Abstract
Acanthamoeba keratitis (AK) is an unusual infectious disease of the cornea which sometimes leads to blindness. We report the experience of adding oral voriconazole in conjunction with topical antiacanthamoebic drops to treat refractory AK. A 20-year-old girl experienced a deep stromal keratitis with large epithelial defect in the left eye, suspected as AK. The initial best-corrected visual acuity (BCVA) of the eye was counting finger. She received topical chlorhexidine 0.02% and voriconazole 1% during the first 14 days but in vain. Oral voriconazole was administered and resulted in a rapid regression of the lesion. A total resolution was achieved after 2 weeks of triple combination therapy. The BCVA of the left eye finally achieved 20/20 at 6-month follow-up. Although oral voriconazole was seldom used in treating acute AK, the additional use of oral voriconazole combined with topical antiacanthamoebic drugs may help to achieve a successful treatment effect in refractory stromal AK.
Keywords: Acanthamoeba keratitis, oral voriconazole, resistant, stromal keratitis
Introduction
Acanthamoeba keratitis (AK) is an unusual infectious disease of cornea. The most common risk factor is soft contact lens wear. Others include exposure to water sources, chronic ocular surface disease, ocular trauma, and concomitant infectious keratitis.[1] The prognosis of AK has improved in the past 2 decades.[2] The diamidines (i.e., propamidine and hexamidine) and biguanides (i.e., polyhexamethylene biguanide and chlorhexidine) are currently the most effective cysticidal antiamoebics in vitro and their use is supported by many case series.[3] Recent case reports also indicated topical voriconazole 1% as an adjunct to biguanide and diamidine therapy in refractory cases.[4] However, delayed diagnosis and ineffective treatment can lead to a poor prognosis.[3] Worse factors include visual acuity of < 20/50 and more severe disease, such as stromal involvement, at presentation.[5] The uncontrolled cases will progress to ulceration, anterior uveitis with or without hypopyon, and even corneal perforation.[6] In literature, oral voriconazole is seldom used in acute AK. We reported a young girl with resistant stromal AK finally treated successfully with adjuvant oral voriconazole.
Case Report
A 20-year-old girl wore orthokeratology lenses for years and used to clean the contact lenses with water from drinking fountain. The patient felt discomfort in the left eye off and on for 2 months and received topical levofloxacin eyedrops. The symptoms progressed to pain, photophobia, and tearing abruptly in 2 days, and the patient was referred to our clinic for severely stromal keratitis of the left eye. Visual acuity was 20/20 and counting finger in the right and the left eye, respectively. The left cornea demonstrated a large, irregular epithelial defect measuring 5 mm horizontally and 4.5 mm vertically accompanied with a deep stromal keratitis and radial neuritis [Figure 1a] on the 1st day of hospitalization. After taking samples from the scraped cornea and the lens cases, microbiological cultures for bacteria, fungus, and Acanthamoeba and polymerase chain reaction for Acanthamoeba were performed. The patient was started on topical chlorhexidine gluconate 0.02% and levofloxacin 0.5% ophthalmic solution hourly. On the 3rd day of hospitalization, the condition did not improve [Figure 1b] and topical voriconazole 1% was instituted hourly as an adjuvant for both fungal and Acanthamoeba infection. Surgical debridement and repeat cultures were performed on the third and 12th day of hospitalization due to no organism found in the prior samples and new stromal infiltration was noted [Figure 1c and d]. The results finally confirmed the presence of Acanthamoeba on the 13th day of hospitalization. On the 15th day of hospitalization, after discussion with her family, oral voriconazole 200 mg twice daily was added to the concurrent therapies, which resulted in a rapid and almost complete resolution of the corneal inflammation [Figure 2a-d]. The triple combination therapy consisting of topical chlorhexidine gluconate 0.02% and voriconazole 1% and oral voriconazole was continued for a total of 1-month duration, followed by slowly tapering of the topical medications over the next 2 months. Liver function tests were normal throughout the course of treatment. Best-corrected visual acuity (BCVA) returned to 20/30 in the left eye 2 months from the initial treatment, and the cornea remained quiet. Final BCVA achieved 20/20 in the left eye 6 months later.
Figure 1.
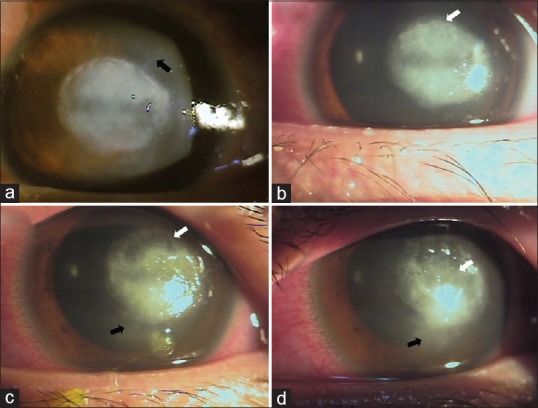
(a) The 1st day of hospitalization, a deep stromal keratitis with radial neuritis (black arrow) can be found. (b) The 3rd day, partial keratectomy was performed at the location that white arrow indicated. (c) The 10th day, new stromal infiltration (black arrow) was found. The darker area (white arrow) was the location that received keratectomy on the 3rd day. (d) The 12th day, the stromal infiltration (black arrow) progressed. The second partial keratectomy was performed at the location that white arrow indicated. This is the postoperative picture
Figure 2.
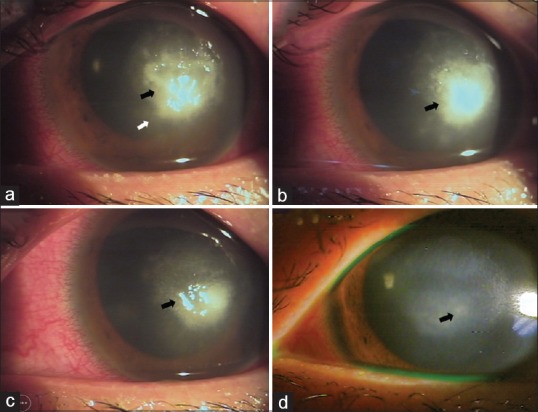
(a) The 16th day of hospitalization. The infiltration area (white arrow) became less prominent after taking oral voriconazole for only 1 day. (b-d) The 20th, 24th, 39th day, respectively, the infiltration area (black arrow) decreased day by day and finally became faint scar
Discussion
Biguanides and diamidines are currently available and most often used antiacanthamoebal agents offering both trophozoicidal and cysticidal effects. Clinically, a combination therapy of topical biguanides and diamidines, topical biguanides and antifungals, or topical biguanides and oral ketoconazole has been utilized to overcome high resistance of Acanthamoebal cysts. Diamidines, however, are still unavailable in some places. Studies have been seeking for more effective managements especially in treating more advanced cases.
Voriconazole, an antifungal agent, has been proved to have good cysticidal effect against Acanthamoeba through in vitro study.[7] Although the activity of topical voriconazole and chlorhexidine against AK were similar in the other study, they believe topical voriconazole has better corneal and anterior chamber penetration and lower cellular toxicity on cornea than topical chlorhexidine.[8] Successful treatment of chlorhexidine- and polyhexamethylene biquanide (PHMB)-resistant AK with voriconazole 1% as an adjuvant has been reported.[4] Oral voriconazole, on the other hand, is believed to be effective for chronic stromal AK as monotherapy and for intraocular disseminated AK in combination with chlorhexidine and topical voriconazole, making it a promising alternative for refractory AK.[2,9] In our case, acute stromal AK resistant to topical chlorhexidine and voriconazole also had a good response to additional oral voriconazole. Due to clinically ambiguous presentation of Acanthamoeba and fungal keratitis, as well as lack of microbiological evidence, early combination of topical voriconazole 1% and chlorhexidine was chosen to treat severe epithelial and stromal inflammation. However, a rapid resolution was obtained only after application of oral voriconazole. Arnalich-Montiel et al. have suggested oral voriconazole to achieve a more sustained therapeutic dose, which turns out to be more efficient for severe stromal AK.[9] The disease course is shorter in our case than those reported by Tu et al. who elected oral voriconazole as monotherapy after recurrence of stromal AK.[2] We used oral voriconazole in addition to topical chlorhexidine and voriconazole after 2 weeks initially ineffective treatment. The inflammation regressed in 1 month and there was no recurrent disease. She had her final BCVA 20/20 in her affected eye. Early intervention of this triple combination therapy prevents AK from further deteriorating and provides fast recovery.
In conclusion, we report a successful treatment of severe stromal AK by using oral voriconazole combined with topical chlorhexidine and voriconazole. We believe this triple combination therapy to be a potential regimen for AK refractory to traditional antiacanthamoebal medications, especially those with deep stromal involvement.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors declare that there are no conflicts of interests of this paper.
References
- 1.Tanhehco T, Colby K. The clinical experience of acanthamoeba keratitis at a tertiary care eye hospital. Cornea. 2010;29:1005–10. doi: 10.1097/ICO.0b013e3181cf9949. [DOI] [PubMed] [Google Scholar]
- 2.Tu EY, Joslin CE, Shoff ME. Successful treatment of chronic stromal acanthamoeba keratitis with oral voriconazole monotherapy. Cornea. 2010;29:1066–8. doi: 10.1097/ICO.0b013e3181cbfa2c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dart JK, Saw VP, Kilvington S. Acanthamoeba keratitis: Diagnosis and treatment update 2009. Am J Ophthalmol. 2009;148:487–99.e2. doi: 10.1016/j.ajo.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 4.Bang S, Edell E, Eghrari AO, Gottsch JD. Treatment with voriconazole in 3 eyes with resistant acanthamoeba keratitis. Am J Ophthalmol. 2010;149:66–9. doi: 10.1016/j.ajo.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 5.Chew HF, Yildiz EH, Hammersmith KM, Eagle RC, Jr, Rapuano CJ, Laibson PR, et al. Clinical outcomes and prognostic factors associated with acanthamoeba keratitis. Cornea. 2011;30:435–41. doi: 10.1097/ICO.0b013e3181ec905f. [DOI] [PubMed] [Google Scholar]
- 6.Maycock NJ, Jayaswal R. Update on acanthamoeba keratitis: Diagnosis, treatment, and outcomes. Cornea. 2016;35:713–20. doi: 10.1097/ICO.0000000000000804. [DOI] [PubMed] [Google Scholar]
- 7.Iovieno A, Miller D, Ledee DR, Alfonso EC. Cysticidal activity of antifungals against different genotypes of acanthamoeba. Antimicrob Agents Chemother. 2014;58:5626–8. doi: 10.1128/AAC.02635-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martín-Navarro CM, López-Arencibia A, Arnalich-Montiel F, Valladares B, Piñero JE, Lorenzo-Morales J, et al. Evaluation of the in vitro activity of commercially available moxifloxacin and voriconazole eye-drops against clinical strains of acanthamoeba. Graefes Arch Clin Exp Ophthalmol. 2013;251:2111–7. doi: 10.1007/s00417-013-2371-y. [DOI] [PubMed] [Google Scholar]
- 9.Arnalich-Montiel F, Martín-Navarro CM, Alió JL, López-Vélez R, Martínez-Carretero E, Valladares B, et al. Successful monitoring and treatment of intraocular dissemination of acanthamoeba. Arch Ophthalmol. 2012;130:1474–5. doi: 10.1001/archophthalmol.2012.2376. [DOI] [PubMed] [Google Scholar]


