of 40 mg/kg was 1.67 ± 0.28 µg/mL, which was lower than the MIC for H. parasuis (approximately 2 µg/mL) isolated clinically from swine. Similar to those of other macrolide drugs, TIL has a long half-life and can result in high concentrations in swine lung tissue. A pulmonary PK study after oral administration of a single dose of 40 mg/kg TIL in 6 healthy pigs was conducted by Zhang et al. [30]. In that study, bronchoalveolar lavage was utilized for quantitation of pulmonary epithelial lining fluid (PELF) volume and a urea dilution method was used to determine the concentration of TIL in PELF. The values of Tmax and Cmax were 40.80 ± 6.57 h and 5.36 ± 0.74 µg/mL, and values were higher than 4 µg/mL from 6 h to 48 h post-treatment but showed a rapid decrease from 4.72 µg/mL at 48 h to 0.68 µg/mL at 96 h. However, it has been reported that when TIL was added to the ration of healthy pigs as a medicated premix dose of 200 mg/kg and given for 2, 4, 7, 10, and 14 days, the TIL concentrations in lung tissue ranged from 0.73 to 1.43 µg/mL [26], which are lower than the MIC for H. parasuis. There are no previous reports of pulmonary PK profiles of TIL in infected pigs, and the results of our study indicate that there was no significant difference between the PK profiles of infected and healthy pigs. Our results, together with those of Zhang et al. [30], indicate that the recommended dose of TIL for control of pneumonia attributable to H. parasuis in swine should be 20–40 mg/kg body weight given as a single treatment.
In conclusion, this study has elucidated the PKs of TIL in vivo in healthy pigs and in pigs experimentally infected with H. parasuis, and there were no significant differences between the PK profiles of the infected and healthy pigs. Since TIL is an antibiotic that is widely used clinically, the PKs in disease model reported in this study will be useful in further investigations such as the pharmacodynamics (PD) study, PK-PD study and so on.
Acknowledgments
This article was supported by the National Natural Science Foundation of China (31660729). Scientific and technical help from the staff in the laboratories of Key Laboratory of Tarim Animal Husbandry Science and Technology of Xinjiang Production & Construction Corps is gratefully acknowledged.
Footnotes
Conflict of Interest: The authors declare no conflicts of interest.
References
- 1.Aarestrup FM, Seyfarth AM, Angen Ø. Antimicrobial susceptibility of Haemophilus parasuis and Histophilus somni from pigs and cattle in Denmark. Vet Microbiol. 2004;101:143–146. doi: 10.1016/j.vetmic.2004.02.012. [DOI] [PubMed] [Google Scholar]
- 2.Ayling RD, Baker SE, Pleek ML, Simon AJ, Nicholas RAJ. Comparison of in vitro activity of danofloxacin, florfenicol, oxytetracycline, spectinomycin and tilmicosin against recent field isolates of Mycoplasma bovis. Vet Rec. 2000;146:745–747. doi: 10.1136/vr.146.26.745. [DOI] [PubMed] [Google Scholar]
- 3.Buxton ILO, Benet LZ. Pharmacokinetics: the dynamics of drug absorption, distribution, metabolism and elimination. In: Brunton LL, Chabner BA, Knollmannn BC, editors. Goodman & Giman's The Pharmacological Basis of Therapeutics. 12 ed. New York: McGraw-Hill; 2011. [Google Scholar]
- 4.Clark C, Dowling PM, Ross S, Woodbury M, Boison JO. Pharmacokinetics of tilmicosin in equine tissues and plasma. J Vet Pharmacol Ther. 2008;31:66–70. doi: 10.1111/j.1365-2885.2007.00909.x. [DOI] [PubMed] [Google Scholar]
- 5.Dayao DA, Kienzle M, Gibson JS, Blackall PJ, Turni C. Use of a proposed antimicrobial susceptibility testing method for Haemophilus parasuis . Vet Microbiol. 2014;172:586–589. doi: 10.1016/j.vetmic.2014.06.010. [DOI] [PubMed] [Google Scholar]
- 6.DeRosa DC, Veenhuizen MF, Bade DJ, Shryock TR. In vitro susceptibility of porcine respiratory pathogens to tilmicosin. J Vet Diagn Invest. 2000;12:541–546. doi: 10.1177/104063870001200608. [DOI] [PubMed] [Google Scholar]
- 7.Frank GH, Briggs RE, Loan RW, Purdy CW, Zehr ES. Effects of tilmicosin treatment on Pasteurella haemolytica organisms in nasal secretion specimens of calves with respiratory tract disease. Am J Vet Res. 2000;61:525–529. doi: 10.2460/ajvr.2000.61.525. [DOI] [PubMed] [Google Scholar]
- 8.Gorham PE, Carroll LH, McAskill JW, Watkins LE, Ose EE, Tonkinson LV, Merrill JK. Tilmicosin as a single injection treatment for respiratory disease of feedlot cattle. Can Vet J. 1990;31:826–829. [PMC free article] [PubMed] [Google Scholar]
- 9.Han C, Qi CM, Zhao BK, Cao J, Xie SY, Wang SL, Zhou WZ. Hydrogenated castor oil nanoparticles as carriers for the subcutaneous administration of tilmicosin: in vitro and in vivo studies. J Vet Pharmacol Ther. 2009;32:116–123. doi: 10.1111/j.1365-2885.2008.01009.x. [DOI] [PubMed] [Google Scholar]
- 10.Hansen MS, Pors SE, Jensen HE, Bille-Hansen V, Bisgaard M, Flachs EM, Nielsen OL. An investigation of the pathology and pathogens associated with porcine respiratory disease complex in Denmark. J Comp Pathol. 2010;143:120–131. doi: 10.1016/j.jcpa.2010.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ibrahim AE, Abdel-Daim MM. Modulating effects of Spirulina platensis against tilmicosin-induced cardiotoxicity in mice. Cell J. 2015;17:137–144. doi: 10.22074/cellj.2015.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kang S, Li Z, Yin Z, Jia R, Song X, Li L, Chen Z, Peng L, Qu J, Hu Z, Lai X, Wang G, Liang X, He C, Yin L. The antibacterial mechanism of berberine against Actinobacillus pleuropneumoniae. Nat Prod Res. 2015;29:2203–2206. doi: 10.1080/14786419.2014.1001388. [DOI] [PubMed] [Google Scholar]
- 13.Keleş O, Bakirel T, Şener S, Baktir G, Daǧoǧlu G, Özkan O. [Pharmacokinetics and tissue levels of tilmicosin in fowls] Turk J Vet Anim Sci. 2001;25:629–634. Turkish. [Google Scholar]
- 14.Li X, Xie S, Pan Y, Qu W, Tao Y, Chen D, Huang L, Liu Z, Wang Y, Yuan Z. Preparation, characterization and pharmacokinetics of doxycycline hydrochloride and florfenicol polyvinylpyrroliddone microparticle entrapped with hydroxypropyl-β-cyclodextrin inclusion complexes suspension. Colloids Surf B Biointerfaces. 2016;141:634–642. doi: 10.1016/j.colsurfb.2016.02.027. [DOI] [PubMed] [Google Scholar]
- 15.Lindecrona RH, Friis C, Nielsen JP. Pharmacokinetics and penetration of danofloxacin into the gastrointestinal tract in healthy and in Salmonella typhimurium infected pigs. Res Vet Sci. 2000;68:211–216. doi: 10.1053/rvsc.1999.0361. [DOI] [PubMed] [Google Scholar]
- 16.Liu J, Fung KF, Chen Z, Zeng Z, Zhang J. Pharmacokinetics of florfenicol in healthy pigs and in pigs experimentally infected with Actinobacillus pleuropneumoniae. Antimicrob Agents Chemother. 2003;47:820–823. doi: 10.1128/AAC.47.2.820-823.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.MacInnes JI, Paradis MA, Vessie GH, Slavic L, Watson S, Wilson JB, Aramini JJ, Dick CP. Efficacy of prophylactic tilmicosin in the control of experimentally induced Haemophilus parasuis infection in pigs. J Swine Health Prod. 2003;11:174–180. [Google Scholar]
- 18.Modric S, Webb AI, Davidson M. Effect of respiratory tract disease on pharmacokinetics of tilmicosin in rats. Lab Anim Sci. 1999;49:248–253. [PubMed] [Google Scholar]
- 19.Naccari F, Giofrè F, Pellegrino M, Calò M, Licata P, Carli S. Effectiveness and kinetic behaviour of tilmicosin in the treatment of respiratory infections in sheep. Vet Rec. 2001;148:773–776. doi: 10.1136/vr.148.25.773. [DOI] [PubMed] [Google Scholar]
- 20.Oliveira S, Blackall PJ, Pijoan C. Characterization of the diversity of Haemophilus parasuis field isolates by use of serotyping and genotyping. Am J Vet Res. 2003;64:435–442. doi: 10.2460/ajvr.2003.64.435. [DOI] [PubMed] [Google Scholar]
- 21.Oliveira S, Pijoan C, Morrison R. Evaluation of Haemophilus parasuis control in the nursery using vaccination and controlled exposure. J Swine Health Prod. 2004;12:123–128. [Google Scholar]
- 22.Ramadan A. Pharmacokinetics of tilmicosin in serum and milk of goats. Res Vet Sci. 1997;62:48–50. doi: 10.1016/s0034-5288(97)90179-x. [DOI] [PubMed] [Google Scholar]
- 23.Rassouli A, Al-Qushawi A, Atyabi F, Peighambari SM, Esfandyari-Manesh M, Shams GR. Pharmacokinetics and bioavailability of three promising tilmicosin-loaded lipid nanoparticles in comparison with tilmicosin phosphate following oral administration in broiler chickens. Turk J Vet Anim Sci. 2016;40:540–547. [Google Scholar]
- 24.Sang K, Hao H, Huang L, Wang X, Yuan Z. Pharmacokinetic-pharmacodynamic modeling of enrofloxacin against Escherichia coli in broilers. Front Vet Sci. 2015;2:80. doi: 10.3389/fvets.2015.00080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shen J, Li C, Jiang H, Zhang S, Guo P, Ding S, Li X. Pharmacokinetics of tilmicosin after oral administration in swine. Am J Vet Res. 2005;66:1071–1074. doi: 10.2460/ajvr.2005.66.1071. [DOI] [PubMed] [Google Scholar]
- 26.Thompson T, Darby J, Moran J, Tonkinson L, Blais J, Chamberlain S. Proceedings of the 6th International Congress of the European Association for Veterinary Pharmacology and Therapeutics; 7-11 August 1994; Edinburgh, UK. [Google Scholar]
- 27.Vahle JL, Haynes JS, Andrews JJ. Experimental reproduction of Haemophilus parasuis infection in swine: clinical, bacteriological, and morphologic findings. J Vet Diagn Invest. 1995;7:476–480. doi: 10.1177/104063879500700409. [DOI] [PubMed] [Google Scholar]
- 28.van Miert A. Influence of febrile disease on the pharmacokinetics of veterinary drugs. Annal Vet Res. 1990;21(Suppl 1):11S–28S. [PubMed] [Google Scholar]
- 29.Wang C, Zhao M, Liu YR, Luan X, Guan YY, Lu Q, Yu DH, Bai F, Chen HZ, Fang C. Suppression of colorectal cancer subcutaneous xenograft and experimental lung metastasis using nanoparticle-mediated drug delivery to tumor neovasculature. Biomaterials. 2014;35:1215–1226. doi: 10.1016/j.biomaterials.2013.08.091. [DOI] [PubMed] [Google Scholar]
- 30.Zhang P, Hao H, Li J, Ahmad I, Cheng G, Chen D, Tao Y, Huang L, Wang Y, Dai M. The epidemiologic and pharmacodynamic cutoff values of tilmicosin against Haemophilus parasuis. Front Microbiol. 2016;7:385. doi: 10.3389/fmicb.2016.00385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhou X, Xu X, Zhao Y, Chen P, Xuan Z, Chen H, Cai X. Distribution of antimicrobial resistance among different serovars of Haemophilus parasuis isolates. Vet Microbiol. 2010;141:168–173. doi: 10.1016/j.vetmic.2009.05.012. [DOI] [PubMed] [Google Scholar]