Abstract
Background
Application of objective measurement of stroke gait with accelerometer-based wearable technology and associated algorithms is increasing, despite reports questioning the accuracy of this technique in quantifying specific stroke-related gait impairments. The aim of this study is to determine the feasibility, validity and reliability of a low-cost open-source system incorporating algorithms and a single tri-axial accelerometer-based wearable to quantify gait characteristics in the laboratory and community post-stroke.
Methods
Twenty-five participants with stroke wore the wearable (AX3, Axivity) on the lower back during a laboratory 2 minute continuous walk (preferred pace) on two occasions a week apart and continuously in the community for two consecutive 7 day periods. Video, instrumented walkway (GaitRite) and an OPAL accelerometer-based wearable were used as laboratory references.
Results
Feasibility of the proposed system was good. The system was valid for measuring step count (ICC 0.899). Inherent differences in gait quantification between algorithm and GaitRite resulted in difficulties comparing agreement between the different systems. Agreement was moderate-excellent (ICC 0.503–0.936) for mean and variability gait characteristics vs. OPAL. Agreement was moderate-poor between the system and OPAL for asymmetry characteristics. Moderate-excellent reliability (ICC 0.534–0.857) was demonstrated for 11/14 laboratory measured gait characteristics. Community test-retest reliability was good-excellent (ICC 0.867–0.983) for all except one (ICC 0.699) of the 19 gait characteristics.
Conclusion
The proposed system is a low-cost, reliable tool for quantifying gait post-stroke with multiple potential applications. Further refinement to optimise gait quantification algorithms for certain gait characteristics including gait asymmetry is required.
Keywords: Stroke, Gait, Physical activity, Reliability, Validity, Accelerometer
Background
Gait impairments such as reduced gait speed and temporal asymmetry are common after stroke, limiting community ambulation [1] and physical activity [2]. Reduced physical activity predisposes this at-risk population to increased morbidity, stroke recurrence, and further cardiometabolic disease [3].
Quantification of gait after stroke via examination of spatio-temporal characteristics (e.g. step length and velocity, which, in relation to gait outcomes (see below), we term ‘micro’ characteristics [4]) commonly occurs in a gait laboratory. Laboratory testing relies on expensive equipment and technical support, limiting data capture to specialist centres and analysis to a sparse number of gait cycles that are produced under highly controlled conditions. In clinical practice when laboratory facilities are not available, functional measures such as the ten metre walk test [5] and the Dynamic Gait Index [6] are commonly used to measure gait after stroke [5]. These approaches are limited however for three key reasons: measures of gait velocity and function may not detect gait quality or asymmetry; one-off testing in a controlled environment does not inform about day to day variability in performance or the challenges of real-world walking and visual observation and stop watch timing can be limited by observer error. Instrumented walkways such as the GaitRite system are another potential method of measuring gait via a pressure sensitive mat that detects footfall location and timing during walking [7]. Electronic measurement with the GaitRite system reduces observer bias and the system has been shown to have good to excellent intra and inter-rater reliability in sub-acute stroke [8]. One-off testing with the GaitRite system however prohibits understanding of community walking.
The use of accelerometer-based wearable technology (wearables) to quantify micro gait characteristics has gained popularity in stroke research with open-source, data processing platforms facilitating ease of application [9, 10]. Wearable technology offers a low-cost method of quantifying gait in the clinic and can reduce the bias of manual recording techniques [11]. In the community wearable technology can be used to increase ecological validity and reduce observer bias and attentional compensation associated with clinic testing [12].
Capturing levels of physical activity is also possible using wearables [13] and this field appears more advanced in stroke research than measurement of spatio-temporal features of gait which is, by comparison, novel. Traditionally, physical activity outcomes that describe the ‘volume’ of activity after stroke such as step count are reported [14] but these have now been extended to include more nuanced and informative outcomes such as the pattern and variability of activity [15, 16]. We refer to this grouping of volume, pattern and variability physical activity measures as ‘macro’ gait outcomes [4].
Research examining the application of wearables to measure micro and macro gait outcomes in stroke is emerging [17–21]. Although this application of wearable technology is promising, a number of potential problems require consideration for future use of wearable technology in stroke. Potential problems include: application of inertial measurement units with short battery lives necessitating regular recharging (limiting community application) [22]; use of multiple wearables resulting in a high researcher/participant burden [4]; use of engineering terminology to describe gait measures reducing clinical application [4] and validation against manual recording techniques leading to potential bias [21]. The hemiparetic gait pattern adds a further challenge to development of accurate algorithms for detection and processing of discrete spatio-temporal features such as step asymmetry [17]. Also, to date research has focused on measuring either physical activity or spatio-temporal aspects of gait, rather than integrating both which would allow for more targeted rehabilitation approaches. The use of a single wearable that could capture both spatio-temporal and physical activity aspects of gait over time in the community could address some of the problems highlighted above. Previous work has demonstrated the feasibility of instrumenting gait with a single wearable positioned on the fifth lumbar vertebrae [23, 24]. This location enables the optimal functionality of the algorithms selected for both spatio-temporal and physical activity aspects of gait in healthy participants. This functionality however, has not been confirmed in stroke where pathological gait is commonly observed.
The aims of this study were to determine the feasibility, reliability and validity of a low-cost open-source system, incorporating algorithms and a single tri-axial accelerometer-based wearable (AX3), to comprehensively quantify gait in terms of both spatio-temporal (micro) and physical activity (macro) outcomes in the laboratory and community post-stroke.
Methods
Study design: Cross-sectional (Time point 1 and Time point 2) and observational/longitudinal (Week 1 and Week 2).
Setting: Gait laboratory, Clinical Ageing Research Unit, Campus for Ageing and Vitality, Newcastle upon Tyne and community settings in North East England.
Participants: Inclusion criteria
Community dwelling stroke survivor; at least 1 month post-stroke onset; mild to moderate gait deficit defined by clinical observation of asymmetry of gait including reduced stance time, increased swing time in the affected limb and/or reduced gait speed/balance problems; no changes in gait-related ability over the past month based on self-report and able to walk 10 m with/without a stick (cane or quadropod cane). Exclusion criteria: medical problems other than stroke impacting on gait e.g. osteoarthritis. Participants were recruited via advertisement or therapist referral. All eligible participants were consecutively invited to participate in the study. The study was approved by the Greater Manchester West Research and Ethics Committee. All subjects gave informed written consent for the study according to the Declaration of Helsinki.
Demographic and clinical measures
Participant age, gender, date of stroke, stroke type (Oxford Community Stroke Project Classification [25]), stroke impairment (National Institute of Health Stroke Scale [26] hemiplegia (clinical observation by two independent experienced clinicians), walking stick use, ankle foot orthosis (AFO) use, height and weight were recorded at baseline.
Test protocol for laboratory-based outcomes
Participants were asked to walk for 2 minutes continuously around a 25 m track at self-selected speed in a laboratory instrumented with a GaitRite system whilst wearing an AX3 wearable (see instrumentation) affixed with double sided tape and Hypafix (BSN Medical Limited, Hull, UK) at the fifth lumbar vertebrae (L5). A continuous rather than intermittent walk was chosen based on previous methodological findings [27].
Validity
Three tools were used during the walking trial to establish the validity of the AX3 wearable: GaitRite instrumented walkway; high grade wearable data capture system (OPAL, APDM) and video (to facilitate manual step count checking and visual inspection of stroke related impairment). The GaitRite mat was placed in the 25 m circuit (see instrumentation and Fig. 1) to allow measurement of the spatio-temporal aspects of gait. The single wireless OPAL device was affixed directly adjacent to the AX3 at L5 and held in place by double sided tape and Hypafix (see instrumentation).
Fig. 1.
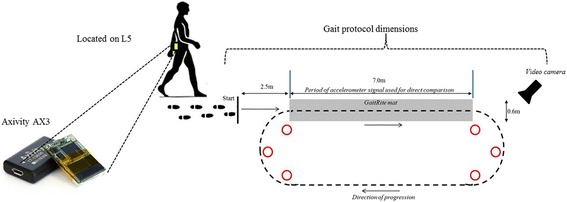
Clinic protocol and positioning of AX3 wearable
Test-retest reliability
Test-retest reliability of the AX3 was established by repeating the walking trial 1 week later (± 2 days) and comparing measures taken at the first walking trial (T1) with the second (T2). Walking aid and AFO conditions were matched over trials.
Test protocol for community-based outcomes
In order to assess feasibility and test-retest reliability of the AX3 wearable in the community participants were asked to wear the AX3 wearable for two consecutive 7 day periods. After completing the laboratory protocol at T1 participants were provided with an AX3 wearable to wear for 7 days in the community (Week 1). The wearable was worn continuously except for skin cleaning or during bathing/swimming (the wearable was water resistant but not waterproof). Participants, or a family member who could assist, were instructed how to remove and reattach the wearable. The data from the wearable was downloaded on the participants return to the clinic at T2. The participants were then asked to wear the wearable for a second consecutive 7 days (Week 2). The wearable was returned by participants in a pre-paid envelope and data downloaded. During the 2 week measurement period participants completed a daily log of daily activities wear time and any problems with the wearable. This log was reviewed at T2 clinic appointment and each participant was questioned on comfort and application of the wearable. This data was used alongside wearable data capture to assess feasibility.
Instrumentation
Low-cost wearable
The AX3 is a single tri-axial accelerometer-based wearable (AX3, Axivity, York, UK https://axivity.com/, cost ≈£100, dimensions 23.0 mm × 32.5 mm × 7.6 mm). The AX3 weighs 11 g, has a memory of 512 Mb and a battery life of 14 days. AX3 data capture is 100 Hz (16-bit resolution) at a range of ±8 g. Recorded AX3 accelerations were stored locally on the device’s internal memory and downloaded upon the completion of each walking trial.
Video
A Samsung W200, 25 Hz video camera was used to record walking trials to allow visual inspection for manual counting of steps within the gait task and visual observation of asymmetry.
Instrumented walkway
Dimensions were 7.0 m × 0.6 m and had a spatial accuracy of 1.27 cm and a temporal accuracy of one sample (240 Hz, ~4.17 ms) (GaitRite: Platinum model GaitRite, software version 4.5, CIR systems, NJ, USA). Gaitrite has been used extensively in the quantification of spatio-temporal measures in stroke [8, 28].
High-cost wearable system The OPAL wireless accelerometer-based wearable system (APDM, Inc., Portland, OR, USA, https://www.apdm.com/wearable-sensors) comprises a tri-axial accelerometer, gyroscope and magnetometer [18] (128 Hz, 8Gb, 16 h of logging 8 h of streaming). The OPAL system has been used previously in stroke for quantification of spatio-temporal measures [18, 20]. Only accelerometer data were used in the analysis.
Data synchronisation
Video, GaitRite and OPAL were synchronised in time with the AX3 recordings. The quartz-stabilized real-time clock of the AX3 and OPAL systems (accuracy: 20 ppm) were synchronized with the computer used for the GaitRite recordings, and for each walking trial, the start and stop time were recorded by the assessor. Start and stop times were subsequently input to a bespoke MATLAB program that automatically segmented and analysed the accelerometer data. AX3 and OPAL data corresponding to steps leading to and after contact with the GaitRite were excluded from analysis so a direct comparison could be made between the wearables and instrumented walkway.
Wearable algorithms
Micro (spatio-temporal) outcomes
The 14 temporal and spatial gait characteristics defined by Lord et al. (2013) [29] were quantified from the AX3 and OPAL wearables and GaitRite. Mean gait values were calculated for step time, stance time, (time stance foot was in contact with the ground for a given stride), swing time (duration a foot was not in contact with the ground for a given stride), step length and step velocity. The standard deviation from all steps was calculated to determine step variability. Asymmetry was calculated as the absolute difference between consecutive left and right steps. Algorithm and data segmentation techniques applied to both the AX3 and the OPAL data and rationale have been described in full previously [9]. In brief the vertical acceleration underwent continuous wavelet transformation to estimate initial contact and final contact in the gait cycle while the inverted pendulum model was used in conjunction with those outcomes for spatial data.
Macro (physical activity) outcomes
A validated free-living algorithm [30] was used to quantify macro characteristics (e.g. volume, pattern and variability) Volume was quantified as total daily step count. Pattern was quantified as number of daily walking bouts (minimum bout length defined as three steps [31]), mean length of walking bouts (s) and alpha (α) as the distribution of ambulatory bouts (a lower α indicates that the distribution is derived from a greater proportion of longer bouts [32, 33]). Variability was described as the within subject variability of bout length calculated from the maximum likelihood technique due to non-normality of data [34]. A high variability indicates a more varied pattern of walking.
Statistical analysis
Analysis was completed using SPSS v23 (IBM). Normality of data was tested with a Shapiro-Wilk test. Descriptive statistics (median and interquartile range) were calculated for gait characteristics measured by AX3 and OPAL wearables and GaitRite. Bland-Altman plots were used to visually check for non-linear or heteroscedastic distributions of error between AX3 and clinic references. Data for two participants who wore a fixed plastic AFO were removed from the analysis as individual data analysis (including video observations) revealed the algorithms applied were not appropriate for these two participants. This finding was likely due to fixed nature of the AFO impacting on heel strike and the performance of the algorithm which was developed based on the detection of initial and final contact within the gait cycle. Individuals who wore a push aequi AFO were able to achieve some degree of plantarflexion therefore were included in the analysis.
Agreement between AX3 measurements and video, OPAL and GaitRite and on AX3 measures at T1 compared with T2 were formally tested using intraclass correlation coefficient, Spearman’s rank correlation coefficients (r) and limits of agreement (LoA) expressed as a percentage of the mean of the two measures and the 95% LoA.
For all analysis statistical significance was set at p < 0.05. Predefined acceptance ratings for ICCs were set at excellent (≥.900, 0.0–4.9%), good (0.750–0.899, 5.0–9.9%), moderate (0.500–0.749, 10.0–49.9%) and poor (<0.500, >50.0%) [35].
Participant characteristics
Participant demographic and clinical data are shown in Table 1. The sample had a heterogeneous mix of gait speeds (range 0.14–1.4 m/s). Video observation of participants by two experienced clinicians showed 15 of the 23 participants (65%) had marked hemiplegia (moderate to severe) impacting on gait symmetry.
Table 1.
Participant characteristics
| Demographics (n = 25) | |
| Gender (male/female) | 19/4 |
| Age (years) | 63 ± 11 |
| Stroke characteristics | |
| Time since stroke (months) | 66 ± 48 (range 5–201) |
| Stroke subtype (OCSP) | |
| Total anterior circulation | 11 |
| Partial anterior circulation | 6 |
| Lacunar | 3 |
| Posterior circulation | 3 |
| Stroke impairment (number (%)) | |
| NIHSS score (0–40) | 4 ± 3 (range 0–11) |
| NIHSS lower limb score (0–4) | 1 ± 0.7 (range 0–3) |
| Walking speed (m/s) | 0. 9 ± 0.4 |
| Marked Hemiplegia (Yes/No) | 15/8 |
| Walking aid | 3 (13%) |
| Push Aequi ankle foot orthosis | 4 (17%) |
OCSP Oxford community Stroke Project, % Percentage, NIHSS National Institute for Health Stroke Scale
Results
Laboratory-based measures Feasibility
25/25 participants completed the testing protocol with no adverse events or AX3 wearable missing data. We were able to quantify all fourteen spatio-temporal gait characteristics in all 23 participants included in the analysis.
Validity (AX3 wearable system vs. clinic references)
Absolute agreement between AX3 wearable and video step count was good (median 210 (interquartile range 41) vs. 206 (36), median difference 4 (2%), ICC 0.899, P ≤ 0.01, LoA expressed as a percentage of the mean of the two measures 0.4 (95% LoA 49.6, −38.6).
Table 2 demonstrates agreement for spatio-temporal measurement between AX3 wearable system and two references (GaitRite and OPAL). Absolute agreement between the system and GaitRite was moderate to good for mean step velocity, step time, stance time, step time and stance time variability (ICCs 0.724–0.802) but poor for all other micro characteristics. Absolute agreement between the system and OPAL was moderate to excellent for all mean and variability characteristics and swing and stance time asymmetry (ICCs 0.504–0.974) but poor for step length and step time asymmetry. Overall agreement between the system and references was superior for mean and variability characteristics compared with asymmetry characteristics.
Table 2.
Laboratory based agreement between AX3 wearable system, Gait Rite and OPAL for micro gait characteristics
| Variable | AX3 wearable system vs. GaitRite | AX3 wearable system vs. OPAL | ||||
|---|---|---|---|---|---|---|
| ICC | r | LoA % (95% LoA) | ICC | r | LoA % (95% LoA) | |
| Micro gait characteristics | ||||||
| Mean | ||||||
| Step velocity (m/s) | 0.744** | 0.632** | 1.1 (0.06, −0.043) | 0.923** | 0.871** | 0.4 (0.19, 0.22) |
| Step length (m) | −0.411 | 0.035 | 1.5 (0.56, −0.35) | 0.831** | 0.784** | 0.6 (0.22, −0.18) |
| Step time (s) | 0.797** | 0.917** | 1.1 (0.38, −0.38) | 0.890** | 0.948** | 0.6 (0.25, −0.17) |
| Swing time (s) | 0.431* | 0.558** | 1.3 (0.40, −0.21) | 0.900** | 0.944** | 0.8 (0.22, −0.17) |
| Stance time (s) | 0.758** | 0.902** | 1.2 (0.50, −0.60) | 0.876** | 0.871** | 0.6 (0.28, −0.17) |
| Variability | ||||||
| Step velocity (m/s) | 0.052 | 0.261 | 3.8 (0.28, −0.05) | 0.658** | 0.503* | 2.1 (0.17, −0.23) |
| Step length (m) | 0.457** | 0.121 | 2.9 (0.175,-0.036) | 0.884** | 0.616** | 1.6 (0.08, −0.104) |
| Step time (s) | 0.802** | 0.688** | 4.5 (0.25, −0.13) | 0.972** | 0.940** | 1.6 (0.09, −0.10) |
| Swing time (s) | 0.389 | 0.694** | 6.4 (0.33, −0.15) | 0.968** | 0.928** | 1.7 (0.1, −0.11) |
| Stance time (s) | 0.724** | 0.766** | 4.3 (0.26, −0.12) | 0.974** | 0.936** | 1.5 (0.09, −0.11) |
| Asymmetry | ||||||
| Step length (m) | 0.442 | 0.001 | 4.5 (0.25, −0.18) | 0.464 | 0.381 | 3.6 (0.2, −0.22) |
| Step time (s) | 0.178 | 0.601** | 3.9 (0.49, −0.75) | 0.492* | 0.558** | 4 (0.13, −0.08) |
| Swing time (s) | 0.320 | 0.454* | 6.7 (0.23, −0.33) | 0.539* | 0.733** | 4.7 (0.13, −0.08) |
| Stance time (s) | 0.439 | 0.570** | 6 (0.216, −0.30) | 0.504* | 0.592** | 4.9 (0.15, −0.09) |
Vs. versus, ICC Intraclass correlation coefficient, r Spearman’s rank correlation coefficient, LoA% limits of agreement as a percentage of the mean of the two systems
**p ≤ 0.01 *p ≤ 0.05
Reliability
Table 3 demonstrates the agreement between laboratory AX3 wearable system micro outcome measurement (T1 vs. T2). Absolute agreement was moderate to excellent (ICCs 0.534–0.858) for all measures except mean step length, step velocity variability and step length asymmetry. Relative agreement was moderate to excellent (r 0.525–0.941) for all measure except step velocity variability and step length asymmetry.
Table 3.
Laboratory based test-retest reliability (1 week apart) for AX3 wearable system micro gait measurement
| Variable | Median (IQR) | Correlations/agreements | ||||
|---|---|---|---|---|---|---|
| Time point 1 | Time point 2 | Median difference (%) | ICC | LoA % (95% LoA) | r | |
| Mean | ||||||
| Step velocity (m/s) | 1.08 (0.40) | 1.08 (0.345) | 0 (0%) | 0.534* | 1.0 (0.34, −0.30) | 0.547** |
| Step length (m) | 0.657 (0.113) | 0.642 (0.140) | −0.015 (−2%) | 0.419 | 1.0 (0.31, −0.32) | 0.572** |
| Step time (s) | 0.600 (0.130) | 0.601 (0.123) | −0.001(0.2%) | 0.844** | 1.0 (0.28, −0.3) | 0.941** |
| Swing time (s) | 0.485 (0.174) | 0.467 (0.117) | −0.018 (−4%) | 0.858** | 1.0 (0.24, −0.28) | 0.926** |
| Stance time (s) | 0.743 (0.136) | 0.740 (0.130) | −0.003 (−0.4%) | 0.819** | 0.78 (0.32, −0.34) | 0.930** |
| Variability | ||||||
| Step velocity (m/s) | 0.150 (0.053) | 0.162 (0.130) | 0.012 (7%) | 0.343 | 3.7 (0.33, −0.26) | 0.427* |
| Step length (m) | 0.082 (0.077) | 0.123 (0.131) | 0.041 (33%) | 0.632** | 2.8 (0.21, −0.13) | 0.693** |
| Step time (s) | 0.056 (0.097) | 0.082 (0.208) | 0.026 (32%) | 0.777** | 4.17 (0.36, −0.24) | 0.886** |
| Swing time (s) | 0.063 (0.098) | 0.082 (0.168) | 0.019 (23%) | 0.793** | 4.1(0.33, −0.23) | 0.901** |
| Stance time (s) | 0.062 (0.104) | 0.087 (0.195) | 0.025 (29%) | 0.784** | 4 (0.36, −0.24) | 0.909** |
| Asymmetry | ||||||
| Step length (m) | 0.084 (0.216) | 0.106 (0.125) | 0.022 (21%) | −0.194 | 5.1 (0.36, −0.32) | 0.015 |
| Step time (s) | 0.045 (0.085) | 0.036 (0.077) | 0.009 (25%) | 0.813** | 3.6 (0.14, −0.12) | 0.628** |
| Swing time (s) | 0.044 (0.077) | 0.035 (0.082) | −0.009 (26%) | 0.857** | 3.3 (0.12, −0.10) | 0.545** |
| Stance time (s) | 0.045 (0.087) | 0.042 (0.075) | −0.003 (7%) | 0.857** | 3.2 (0.11, −0.11) | 0.525** |
T1 Time point 1, T2 Time point 2, IQR Interquartile range, ICC Intraclass correlation coefficient, LoA% limits of agreement as a percentage of the mean of the two systems, r Spearman’s rank correlation coefficient
**p ≤ 0.01 *p ≤ 0.05
Community based outcomes
Feasibility
25/25 participants completed the community free living protocol 24 h a day for 7 days, only removing to bathe. There were no missing data sets. The AX3 battery life lasted for over the seven-day monitoring period. Participant logs and questioning during clinic visits indicated participants found the AX3 monitor comfortable to wear and easy to apply. Participants with upper limb impairment reported they either got an informal carer to assist with the application or managed an adapted technique of application with one arm.
Table 4 demonstrates agreement between community habitual physical activity and spatio-temporal measurement by AX3 wearable system (Week 1 vs. Week 2). Absolute agreement was moderate to excellent for all measures (ICCs 0.668–0.982).
Table 4.
Community based test-retest reliability for AX3 wearable system micro and micro gait measurement
| Variables | Median (IQR) | Agreement | ||||
|---|---|---|---|---|---|---|
| Week 1 | Week 2 | Median difference (%) | ICC | LoA % (95% LoA) | r | |
| Macro characteristics | ||||||
| Total daily step count | 7825 (6428) | 7191 (5920) | −634 (−9%) | 0.917** | 0.9 (3138, −4470) | 0.892** |
| Mean walking bout length (s) | 17.12 (2.56) | 16.3 (6.2) | −0.82 (−5%) | 0.919** | 0.4 (3.036, −3.565) | 0.894** |
| Total number of daily walking bouts | 535 (288) | 462 (237) | −73 (16) | 0.867** | 2 (226,-272) | 0.823** |
| Alpha (unit less) | 1.614 (0.535) | 1.615 (0.068) | 0.001 (0.06) | 0.948** | 0.1 (0.05, −0.046) | 0.853** |
| Variability (s) | 0.840 (0.057) | 0.842 (0.105) | 0.002 (0.2%) | 0.887** | 0.2 (0.08, −0.094) | 0.801** |
| Micro characteristics | ||||||
| Mean | ||||||
| Step velocity (m/s) | 1.05 (0.165) | 1.07 (0.152) | 0.02 (1.9) | 0.958** | 0.17 (0.087, −0.093) | 0.914** |
| Step length (m) | 0.610 (0.085) | 0.610 (0.085) | 0 (0) | 0.969** | 1.2 (0.034, −0.038) | 0.940** |
| Step time (s) | 0.613 (0.353) | 0.622 (0.38) | 0.009 (1) | 0.951** | 0.07(0.022, −0.018) | 0.889** |
| Swing time (s) | 0.474 (0.032) | 0.475 (0.030) | 0.001 (0.2) | 0.962** | 0.07 (0.02,-0.013) | 0.925** |
| Stance time (s) | 0.764 (0.040) | 0.766 (0.047) | 0.002 (0.2) | 0.942** | 0.1 (0.026, −0.026 | 0.863** |
| Variability | ||||||
| Step velocity (m/s) | 0.385 (0.048) | 0.383 (0.042) | −0.002 (−0.5) | 0.905** | 0.2 (0.04, −0.0345) | 0.914** |
| Step length (m) | 0.162 (0.021) | 0.159 (0.017) | 0.003 (−2%) | 0.944** | 0.12 (0.034, −0.0384) | 0.940** |
| Step time (s) | 0.183 (0.041) | 0.181 (0.044) | −0.002 (−1) | 0.982** | 0.17 (0.018, −0.0149) | 0.889** |
| Swing time (s) | 0.152 (0.040) | 0.150 (0.039) | −0.002 (−1.3) | 0.983** | 0.15 (0.0119,-0.0113) | 0.925** |
| Stance time (s) | 0.193 (0.042) | 0.193 (0.044) | 0 (0) | 0.982** | 0.2 (0.0189, −0.0169) | 0.863** |
| Asymmetry | ||||||
| Step length (m) | 0.082 (0.019) | 0.090 (0.021) | 0.008 (9%) | 0.668** | 0.7 (0.0337, −0.0245) | 0.599** |
| Step time (s) | 0.123 (0.037) | 0.120 (0.044) | −0.003 (−2.5) | 0.875** | 0.6 (0.0357, −0.0344) | 0.788** |
| Swing time (s) | 0.109 (0.040) | 0.101 (0.049) | −0.008 (−8%) | 0.925** | 0.5 (0.026, −0.0261) | 0.850** |
| Stance time (s) | 0.123 (0.04) | 0.109 (0.030) | −0.01 (−13%) | 0.878** | 0.6 (0.0357, −0.0398) | 0.742** |
IQR Interquartile range, s seconds, ICC Intraclass correlation coefficient, LoA% limits of agreement as a percentage of the mean of the two systems, r Spearman’s rank correlation coefficient
**p ≤ 0.01 *p ≤ 0.05
Discussion
This is the first study to investigate the feasibility, reliability and validity of a low-cost system incorporating algorithms and a single tri-axial accelerometer-based wearable (AX3) in quantifying a comprehensive assessment of both micro and macro gait characteristics post-stroke. The feasibility of using the AX3 wearable system was excellent with individuals with mild to moderate gait impairment following stroke. In the laboratory validity of the AX3 wearable system measurement of micro characteristics was assessed by comparison to three references (video, GaitRite, OPAL) with positive results. Test re-test reliability of the AX3 wearable system in both the laboratory and the community was moderate to excellent for all bar three of the gait measurements.
Breaking down the raw signal from a single wearable to quantify discrete gait characteristics is a potentially useful approach for quantifying specific gait impairments post-stroke and allows ‘real world’ measurement of these characteristics. Quantification of spatio-temporal characteristics by the AX3 system was compared with two references (GaitRite and OPAL). Agreement for mean gait characteristics between the AX3 wearable system and GaitRite was moderate to good for three measures, but poor for swing time and step length. The poor agreement for swing time may have been due to a limitation of the algorithm which estimated swing time from the difference between stride time and stance time which could lead to small inaccuracies [9]. Poor agreement between step length may have been due to the algorithm as it is based on a healthy model of gait assuming a rhythmical, linear and compass gait cycle (circular trajectory [36]) which is often not present with marked asymmetry common post-stroke and consequently the model may require refinement in this population. Indeed, a previous study using a single inertial measurement unit has indicated that a higher error rate is present in the detection of initial contact, swing time and stance time in pathological gait (including hemiplegic gait) in comparison to healthy elderly individuals [18]. Previous studies have also indicted it may be necessary to apply an individual correction factor to estimate step/stride length with accelerometry in people with neurological conditions including stroke [21].
Although GaitRite has been used in the stroke population to quantify gait characteristics [28], limitations have been observed when making comparisons of wearable measures to instrumented walkways [9]. Limitations relate to inherent differences in mechanisms of data capture as instrumented walkways such as GaitRite use pressure sensing to capture discrete foot falls whereas wearables continuously track acceleration This may have been the reason that the agreement between AX3 wearable system and GaitRite was poor on a number of measures. Agreement between the two wearable systems was better on mean, variability and asymmetry characteristics compared to agreement between the wearable system and the instrumented walkway.
Gait asymmetry is a common consequence of stroke and target of rehabilitation. Formal statistical tests of agreement indicated poor levels of agreement for asymmetry characteristics between the system and references. To explore these findings further individual participant data and formal agreement testing was conducted to explore if gait asymmetry (defined by video observation by experienced stroke clinicians and NIHSS lower limb scores) affected algorithm accuracy (data not reported). Post-hoc analysis indicated agreement was inferior for those with higher levels of asymmetry indicating this requires further exploration and algorithms may require refinement for those with marked gait asymmetry, or alternative placement and algorithms sought., Placement of a wearable sensor with appropriate adaptation of algorithms on each lower limb rather than the lower back may be more suitable for detecting asymmetry gait characteristics [18] but this would double patient burden, cost and increase technical complexity for synchronisation and data fusion. The reliability and validity of bilateral ankle accelerometers has been previously established in a small convenience sample (n = 12) for determining walking speeds and bouts of walking activity in the clinic after stroke [19] but the study did not explore gait asymmetry. More recent work on a small sample of hemiparetic stroke participants (n = 10) has indicated promise for accurate measurement of spatio-temporal parameters of gait with a system incorporating magneto-inertial units positioned on both ankles [20]. These results will need to be confirmed in a larger sample and are potentially limited by the use of magneto-inertial units requiring frequent recharging.
Alongside the novel use of wearables to quantify spatio-temporal gait characteristics post-stroke, wearables have been used for some time to capture physical activity outcomes. Review of psychometric data, however, has indicated that no single device is ideal at present for the measurement of physical activity after stroke [13]. As daily step count is linearly associated with reduced long-term all-cause mortality [37], and daily step count can be reduced by stroke impairments, it is imperative we have accurate measures of this variable post-stroke. Step count estimated by the system proposed here was accurate across a range of gait speeds when compared to video.
Establishing test retest reliability is important to determine whether there is consistency of measurement across time and subsequent use for longitudinal measurement of gait. Test-retest reliability was excellent for all macro characteristics captured in the community (ICC 08.67–0.917) and good to excellent for all except one of the 14 ‘micro’ characteristics. A recent summary of the test-retest reliability of physical activity measurement using wearable devices in stroke indicated that test retest reliability varied markedly across devices (ICCs 0.68–0.989) [13]. Findings from a number of studies testing measurement on multiple occasions indicted that the Step Watch Activity Monitor was the most reliable device for use to capture step count after stroke. Excellent test-retest reliability for step count was also demonstrated for the AX3 wearable in the current study and the AX3 also allowed for the reliable measurement of pattern and variability of gait activity and spatio-temporal gait characteristics. The AX3 wearable could be used to measure intervention response across a comprehensive range of gait measures in the laboratory and the community after stroke.
Limitations
Study limitations include the sample’s relatively high average gait speed and mild level of impairment as measured by the NIHSS meaning the sample may not have been representative of a typical stroke population. The use of gait speed and the NIHSS scale to characterise the sample did not allow the capture of data on quality of gait and hemiplegia. Individual levels of gait asymmetry and hemiplegia were assessed by clinical observation from video and indicated that almost two thirds of the sample had moderate to severe hemiplegia resulting in gait asymmetry. The sample may have been representative of community dwelling stroke survivors, but this data was not captured by the selected measures. This subjective data would have been strengthened by the inclusion of a measure of impairment such as the Fugl-Meyer motor assessment [38] The study excluded participants who wore a fixed ankle foot orthosis (AFO) due to the impact of the AFO on heel strike, meaning algorithms applied were unsuitable. Results from this study can therefore only be applied to stroke survivors who do not use a fixed AFO. The sample was not powered but was based upon previous sample sizes of studies of a similar nature [39, 40]. The study compared AX3 wearable system measures to video, and two other high-cost systems: GaitRite and OPAL. Comparing wearable measures to a camera-based motion capture system would have provided an alternative gold standard that may be worth considering in the future.
Conclusion
Although the low-cost AX3 wearable system demonstrates promise as a feasible and reliable tool with which to measure a comprehensive range of gait characteristics after stroke further work is needed to establish the system’s validity. Gait asymmetry is a common problem after stroke and the systems current algorithms will need to be refined/developed in order to capture this complex pathological gait characteristic.
Multiple applications in the stroke population including: monitoring symptoms; determining intervention and therapeutic effects; analysing relationships between daily fluctuations in activity and stroke impairments such as fatigue; and for patient feedback and assisting with self-management programmes, highlight the important role wearable systems have in future stroke management and the need for further refinement in this area.
Acknowledgements
We would like to thank all the volunteers who participated in this research.
Funding
A Medical Research Council Centenary award supported the delivery of this research. This report is independent research supported by Health Education England and the National Institute for Health Research (HEE/ NIHR ICA Programme Clinical Lectureship, Dr. Sarah Anne Moore, ICA-CL-2015-01-012). The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. LR, AH, SDD and AG are supported by the NIHR Newcastle Biomedical Research Centre (BRC) and Unit (BRU) based at Newcastle upon Tyne Hospitals NHS Foundation Trust and Newcastle University. The work was also supported by the NIHR/Wellcome Trust Clinical Research Facility (CRF) infrastructure at Newcastle upon Tyne Hospitals NHS Foundation Trust.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AFO
Ankle foot orthosis
- Hz
Hertz
- ICC
Intraclass correlation coefficient
- L5
Fifth lumbar vertebrae
- m/s
Meters per second
- ms
Milliseconds
- NIHSS
National Institute of Health Stroke Scale
- T1
Time point 1
- T2
Time point 2
Authors’ contributions
SM, AG, SL, LR designed the study and wrote initial protocols. Participant recruitment and testing were undertaken by SM, AH, AG. Data collection and analysis was undertaken by SM, AH, AG, SDD. Substantial contributions to the interpretation of the data were made by all authors. All authors read and approved the manuscript.
Ethics approval and consent to participate
The Greater Manchester West Research and Ethics Committee approved the study (NRES Committee Northwest-Greater Manchester West 15/NW/0731). All subjects gave informed written consent for the study according to the Declaration of Helsinki.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fulk GD, Reynolds C, Mondal S, Deutsch JE. Predicting home and community walking activity in people with stroke. Arch Phys Med Rehabil. 2010;91:1582–1586. doi: 10.1016/j.apmr.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Moore SA, Hallsworth K, Ploetz T, Ford GA, Rochester L, Trenell MI. Physical activity, sedentary behaviour and metabolic control following stroke: a cross-sectional and longitudinal study. PLoS One. 2013;8:1–6. doi: 10.1371/journal.pone.0055263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hackam DG, Spence D. Combining multiple approaches for the secondary prevention of vascular events after stroke. A quantitative modeling study. Stroke. 2007;38:1881–1885. doi: 10.1161/STROKEAHA.106.475525. [DOI] [PubMed] [Google Scholar]
- 4.Del Din S, Godfrey A, Mazzà C, Lord S, Rochester L. Free-living monitoring of Parkinson's disease: lessons from the field. Mov Disord. 2016;31:1293. doi: 10.1002/mds.26718. [DOI] [PubMed] [Google Scholar]
- 5.Wade DT. Measurement in neurological rehabilitation. Oxford: Oxford University Press; 1992. [PubMed] [Google Scholar]
- 6.Lin J-H, Hsu M-J, Hsu H-W, Wu H-C, Hsieh C-L. Psychometric comparisons of 3 functional ambulation measures for patients with stroke. Stroke. 2010;41:2021–2025. doi: 10.1161/STROKEAHA.110.589739. [DOI] [PubMed] [Google Scholar]
- 7.McDonough AL, Batavia M, Chen FC, Kwon S, Ziai J. The validity and reliability of the GAITRite system's measurements: a preliminary evaluation. Arch Phys Med Rehabil. 2001;82:419–425. doi: 10.1053/apmr.2001.19778. [DOI] [PubMed] [Google Scholar]
- 8.Wong JS, Jasani H, Poon V, Inness EL, McIlroy WE, Mansfield A. Inter- and intra-rater reliability of the GAITRite system among individuals with sub-acute stroke. Gait Posture. 2014;40:259–261. doi: 10.1016/j.gaitpost.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 9.Del Din S, Godfrey A, Rochester L: Validation of an accelerometer to quantify a comprehensive battery of gait characteristics in healthy older adults and Parkinson’s disease: toward clinical and at home use. IEEE J Biomed Health Inform. 2015;20(3):1–1. [DOI] [PubMed]
- 10.Byun S, Han JW, Kim TH, Kim KW. Test-retest reliability and concurrent validity of a single tri-axial accelerometer-based gait analysis in older adults with normal cognition. PLoS One. 2016;11:e0158956. doi: 10.1371/journal.pone.0158956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Godfrey A, Lara J, Del Din S, Hickey A, Munro CA, Wiuff C, Chowdhury SA, Mathers JC, Rochester L. iCap: instrumented assessment of physical capability. Maturitas. 2015;82:116–122. doi: 10.1016/j.maturitas.2015.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hobert MA, Maetzler W, Aminian K, Chiari L. Technical and clinical view on ambulatory assessment in Parkinson's disease. Acta Neurol Scand. 2014;130:139–147. doi: 10.1111/ane.12248. [DOI] [PubMed] [Google Scholar]
- 13.Fini NA, Holland AE, Keating J, Simek J, Bernhardt J. How is physical activity monitored in people following stroke? Disabil Rehabil. 2014;37(19):1–15. [DOI] [PubMed]
- 14.Shaughnessy M, Michael KM, Sorkin JD, Macko RF. Steps after stroke: capturing ambulatory recovery. Stroke. 2005;36:1305–1307. doi: 10.1161/01.STR.0000166202.00669.d2. [DOI] [PubMed] [Google Scholar]
- 15.Mahendran N, Kuys SS, Brauer SG. Recovery of ambulation activity across the first six months post-stroke. Gait Posture. 2016;49:271–276. doi: 10.1016/j.gaitpost.2016.06.038. [DOI] [PubMed] [Google Scholar]
- 16.Roos MA, Rudolph KS, Reisman DS. The structure of walking activity in people after stroke compared with older adults without disability: a cross-sectional study. Phys Ther. 2012;92:1141–1147. doi: 10.2522/ptj.20120034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Storm FA, Heller BW, Mazzà C. Step detection and activity recognition accuracy of seven physical activity monitors. PLoS One. 2015;10:e0118723. doi: 10.1371/journal.pone.0118723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Trojaniello D, Ravaschio A, Hausdorff JM, Cereatti A. Comparative assessment of different methods for the estimation of gait temporal parameters using a single inertial sensor: application to elderly, post-stroke, Parkinson's disease and Huntington's disease subjects. Gait Posture. 2015;42:310–316. doi: 10.1016/j.gaitpost.2015.06.008. [DOI] [PubMed] [Google Scholar]
- 19.Dobkin BH, Xu X, Batalin M, Thomas S, Kaiser W. Reliability and validity of bilateral ankle accelerometer algorithms for activity recognition and walking speed after stroke. Stroke. 2011;42:2246–2250. doi: 10.1161/STROKEAHA.110.611095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Trojaniello D, Cereatti A, Pelosin E, Avanzino L, Mirelman A, Hausdorff JM, Della Croce U. Estimation of step-by-step spatio-temporal parameters of normal and impaired gait using shank-mounted magneto-inertial sensors: application to elderly, hemiparetic, parkinsonian and choreic gait. J Neuroeng Rehabil. 2014;11:1–12. doi: 10.1186/1743-0003-11-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Esser P, Dawes H, Collett J, Feltham MG, Howells K. Assessment of spatio-temporal gait parameters using inertial measurement units in neurological populations. Gait Posture. 2011;34:558–560. doi: 10.1016/j.gaitpost.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 22.Horak F, King L, Mancini M. Role of body-worn movement monitor Technology for Balance and Gait Rehabilitation. Phys Ther. 2015;95:461–470. doi: 10.2522/ptj.20140253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Godfrey A, Del Din S, Barry G, Mathers JC, Rochester L. Instrumenting gait with an accelerometer: a system and algorithm examination. Med Eng Phys. 2015;37:400–407. doi: 10.1016/j.medengphy.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hickey A, Del Din S, Rochester L, Godfrey A. Detecting free-living steps and walking bouts: validating an algorithm for macro gait analysis. Physiol Meas. 2017;38:N1–N15. doi: 10.1088/1361-6579/38/1/N1. [DOI] [PubMed] [Google Scholar]
- 25.Bamford J, Sandercock P, Dennis M, Warlow C, Burn J. Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet. 1991;337:1521–1526. doi: 10.1016/0140-6736(91)93206-O. [DOI] [PubMed] [Google Scholar]
- 26.Brott T, Adams H, Olinger M, Marler J, Barsan M, Biller M, Spilker J, Holleran R, Eberle R, Hertzberg V, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20:864–870. doi: 10.1161/01.STR.20.7.864. [DOI] [PubMed] [Google Scholar]
- 27.Galna B, Lord S, Rochester L. Is gait variability reliable in older adults and Parkinson's disease? Towards an optimal testing protocol. Gait Posture. 2013;37:580–585. doi: 10.1016/j.gaitpost.2012.09.025. [DOI] [PubMed] [Google Scholar]
- 28.Kuys SS, Brauer SG, Ada L. Test-retest reliability of the GAITRite system in people with stroke undergoing rehabilitation. Disabil Rehabil. 2011;33:1848–1853. doi: 10.3109/09638288.2010.549895. [DOI] [PubMed] [Google Scholar]
- 29.Lord S, Galna B, Verghese J, Coleman S, Burn D, Rochester L. Independent domains of gait in older adults and associated motor and nonmotor attributes: validation of a factor analysis approach. J Gerontol Ser A Biol Med Sci. 2013;68:820–827. doi: 10.1093/gerona/gls255. [DOI] [PubMed] [Google Scholar]
- 30.Hickey A, Del Din S, Rochester L, Godfrey A. Detecting free-living steps and walking bouts: validating an algorithm for macro gait analysis. Physiol Meas. 2016;38:N1. doi: 10.1088/1361-6579/38/1/N1. [DOI] [PubMed] [Google Scholar]
- 31.Del Din S, Godfrey A, Galna B, Lord S, Rochester L. Free-living gait characteristics in ageing and Parkinson’s disease: impact of environment and ambulatory bout length. J Neuroeng Rehabil. 2016;13:1–12. doi: 10.1186/s12984-016-0154-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lord S, Chastin SFM, McInnes L, Little L, Briggs P, Rochester L. Exploring patterns of daily physical and sedentary behaviour in community-dwelling older adults. Age Ageing. 2011;40:205–210. doi: 10.1093/ageing/afq166. [DOI] [PubMed] [Google Scholar]
- 33.Chastin SFM, Baker K, Jones D, Burn D, Granat MH, Rochester L. The pattern of habitual sedentary behavior is different in advanced Parkinson's disease. Mov Disord. 2010;25:2114–2120. doi: 10.1002/mds.23146. [DOI] [PubMed] [Google Scholar]
- 34.Rochester L, Chastin SFM, Lord S, Baker K, Burn DJ. Understanding the impact of deep brain stimulation on ambulatory activity in advanced Parkinson’s disease. J Neurol. 2012;259:1081–1086. doi: 10.1007/s00415-011-6301-9. [DOI] [PubMed] [Google Scholar]
- 35.Hartmann A, Luzi S, Murer K, de Bie RA, de Bruin ED. Concurrent validity of a trunk tri-axial accelerometer system for gait analysis in older adults. Gait Posture. 2009;29:444–448. doi: 10.1016/j.gaitpost.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 36.Zijlstra W, Hof AL. Assessment of spatio-temporal gait parameters from trunk accelerations during human walking. Gait Posture. 2003;18:1–10. doi: 10.1016/S0966-6362(02)00190-X. [DOI] [PubMed] [Google Scholar]
- 37.Dwyer T, Pezic A, Sun C, Cochrane J, Venn A, Srikanth V, Jones G, Shook R, Sui X, Ortaglia A, et al. Objectively measured daily steps and subsequent long term all-cause mortality: the Tasped prospective cohort study. PLoS One. 2015;10:e0141274. doi: 10.1371/journal.pone.0141274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gladstone DJ, Danells CJ, Black SE. The Fugl-Meyer assessment of motor recovery after stroke: a critical review of its measurement properties. Neurorehabil Neural Repair. 2002;16:232–240. doi: 10.1177/154596802401105171. [DOI] [PubMed] [Google Scholar]
- 39.Haeuber E, Shaughnessy M, Forrester L, Coleman K, Macko R. Accelerometer monitoring of home- and community-based ambulatory activity after stroke. Arch Phys Med Rehabil. 2004;85:1997–2001. doi: 10.1016/j.apmr.2003.11.035. [DOI] [PubMed] [Google Scholar]
- 40.Hale LA, Pal J, Becker I. Measuring free-living physical activity in adults with and without neurologic dysfunction with a Triaxial accelerometer. Arch Phys Med Rehabil. 2008;89:1765–1771. doi: 10.1016/j.apmr.2008.02.027. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.


