Abstract
Introduction and aims:
Screening can play a major role in reducing deaths associated with cancer. Breast self-examination (BSE) is a cheap, non-complicated and non-invasive method for breast cancer screening. This study aimed to examine the effects of an educational intervention based on the health belief model (HBM) on BSE behavior in women referred to health centers in Fasa, Iran.
Methods:
This quasi-experimental study was conducted on 92 women, divided into an experimental and a control group. Data were collected using a validated questionnaire covering demographic characteristics, knowledge, HBM constructs and breast self-examination performance. An educational program was performed in five sessions through group discussion with questions and answers and training videos for participants in the experimental group. Questionnaires were filled before and three months after the intervention in the two groups. Data were analyzed with SPSS-22 software for descriptive and analytical statistics.
Results:
The results of this study showed that the mean scores for knowledge, HBM constructs and self-examination behavior in the experimental group were elevated compared to the control group after the intervention (P<0.001).
Conclusions:
Education based on the HBM is effective in promoting breast self-examination behavior. Thus development and implementation of training programs based on the model are proposed for officers involved in education and health promotion in Iran.
Keywords: Education, breast cancer, health belief model, breast self-examination, women
Introduction
Breast cancer occurs in the breast tissue, particularly in the lobules responsible for transferring milk to the nipple (Mousavi et al., 2013). Breast cancer can occur in both sexes (Hankinson t al.,2008), but it occurs mainly in women (National Institutes of Health, 2008). Breast cancer is the leading cause of cancer deaths in women worldwide. Based on available statistics in 2008, 1384000 women were diagnosed with breast cancer, from whom 450,000 cases died (Youlden et al., 2012). This cancer is the second leading cause of cancer death in the United States Poursafa et al., 2015, so that in 2015, the number of new cases of breast cancer among women was 231840 and the number of deaths was about 40,290 (Atlanta: American Cancer Society, 2015). The incidence rate of the disease in Asian countries has increased (Rastad et al., 2013). For example, the incidence of breast cancer has doubled in Iran during the past 30 years (Babu et al., 2011). This cancer is the most common cancer among women by a rate of 21.4 percent (Haghighi et al., 2012). Age of diagnosis in Iran is 10 years earlier than that in developed countries. The most common age of diagnosis in Iran is 45-54 years (Sadjadi et al., 2009).
The timely detection of this cancer at an early stage and provision of appropriate treatment can enhance the chance of recovery and increase the lifetime of patients by than 90% (Yavari et al., 2006). The disease can be detected in time through screening, which can be lifesaving (Kadivar et al., 2012). Breast self-examination (BSE), clinical breast examination (CBE) by a physician, and mammography are three instruments recommended for breast cancer screening (Gursoy et al., 2009). BSE is highly useful in breast cancer screening as it is cheap, easy, confidential, uncomplicated, and without the need for special equipment (Kashfi et al., 2012).
Research has shown that BSE is the most important step in detecting tumors at an early stage, so that more than 65% of lumps in the breast can be detected by the patient (Marinhoet al., 2003). Today, a significant number of women are diagnosed with advanced stages of the disease that can be attributed to a lack of knowledge and awareness about screening (Othman et al., 2015). Previous studies have demonstrated that women’s knowledge about breast cancer screening is poor and a small number of women do screening for early detection of the disease (Arevian et al., 2011; Mahfouz et al., 2013). Training programs play an important role in promoting breast cancer examination and treatment among women (Rezaeian et al., 2014). Effective intervention for promotion of early detection of breast cancer requires a useful and effective behavior change model (Hatefnia et al., 2010). Health Belief Model (HBM) is one of the models that have been applied to BSE (Lotfi et al., 2012). HBM was introduced in 1950 by social psychologists at the US Public Health Services in order to explain and predict factors involved in failure of screening programs for early detection of tuberculosis (Steckler et al., 2010). The HBM is used as a systematic way to identify, explain, and predict preventive health behaviors. The main strength of this model is the use of simple constructs associated with health making its implementation, application and testing simple. HBM provides a theoretical framework useful for the study of cognitive factors and focuses on variables, which are prerequisites for a healthy behavior. Hence, it has been the basis for many practical interventions in a wide range of behaviors (KhaniJeihooni et al., 2015). HBM states that health-related behaviors of people are based on their perceived susceptibility (refers to one’s perception of the risk or the chances of contracting a health disease or condition), perceived severity (a person’s perception of the seriousness of the consequences of contracting a disease), perceived benefit (One’s belief in the efficacy of the advised action to reduce risk or seriousness of impact), perceived barrier (One’s opinion of tangible and psychological costs of the advised action), cues to action (Strategies to activate “readiness”), and self-efficacy (Confidence in one’s ability to take action) (Shojaei Zadeh et al., 2014) (Figure 1).
Figure 1.
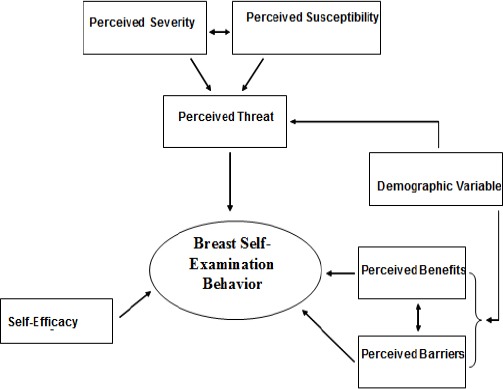
Conceptual Framework of This Study (KhaniJeihooniet al., 2015)
Given the importance of screening for early diagnosis and treatment of breast cancer as well as the low rate of BSE among Iranian women (7%) as reported by Aghamolaei et al.(2011) an intervention is needed to promote breast screening among these women. This study aimed to determine the effectiveness of the HBM-based education on BSE behavior among women referring to health centers in Fasa, Iran.
Materials and Methods
Sample
This study is a quasi-experimental before and after study carried out in two health centers in Fasa city, Fars Province, Iran in 2015. A sample of 92 women was randomly selected from among women who referred to the health center based on the inclusion criteria (older than 20 years, with no history of benign or malignant breast disease) to participate in the study. The criteria of excluding the study including: having the history of breast malignant diseases, pregnancy, breast feeding, relocation during the studding and absence more than one session in the training sessions.
Measures
In this study, a questionnaire based on HBM was used that consisted of sections on demographics (age, average number of children, marital status, educational level, Job and Family History of Cancer), knowledge, and HBM constructs .20 items on knowledge (for example: Breast self-examination is the most important means of early detection of breast cancer) (score 1 for correct and 0 for wrong answers) 8 items on perceived susceptibility (the women’s opinion about chances of getting breast cancer), 8 items on perceived severity (about complications due to breast cancer), 6 items on perceived benefits (about the benefits of breast self-examination behavior), 6 items on perceived barriers(including barriers to breast self-examination behavior), 8 items on self-efficacy (including the ability to do breast self-examination behavior). All HBM items were scored based on a standard 5-point Likert scale ranging from totally agree to totally disagree (score 5 to 1). BSE behavior was tested using 6 items (view the any changes in color or skin of the breasts) (score 1 for I do and 0 for I do not do) (Kashfi et al., 2012).
The validity of the questionnaire items was evaluated with an Item CVI of higher than 0.15, and CVR of higher than 0.77 based on exploratory factor analysis including 6 factors. To determine the face validity of the instrument, a list of developed items were piloted to 40 women with demographic, economic, and social characteristics similar to that of target population. In order to determine the content validity of the instrument, expert opinion was obtained from twelve specialists and experts outside the research team (10 in the field of health education and health promotion, 1 in obstetrics and gynecology, and 1 in vital statistics. Lawshe’sContent Validity Ratio (0.56 fora panel size of 12) was used for selecting essential items to be included in subsequent analysis. In this study, the CVR ofthe majority of items was higher than 0.70.
Cronbach’s alpha reliability of the research instrument was 0.86. The reliability values for knowledge, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, and self-efficacy were 0.85, 0.75, 0.80, 0.79, 0.82, and 0.77, respectively. Due to the fact that Cronbach’s alpha values for each of the subscales and constructs studied in this research were above 0.70, the reliability of the instrument was evaluated as acceptable.
Data Collection Procedures
The questionnaires were administered to both experimental and control groups before and three months after the educational intervention. The training program included five one-hour training sessions based on group discussion with questions and answers, and video demonstration for the experimental group with the aim of teaching them about the disease, risk factors, complications and screening methods including BSE, and when and how to correctly perform SBE. The training sessions were held in one of the rooms of the health center by the researchers.
Statistical Analysis
Data were analyzed using SPSS 22 via descriptive and analytical statistical methods. The mean scores of the two groups on awareness, performance, and HBM constructs were compared via independent samples t-test and paired samples t-test before and after the treatment.
Results
Their average age in the experimental and control groups was 30.39 ± 8.19 and 28.23 ± 7.30 respectively, and the average number of children reported by participants in the Experimental and control groups was 1.78 ± 1.31 and 1.10 ± 1.26 respectively. The results of Chi-square test revealed no significant difference between the two groups regarding the demographic variables (Table 1).
Table 1.
Comparison of the Experimental and Control Groups Regarding Demographic Variables
| Group | Experimental group | Control group | P- value | |||
|---|---|---|---|---|---|---|
| Variable | Frequency | Percent | Frequency | Percent | ||
| Marital status | Married | 42 | 91.3 | 42 | 91.3 | |
| Widowed | 3 | 6.52 | 2 | 4.35 | ||
| Divorced | 1 | 2.18 | 2 | 4.35 | 0.42 | |
| Education level | Illiterate | 2 | 4.35 | 1 | 2.17 | |
| ≤12th (grade) | 26 | 56.52 | 29 | 63.04 | ||
| >12th (grade) | 18 | 39.13 | 16 | 34.79 | 0.23 | |
| Job | Housewife | 38 | 82.6 | 39 | 84.78 | |
| Employee | 8 | 17.4 | 7 | 15.22 | 0.25 | |
| Family History of Cancer | yes | 3 | 6.52 | 4 | 8.69 | |
| No | 43 | 93.48 | 42 | 91.31 | 0.67 | |
The changes in mean scores on HBM constructs and BSE in the two groups before and after the educational intervention are presented in Table 2.
Table 2.
Comparison of The Mean Scores of HBM Constructs in The Experimental and Control Groups Before and After The Intervention
| Variables | Group | Before the intervention Mean±SD |
After the intervention Mean±SD |
p-value |
|---|---|---|---|---|
| Experimental group | 023.44±8.36 | 3.02±17.13 | p<0.001 | |
| knowledge | Control group | 3.44±8.06 | 3.87±8.89 | 0.11 |
| p-value | 0.68 | 001.0>p | ||
| Experimental group | 4.25±15.11 | 4.33±28.14 | 0.007 | |
| Perceived susceptibility | Control group | 4.36±14.20 | 4.32±14.79 | 0.23 |
| p-value | 0.92 | 0.04 | ||
| Experimental group | 4.12±15.24 | 4.01±26.75 | p<0.001 | |
| Perceived severity | Control group | 4.52±13.89 | 4.33±15.20 | 0.36 |
| p-value | 0.49 | 001.0>p | ||
| Experimental group | 1.41±10.13 | 1.23±22.20 | p<0.001 | |
| Perceived benefits | Control group | 1.65±11 | 1.67±84.10 | 0.18 |
| p-value | 0.23 | 001.0>p | ||
| Perceived barriers | Experimental group | 5.14±23.40 | 5.45±14.22 | p<0.001 |
| Control group | 5.20±22.20 | 5.43±20.48 | 0.82 | |
| p-value | 0.79 | 001.0>p | ||
| Experimental group | 5.28±14.22 | 5.34±29.08 | p<0.001 | |
| Control group | 5.75±14.59 | 5.32±15.45 | 0.08 | |
| Self-efficacy | p-value | 0.07 | 001.0>p | |
| Breast self-examination behavior | Experimental group | 0.80±0.90 | 0.45±3.11 | p<0.001 |
| Control group | 0.95±1 | 0.97±1.25 | 0.39 | |
| p-value | 0.32 | 001.0>p |
Discussion
Studies have shown that one of the causes of failure to do BSE is the lack of awareness of how to do it (Fontana et al., 2008; Abolfotouh et al., 2015). This study aimed to determine the effectiveness of the HBM-based education on BSE behavior among women referring to health centers in Fasa.
In this study, a significant increase was observed between the mean scores of knowledge for the Experimental and control group after the educational intervention. This is consistent with findings of other studies (Kashfi et al., 2012; Hatefnia et al., 2010; Lotfi et al., 2012; Karimi et al., 2008; Heidari et al., 2008; Alwabr GMA, 2016)
Gursoy et al., (2009) compared the effects of three methods of individual training, group training, and training through educational pamphlets on women’s knowledge and belief about BSE. The results showed that all three types of educational interventions were effective in raising awareness of participants in this area. These findings show that proper intervention can increase the level of awareness among women about breast cancer and ways of its early diagnosis.
The results of the present study indicate a significant increase in the post-test mean scores on perceived susceptibility and severity in the experimental group compared to the control group.
Based on previous studies, women who deem breast cancer as a serious illness and think they are susceptible to it, are more likely to do breast examination on a regular basis (Abolfotouh et al., 2015).
Rezaeian et al., (2014), Hatefnia et al., (2010), Aghamolaei et al.(2011) and Gozum et al., (2010) showed that women in the Experimental group felt more exposed to danger after the intervention than the control group and had a greater understanding of the seriousness of the risk and its complications.
The results of this study showed a significant increase in the post-test mean score of perceived benefits in the Experimental group compared to the control group. In studies by Hasani et al., (2011) and Canbulat and Uzun (2008), women who did BSE achieved higher scores on perceived benefits than women who did not do BSE.
Studies by Kalan-Farmanfarma et al., (2014), Rezaeian et al., (2014) and Lotfi et al., (2012) reported higher post-test mean scores on perceived benefits in the experimental group after the intervention which consistent with results of this study . Aghamolaei et al., (2011) found that training had no significant effect on improving the perceived benefits. This is inconsistent with the results of this study because the score of this construct in this study was high.
The construct of perceived barriers is the most important aspect in predicting preventive behaviors (Rezaeian et al., 2014; Karimi et al., 2008). In previous studies, BSE behavior was associated with lower perceived barriers (Secginli et al., 2006).
The results showed a significant reduction in post-test mean score of perceived barriers in the experimental group compared to the control group. This is consistent with the finding by Hatefnia et al., (2010), Moodi et al, (2013), Gursoy et al., (2009), Rezaeian et al., (2014) and Lotfi et al., (2012) who reported the significant impact of educational interventions on reducing perceived barriers to breast cancer screening behaviors.
Self-efficacy, which included the participants’ confidence in their ability to perform BSE and detect tumors successfully and correctly in this study, has been reported as the most powerful predictor of BSE behavior (Hasani et al., 2011).
The results of this study showed a significant improvement in the self-efficacy score of the experimental group as compared to the control group after the intervention. Studies by Kessler et al., (2012), Tavafian et al., (2009), Lotfi et al., (2012) and Heidari et al., (2008) also demonstrated that the self-efficacy of women who did BSE behavior was significantly higher than women who did not.
Another study showed that women’s perceived barriers and self-efficacy are predictors of BSE behavior (Abolfotouh et al., 2015).
Studies have shown that women’s higher level of knowledge of breast cancer increases their BSE behavior 26. Therefore, it is expected that an increase in awareness of women increase their BSE performance. The results showed that BSE behavior among women participating in the study increased after the intervention. Similarly, studies by Alwabr (2016), Kashfi et al., (2012), Bakhtari et al., (2011), Rastad et al., (2013), Lotfi et al., (2012), Heidari et al., (2008), Karimi et al., (2008) and Beydağ et al., (2010) showed that an increase in women’s awareness enhanced their BSE behavior.
The limitation of this study was the short follow-up. It is recommended that patients be evaluated in a longer time frame so that the persistence of behavior can be evaluated, also self-reporting the BSE. BSE has low sensitivity in breast cancer detection rather than mammography and clinical examination which is considered as another limitation.
In conclusion, the results of this study demonstrated the effectiveness of educational HBM-based interventions on promoting BSE. Therefore, it is recommended that healthcare providers use educational interventions based on this model to reduce deaths from breast cancer and promote women’s health.
Authors’ Note
For ethical considerations, informed consent was obtained from the participants before administration of the questionnaire. In addition, this study was certified and registered by Vice Chancellor for Research at Fasa University of Medical Sciences.
Funding
This research was financially supported by Fasa University of Medical Sciences (grant No. 94091).
Authors’ Contribution
Zahra Khiyali and AliKhaniJeihooni served as the main investigator, performed the literature review, managed the study, and contributed to writing the paper. Farzaneh Aliyan and Morteza Mansourian the acquisition of data and contributed to the study design and writing the first draft. Zahra Khiyali, Farzaneh Aliyan, Ali KhaniJeihooni, Seyyed Hannan Kashfi contributed to the analysis and interpretation of data.
Declaration of Conflicting Interests
The authors declare that they have no conflict of interest with respect to the research, authorship, and/or publication of this article.
References
- Abolfotouh MA, BaniMustafa AA, Mahfouz AA, et al. Using the health belief model to predict breast self-examination among Saudi women. BMC Public Health. 2015;15:1163–75. doi: 10.1186/s12889-015-2510-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aghamolaei T, Hasani L, Tavafian SS, Zare S. Improving breast self-examination: an educational intervention based on health belief model. Iran J Cancer Prev. 2011;4:82–7. [Google Scholar]
- Alwabr GMA. Breast cancer educational program and breast self-examination in Sana'a, Yemen. Curr Life Sci. 2016;2:27–35. [Google Scholar]
- Arevian M, Noureddine S, Abboud S. Beliefs related to breast cancer and breast cancer screening among Lebanese Armenian Women. Health Care Women Int. 2011;32:972–89. doi: 10.1080/07399332.2011.580405. [DOI] [PubMed] [Google Scholar]
- Atlanta: American Cancer Society. Cancer Facts and Figures. 2015. [Published 2015. Accessed January 2015]. AmericanCancerSociety. http://www.cancer.org/research/cancerfactsstatistics/cancerfactsfigures2015/index .
- Babu GR, Samari G, Cohen SP, et al. Breast cancer screening among females in iran and recommendations for improved practice: A review. Asian Pac J Cancer Prev. 2011;12:1647–55. [PubMed] [Google Scholar]
- BakhtariAghdam F, Nurizadeh R, Sahebi L. The effect of education based on health belief model in promoting the belief and behavior of breast cancer screening in women referring to Tabriz health centers. Med J Tabriz Univ Med Sci. 2011;33:25–31. [Google Scholar]
- Beydağ KD, Yürügen B. The effect of breast self-examination (Bse) education given to mid- wifery students on their knowledge and attitudes. Asian Pac J Cancer Prev. 2010;11:1761–4. [PubMed] [Google Scholar]
- Canbulat N, Uzun O. Health beliefs and breast cancer screening behaviors among female health workers in Turkey. Eur J Oncol Nurs. 2008;12:148–56. doi: 10.1016/j.ejon.2007.12.002. [DOI] [PubMed] [Google Scholar]
- Fontana M, Bischoff A. Uptake of breast cancer screening measures among immigrant and Swiss women in Switzerland. Swiss Med Wkly. 2008;138:752–8. doi: 10.4414/smw.2008.12328. [DOI] [PubMed] [Google Scholar]
- Gozum S, Karayurt O, Kav S, Platin N. Effectiveness of peer education for breast cancer screening and health beliefs in eastern Turkey. Cancer Nurs. 2010;33:213–20. doi: 10.1097/NCC.0b013e3181cb40a8. [DOI] [PubMed] [Google Scholar]
- Gursoy AA, Ylmaz F, Nural N, et al. A different approach tobreast self examination education: Daughters educating mothers creates positive results in Turkey. Cancer Nurs. 2009;3:127–34. doi: 10.1097/NCC.0b013e3181982d7b. [DOI] [PubMed] [Google Scholar]
- Haghighi F, Portaghali P, RafatyJavanbakht L, et al. Knowledge, at-titude, and practice of female teachers regarding breast cancer screening in Birjand. Mod Care J. 2012;9:146–55. [Google Scholar]
- Hankinson S, Tamimi R, Hunter D. Breast cancer. In: Adami HO, Hunter D, editors. Trichopoulos. Textbook of Cancer Epidemiology. 2nd ed. Vol. 2008. New York, NY: Oxford University Press; 2008. [Google Scholar]
- Hasani L, Aghamolaei T, Tavafian S, Zare S. Constructs of the health belief model as predicting factors in breast self-examination. Hayat. 2011;17:62–9. [Google Scholar]
- Hatefnia E, Niknami Sh, Mahmoudi M, et al. The effects of health belief model education on knowledge attitude and behavior of Tehran pharmaceutical industry employees regarding breast cancer and mammography. Behbood Sci Quarterly. 2010;14:42–53. [Google Scholar]
- Heidari Z, Mahmoudzadeh-Sagheb HR, Sakhavar N. Breast cancer screening knowledge and practice amongwomen in southeast of Iran. Acta Med Iran. 2008;46:321–8. [Google Scholar]
- [Updated September 2, 2014 Accessed]. http://www.cdc.gov/cancer/breast/statistics/
- Jeihooni AK, Hidarnia A, Kaveh MH, et al. The effect of an educational program based on health belief model on preventing osteoporosis in women. Int J Prev Med. 2015;6:115. doi: 10.4103/2008-7802.170429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeihooni AK, Hidarnia A, Kaveh MH, et al. Effects of an osteoporosis prevention program based on health belief model among females. Nurs Midwifery. 2015;4:e26731. doi: 10.17795/nmsjournal26731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadivar H, Goff BA, Phillips W R, et al. Nonrecommended breast and colorectal cancer screening for youngwomen: A vignette-based survey. Am J Prev Med. 2012;43:231–9. doi: 10.1016/j.amepre.2012.05.022. [DOI] [PubMed] [Google Scholar]
- Kalan-Farmanfarma K, Zareban I, Jalili Z, ShahrakiPour M. Effectiveness of education based on the health belief model on performing preventive measures for breast cancer among female teachers in Zahedan. J Educ Community Health. 2014;1:11–18. [Google Scholar]
- Karimi M, Hasani M, KHoram R, et al. The effectof health education based on Health Belife Model on breastself-examination in unit worker in zarandieh. Tabib Search. 2008;10:283–91. [Google Scholar]
- Kashfi SM, KhaniJeihooni A, Yazdankhah M. The effect of education about breast self-examination on knowledge, attitude and practice of women in Nourabad Mamasani health clinics, 2009. J Jahrom Univ Med Sci. 2012;10:40–5. [Google Scholar]
- Kessler TA. Increasing mammography and cer- vical cancer knowledge and screening behaviors with an educational program. Oncol Nurs Forum. 2012;39:61–8. doi: 10.1188/12.ONF.61-68. [DOI] [PubMed] [Google Scholar]
- Lotfi B, Hashemi SZ, Ansari-Moghadam A. Investigation of the impact of HBM-based training on BSE in women referred to health centers in Zahedan in 2010-2011. J Health Scope. 2011;1:39–43. [Google Scholar]
- Mahfouz AA, Hassanein MH, Nahar S, et al. Breast cancer knowledge and related behaviors among women in Abha city, southwestern Saudi Arabia. J Cancer Educ. 2013;28:516–20. doi: 10.1007/s13187-013-0495-8. [DOI] [PubMed] [Google Scholar]
- Marinho LA, Costa-Gurgel MS, Cecatti JG, et al. Knowledge, attitude and practice of breast self-examination in health centers. Rev Saude Publica. 2003;37:576–82. doi: 10.1590/s0034-89102003000500005. [DOI] [PubMed] [Google Scholar]
- Moodi M, Norozi E, Rezaeiyan M, et al. Comparing the effectiveness of three educational interventions based on health belief model on mammography screening behaviors in Women above 40 Years in Isfahan, Iran. J Health Syst Res. 2013;9:385–94. [Google Scholar]
- Mousavi SM, Försti A, Sundquist K, Hemminki K. Do reproductive factors influence T, N, and M classes of ductal and lobular breast cancers?A nation-wide follow-up study. PLoS One. 2013;8:1–10. doi: 10.1371/journal.pone.0058867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National institutes of health, national cancer institute. Cancer health disparities. 2008. [cancerhealth-disparities November 15, 2014]. Retrieved from http://www.cancer.gov/cancertopics/factsheet/disparities/
- Othman A, Ahram M, Al-Tarawneh MR, et al. Knowledge, attitudes and practices of breast cancer screening among women in Jordan. Health Care Women Int. 2015;36:578–92. doi: 10.1080/07399332.2014.926900. [DOI] [PubMed] [Google Scholar]
- Poursafa P, Kelishadi R, Ghasemian A, et al. Trends in health burden of ambient particulate matter pollution in Iran, 1990–2010: findings from the global burden of disease study 2010. Environ Sci Pollut Res Int. 2015;22:18645–53. doi: 10.1007/s11356-015-5545-9. [DOI] [PubMed] [Google Scholar]
- Rastad H, Shokohi L, Dehghani SL, MotamedJahromi M. Assessment of the awareness and practice of women vis-à-vis breast self-examination in Fasa in 2011. J Fasa Univ Med Sci. 2013;3:75–80. [Google Scholar]
- Rezaeian M, Sharifirad GH, Mostafavi F, et al. The effects of breast cancer educational intervention on knowledge and health beliefs of women 40 years and older, Isfahan, Iran. J Educ Health Promot. 2014;3:59–64. doi: 10.4103/2277-9531.131929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadjadi A, Nouraie M, Ghorbani A, et al. Epidemiology of breast cancer in the Islamic Republic of Iran: first results from a populationbasedcancer registry. East Mediterr Health J. 2009;15:1426–31. [PubMed] [Google Scholar]
- Secginli S, Nahcivan NO. Factors associated with breast cancer screeningbehaviours in a sample of Turkish women: a questionnaire survey. Int J Nurs Stud. 2006;43:161–71. doi: 10.1016/j.ijnurstu.2005.02.004. [DOI] [PubMed] [Google Scholar]
- Shojaei Zadeh D, Changizi M, Sadeghi R. The effect of education about addiction through health belief model (HBM) on knowledge and perceptions of high school students in Shadegan. J Sci Todays World. 2014;3:240–4. [Google Scholar]
- Steckler A, McLeroy KR, Holtzman D, Godfrey H. Hochbaum (1916-1999): from social psychology to health behavior and health education. Am J Public Health. 2010;100:1864. doi: 10.2105/AJPH.2009.189118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavafian SS, Hasani L, Aghamolaei T, et al. Prediction of breast self-examination in a sample of Iranian women: an application of the Health Belief Model. BMC Womens Health. 2009;9:37. doi: 10.1186/1472-6874-9-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yavari P, Mehrabi Y, Pourhoseinqoli MA. Awareness and action of women toward breast self-examination: a case-control study. J Ardabil Univ Med Sci. 2006;5:371–7. [Google Scholar]
- Youlden DR, Cramb SM, Dunn NA, et al. The descriptive epidemiology of female breast cancer: an international comparison of screening, incidence, survival and mortality. Cancer Epidemiol. 2012;36:237–48. doi: 10.1016/j.canep.2012.02.007. [DOI] [PubMed] [Google Scholar]


