Abstract
Background:
Breast cancer is the second leading cause of cancer death in women around the world. The degree of adoption of a preventive lifestyle offers valuable information for planning appropriate intervention programs for improving women’s health. The objective of the present study was to assess the levels of breast cancer related knowledge among a Northern Saudi population.
Methodology:
In this cross sectional study, data were obtained from 566 Saudi volunteers living in the city of Hail, the Kingdom of Saudi Arabia (KSA).
Results:
With regard to breast cancer risk factors, 427/566 (75.4%) of participants answered in the affirmative to whether breast cancer could be inherited. For early puberty and late menopause, 209/566 (37%) were in agreement with increased risk, for low and delayed child birth, 261/566 (46%), and for overweight and obesity, 210/566(37%). For the question of whether natural breast feeding can reduce the risk of breast cancer, only 35/566 (6.2%) said yes.
Conclusion:
There is a general lack of knowledge regarding several BC risk factors among the northern Saudi community which necessitates urgent implementation of educational programs.
Keywords: Breast cancer, awareness, prevention, Saudi Arabia
Introduction
Breast cancer (BC) continues to be a major public health problem worldwide in both developed and developing countries. It is the second leading cause of cancer death in women around the world (Ferlay et al., 2015). Although, BC rates are increasing in developed as well as developing countries, there is marked geographical variation in incidence rates, being highest in the developed world and lowest in the developing countries in Asia, Middle East, and Africa (IARC, 2008). BC carries significant socio-economic, emotional, and public health consequences.
BC incidence rates in Arab women have increased during the last 24 years, but women are still being diagnosed with BC at more advanced stages of the disease (Al-Saad et al., 2009; Miller 2010; Brown et al., 2012; Othman et al., 2015). Despite the low cancer incidence in the KSA, the country must be prepared to face the challenge of predictable increase in cancer burden attributed to growth and aging of population (Ibrahim et al., 2008).
In the Kingdom of Saudi Arabia (KSA), breast cancer is considered as the most common malignancy and represents the second leading cause of cancer deaths after lung cancer (Saggu et al., 2015). In Saudi Arabia, studies reported insufficient awareness about breast cancer and its early detection methods, which have a negative influence on the practice of breast self-examination among females (Radi, 2013).
Although multiple risk factors may enhance the likelihoods of developing breast cancer, but lifestyle factors appear to have a greater impact on it. Prevention has been recommended as an effective way to decrease the burden of BC (Khazaee-Pool et al., 2014a; Khazaee-Pool, et al., 2014b). Furthermore, a health-promoting lifestyle has been recommended for BC prevention (Magné, et al., 2011; Khazaee-Pool et al., 2017).
A number of BC risk factors have been recognized in different geographical regions and ethnic groups (Rosner et al., 1994; Lipworth, 1995). These include genetic, reproductive, environmental and socioeconomic risk factors, (Dumitrescu and Cotarla 2005) obesity, young age at menarche, late age at first child, short period of lactation and being physically inactive (Jemal et al., 2011; Naser et al., 2014).
Examining BC preventive lifestyles offers valuable information for planning appropriate intervention programs for improving women’s healthy lifestyle. Community educational programs that implement thoroughly Knowledge regarding these risk factors absolutely prevent many cases and render early detection of others. Therefore, the aim of the present study was to assess the levels of breast cancer related knowledge among Northern Saudi population.
Materials and Methods
This is a cross sectional study, data were obtained from 566 Saudi volunteers living in the city of Hail, the Kingdom of Saudi Arabia (KSA). Participants were randomly selected by simple random regardless to age, gender and education.
Purposeful questionnaire was designed and used for collection of the required data. The following information were obtained from each participant: age, sex, BC may be inherited, hormonal exposure (Estrogen (RE)) increase the risk of BC, do you think that some food can prevent BC, do you think that some food can cause BC, don’t food can prevent or cause BC, Know some food can prevent and cause BC, early puberty and late menopause increase the risk of BC, delayed and repeating child birth increase the risk of BC, natural breast feeding decreases the risk of BC, overweight or obesity increase the risk of BC, cosmetics increase the risk of BC, radiation exposure increases the risk of BC, cigarette smoking and some viruses increase the risk of BC.
Data analysis
Statistical Package for Social Sciences (version 16) was used for analysis and to perform Pearson Chi-square test for statistical significance (P value). The 95% confidence level and confidence intervals were used. P value less than 0.05 was considered statistically significant.
Ethical consent
Each participant was asked to sign a written ethical consent during the questionnaire’s interview. The informed ethical consent form was designed and approved by the ethical committee of the College of Medicine (University of Hail, KSA) Research Board.
Results
This surveyed 566 volunteers living in city of Hail, Northern Kingdom of Saudi Arabia (KSA), their ages ranging from 14-52 years with a mean age of 26 years. Out of 566 participants, 165/566 (29.2%) were males and 401/566 (70.8%) were females. Out of the 566 participants, 106-566 (18.7%) were with basic education level, 46/566(8.1%) were with secondary education and 414/566 (73.1%) were with university education level. With regard to the age, the majority of the study population were at age group 20-24 years representing 299/566(52.8%), followed by age ranges 25-29, 35-39, 30-34,40+ and <20 years constituting 67/566(11.8%), 52/566(9.2%), 51/566(9%), 51/566(9%) and 46/566(8.1%), respectively, as shown in Figure 1.
Figure 1.
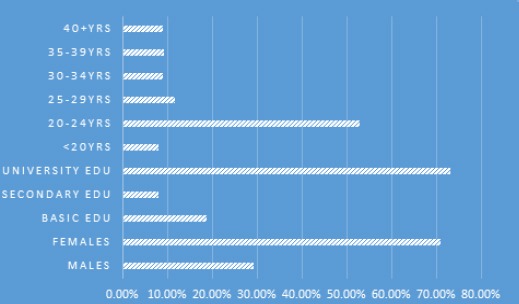
Description of The Study Population by Demographical Characteristics
The distribution of males and females was relatively comparable among all age groups. For males the majority were at age group 20-24 years followed by 25-29 representing 129/165 (78.2%) and 18/165 (10.9%) respectively. For females the majority were at age range 20-24 years followed by 40+ constituting 170/401 (42.4%) and 50/401 (12.5%) in this order, as indicated in Table 1, Figure 2.
Table 1.
Distribution of the Study Population by Age, Education and Sex
| Variable | Category | Males | Females | Total |
|---|---|---|---|---|
| Age | ||||
| <20 years | 6 | 40 | 46 | |
| 20-24 | 129 | 170 | 299 | |
| 25-29 | 18 | 49 | 67 | |
| 30-34 | 4 | 47 | 51 | |
| 35-39 | 7 | 45 | 25 | |
| 40+ | 1 | 50 | 51 | |
| Total | 165 | 401 | 566 | |
| Education | ||||
| Basic | 4 | 102 | 106 | |
| Secondary | 9 | 37 | 46 | |
| University | 152 | 262 | 414 | |
| Total | 165 | 401 | 566 | |
Figure 2.
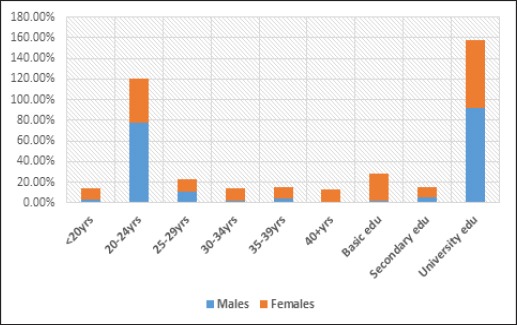
Description of the Study Population by Age, Education and Sex
With regard to the education level, the majority males were at university level followed by secondary school level representing 152/165 (92%) and 9/165 (5.5%) respectively. Moreover, the majority of females were at university level followed by basic education level constituting 262/401 (%) and 102/401 (%) respectively, as indicated in Table 1, Figure 2.
With regard to breast cancer risk factors, when asking participants, whether breast cancer can be inherited or not, 427/566 (75.4%) answered yeas and the remaining 139/566 (24.6%) answered no. For early puberty and late menopause, whether they risk for breast cancer, 209/566 (37%) agree and the remaining 357 (63%) disagree. For low and delayed child birth, whether they risk for breast cancer, 261/566 (46%) agree and the remaining 305 (54%) disagree. For natural breast feeding, whether it can reduce the risk of breast cancer, only 35/566 (6.2%) agree and the remaining 531/566 (93.8%) disagree. For overweight and obesity, whether it can increase the risk of breast cancer, only 210/566 (37%) agree and the remaining 356/566 (63%) disagree.
When asking them about their knowledge and perception about food, 81/566 (14.3%) were found to know that certain types of food can prevent or reduce the risk of breast cancer, 48/655 (8.5%) were found to know that certain types of cause or increase the risk of breast cancer, 377/566 (66.6%) don’t know any food that can prevent or cause cancer and the remaining 60/566 (10.6%) were found to know that certain types of food can prevent or lower the risk of breast cancer and other can cause or increase the risk, as shown in Figure 3.
Figure 3.
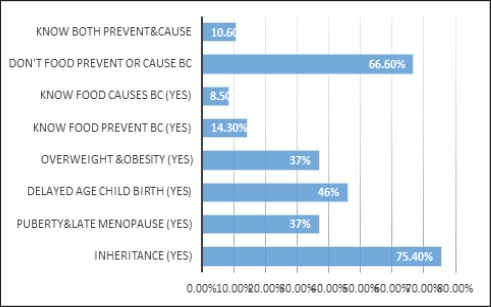
Description of the Study Population by Positive Response BC Risk Factors
With regard to hormonal exposure (estrogen) after menopause, 270/566 (47.7%) believe that it increases the risk of breast cancer and the remaining 296/566 (52.3%) don’t believe that. About 210/566 (37%) think that intensive and prolonged use of certain cosmetics can increase the risk of breast cancer and the remaining 356/566 (63%) don’t.
With regard to radiation exposure, 473/566 (83.6%) think that exposure to radiation may increase the risk of breast cancer and the remaining 93/566 (16.4%) don’t. Moreover, 428/566 (75.6%) believe that smoking is a risk factor for breast cancer and the remaining 138/566 (24.4%) don’t. Around 301/566 (53%) think that certain types of viruses can contribute to the etiology of breast cancer and the remaining 265/566 (47%) don’t, as shown in Figure 4.
Figure 4.
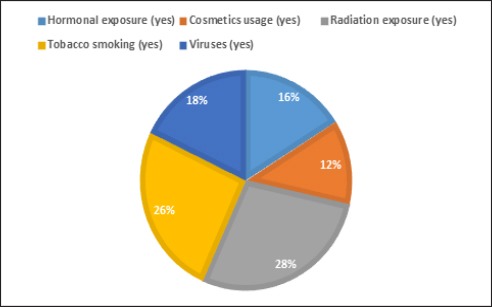
Description of the Study Population by Positive Response (Yes) BC Risk Factors
With regard to the knowledge toward different BC risk factors and sex. Out of 165 males 25 (15.2%), 11 (6.7%), 116 (70.3%) and 13 (7.9%) participants believe that some food prevent BC, some food cause BC, don’t food prevent or cause BC, know some food prevent and cause BC, respectively. Out of 399 females 56 (14%), 37 (9.3%), 261 (65.4%) and 45 (11.3%) participants believe that some food prevent BC, some food cause BC, don’t food prevent or cause BC, know some food prevent and cause BC, respectively.
Out of 163 males, 70 (43%) believe that early puberty and late menopause increase the risk of BC and the remaining 93 (57%) don’t. Out of 396 females, 139 (35%) believe that early puberty and late menopause increase the risk of BC and the remaining 257(65%) don’t.
Out of 163 males, 90 (55.6%) believe that delayed and repeating child birth increase the risk of BC and the remaining 72 (44.4%) don’t. Out of 397 females, 171 (43%) believe that early puberty and late menopause increase the risk of BC and the remaining 226 (57%) don’t.
Out of 163 males, 13 (8%) believe that natural breast feeding decreases the risk of BC and the remaining 150 (92%) don’t. Out of 398 females, 23 (5.8%) believe that early puberty and late menopause increase the risk of BC and the remaining 375 (94.2%) don’t.
Out of 165 males, 100 (60.6%) believe that overweight or obesity increase the risk of BC and the remaining 65 (39.4%) don’t. Out of 400 females, 255 (63.8%) believe that early puberty and late menopause increase the risk of BC and the remaining 145 (36.2%) don’t, as indicated in Table 2, Figure 5.
Table 2.
Distribution of the Study Population by Sex and Breast Cancer Risk Factors
| Variable | Category | Males | Females |
|---|---|---|---|
| Think some food prevent BC | Yes | 25 | 56 |
| Think some food cause BC | Yes | 11 | 37 |
| Don’t food prevent or cause BC | Yes | 116 | 261 |
| Know some food prevent and cause BC | Yes | 13 | 45 |
| Total | 165 | 399 | |
| Early puberty and late menopause increase the risk of BC | |||
| Yes | 70 | 139 | |
| NO | 93 | 257 | |
| Total | 163 | 396 | |
| Delayed and repeating child birth increase the risk of BC | |||
| Yes | 90 | 171 | |
| No | 72 | 226 | |
| Total | 162 | 397 | |
| Natural breast feeding decreases the risk of BC | |||
| Yes | 13 | 23 | |
| No | 150 | 375 | |
| Total | 163 | 398 | |
| Overweight or obesity increase the risk of BC | |||
| Yes | 100 | 255 | |
| No | 65 | 145 | |
| Total | 165 | 400 | |
Figure 5.
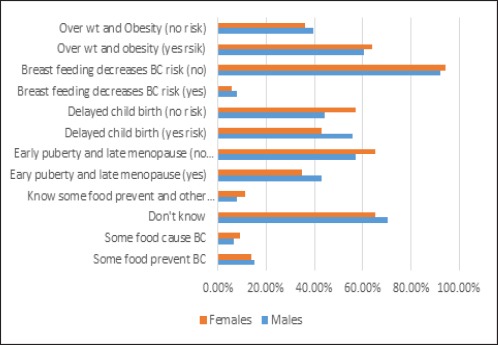
Description of the Study Population by Positive Response (Yes) BC Risk Factors and Sex
Table 3 summarizes the distribution of the study population by sex and breast cancer risk factors. For inheritance as a risk factor, 33 (20%) out of 165 males don’t know, whereas, 106 (26.8%) out of 396 females don’t know, that breast cancer has inherited genes. For hormonal exposure (ER) as a risk factor, 77 (46.7%) out of 165 males don’t know, whereas, 203 (52.3%) out of 397 females don’t know. For some cosmetics as a risk factor, 70 (42.4%) out of 165 males don’t know, whereas, 280 (70.5%) out of 396 females don’t know. For radiation exposure as a risk factor, 18 (10.9%) out of 165 males don’t know, whereas, 69 (17.4%) out of 396 females don’t know. For tobacco smoking as a risk factor, 24 (14.5%) out of 165 males don’t know, whereas, 114 (28.4%) out of 401 females don’t know. For some viruses as a risk factor, 77 (46.7%) out of 165 males don’t know, whereas, 188 (47.7%) out of 394 females don’t know, as shown in Figure 6.
Table 3.
Distribution of the Study Population by Sex and Breast Cancer Risk Factors
| Variable | Category | Males | Females |
|---|---|---|---|
| Inheritance | |||
| Yes | 132 | 290 | |
| No | 33 | 106 | |
| Total | 165 | 396 | |
| Hormones | |||
| Yes | 85 | 185 | |
| No | 77 | 203 | |
| Total | 162 | 388 | |
| Cosmetics | |||
| Yes | 92 | 117 | |
| No | 70 | 280 | |
| Total | 162 | 397 | |
| Radiation | |||
| Yes | 146 | 327 | |
| No | 18 | 69 | |
| Total | 164 | 396 | |
| Smoking | |||
| Yes | 141 | 287 | |
| No | 24 | 114 | |
| Total | 165 | 401 | |
| Viruses | |||
| Yes | 89 | 206 | |
| No | 77 | 188 | |
| Total | 165 | 394 | |
Figure 6.
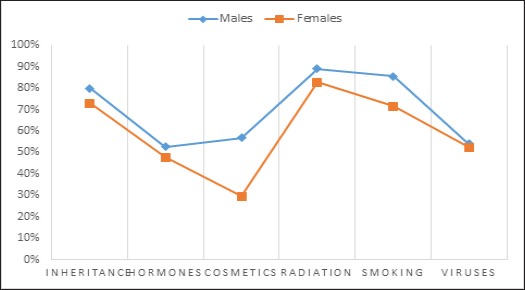
Description of the Study Population by Positive Response (Yes) BC Risk Factors and Sex
Discussion
The present study assessed the knowledge and perception of the northern Saudi population towards some common BC risk factors. Due to low response of the less educated individuals, the great majority of the participants were with university level of education. This may give rise to the highest level positive knowledge and perception towards the evaluated risk factors. On the other hand most of the study population were at relatively younger age. This may give rise to relatively higher level negative knowledge and perception towards the evaluated risk factors. Moreover, the response of males was very low, since most think that BC is a women issue.
Although many developing countries have implemented preventive efforts to fight BC with variable levels of success, but new breast cancer rates are still in elevation in many countries.
In the present study 24.6% of the study subjects believed that BC can’t be inherited, though this fact was established for decades (Apsalikov et al., 2016; Kuchenbaecker et al., 2017). About 63% of the study subjects think that early puberty and late menopause don’t increase the risk of breast cancer, which is relatively higher percentage. Early puberty and/or late menopause, later age at first pregnancy as well as a family history are well established BC risk factors (Espié et al., 2013). Around 54% of the study subject believe that age at first child birth (late age pregnancy) is not a risk factor of BC. Although several studies showed that the risk factors most strongly associated with breast cancer including age, place of residence, family risk, genetics, reproductive history, hormones exposure, tobacco use, alcohol intake, physical activity, participation in screening and breast density (Tapia et al., 2017; Peiris et al., 2017).
On the other hand only 6.2% of the participants believe that natural breast feeding can reduce the risk of breast cancer. Breastfeeding reduces women’s risk of breast cancer. Since exclusive breastfeeding has a stronger hormonal effect, it could theoretically result in a greater reduction in breast cancer risk than any breastfeeding mode. No meta-analysis has examined breast cancer risk by breastfeeding mode (Unar-Munguía et al., 2017).
In the present study, 63% of the participants believe that overweight and obesity don’t increase the risk of BC. There is growing scientific evidence linking excess body weight to BC risk, particularly among postmenopausal women (Kruk, 2014; Munsell et al., 2014).
Approximately 66.6% of the participant don’t whether there are certain types of food can prevent or increase the risk of BC. Vitamin C intake has been inversely associated with breast cancer risk in case-control studies (Hutchinson et al., 2012). Mate’ intake showed strong inverse associations with some high-risk hormone-related factors: early menarche, nulliparity, low breastfeeding, long reproductive years and high number of ovulatory cycles (Ronco et al., 2017). Several epidemiological investigations have been conducted to evaluate the relationship between dietary cholesterol intake and risk of breast cancer. A meta-analysis indicated that dietary cholesterol was associated with an increased risk of breast cancer (Li et al., 2016).
About 52.3% of the participants in the present study believe that hormonal exposure (estrogen) after menopause is not a risk factor of BC. Hormonal contraceptives and hormone replacement therapies are classified as carcinogenic to humans (group 1) by the International Agency for Research on Cancer (IARC) (Grevers et al., 2012). Around 37% persons think that intensive and prolonged use of certain cosmetics can increase the risk of breast cancer. Role of hair dyes in the etiology of breast cancer has occasionally raised concern but some studies found that use of hair dyes is associated with breast cancer incidence. Remnants of prohibited aromatic amines have been found in many hair dye products, and elevated levels of DNA-adducts of these amines have been detected from breast epithelial cells of hair dye users. However, the IARC working group has concluded that there is inadequate evidence for carcinogenicity of personal hair dye use and limited evidence in experimental animals for carcinogenicity of hair colorants (Heikkinen et al., 2015). Furthermore, many cosmetic products have been reported as carcinogenic particularly for breast (Darbre et al., 2014; Myers et al., 2014).
In the current study 83.6% think that exposure to radiation may increase the risk of breast cancer. Epidemiological studies have indicated an increasing incidence of radiation induced secondary cancer (SC) in breast cancer patients after radiotherapy (RT), most commonly in the contra-lateral breast (CLB) (Athiyaman et al., 2016). The occupational X-ray radiation exposure was associated with increasing cancer risk, which indicates that proper intervention and prevention strategies may be needed in order to bring down the occupational cancer risk (Wang et al., 2015).
Moreover, 75.6% of the study subjects believe that tobacco smoking is a risk factor for breast cancer and the remaining 138/566(24.4%) don’t. It was reported that passive smoking is associated with an increased risk of breast cancer, and the risk seems to increase as the level of passive exposure to smoke increases. Women with passive exposure to smoke in the workplace have a higher risk of breast cancer than those exposed to their husband’s smoking (Chen et al., 2014).
About 53% of the study population in the present study think that certain types of viruses can contribute to the etiology of breast cancer and the remaining 265/566(47%) don’t. There have been several reports on the role of human papillomavirus (HPV) in the etiology of breast cancer. It was reported that that women who develop viral warts are at a significantly higher risk of developing breast cancer than women who have not diagnosed with viral warts (Atique et al., 2017).
In a study assessed the levels of breast cancer awareness among Saudi females, and to compare between house wives and employee’s women regarding knowledge and practical of breast cancer. The majority of participants showed good knowledge regarding risk factors of breast cancer (93.3%), family history, contraceptive hormones, wearing tight bra, obesity, late menopause, and bearing the first child after age 30 years, (75%, 71.7%, 63.7%, 55.3%, 43.7%, 41.3%, respectively) (Mohammed et al., 2014). Another study from found that, about 26.4% believe that breast cancer affect females only, hence, 4.3% believe that breast cancer affect males only. Also the knowledge in regard to the breast cancer inheritance was very low, only 7.9% believed that breast cancer can be inherited (Ahmed et al., 2017).
In cross-sectional survey performed on male high school students across schools in Jeddah concluded that, knowledge of BC among male high school students in Saudi Arabia is still limited, and, therefore, programs and activities need to be established to increase awareness among high school students (Al-Amoudi et al., 2016). Another study evaluated the level of breast cancer awareness and perceived barriers to seeking medical care among Saudi women, using internationally validated tool, emphasized the critical need for an effective national breast cancer education program to increase public awareness and early diagnosis (Al-Khamis, 2016). Another study to identify breast cancer knowledge, practice and screening barriers among women attending primary health centers (PHC) in Madinah, Saudi Arabia, concluded that the high levels of poor knowledge about cancer breast observed in this study reflect the need for greater efforts to increase breast awareness education (Al-Zalabani et al., 2016). In other regions of Saudi Arabia; Al-Qassim it has been reported that the level of awareness of the females regarding breast cancer and BSE is not adequate and a health education program about breast cancer should be introduced in the region (Jahan et al., 2006).
The limitations of this study were its cross sectional settings, as well as, the clustering of participants among educated relatively younger age section.
In conclusion, the findings of the current study may help health experts and policy makers to be aware of the vital role of cultural and operational strategies in breast cancer prevention and control. Moreover, the findings of the present study will improve our understanding of the perspectives of the factors that influence BC prevention in relation to lifestyle.
References
- Ahmed HG, Ashankyty IM, Alrashidi AG, et al. Assessment of breast cancer awareness level among Saudi medical students. JCancer Prev Curr Res. 2017;7:00240. [Google Scholar]
- Al-Amoudi S, AlHomied MT, AlSayegh NY, et al. Breast cancer knowledge among male high school students in Saudi Arabia. J Cancer Educ. 2016;31:784–8. doi: 10.1007/s13187-015-0951-8. [DOI] [PubMed] [Google Scholar]
- Al-Khamis NK. Low awareness of breast cancer and considerable barriers to early presentation among Saudi women at a primary care setting. J Cancer Educ. 2016;10:1–7. doi: 10.1007/s13187-016-1119-x. [DOI] [PubMed] [Google Scholar]
- Al-Saad S, Al-Shinnawi H, Mahmood Shamsi N. Risk factors of breast cancer in Bahrain. Bahrain Medical Bulletin. 2009;31:1–11. [Google Scholar]
- Al-Zalabani AH, Alharbi KD, Fallatah NI, et al. Breast cancer knowledge and screening practice and barriers among women in Madinah, Saudi Arabia. J Cancer Educ. 2016;2016 doi: 10.1007/s13187-016-1057-7. https://doi.org/10.1007/s13187-016-1057-7 . [DOI] [PubMed] [Google Scholar]
- Apsalikov B, Manambaeva Z, Ospanov E, et al. BRCA1 and TP53 gene-mutations: Family predisposition and radioecological risk of developing breast cancer. Asian Pac J Cancer Prev. 2016;17:4059–62. [PubMed] [Google Scholar]
- Athiyaman H MA, Chougule A, Hs K. Estimated risk of radiation induced contra lateral breast cancer following chest wall irradiation by conformal wedge field and forward intensity modulated radiotherapy technique for post-mastectomy breast cancer patients. Asian Pac J Cancer Prev. 2016;17:5107–11. doi: 10.22034/APJCP.2016.17.12.5107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atique S, Hsieh CH, Hsiao RT, et al. Viral warts (Human Papilloma Virus) as a potential risk for breast cancer among younger females. Comput Methods Programs Biomed. 2017;144:203–7. doi: 10.1016/j.cmpb.2017.03.024. [DOI] [PubMed] [Google Scholar]
- Brown R, Kerr K, Haoudi A, Darzi A. Tackling cancer burden in the Middle East: Qatar as an example. Lancet Oncol. 2012;13:501–8. doi: 10.1016/S1470-2045(12)70461-8. [DOI] [PubMed] [Google Scholar]
- Chen C, Huang Y-B, Liu X-O, et al. Active and passive smoking with breast cancer risk for Chinese females: a systematic review and meta-analysis. Chin J Cancer. 2014;33:306–16. doi: 10.5732/cjc.013.10248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darbre PD, Harvey PW. Parabens can enable hallmarks and characteristics of cancer in human breast epithelial cells: a review of the literature with reference to new exposure data and regulatory status. J Appl Toxicol. 2014;34:925–38. doi: 10.1002/jat.3027. [DOI] [PubMed] [Google Scholar]
- Dumitrescu RG, Cotarla I. Understanding breast cancer risk –where do we stand in 2005? J Cell Mol Med. 2005;9:208–21. doi: 10.1111/j.1582-4934.2005.tb00350.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkum N, Al-Tweigeri T, Ajarim D, et al. Obesity is a significant risk factor for breast cancer in Arab women. BMC Cancer. 2014;14:788. doi: 10.1186/1471-2407-14-788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espié M, Lalloum M, Coussy F. Epidemiology and risk factors of breast cancer. Soins. 2013;776:22–4. [PubMed] [Google Scholar]
- Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:359–86. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- Grevers X, Grundy A, Poirier AE, et al. Cancer incidence attributable to the use of oral contraceptives and hormone therapy in Alberta in 2012. CMAJ Open. 2016;4:754–9. doi: 10.9778/cmajo.20160046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heikkinen S, Pitkäniemi J, Sarkeala T, Malila N, Koskenvuo M. Does hair dye use increase the risk of breast cancer?A population-based case-control study of finnish women. PLoS One. 2015;10:e0135190. doi: 10.1371/journal.pone.0135190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchinson J, Lentjes MA, Greenwood DC, et al. Vitamin C intake from diary recordings and risk of breast cancer in the UK dietary cohort consortium. Eur J Clin Nutr. 2012;66:561–8. doi: 10.1038/ejcn.2011.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim EM, Zeeneldin AA, Sadiq BB, Ezzat AA. The present and the future of breast cancer burden in the Kingdom of Saudi Arabia. Med Oncol. 2008;25:387–93. doi: 10.1007/s12032-008-9051-5. [DOI] [PubMed] [Google Scholar]
- International Agency for Research on Cancer (IARC) Breast cancer statistics 2008. 2008. [http://globocan.iarc.fr/factsheet.asp. ]
- Jahan S, Al-Saigul M, Abdelgadir H. Breast cancer: Knowledge, attitudes and practices of breast self-examination among women in Qassim region of Saudi Arabia. Saudi Med J. 2006;27:1737–41. [PubMed] [Google Scholar]
- Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- Khazaee-Pool M, Montazeri A, Majlessi F, et al. Breast cancer-preventive behaviors: exploring Iranian women's experiences. BMC Womens Health. 2014a;14:41. doi: 10.1186/1472-6874-14-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khazaee-pool M, Majlessi F, Foroushani AR, et al. Perception of breast cancer screening among iranian women without experience of mammography: a qualitative study. Asian Pac J Cancer Prev. 2014b;15:3965–71. doi: 10.7314/apjcp.2014.15.9.3965. [DOI] [PubMed] [Google Scholar]
- Khazaee-Pool M, Pashaei T, Jahangiry L, Ponnet K, Gholami A. Exploring breast cancer preventive lifestyle and social support of Iranian women: a study protocol for a mixed-methods approach. Int J Equity Health. 2017;16:97. doi: 10.1186/s12939-017-0592-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruk J. Overweight, obesity, oxidative stress and the risk of breast cancer. Asian Pac J Cancer Prev. 2014;15:9579–86. doi: 10.7314/apjcp.2014.15.22.9579. [DOI] [PubMed] [Google Scholar]
- Kuchenbaecker KB, McGuffog L, Barrowdale D, et al. Evaluation of polygenic risk scores for breast and ovarian cancer risk prediction in BRCA1 and BRCA2 mutation carriers. J Natl Cancer Inst. 2017;109:djw302. doi: 10.1093/jnci/djw302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C, Yang L, Zhang D, Jiang W. Systematic review and meta-analysis suggest that dietary cholesterol intake increases risk of breast cancer. Nutr Res. 2016;36:627–35. doi: 10.1016/j.nutres.2016.04.009. [DOI] [PubMed] [Google Scholar]
- Lipworth L. Epidemiology of breast cancer. Eur J Cancer Prev. 1995;4:7–30. doi: 10.1097/00008469-199502000-00002. [DOI] [PubMed] [Google Scholar]
- Magné N, Melis A, Chargari C, et al. Recommendations for a lifestyle which could prevent breast cancer and its relapse: Physical activity and dietetic aspects. Crit Rev Oncol Hematol. 2011;80:450–9. doi: 10.1016/j.critrevonc.2011.01.013. [DOI] [PubMed] [Google Scholar]
- Miller AB. Screening for breast cancer in the Eastern Mediterranean Region. East Mediterr Health J. 2010;16:1022–24. [PubMed] [Google Scholar]
- Mohammed R, Mansour MAM, Dorgham LSH. Breast cancer awareness among Saudi Females in Taif, Saudi Arabia. IJSR. 2014;3:439–45. [Google Scholar]
- Munsell MF, Sprague BL, Berry DA, Chisholm G, Trentham-Dietz A. Body mass index and breast cancer risk according to postmenopausal estrogen-progestin use and hormone receptor status. Epidemiol Rev. 2014;36:114–36. doi: 10.1093/epirev/mxt010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers SL, Yang CZ, Bittner GD, et al. Estrogenic and anti-estrogenic activity of off-the-shelf hair and skin care products. J Expo Sci Environ Epidemiol. 2015;25:271–7. doi: 10.1038/jes.2014.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Othman A, Ahram M, Al-Tarawneh MR, Shahrouri M. Knowledge, attitudes and practices of breast cancer screening among women in Jordan. Health Care Women Int. 2015;36:578–92. doi: 10.1080/07399332.2014.926900. [DOI] [PubMed] [Google Scholar]
- Peiris HH, Mudduwa LK, Thalagala NI, Jayatilaka KA. Do breast cancer risk factors affect the survival of breast cancer patients in Southern Sri Lanka? Asian Pac J Cancer Prev. 2017;18:69–79. doi: 10.22034/APJCP.2017.18.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radi SM. Breast cancer awareness among Saudi females in Jeddah. Asian Pac J Cancer Prev. 2013;14:4307–12. doi: 10.7314/apjcp.2013.14.7.4307. [DOI] [PubMed] [Google Scholar]
- Ronco AL, Espinosa E, Calderon JM, et al. 'Mate'intake, hormone-based risk factors and breast cancer: a case-control study. Asian Pac J Cancer Prev. 2017;18:941–8. doi: 10.22034/APJCP.2017.18.4.941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosner B, Colditz GA, Willett WC. Reproductive risk factors in a prospective study of breast cancer: the nurses'health study. Am J Epidemiol. 1994;139:819–35. doi: 10.1093/oxfordjournals.aje.a117079. [DOI] [PubMed] [Google Scholar]
- Saggu S, Rehman H, Zahid KA, Abid A. Recent incidence and descriptive epidemiological survey of breast cancer in Saudi Arabia. Saudi Med J. 2015;36:1176–80. doi: 10.15537/smj.2015.10.12268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tapia KA, Garvey G, Mc Entee M, Rickard M, Brennan P. Breast cancer in Australian Indigenous women: incidence, mortality, and risk factors. Asian Pac J Cancer Prev. 2017;18:873–84. doi: 10.22034/APJCP.2017.18.4.873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unar-Munguía M, Torres-Mejía G, Colchero MA, González de Cosío T. Breastfeeding mode and risk of breast cancer: A dose-response meta-analysis. J Hum Lact. 2017;33:422–34. doi: 10.1177/0890334416683676. [DOI] [PubMed] [Google Scholar]
- Wang FR, Fang QQ, Tang WM, et al. Nested case-control study of occupational radiation exposure and breast and esophagus cancer risk among medical diagnostic X ray workers in Jiangsu of China. Asian Pac J Cancer Prev. 2015;16:4699–704. doi: 10.7314/apjcp.2015.16.11.4699. [DOI] [PubMed] [Google Scholar]


