Abstract
INTRODUCTION:
Fear of childbirth is a common problem in pregnant women, which in many cases leads to maternal requested cesarean. A midwife, as a responsible person, plays an important role in providing advice and giving care to mothers during pregnancy, delivery, and the postpartum period. The present study was conducted with the aim of determining the effect of individual counseling program by a midwife on fear of childbirth in primiparous women.
MATERIALS AND METHODS:
This clinical trial was conducted in 2015–16, on ninety primiparous women with gestational ages of 28–30 weeks, who presented themselves at health-care centers in Mashhad. The individuals were randomly divided into two groups: intervention and control. The intervention group received the counseling program individually during three sessions, and the routine care was given to the control group. Data collection tools the Wijma Delivery Expectancy/Experience Questionnaire. The data were collected at recruitment during 34–36 weeks of pregnancy and were analyzed using SPSS 16 software and the statistical tests: Chi-square and t-test, and P < 0.05 was considered to be significant.
RESULTS:
During weeks 34–36 of pregnancy, the mean scores for fear of childbirth in the intervention group and control group were 39.733 ± 17.085 and 65.666 ± 15.019, respectively, and there was a significant difference between the two groups (P < 0.001).
CONCLUSION:
The individual counseling program provided by the midwife to the primiparous women during pregnancy resulted in reduced fear of childbirth.
Keywords: Fear of childbirth, individual counseling, primiparous women
Introduction
Fear of childbirth is a common problem in pregnant women which often leads to cesarean section.[1] The fear of giving birth exists in between 6% and 10% of pregnant women, and planned cesarean section without medical reasons is more common among these people.[2] According to the study of Handelzalts et al., the only psychological variable in request of a mother for cesarean childbirth is fear of childbirth.[3] The prevalence of childbirth fear has been reported to be 20% in Scandinavian countries, the UK, Australia, and Sweden which about 6%–10% of it has been severe fear of childbirth.[4] In Iran, about 5%–20% of pregnant women are afraid of childbirth in a way that one out of every five pregnant women is afraid of childbirth.[5] Nearly 55.8% of women were afraid of childbirth in the study of Khorsandi et al.[6] There is an inverse relation between the number of pregnancies and childbirth fear in a way that fear of childbirth was higher in women with the first experience of childbirth compared to those who had this experience.[7] Some of the causes of childbirth fear are maternal and mental characteristics of mother, intolerance to pain, observation or hearing of surrounding experiences and worries about adverse effects of physical activity, and distrust of childbirth agents.[8] According to the study of Fenwick et al., fear of unknowns, lack of confidence in childbirth, internalization of negative narratives of other women, and birth pain are higher in women with the first experience of childbirth compared to those who had this experience.[9] There have so far been some studies in the field of reducing fear of childbirth such as classes to prepare for childbirth, relaxation, cognitive-behavioral, and educational interventions[10,11,12,13] which have been effective in reduction of fear of childbirth, but between 20% and 80% of pregnant women continue to experience some levels of childbirth fear, and the level of childbirth fear has increased over time[14] in a way that 83% of pregnant women had severe childbirth fear[15] in the study of Moasheri et al., (2015) given that natural delivery is the best way of giving birth in most pregnant women, and approximately 85–90% of deliveries can be done naturally without any treatment intervention, and performing cesarean section surgery which according to the World Health Organization (WHO) is about 10%–15% acceptable is limited to cases where delivery is not possible through the natural channel and in general in condition when life of the mother and the fetus in the absence of surgical intervention is compromised.[16] However, according to interventions, the rate of delivery of cesarean delivery in Iran is still reported to be 3–4 times higher the global standard, and based on systematic review and meta-analysis of Azami-Aghdash et al. (2014) conducted in Iran, the prevalence of cesarean section is 48% throughout the country[17] which is higher than the acceptable percentage of the WHO.[18] Hence, there is the need for more studies in the field of women's request for cesarean section which one of its most important causes is fear of childbirth. Another midwifery intervention to reduce the fear of childbirth is counseling. Consulting examines the deep problems faced by the individual during pregnancy.[19] According to the definition provided by the International Confederation of Midwives (2005), midwife as a responsible person has an important role in providing counseling, support, care, and advice during pregnancy, childbirth, and postpartum period, and counseling and individual training for mothers in reproductive age, especially during pregnancy, childbirth, and postpartum have been mentioned to be one of the four principles of the midwifery care provision.[20]
In the study of Toohill et al. in Australia, two counseling sessions for pregnant women could reduce the fear of childbirth during pregnancy.[13] Larsson et al. concluded in Sweden that mid-pregnancy consultation failed to reduce the level of fear although pregnant women expressed satisfaction with counseling.[2] Ryding et al. conducted a study to assess the midwife's counsel on fear of childbirth and concluded that women in the intervention group were more afraid than the control group although they expressed satisfaction with counseling.[21]
Most studies conducted in the field of counseling on fear of childbirth, require psychological and psychoanalytic skills.[12,22,23,24] However, Birth Emotions - Looking to Improve Expectant Fear [BELIFE] counseling program (which is the current expectation of women and their feelings about the fear of childbirth) is designed according to the goal of midwifery care and its content is based on the consulting model in Gamble's study.
With respect to high incidence of cesarean delivery in the country and limited studies done in the field of fear of delivery, there are still not enough available evidences about an effective program of counseling for reducing childbirth fears. Hence, the present study was carried out with the objective of determining the effect of individual counseling program of midwives on fear of childbirth of mothers with the first experience of delivery in Mashhad health centers.
Materials and Methods
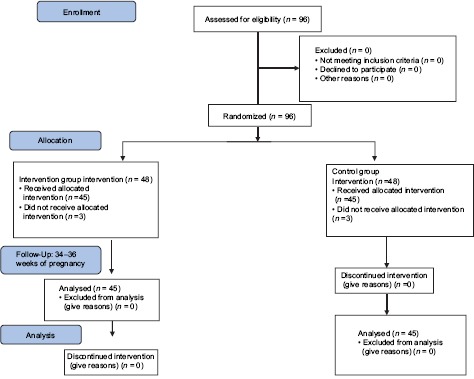
Act on sampling and carrying out the research was done in this clinical trial study with IRCT2016042827653N1 code after approval by the ethics committee in the university's research unit and taking written consent from them and by consideration of ethical codes. Sampling was done from March 2015 to October 2016 on ninety pregnant women referring to Mashhad health centers. Initially, one of the Mashhad health centers was selected randomly from the Mashhad health centers, and then, four centers which were similar in terms of social conditions were selected. Allocation of two groups to these centers was also done randomly and by draw. Subsequently, sampling was performed in each center with an unpredictable and easy method. Sample size was calculated to be 42 individuals in each group based on a guideline that was performed on twenty individuals in each research unit (ten individuals in each group) with 95% confidence coefficient and 80% power using the formula for comparing the means and 48 individuals were identified in each group by considering 15% sample loss. The criteria for entering the study included: being Iranian, using Persian language, being resident of Mashhad, having age 18–35 years old, having gestational age 28–30 weeks, having singleton pregnancy, having minimum fifth-grade primary education, having low-risk pregnancy and having the score of 38–84 in fear of childbirth score based on A version of Wijma Delivery Expectancy/Experience Questionnaire (W-DEQ) fear questionnaire and lack of a history or current infection to the medical condition, severe embryonic anomalies, substance abuse, and drug addiction, psychotropic drugs, stimulants and alcoholic beverages, confronting unpleasant and stressful events 6 months before the start of the study, history of infertility, and speech and hearing disorders; exclusion criteria included: not attending one of the counseling sessions and reluctance of the mother to continue to collaborate in research and counseling by the psychologist. Each group consisted of 48 individuals at the beginning of study, but three individuals were excluded from the control group in the 34–36 weeks of pregnancy and three individuals were excluded from the intervention group during the study [Diagram 1]. The data collection toll included demographic-midwifery form, W-DEQ expectancy, and childbirth experience questionnaire versions A and B. Demographic-midwifery form consisted of 23 questions in the field of midwifery and demographic characteristics. W-DEQ childbirth expectancy questionnaire was used to evaluate childbirth fear. Two separate translators independently translated the questionnaire into Persian to obtain a questionnaire equivalent to the original language and then two other translators independently translated the translated version into English and then the prepared version was compared to the original version by a bilingual specialist after finalization. Then, the final version was evaluated by ten faculty members from the Faculty of Nursing and Midwifery and the Faculty of Psychology for determining the content validity, and some changes were made in it; this version was sent to the original creator, Wijma in Sweden, and it was used in Iranian society after it was approved by Wijiema. This questionnaire contains 33 questions, and answering the questions of this questionnaire is based on the 6-point Likert scale based on which zero means “completely” and 5 is in the sense of “not at all.” Minimum score of it was calculated to be zero and its maximum score was calculated to be 165. The reliability of version A of Wijma Expectancy Questionnaire has been approved by Toohil in Australia with Cronbach's alpha coefficient of 0.87.[13] Version B of Wijma expectancy questionnaire has been approved by Fenwick et al. in Australia with a Cronbach's alpha of 0.87.[4] In the present study, these questionnaires were first completed by thirty of the studied population who were not involved in the study process to determine the reliability, and reliability of questionnaires A and B was determined by Cronbach's alpha coefficient of 0.71 and 0.77.
Diagram 1.
Describing the stages of performing the intervention
At first, the score of fear of childbirth would be evaluated using Wijma Questionnaire (version A). Then, women who scored between 38 and 84 (medium and high fears) would enter the study, and the research objectives would be explained to them in the right place (the room reserved for the meetings). In the intervention group, in addition to receiving the usual services of health centers, individual counseling was done face to face based on the content of the consultation model in the Gamble's study. The consultation was conducted by researcher in three sessions (60–45 min) every 2 weeks based on the days of the mother's visit to the health centers during the weeks (28-30,30-32,32-34). The content of the consultation in each session included:first session (weeks 28–30), after communicating with the expectant mother, encouraging to express emotions and attitudes about childbirth through open questions, active listening, and feedback on women's concerns. Second session (30–32 weeks): Asking questions from women for communicating between preset feelings and behaviors with predetermined beliefs and expectations about important aspects for the evaluation of feelings and thoughts about giving birth, providing information about the stages of natural delivery, and solving abortions and strengthening positive thoughts of mother. Third session (32–34 weeks): Strengthening positive approaches to delivery (proposing positive strategies to reduce childbirth fears) and providing solutions The woman was asked questions with regard to identifying and deciding about potential solutions, such as: choosing the type of delivery. And her decision was helped and supported.
Follow-up using phone calls was done during the study to remind the next session of consultation as well as to answer the questions for a maximum of 10 min. The control group received the usual care of health center and was referred to midwife of the health center for necessary action in case of having high fear score. Fear of delivery was again measured in two intervention and control groups in weeks (34–36) and 24 h after childbirth and results were compared, and the level of satisfaction among the individuals in counseling group was also measured. Pre- and post-test results were compared in both groups. Normality of quantitative variables was tested using Kolmogorov–Smirnov test. Statistical analysis was performed by Statistical Package for the Social Sciences, version 16, SPSS Inc, Chicago, Illinois, USA (SPSS). using descriptive statistics (mean, standard deviation, median, and frequency distribution) and independent t-test, paired t-test, Chi-square test, Fisher's exact test, and Mann–Whitney test.
Results
In this study, both groups were homogeneous in terms of maternal education level (P = 0.382), maternal occupatio n (P = 1), socioeconomic status (P = 0.542), abortion history (P = 0.714), maternal pregnancy status (P = 0.258), body mass index (P = 0.799), maternal information (P = 0.159), preference for childbirth (P = 0.058), age (P = −0.876), safe delivery classes (P = 0.832), and educational classes in health center (P = 0.001).
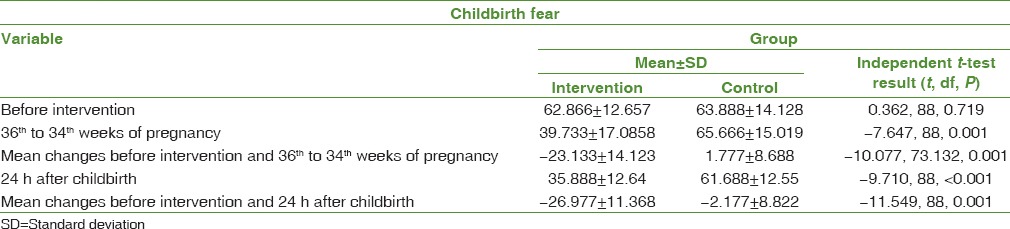
Comparison of mean scores of childbirth fear in two groups with independent t-test showed that there is no significant difference between the two groups in terms of mean scores before intervention (P = 0.719). The results of weeks 36–34 of the same test showed that the mean scores of fear of childbirth in the two groups were statistically significant (P < 0.001). Evaluation of changes in mean scores of childbirth fear during the study (the difference between the mean scores of childbirth fear in the preintervention phase and the 36th–34th weeks of pregnancy) by independent t-test shows that mean scores of fear of childbirth in two groups are statistically significant (P < 0.001). Independent t-test showed that the mean score of fear of childbirth in 24 h after delivery in two groups is statistically significant (P < 0.001). Evaluation of mean changes of scores of fear of childbirth during the study (the difference in the mean scores of fear of childbirth in the preintervention and 24 h after childbirth) by independent t-test shows that the mean changes of scores of fear of childbirth in two groups are statistically significant (P < 0.001) [Table 1].
Table 1.
Comparison of mean and standard deviation of fear of delivery in primiparous women in intervention and control groups
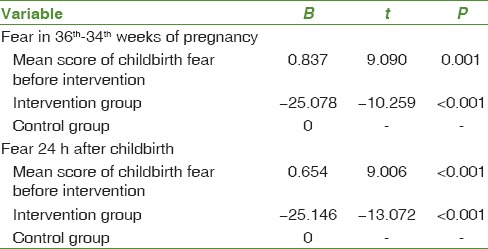
All interventional variables were entered into the general linear model using the covariance analysis test to eliminate the effect of confounding variables so that the effect of group is determined after elimination of their effects. Nonsignificant variables were, respectively, omitted from the most P value of the model using backward method. The variable of medium score of fear of childbirth before counseling was considered as interventional variable which with its elimination, mean scores of childbirth fear after counseling at 36–34 weeks of gestation, and 24 h after delivery in the intervention group had a statistically significant difference with the control group (P < 0.001). In a way that 25 scores were reduced from childbirth fear score in the intervention group compared to the control group [Table 2].
Table 2.
The results of covariance analysis for effect of counseling intervention on mean score of “childbirth fear” by controlling the variable of mean scores for “fear of giving birth” before counseling
Satisfaction with counseling in individuals who received individual counseling was 40% very high, 50% high, and 10% partially.
Discussion
The present study showed that an individual counseling program provided by a midwife based on a counseling consultant by a midwife based on BELIFE counseling (which is the current expectations of women and their feelings about the fear of childbirth) is effective in reducing fear of childbirth in a way that the level of fear of childbirth in primiparous women in the weeks 36–34 of pregnancy in the intervention group was significantly lower than the control group. The results of the study of Toohill et al. showed that two BELIFE counseling through phone call at the 24th and 34th weeks of pregnancy in women with high levels of fear reduced 10 scores in the mean fear of childbirth in the intervention group compared to the control group 2 weeks after the intervention[13] which was consistent with the results of the present study. The research population in the study of Toohil were multiparous and nulliparous women while the research population in the present study consisted of primiparous women. There was 40% drop in samples in the study of Toohil et al. which one of its most important reasons can be counseling through phone call and the absence of face-to-face meetings. It was shown in the study of Larsson et al. which evaluated longitudinal effects of previous counseling programs on fear of childbirth that the degree of fear of childbirth in the middle of pregnancy, 2 months, and 1 year after childbirth has not been different in two groups[2] which its results were not consistent with the present study. Lack of consistency with the present study can be due to differences in counseling content as well as differences in measurement tool for fear of childbirth. A researcher made self-report tool was used in the study of Larson and questionnaires were sent to the samples by post while Wijma tool was used in the present study to evaluate the score of fear of childbirth and questionnaires were completed in the presence of the researcher. The study of Khorsandi et al. showed that nine sessions of group training for relaxation based on calming and illustration related to childbirth in the second trimester of pregnancy reduced 10 scores in the mean scores of childbirth fear in the intervention group compared to the control group in primiparous women[11] which was consistent with the results of the present study. Tool for the measurement of fear and counseling content was among differences between the study of Khorsandi and the present study and Hartman childbirth Attitude Tool was used in the study of Khorsandi and training was done in groups and by researcher along with a trainer while Wijma tool was used in the present study to measure the level of fear and counseling to pregnant women was done individually by the midwife based on the fear of giving birth.
Saisto et al. concluded that psychometric treatment in cognitive and behavioral exercises provided by a gynecologist and psychologist reduced the fear of childbirth[12] which was consistent with the results of the present study. Individual counseling based on BELIFE does not require advanced psychotherapy capabilities and its content explores the source of fear and it can be implemented by the midwife. Counseling is an important part of midwife's role. Counseling provides the right information and helps mothers to make informed choices which are the best options for them. Consultation on maternal issues requires good listening skills and a sense of companion to increase the confidence of pregnant women.[25]
The result of the study by Kizilirmak and Baser showed that two training sessions in the third trimester of pregnancy, which included information on childbirth, familiarity with the delivery room, and learning about the childbirth process, could reduce the mean score of childbirth fear by 15 in the intervention group compared to the control group[26] which was consistent with the results of the present study. The educational method and content were among differences between the study of Kisermark and the present study as well as the fact that Kisermark evaluated the mean level of fear. In the present study, counseling was based on BELIFE which included active listening and responding to the feelings of pregnant women and providing information about the cause of childbirth fear. Middle and high levels of fear were measured in the present study, and the counseling program was able to reduce the mean of fear of delivery by 25 in the middle and high levels in the intervention group compared to the control group.
The results of study of Raiding et al. showed that the midwife's consultation has no effect on the fear of childbirth and the experience of childbirth, and the results were not consistent with the present study. One of the positive aspects of this study was counseling by midwife given that most pregnant women do not tend to meet and work with a psychologist or psychiatrist to express their concerns and fears about giving birth, and in addition, psychologists do not know as much as midwives in terms of all fields and aspects of childbirth. Some limitations of the present study were individual, mental, and psychological differences of research units in completing the questionnaires as well as selection of four available centers covered by Health Center No. 1 based on their similar social condition which limits the generalization of results to the entire society.
Conclusion
It is recommended based on positive outcomes of the midwife's individual counseling program on the reduction of fear of delivery during pregnancy that this program is implemented by midwife along with care programs at health centers by including of evaluation of childbirth fear in perinatal psychological screening of pregnant women at health centers.
Financial support and sponsorship
This study was financially supported by the Mashhad University of Medical Sciences, Mashhad, Iran.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This study is part of a research thesis proposal approved by the Mashhad University of Medical Sciences on December 03, 2016 with Code No. 941345 and IRCT 2016042827653N1 that sponsored by the Department of Mashhad University of Medical Sciences. We are thankful for the help and assistance given by that department.
References
- 1.Storksen HT, Eberhard-Gran M, Garthus-Niegel S, Eskild A. Fear of childbirth; the relation to anxiety and depression. Acta Obstet Gynecol Scand. 2012;91:237–42. doi: 10.1111/j.1600-0412.2011.01323.x. [DOI] [PubMed] [Google Scholar]
- 2.Larsson B, Karlström A, Rubertsson C, Hildingsson I. The effects of counseling on fear of childbirth. Acta Obstet Gynecol Scand. 2015;94:629–36. doi: 10.1111/aogs.12634. [DOI] [PubMed] [Google Scholar]
- 3.Handelzalts JE, Fisher S, Lurie S, Shalev A, Golan A, Sadan O. Personality, fear of childbirth and cesarean delivery on demand. Acta Obstet Gynecol Scand. 2012;91:16–21. doi: 10.1111/j.1600-0412.2011.01287.x. [DOI] [PubMed] [Google Scholar]
- 4.Fenwick J, Gamble J, Creedy DK, Buist A, Turkstra E, Sneddon A, et al. Study protocol for reducing childbirth fear: A midwife-led Psycho-education intervention. J Pregnancy Childbirth. 2013;13:11–6. doi: 10.1186/1471-2393-13-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nasiri F, Sharifi SH. Its fear of childbirth and the type of personality in pregnant women. J Obstet Gynecol Infertil. 2013;66:18–25. [Google Scholar]
- 6.Khorsandi M, Vakilian K, Nasirzadeh M. Investigating different factors of fear in normal delivery among pregnant women, in Arak - A cross sectional study. J Fasa Univ Med Sci. 2014;4:161. [Google Scholar]
- 7.Taheri Z, Khorsandi M, Amiri M, Hasanzade A. Investigating the causes of fear of childbirth in Shahrekord pregnant women, in 2013. J Rafsanjan Univ Med Sci. 2015;14:345–50. [Google Scholar]
- 8.Karaçam Z, Ançel G. Depression, anxiety and influencing factors in pregnancy: A study in a Turkish population. Midwifery. 2009;25:344–56. doi: 10.1016/j.midw.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 9.Fenwick J, Toohill J, Creedy D, Smith J, Gamble J. Sources, responses and moderators of childbirth fear in Australian women: A qualitative investigation. Midwifery. 2015;31:239–46. doi: 10.1016/j.midw.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 10.Mehdizadeh A, Roosta F, Chaichian S, Alaghehbandan R. Evaluation of the impact of birth preparation courses on the health of the mother and the newborn. Am J Perinatol. 2005;22:7–9. doi: 10.1055/s-2004-837738. [DOI] [PubMed] [Google Scholar]
- 11.Khorsandi M, Ghofranipour F, Heydarnia A, Faghihzadeh S, Vafaei M, Rousta F, et al. The effect of childbirth preparation classes on childbirth fear and normal delivery among primiparous women. J Arak Med Univ. 2008;11:29–36. [Google Scholar]
- 12.Saisto T, Salmela-Aro K, Nurmi JE, Könönen T, Halmesmäki E. A randomized controlled trial of intervention in fear of childbirth. Obstet Gynecol. 2001;98(5 Pt 1):820–6. doi: 10.1016/s0029-7844(01)01552-6. [DOI] [PubMed] [Google Scholar]
- 13.Toohill J, Fenwick J, Gamble J, Creedy DK, Buist A, Turkstra E, et al. A randomized controlled trial of a psycho-education intervention by midwives in reducing childbirth fear in pregnant women. Birth. 2014;41:384–94. doi: 10.1111/birt.12136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lopukhova OG, Kashshapova EV. Fear of childbirth in pregnant women: External and internal factors. Psychol Russ. 2015;8:114–25. [Google Scholar]
- 15.Moasheri N, Sharifzadeh G, soltanzadeh V, Khosravi Z, Rakhshani F. Relationship between fear of pain, fear of delivery and attitude towards cesarean section with preferred mode of delivery among pregnant women. Iran J Obstet Gynecol Infertil. 2015;18:8–16. [Google Scholar]
- 16.Miri Farahani L, Abbasi Shavazi MJ. Caesarean section change trends in Iran and some demographic factors associated with them in the past three decades. J Fasa Univ Med Sci. 2012;2:127–34. [Google Scholar]
- 17.Azami-Aghdash S, Ghojazadeh M, Dehdilani N, Mohammadi M, Asl Amin Abad R. Prevalence and causes of cesarean section in Iran: Systematic review and meta-analysis. Iran J Public Health. 2014;43:545–55. [PMC free article] [PubMed] [Google Scholar]
- 18.Gibbons L, Belizan JM, Lauer JA, Betran AP, Merialdi M, Althabe F. Inequities in the use of cesarean section deliveries in the world. Am J Obstet Gynecol. 2012;206:331.e1–19. doi: 10.1016/j.ajog.2012.02.026. [DOI] [PubMed] [Google Scholar]
- 19.Delaram M, Soltanpour F. The effect of counseling in third trimester on anxiety of nulliparous women at the time of admission for Labor Zahedan. J Res Med Sci. 2012;14:61–5. [Google Scholar]
- 20.Hemminki E, Long Q, Zhang WH, Wu Z, Raven J, Tao F, et al. Impact of financial and educational interventions on maternity care: Results of cluster randomized trials in rural China, CHIMACA. Matern Child Health J. 2013;17:208–21. doi: 10.1007/s10995-012-0962-6. [DOI] [PubMed] [Google Scholar]
- 21.Ryding EL, Persson A, Onell C, Kvist L. An evaluation of midwives’ counseling of pregnant women in fear of childbirth. Acta Obstet Gynecol Scand. 2003;82:10–7. doi: 10.1034/j.1600-0412.2003.820102.x. [DOI] [PubMed] [Google Scholar]
- 22.Rouhe H, Salmela-Aro K, Toivanen R, Tokola M, Halmesmäki E, Saisto T. Life satisfaction, general well-being and costs of treatment for severe fear of childbirth in nulliparous women by psychoeducative group or conventional care attendance. Acta Obstet Gynecol Scand. 2015;94:527–33. doi: 10.1111/aogs.12594. [DOI] [PubMed] [Google Scholar]
- 23.Klabbers GA, Wijma K, Paarlberg KM, Emons WH, Vingerhoets AJ. Treatment of severe fear of childbirth with haptotherapy: Design of a multicenter randomized controlled trial. BMC Complement Altern Med. 2014;14:385. doi: 10.1186/1472-6882-14-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Saisto T, Toivanen R, Salmela-Aro K, Halmesmäki E. Therapeutic group psychoeducation and relaxation in treating fear of childbirth. Acta Obstet Gynecol Scand. 2006;85:1315–9. doi: 10.1080/00016340600756920. [DOI] [PubMed] [Google Scholar]
- 25.Gamble J, Creedy D, Moyle W. Counselling processes to address psychological distress following childbirth: Perceptions of women Australian. Midwifery. 2004;17:12–5. [Google Scholar]
- 26.Kizilirmak A, Baser M. The effect of education given to primigravida women on fear of childbirth. Appl Nurs Res. 2016;29:19–24. doi: 10.1016/j.apnr.2015.04.002. [DOI] [PubMed] [Google Scholar]


