Abstract
Histoplasmosis is considered one of the most important endemic and systemic mycoses worldwide. Until now few molecular techniques have been developed for its diagnosis. The aim of this study was to develop and evaluate three real time PCR (qPCR) protocols for different protein-coding genes (100-kDa, H and M antigens) using an animal model. Fresh and formalin-fixed and paraffin-embedded (FFPE) lung tissues from BALB/c mice inoculated i.n. with 2.5x106 Histoplasma capsulatum yeast or PBS were obtained at 1, 2, 3, 4, 8, 12 and 16 weeks post-infection. A collection of DNA from cultures representing different clades of H. capsulatum (30 strains) and other medically relevant pathogens (36 strains of related fungi and Mycobacterium tuberculosis) were used to analyze sensitivity and specificity. Analytical sensitivity and specificity were 100% when DNAs from the different strains were tested. The highest fungal burden occurred at first week post-infection and complete fungal clearance was observed after the third week; similar results were obtained when the presence of H. capsulatum yeast cells was demonstrated in histopathological analysis. In the first week post-infection, all fresh and FFPE lung tissues from H. capsulatum-infected animals were positive for the qPCR protocols tested except for the M antigen protocol, which gave variable results when fresh lung tissue samples were analyzed. In the second week, all qPCR protocols showed variable results for both fresh and FFPE tissues. Samples from the infected mice at the remaining times post-infection and uninfected mice (controls) were negative for all protocols. Good agreement was observed between CFUs, histopathological analysis and qPCR results for the 100-kDa and H antigen protocols. We successfully standardized and validated three qPCR assays for detecting H. capsulatum DNA in fresh and FFPE tissues, and conclude that the 100-kDa and H antigen molecular assays are promising tests for diagnosing this mycosis.
Introduction
Histoplasmosis is a disease caused by the dimorphic fungus Histoplasma capsulatum, which is considered one of the most important endemic mycoses and has caused outbreaks worldwide [1]. This disease is most frequently diagnosed in the Americas. The infection is acquired via the respiratory route, particularly when soils enriched with contaminated bird or bat excreta are disturbed, giving rise to infectious aerosols [2]. Clinical manifestations are variable and are especially severe in immunosuppressed patients, especially those living with HIV/AIDS, in whom histoplasmosis presents with significant morbidity and mortality [3], especially in those countries with limited access to rapid diagnostics or antiretroviral therapies, with up to 48% mortality reported [4,5].
Conventional laboratory methods used for diagnosis of histoplasmosis, such as blood cultures and histopathological analysis with visualization of the small yeast in fresh or formalin-fixed paraffin embedded (FFPE) tissues, have variable sensitivity (~50%) [2,3] and cultures may take up to 6 weeks to grow, delaying considerably the diagnosis [6,7]. Immunological tests that detect antibodies are less sensitive when used in immunocompromised persons, who often cannot mount a good humoral immune response [8]; a sensitivity of immunological tests has been reported ranging between 38% and 70% [6]. Detection of circulating Histoplasma antigens in urine has proven highly sensitive (95%) [5,9,10], but this test is not widely available; therefore each test has limitations [11].
A few molecular approaches have been developed by different groups and are all “in house” methods [4,12–17]. The most common target used for molecular diagnosis of histoplasmosis has been the gene coding for a specific 100-kDa protein reported as essential for the survival of H. capsulatum in human cells [18]. Many groups have reported the 100-kDa protein as a molecular target using quantitative and qualitative assays via PCR in fresh and FFPE tissues, as well as the loop-mediated isothermal amplification (LAMP) test [14,15,19–22]. The small-subunit rRNA (18S) gene of H. capsulatum has also been employed in nested-PCR and quantitative real time PCR (qPCR) assays [13,23,24]. The genes encoding the H and M antigens have also been used as molecular targets, as they both are specific proteins widely used for immunodiagnostic assays; M antigen target has been described by Guedes et al using a conventional PCR, and H antigen by Bracca et al in a nested PCR, both with specificity and sensitivity above 90% [25,26]. Currently, DNA-based diagnostic tests are not yet established as a routine diagnostic tool for histoplasmosis, universal molecular targets have not been established and some proposed tests have not been validated in human samples; for those reasons, at present no consensus molecular diagnostic test has been established and no PCR assays are commercially available.
Animal models are important in order to evaluate the performance of molecular biology based tests for identifying fungal DNA and they can also help to understand the kinetics of fungal DNA during infection. Very few murine models (two reports in the literature) have been described for validating a nested PCR assay [23,24], but none have been described for quantitative real time PCR assays.
Thus, there is an important and urgent need to develop new and rapid molecular assays for the diagnosis of histoplasmosis with high sensitivity and specificity, similar to those currently used for other pathogens such as Aspergillus spp [27–29]. The aim of this study was to design and evaluate quantitative real time PCR (qPCR) protocols targeting three protein-coding genes (100-kDa protein, H and M antigens) in a controlled histoplasmosis infection using an animal model.
Materials and methods
Strains and DNA collection
A collection of 30 DNAs extracted from cultures of H. capsulatum, representing six different clades described so far [30], and 36 DNAs extracted from medically relevant pathogens were used to evaluate the performance of the new designed qPCR assays (Tables 1 and 2). Isolates were provided by the Mycotic Diseases Branch (MDB), CDC, Atlanta, USA and the Corporación para Investigaciones Biológicas (CIB), Medellín Colombia. DNAs of different H. capsulatum clades and from medically relevant pathogens were quantified and adjusted to 1 ng/μl of concentration for the assays. In addition, mouse DNA (Promega, Madison, WI, USA) was used. Genomic DNA extraction process from the strain culture collection was performed using QIAamp® DNA Mini Kit (Qiagen; Valencia, CA, USA) as described by the manufacturer.
Table 1. Collection of DNA from cultures of H. capsulatum representing different clades.
| Species | Isolate name | Variety |
|---|---|---|
| NAm1 | 1001 | capsulatum |
| 2212 | capsulatum | |
| 2763 | capsulatum | |
| 2771 | capsulatum | |
| NAm2 | 1000/H8 | capsulatum |
| 1003/H11 | capsulatum | |
| 1006 | capsulatum | |
| 1008 | capsulatum | |
| 2404/H77 | capsulatum | |
| 2434/H84 | capsulatum | |
| 2436/H86 | capsulatum | |
| 2472/H97 | capsulatum | |
| 2474 | capsulatum | |
| 2475 | capsulatum | |
| LAmA | 2134 | capsulatum |
| 2350/H60 | capsulatum | |
| 2352/H62 | capsulatum | |
| 2353/H63 | capsulatum | |
| 2355/H73 | capsulatum | |
| 2358/H67 | capsulatum | |
| 2367/H76 | capsulatum | |
| LAmB | 2349/H59 | capsulatum |
| 2359/H68 | capsulatum | |
| 2363/H70 | capsulatum | |
| 2365/H75 | capsulatum | |
| 2368 | capsulatum | |
| Netherlands | 4741/H176 | capsulatum |
| Africa | 2444/H91 | duboisii |
| 5822 | duboisii | |
| 5823 | duboisii |
Table 2. Collection of DNA from cultures of medically relevant pathogens.
| Strains | Strain source |
|---|---|
| Aspergillus fumigatus | IFI 03–0127 |
| Aspergillus ustus | IFI 01–0058 |
| Aspergillus niger | IFI 03–0235 |
| Aspergillus terreus | IFI 02–0228 |
| Aspergillus versicolor | NRRL 236 |
| Aspergillus flavus | IFI 01–0074 |
| Fusarium moniliforme | B6584 |
| Fusarium solani | B5730 |
| Fusarium oxysporum | B6936 |
| Rhizopus microsporus | B4209 |
| Rhizopus arrhizus (oryzae) | B4386 |
| Absidia corymbifera | B6587 |
| Cunninghamella elegans | NRRL 28624 |
| Apophysomyces elegans | NRRL 28632 |
| Syncephalastrum racemosum | B6101 |
| Penicillium marneffei | B6471 |
| Penicillium sp. | B5449 |
| Penicillium sp. | B5454 |
| Scedosporium apiospermum | B5400 |
| Chrysosporium keratinophilum | B1980 |
| Candida albicans | CAS 12–3800 |
| Candida glabrata | CAS 99–236 |
| Candida parapsilosis | CAS 10–2433 |
| Candida krusei | CAS 11–3417 |
| Candida tropicales | CAS 11–2787 |
| Candida dubliniensis | CAS 98–174 |
| Candida lusitaniae | CAS 11–3483 |
| Cryptococcus neoformans | 2012–820513 |
| Cryptococcus gatti (D) | SA 03–0241 |
| Sporothrix schenckii | B3759 |
| Blastomyces dermatitidis | 2010–24457 |
| Blastomyces dermatitidis | B3591 |
| Coccidioides immitis | 2010–18016 |
| Coccidioides posadasii | 2011–02345 |
| Paracoccidioides brasiliensis | PB 339 |
| Mycobacterium tuberculosis | H57Rv |
Primer and probe design
Known sequences of the three important H. capsulatum protein-coding genes (100-kDa, H and M antigens) were retrieved from the GenBank database (accession numbers: AJ005963.1, U20346.1 and AF026268.2) and sequences for each of the three genes were aligned using the Clustal X program. The alignments were enriched by additional in-house sequencing of more isolates from each of the known H. capsulatum clades [30], and then scanned for regions of high intraspecies sequence conservation that could be used for designing primers and probes (S1–S3 Files).
All primers and probes were designed de novo and tested with Blast (Basic Local Alignment Search Tool; NCBI). No matches to other microorganisms or human DNA were observed. TIB MOLBIOL, Adelphia, NJ, USA was consulted for fine-tuning of the designs.
Real time PCR assay
Primers and probes were standardized using different concentrations (0.1μM, 0.2μM and 0.3μM) and two annealing temperatures (58°C and 60°C). Optimal conditions for each protocol were chosen as follows: the qPCR was performed in a mixture (25μl) that contained 1X Maxima Probe qPCR Master Mix (2X) (Thermo Fisher Scientific, USA), 0.2μM primers for the 100-kDa and M antigen protocols, and 0.3μM primers for H antigen protocol, 0.3μM probe for all protocols and 1 ng genomic DNA. Primer and probe sequences are shown in Table 3. qPCR was performed using a Rotor-Gene 6000 thermocycler (Qiagen; Valencia, CA, USA) under the following conditions: 95°C for 10 min, followed for 50 cycles of 95°C for 15 sec, 58°C for 30 sec and 72°C for 10 sec. The amplicons generated had lengths of 90 bp, 104 bp and 173 bp for the 100-kDa, H and M antigen protocols, respectively. Positive (H. capsulatum DNA) and negative controls (sterile distilled water) were included in each qPCR assay. Additionally, conventional PCR using the actin housekeeping gene was performed to assess the presence of amplifiable murine DNA and to detect PCR inhibitors following the protocol described by Bialek et al [23].
Table 3. Sequences of the primers and probes for each molecular target.
| Primers and probes | Sequence 5’-3’ | Protein-coding genes |
|---|---|---|
| 84R22 (Forward) | 5`GCAGARAATTCGACCYCAAGCC 3’ | 100-kDa |
| 15F23 (Reverse) | 5`GTATCCCACAGCATCMYGGAGGT 3’ | |
| 45L23 | 5`6FAM-CCTTCTTGCAACTYCCYGCGTCT-BBQ 3’ | |
| 2F (Forward) | 5`CACCGAGATAAAGGTGTCGA 3’ | H Antigen |
| 2R (Reverse) | 5`GGATCAGGGCTGAAACCTTC 3’ | |
| 2P | 5`6FAM-CTGCCCAACGGTCCAACCACA-BBQ 3’ | |
| F1 (Forward) | 5`CGCCRACGGGCTTTCCAT 3’ | M Antigen |
| R1 (Reverse) | 5`CATCGCTTGATCCCCAACG 3’ | |
| TM | 5`6FAM-ACCYSTTGGGTATTGCGTTGAGG-BBQ 3’ |
Determining analytical sensitivity
The PCR products were cloned in TOPO® TA Cloning Kit (Thermo Fisher Scientific, USA). All PCR products were inserted into pCR™4-TOPO® vector and transformed into TOP10 chemically competent Escherichia coli cells. Plasmids were extracted using PureLink® Quick Plasmid Miniprep (Thermo Fisher Scientific, USA).
Analytical sensitivity was obtained by serial dilution of H. capsulatum plasmid DNA (10ng until 1fg of DNA/μl). A standard curve and the crossing points (threshold cycle) were obtained in order to calculate copy number for each qPCR protocol.
Mouse model of pulmonary histoplasmosis
H. capsulatum strain
Histoplasma capsulatum yeasts (CIB1980 strain) were cultured in 200ml Brain Heart Infusion (BHI) broth medium (BDBBL, Franklin Lakes, NJ, USA) supplemented with 10% glucose (Sigma-Aldrich, Saint Louis, MO, USA), 0.1% L-cystine (Sigma-Aldrich, Bogotá, Colombia) and 100 U/ml Penicillin-100 μg/ml Streptomycin (GIBCO Invitrogen Corporation, Carlsbad, CA, USA) at 36°C and 150 rpm for 48 hours. Yeasts were centrifuged at 25°C, 3000 rpm during 5 min, the pellet was resuspended in 100μl of 1X phosphate-buffered saline (PBS) (GIBCO Invitrogen Corporation, Carlsbad, CA, USA) and the yeasts were counted using a haemocytometer and adjusted to 2.5x106 cells contained in 60μl in order to infect the mice.
Recovery of fungal virulence of H. capsulatum strain
BALB/c mice (n = 3) were intravenously (i.v.) inoculated through the tail vein with 5x106 viable yeast cells of H. capsulatum isolate 1980. After 4 weeks, mice were euthanized and affected organs (spleen, liver and lungs) extracted. The organs were macerated and cultured at 37°C in BBL Brain Heart Infusion (BHI) supplemented agar for two weeks. The H. capsulatum virulence-recovered yeast phase was subcultured at least twice weekly and then used for the intranasal (i.n.) inoculation of animals.
Animals and H. capsulatum infection
BALB/c mice were provided from the breeding colony maintained at Corporación para Investigaciones Biológicas (CIB, Medellín, Colombia). Mice were housed in the animal facility at the CIB in a caging system (RAIR HD Super Mouse 750TM Racks system, Lab Products, Inc. Seaford, DE, USA) equipped with high efficiency particulate air (HEPA) filters with controlled room temperature at 20–24°C; and under sterile conditions and provided with sterilized food and water ad libitum. Seven-week-old male mice were used in this study. Two experimental groups of mice were gathered, which consisted of infected or non-infected control mice (n = 140). Each group consisted of 70 animals, and from these, 10 mice were used for each post-infection period evaluated (1, 2, 3, 4, 8, 12 and 16 weeks). Infected mice were challenged intranasally with 60μl of 2.5x106 H. capsulatum yeast cells, and mice were previously anesthetized via intramuscular injection of 50μl Ketamine-Xylazine solution at 80mg/kg Ketamine (Laboratorios Biosano, Santiago, Chile) and 8mg/kg Xylazine (Bayer S.A., Bogotá, Colombia). Mice used as controls were inoculated with 60μl of PBS 1X under the same conditions. Cages were checked once daily for dead or moribund mice and no animals were found dead prior to sacrifice at the periods evaluated; every effort was made to minimize suffering of animals. Mice were euthanized at the different evaluation periods described above, chosen as the final point, using anesthesia followed by cervical dislocation. Lungs were removed for quantification of fungal burden by colony-forming units (CFU) and DNA extraction (5 mice per period), and histopathological analysis (5 mice per period). The number of animals used in this study was rationally chosen to obtain statistical significance in accordance with other studies described in the literature [31–33].
Ethics statement
This study was performed according to recommendations of European Union, Canadian Council on Animal Care, and Colombian regulations (Law 84/1989, Resolution No. 8430/1993). The protocol was approved by the Ethics in Research Committee of the CIB (Comité de ética, Act No. 098).
Colony forming units (CFU) determination
Lungs were removed, homogenized and processed following the protocol described by Pino-Tamayo et al with some modifications [31]. Briefly, lungs were weighed and homogenized in 2ml sterile PBS/ 1% Penicillin–Streptomycin solution [(GIBCO Invitrogen Corporation, Carlsbad, CA, USA) to a final concentration of 100 U/ml Penicillin– 100 μg/ml Streptomycin] using a gentleMACS Dissociator (Miltenyi Biotec, Teterow, Germany). Homogeneous suspensions were diluted (101 to 104) and 0.5ml of each dilution was plated on duplicate petri plates with Brain Heart Infusion (BHI) agar medium (BDBBL, Franklin Lakes, NJ, USA) supplemented with 10% glucose, 0.1% L-cystine, 100 U/ml Penicillin-100 μg/ml Streptomycin and 5% sheep erythrocytes (MDM Científica, Medellín, Colombia). Incubation was done at 36°C, 5% CO2 for 15 days. The CFU count was calculated as previously described [31]. The remaining homogenized tissues were stored at -20°C until DNA extraction.
Histopathological analysis
Lungs of mice were recovered and processed for histopathological analysis following the protocol described by Pino-Tamayo et al [31] with some modifications. Briefly, lungs were perfused with 1X PBS to wash out red blood cells, followed by formalin solution to fix tissues [Formaldehyde solution, (EM Science, Gibbstown, NJ) to a final concentration of 4%, sodium dihydrogen phosphate (Merck, Darmstadt, Germany) to a final concentration of 0.15M and sodium hydroxide (Sigma-Aldrich, Saint Louis, MO, USA) to a final concentration of 0.11M]. Lungs were removed and submerged in 4% formalin for a maximum of 24 hours. Fixed tissues were embedded in paraffin (FFPE) and cut. FFPE tissue sections were stained with Grocott’s methenamine silver to identify H. capsulatum yeast cells. Tissues were photographed using a Nikon Eclipse Ci-L microscope (Nikon Instruments Inc.,Melville, USA) and a Nikon DS-Fi2 high-definition color digital camera, and analyzed using NIS Elements 4.30.02 Laboratory Image Software (Nikon Instruments Inc., Melville, USA) and ImageJ Software (National Institutes of Health, NIH, Maryland, USA).
DNA extraction from lung tissues
Nucleic acids were extracted from fresh lung tissues and FFPE samples using QIAamp® DNA Mini Kit (Qiagen; Valencia, CA, USA) and QIAamp® DNA FFPE Tissue Kit (Qiagen; Valencia, CA, USA) respectively, according to the manufacturer’s instructions and modifications described previously [34].
Statistical analysis
Data analysis was performed using Graph Pad Prism software version 7 (GraphPad Software, Inc., La Jolla, CA, USA). Fungal burden was expressed as the mean ± SD number of CFU per g of tissue. In order to determine the agreement between the qPCR and either direct examination or culture (CFU), Kappa analysis was performed, using the statistical software STATA version 11.
Results
Design of primers and probes for the three H. capsulatum gene targets
Different primers and probes were initially designed for each of the three molecular targets. A total of 5 probe and 13 primer locations were considered for the genes coding for the 100-kDa protein and H and M antigens (full alignments are shown in S1–S3 Files). Three qPCR protocols were selected, for the H. capsulatum protein-coding genes for 100-kDa, H and M antigen, respectively, and the best signal for each target was determined using different combinations of melting temperatures and primer and probe concentrations (Table 3). No other microorganisms or human DNA had sequence matches with primers/probes. No amplification signals were detected in the negative controls.
Analytical sensitivity and specificity of the molecular assays
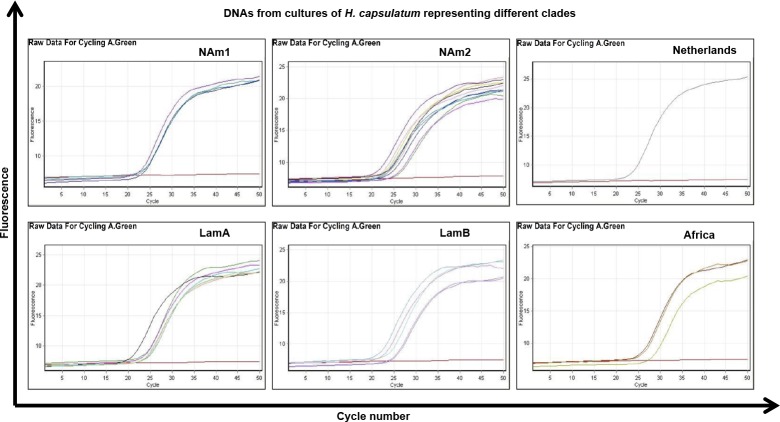
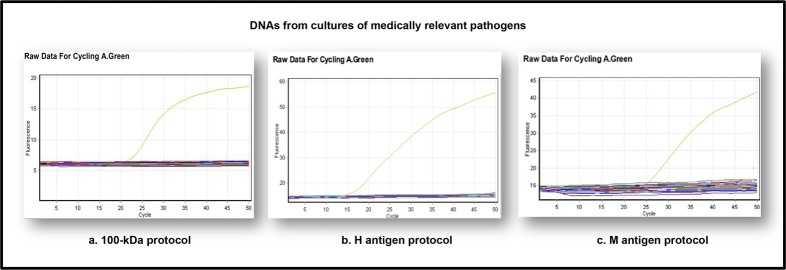
DNAs extracted from 66 strains were used to evaluate the performance of the real time PCR assay. From these, the 30 DNA H. capsulatum strains representing the different clades described by Kasuga et al [30] were all positive when tested using the three protocols (Fig 1) and Ct values are presented in Table 4. The DNA from the 36 strains from other medically relevant pathogens were all negative (Fig 2). The absence of cross-reaction with mouse DNA was also confirmed.
Fig 1. Standardization of qPCR protocols: Sensitivity of the real time PCR using 30 different Histoplasma DNAs representing 6 of the 8 clades described.
Example of 100-kDa qPCR protocol. NAm1: n = 4, Nam2: n = 10, LamA: n = 7, LamB: n = 5, Netherlands: n = 1, Africa: n = 3.
Table 4. Average of crossing point (threshold cycle) for each H. capsulatum clade for the three qPCR protocols.
| H. capsulatum clades | Ct value of real time PCR protocols | ||
|---|---|---|---|
| 100-kDa | H antigen | M antigen | |
| Nam1 | 20 | 20 | 24 |
| Nam2 | 20 | 22 | 24 |
| LamA | 21 | 23 | 25 |
| LamB | 21 | 23 | 24 |
| Netherlands | 21 | 23 | 24 |
| Africa | 24 | 24 | 27 |
Fig 2. Standardization of qPCR protocols: Specificity of the real time PCR using DNAs from other important medical pathogens.
Example of 100-kDa, H and M qPCR protocols, testing fungal and Mycobacterium DNA from 36 reference isolates. Signal is observed with H. capsulatum DNA (yellow line), the remaining samples are negative.
The detection limit was 1 fg of DNA per μl of sample, which needs 2, 1 and 43 DNA copies/μl for the 100-kDa, H and M antigen protocols respectively, when the coefficient r2 of the linear regression between crossing-point values and different dilutions of genomic DNA was determined (r2 > 0.99). The analytical sensitivity assay was performed with a single round of PCR.
Fungal burden and histopathological analysis of the lungs
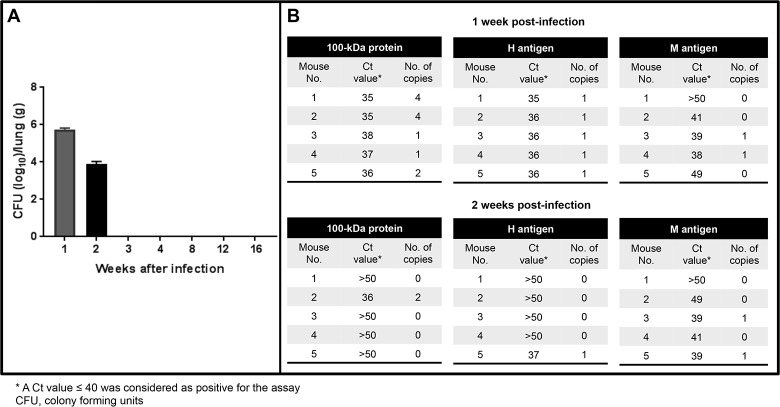
Animal infection was confirmed by analyzing the CFUs, which showed infection (fungal burden) in the lungs during the first two weeks post-infection. The highest fungal burden occurred at first week post-infection and full fungal clearance was observed from the third week (Fig 3A). Cultures of lungs were negative in the remaining periods studied. Mean fungal burden was 5.7 CFU (± 0.2 Log10/g of tissue) and 3.9 CFU (± 0.2 Log10/g of tissue) in the first and second week, respectively (Fig 3A). A statistically significant reduction in the fungal burden was observed in the lungs of infected mice when the first week post-infection was compared with the other periods evaluated (P < 0.00001).
Fig 3. Fungal burden and detection of Histoplasma DNA in fresh lung tissues using the three molecular targets.
A) Quantitative analysis of colony forming units (CFUs) evaluated in lungs of mice challenged i.n. with 2.5x106 H. capsulatum yeast cells at different weeks post-infection. B) Results of qPCR represented with Ct values and number of copies for each protocol at the first and second weeks post-infection.
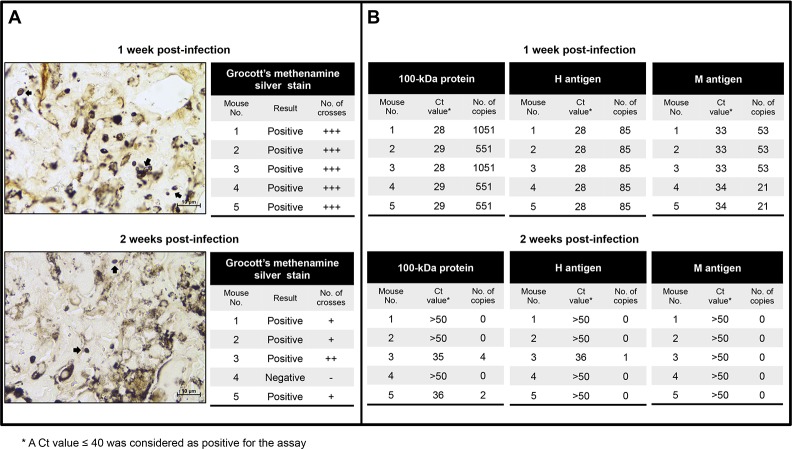
Histopathological analysis of lung tissues from infected mice demonstrated the presence of H. capsulatum yeast cells only during the first two weeks, as was observed for the CFU. In the first week, all the FFPE tissue sections showed fungal cells in high quantity (+++) (Fig 4A), while in the second week post-infection 4 out of 5 mice showed low numbers of yeast cells (+ to ++) and one was negative (Fig 4A).
Fig 4. Histopathological analysis and detection of Histoplasma DNA in FFPE lung tissues using the three molecular targets.
A) Microphotographs from lung sections stained with Grocott’s methenamine silver from mice infected with 2.5x106 H. capsulatum yeast cells at the first and second weeks post-infection, with the respective semiquantification measured by crosses of H. capsulatum yeast cells. Magnification 100X. B) Results of qPCR are represented with Ct values and number of copies for each protocol at the first and second weeks post-infection.
Detection of Histoplasma DNA in the lungs of mice
Real time PCR was performed in order to detect and quantify H. capsulatum DNA in fresh and FFPE lung tissue samples.
Molecular assays were positive for all fresh lung tissue samples at the first week post-infection for the 100-kDa protein and H antigen protocols with a number of copies detected ranging from 1 to 4, while only two of five samples were positive for the M antigen protocol with 1 copy detected (Fig 3B). Of note, at the second week post-infection only one sample was positive for the 100-kDa protein (2 copies detected), one for the H antigen (1 copy detected) and two samples were positive for the M antigen protocol (1 copy for both samples) (Fig 3B). These real time PCR assays showed good agreement with the CFU results for the 100-kDa protein and H protein protocols (Kappa = 0.68 for both) and not good agreement for the M antigen protocol (Kappa = 0.49); it should be kept in mind that CFU results shown in Fig 3A are on a logarithmic scale.
Interestingly, at the first week post-infection all the FFPE lung tissue samples from infected mice were positive for all three protocols tested, with number of detected copies ranging from 21 to 1051 (Fig 4B), whereas in the second week post-infection only two samples were positive for the 100-kDa protein (with 2 and 4 copies detected), one for the H antigen (1 copy detected) and none for the M antigen protocol (Fig 4B). Comparison between real time PCR assays for the 100-kDa protein and histopathological analysis with FFPE samples showed a very good agreement (Kappa = 0.84), and similar but lower agreements were observed when the H and M antigen protocols were analyzed (Kappa = 0.75 and 0.65 respectively).
A sample was considered positive for the assay when a Ct value was ≤ 40. This crossing point (threshold cycle) was selected based on experience in our research groups, on the evaluation of qPCR conditions and on studies in the literature that focused on identifying other fungal pathogens in animal models [35,36]. No signal amplification was detected for fresh and FFPE lung tissue samples in the remaining periods evaluated. All samples from uninfected mice (controls) were negative for all three protocols evaluated. In order to determine the presence of PCR inhibitors, the β-actin DNA gene was amplified and was positive for all lung samples tested indicating the absence of PCR inhibitors.
Discussion
We have developed and evaluated three real time PCR assays for the detection of H.capsulatum using different protein-coding gene targets (100-kDa, H and M antigens). To our knowledge, they are the first real time PCR assays reported for this pathogen to be evaluated using an animal model, BALB/c mice inoculated via the intranasal route with H. capsulatum yeast cells.
Protein-coding genes were selected as molecular targets on the basis of their established diagnostic importance. In the case of the 100-kDa target, the protein is essential for the survival of H. capsulatum in human cells [18] and has been used in a nested PCR molecular assay for detecting the fungus in animal and human samples for many years [15–17,19–22]. H antigen is a ß glycosidase and M antigen a catalase that have been used for detecting antibodies against H. capsulatum in body fluids in routine diagnosis for decades [7,37], however there have been few reports of their use in molecular assays and none for real time PCR assays [25,26].
We designed de novo for the first time three protein-coding gene primer/probe sets for detecting DNA of H. capsulatum in real time PCR and showed 100% specificity and analytical sensitivity, with a high detection limit of copies for 100-kDa, H and M antigen protocols (2, 1 and 43 DNA copies/μl respectively). The three assays were able to detect DNA extracted from H. capsulatum isolates from 6 different clades, as shown in Fig 1 for the 100-kDa assay as an example. The different clades were taken into consideration in the assay designs with the purpose of detecting H. capsulatum DNA distributed worldwide, although more studies using animal or human tissues infected with different clades will be need to verify the capacity of “universal detection”.
There have been very few reports of animal models for validating diagnostic tests, and those were typically for aspergillosis or candidiasis [27,38–40]. Animal models for histoplasmosis have also been developed, but not used for quantitative molecular assays [19,23]. In our study, fungal burden on lung tissues showed infection during the first two weeks with 5.7 CFU (Log10/g of tissue) and 3.9 CFU (Log10/g of tissue), respectively and clearance was observed from the third week (Fig 3A); clearance presumably indicates control of the infection in BALB/c mice. Our findings are in agreement with another study reported by Bialek et al [23], who showed fungal burden peaking on day 5 and declining thereafter, and with cultures being completely negative from day 15 onwards, in lungs of ICR mice.
In this study, results of histopathological analysis were similar to those described for CFU. Histoplasma capsulatum yeast cells were observed only during the first two weeks; in the second week the number of yeast cells decreased and was negative at third week, a finding that indicates a clearance of infection. Other studies have been performed using an animal model but no histopathological analysis was done [23] or the analyses performed were of other sample types such as spleen tissues [24].
The 100-kDa and H antigen molecular assays were positive for all fresh and FFPE lung tissue samples at the first week post-infection, at the second week post-infection a few samples were still positive (Figs 3B and 4B), and all samples were negative from the third week, as was observed also in the CFU and histopathological analyses. Our real time PCR results using the 100-kDa and H antigens protocols showed a good agreement with CFU and histopathological analysis results, particularly in FFPE lung tissues, where a higher number of copies were detected and where also the M antigen protocol gave excellent and reliable results. It may be asked why the M antigen assay failed to detect infection in fresh tissues at first week post-infection, and we consider as a possibility that the longer amplicon length of this assay (173bp vs 104 and 90bp) may cause difficulties when samples contain partly degraded DNA.
With respect to CFU and histopathological analyses, no previous study has compared the results with quantitative molecular assays such as real time PCR.
Our results using the qPCR assay for the detection of the 100-kDa protein and H antigen are concordant with those of Bialek et al [23] using the nested PCR for the small-subunit (18S) rRNA gene as a target with good correlation measured by CFU. A year later the same group [24] compared the nested PCR results with histopathological stain (Grocott) and reported the nested PCR as the most sensitive method but not significantly more sensitive than the Grocott stain. We also found that our real time PCR protocols had very good agreement with the Grocott stain.
The sensitivity of our qPCR assay using the actin housekeeping gene in order to detect the presence of amplifiable murine DNA and to detect PCR inhibitors in fresh and FFPE tissues was 100%. With this result we demonstrate that a controlled fixation of the tissues, a proper storage time and adequate temperature process are important in order to obtain DNA of high quality and amplifiable via PCR methods. Some authors have demonstrated the negative effect of formalin fixation during the process due to cross-linking and fragmentation of DNA [19,34,41,42], for that reason other authors have been working to improve the protocols [34,43].
Conclusions
We successfully standardized and validated three qPCR assays for detecting H. capsulatum DNA in a collection of DNA from different clades and also in fresh and FFPE tissues from infected animals. Our results showed that the 100-kDa and H antigen molecular assays both have high sensitivity for detecting Histoplasma capsulatum DNA in tissues from infected mice. We suggest that these novel molecular assays are promising tests for diagnosing this important mycosis in clinical samples.
Supporting information
The final choices of primer and probe sequences are shown highlighted in yellow and turquoise, respectively.
(PDF)
The final choices of primer and probe sequences are shown highlighted in yellow and turquoise, respectively.
(PDF)
The final choices of primer and probe sequences are shown highlighted in yellow and turquoise, respectively.
(PDF)
Acknowledgments
This study was supported by Colciencias (Departamento Administrativo de Ciencia, Tecnología e Innovación), Bogotá, Colombia, Project code number 221356933625; Fondo de Investigaciones de la Universidad del Rosario (FIUR), Bogotá, Colombia, code DVG154; Comité para el Desarrollo de la Investigación (CODI) of Universidad de Antioquia through the Sustainability Strategy Program 2016–2017 and the Mycotic Diseases Branch, CDC, Atlanta, USA.
We thank Dr. Lina Salazar for her support in providing the histopathological analysis and we also thank IMMY Company, Norman, Oklahoma, USA for a travel grant for the student supporting our project.
Data Availability
All relevant data are within the paper.
Funding Statement
This study was supported by Colciencias (Departamento Administrativo de Ciencia, Tecnología e Innovación), Bogotá, Colombia, Project code number 221356933625 to BLG; Fondo de Investigaciones de la Universidad del Rosario (FIUR), Bogotá, Colombia, code DVG154 to BLG; Comité para el Desarrollo de la Investigación (CODI) of Universidad de Antioquia through the Sustainability Strategy Program 2016-2017 and the Mycotic Diseases Branch, CDC, Atlanta, USA, and the IMMY Company, Norman, Oklahoma, USA for a travel grant for the student supporting our project. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Wheat J, Azar M, Bahr N, Spec A, Relich R, Hage C. Histoplasmosis. Infect. Dis. Clin. N. Am. 2016;30:207–227. doi: 10.1016/j.idc.2015.10.009 [DOI] [PubMed] [Google Scholar]
- 2.Deepe GS. Histoplasma capsulatum In: Principles and practice of infectious diseases. In: Mandell GL, Bennett JE, Dolin R, Blaser MJ, eds. Philadelphia, USA: Elsevier; 2015, 2949–2962. [Google Scholar]
- 3.Gómez BL and Tobón AM. Histoplasmosis In: Enfermedades Infecciosas de Homo sapiens. Vesga O, Vélez L, Leiderman E, Restrepo AM, eds. Medellín, Colombia: Editorial CIB; 2014, 2305–2322. [Google Scholar]
- 4.Kauffman CA. Histoplasmosis. Clin. Chest. Med. 2009;30:217–225. doi: 10.1016/j.ccm.2009.02.002 [DOI] [PubMed] [Google Scholar]
- 5.Scheel C, Samayoa B, Herrera A, Lindsley MD, Benjamin L, Reed Y, et al. Development and evaluation of an enzyme-linked immunosorbent assay to detect Histoplasma capsulatum antigenuria in immunocompromised patients. Clin. Vaccine Immunol. 2009;16:852–858. doi: 10.1128/CVI.00066-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hage CA, Ribes JA, Wengenack NL, Baddour LM, Assi M, McKinsey DS, et al. A multicenter evaluation of tests for diagnosis of histoplasmosis. Clin. Infect. Dis. 2011;53(5):448–54. doi: 10.1093/cid/cir435 [DOI] [PubMed] [Google Scholar]
- 7.Kauffman C. Histoplasmosis In: Essentials of Clinical Mycology. Pappas P, Sobel J, Dismukes W, eds. New York, USA: Springer; 2011, 321–335. [Google Scholar]
- 8.Arango M, Castañeda E, Agudelo CI, De Bedout C, Agudelo CA, Tobón A, et al. Colombian Histoplasmosis Study Group. Histoplasmosis: Results of the Colombian National Survey, 1992–2008. Biomédica. 2011;31(3)344–356. doi: 10.1590/S0120-41572011000300007 [DOI] [PubMed] [Google Scholar]
- 9.Zhang X, Gibson B, Daly TM. Evaluation of commercially available reagents for the diagnosis of Histoplasmosis infection in immunocompromised patients. J. Clin. Microbiol. 2013;51:4095–101. J Clin Microbiol. 2013 Dec; 51(12): 4095–4101. doi: 10.1128/JCM.02298-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cáceres D, Scheel C, Tobón AM, Ahlquist A, Restrepo A, Brandt M, et al. Validation of an Enzyme-Linked Immunosorbent Assay That Detects Histoplasma capsulatum Antigenuria in Colombian Patients with AIDS for Diagnosis and Follow-Up during Therapy. Clin. Vaccine Immunol. 2014;21(9):1364–1368. doi: 10.1128/CVI.00101-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kauffman C, Miceli MH. Histoplasmosis and Blastomycosis in Solid Organ Transplant Recipients. J. Fungi. 2015;1:94–106. doi: 10.3390/jof1020094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chemaly RF, Tomford JW, Hall GS, Sholtis M, Chua JD, Procop GW. Rapid diagnosis of Histoplasma capsulatum endocarditis using the AccuProbe on an excised valve. J. Clin. Microbiol. 2001;39(7):2640–2641. doi: 10.1128/JCM.39.7.2640-2641.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simon S, Veron V, Boukhari R, Blanchet D, Aznar C. Detection of Histoplasma capsulatum DNA in human samples by real-time polymerase chain reaction. Diag. Microbiol. Infect. Dis. 2010;66:268–273. doi: 10.1016/j.diagmicrobio.2009.10.010 [DOI] [PubMed] [Google Scholar]
- 14.Rickerts V, Bialek R, Tintelnot K, Jacobi V, Just-Nubling G. Rapid PCR based diagnosis of disseminated histoplasmosis in an AIDS patient. Eur. J. Clin. Microbiol. Infect. Dis. 2002;21(11):821–823. doi: 10.1007/s10096-002-0833-y [DOI] [PubMed] [Google Scholar]
- 15.Moubon D, Simon S, Aznar C. Histoplasmosis diagnosis using a polymerase chain reaction method. Application on human samples in French Guiana, South America. Diagn. Microbiol. Infect. Dis. 2007;58:441–444. doi: 10.1016/j.diagmicrobio.2007.03.008 [DOI] [PubMed] [Google Scholar]
- 16.Toranzo AI, Tiraboschi IN, Fernández N, Ibarra-Camou B, Rivas MC, Lee W, et al. Diagnóstico molecular de histoplasmosis humana en muestras de sangre entera. Rev. Argent. Microbiol. 2009;41:20–26. [PubMed] [Google Scholar]
- 17.Buitrago MJ, Canteros C, Frías De León G, González A, Marques-Evangelista De Oliveira M, Muñoz CO, et al. Comparison of PCR protocols for detecting Histoplasma capsulatum DNA through a multicenter study. Rev. Iberoam. Micol. 2013;30(4):256–260. doi: 10.1016/j.riam.2013.03.004 [DOI] [PubMed] [Google Scholar]
- 18.Porta A, Colonna-Romano S, Callebaut I, Franco A, Marzullo L, Kobayashi GS, et al. An homologue of the human 100-kDa protein (p100) is differentially expressed by Histoplasma capsulatum during infection of murine macrophages. Biochem. Biophys. Res. Commun. 1999;254:605–613. doi: 10.1006/bbrc.1998.9894 [DOI] [PubMed] [Google Scholar]
- 19.Bialek R, Feucht A, Aepinus C, Just-Nubling G, Robertson VJ, Knobloch J, et al. Evaluation of two nested PCR assays for detection of Histoplasma capsulatum DNA in human tissue. J. Clin. Microbiol. 2002;40(5):1644–1647. doi: 10.1128/JCM.40.5.1644-1647.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muñoz C, Gómez BL, Tobón A, Arango K, Restrepo A, Correa MM, et al. Validation and clinical application of a molecular methods for identification of Histoplasma capsulatum in human specimens in Colombia, South America. Clin. Vacc. Immunol. 2010;17:62–67. doi: 10.1128/CVI.00332-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koepsell S, Hinrichs S, Iwena P. Applying a Real-Time PCR Assay for Histoplasma capsulatum to Clinically Relevant Formalin-Fixed Paraffin-Embedded Human Tissue. J. Clin. Microb. 2012;50(10):3395–3397. doi: 10.1128/JCM.01705-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scheel C, Zhou Y, Theodoro R, Abrams B, Balajee A, Litvintseva A. Development of a Loop-Mediated Isothermal Amplification Method for Detection of Histoplasma capsulatum DNA in Clinical Samples. J. Clin. Microbiol. 2014;52(2):483–488. doi: 10.1128/JCM.02739-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bialek R, Fischer J, Feucht A, Najvar LK, Dietz K, Knobloch J, et al. Diagnosis and monitoring of murine histoplasmosis by a nested PCR assay. J. Clin. Microbiol. 2001;39(4):1506–1509. doi: 10.1128/JCM.39.4.1506-1509.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bialek R, Ernst F, Dietz K, Najvar LK, Knobloch J, Graybill JR, et al. Comparison of staining methods and a nested PCR assay to detect Histoplasma capsulatum in tissue sections. Am. J. Clin. Pathol. 2002;117(4):597–603. doi: 10.1309/MH5B-GAQ2-KY19-FT7P [DOI] [PubMed] [Google Scholar]
- 25.Bracca A, Tosello ME, Girardini JE, Amigot SL, Gómez C, Serra E. Molecular detection of Histoplasma capsulatum var. capsulatum in human clinical samples. J. Clin. Microbiol. 2003;41(4):1753–1755. doi: 10.1128/JCM.41.4.1753-1755.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guedes HL, Guimaraes AJ, Muniz Mde M, Pizzini CV, Hamilton AJ, Peralta JM, et al. PCR assay for identification of Histoplasma capsulatum based on the nucleotide sequence of the M antigen. J. Clin. Microbiol. 2003;41(2): 535–539. doi: 10.1128/JCM.41.2.535-539.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Loeffler J, Kloepfer K, Hebart H, Najvar L, Graybill JR, Kirkpatrick WR, et al. Polymerase Chain Reaction Detection of Aspergillus DNA in Experimental Models of Invasive Aspergillosis. J. Infect. Dis. 2002;185:1203–1206. doi: 10.1086/339824 [DOI] [PubMed] [Google Scholar]
- 28.White L, Bretagne S, Klingspor L, Melchers W, McCulloch E, Schulz B, et al. Aspergillus PCR: One Step Closer to Standardization. J. Clin. Microbiol. 2010;48(4):1231–1240. doi: 10.1128/JCM.01767-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.White L, Barnes RA, Springer J, Klingspor L, Cuenca-Estrella M, Morton O, et al. Clinical Performance of Aspergillus PCR for Testing Serum and Plasma: a Study by the European Aspergillus PCR Initiative. J. Clin. Microbiol. 2015;53(9):2832–2837. doi: 10.1128/JCM.00905-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kasuga T, White TJ, Koenig G, McEwen J, Restrepo A, Castañeda E, et al. Phylogeography of the fungal pathogen Histoplasma capsulatum. Mol. Ecol. 2003;12:3383–3401. doi: 10.1046/j.1365-294X.2003.01995.x [DOI] [PubMed] [Google Scholar]
- 31.Pino-Tamayo PA, Puerta-Arias JD, Lopera D, Urán-Jiménez ME and González A. Depletion of Neutrophils Exacerbates the Early Inflammatory Immune Response in Lungs of Mice Infected with Paracoccidioides brasiliensis. Mediators of Inflammation. 2016;2016:1–17. doi: 10.1371/journal.pone.0163985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Castelli M, Buitrago MJ, Bernal-Martínez L, Gómez-López A, Rodríguez-Tudela JL, Cuenca-Estrella M. Development and Validation of a Quantitative PCR Assay for Diagnosis of Scedosporiosis. J. Clin. Microbiol. 2008;46(10):3412–3416. doi: 10.1128/JCM.00046-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Puerta-Arias JD, Pino-Tamayo PA, Arango J, González A. Depletion of Neutrophils Promotes the Resolution of Pulmonary Inflammation and Fibrosis in Mice Infected with Paracoccidioides brasiliensis. PLOS ONE. 2016;11(9):1–23. doi: 10.1371/journal.pone.0163985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Muñoz -Cadavid C, Rudd S, Zaki SR, Patel M, Moser SA, Brandt ME et al. Improving Molecular Detection of Fungal DNA in Formalin-Fixed Paraffin-Embedded Tissues: Comparison of Five Tissue DNA Extraction Methods Using Panfungal PCR. J. Clin. Microbiol. 2010;48(6):2147–53. doi: 10.1128/JCM.00459-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bernal-Martínez L, Buitrago MJ, Castelli MV, Rodríguez-Tudela JL, Cuenca-Estrella M. Detection of invasive infection caused by Fusarium solani and non-Fusarium solani species using a duplex quantitative PCR-based assay in a murine model of fusariosis. Medical Mycology. 2012;50(3):270–275. doi: 10.3109/13693786.2011.604047 [DOI] [PubMed] [Google Scholar]
- 36.Muraosa Y, Zaninelli A, Trabasso P, Matsuzawa T, Taguchi H, Moretti ML, et al. Development of cycling probe-based real-time PCR system to detect Fusarium species and Fusarium solani species complex (FSSC). Int. J. Med. Microbiol. 2014;304(3–4):505–511. doi: 10.1016/j.ijmm.2014.03.001 [DOI] [PubMed] [Google Scholar]
- 37.Lindsley MD, Warnock DW, Morrison CJ. Serological and molecular diagnosis of fungal infection In: Rose NR, Hamilton RG, Detrick B, eds. Manual of Molecular and Clinical Laboratory Immunology, 7th ed.ASM Press, Washington DC, 2006, 569–605. [Google Scholar]
- 38.Hussain Z, Elsayed S, Fitzgerald V, Hall A. Comparison of PCR to histology for the diagnosis of invasive candidiasis in a murine model. Scand. J. Infect. Dis. 2001;33(1):51–5. [DOI] [PubMed] [Google Scholar]
- 39.Walsh TJ, Wissel MC, Grantham KJ, Petraitiene R, Petraitis V, Kasai M, et al. Molecular detection and species-specific identification of medically important Aspergillus species by real-time PCR in experimental invasive pulmonary aspergillosis. J. Clin. Microbiol. 2011;49(12):4150–7. doi: 10.1128/JCM.00570-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schell WA, Benton JL, Smith PB, Poore M, Rouse JL, Boles DJ, et al. Evaluation of a digital microfluidic real-time PCR platform to detect DNA of Candida albicans in blood. Eur. J. Clin. Microbiol. Infect. Dis. 2012;31(9):2237–45. doi: 10.1007/s10096-012-1561-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dannaoui E, Schwarz P, Slany M, Loeffler J, Tomine A, Cuenca-Estrella M, et al. Molecular Detection and Identification of Zygomycetes Species from Paraffin-Embedded Tissues in a Murine Model of Disseminated Zygomycosis: a Collaborative European Society of Clinical Microbiology and Infectious Diseases (ESCMID) Fungal Infection Study Group (EFISG) Evaluation. J. Clin. Microbiol. 2010;48(6):2043–2046. doi: 10.1128/JCM.02319-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Taga M, Eguchi H, Shinohara T, Takahashi K, Ito R, Yasui W, et al. Improved PCR amplification for molecular analysis using DNA from long-term preserved formalin-fixed, paraffin-embedded lung cancer tissue specimens. Int. J. Clin. Exp. Pathol. 2013;6(1):76–79. [PMC free article] [PubMed] [Google Scholar]
- 43.Wu L, Patten N, Yamashiro CT, Chui B. Extraction and amplification of DNA from formalin-fixed, paraffin-embedded tissues. Appl. Immunohistochem. Mol. Morphol. 2002;10(3):269–274. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The final choices of primer and probe sequences are shown highlighted in yellow and turquoise, respectively.
(PDF)
The final choices of primer and probe sequences are shown highlighted in yellow and turquoise, respectively.
(PDF)
The final choices of primer and probe sequences are shown highlighted in yellow and turquoise, respectively.
(PDF)
Data Availability Statement
All relevant data are within the paper.