Abstract
The multifocal intraocular lenses (IOLs) available are often able to restore visual function and allow spectacle independence after their implantation with great levels of patient satisfaction. The factors associated with the postoperatory success include the careful selection of the patient, the knowledge about the IOLs’ design, and their visual performance added to the proper surgical technique and management of possible complications as demonstrated by the evidence available.
Keywords: Cataract surgery, multifocal intraocular lenses, patient satisfaction, refractive lens exchange, spectacle independence
Introduction
The technology of the multifocal intraocular lenses (IOLs) is advancing as the objectives of the cataract surgery are becoming more embracing. Nowadays, patients have more expectations about their vision and frequently desire the spectacle independence after cataract surgery. In addition, they do not expect any complication or unsatisfactory result.[1,2,3]
In this context, the multifocal IOLs were developed to enhance outcomes of cataract surgery improving near vision by dividing light in different focuses, which changes the vision physiology because of the light dispersion that happens when it enters into the eye.[1,2] As a result, visual symptoms such as halos, glare, and lower contrast sensitivity may occur.[3,4,5]
With the objective of getting a more physiological division of light and, in this way, to optimize the spectacle independence and also provide better vision quality and less visual symptoms for the patient, recent researches aim to enhance the optical design of the multifocal IOLs.[1,2] Although it is still a developing technology, the available multifocal IOLs are often able to restore visual function and allow spectacle independence after the surgery with great levels of patient satisfaction.[1,2,3,6]
The careful selection of the patient, the knowledge about the IOLs’ design, and their visual performance added to the proper surgical technique and management of possible complications are the key for the success implantation of the multifocal IOLs.[1,4,6]
Types of Multifocal Intraocular Lenses
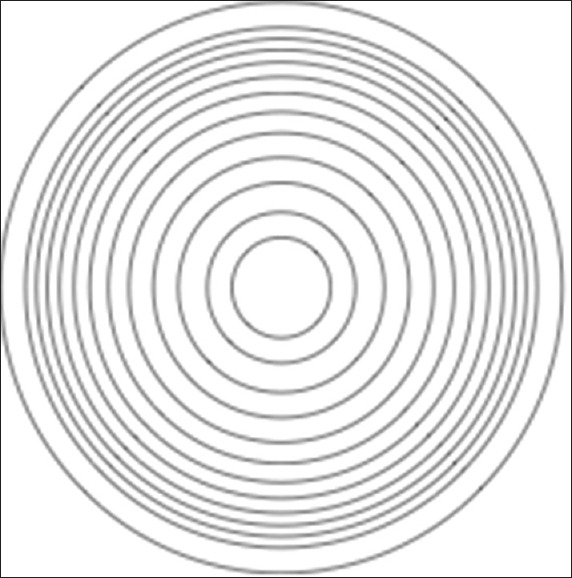
The multifocal IOLs refract or diffract, or both, the light from an object simultaneously to the far and near vision and part of this light disperses. Therefore, they are classified as refractive [Figure 1], diffractive [Figure 2], or combined.[1,4]
Figure 1.

Schematic design of refractive intraocular lenses showing the different refractive power annular zones
Figure 2.
Schematic design of diffractive intraocular lenses showing the concentric zones that diffracts light providing focus at different distances
This division of light to different focuses may occur as result of some combinations: two or more different anterior spherical refractive surfaces, a posterior spherical refractive surface with a multiple anterior aspheric surface, an anterior spherical refractive surface with multiple posterior diffractive structured surfaces, or a biconvex lens with longitudinal aberrations on the anterior surface.[1]
The refractive models reach multifocality by their different refractive power annular zones and usually provide proper far and intermediate vision; however, sometimes, near vision is not sufficient. They are dependent of pupil dynamics, very sensitive to their centering, may cause halos and glare, and reduce the contrast sensitivity.[1,4] In addition, some refractive designs include a continuous change in curvature between zones providing functional vision across all distances.[6]
The diffractive models are composed by diffractive microstructures in concentric zones that get closer to each other as they distance from the center. They generally provide good far and near vision, but the intermediate vision may not be satisfactory in some cases. They are not so dependent of pupil dynamics and more tolerant to their centering, but they usually affect the contrast sensitivity in a greater scale.[1,4] Although contrast sensitivity in patients with multifocal IOLs is diminished compared with those with monofocal IOLs, it is usually within the normal range of contrast.[1]
The multifocal IOLs’ optics may be rotationally symmetric (all diffractive models and most of the refractive) or rotationally asymmetric (some refractive models). There are also aspheric designs that aim to reduce the spherical aberrations and enhance the contrast sensitivity.[1,2,4,7]
The summary of the technical features, possible symptoms, and indications of the different multifocal IOL models available are shown in Tables 1-4 (Alió JL. Modern Presbyopic IOL's: What do they offer, what can we get? Presented in the American Academy of Ophthalmology Congress, 2015) and more detailed in the book “Multifocal IOLs: The Art and the Practice", written by Alió and Pikkel.[4]
Table 1.
Diffractive technology intraocular lenses (I) show the main models available of these intraocular lenses, their figures, and specific technical features as those with clinical studies published or not
| Diffractive technology IOLs (I) | Figure | Incision size (mm) | Asphericity | Near add | Pupil dependence (percentage of light N/F) | Clinical studies |
|---|---|---|---|---|---|---|
| AT-LISA Bi/Tri (ZEISS) |  |
1.8 | Neutral | +3.75/trifocal/+1.75 | Dependent (35/65) Tri 50-20-30 | Published |
| Fine Vision (PhysIOL) |  |
1.8 | Neutral | +3.5/trifocal/+1.75 | Dependent (35/17/48) | Published |
| ReStor (ALCON) |  |
2.2 | −0.1-−0.2 | +4/+3/+2.5 | Dependent (50/50) | Published |
| Seelens MF (HANITA) |  |
1.8 | Neutral | +3 | Dependent (65/35) | Published |
| Tecnis MF (AMO) |  |
2.2 | −0.27 | +4/+3.25/+2.75 | Independent (50/50) | Published |
| Tecnis Symfony (AMO) |  |
2.2 | −0.27 Chromatic aberration correction | +3 Echellete expanded DOF | Independent Expanded DOF | Published |
| PanOptix (ALCON) |  |
2.2 | −0.1 | +3.25/trifocal/+2.17 | Independent (44/22/22) | Not yet published |
IOLs = Intraocular lenses, DOF = Depth of focus, N/F = Near/Far
Table 4.
Refractive technology intraocular lenses (II) show the main indications and possible symptoms of these intraocular lenses already published
| Refractive technology IOLs (II) | Intraocular optical quality | Contrast sensitivity | Worst outcome | Night vision | Better candidates |
|---|---|---|---|---|---|
| Mplus (Oculentis) +3 | +++ (plate haptic) | Not affected | All distances good | Sectorial halo | Not in extreme pupils |
| Mplus X (Oculentis) | +++ (plate haptic) | Not affected | Near vision | Sectorial halo+/− | Intermediate/functional vision |
| Rayner M-flex | NR | Decreased | All distances good? | Glare, halos | Bifocal |
IOLs = Intraocular lenses, NR = Not reported
Table 2.
Diffractive technology intraocular lenses (II) show the main indications and possible symptoms of these intraocular lenses already published
| Diffractive technology IOLs (II) | Intraocular optical quality | Contrast sensitivity | Worst outcome | Night vision | Better candidate |
|---|---|---|---|---|---|
| AT-LISA Bi/Tri (ZEISS) | +++ | Decreased | Intermediate vision/trifocal in study | Halos, glare | Universal (trifocal) |
| Fine Vision (PhysIOL) | +++ | Decreased +/− | In study | Halos, glare | Universal |
| ReStor (ALCON) +2.5/+3/+4 | ++++ | Decreased | Near vision limited in low add. Intermediate in +4 | Halos, glare | Costumized according to patients. Good pupil reactivity |
| Seelens MF (HANITA) | ++++ | Decreased | Intermediate | Halos, glare | Bifocal |
| Tecnis MF (AMO) +2.75/+3.25/+4 | +++ | Decreased | Near vision limited in low add. Intermediate in+4 | Halos+++ | Bifocal, pupil independent |
| Tecnis Symfony (AMO) | +++ | Decreased | Near vision | Halos−, glare− | Universal |
| PanOptix (ALCON) | +++ | +/− | Not yet published | Not yet published | Not yet published |
IOLs = Intraocular lenses
Table 3.
Refractive technology intraocular lenses (I) show the main models available of these intraocular lenses, their figures, and specific technical features as those with clinical studies published or not
| Refractive technology IOLs (I) | Figure | Incision size (mm) | Asphericity | Near add | Pupil dependence (percentage of light N/F) | Clinical studies |
|---|---|---|---|---|---|---|
| Mplus (Oculentis) |  |
2 | Neutral | +3/+1’5 | Independent between 2 and 6 mm (80/20) | Published |
| Mplus X (Oculentis) |  |
2 | Neutral | +3 plus Varifocal | Same | Not available |
| Rayner M-flex |  |
2.75 | Neutral | +4/+3 | Pupil dependent | Published |
IOLs = Intraocular lenses, N/F = Near/Far
Outcomes
The patient's satisfaction depends on careful and individualized selection based on the preexisting conditions, visual needs, and realistic expectations, and on the knowledge of the different optical designs and visual performances of the multifocal IOLs, and the proper surgical technique and eventual complications management.[1,4]
A recent meta-analysis of peer-reviewed publications revealed evidence of high levels of patient's satisfaction in general. The spectacle independence was 80% or more in 91.6% for distance vision, 100% for intermediate vision, and 70% for near vision in the different groups studied. The binocular uncorrected vision of 0.30 logMAR was achieved in 100% for distance visual acuity, 96% for intermediate visual acuity, and 97.3% for near visual acuity of the patients included in the study.[1,6]
The trifocal models are better for those patients who require a good intermediate vision. A study carried out by our group comparing the trifocal AT LISA tri 839MP (Carl Zeiss Meditec) and Fine Vision (PhysIOL). IOLs showed better visual acuities in intermediate vision with AT LISA tri 839MP.[8] The same study also compared the visual outcomes of the monofocal Acri. Smart 48S (Carl Zeiss Meditec) and the bifocal AcrySoft ReSTOR SN6AD1 (Alcon) IOLs. Considering distance vision, the monofocal Acri. Smart 48S (Carl Zeiss Meditec) and the trifocal AT LISA tri 839MP (Carl Zeiss Meditec) IOLs achieved better outcomes. Regarding the near-vision outcomes, there were no statistically significant differences among the multifocal IOLs analyzed.[8]
In contrast, previous review studies[9] and a recent prospective randomized controlled trial of 4 multifocal IOLs (Acrysof Restor SN6AD3 apodized multifocal, AT LISA 366D diffractive multifocal, Tecnis ZMA00 diffractive multifocal, and Rezoom refractive multifocal)[10] found no differences in the uncorrected distance visual acuity between the diffractive and refractive IOLs analyzed although concerning the uncorrected near visual acuity, the diffractive group had a better performance.[6,9,10]
In fact, there are new and more sophisticated multifocal IOLs, including the expanded depth of focus class that creates one elongated focal point. This emerging technology uses new methods to enhance the range of vision without splitting light rays aiming to improve patient expectations across all distances, and these lenses may be related to low incidence of photic phenomena, such as halos and glare. However, published evidence does not exist so far about the outcomes of these lenses, and studies are ongoing at this moment to demonstrate the potential advantages and/or the limitations of these new models based on their clinical performance.[6]
Complications and Treatment
The main reasons for patient dissatisfaction following a multifocal intraocular lens implantation are residual ametropia, posterior capsule opacification (PCO), dry eye, IOL decentration, inadequate pupil size, and wavefront abnormalities.[1,6]
Residual ametropia is one of the most common reasons of patient dissatisfaction after multifocal IOL implantation as the multifocal IOLs are more sensitive to residual refractive error. It may occur as result of inaccuracies in the biometric analysis, inadequate selection of the IOL power, limitations of the calculation formulas, or errors in the IOL position. The management with myopic and hyperopic laser in situ keratomileusis or photorefractive keratectomy enhancements after cataract surgery is shown to be efficient, predictable, and safe. When the excimer laser is not available, the option is the IOL exchange or piggyback lens implantation.[1,4]
PCO is very common and usually results in blurred vision and/or photopic phenomena in patients after long-term multifocal IOL implantation.[4,6] The higher rates of PCO were found in patients with hydrogel IOLs, rounded-edged IOLs, IOLs placed in the sulcus, and large capsulorhexis when compared to other materials, sharp posterior optic edge, placed in the capsular bag and small capsulorhexis, respectively.[11] The better solution for it is the capsulotomy with Nd:YAG laser, which is fast and has low rates of complications.[4,6,11] However, before the treatment with Nd:YAG laser, the surgeon should be sure that all other possible causes of patient dissatisfaction are treated or discarded as the risks of an IOL exchange are higher with a previous posterior capsulotomy.[4,6]
Dry eye is a multifactorial disease of the tear film and the ocular surface associated with discomfort, blurred vision, and photopic phenomena. Nevertheless, it is usual in the elderly population and, in addition, cataract surgery may induce or increase it mainly by reducing corneal sensitivity through the incision although the postoperative treatment may also play a role in that. The guidelines to treat dry eye include starting with eyelid hygiene and the use of artificial drops. Other options for more severe cases are the use of cyclosporine, punctual plugs implantation (especially in those with aqueous deficiency and no inflammation associated), and platelet-rich plasma drops.[4,6,12]
Inadequate pupil size affects the visual acuity after multifocal IOL implantation because the pupil size determines the multifocal IOLs zones used. Patients with very small postoperative pupils and complaining about poor near vision should be treated with the use of cyclopentolate drops or a 360° argon iridoplasty (0.5 s, 500 mW, and 500 micra). On the other hand, patients with very large postoperative pupils and complaints about increased photopic phenomena should be treated with brimonidine tartrate 0.2% drops.[1,4]
IOL decentration may affect visual function depending on the degree of decentration, the IOL design, and the pupil size. A study comparing the performance of two diffractive and two refractive multifocal IOLs with different levels of decentration in an eye model with a 3 mm pupil found that for the total diffractive structured ZM900, both far and near modulation transfer function (MTF) were affected starting at decentrations of 0.75 mm. MTF is an objective metric of contrast sensitivity representing the loss of contrast produced by the optics of the eye. MTF is therefore the ability of a lens system to display the ratio of image contrast to object contrast for ocular optics as a function of the spatial frequency of a sinusoidal grating.[13,14] For the diffractive, but with a monofocal peripheral part ReSTOR (+4) IOL, the near MTF decreases as the decentration degree increases while the far MTF tends to improve. For the refractive IOLs studied (ReZoom and SFX-MV1), the far MTF deteriorates starting at decentrations of 0.75 and 1 mm, respectively, with no changes in near MTF even in 1 mm decentrations.[15] The treatment with Argon laser iridoplasty avoids IOL explantation in the majority of the cases.[1,6] When necessary, the multifocal IOL explantation should be performed in the first 6 months after the surgery because of the scarring tissue that makes the surgery more difficult and so with higher complication risk. Another important factor to consider in the multifocal IOL explantation procedure is the presence of the capsular tension ring that makes the surgery easier.[16]
Conclusions
Multifocal IOLs are good options to correct pseudophakic presbyopia as they achieve spectacle independence in the majority of the cases with high levels of patient satisfaction. The visual needs of each patient should be carefully analyzed to choose the multifocal model that best fits their lifestyle.[1,2,6]
To obtain success after surgery, it is crucial to adequately select the patient, include an extensive preoperative evaluation of ocular surface and macula, as well as determine the correct IOL and surgical technique, because the several models have different visual performances. It is also very important to spend some chair time with the patient to explain all factors involved in the outcomes of the surgery and possible complications management.[6,8]
However, some patients may be dissatisfied and the most common complaints are blurred vision and photopic phenomena, usually due to residual refractive errors, PCO, dry eye, inadequate pupil size, wavefront abnormalities, and IOL decentration. Thus, most of these complications if managed properly may not affect the visual outcomes and the patient's satisfaction and quality of life.[1,6]
Financial support and sponsorship
Nil.
Conflicts of interest
The authors declare that there are no conflicts of interests of this paper.
References
- 1.Alió JL, Plaza-Puche AB, Fernandez-Buenaga R, Pikkel J, Maldonado M. Multifocal Intraocular Lenses: An Overview on the Technology, Indications, Outcomes, Complications and their Management. Survey of Ophthalmol. doi: 10.1016/j.survophthal.2017.03.005. In Review Process. [DOI] [PubMed] [Google Scholar]
- 2.Maurino V, Allan BD, Rubin GS, Bunce C, Xing W, Findl O. Moorfields IOL Study Group. Quality of vision after bilateral multifocal intraocular lens implantation: A randomized trial – AT LISA 809M versus AcrySof ReSTOR SN6AD1. Ophthalmology. 2015;122:700–10. doi: 10.1016/j.ophtha.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 3.Alio JL, Plaza-Puche AB, Javaloy J, Ayala MJ, Moreno LJ, Piñero DP. Comparison of a new refractive multifocal intraocular lens with an inferior segmental near add and a diffractive multifocal intraocular lens. Ophthalmology. 2012;119:555–63. doi: 10.1016/j.ophtha.2011.08.036. [DOI] [PubMed] [Google Scholar]
- 4.Alió JL, Pikkel J. Multifocal intraocular lenses: The art and the practice. Essentials in Ophthalmology. Switzerland: Springer International Publishing; 2014. [Google Scholar]
- 5.Alió JL, Vega-Estrada A, Plaza-Puche AB. Clinical outcomes with a new microincisional diffractive multifocal IOL. Eye Vis (Lond) 2015;2:2. doi: 10.1186/s40662-015-0012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rosen E, Alió JL, Dick HB, Dell S, Slade S. Efficacy and safety of multifocal intraocular lenses following cataract and refractive lens exchange: Metaanalysis of peer-reviewed publications. J Cataract Refract Surg. 2016;42:310–28. doi: 10.1016/j.jcrs.2016.01.014. [DOI] [PubMed] [Google Scholar]
- 7.Denoyer A, Le Lez ML, Majzoub S, Pisella PJ. Quality of vision after cataract surgery after Tecnis Z9000 intraocular lens implantation: Effect of contrast sensitivity and wavefront aberration improvements on the quality of daily vision. J Cataract Refract Surg. 2007;33:210–6. doi: 10.1016/j.jcrs.2006.10.035. [DOI] [PubMed] [Google Scholar]
- 8.Plaza-Puche AB, Alio JL. Analysis of defocus curves of different modern multifocal intraocular lenses. Eur J Ophthalmol. 2016;26:412–7. doi: 10.5301/ejo.5000780. [DOI] [PubMed] [Google Scholar]
- 9.Cochener B, Lafuma A, Khoshnood B, Courouve L, Berdeaux G. Comparison of outcomes with multifocal intraocular lenses: A meta-analysis. Clin Ophthalmol. 2011;5:45–56. doi: 10.2147/OPTH.S14325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rasp M, Bachernegg A, Seyeddain O, Ruckhofer J, Emesz M, Stoiber J, et al. Bilateral reading performance of 4 multifocal intraocular lens models and a monofocal intraocular lens under bright lighting conditions. J Cataract Refract Surg. 2012;38:1950–61. doi: 10.1016/j.jcrs.2012.07.027. [DOI] [PubMed] [Google Scholar]
- 11.Findl O, Buehl W, Bauer P, Sycha T. Interventions for preventing posterior capsule opacification. Cochrane Database Syst Rev. 2010:CD003738. doi: 10.1002/14651858.CD003738.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alio JL, Colecha JR, Pastor S, Rodriguez A, Artola A. Symptomatic dry eye treatment with autologous platelet-rich plasma. Ophthalmic Res. 2007;39:124–9. doi: 10.1159/000100933. [DOI] [PubMed] [Google Scholar]
- 13.Kawamorita T, Uozato H. Modulation transfer function and pupil size in multifocal and monofocal intraocular lenses in vitro . J Cataract Refract Surg. 2005;31:2379–85. doi: 10.1016/j.jcrs.2005.10.024. [DOI] [PubMed] [Google Scholar]
- 14.Prieto PM, Vargas-Martín F, Goelz S, Artal P. Analysis of the performance of the Hartmann-Shack sensor in the human eye. J Opt Soc Am A Opt Image Sci Vis. 2000;17:1388–98. doi: 10.1364/josaa.17.001388. [DOI] [PubMed] [Google Scholar]
- 15.Soda M, Yaguchi S. Effect of decentration on the optical performance in multifocal intraocular lenses. Ophthalmologica. 2012;227:197–204. doi: 10.1159/000333820. [DOI] [PubMed] [Google Scholar]
- 16.Fernández-Buenaga R, Alio JL, Muñoz-Negrete FJ, Barraquer Compte RI, Alio-Del Barrio JL. Causes of IOL explantation in Spain. Eur J Ophthalmol. 2012;22:762–8. doi: 10.5301/ejo.5000168. [DOI] [PubMed] [Google Scholar]


