Abstract
Respiratory diseases, especially asthma, are common in children. While spirometry contributes to asthma diagnosis and management in older children, it has a limited role in younger children whom are often unable to perform forced expiratory manoeuvre. The development of novel diagnostic methods which require minimal effort, such as forced oscillation technique (FOT) is, therefore, a welcome and promising addition. FOT involves applying external, small amplitude oscillations to the respiratory system during tidal breathing. Therefore, it requires minimal effort and cooperation. The FOT has the potential to facilitate asthma diagnosis and management in pre-school children by faciliting the objective measurement of baseline lung function and airway reactivity in children unable to successfully perform spirometry. Traditionally the use of FOT was limited to specialised centres. However, the availability of commercial equipment resulted in its use both in research and in clinical practice. In this article, we review the available literature on the use of FOT in childhood asthma. The technical aspects of FOT are described followed by a discussion of its practical aspects in the clinical field including the measurement of baseline lung function and associated reference ranges, bronchodilator responsiveness and bronchial hyper-responsiveness. We also highlight the difficulties and limitations that might be encountered and future research directions.
Keywords: Asthma, Forced oscillation technique, Impulse oscillatory, Pre-school, Children, Pulmonary function test
Core tip: Respiratory diseases, such as asthma, are especially common in children. Although their diagnosis and management are facilitated by using spirometry in older children, the use of the latter remains limited in younger children because of their inability to perform forced expiratory manoeuvre. Therefore, the use of new methods which require minimal effort and cooperation from children, such as the forced oscillation technique (FOT) is a welcome and promising addition to identify children with underlying airway function abnormalities. In this article, we review the available literature on the use of FOT in childhood asthma.
INTRODUCTION
Asthma is the most common chronic childhood disease worldwide[1]. It is often difficult to diagnose in infants and young children due to lack of objective measures, such as spirometry[2-4].
Spirometry is the gold standard method to assess lung function in older children and adults. However, obtaining acceptable and repeatable spirometry measures requires significant efforts and high level of cooperation[5-7]. Therefore, the diagnosis and management of childhood asthma remain suboptimal, in young children and older children who cannot perform an acceptable forced expiratory manoeuver.
One potential lung function method suitable for use in young children and older children unable to perform spirometry is the forced oscillation technique (FOT). The FOT was developed by DuBois et al[8] in 1956, to measure the mechanical behaviour of the respiratory system. Over the years, the FOT has been used in research and more recently in clinical practice[9-12]. The application of FOT has expanded to the point where commercial equipment are now widely available. Standardized approaches for the collection of FOT outcomes have been established by the European Respiratory Society (ERS) and the American Thoracic Society (ATS) in pre-school children[9].
One significant advantage of the FOT is its application during tidal breathing and the subsequent reduction in the level of active participation and cooperation required from the individual being tested. As a result, this technique can be feasibly used in children as young as two years of age[13]. Consequently, the FOT opens new frontiers in the application of objective measurements of respiratory function in young children and offers improvements in the diagnosis and management of asthma in young children.
In this review we have summarised the available literature on the use of FOT in childhood asthma. The technical aspects of FOT are briefly described followed by a discussion of its practical aspects in the clinical field, including the measurement of baseline lung function and associated reference ranges, bronchodilator responsiveness and bronchial hyper-responsiveness. We also highlight the difficulties and limitations that might be encountered and future research directions.
Technical aspects of FOT
The basic principle of FOT involves the application of external signals into the respiratory system and measuring the resulting response of that system[10]. This response is termed the respiratory system impedance (Zrs). The Zrs can be determined when flow and pressure are measured across a known frequency range at the airway opening and is represented as the resistance (Rrs) and reactance (Xrs) of the respiratory system
Zrs = Pao / V’ao = Rrs + j Xrs
where Pao is the pressure V’ao is the flow measured at the airway opening and j = √ (-1)
Resistance (Rrs) represents the component of Zrs that is a function of both Pao and V‘ao, equating to the resistive properties of the respiratory system. Reactance (Xrs) is the out-of-phase component that is a function of both Pao and volume, reflecting elatic recoil of the respiratory system. Both Rrs and Xrs are determined when oscillatory (sound waves) signals are applied at the airway opening (and hence to the whole respiratory system).
It is important to be aware that the respiratory impedance is frequency-dependent: (1) At low frequencies, (2-4 Hz) as the oscillations are transmitted more distally into the lungs, Rrs and Xrs tend to reflect the properties of the peripheral respiratory system; (2) at higher frequencies, (> 20 Hz) the Zrs reflects the resistive and inertive properties of the proximal conducting airways.
It is critical to note that Rrs and Xrs reflect mechanical properties of the entire respiratory system, including the airway, lung and chest wall[10]. It is therefore not possible to assign specific anatomical changes (for example central airway obstruction) to changes in any one FOT outcome at a specific frequency (see below for further details).
As the airway and the lung tissue are both flow and volume-dependant, the characteristic of the oscillatory signals used is important. These signals can take any of the following common forms: (1) Single frequency; (2) impulse oscillation system[14]; (3) pseudorandom noise (the simultaneous application of several frequency components).
The oscillation signal that is most commonly applied encompasses the medium frequency range, generally including frequencies between 2 Hz and 20 Hz. The advantage of using mid-range frequencies is that the oscillatory signals can be superimposed on the tidal breathing and therefore result in a broader application[10]. For more details reviews on the technical aspects of FOT, readers are directed to review (oscillation mechanics of respiratory system) by Bates et al[15].
Practical aspects of FOT
This section summaries the available equipment, feasibility, repeatability, and finally the collection and reporting of FOT data in young children.
Equipment
The availability of FOT commercial equipment has resulted in the increased uptake of FOT in clinical practice and especially in young children. The FOT equipment includes (Figure 1): (1) A loudspeaker or similar to generate the oscillatory signals; (2) a pneumotachograph and pressure transducers to measure pressure and flow; (3) a mouth piece containing a bacterial filter to prevent cross infection between patients. A typical arrangement of the forced oscillatory impedance measurement, adapted from[9].
Figure 1.
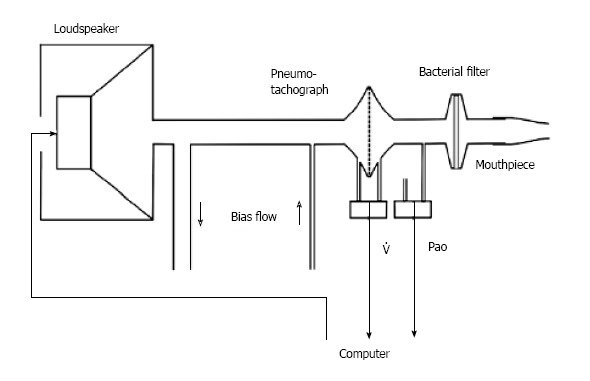
Typical arrangement of the forced oscillatory impedance measurement, adapted from. Pao: Input pressure at the airway opening; V’ao: Output flow.
Feasibility
The feasibility and success rates of FOT are, understandably, age-dependent. The success rate in children 4 years of age and older exceeds 80%[13,16,17], while it ranges from 83% to 100% in healthy children aged 2-7 year[13,18] and between 57% to 100% in children with asthma aged between 3 to 5 years[13,16]. In young children with acute asthma the success rate of FOT reduced to 24% and 65% in three and eight-year-old children respectively, However, it was higher than that of spirometry in the same population[12]. Furthermore, the feasibility of FOT measurements increases noticeably with practice in children.
The feasibility of FOT with challenge testing has been assessed in several research studies and has been shown to be feasible in young children using either inhaled adenosine monophosphate (AMP)[19], free running[20], methacholine[21-23], hypertonic saline[21], cold air[24] or mannitol challenge[25].
Collection of FOT data
For adequate collection of the data, the child should be seated with their back straight and their neck either in the neutral position or slightly extended. FOT is usually performed with the mouthpiece which incorporates a bacterial filter and a nose clip-on. A staff member or a parent needs to support the child’s cheeks as well as the floor of his mouth, as shown in Figure 2. An acquisition period should cover several breathing cycles, typically lasting 8-16 s. The results, computed as the mean value of the three to five acceptable measurements, also include the measurement of the coefficient of variation calculated from the standard deviation (SD) of the measurements. Acceptable measures are the one which have no artefacts such as leak, incomplete expiration, glottis closure, swallowing and the child obstructing the mouthpiece with their tongue are easily identified[9] (Figure 2).
Figure 2.
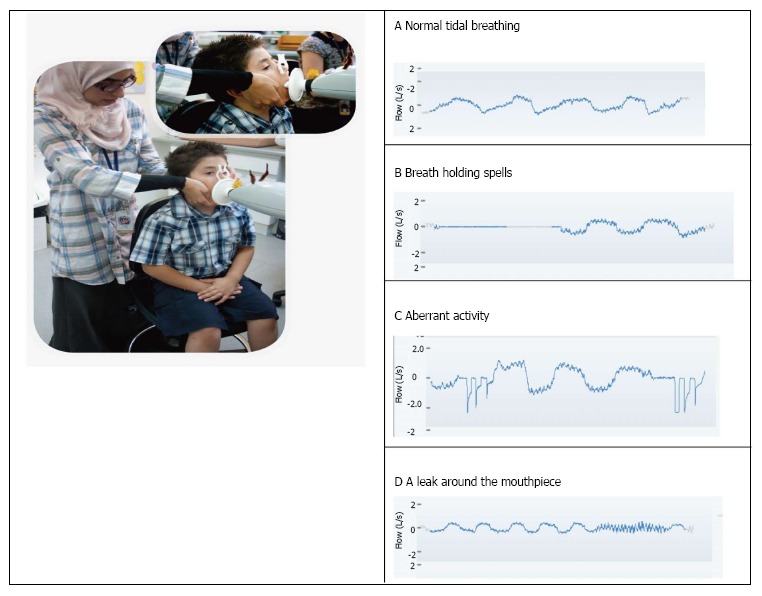
Demonstration of lung function measurements using FOT. On the left, a photograph of the FOT test being performed in a 5-year-old boy. The hands of the investigator support the cheeks and the floor of the mouth of the child. The nose is blocked using a nose clip. The lips are sealed around the mouthpiece. On the right, Different breathing patterns during FOT measurements are shown, as observed on the flow-time trace in L/s. A: Normal tidal breathing; B: Breath holding spells; C: An aberrant activity (e.g., coughing, swallowing, or noise); D: A leak around the mouthpiece. FOT: Forced oscillation technique.
Repeatability
Repeatability is an important issue when considering the role of a lung function measures. The short-term repeatability of FOT in heathy children has been assessed and it is summarized in Table 1 below. The long term (two weeks) and short term repeatability were both similar[19].
Table 1.
Fifteen minutes’ repeatability of Forced oscillation technique in healthy children
| Author | Year | n | Rrs | Xrs |
| Hall et al[13] | 2007 | 58; field | ~2 or ~ 30% | 1.2 - 1.7 |
| Malmberg et al[18] | 2002 | 19; placebo | 1.1 or ~ 12% | 1.3 |
| Klug et al[16] | 1998 | 120 | 2.6 or ~ 20% | 2 |
Rrs: Respiratory system resistance; Xrs: Respiratory system reactance) in hPa/s per L.
Reporting and interpreting FOT data
Commonly reported FOT outcomes include resistance (Rrs), reactance (Xrs) at different frequencies, resonance frequency (Fres), frequency dependence (Fdep), and the area under reactance curve (AX), as illustrated in Figure 3. The reported Rrs variable includes, in the same measurement, the Rrs of the airway, that of the chest wall, and that of the lung tissue. As airway Rrs dominates Rrs in the mid frequencies[26], it can be considered a surrogate of airway resistance[27,28]. As frequency decreases to below approximately 4 Hz Rrs will increasing include peripheral respiratory resistance and be reflective of the peripheral airways and the lung. As Xrs, on the other hand, is dominated by elastic properties of the respiratory tissue, reflecting the elastic and inertive properties of the respiratory system, it is negative at low frequencies. The point at which Xrs crosses the zero, representing the inertial properties of the larger airways[29], is called the Fres, which is the frequency at which elastive and inertive properties of the lung are balanced, and which becomes positive at higher frequencies[30]. The Fdep of that resistance is thought to reflect peripheral airway resistance[31], as, for example, in patients with obstructive airway diseases, it is generally higher than normal subjects due to the difference in airway resistance[30]. However, to date there are no studies directly confirming this.
Figure 3.
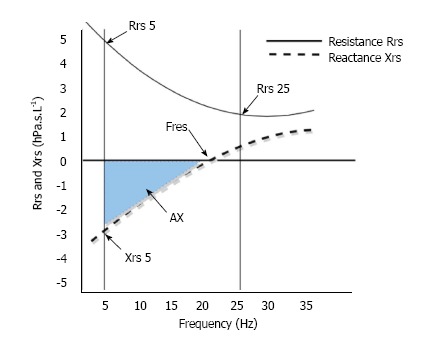
Changes in resistance (Rrs) and reactance (Xrs) as function of oscillation frequency.
The area under the reactance curve (AX) is the sum of the Xrs from a Xrs at 5 Hz until Fres (i.e., when Xrs is zero, as in Figure 3) [29]. Studies have shown that Xrs and AX are better representative of peripheral airway obstruction than Rrs[29] and that AX and Fres clearly distinguish healthy children from those with small airway disease and asthma[32].
The FOT outcomes alter with growth and therefore need to be reported as both absolute values and as a function of a predicted value. Expressing outcomes as z or SD scores is the most appropriate. Z scores allows the easy estimation of the lower limit of normal (being either -1.64 or -1.96) and avoids the diagnostic uncertainly that can arise when using percent predicted and a fixed cut off for the presence of abnormal lung function[33,34].
Reference range of FOT measurements
Numerous studies have reported reference data in healthy children using a variety of FOT outcomes[13,35-44]. The FOT outcomes are generally reported to change with age, height and gender. There is some variability due to the different ethnicity, gender, age, weight, height, equipment and the methodology used in those studies and it is important that users carefully review potential reference equations to match the populations, equipment and protocols used as closely as possible to their own circumstances[37,45]. Reporting and comparing the relevant z-scores for these measurements simplifies the interpretation as the possible confounders reported earlier have already been taken into consideration when calculating these scores. Table 2 below summarises those studies and shows those differences.
Table 2.
Populations of healthy children studied using forced oscillation technique since 2005, adopted and modified from
| Ref. | Year of publication | Ethnic group - Country of study | Subject number | Age in years | Height (cm) | Reported prediction equation variables |
| Frei et al[35] | 2005 | Caucasian - Canadian | 222 | 3-10 | 90-155 | Rrs at 5-35 Hz Xrs at 5-35 Hz Fres, AX |
| Dencker et al[36] | 2006 | Caucasian - Scandinavian | 360 | 2-11 | 90-162 | Rrs at 5-20 Hz Xrs at 5-20 Hz Fres |
| Amra et al[37] | 2008 | Asian - Iranian | 509 | 5-18 | 127-197 | Rrs at 5-25 Hz Xrs at 5-25 Hz |
| Nowowiejska et al[38] | 2008 | Caucasian - Polish | 626 | 3-18 | 95-193 | Rrs at 5-35 Hz Xrs at 5-35 Fres |
| Vu et al[39] | 2008 | Asian - Vietnamese | 175 | 6-11 | 111-154 | Rrs at 8 Hz Xrs at 8 Hz |
| Vu et al[40] | 2010 | Asian - Vietnamese | 95 | 6-11 | 111-134 | Rrs at 8 Hz Xrs at 8 Hz |
| Calogero et al[41] | 2010 | Italian | 163 | 2-6 | 101-114 | Rrs at 6-10 Hz Xrs at 6-10 Hz |
| Park et al[42] | 2011 | Korean | 133 | 3-6 | 95-121 | Rrs at 5, 10 Xrs at 5, 10 RF, AX |
| Calogero et al[43] | 2013 | Caucasian Italian and Australian | 760 | 2-13 | 90-160 | Rrs at 6, 8, 10 Hz Xrs at 6, 8, 10 Hz Fres, AX |
| Shackleton et al[44] | 2013 | Mexican | 584 | 3-5 | 87-119 | Rrs at 6 and 8 Hz Xrs at 6 and 8 Hz |
| Hagiwara et al[46] | 2014 | Japanese | 537 | 6-15 | 111-174 | Rrs at 5 and 20 Hz Rrs5-20 |
IOS: Impulse oscillation system; Rrs: Respiratory system resistance; Xrs: Respiratory system reactance) in hPa/s per L; Fres: Resonant frequency; RF: Resonant frequency; AX: Area under the Xrs curve from 5 Hz to Fres; MF: Multi-frequency system; Fdep: Frequency dependence of Rrs between 4–24 Hz; SF: Single frequency system.
Clinical applications of FOT in children with asthma
By incorporating measurements of bronchodilator Responsiveness (BDR) and bronchial hyper-responsiveness (BHR), the utility of FOT to assist in the diagnosis of asthma in young children may be increased[47]. The official ATS/ERS statement on pulmonary function testing in preschool children stated that FOT is a promising tool in diagnosing and following up children with asthma[9]. Other studies also suggest that the FOT may be useful in assessing asthma control, compliance to medication, and in the follow up of these young children[48].
Baseline FOT and the severity of asthma
In children aged 5 years and above, spirometry adequately assesses baseline lung function and the results correlate well with asthma severity[49]. When comparing spirometry and FOT in children older than 6 years of age, those with asthma have lower baseline FOT than with spirometry when compared to healthy children[50]. Whilst few studies have examined baseline airway obstruction in young children with asthma using FOT. Klug et al[51] reported that young children with stable asthma demonstrated impaired baseline lung function when assessed using FOT. Oostveen et al[17] showed that, when compared to healthy 4-year-old children, those children with persistent wheeze had worse baseline lung function than those with transient wheeze as assessed by FOT. Children with a history of recurrent wheeze and/or asthma recruited from clinics tend to have worse lung function expressed in FOT even when asymptomatic[18,52]. However, other studies conducted in children with history of wheeze and recruited from the community have similar FOT outcomes to healthy children[53,54]. The ability of FOT to determine asthma severity remains therefore questionable, especially in children on asthma medication[49]. Further studies are therefore needed to explore the relationship between baseline lung function using FOT and asthma severity in young children with asthma.
Bronchodilator response using FOT
The assessment of bronchodilator responsivess using FOT in young children with asthma has been encouraged in clinical practice[10]. Critical the the assessment of increased responsiveness associated with asthma is an understanding of the response of healthy children with bronchodilators. The assessment of change in FOT outcomes during the assessment of BDR has been expressed as absolute change or relative change from the baseline in the Rrs, Xrs and AX, the use of AX has been explored in a few studies and is shown to be a good outcome in assessing the BDR in children with asthma[17,29,32].
In the most recent study which assessed BDR in children (Calogero et al[43]), cut-offs for a positive BDR in healthy Caucasian children were defined as 34% and 50% for Rrs and Xrs, respectively expressed as a relative change from the baseline lung function. In a study looking at the uses of pseudorandom FOT signal (4–48 Hz) in quantifying BDR in healthy young children, children with cystic fibrosis, neonatal chronic lung disease and children with asthma and/or current wheeze, Thamrin et al[53] recommended a positive BD response of 40% and 65% for Rrs and Xrs, respectively expressed as a relative change from the baseline lung function[53]. Another study, conducted by Oostveen et al[17] in Belgium on 4 years old healthy and wheezy children (n = 325) using FOT, recommended a positive BDR at Rrs 4 of 43% expressed as absolute changes. Cut-off values for BDR in previous studies are summarized and listed in Table 3. In general, > 30% decrease in Rrs after bronchodilator is suggestive of asthma.
Table 3.
Reported bronchodilator responsiveness in young healthy and wheezy children using forced oscillation technique since 2005
| Ref. | Ethnic group age, yr | n | Variable | Dose | Waiting time (n) | Absolute BDR | Relative BDR, (%) |
| Thamrin et al[53], 2007 | Healthy Caucasian (3-7) | 78 | Rrs 6,8,10 Xrs 6,8,10 | Salbutamol 600 mg | 15 | Rrs 6 -35.0, -3.1 Rrs 8 -35.0, -4.4 Rrs 10 -32.3, -3.7 Xrs 6 -0.27, 1.66 Xrs 8 - 0.04, 1.82 Xrs 10 -0.00, 2.03 | Rrs 6: 42% Rrs 8: 37% Rrs 10: 39% Xrs 6: 61% Xrs 8: 67% Xrs 10: 63% |
| Thamrin et al[53], 2007 | Asthmatics Caucasian (3-7) | 57 | Rrs 6, 8, 10 Xrs 6, 8, 10 | Salbutamol 600 µg | 15 | Rrs 6 -37.0, 8.8 Rrs8 -33.1, 9.7 Rrs 10 -33.4, 4.5 Xrs 6 -0.21, 2.30 Xrs 8 -0.13, 2.47 Xrs 10 -0.12, 2.22 | Rrs 6: 42% Rrs 8: 37% Rrs 10: 39% Xrs 6: 61% Xrs 8: 67% Xrs 10: 63% |
| Lan Vu et al[39], 2008 | Healthy Vietnamese (6–11) | 175 | Rrs 8 Hz Xrs 8 Hz | Salbutamol 200 µg | 5 | Rrs 8 -11.8,13.4 Xrs 8 4.09, - 5.78 | Rrs 8: 38% Xrs 8: 16% |
| Lan Vu et al[40], 2010 | Asthmatic Vietnamese (6-10) | 103 | Rrs 8 Hz Xrs 8 Hz | Salbutamol 200 µg | 5 | -- | Rrs 8: 13% Xrs: 32% |
| Oostveen et al[55], 2010 | Asthmatic Belgian -4 | 313 | Rrs 4 | Salbutamol 200 µg | 15 | -- | Rrs 4: 22% AX: 15.77% |
| Calogero et al[41], 2010 | Healthy Italian (3-6) | 163 | Rrs 8 Xrs8 | Salbutamol 200 µg | 15 | -- | Rrs 8: 35% Xrs 8: 34%-61% |
| LEE et al[57], 2012 | Healthy Korean | 161 | Rrs 5, 10, 15, 20, 25, 35 Xrs 5, 10, 15, 20, 25, 35 | Salbutamol 200 µg | 15 | Rrs 5 -0.127 Rrs 10 -0.098 Rrs 15 -0.073 Rrs 20 -0.056 Rrs 25 -0.056 Rrs 35 -0.057 Xrs 5 0.062 Xrs 10 0.057 Xrs 15 0.059 Xrs 20 0.044 Xrs 25 0.033 Xrs 35 0.054 Fres -2.167 | Rrs 5: 11.8 Rrs 10: 10.8 Rrs 15: 8.7 Rrs 20: 6.972 Rrs 25: 7.029 Rrs 35: 6.095 Xrs 5: 13.474 Xrs 10: 25.946 Fres: 10.457 |
| Calogero et al[43], 2013 | Healthy Australian and Italian (2-16) | 502 | Rrs 6, 8, 10 Xrs 6, 8, 10 Fres, AX | Salbutamol 200 µg | 15 | Rrs 6 -2.9 Rrs 8 -2.74 Rrs 10 -2.39 Xrs 6 -1.80 Xrs 8 - 1.93 Xrs 10 -1.90 AX -33 Fres -12 | Rrs 6: 34 Rrs 8: 32 Rrs 10: 31 Xrs 6: 50 Xrs 8: 65 Xrs 10: 74 AX: 81 Fres: 47 |
BDR: Bronchodilator responsiveness; Rrs: Respiratory system resistance; Xrs: Respiratory system reactance in hPa/s per L; Fres: Resonant frequency; AX: Area under the Xrs curve from 5 Hz to Fres; MF: Multi-frequency system; Fdep: Frequency dependence of Rrs between 4-24 Hz.
The previous studies in healthy and wheezy young children have not conducted a ROC analysis to formally establish the sensitivity and specificity of a certain BDR cut off to be assessed. Limitations to the wider use of FOT in assessing BDR include the variability of medications, their timing and dosage between the different studies (Table 3).
Bronchial hyper-responsiveness using FOT
Bronchial hyper-responsiveness, usually assessed using spirometry, is the gold standard for confirming a diagnosis of asthma in older children and adults[58,59]. However, false negative or false positive results can occur in young children who cannot perform an acceptable manoeuvre. BHR has been assessed in young children using other methods including FOT, interrupter technique, whole-body plethysmography and transcutaneous oxygen measurement SPO2[5,47,60-63].
Bronchial hyper-responsiveness studies comparing FOT with different lung function measures have reported FOT to be as effective as spirometry[63-69] and as sensitive as body plethysmography[70] and transcutaneous PO2[50] in older children with asthma. BHR has been assessed using FOT in children younger than 7 years of age with a range of challenge tests including adenosine monophosphate (AMP)[19], cold air[24], normal saline[21] methacholine[22,62,63,66,68,71], mannitol[25] and exercise[20,72] demonstrating that FOT can be reliably used in young children for challenge testing.
FOT characterization of BHR has been shown to be correlated to asthma severity[73] and to be sensitive to the response to immune therapy[74]. Another study has shown that cough variant asthma showed less BHR in comparison to classical asthma children[75].
Despite the above studies have clearly demonstrated the use of FOT to assess BHR in children, there are few studies demonstrating the best cut off value of BHR between healthy and children with asthma using FOT. Further work is needed before establishing FOT use as clinical tool to assess BHR in children.
Limitation of FOT in children and future direction
Although forced oscillation technique can contribute to the diagnosis and management of childhood asthma, it has some limitations. Although, unlike spirometry, it does not require forced expiratory manoeuvres, it still require some cooperation by children to achieve successful repeatable measures. It is therefore both age and cooperation dependant. The practical advantage of the availability and affordability of different FOT commercial equipment, the Rrs and Xrs output are not always measured at the same frequencies by all these devices. This makes the comparison between different studies challenging. The standardization of the available commercial equipment is therefore still needed and FOT guidelines are currently being reviewed by the ATS and ERS.
As the available FOT reference equations have been constructed in specific populations, these findings cannot be generalised to other ethnic groups. Further studies are therefore still required to establish FOT reference values in other populations or ethnic groups. The assessment of BDR using FOT is not widely implemented because of differences amongst the relevant studies, including differences in the medications used, as well as their timing and dosage. Further studies are therefore required to establish an international standard protocol for this assessment as currently BDR still has not been studied in relation to recent symptoms in young children with wheeze, developing such studies would help not only in the follow up of children with wheeze, but also to ascertain the level of control of asthma symptoms and the compliance to medication in children with asthma.
Further research is also required to assess BHR, particularly in young children, in addition to standardise the use of FOT in young children for BHR assessment.
Recently there are new studies that have reported Rrs or Xrs from either expiration or inspiration (or both), including flow limitation within a breath. Those studies suggest that this approach is more sensitive than standard reporting of FOT. However, significant work is required prior to the intrdocution of these outcomes into clinical practice and this remains an area for the future studies[76,77].
In conclusion, with the relatively high prevalence of childhood asthma, FOT has been proven to be a useful tool to aid in its diagnosis and management especially in children unable to perform spirometry. As the recent availability of commercial equipment has increased its use both in research and in clinical practice, clinicians have to understand the emerging role of FOT in clinical practice and how to interpret its results in order to optimise clinical management of children with asthma.
Footnotes
Conflict-of-interest statement: The authors have no conflict of interest to declare.
Manuscript source: Invited manuscript
Specialty type: Medical laboratory technology
Country of origin: United Arab Emirates
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
Peer-review started: February 28, 2017
First decision: September 4, 2017
Article in press: November 1, 2017
P- Reviewer: Fretzayas A, Ni Y S- Editor: Cui LJ L- Editor: A E- Editor: Lu YJ
Contributor Information
Afaf Alblooshi, Department of Pediatrics, United Arab Emirates University, Al-Ain, United Arab Emirates. afaf.alblooshi@uaeu.ac.ae.
Alia Alkalbani, Department of Pediatrics, Tawam Hospital, Al-Ain, United Arab Emirates.
Ghaya Albadi, Department of Pediatrics, United Arab Emirates University, Al-Ain, United Arab Emirates.
Hassib Narchi, Department of Pediatrics, United Arab Emirates University, Al-Ain, United Arab Emirates.
Graham Hall, Department of Children’s Lung Health, Telethon Kids Institute, Perth 6000, Australia; School of Physiotherapy and Exercise Science, Curtin University and Centre of Child Health Research, University of Western Australia, Perth 6000, Australia.
References
- 1.Braman SS. The global burden of asthma. Chest. 2006;130:4S–12S. doi: 10.1378/chest.130.1_suppl.4S. [DOI] [PubMed] [Google Scholar]
- 2.Pattemore PK, Asher MI, Harrison AC, Mitchell EA, Rea HH, Stewart AW. The interrelationship among bronchial hyperresponsiveness, the diagnosis of asthma, and asthma symptoms. Am Rev Respir Dis. 1990;142:549–554. doi: 10.1164/ajrccm/142.3.549. [DOI] [PubMed] [Google Scholar]
- 3.Mai XM, Nilsson L, Kjellman NI, Björkstén B. Hypertonic saline challenge tests in the diagnosis of bronchial hyperresponsiveness and asthma in children. Pediatr Allergy Immunol. 2002;13:361–367. doi: 10.1034/j.1399-3038.2002.01011.x. [DOI] [PubMed] [Google Scholar]
- 4.Global Initiative for Asthma. Global strategy for asthma management and prevention 2017. Available from: http://www.ginasthma.org.
- 5.Kanengiser S, Dozor AJ. Forced expiratory maneuvers in children aged 3 to 5 years. Pediatr Pulmonol. 1994;18:144–149. doi: 10.1002/ppul.1950180305. [DOI] [PubMed] [Google Scholar]
- 6.Crenesse D, Berlioz M, Bourrier T, Albertini M. Spirometry in children aged 3 to 5 years: reliability of forced expiratory maneuvers. Pediatr Pulmonol. 2001;32:56–61. doi: 10.1002/ppul.1089. [DOI] [PubMed] [Google Scholar]
- 7.Arets HG, Brackel HJ, van der Ent CK. Forced expiratory manoeuvres in children: do they meet ATS and ERS criteria for spirometry? Eur Respir J. 2001;18:655–660. doi: 10.1183/09031936.01.00204301. [DOI] [PubMed] [Google Scholar]
- 8.Dubois AB, Botelho SY, Comroe JH Jr. A new method for measuring airway resistance in man using a body plethysmograph: values in normal subjects and in patients with respiratory disease. J Clin Invest. 1956;35:327–335. doi: 10.1172/JCI103282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beydon N, Davis SD, Lombardi E, Allen JL, Arets HG, Aurora P, Bisgaard H, Davis GM, Ducharme FM, Eigen H, et al. An official American Thoracic Society/European Respiratory Society statement: pulmonary function testing in preschool children. Am J Respir Crit Care Med. 2007;175:1304–1345. doi: 10.1164/rccm.200605-642ST. [DOI] [PubMed] [Google Scholar]
- 10.Oostveen E, MacLeod D, Lorino H, Farré R, Hantos Z, Desager K, Marchal F; ERS Task Force on Respiratory Impedance Measurements. The forced oscillation technique in clinical practice: methodology, recommendations and future developments. Eur Respir J. 2003;22:1026–1041. doi: 10.1183/09031936.03.00089403. [DOI] [PubMed] [Google Scholar]
- 11.Marchal F, Hall GL. Forced oscillation technique. Paediatric Lung Function. European Respiratory Society J Ltd. 2010;47:121–136. [Google Scholar]
- 12.Ducharme FM, Davis GM. Respiratory resistance in the emergency department: a reproducible and responsive measure of asthma severity. Chest. 1998;113:1566–1572. doi: 10.1378/chest.113.6.1566. [DOI] [PubMed] [Google Scholar]
- 13.Hall GL, Sly PD, Fukushima T, Kusel MM, Franklin PJ, Horak F Jr, Patterson H, Gangell C, Stick SM. Respiratory function in healthy young children using forced oscillations. Thorax. 2007;62:521–526. doi: 10.1136/thx.2006.067835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davis SD, Eber E, Koumbourlis AC. Applications and Interpretation Sharon I.S. Rounds: Springer. Diagnostic Tests in Pediatric Pulmonology. 2014:161–162. [Google Scholar]
- 15.Bates JH, Irvin CG, Farré R, Hantos Z. Oscillation mechanics of the respiratory system. Compr Physiol. 2011;1:1233–1272. doi: 10.1002/cphy.c100058. [DOI] [PubMed] [Google Scholar]
- 16.Klug B, Bisgaard H. Specific airway resistance, interrupter resistance, and respiratory impedance in healthy children aged 2-7 years. Pediatr Pulmonol. 1998;25:322–331. doi: 10.1002/(sici)1099-0496(199805)25:5<322::aid-ppul6>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 17.Oostveen E, Dom S, Desager K, Hagendorens M, De Backer W, Weyler J. Lung function and bronchodilator response in 4-year-old children with different wheezing phenotypes. Eur Respir J. 2010;35:865–872. doi: 10.1183/09031936.00023409. [DOI] [PubMed] [Google Scholar]
- 18.Malmberg LP, Pelkonen A, Poussa T, Pohianpalo A, Haahtela T, Turpeinen M. Determinants of respiratory system input impedance and bronchodilator response in healthy Finnish preschool children. Clin Physiol Funct Imaging. 2002;22:64–71. [PubMed] [Google Scholar]
- 19.Hall GL, Gangell C, Fukushima T, Horak F, Patterson H, Stick SM, Sly PD, Franklin PJ. Application of a shortened inhaled adenosine-5’-monophosphate challenge in young children using the forced oscillation technique. Chest. 2009;136:184–189. doi: 10.1378/chest.08-2848. [DOI] [PubMed] [Google Scholar]
- 20.Malmberg LP, Mäkelä MJ, Mattila PS, Hammarén-Malmi S, Pelkonen AS. Exercise-induced changes in respiratory impedance in young wheezy children and nonatopic controls. Pediatr Pulmonol. 2008;43:538–544. doi: 10.1002/ppul.20805. [DOI] [PubMed] [Google Scholar]
- 21.Wilson NM, Bridge P, Silverman M. Bronchial responsiveness and symptoms in 5-6 year old children: a comparison of a direct and indirect challenge. Thorax. 1995;50:339–345. doi: 10.1136/thx.50.4.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilson N, Bridge P, Phagoo S, Silverman M. The measurement of methacholine responsiveness in 5 year old children: three methods compared. Eur Respir J. 1995;8:364–370. doi: 10.1183/09031936.95.08030364. [DOI] [PubMed] [Google Scholar]
- 23.Klug B, Bisgaard H. Measurement of lung function in awake 2-4-year-old asthmatic children during methacholine challenge and acute asthma: a comparison of the impulse oscillation technique, the interrupter technique, and transcutaneous measurement of oxygen versus whole-body plethysmography. Pediatr Pulmonol. 1996;21:290–300. doi: 10.1002/(SICI)1099-0496(199605)21:5<290::AID-PPUL4>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 24.Nielsen KG, Bisgaard H. Lung function response to cold air challenge in asthmatic and healthy children of 2-5 years of age. Am J Respir Crit Care Med. 2000;161:1805–1809. doi: 10.1164/ajrccm.161.6.9905098. [DOI] [PubMed] [Google Scholar]
- 25.Alblooshi AS, Simpson SJ, Stick SM, Hall GL. The safety and feasibility of the inhaled mannitol challenge test in young children. Eur Respir J. 2013;42:1420–1423. doi: 10.1183/09031936.00041713. [DOI] [PubMed] [Google Scholar]
- 26.Frey U. Forced oscillation technique in infants and young children. Paediatr Respir Rev. 2005;6:246–254. doi: 10.1016/j.prrv.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 27.Bates JH, Daróczy B, Hantos Z. A comparison of interrupter and forced oscillation measurements of respiratory resistance in the dog. J Appl Physiol (1985) 1992;72:46–52. doi: 10.1152/jappl.1992.72.1.46. [DOI] [PubMed] [Google Scholar]
- 28.Jackson AC, Tennhoff W, Kraemer R, Frey U. Airway and tissue resistance in wheezy infants: effects of albuterol. Am J Respir Crit Care Med. 1999;160:557–563. doi: 10.1164/ajrccm.160.2.9808137. [DOI] [PubMed] [Google Scholar]
- 29.Goldman MD, Saadeh C, Ross D. Clinical applications of forced oscillation to assess peripheral airway function. Respir Physiol Neurobiol. 2005;148:179–194. doi: 10.1016/j.resp.2005.05.026. [DOI] [PubMed] [Google Scholar]
- 30.Grimby G, Takishima T, Graham W, Macklem P, Mead J. Frequency dependence of flow resistance in patients with obstructive lung disease. J Clin Invest. 1968;47:1455–1465. doi: 10.1172/JCI105837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goldman MD. Clinical application of forced oscillation. Pulm Pharmacol Ther. 2001;14:341–350. doi: 10.1006/pupt.2001.0310. [DOI] [PubMed] [Google Scholar]
- 32.Meraz E, Nazeran H, Goldman M, Nava P, Diong B. Impulse oscillometric features of lung function: towards computer-aided classification of respiratory diseases in children. Conf Proc IEEE Eng Med Biol Soc. 2008;2008:2443–2446. doi: 10.1109/IEMBS.2008.4649693. [DOI] [PubMed] [Google Scholar]
- 33.Stanojevic S, Wade A, Lum S, Stocks J. Reference equations for pulmonary function tests in preschool children: a review. Pediatr Pulmonol. 2007;42:962–972. doi: 10.1002/ppul.20691. [DOI] [PubMed] [Google Scholar]
- 34.Stanojevic S, Wade A, Stocks J. Reference values for lung function: past, present and future. Eur Respir J. 2010;36:12–19. doi: 10.1183/09031936.00143209. [DOI] [PubMed] [Google Scholar]
- 35.Frei J, Jutla J, Kramer G, Hatzakis GE, Ducharme FM, Davis GM. Reference values for respiratory system impedance by using impulse oscillometry in children aged 2–11 years. Chest. 2005;128:1266–1273. doi: 10.1378/chest.128.3.1266. [DOI] [PubMed] [Google Scholar]
- 36.Dencker M, Malmberg LP, Valind S, Thorsson O, Karlsson MK, Pelkonen A, Pohjanpalo A, Haahtela T, Turpeinen M, Wollmer P. Reference values for respiratory system impedance by using impulse oscillometry in children aged 2-11 years. Clin Physiol Funct Imaging. 2006;26:247–250. doi: 10.1111/j.1475-097X.2006.00682.x. [DOI] [PubMed] [Google Scholar]
- 37.Amra B, Soltaninejad F, Golshan M. Respiratory resistance by impulse oscillometry in healthy Iranian children aged 5-19 years. Iran J Allergy Asthma Immunol. 2008;7:25–29. [PubMed] [Google Scholar]
- 38.Nowowiejska B, Tomalak W, Radliński J, Siergiejko G, Latawiec W, Kaczmarski M. Transient reference values for impulse oscillometry for children aged 3-18 years. Pediatr Pulmonol. 2008;43:1193–1197. doi: 10.1002/ppul.20926. [DOI] [PubMed] [Google Scholar]
- 39.Vu LT, Demoulin B, Nguyen YT, Nguyen MT, Marchal F. Respiratory impedance and response to salbutamol in healthy Vietnamese children. Pediatr Pulmonol. 2008;43:1013–1019. doi: 10.1002/ppul.20904. [DOI] [PubMed] [Google Scholar]
- 40.Vu LT, Demoulin B, Nguyen MT, Nguyen YT, Marchal F. Respiratory impedance and response to salbutamol in asthmatic Vietnamese children. Pediatr Pulmonol. 2010;45:380–386. doi: 10.1002/ppul.21201. [DOI] [PubMed] [Google Scholar]
- 41.Calogero C, Parri N, Baccini A, Cuomo B, Palumbo M, Novembre E, Morello P, Azzari C, de Martino M, Sly PD, et al. Respiratory impedance and bronchodilator response in healthy Italian preschool children. Pediatr Pulmonol. 2010;45:1086–1094. doi: 10.1002/ppul.21292. [DOI] [PubMed] [Google Scholar]
- 42.Park JH, Yoon JW, Shin YH, Jee HM, Wee YS, Chang SJ, Sim JH, Yum HY, Han MY. Reference values for respiratory system impedance using impulse oscillometry in healthy preschool children. Korean J Pediatr. 2011;54:64–68. doi: 10.3345/kjp.2011.54.2.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Calogero C, Simpson SJ, Lombardi E, Parri N, Cuomo B, Palumbo M, de Martino M, Shackleton C, Verheggen M, Gavidia T, et al. Respiratory impedance and bronchodilator responsiveness in healthy children aged 2-13 years. Pediatr Pulmonol. 2013;48:707–715. doi: 10.1002/ppul.22699. [DOI] [PubMed] [Google Scholar]
- 44.Shackleton C, Barraza-Villarreal A, Chen L, Gangell CL, Romieu I, Sly PD. Reference ranges for Mexican preschool-aged children using the forced oscillation technique. Arch Bronconeumol. 2013;49:326–329. doi: 10.1016/j.arbres.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 45.Frei J, Jutla J, Kramer G, Hatzakis GE, Ducharme FM, Davis GM. Impulse oscillometry: reference values in children 100 to 150 cm in height and 3 to 10 years of age. Chest. 2005;128:1266–1273. doi: 10.1378/chest.128.3.1266. [DOI] [PubMed] [Google Scholar]
- 46.Hagiwara S, Mochizuki H, Muramatsu R, Koyama H, Yagi H, Nishida Y, Kobayashi T, Sakamoto N, Takizawa T, Arakawa H. Reference values for Japanese children’s respiratory resistance using the LMS method. Allergol Int. 2014;63:113–119. doi: 10.2332/allergolint.13-OA-0591. [DOI] [PubMed] [Google Scholar]
- 47.Bisgaard H, Klug B. Lung function measurement in awake young children. Eur Respir J. 1995;8:2067–2075. doi: 10.1183/09031936.95.08122067. [DOI] [PubMed] [Google Scholar]
- 48.Shi Y, Aledia AS, Galant SP, George SC. Peripheral airway impairment measured by oscillometry predicts loss of asthma control in children. J Allergy Clin Immunol. 2013;131:718–723. doi: 10.1016/j.jaci.2012.09.022. [DOI] [PubMed] [Google Scholar]
- 49.Bacharier LB, Strunk RC, Mauger D, White D, Lemanske RF Jr, Sorkness CA. Classifying asthma severity in children: mismatch between symptoms, medication use, and lung function. Am J Respir Crit Care Med. 2004;170:426–432. doi: 10.1164/rccm.200308-1178OC. [DOI] [PubMed] [Google Scholar]
- 50.Holmgren D, Engström I, Bjure J, Sixt R, Aberg N. Respiratory resistance and transcutaneous PO2 during histamine provocation in children with bronchial asthma. Pediatr Pulmonol. 1993;15:168–174. doi: 10.1002/ppul.1950150308. [DOI] [PubMed] [Google Scholar]
- 51.Klug B, Bisgaard H. Lung function and short-term outcome in young asthmatic children. Eur Respir J. 1999;14:1185–1189. doi: 10.1183/09031936.99.14511859. [DOI] [PubMed] [Google Scholar]
- 52.Song TW, Kim KW, Kim ES, Park JW, Sohn MH, Kim KE. Utility of impulse oscillometry in young children with asthma. Pediatr Allergy Immunol. 2008;19:763–768. doi: 10.1111/j.1399-3038.2008.00734.x. [DOI] [PubMed] [Google Scholar]
- 53.Thamrin C, Gangell CL, Udomittipong K, Kusel MM, Patterson H, Fukushima T, Schultz A, Hall GL, Stick SM, Sly PD. Assessment of bronchodilator responsiveness in preschool children using forced oscillations. Thorax. 2007;62:814–819. doi: 10.1136/thx.2006.071290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Marotta A, Klinnert MD, Price MR, Larsen GL, Liu AH. Impulse oscillometry provides an effective measure of lung dysfunction in 4-year-old children at risk for persistent asthma. J Allergy Clin Immunol. 2003;112:317–322. doi: 10.1067/mai.2003.1627. [DOI] [PubMed] [Google Scholar]
- 55.Oostveen E, Dom S, Desager K, Hagendorens M, De Backer W, Weyler J. Expression of bronchodilator response using forced oscillation technique measurements: absolute versus relative. Eur Respir J. 2010;36:213. doi: 10.1183/09031936.00025310. [DOI] [PubMed] [Google Scholar]
- 56.Nielsen KG, Bisgaard H. Discriminative capacity of bronchodilator response measured with three different lung function techniques in asthmatic and healthy children aged 2 to 5 years. Am J Respir Crit Care Med. 2001;164:554–559. doi: 10.1164/ajrccm.164.4.2006119. [DOI] [PubMed] [Google Scholar]
- 57.Lee JY, Seo JH, Kim HY, Jung YH, Kwon JW, Kim BJ, Kim HB, Lee SY, Jang GC, Song DJ, et al. Reference values of impulse oscillometry and its utility in the diagnosis of asthma in young Korean children. J Asthma. 2012;49:811–816. doi: 10.3109/02770903.2012.716472. [DOI] [PubMed] [Google Scholar]
- 58.Kersten ET, Driessen JM, van der Berg JD, Thio BJ. Mannitol and exercise challenge tests in asthmatic children. Pediatr Pulmonol. 2009;44:655–661. doi: 10.1002/ppul.21034. [DOI] [PubMed] [Google Scholar]
- 59.Subbarao P, Brannan JD, Ho B, Anderson SD, Chan HK, Coates AL. Inhaled mannitol identifies methacholine-responsive children with active asthma. Pediatr Pulmonol. 2000;29:291–298. doi: 10.1002/(sici)1099-0496(200004)29:4<291::aid-ppul9>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 60.Yong SC, Smith CM, Wach R, Kurian M, Primhak RA. Methacholine challenge in preschool children: methacholine-induced wheeze versus transcutaneous oximetry. Eur Respir J. 1999;14:1175–1178. doi: 10.1183/09031936.99.14511759. [DOI] [PubMed] [Google Scholar]
- 61.Mayer OH, Clayton RG Sr, Jawad AF, McDonough JM, Allen JL. Respiratory inductance plethysmography in healthy 3- to 5-year-old children. Chest. 2003;124:1812–1819. doi: 10.1378/chest.124.5.1812. [DOI] [PubMed] [Google Scholar]
- 62.Choi SH, Sheen YH, Kim MA, Baek JH, Baek HS, Lee SJ, Yoon JW, Rha YH, Han MY. Clinical Implications of Oscillatory Lung Function during Methacholine Bronchoprovocation Testing of Preschool Children. Biomed Res Int. 2017;2017:9460190. doi: 10.1155/2017/9460190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yoon JW, Shin YH, Jee HM, Chang SJ, Baek JH, Choi SH, Kim HY, Han MY. Useful marker of oscillatory lung function in methacholine challenge test-comparison of reactance and resistance with dose-response slope. Pediatr Pulmonol. 2014;49:521–528. doi: 10.1002/ppul.22866. [DOI] [PubMed] [Google Scholar]
- 64.Peták F, Czövek D, Novák Z. Spirometry and forced oscillations in the detection of airway hyperreactivity in asthmatic children. Pediatr Pulmonol. 2012;47:956–965. doi: 10.1002/ppul.22551. [DOI] [PubMed] [Google Scholar]
- 65.Klug B, Bisgaard H. Measurement of the specific airway resistance by plethysmography in young children accompanied by an adult. Eur Respir J. 1997;10:1599–1605. doi: 10.1183/09031936.97.10071599. [DOI] [PubMed] [Google Scholar]
- 66.Schulze J, Smith HJ, Fuchs J, Herrmann E, Dressler M, Rose MA, Zielen S. Methacholine challenge in young children as evaluated by spirometry and impulse oscillometry. Respir Med. 2012;106:627–634. doi: 10.1016/j.rmed.2012.01.007. [DOI] [PubMed] [Google Scholar]
- 67.Bailly C, Crenesse D, Albertini M. Evaluation of impulse oscillometry during bronchial challenge testing in children. Pediatr Pulmonol. 2011;46:1209–1214. doi: 10.1002/ppul.21492. [DOI] [PubMed] [Google Scholar]
- 68.Takami S, Mochizuki H, Muramatsu R, Hagiwara S, Arakawa H. Relationship between bronchial hyperresponsiveness and lung function in children age 5 and 6 with and without asthma. Respirology. 2013;18:682–687. doi: 10.1111/resp.12061. [DOI] [PubMed] [Google Scholar]
- 69.Kim HY, Shin YH, Jung DW, Jee HM, Park HW, Han MY. Resistance and reactance in oscillation lung function reflect basal lung function and bronchial hyperresponsiveness respectively. Respirology. 2009;14:1035–1041. doi: 10.1111/j.1440-1843.2009.01605.x. [DOI] [PubMed] [Google Scholar]
- 70.Buhr W, Jörres R, Berdel D, Làndsér FJ. Correspondence between forced oscillation and body plethysmography during bronchoprovocation with carbachol in children. Pediatr Pulmonol. 1990;8:280–288. doi: 10.1002/ppul.1950080413. [DOI] [PubMed] [Google Scholar]
- 71.Jee HM, Kwak JH, Jung DW, Han MY. Useful parameters of bronchial hyperresponsiveness measured with an impulse oscillation technique in preschool children. J Asthma. 2010;47:227–232. doi: 10.3109/02770901003624259. [DOI] [PubMed] [Google Scholar]
- 72.Schweitzer C, Abdelkrim IB, Ferry H, Werts F, Varechova S, Marchal F. Airway response to exercise by forced oscillations in asthmatic children. Pediatr Res. 2010;68:537–541. doi: 10.1203/PDR.0b013e3181f851d2. [DOI] [PubMed] [Google Scholar]
- 73.Wang JY. The study of bronchial hyperresponsiveness in asthmatic children by forced oscillation technique. Asian Pac J Allergy Immunol. 1991;9:51–56. [PubMed] [Google Scholar]
- 74.Chen WY, Yu J, Wang JY. The effect of immunotherapy on bronchial hyperresponsiveness in asthmatic children. Asian Pac J Allergy Immunol. 1994;12:15–20. [PubMed] [Google Scholar]
- 75.Mochizuki H, Arakawa H, Tokuyama K, Morikawa A. Bronchial sensitivity and bronchial reactivity in children with cough variant asthma. Chest. 2005;128:2427–2434. doi: 10.1378/chest.128.4.2427. [DOI] [PubMed] [Google Scholar]
- 76.Lombardi E, Sly P, Parri N, Simpson SJ, Calogero C. Respiratory Impedance Using Forced Oscillation Technique In 3-13 Year-Old Children With A History Of Wheezing. B107 Tools of the trade: modalities for evaluating pediatric lung disease. Am Thoracic Soc. 2013:A3696. [Google Scholar]
- 77.Chacko A, Czovek D, Mills D, Shackleton C, Hantos Z, Sly PD. Acute Changes In Dynamic Airway Mechanics In Young Children With Viral Wheeze Is Detectable Via Temporal Forced Oscillation Technique. a106 Assessing pediatric lung disease: lung function and beyond. Am Thoracic Soc. 2015:A2337. [Google Scholar]


