Abstract
PURPOSE:
To report our experience in air-assisted manual dissection deep anterior lamellar keratoplasty (DALK) for the treatment of corneal scar with previous inflammation and fibrosis.
MATERIALS AND METHODS:
We retrospectively reviewed the medical history of 21 patients (male:female = 13:8 mean age 41.9 years old) with corneal pathology from previous infection and inflammation. Trephination diameter ranged from 7.0 to 8.0 mm, and the graft was oversized by 0.25–0.50 mm. Debulking technique was performed to expose Descemet's membrane after filling stroma with air. Starting from postoperative 3 months, selective suture removal was performed to reduce corneal astigmatism.
RESULTS:
The mean follow-up period was 59.9 ± 19.8 (20–96) months. Intraoperative microperforation occurred in 2 eyes (9.5%); however, there was no shift to penetrating keratoplasty. Air-bubble tamponade was performed in 7 eyes (33.3%) for postoperative gapping of the graft. There were 2 failed grafts (9.5%) due to corneal ulcer while all the other grafts remained clear throughout follow-up. The mean preoperative best-corrected visual acuity (BCVA) was 1.84 ± 0.66 logMAR, which improved to 0.74 ± 0.63 (P < 0.01). The average sphere power was − 0.88 ± 3.88 diopter (D), average cylinder power 3.03 ± 1.46D, and average endothelial count 1877 ± 375 cells/mm2.
CONCLUSION:
In severe ocular surface diseases, big-bubble technique frequently failed to separate predescemtic plane; however, it effectively created air-filled stroma which was easier to remove. Although BCVA was suboptimal due to ocular surface disorders, graft survival and clarity rate is high, justifying the application of DALK in these cases.
Keywords: Deep anterior lamellar keratoplasty, fibrosis, inflammation
Introduction
For the management of corneal opacity, penetrating keratoplasty (PKP) is preferred by most surgeons and has been considered as gold standard for a long time,[1] because the surgical technique is well developed, and optical outcome is relatively favorable.[2] However, there is a potential higher risk of graft failure and inferior tectonic strength of the wound after replacement of full-thickness cornea,[3,4] and the major reason of graft failure results from endothelial rejection.[5] More surgeons now choose lamellar keratoplasty to replace only the diseased part of the cornea while leaving the healthy Descemet's membrane (DM) and endothelium intact. This reduces the risk of endothelial cell (EC) loss and provides stable EC density (ECD) postoperatively, also avoids endothelium rejection, and thus provides higher graft survival rate.[6,7] The main indications for deep anterior lamellar keratoplasty (DALK) are corneal pathology not affecting endothelium, such as keratoconus, corneal scar, stromal dystrophies,[3] and other indications including therapeutic keratoplasty for corneal infection[8] and ocular surface reconstruction.[9]
In DALK procedures, several different stromal dissecting techniques aiming to bare DM have been reported. These techniques include “divide and conquer,” hydrodelamination,[10] viscodissection,[11] big-bubble,[12] and also air-viscobubble technique.[7] The goal in above-mentioned techniques is mainly to expose the DM (descemtic DALK) or at least to dissect into a predescemetic plane (predescemetic DALK).[13]
Big-bubble technique has gained popularity because of shorter surgical time, lower risk of perforation, and visual result comparable with PKP.[10,14] However, even the most experienced surgeons may fail to create big bubble but instead fill stroma with numerous small bubbles, especially if the corneal pathology is related to strong inflammation or fibrotic change on ocular surface.[15] Attempt to obtain a descemtic plane (descemtic DALK) may be very difficult in these situations,[15] and intraoperative complications such as DM microperforation might also occur when injecting the air, which require additional manipulation or conversion to PKP.[16]
In such challenging cases, meticulous layer-by-layer debulking technique to achieve maximal stromal removal may be the procedure of choice. Although variable thickness of stroma is often let behind, comparable optical result has been reported.[15] In this retrospective study, we collected cases with corneal opacity resulting from previous inflammatory ocular surface diseases and compare our result with outcome after DALK by debulking technique reported in previous literatures. To our knowledge, this is the first study to investigate efficacy and safety of manual dissection of DALK in these corneal pathologies.
Materials and Methods
Patients
We retrospectively reviewed the medical records of patients who had undergone DALK between 2008 and 2014 in the Department of Ophthalmology, Chang Gung Memorial Hospital, Linko. Patients with preoperative diagnoses of keratoconus, stromal dystrophy, or noninflammatory corneal scar such as scar after radial keratotomy were excluded from this study. A permission to conduct this retrospective analysis was obtained from the Institutional Review Board of Chang Gung Memorial Hospital, Linko.
Surgical technique
Preoperatively, corneal pachymetry was performed at the central cornea and at 12, 3, 6, and 9 o’clock along an 8 mm diameter. A 7.0–8.0 mm vacuum trephine was used to cut the recipient cornea down to about one-half in depth if the original central corneal thickness (CCT) was over 500 μm. When CCT was below 500 μm, an attempt was made to leave approximately 250 μm of posterior stroma. When the corneal thickness was very thin as in patient 5 and 10 whose CCT was only 240 and 130 μm, respectively, vacuum trephine was used only to cut through the epithelial layer along the superficial stroma. Once the vertical cut was made, lamellar dissection to remove the anterior stroma was performed with a crescent knife. A 27-gauge needle was inserted parallel the posterior stroma then removed. Then, a cannula connected to a 1 mL syringe was inserted into the track, and air was slowly injected into the stroma. Unlike keratoconus cornea in which a big bubble may form above the DM, after air injection, big bubble was difficult to form in these previously inflamed corneas. Instead, an air-containing, inflated stroma was formed. Air injection was performed at least at three different sites so that most of the posterior stroma became air-filled and foam-like. After removing the anterior stroma, in some patients, aqueous humor was aspirated to decompress the anterior chamber through paracentesis using a 27-gauge needle. A 15° sharp point knife was used to cut (but not penetrate) and divide the posterior stroma into four quadrants, and consecutively, each quadrant was further dissected with a crescent knife to expose the residual stromal tissue. At this point, the stromal bed was flushed with balanced salt solution, and because the residual stromal tissue will obscure the viewing of the iris, the third and last round of lamellar dissection will start from area containing the most residual stroma. In our practice, we did not intentionally expose the DM in each case as the chance of perforation increases by doing so. Rather, using the air injection-and-observation method, we remove the visible residual stromal tissue as best as possible until grossly the detail of the iris and lens can be seen. For very tiny stromal tissue, a specific forceps from Storz (cat. no. 64090) was used, which has a tip of concaved teeth that can be used as a hook to elevate the stromal fibers from the recipient bed. In area where DM was exposed, the intraocular pressure was lowered by paracentesis, viscoelastic material was injected to separate the residual stroma and DM, and then DALK spatula was inserted to extend the separation. If microperforation occurred during the procedure, an excised stromal tissue block was placed over the perforation site to prevent aqueous humor leakage, and surrounding stromal tissue was removed as best as possible. At the completion of the debulking procedure, DM was scrapped off from donor cornea, which was oversized by 0.25–0.5 mm. The donor cornea was sutured to recipient bed with 16 stitches of interrupted 10-0 nylon sutures. A therapeutic soft contact lens was inserted at the end of surgery.
Postoperatively, the patients received topical 0.1% betamethasone starting from hourly (gradually reduced to four times a day), levofloxacin four times a day, and Tobradex ointment twice a day (adjusted to daily). The patients were examined daily by slit lamp biomicroscopy and tonopen. Small gap between DM and graft tends to seal days later, but grossly detached DM from the graft especially with microperforation needs air tamponade by injecting air into anterior chamber and drainage of fluid from the junction of wound. Depending on the severity of astigmatism, selective suture removal/resuture started from postoperative 3 months, and all sutures were removed approximately within 2 years. Spectacle or rigid contact lens correction was performed every half year and so was specular microscopy.
Statistical analysis
Data including age, visual acuity, keratometry, refractive error, pachymetry, ECD, and postoperative follow-up period were analyzed by SPSS statistical software (IBM Corp., released 2011, IBM SPSS Statistics for Mac, version 20.0, IBM Corp., Armonk, NY, USA). P < 0.05 was considered to be statistically significant.
Institutional Review Board or Ethics Committee approval
This study was approved by Institutional Review Board of Chang Gung Medical Foundation in Taiwan (IRB No. 201600598B0) and adhered to tenets of the Declaration of Helsinki.
Results
Demographic, etiology, and graft condition
Twenty-one patients were included in this study. There were 13 males and 8 females. The mean age was 41.9 ± 21.8 (5–80) years old, and the mean follow-up period was 59.9 ± 19.8 (20–96) months. The corneal pathology was caused by herpes simplex virus (HSV) or other viral infection (n = 3), chemical burn (n = 2), dry eye syndrome due to graft-versus-host disease or rheumatoid arthritis (RA) (n = 3), neurotrophic keratopathy (n = 3), bacterial keratitis (n = 4), Stevens–Johnson syndrome (SJS, n = 2), ocular rosacea (n = 2), and penetrating trauma or laceration (n = 2). Table 1 summarizes patients’ gender, sex, corneal pathology, preoperative visual acuity, and surgical technique. Overall, the DALK surgeries were carried out with layer-by-layer manual stromal dissection to expose the DM after failure of big-bubble formation. The average recipient bed size was 7.46 ± 0.29 mm (7.0–8.0 mm), and the average donor cornea was 7.79 ± 0.34 mm (7.25–8.25 mm). The reason to slightly oversize the graft is to prevent flattening of the graft after suturing. Using this technique, the stromal tissue was successfully removed in 21 eyes [Figure 1]. No eyes required intraoperative conversion to PKP. Secondary procedure with air-bubble tamponade was performed in 7 eyes (33.3%) to seal the gap between the graft and DM.
Table 1.
Demographic and preoperative data
| Number/sex/age (years) | Eye | Corneal pathology | Underlying ocular condition | Recipient size (mm) | Donor size (mm) | Re-bubbling times | Outcome | Follow-up period (months) |
|---|---|---|---|---|---|---|---|---|
| 1/male/39 | OD | Chemical burn | 7.5 | 7.75 | 0 | Success | 66 | |
| 2/male/18 | OD | HSV keratitis | 7.5 | 8.0 | 1 | Success | 76 | |
| 3/female/31 | OS | SJS | Glaucoma | 7.5 | 7.75 | 1 | Success | 46 |
| 4/male/28 | OS | Corneal laceration | Glaucoma | 7.5 | 7.75 | 0 | Success | 45 |
| 5/female/55 | OS | Bacterial keratitis | PDR | 7.0 | 7.25 | 0 | Success | 64 |
| 6/male/5 | OS | Chemical burn | Amblyopia | 7.0 | 7.25 | 1 | Success | 72 |
| 7/female/35 | OD | Ocular rosacea/corneal ulcer | 7.0 | 7.25 | 0 | Success | 81 | |
| 8/female/34 | OS | SJS | 7.5 | 8.0 | 2 | Success | 53 | |
| 9/male/11 | OS | Neurotrophic keratopathy | 7.75 | 8.25 | 0 | Success | 53 | |
| 10/female/66 | OD | Bacterial keratitis | 7.5 | 8.0 | 2 | Success | 32 | |
| 11/female/77 | OS | Sicca syndrome | Dry eye | 7.5 | 7.75 | 0 | Success | 40 |
| 12/male/37 | OD | HSV keratitis | 8.0 | 8.25 | 2 | Success | 38 | |
| 13/male/9 | OD | Bacterial keratitis | 7.5 | 7.75 | 1 | Success | 72 | |
| 14/male/80 | OS | Neurotrophic keratopathy | 7.0 | 7.25 | 0 | Success | 87 | |
| 15/female/61 | OD | Penetrating trauma | Amblyopia | 7.5 | 8.0 | 0 | Success | 96 |
| 16/male/51 | OS | HSV keratitis | 7.5 | 7.75 | 0 | Success | 38 | |
| 17/male/36 | OD | Bacterial keratitis | 8.0 | 8.25 | 0 | Success | 38 | |
| 18/male/35 | OS | GVHD/dry eye, postcorneal ulcer | Dry eye | 7.5 | 8.0 | 0 | Success | 81 |
| 19/female/62 | OS | RA/dry eye, postcorneal ulcer | Dry eye | 7.5 | 7.75 | 0 | Success | 36 |
| 20/male/41 | OS | Neurotrophic keratopathy | Dry eye and exposure keratitis | 8.0 | 8.25 | 0 | Failure | 20 |
| 21/male69 | OD | Ocular rosacea/dry eye | Dry eye | 7.25 | 7.5 | 0 | Failure | 65 |
| Mean age: 41.9±21.8 | 7.46±0.29 | 7.79±0.34 | 59.9±19.8 |
OD = Right eye, OS = Left eye, HSV = Herpes simplex virus, SJS = Stevens-Johnson syndrome, PDR = Proliferative diabetic retinopathy, GVHD = Graft-versus-host disease, RA = Rheumatoid arthritis
Figure 1.
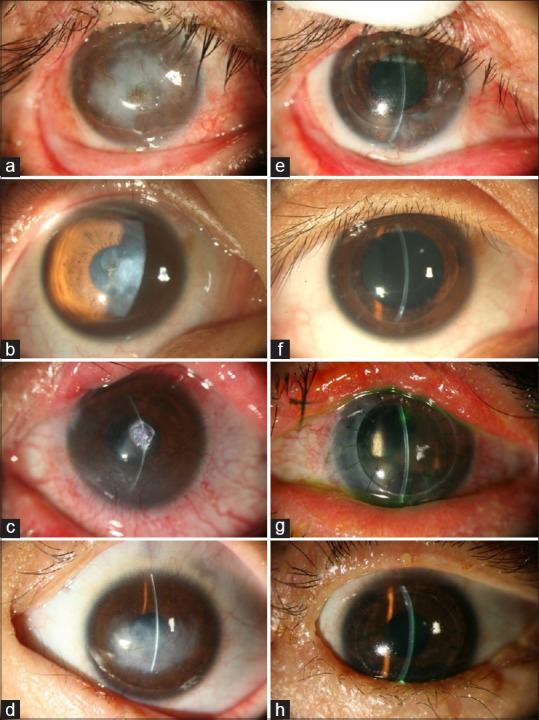
Representative pre- and post-operative photos of patients receiving DALK. (a) A 39-year-old male patient suffered from chemical burn OD. The corneal was reconstructed by conjunctivolimbal autograft with residual stromal opacity, and the vision was CF/30 cm. (e) The graft remained clear 5 years after DALK, and the BCVA reached 20/60. (b) A 18-year-old male suffered from HSV stromal keratitis OD, BCVA was 20/250. (f) Microperforation of DM was experienced during surgery, but the graft remained clear 5 years after DALK. The endothelial cell count was 1947/mm2, and BCVA was 20/25. (c) A 31-year-old female was a case of SJS with corneal scarring, neovascularization, and extreme thinning. Central corneal perforation OS was sealed with Histoacryl glue, and the vision was HM/20 cm. (g) Four years after DALK, the graft remained clear. Limited by preexisting advanced glaucoma, the BCVA was CF/60 cm. (d) An 11-year-old boy received meningioma excision with resulting neurotrophic and exposure keratitis OS. The vision was CF/10 cm. (h) The patient received DALK combined with permanent tarsorrhaphy. Four years after DALK, the graft remained clear, and the BCVA improved to 20/25 (DALK = Deep anterior lamellar keratoplasty, OD = Right eye, OS = Left eye, CF = Counting fingers, HM = Hand motion, HSV = Herpetic simplex virus, BCVA = Best-corrected visual acuity, SJS = Stevens–Johnson syndrome, DM = Descemet's membrane)
Visual outcome and refractive results
Two cases with graft failure due to late corneal ulcer (cases 20, 21) were excluded for visual outcome analysis. For the remaining 19 cases, Figure 2 and Table 2 shows comparison between pre- and post-operative best-corrected visual acuity (BCVA 1 year after surgery and afterward), refractive error, and keratometric readings. BCVA improved from hand motion (HM) to counting fingers (CF) in 3 (15.7%), Snellen acuity increased 1–3 lines in 6 (31.5%), 4–6 lines in 4 (21.1%), and more than 7 lines increase in 4 (21.1%). The average final BCVA after DALK was logMAR 0.74 ± 0.63 (0–2.0). A statistically significant improvement in visual acuity was observed compared with preoperative BCVA (logMAR 1.84 ± 0.66; P < 0.01). Inferior visual outcome was observed in cases with preexisting advanced glaucoma (Case 3), postoperative corneal interface opacity (cases 8 and 14), and also cases with preexisting deprivation amblyopia (cases 6 and 15) or diabetic retinopathy (Case 5). There was great variation in postoperative spherical power ranging from − 10 to + 7.75D (mean: −0.88 ± 3.88D). The average cylinder power was 3.03 ± 1.46D (0–8.5D).
Figure 2.
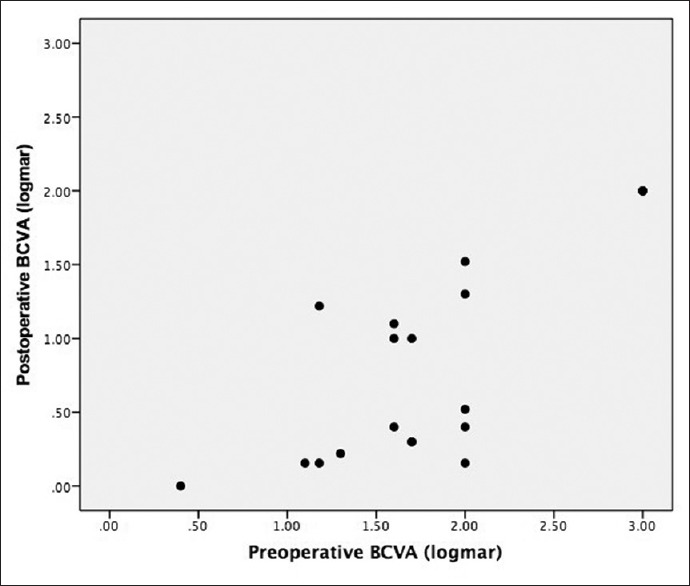
Scatter plot between pre- and post-operative best-corrected visual acuity
Table 2.
Preoperative and postoperative data
| Case number | Preoperative | Postoperative | Total | KM cylinder (D) | Preoperative CCT (µm) | Postoperative CCT (µm) | EC count | Subsequent surgeries | Complications | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BCVA | LogMAR | BCVA | LogMAR | Spherical (D) | Cylinder (D) | |||||||
| 1 | CF/30 | 2 | 0.3 | 0.52 | 1 | 3 | 5.25 | 401 | 540 | 1909 | Pannus excision, AMT | |
| 2 | 0.08 | 1.1 | 0.7 | 0.155 | −2.25 | 6 | 5 | 377 | 650 | 1947 | DM tear | |
| 3 | HM/20 | 3 | CF/60 | 2 | 7.75 | 0.25 | 5.5 | 240 | 297 | NA | Cataract | |
| 4 | 0.07 | 1.18 | 0.7 | 0.155 | −10 | 1.5 | 2 | 469 | 490 | 2336 | Trabeculectomy | |
| 5 | CF/80 | 2 | 0.05 | 1.3 | NA | NA | 10 | 738 | 504 | 1526 | ||
| 6 | HM/100 | 3 | CF/20 | 2 | −6.25 | 3 | 5 | 395 | 537 | 1265 | Resuture | |
| 7 | 0.05 | 1.3 | 0.6 | 0.22 | −8.5 | 2.75 | 4.5 | 250 | 591 | NA | AMD, tarsorrhaphy | PED |
| 8 | 0.01 | 1.18 | 0.06 | 1.22 | 7.5 | 0.25 | 2.5 | 130 | 560 | NA | Interface opacity (fibrosis), cataract | |
| 9 | CF/10 | 2 | 0.7 | 0.155 | −0.25 | 4 | 0.6 | 600 | 643 | 2217 | Tarsorrhaphy | |
| 10 | 0.02 | 1.7 | 0.1 | 1 | 2.25 | 3.75 | 2.75 | 524 | 691 | 1812 | ||
| 11 | HM/60 | 3 | CF/60 | 2 | 7.5 | 0 | 2.5 | 713 | 600 | 1984 | AMT | PED |
| 12 | 0.03 | 1.6 | 0.4 | 0.4 | 1 | 1.5 | 6 | 550 | 555 | 2139 | Reform AC, resuture | DM tear, DMF |
| 13 | 0.02 | 1.7 | 0.5 | 0.3 | −0.3 | 8.5 | 5.5 | 350 | 502 | 2272 | ||
| 14 | CF/50 | 2 | 0.03 | 1.52 | NA | NA | 6.2 | 378 | 498 | 2129 | Interface opacity | |
| 15 | 0.03 | 1.6 | 0.08 | 1.1 | 7.5 | 4 | 3 | 395 | 771 | 1854 | ||
| 16 | 0.03 | 1.6 | 0.1 | 1 | NA | NA | NA | 345 | 608 | NA | AMT, tissue glue | PED |
| 17 | 0.4 | 0.4 | 1.0 | 0 | 0.25 | 2.5 | 1.25 | 274 | 575 | NA | ||
| 18 | 0.02 | 1.7 | 0.5 | 0.3 | 3.75 | 5.5 | NA | 501 | 562 | 1845 | ||
| 19 | CF/30 | 2 | 0.4 | 0.4 | 2.25 | 1.75 | NA | 420 | 501 | 1042 | AMT | PED |
| Mean | 1.84±0.66 | 0.74±0.63 | −0.88±3.88 | 3.03±1.46 | 3.89±2.67 | 423.7±156.0 | 561.9±97.3 | 1876.9±375.4 | ||||
| P | 0.01* | 0.002* | ||||||||||
*P≤0.05, statistically significant. BCVA = Best-corrected visual acuity, LogMAR = Logarithm of the minimal angle of resolution, CCT = Central corneal thickness, EC = Endothelial cell, KM = Keratometry, CF = Counting finger, HM = Hand motion, NA = Not available, AMD = Amniotic membrane dressing, AMT = Amniotic membrane transplantation, AC = Anterior chamber, DM = Descemet's membrane, PED = Persistent epithelium defect, DMF = Descemet's membrane folding
Pachymetry and corneal endothelial density
Table 2 lists the pre- and post-operative pachymetry and demonstrated a statistically significant increase in CCT after surgery (561.9 ± 97.3 μm vs. 423.7 ± 156.0 μm; P= 0.002). All images of the preoperative corneal endothelium were not recognizable due to dense corneal opacity; therefore, the preoperative EC count was not available. After 12 months, mean ECD was 1877 ± 375 cell/mm2 in 14 cases while 3 eyes were unable to obtain EC count due to interface opacity and residual corneal scar after DALK, and two cases refused to have this examination. In our study, only four patients (patients 3, 6, 8, and 10) received postoperative anterior segment OCT examination, and the mean residual stromal thickness was 32.4 ± 10.40 (23.2–41.7) μm.
Complications
Postoperative complications are summarized in Table 2. The common intraoperative complication was DM tear (n = 2), which occurred during manual stromal dissection. DM folding was noted in 1 (5%) eyes with history of herpes simplex keratitis (HSK), and the fold did not resolve through the follow-up.
Clear graft-host interface was observed postoperatively in 19 of 21 eyes (90%) while interface opacity was identified in 2 (10%; one case with SJS and the other with neurotrophic keratopathy). Interface opacity remained unchanged in both eyes, resulting in poorer visual outcome.
Delayed reepithelialization (persistent epithelium defect over 1 month) after surgery was observed in 4 (19%) eyes and required amniotic membrane transplantation/dressing as a subsequent surgery. Sicca syndrome was the most common corneal pathology (2 eyes); the other causes include HSK scar (n = 1) and ocular rosacea (n = 1). Tarsorrhaphy was necessary to promote reepithelialization in one case with ocular rosacea and another with neurotrophic keratopathy.
Postoperative glaucoma occurred in 1 eye (5%), which was secondary to the use of topical steroid, and was successfully treated with trabeculectomy. There is no epithelial rejection or stromal rejection. Postoperative transient grafts edema all responded well to intensive corticosteroid, graft regained clarity within 1 month of treatment.
Discussion
Corneal stromal disease (opacity, scar, etc.) that occurred after episode of inflammation or fibrosis can affect visual outcome to various extent.[17,18] In previous practice, traditional PKP was considered effective for visual rehabilitation; however, studies have shown that incidence of graft failure increased especially in patients with previous herpetic keratitis.[19,20] In addition, other ocular surface diseases such as chemical burn, dry eye, SJS, ocular rosacea, and RA manifesting as neovascularization and inflammation have also been shown to compromise graft survival.
The most important advantage of DALK is to preserve healthy recipient endothelium and prevent endothelial rejection. Compared with PKP, DALK has been reported to have lower mean annual EC loss rate (5.8% vs. 14.2%; Kubaloglu et al.[21]), lower EC loss rate at postoperative 12 months (12.9% vs. 27.7%; Cheng et al.[22]), and higher EC count at postoperative 24 months (1900/mm2 vs. 1416/mm2; Kim et al.[23]). In this study, we evaluate the efficacy and safety of manually dissected DALK in above-mentioned recalcitrant corneal conditions.
In previous literature, low success rate to expose DM was observed in some corneal pathology such as scar following bacterial keratitis;[15] and complications such as DM rupture were likely to occur when performing pneumatic dissection (big-bubble technique) in corneas with extensive scar.[24] Despite this fact, after corneal stroma is inflated with air and becomes foam-like, it appears that the residual stromal tissue could be dissected easier. Such air-assisted manual DALK was first reported by Balestrazzi et al.[25] and Leccisotti.[26] Because we were very cautious when approaching the DM, the resulting rate of DM tear was around 11%, which was lower than Melles's original paper which reported a 14% incidence of microperforation with his lamellar dissection technique.[27] In this report, none of our patients had intraoperative conversion to PKP. Furthermore, the visual results of patient with DM perforation did not differ significantly from patients with intact DM. This finding is similar to that reported by Sugita and Kondo.[28] Two years after surgery, the EC count was 1947 and 2139 cells/mm,2 respectively, for the two patients with microperforation (cases 2 and 12), suggesting that with careful manipulation, DALK can still be preceded without significant loss of ECs.
Compared with previous reports for DALK for keratoconus, our study showed similar endothelial count at postoperative 2 years (1876 vs. 1900; Kim et al.[23]), similar refractive astigmatism (3.0 D vs. 3.37D; Cheng et al.[22]), but smaller myopic shift (−0.88D vs. −4.68D; Amayem et al.[29]). However, the overall visual outcome in our patients was inferior to other reports using lamellar keratoplasty and big-bubble technique for keratoconus.[30,31] Nevertheless, relative poor visual outcome (BCVA < 20/200) was only found in eyes with coexisting amblyopia, diabetic retinopathy, advanced glaucoma, and postoperative persistent epithelial defect, otherwise most of the postoperative complications were similar to previous studies.[32] However, this study presented with higher rate of ocular surface problem such as lagophthalmos, sicca syndrome, and SJS. The related delayed epithelial reepithelialization and recurrent epithelial erosion need therapeutic contact lens, tarsorrhaphy, amniotic membrane dressing, or grafting to augment reepithelialization. Sometimes, the cornea is healed with uneven surface, which is detrimental to visual recovery.
Another factor contributing to poorer visual performance was interface scarring and irregularities, especially if the plane of lamellar separation is not deep enough.[33] There were 2 eyes with graft-host interface opacity after DALK (cases 8 and 14), which resulted in poor visual outcome. Big-bubble procedure, the most reliable technique in baring DM, has been routinely performed in DALK with favorable visual outcome; however, the success rate for fibrotic corneas was much lower than keratoconus.[34,35] According to previous studies, which compared successful and unsuccessful big-bubble technique, retention of posterior stroma after attempted DM baring might delay visual recovery, yet there was no significant difference in postoperative visual acuity.[7,36,37] The use of “divide-and-conquer” and “hydration-and-observation” technique in our study for stromal lamellar dissection after initial attempt of pneumatic dissection allows maximal removal of stromal tissue, leaving dissecting plane very close to DM. It has been reported that eyes with a residual stromal thickness less than 20 μm had visual acuities similar to eyes after PKP, whereas those with a residual thickness more than 80μm had a significantly reduced visual acuity.[38] The mean residual stromal thickness in this study was 32.4 μm, which was similar to the report by Knutsson et al. (30.5 μm),[39] but much thinner than that by Borderie et al. (87 μm).[40]
Conclusion
In the presence of healthy recipient endothelium, DALK is more feasible in that it does not cause immune-mediated endothelial rejection; therefore, DALK is preferable than PKP in restoring stromal clarity in severe ocular surface diseases such as chemical burn, SJS, and ocular rosacea as shown in this study. Despite sometimes very time-consuming, the surgery is worth doing in that long-term graft survival is more likely than PKP. However, in patients with compromised ocular surface defense, any form of keratoplasty should be performed cautiously; and therapeutic contact lens, amniotic membrane dressing or grafting, or tarsorrhaphy should be performed timely when patients are at high risk of postoperative delayed reepithelialization.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors declare that there are no conflicts of interests of this paper.
References
- 1.Sögütlü Sari E, Kubaloglu A, Ünal M, Piñero Llorens D, Koytak A, Ofluoglu AN, et al. Penetrating keratoplasty versus deep anterior lamellar keratoplasty: Comparison of optical and visual quality outcomes. Br J Ophthalmol. 2012;96:1063–7. doi: 10.1136/bjophthalmol-2011-301349. [DOI] [PubMed] [Google Scholar]
- 2.al Faran MF, Tabbara KF. Corneal dystrophies among patients undergoing keratoplasty in Saudi Arabia. Cornea. 1991;10:13–6. [PubMed] [Google Scholar]
- 3.Reinhart WJ, Musch DC, Jacobs DS, Lee WB, Kaufman SC, Shtein RM. Deep anterior lamellar keratoplasty as an alternative to penetrating keratoplasty a report by the american academy of ophthalmology. Ophthalmology. 2011;118:209–18. doi: 10.1016/j.ophtha.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 4.Borderie VM, Boëlle PY, Touzeau O, Allouch C, Boutboul S, Laroche L. Predicted long-term outcome of corneal transplantation. Ophthalmology. 2009;116:2354–60. doi: 10.1016/j.ophtha.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 5.Patel SV, Hodge DO, Bourne WM. Corneal endothelium and postoperative outcomes 15 years after penetrating keratoplasty. Am J Ophthalmol. 2005;139:311–9. doi: 10.1016/j.ajo.2004.09.045. [DOI] [PubMed] [Google Scholar]
- 6.Chen G, Tzekov R, Li W, Jiang F, Mao S, Tong Y. Deep anterior lamellar keratoplasty versus penetrating keratoplasty: A meta-analysis of randomized controlled trials. Cornea. 2016;35:169–74. doi: 10.1097/ICO.0000000000000691. [DOI] [PubMed] [Google Scholar]
- 7.Sarnicola V, Toro P, Sarnicola C, Sarnicola E, Ruggiero A. Long-term graft survival in deep anterior lamellar keratoplasty. Cornea. 2012;31:621–6. doi: 10.1097/ICO.0b013e31823d0412. [DOI] [PubMed] [Google Scholar]
- 8.Sarnicola E, Sarnicola C, Sabatino F, Tosi GM, Perri P, Sarnicola V. Early deep anterior lamellar keratoplasty (DALK) for acanthamoeba keratitis poorly responsive to medical treatment. Cornea. 2016;35:1–5. doi: 10.1097/ICO.0000000000000681. [DOI] [PubMed] [Google Scholar]
- 9.Fogla R, Padmanabhan P. Deep anterior lamellar keratoplasty combined with autologous limbal stem cell transplantation in unilateral severe chemical injury. Cornea. 2005;24:421–5. doi: 10.1097/01.ico.0000151550.51556.2d. [DOI] [PubMed] [Google Scholar]
- 10.Amayem AF, Anwar M. Fluid lamellar keratoplasty in keratoconus. Ophthalmology. 2000;107:76–9. doi: 10.1016/s0161-6420(99)00002-0. [DOI] [PubMed] [Google Scholar]
- 11.Melles GR, Remeijer L, Geerards AJ, Beekhuis WH. A quick surgical technique for deep, anterior lamellar keratoplasty using visco-dissection. Cornea. 2000;19:427–32. doi: 10.1097/00003226-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Archila EA. Deep lamellar keratoplasty dissection of host tissue with intrastromal air injection. Cornea 1984. 1985;3:217–8. [PubMed] [Google Scholar]
- 13.Sarnicola V, Toro P. Blunt cannula for descemetic deep anterior lamellar keratoplasty. Cornea. 2011;30:895–8. doi: 10.1097/ICO.0b013e3181e848c3. [DOI] [PubMed] [Google Scholar]
- 14.Anwar M, Teichmann KD. Big-bubble technique to bare Descemet's membrane in anterior lamellar keratoplasty. J Cataract Refract Surg. 2002;28:398–403. doi: 10.1016/s0886-3350(01)01181-6. [DOI] [PubMed] [Google Scholar]
- 15.Huang T, Zhang X, Wang Y, Zhang H, Huand A, Gao N. Outcomes of deep anterior lamellar keratoplasty using the big-bubble technique in various corneal diseases. Am J Ophthalmol. 2012;154:282–9.e1. doi: 10.1016/j.ajo.2012.02.025. [DOI] [PubMed] [Google Scholar]
- 16.Sarnicola V, Toro P. Deep anterior lamellar keratoplasty in herpes simplex corneal opacities. Cornea. 2010;29:60–4. doi: 10.1097/ICO.0b013e3181a317d3. [DOI] [PubMed] [Google Scholar]
- 17.Yalniz-Akkaya Z, Burcu Nurozler A, Yildiz E, Onat M, Budak K, Duman S. Repeat penetrating keratoplasty: Indications and prognosis, 1995-2005. Eur J Ophthalmol. 2009;19:362–8. doi: 10.1177/112067210901900306. [DOI] [PubMed] [Google Scholar]
- 18.Al-Mezaine H, Wagoner MD King Khaled Eye Specialist Hospital Cornea Transplant Study Group. Repeat penetrating keratoplasty: Indications, graft survival, and visual outcome. Br J Ophthalmol. 2006;90:324–7. doi: 10.1136/bjo.2005.079624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Epstein RJ, Seedor JA, Dreizen NG, Stulting RD, Waring GO, 3rd, Wilson LA, et al. Penetrating keratoplasty for herpes simplex keratitis and keratoconus. Allograft rejection and survival. Ophthalmology. 1987;94:935–44. doi: 10.1016/s0161-6420(87)33356-1. [DOI] [PubMed] [Google Scholar]
- 20.Ficker LA, Kirkness CM, Rice NS, Steele AD. Longterm prognosis for corneal grafting in herpes simplex keratitis. Eye (Lond) 1988;2(Pt 4):400–8. doi: 10.1038/eye.1988.73. [DOI] [PubMed] [Google Scholar]
- 21.Kubaloglu A, Koytak A, Sari ES, Akyol S, Kurnaz E, Ozerturk Y. Corneal endothelium after deep anterior lamellar keratoplasty and penetrating keratoplasty for keratoconus: A four-year comparative study. Indian J Ophthalmol. 2012;60:35–40. doi: 10.4103/0301-4738.90490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheng YY, Visser N, Schouten JS, Wijdh RJ, Pels E, van Cleynenbreugel H, et al. Endothelial cell loss and visual outcome of deep anterior lamellar keratoplasty versus penetrating keratoplasty: A randomized multicenter clinical trial. Ophthalmology. 2011;118:302–9. doi: 10.1016/j.ophtha.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 23.Kim MH, Chung TY, Chung ES. A retrospective contralateral study comparing deep anterior lamellar keratoplasty with penetrating keratoplasty. Cornea. 2013;32:385–9. doi: 10.1097/ICO.0b013e318254be4e. [DOI] [PubMed] [Google Scholar]
- 24.Scorcia V, Beltz J, Busin M. Small-bubble deep anterior lamellar keratoplasty technique. JAMA Ophthalmol. 2014;132:1369–71. doi: 10.1001/jamaophthalmol.2014.2756. [DOI] [PubMed] [Google Scholar]
- 25.Balestrazzi A, Malandrini A, Traversi C, Martone G, Caporossi A. Air-guided manual deep anterior lamellar keratoplasty: Long-term results and confocal microscopic findings. Eur J Ophthalmol. 2007;17:897–903. doi: 10.1177/112067210701700605. [DOI] [PubMed] [Google Scholar]
- 26.Leccisotti A. Air-assisted manual deep anterior lamellar keratoplasty for treatment of herpetic corneal scars. Cornea. 2009;28:728–31. doi: 10.1097/ICO.0b013e3181930a7e. [DOI] [PubMed] [Google Scholar]
- 27.Melles GR, Remeijer L, Geerards AJ, Beekhuis WH. The future of lamellar keratoplasty. Curr Opin Ophthalmol. 1999;10:253–9. doi: 10.1097/00055735-199908000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Sugita J, Kondo J. Deep lamellar keratoplasty with complete removal of pathological stroma for vision improvement. Br J Ophthalmol. 1997;81:184–8. doi: 10.1136/bjo.81.3.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Amayem AF, Hamdi IM, Hamdi MM. Refractive and visual outcomes of penetrating keratoplasty versus deep anterior lamellar keratoplasty with hydrodissection for treatment of keratoconus. Cornea. 2013;32:e2–5. doi: 10.1097/ICO.0b013e31825ca70b. [DOI] [PubMed] [Google Scholar]
- 30.Fogla R, Padmanabhan P. Results of deep lamellar keratoplasty using the big-bubble technique in patients with keratoconus. Am J Ophthalmol. 2006;141:254–9. doi: 10.1016/j.ajo.2005.08.064. [DOI] [PubMed] [Google Scholar]
- 31.Sarnicola V, Toro P, Gentile D, Hannush SB. Descemetic DALK and predescemetic DALK: Outcomes in 236 cases of keratoconus. Cornea. 2010;29:53–9. doi: 10.1097/ICO.0b013e3181a31aea. [DOI] [PubMed] [Google Scholar]
- 32.Han DC, Mehta JS, Por YM, Htoon HM, Tan DT. Comparison of outcomes of lamellar keratoplasty and penetrating keratoplasty in keratoconus. Am J Ophthalmol. 2009;148:744–51.e1. doi: 10.1016/j.ajo.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 33.Trimarchi F, Poppi E, Klersy C, Piacentini C. Deep lamellar keratoplasty. Ophthalmologica. 2001;215:389–93. doi: 10.1159/000050894. [DOI] [PubMed] [Google Scholar]
- 34.Silva CA, Schweitzer de Oliveira E, Souza de Sena Júnior MP, Barbosa de Sousa L. Contrast sensitivity in deep anterior lamellar keratoplasty versus penetrating keratoplasty. Clinics (Sao Paulo) 2007;62:705–8. doi: 10.1590/s1807-59322007000600008. [DOI] [PubMed] [Google Scholar]
- 35.Bahar I, Kaiserman I, Srinivasan S, Ya-Ping J, Slomovic AR, Rootman DS. Comparison of three different techniques of corneal transplantation for keratoconus. Am J Ophthalmol. 2008;146:905–12.e1. doi: 10.1016/j.ajo.2008.06.034. [DOI] [PubMed] [Google Scholar]
- 36.Bhatt UK, Fares U, Rahman I, Said DG, Maharajan SV, Dua HS. Outcomes of deep anterior lamellar keratoplasty following successful and failed ’big bubble’. Br J Ophthalmol. 2012;96:564–9. doi: 10.1136/bjophthalmol-2011-300214. [DOI] [PubMed] [Google Scholar]
- 37.Feizi S, Einollahi B, Yazdani S, Hashemloo A. Graft biomechanical properties after penetrating keratoplasty in keratoconus. Cornea. 2012;31:855–8. doi: 10.1097/ICO.0b013e31823f8ce4. [DOI] [PubMed] [Google Scholar]
- 38.Ardjomand N, Hau S, McAlister JC, Bunce C, Galaretta D, Tuft SJ, et al. Quality of vision and graft thickness in deep anterior lamellar and penetrating corneal allografts. Am J Ophthalmol. 2007;143:228–35. doi: 10.1016/j.ajo.2006.10.043. [DOI] [PubMed] [Google Scholar]
- 39.Knutsson KA, Rama P, Paganoni G. Modified big-bubble technique compared to manual dissection deep anterior lamellar keratoplasty in the treatment of keratoconus. Acta Ophthalmol. 2015;93:431–8. doi: 10.1111/aos.12705. [DOI] [PubMed] [Google Scholar]
- 40.Borderie VM, Sandali O, Bullet J, Gaujoux T, Touzeau O, Laroche L. Long-term results of deep anterior lamellar versus penetrating keratoplasty. Ophthalmology. 2012;119:249–55. doi: 10.1016/j.ophtha.2011.07.057. [DOI] [PubMed] [Google Scholar]


