Abstract
Background
Malaria in Senegal is due essentially to infections by Plasmodium falciparum and, to a lesser extent to Plasmodium malariae and Plasmodium ovale. By the use of molecular methods, detection of Plasmodium vivax has been recently reported in the region of Kedougou, raising the question of appraisal of its potential prevalence in this setting.
Methods
A retrospective serological study was carried out using 188 samples taken from 2010 to 2011 in a longitudinal school survey during which 48 asymptomatic children (9–11 years) were recruited. Four collections of samples collected during two successive dry and rainy seasons were analysed for antibody responses to P. vivax and P. falciparum. Recombinant P. falciparum and P. vivax MSP1 antigens and total P. falciparum schizont lysate from African 07/03 strain (adapted to culture) were used for ELISA. Nested PCR amplification was used for molecular detection of P. vivax.
Results
A surprising high prevalence of IgG responses against P. vivax MSP1 was evidenced with 53% of positive samples and 58% of the individuals that were found positive to this antigen. There was 77% of responders to P. falciparum outlined by 63% of positive samples. Prevalence of responders did not differ as function of seasons. Levels of antibodies to P. falciparum fluctuated with significant increasing between dry and rainy season (P < 0.05), contrary to responses to P. vivax. There was a significant reciprocal relationship (P < 10−3) between antibody responses to the different antigens, but with weak coefficient of correlation (Rho around 0.3) underlining a variable profile at the individual level. Clear molecular signature was found in positive IgG to P. vivax msp1 samples by PCR.
Conclusion
This cross-sectional longitudinal study highlights the unexpected high circulation of P. vivax in this endemic area. Sero-immunology and molecular methods are powerful additive tools to identify endemic sites where relevant control measures have to be settled and monitored.
Keywords: Malaria, Plasmodium falciparum, Plasmodium vivax, ELISA, IgG, MSP1, Asymptomatic carriage, Parasite circulation
Background
Malaria remains a major threat in tropical and sub-tropical regions, with nearly 50% of the world population exposed to infective bites by Anopheles mosquitoes. Of the four species of Plasmodium, Plasmodium falciparum is responsible of 214 million cases in 2015 and almost half million deaths annually [1], essentially in sub-Saharan African children. Scaling up of integrated interventions strategies, including artemisinin-based combination therapy (ACT), universal coverage with long-lasting insecticide-impregnated bed nets (LLINs), systematic diagnosis using rapid tests (RDTs) has considerably reduced the burden of malaria in many countries. Plasmodium vivax has the widest geographic range and is responsible for 390 million clinical infections [2] along with a substantial mortality (1400–14,900 fatal cases) in endemic countries [1, 3]. Plasmodium vivax is the major cause of malaria outside of Africa, is responsible for long-term chronic illness and has dramatic consequences for global health and economy of endemic regions [4–6].
The two parasites coexist in large areas of the tropical and semi-tropical world, except, strikingly, in large parts of sub-Saharan Africa, where P. vivax appears to be almost completely absent [7, 8]. This situation is apparently caused by the high prevalence of the Duffy negative phenotype in the local populations, which was for a long time believed to confer complete protection against P. vivax malaria [9]. However, this belief is now being reconsidered upon several reports of P. vivax infections in Duffy negative individuals [10–15], as well as in countries where either P. vivax was absent, or was not detectable by the available methods as subsequently pointed by several reports for Eastern, Western and Central African countries [12–14, 16, 17].
PCR diagnosis is a highly sensitive method for detection of sub-microscopic circulating parasite species [18, 19]. However, some studies were negative when tracking of P. vivax in investigation of 2588 samples from West and Central Africa [20], and in Senegal by means of real time PCR and genotyping on 484 blood samples [21]. In contrast, recent studies reported molecular evidence of P. vivax infections in symptomatic patients in Senegal [22], in Mali [15] and in Cameroon [23]. The recent positive results from Kedougou region [22] led to enlarge the tracking procedure by investigating P. vivax antibody signature in a retrospective collection of sera selected from a long-term surveillance procedure settled in this geographical area.
In a first step, a screening was performed in a longitudinal survey involving a cohort of 48 asymptomatic school children and investigated for the potential co-circulation of P. vivax and P. falciparum. To this end, IgG responses to recombinant MSP1 antigens from the two species and whole parasite extract from P. falciparum were measured by ELISA. The specific presence of circulating P. vivax parasites in IgG positive samples was also investigated by molecular methods.
Methods
Study area, design and population
The study was conducted in the Kedougou region located in southeast Senegal bordering with Guinea, Mali and Gambia with the objective of investigating arboviruses infections and circulation. Details of the study area such as follow-up of population, climate, rainfall, landscape and fauna, have been previously reported [22, 24, 25]. Malaria investigation was an integral part of the project as a major cause of fever in that area leading to similar symptoms to those from virus infections requiring differential diagnosis. In this region, malaria remains highly prevalent with an incidence > 25‰ of confirmed clinical malaria cases. In Kedougou, transmission is high and seasonal. National Malaria Control Programme reported in 2013–2014 a total of 37,053 confirmed clinical cases including 1012 severe case, resulting in a prevalence of 255.5‰ [26].
The project recruited 48 school children from the Catholic Mission School in Kedougou (28 M/20 F, aged 8–11 years in May 2010) that were followed-up during 2 consecutive years (2010 and 2011) and sampled twice each year during the dry and rainy seasons (May and December, respectively). Children were asymptomatic for malaria episode at the recruitments.
Antigens and ELISA procedure
Recombinant MSP1 antigens from P. falciparum and P. vivax were secreted following infection of Trichoplusia in insect cells (High Five, Invitrogen) with recombinant baculovirus, and purified by chromatography using Talon metal affinity resin, as previously described [27, 28]. The baculovirus expression system has been shown to ensure optimal reproduction of conformational epitopes including EGF domains [29]. The whole parasite extract antigen was from the 07/03 Dielmo strain adapted to in vitro culture. Preparation and use of the schizont extract (SE) was done as described previously [30–32]. Antigens were diluted in PBS and used to coat Immulon-4 plates at a concentration of 1 µg mL−1 for MSPs and diluted at 1:320 for SE after calibration [31].
Levels and prevalence of IgG responses were quantified by ELISA with duplicate sera samples diluted 1:200 using standard procedure already described [33–35]. Positive and negative controls were included in each assay i.e. a pool of 25 sera from clinically immune adults living in the village of Dielmo (a holoendemic area of malaria transmission in Senegal), a pool of 20 sera from P. vivax infected patients from Madagascar (kind gift from Dr Inès Vigan-Womas) and a pool of European and/or African non-immune sera, respectively. Results were expressed as OD ratio = OD sample/OD naive serum pool. Sera showing an OD ratio > 2 (corresponding to the signal of naive controls + 3 SD) were considered sero-positive for prevalence analysis.
Molecular detection of Plasmodium species
The qualitative detection and characterization of Plasmodium spp. were performed on a subset of P. vivax serology-positive and negative samples selected from the four sampling periods and from five children using nested PCR amplification according to the method described by Snounou et al. [19]. Genomic DNA (gDNA) isolated from frozen serum samples as described previously [18, 36] were purified and concentrated using Genomic DNA clean and concentrator™-5 (catalogue number D4014, Zymo Research, Irvine, USA) according to manufacturer’s instructions. For the first round of PCR amplification, Plasmodium genus-specific primers (rPLU6 and rPLU5) were used for amplification of the 18S small subunit ribosomal RNA (18S ssrRNA) genes. The nested amplification was performed using species-specific primers rVIV1 and rVIV2 to amplify a P. vivax-specific 120 bp fragment of ssrRNA genes. DNA from blood samples of confirmed P. falciparum, P. malariae, P. ovale and P. vivax infected patients served for positive controls in all amplifications [22].
Statistical analysis
Antibody levels and prevalence of responders in different groups were compared using the Mann-Withney and Wilcoxon signed rank test, the Spearman rank correlation test for non-normally distributed paired data and the fisher exact test. P values < 0.05 were considered significant. Statistical analyses were performed with R and Statview 5.0 (SAS Institute) software.
Results
Prevalence and levels of antibody responses against antigens tested
Results of prevalence of responders and mean levels of antibody responses against PfMSP1p19, PvMSP1 and SE for each set of samples from 2010 and 2011 are summarized in Table 1. A surprising high prevalence of antibodies to P. vivax was revealed in this survey with 53% of positivity of overall samples tested and a median level of 1.5 OD ratio. When prevalence was calculated as function of the number of children with at least one positive sample against P. vivax MSP1 antigen during the survey, only 20 children remained negative and 28 positive i.e. 58% of responders (Fig. 1).
Table 1.
Prevalence and mean antibody levels measured in sequential samples from 48 children in Kedougou years 2010 and 2011
| Antigen tested | May 2010 | November 2010 | May 2011 | November 2011 | Overall |
|---|---|---|---|---|---|
| No individuals | No = 47 | N = 46 | N = 47 | N = 48 | N = 188 |
| Ag MSP1 | |||||
| Mean OD [min–max] | 0.57 [0–1.93] | 0.62 [0–1.93] | 0.47 [0–1.36] | 0.82 [0–2.25] | 0.52 [0–2.25] |
| P. vivax | |||||
| Mean OD ratio [min–max] | 2.6 [1–7.1] | 2.9 [1–6.4] | 2.2 [1–4.5] | 3.7 [1–7.2] | 2.9 [1–7.2] |
| No positive (prevalence) | 40% | 41% | 25% | 31% | 53% |
| Pf MSP1p19 | |||||
| Mean OD [min–max] | 0.11 [0–0.98] | 0.21 [0–2.10] | 0.10 [0–1.19] | 0.30 [0–2.14] | 0.18 [0–2.14] |
| Mean OD ratio [min–max] | 2.5 [1–16.7] | 4.0 [1–34.7] | 2.3 [1–20.0] | 5.4 [1–33.8] | 3.5 [1–33.8] |
| Prevalence | 43% | 38% | 23% | 46% | 61% |
| Ag SE 07_03 | |||||
| Mean OD [min–max] | 0.58 [0–2.45] | 0.65 [0–2.41] | 0.48 [0–2.39] | 0.82 [0–2.59] | 0.63 [0–2.59] |
| Mean OD ratio [min–max] | 2.5 [1–10.5] | 2.8 [1–10.4] | 2.2 [1–9.6] | 3.5 [1–12.3] | 2.8 [1–12.3] |
| No positive (prevalence) | 45% | 37% | 28% | 46% | 63% |
Fig. 1.
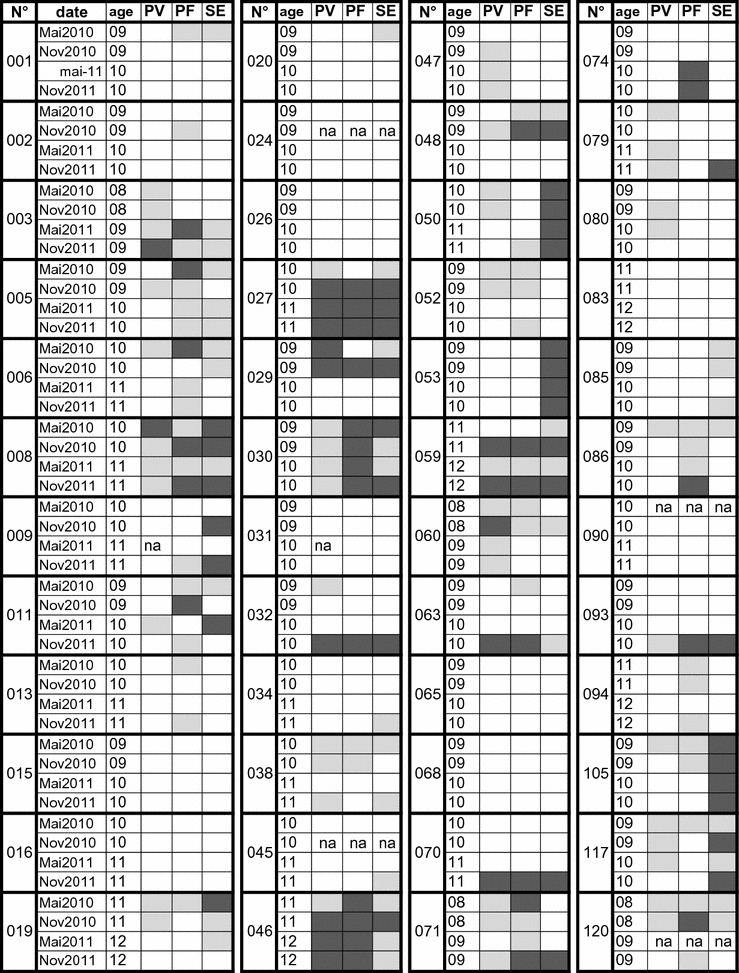
Detailed schematic results of individual responses of children to PvMSP1, PfMSP1p19 and SE during the 2 years’ follow-up. This graph summarizes antibody responses measured during the follow-up for each individual. IgG responses against PvMSP (PV), PfMSPp19 (PF) and Schizont extract (SE) were stratified as function of the magnitude of responses i.e. negative (white square), positive (ODratio > 2 and < 5, light grey square) and strong (ODratio > 5, dark grey square). Missing samples are labeled na
Regarding P. falciparum, prevalence and levels of antibody responses were high with 61 and 63% of positive samples against PfMSP1p19 and SE, respectively and a median OD ratio of 1.6 for the two antigens. When calculating prevalence for the actual number of individuals having a positive sample, 37 children were found positive at least once during the survey i.e. 77% of responders in the survey.
The antigen-specific longitudinal fluctuations of prevalence between the 4 monthly collections of samples were not significant (Table 1, Fisher exact test), except one significant increase of responders against PfMSP1p19 between May (23%) and November (46%) 2011.
Distribution of IgG responses against P. vivax and P. falciparum in individuals followed-up in 2010–2011
Longitudinal analysis of antibody responses measured during the follow-up is detailed for each individual on Fig. 1. Antibody responses were stratified as negative (white), positive (grey) and elevated (OD ratio > 5; dark grey) and illustrated as a function of time for each child. Profiles of antibody responses appeared substantially variable among individuals: some children remained completely antibody negative during the 2-years survey against the two species (n = 9), and some others showed low (n = 10) or high (n = 3) antibody responses to one parasite species (P. vivax or P. falciparum). Of note, 10 children showed antibodies to P. falciparum but not to P. vivax and two children had antibodies to P. vivax alone.
Longitudinal comparison of levels of Ab responses
Mean levels of IgG responses measured in the four sets of samples are plotted on Fig. 2a. The magnitude of antibody responses from positive individuals with ODratio > 2 is illustrated on Fig. 2b. Antibody responses to P. vivax MSP1 fluctuated moderately with a slight significant decrease (P = 0.045, Wilcoxon test) when comparing dry seasons of May 2010 vs May 2011. On the contrary, antibody responses to P. falciparum showed some substantial fluctuations. Antibodies to PfMSP1p19 significantly increased with the rainy seasons in 2010 and 2011 compared to the dry season. In addition, a significant lower level of responses was observed in May 2011 compared to May 2010 (P < 0.05). For the SE antigen, antibody profile of response was almost similar to PfMSP1p19, underlining a significant increase during the rainy season in 2011 and a lower level in May 2011 compared to May 2010.
Fig. 2.
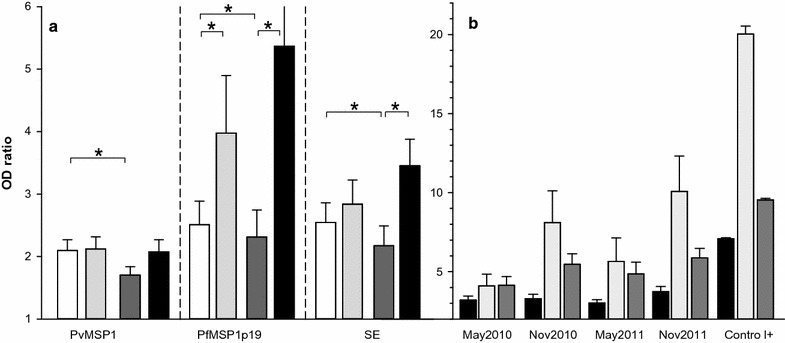
Levels of IgG responses to P. falciparum and P. vivax as function of time of follow-up. Longitudinal fluctuation of antibody levels is plotted in part a as histogram + SE for each Ag in May 2010 (white), November 2010 (light grey), May 2011 (dark grey), November 2011 (black). Asterisks indicate significant different level of Ab (P < 0.05, Wilcoxon signed rank test). In panel b, antibody levels for all positive responders (individuals with ODratio > 2) to PvMSP1 (black), PfMSP1p19 (light grey), SE (dark grey) are shown as histogram plots + SE for each set of samples from May 2010 to November 2011. IgG levels of positive controls are also shown for comparison
Regarding magnitude of antibody responses from high responders, mean levels were quite high (almost 50% of the levels of positive controls). Importantly, some individuals showed strong responses (Fig. 2b) with higher antibody levels than positive immune controls i.e. PvMSP1 (n = 2), PfMSP1p19 (n = 6) and SE (n = 7).
Relationship between antibody responses to the different antigens
The reciprocal correlation between levels of IgG against PvMSP1, PfMSP1p19 and SE was analysed by Spearman rank test and illustrated as XY plot including a linear regression curve on Fig. 3. There was a significant (P < 10−3) inter-relationship between IgG responses to PvMSP1 vs PfMSP1p19 (Rho = 0.56), PvMSP1 vs SE (Rho = 0.49), PvMSP1 vs FfMSP1p19 (Rho = 0.62). As shown on Fig. 3, correlation coefficients were weak from 18 to 32% in all cases. When analyzing by means of three level contingency tables (negative–positive–strong) it appears a score of 35–37% of discrepancy in responses.
Fig. 3.
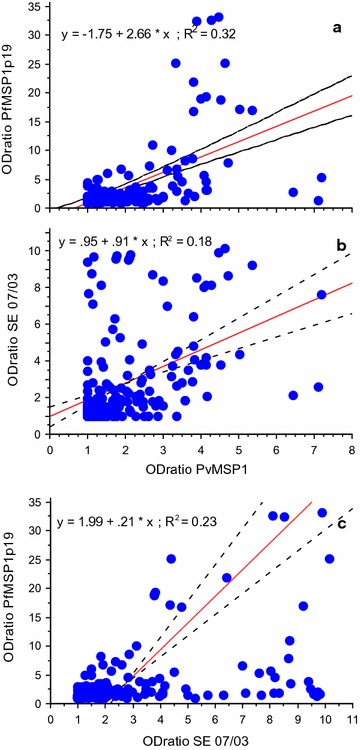
Correlation between IgG responses to the different antigens tested. Relationship between anti-PvMSP1 IgG responses and Ab to PfMSP1p19 and SE are plotted in a and b. Relationship between IgG responses to PfMSP1p19 and SE are plotted in c. Linear regression curve with 95% confidence interval are also plotted including the equation of the respective curve and their coefficient of correlation
Taken together with observations shown on Fig. 1, there is a variable profile of antibody response against P. vivax and P. falciparum at the individual level, outlining a relatively independent (non linear) profile of recognition of the three antigens in such a semi-longitudinal follow-up.
Molecular characterization of the P. vivax parasite in positive individuals
For the confirmation of presence of circulating P. vivax parasite in children, nested PCR testing was performed in a subset of samples that were positive for IgG to P. vivax Msp1 antigen to which were added as control samples from five negative individuals from the same cohort.
Results shown on Fig. 4 revealed the presence of amplified DNA in parasite control samples corresponding to P. falciparum (205 bp), P. vivax (120 bp), P. malariae (144 bp) and P. ovale (375 bp). Importantly, P. vivax 18S ssrRNA gene was also amplified in all selected serology-positive samples, as illustrated in Fig. 4 for samples 8–12 corresponding respectively to samples 008 (May 2010), 027 (November 2010), 046 (May 2011), 032 (November 2011) and 059 (November 2010) and originating from the four survey periods while no amplification was obtained for serology-negative samples as illustrated for the two samples shown in the gel that correspond to samples 015 and 016 from May 2010 and November 2010, respectively.
Fig. 4.
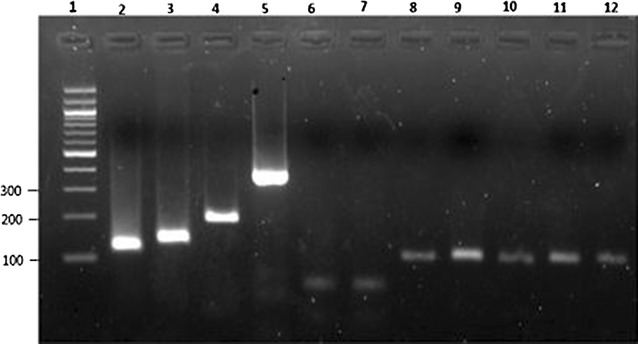
Gel picture showing detection of Plasmodium 18S ssrRNA gene. Lane 1 was loaded with 100 bp DNA Ladder. Positive amplification of P. vivax (120 bp), P. malariae (144 bp), P. falciparum (205 bp), and P. vivax (120 bp) is shown on lanes 2–5, respectively. Positive amplification of P. vivax 18S ssrRNA gene in serology-positive samples to PvMSP1 from five children 008, 027, 046, 032 and 059 (lanes 8–12) and the four sampling periods [May 2010 (lane 8), November 2010 (lanes 9 and 12), May 2011 (lane 10) and November 2011 (lane 11)] is also shown. Lack of amplification of P. vivax serology negative samples 015 (May 2010) and 016 (November 2010) is also shown on lanes 6 and 7, respectively
Discussion
Several recent findings have changed the vision of transmission of P. vivax in Africa with evidence of much more important presence of this parasite in West Africa. The dogma of a protecting barrier against P. vivax infection due to widespread Duffy-negativity in African population [9] has been revisited. There were already observations arguing for the presence of the parasite as nonimmune travelers returning from Central or Western Africa showed clinical infections diagnosed as being due to P. vivax that persisted over years of surveillance [37]. Furthermore, an increasing number of reports highlighted the capacity of P. vivax parasite to invade and infect Duffy negative individuals firstly in endemic areas, such Brazil [38], Ethiopia [39], Madagascar [11], Mauritania [14], but also in West African countries including Cameroon [10, 40], Equatorial Guinea, Angola [12] and recently Mali [15]. Thus, the real burden of P. vivax in Africa is largely unknown. The partial view of P. vivax epidemiology in Africa is due to several reasons starting with the dogma of Duffy-negative resistance to P. vivax infection, the low level of P. vivax parasitaemia compared to P. falciparum hardly detectable on slides, and limited tools available in different laboratories for affordable large-scale screenings. In addition, both relevant methods such as PCR and microscopy may not detect previously-cured P. vivax infections. For these reasons, a species- specific ELISA assay represents a complementary tool for population-based screening surveys in the absence of affordable rapid field test, comparable to the largely distributed ones for P. falciparum field detection.
Several studies underline antibodies to merozoite antigens as valuable biomarkers of immunity [41, 42]. Therefore, among these, MSP1 antigens from P. falciparum and P. vivax are interesting targets as biomarkers of exposure and protection. PfMSP1 has been used for longitudinal retrospective sero-surveillance in the Gambia providing relevant information about population immunity as well as exposure, in the context of declining transmission and immunity [43]. Importantly, MSP1 antigens from P. falciparum, P. vivax, P. malariae, P. ovale were shown to clearly indicate proportional exposure to these species without any cross-reactivity in Zimbabwean population [44]. The baculovirus expressed recombinant MSP1 antigens used in this study are highly recognized antigens harbouring conformational epitopes including EGF domains [45, 46]. They have been reported as relevant vaccine candidates [34, 47], including effective protection in experimental primate model for PvMSP1 [48]. Both MSP1s have been recently used as biomarkers in ELISA multiplex studies in cohorts from Cambodia, Senegal and Côte d’Ivoire [49–51].
Recent studies used serological testing with recombinant P. vivax circumsporozoite protein (PvCSP) and PvMSP1. Both of them are expressed in liver-stage parasite and post-hepatic merozoite even without blood infection and led to substantial levels of prevalence i.e. 13% in Congo by passive case detection [52] and almost 30% in Beninese blood donors [53]. Therefore, PvCSP and PvMSP1 showed high sensitivity and > 96% specificity highlighting the best predictive positive value of 93.3% for PvMSP1 [53]. Compared to single target antigens, whole parasite extracts as SE from P. falciparum used here has the advantage of containing a broad panel of parasite antigens, which moreover are presented in their native conformation. Well-defined SE antigen also appears as relevant antigen tool for monitoring fluctuation of anti-parasite antibody responses as function of transmission [33, 50, 51, 54], however whole parasite extracts are not available for P. vivax, a parasite presently not adapted to long-term in vitro culture.
An important point of this study relies upon the use of school surveys as such cohorts are considered as an appropriate target population somewhat easily accessible. In areas with decreasing transmission, the malaria risk become higher in 5–14 years old children than in the under 5 years old [55]. Therefore, measures of seroprevalence in this age group is very useful for estimating short-term changes in the burden of infection over a broad location. Thus, school-based surveys were revealed as an effective and highly relevant alternative to population-based surveys for identifying potential foci of transmission in areas with varying and/or decreasing transmission [56]. Recently, a pilot survey involving 32 schools in The Gambia identified potential hot spots in a large area of heterogeneous transmission [57]. Here the investigation in a longitudinal manner increased the detection capacity and resulted in a surprising high level of prevalence of IgG responses against P. vivax. The individual prevalence was 58% high i.e. almost twice higher than the result from single transversal measure from the dry season of May 2011. Such level of prevalence is also substantially higher than in Beninese blood donors 28.7% [53], than in Congo clinical cases 13% [52] or than in Cameroon symptomatic, asymptomatic adults (38, 15%) [10, 23]. All these reports were from cross-sectional studies, it is possible that longitudinal studies in those settings could reveal much higher level of circulation of P. vivax. Importantly, screening of schoolchildren in the present study raises the question of the considerable heterogeneity in the geographic distribution of transmission intensity in Senegal as function of climatic variation from north to south, and environmental factors including human activities [26]. In Kedougou, there is a relatively high malaria transmission as indicated by an EIR of 100–200 so that population live in co-endemic area with active transmission of P. falciparum, P. ovale spp. and P. malariae [21]. Strikingly, 9 out of 48 children (19%) remained completely negative during the 2 years of follow-up. Such observation raises the question of existing potential “hot/cold” spots of transmission requiring further investigation. As a matter of fact, living in co-endemic areas with active transmission of P. falciparum, P. ovale spp. and P. malariae was predictive of that exposure to infection by one malaria species would also be predictive of the risk as to exposure to another malaria species [52]. Likewise, responders to P. vivax were also responders to P. falciparum (28 out of 30), an observation supporting the hypothesis that co-circulation is a favorable environment for higher risk of P. vivax circulation. Indeed, co circulation is related to active transmission by mosquitoes as found in Anopheles gambiae and Anopheles funestus [13]. Further investigations are required to address these questions in Kedougou region; a pertinent survey should involve multispecies specific ELISA assay and PCR as complementary tools for malaria surveillance [55].
The presence of circulating P. vivax parasites revealed by nested PCR in a subset of serology-positive individuals tested suggests active P. vivax infections in this asymptomatic cohort with no clinical signs and symptoms of malaria at the time of sampling. P. vivax malaria has an atypically long incubation period in a large proportion of individuals but a typically mild clinical course [58]. Together, the recent [22] and current reports of P. vivax infections respectively in symptomatic and asymptomatic individuals are suggestive of an important circulation of P. vivax parasites in Kedougou. The parallel findings between the PCR positivity and sero-reactivity are in line with studies performed by others groups [49, 59] that observed tight correlations as well.
Conclusion
Taken together, these findings strongly suggest a high level of P. vivax transmission and the ability of the parasite to invade red blood cells and to persist and potentially expand through the human-mosquito transmission cycle. Several complementary investigations on these points are required and the true prevalence of P. vivax in Senegal should be questioned by investigation in other regions.
Authors’ contributions
AT, RP and AAS designed the study. ON and FD conducted the laboratory experiments for antibody responses, MN settled and performed molecular assays. AAS, AS, BDS, OF and MD supervised the collection of field samples and follow-up of children. RP, MN, AT and FD analyzed the data. RP drafted the manuscript, with input from MN and AT, and comments from all other authors. Figures and tables were prepared by RP, MN and ON. All authors contributed to the revision of the draft. All authors read and approved the final manuscript.
Acknowledgements
We are indebted to Dr. Shirley Longacre who generously provided the Pv/Pf MSP1p19 (Vaximax, Paris) and Dr. Marie-Louise Varela for kind substantial contribution to this work. We thank inhabitants of Kedougou and children, parents and teachers of Catholic Mission School for participation to the study.
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
The study was conducted in accordance with the local laws and regulations and was examined and approved by the Senegalese National Health Research Committee under the reference 0081MSP/DS/CNRS. A healthcare worker trained for conducting interviews and complete the questionnaire explained the study objectives, benefits and risks in Peulh (the most commonly spoken language in the area), other languages (Bassari, Malinke, Bedik) or French (the official Senegalese language) to parents/guardians and school administrator before inclusion. Written informed consent to particpate to the study was obtained from parents/legal guardians of children participants. A total of 188 sera were screened for antibodies responses to P. falciparum and P. vivax antigens.
Funding
The present work was supported by the Institut Pasteur Dakar Foundation. Initial study received funding from the United States National Institutes of Health (NIH) AI1069145.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Makhtar Niang, Fode Diop, Ronald Perraut and Aissatou Toure-Balde equally contributed to this work
Contributor Information
Makhtar Niang, Email: Makhtar.Niang@pasteur.sn.
Fode Diop, Email: Fode.Diop@pasteur.sn.
Oulimata Niang, Email: oulimataniang99@yahoo.ca.
Bacary D. Sadio, Email: Bacary.SADIO@pasteur.sn
Abdourahmane Sow, Email: asow20@gmail.com.
Ousmane Faye, Email: Ousmane.FAYE@pasteur.sn.
Mawlouth Diallo, Email: Mawlouth.DIALLO@pasteur.sn.
Amadou A. Sall, Email: Amadou.SALL@pasteur.sn
Ronald Perraut, Email: Ronald.Perraut@pasteur.sn.
Aissatou Toure-Balde, Email: Aissatou.Toure@pasteur.sn.
References
- 1.WHO. World Malaria Report 2016. Geneva: World Health Organization, 2016. http://www.who.int/malaria/publications/world-malaria-report-2016/en/.
- 2.Battle KE, Gething PW, Elyazar IR, Moyes CL, Sinka ME, Howes RE, et al. The global public health significance of Plasmodium vivax. Adv Parasitol. 2012;80:1–111. doi: 10.1016/B978-0-12-397900-1.00001-3. [DOI] [PubMed] [Google Scholar]
- 3.Moreira CM, Abo-Shehada M, Price RN, Drakeley CJ. A systematic review of sub-microscopic Plasmodium vivax infection. Malar J. 2015;14:360. doi: 10.1186/s12936-015-0884-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anstey NM, Russell B, Yeo TW, Price RN. The pathophysiology of vivax malaria. Trends Parasitol. 2009;25:220–227. doi: 10.1016/j.pt.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 5.Gething PW, Elyazar IR, Moyes CL, Smith DL, Battle KE, Guerra CA, et al. A long neglected world malaria map: Plasmodium vivax endemicity in 2010. PLoS Negl Trop Dis. 2012;6:e1814. doi: 10.1371/journal.pntd.0001814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mendis K, Sina BJ, Marchesini P, Carter R. The neglected burden of Plasmodium vivax malaria. Am J Trop Med Hyg. 2001;64:97–106. doi: 10.4269/ajtmh.2001.64.97. [DOI] [PubMed] [Google Scholar]
- 7.Guerra CA, Snow RW, Hay SI. Mapping the global extent of malaria in 2005. Trends Parasitol. 2006;22:353–358. doi: 10.1016/j.pt.2006.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miller LH, Carter R. A review. Innate resistance in malaria. Exp Parasitol. 1976;40:132–146. doi: 10.1016/0014-4894(76)90075-8. [DOI] [PubMed] [Google Scholar]
- 9.Miller LH, Mason SJ, Clyde DF, McGinniss MH. The resistance factor to Plasmodium vivax in blacks. The Duffy-blood-group genotype, FyFy. NEJM. 1976;295:302–304. doi: 10.1056/NEJM197608052950602. [DOI] [PubMed] [Google Scholar]
- 10.Fru-Cho J, Bumah VV, Safeukui I, Nkuo-Akenji T, Titanji VP, Haldar K. Molecular typing reveals substantial Plasmodium vivax infection in asymptomatic adults in a rural area of Cameroon. Malar J. 2014;13:170. doi: 10.1186/1475-2875-13-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Menard D, Barnadas C, Bouchier C, Henry-Halldin C, Gray LR, Ratsimbasoa A, et al. Plasmodium vivax clinical malaria is commonly observed in Duffy-negative Malagasy people. Proc Natl Acad Sci USA. 2010;107:5967–5971. doi: 10.1073/pnas.0912496107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mendes C, Dias F, Figueiredo J, Mora VG, Cano J, de Sousa B, et al. Duffy negative antigen is no longer a barrier to Plasmodium vivax–molecular evidences from the African West Coast (Angola and Equatorial Guinea) PLoS Negl Trop Dis. 2011;5:e1192. doi: 10.1371/journal.pntd.0001192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ryan JR, Stoute JA, Amon J, Dunton RF, Mtalib R, Koros J, et al. Evidence for transmission of Plasmodium vivax among a duffy antigen negative population in Western Kenya. Am J Trop Med Hyg. 2006;75:575–581. [PubMed] [Google Scholar]
- 14.Wurtz N, Lekweiry KM, Bogreau H, Pradines B, Rogier C, Boukhary AO, Hafid JE, Salem MS, et al. Vivax malaria in Mauritania includes infection of a Duffy-negative individual. Malar J. 2011;10:336. doi: 10.1186/1475-2875-10-336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Niangaly A, Gunalan K, Ouattara A, Coulibaly D, Sa JM, Adams M, et al. Plasmodium vivax infections over 3 years in Duffy blood group negative Malians in Bandiagara, Mali. Am J Trop Med Hyg. 2017;97:744–752. doi: 10.4269/ajtmh.17-0254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abdallah TM, Abdeen MT, Ahmed IS, Hamdan HZ, Magzoub M, Adam I. Severe Plasmodium falciparum and Plasmodium vivax malaria among adults at Kassala Hospital, eastern Sudan. Malar J. 2013;12:148. doi: 10.1186/1475-2875-12-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rubio JM, Benito A, Roche J, Berzosa PJ, Garcia ML, Mico M, et al. Semi-nested, multiplex polymerase chain reaction for detection of human malaria parasites and evidence of Plasmodium vivax infection in Equatorial Guinea. Am J Trop Med Hyg. 1999;60:183–187. doi: 10.4269/ajtmh.1999.60.183. [DOI] [PubMed] [Google Scholar]
- 18.Gal S, Fidler C, Turner SU, Lo YD, Roberts DJ, Wainscoat JS. Detection of Plasmodium falciparum DNA in plasma. Ann N Y Acad Sci. 2001;945:234–238. doi: 10.1111/j.1749-6632.2001.tb03891.x. [DOI] [PubMed] [Google Scholar]
- 19.Snounou G, Viriyakosol S, Jarra W, Thaithong S, Brown KN. Identification of the four human malaria parasite species in field samples by the polymerase chain reaction and detection of a high prevalence of mixed infections. Mol Biochem Parasitol. 1993;58:283–292. doi: 10.1016/0166-6851(93)90050-8. [DOI] [PubMed] [Google Scholar]
- 20.Culleton RL, Mita T, Ndounga M, Unger H, Cravo PV, Paganotti GM, et al. Failure to detect Plasmodium vivax in West and Central Africa by PCR species typing. Malar J. 2008;7:174. doi: 10.1186/1475-2875-7-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daniels RF, Deme AB, Gomis JF, Dieye B, Durfee K, Thwing JI, et al. Evidence of non-Plasmodium falciparum malaria infection in Kedougou, Senegal. Malar J. 2017;16:9. doi: 10.1186/s12936-016-1661-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Niang M, Thiam LG, Sow A, Loucoubar C, Bob NS, Diop F, et al. A molecular survey of acute febrile illnesses reveals Plasmodium vivax infections in Kedougou, southeastern Senegal. Malar J. 2015;14:281. doi: 10.1186/s12936-015-0808-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Russo G, Faggioni G, Paganotti GM, Dongho GBD, Pomponi A, De Santis R, et al. Molecular evidence of Plasmodium vivax infection in Duffy negative symptomatic individuals from Dschang, West Cameroon. Malar J. 2017;16:74. doi: 10.1186/s12936-017-1722-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Niang M, Loucoubar C, Sow A, Diagne MM, Faye O, Diallo M, et al. Genetic diversity of Plasmodium falciparum isolates from concurrent malaria and arbovirus co-infections in Kedougou, southeastern Senegal. Malar J. 2016;15:155. doi: 10.1186/s12936-016-1208-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sow A, Loucoubar C, Diallo D, Faye O, Ndiaye Y, Senghor CS, et al. Concurrent malaria and arbovirus infections in Kedougou, southeastern Senegal. Malar J. 2016;15:47. doi: 10.1186/s12936-016-1100-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.PNLP. Bulletin Epidemiologique Annuel du Paludisme au Senegal. Programme National de Lutte contre le Paludisme. 2015; p. 24.
- 27.Bonnet S, Petres S, Holm I, Fontaine T, Rosario S, Roth C, et al. Soluble and glyco-lipid modified baculovirus Plasmodium falciparum C-terminal merozoite surface protein 1, two forms of a leading malaria vaccine candidate. Vaccine. 2006;24:5997–6008. doi: 10.1016/j.vaccine.2006.04.069. [DOI] [PubMed] [Google Scholar]
- 28.Polson HE, Conway DJ, Fandeur T, Mercereau-Puijalon O, Longacre S. Gene polymorphism of Plasmodium falciparum merozoite surface proteins 4 and 5. Mol Biochem Parasitol. 2005;142:110–115. doi: 10.1016/j.molbiopara.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 29.Pizarro JC, Chitarra V, Verger D, Holm I, Petres S, Dartevelle S, et al. Crystal structure of a Fab complex formed with PfMSP1-19, the C-terminal fragment of merozoite surface protein 1 from Plasmodium falciparum: a malaria vaccine candidate. J Mol Biol. 2003;328:1091–1103. doi: 10.1016/S0022-2836(03)00376-0. [DOI] [PubMed] [Google Scholar]
- 30.Aribot G, Rogier C, Sarthou JL, Trape JF, Balde AT, Druilhe P, et al. Pattern of immunoglobulin isotype response to Plasmodium falciparum blood-stage antigens in individuals living in a holoendemic area of Senegal (Dielmo, west Africa) Am J Trop Med Hyg. 1996;54:449–457. doi: 10.4269/ajtmh.1996.54.449. [DOI] [PubMed] [Google Scholar]
- 31.Diop F, Diop G, Niang M, Diouf B, Ndiaye D, Richard V, et al. The value of local malaria strains for serological studies: local strains versus Palo Alto reference strain. Malar J. 2015;14:229. doi: 10.1186/s12936-015-0734-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Perraut R, Guillotte M, Drame I, Diouf B, Molez JF, Tall A, et al. Evaluation of anti-Plasmodium falciparum antibodies in Senegalese adults using different types of crude extracts from various strains of parasite. Microb Infect. 2002;4:31–35. doi: 10.1016/S1286-4579(01)01506-4. [DOI] [PubMed] [Google Scholar]
- 33.Diop F, Richard V, Diouf B, Sokhna C, Diagne N, Trape JF, et al. Dramatic declines in seropositivity as determined with crude extracts of Plasmodium falciparum schizonts between 2000 and 2010 in Dielmo and Ndiop, Senegal. Malar J. 2014;13:83. doi: 10.1186/1475-2875-13-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Perraut R, Marrama L, Diouf B, Sokhna C, Tall A, Nabeth P, et al. Antibodies to the conserved C-terminal domain of the Plasmodium falciparum merozoite surface protein 1 and to the merozoite extract and their relationship with in vitro inhibitory antibodies and protection against clinical malaria in a Senegalese village. J Infect Dis. 2005;191:264–271. doi: 10.1086/426398. [DOI] [PubMed] [Google Scholar]
- 35.Perraut R, Richard V, Varela ML, Trape JF, Guillotte M, Tall A, et al. Comparative analysis of IgG responses to Plasmodium falciparum MSP1p19 and PF13-DBL1alpha1 using ELISA and a magnetic bead-based duplex assay (MAGPIX(R)-Luminex) in a Senegalese meso-endemic community. Malar J. 2014;13:410. doi: 10.1186/1475-2875-13-410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bharti AR, Patra KP, Chuquiyauri R, Kosek M, Gilman RH, Llanos-Cuentas A, et al. Polymerase chain reaction detection of Plasmodium vivax and Plasmodium falciparum DNA from stored serum samples: implications for retrospective diagnosis of malaria. Am J Trop Med Hyg. 2007;77(3):444–446. [PubMed] [Google Scholar]
- 37.Gautret P, Legros F, Koulmann P, Rodier MH, Jacquemin JL. Imported Plasmodium vivax malaria in France: geographical origin and report of an atypical case acquired in Central or Western Africa. Acta Trop. 2001;78:177–181. doi: 10.1016/S0001-706X(00)00181-9. [DOI] [PubMed] [Google Scholar]
- 38.Cavasini CE, Mattos LC, Couto AA, Bonini-Domingos CR, Valencia SH, Neiras WC, et al. Plasmodium vivax infection among Duffy antigen-negative individuals from the Brazilian Amazon region: an exception? Trans R Soc Trop Med Hyg. 2007;101:1042–1044. doi: 10.1016/j.trstmh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 39.Woldearegai TG, Kremsner PG, Kun JF, Mordmüller B. Plasmodium vivax malaria in Duffy-negative individuals from Ethiopia. Trans R Soc Trop Med Hyg. 2013;107:328–331. doi: 10.1093/trstmh/trt016. [DOI] [PubMed] [Google Scholar]
- 40.Mbenda HGN, Das A. Molecular evidence of Plasmodium vivax mono and mixed malaria parasite infections in Duffy-negative native Cameroonians. PLoS ONE. 2014;9:e103262. doi: 10.1371/journal.pone.0103262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fowkes FJ, Richards JS, Simpson JA, Beeson JG. The relationship between anti-merozoite antibodies and incidence of Plasmodium falciparum malaria: a systematic review and meta-analysis. PLoS Med. 2010;7:e1000218. doi: 10.1371/journal.pmed.1000218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Richards JS, Arumugam TU, Reiling L, Healer J, Hodder AN, Fowkes FJ, et al. Identification and prioritization of merozoite antigens as targets of protective human immunity to Plasmodium falciparum malaria for vaccine and biomarker development. J Immunol. 2013;191:795–809. doi: 10.4049/jimmunol.1300778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.van den Hoogen LL, Griffin JT, Cook J, Sepulveda N, Corran P, Conway DJ, et al. Serology describes a profile of declining malaria transmission in Farafenni, The Gambia. Malar J. 2015;14:416. doi: 10.1186/s12936-015-0939-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Amanfo SA, Mduluza T, Midzi N, Cavanagh DR, Mutapi F. Seroepidemiology of Plasmodium species infections in Zimbabwean population. Malar J. 2016;15:267. doi: 10.1186/s12936-016-1325-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chitarra V, Holm I, Bentley GA, Petres S, Longacre S. The crystal structure of C-terminal merozoite surface protein 1 at 1.8 Å resolution, a highly protective malaria vaccine candidate. Mol Cell. 1999;3:457–464. doi: 10.1016/S1097-2765(00)80473-6. [DOI] [PubMed] [Google Scholar]
- 46.del Portillo HA, Longacre S, Khouri E, David PH. Primary structure of the merozoite surface antigen 1 of Plasmodium vivax reveals sequences conserved between different Plasmodium species. Proc Natl Acad Sci USA. 1991;88:4030–4034. doi: 10.1073/pnas.88.9.4030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dodoo D, Aikins A, Kusi KA, Lamptey H, Remarque E, Milligan P, et al. Cohort study of the association of antibody levels to AMA1, MSP119, MSP3 and GLURP with protection from clinical malaria in Ghanaian children. Malar J. 2008;7:142. doi: 10.1186/1475-2875-7-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Perera KL, Handunnetti SM, Holm I, Longacre S, Mendis K. Baculovirus merozoite surface protein 1 C-terminal recombinant antigens are highly protective in a natural primate model for human Plasmodium vivax malaria. Infect Immun. 1998;66:1500–1506. doi: 10.1128/iai.66.4.1500-1506.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kerkhof K, Sluydts V, Heng S, Kim S, Pareyn M, Willen L, et al. Geographical patterns of malaria transmission based on serological markers for falciparum and vivax malaria in Ratanakiri, Cambodia. Malar J. 2016;15:510. doi: 10.1186/s12936-016-1558-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Koffi D, Varela ML, Loucoubar C, Beourou S, Vigan-Womas I, Toure AO, et al. Longitudinal analysis of antibody responses in symptomatic malaria cases do not mirror parasite transmission in peri-urban area of Côte d’Ivoire between 2010 and 2013. PLoS ONE. 2017;12:e0172899. doi: 10.1371/journal.pone.0172899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Perraut R, Varela ML, Loucoubar C, Niass O, Sidibe A, Tall A, et al. Serological signatures of declining exposure following intensification of integrated malaria control in two rural Senegalese communities. PLoS ONE. 2017;12:e0179146. doi: 10.1371/journal.pone.0179146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Culleton R, Ndounga M, Zeyrek FY, Coban C, Casimiro PN, Takeo S, et al. Evidence for the transmission of Plasmodium vivax in the Republic of the Congo, West Central Africa. J Infect Dis. 2009;200:1465–1469. doi: 10.1086/644510. [DOI] [PubMed] [Google Scholar]
- 53.Poirier P, Doderer-Lang C, Atchade PS, Lemoine JP, de l’Isle MLC, Abou-Bacar A, et al. The hide and seek of Plasmodium vivax in West Africa: report from a large-scale study in Beninese asymptomatic subjects. Malar J. 2016;15:570. doi: 10.1186/s12936-016-1620-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Drakeley C, Cook J. Chapter 5. Potential contribution of sero-epidemiological analysis for monitoring malaria control and elimination: historical and current perspectives. Adv Parasitol. 2009;69:299–352. doi: 10.1016/S0065-308X(09)69005-9. [DOI] [PubMed] [Google Scholar]
- 55.Satoguina J, Walther B, Drakeley C, Nwakanma D, Oriero EC, Correa S, et al. Comparison of surveillance methods applied to a situation of low malaria prevalence at rural sites in The Gambia and Guinea Bissau. Malar J. 2009;8:274. doi: 10.1186/1475-2875-8-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bousema T, Griffin JT, Sauerwein RW, Smith DL, Churcher TS, Takken W, et al. Hitting hotspots: spatial targeting of malaria for control and elimination. PLoS Med. 2012;9:e1001165. doi: 10.1371/journal.pmed.1001165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Takem EN, Affara M, Amambua-Ngwa A, Okebe J, Ceesay SJ, Jawara M, et al. Detecting foci of malaria transmission with school surveys: a pilot study in the Gambia. PLoS ONE. 2013;8:e67108. doi: 10.1371/journal.pone.0067108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shute PG, Lupascu GH, Branzei P, Maryon M, Constantinescu P, Bruce-Chwatt LJ, et al. A strain of Plasmodium vivax characterized by prolonged incubation: the effect of numbers of sporozoites on the length of the prepatent period. Trans R Soc Trop Med Hyg. 1976;70:474–481. doi: 10.1016/0035-9203(76)90132-2. [DOI] [PubMed] [Google Scholar]
- 59.Bousema T, Drakeley C, Gesase S, Hashim R, Magesa S, Mosha F, et al. Identification of hot spots of malaria transmission for targeted malaria control. J Infect Dis. 2010;201:1764–1774. doi: 10.1086/652456. [DOI] [PubMed] [Google Scholar]


