Abstract
Mindfulness-based treatments for posttraumatic stress disorder (PTSD) have emerged as promising adjunctive or alternative intervention approaches. A scoping review of the literature on PTSD treatment studies, including approaches such as mindfulness-based stress reduction, mindfulness-based cognitive therapy and metta mindfulness, reveals low attrition with medium to large effect sizes. We review the convergence between neurobiological models of PTSD and neuroimaging findings in the mindfulness literature, where mindfulness interventions may target emotional under- and overmodulation, both of which are critical features of PTSD symptomatology. Recent emerging work indicates that mindfulness-based treatments may also be effective in restoring connectivity between large-scale brain networks among individuals with PTSD, including connectivity between the default mode network and the central executive and salience networks. Future directions, including further identification of the neurobiological mechanisms of mindfulness interventions in patients with PTSD and direct comparison of these interventions to first-line treatments for PTSD are discussed.
Introduction
About 60%–75% of individuals in North America experience a traumatic event at some point in their lifetime.1,2 The 12-month prevalence of posttraumatic stress disorder (PTSD) is estimated to be 2.5%–3.5% in North America, making this condition an important public health issue.2,3 Commonly experienced traumatic events include sexual assault or rape; repeated childhood emotional, physical or sexual abuse or neglect; involvement in a serious accident (e.g., motor vehicle collision); and exposure to war or the combat theatre. Posttraumatic stress disorder is associated with a myriad of symptoms, including intrusions (e.g., unwanted memories or flashbacks), avoidance of trauma reminders (e.g., objects in the environment that symbolize the trauma), negative alterations in cognitions and mood (e.g., altered view of the self, world, and others) and alterations in arousal (e.g., hypervigilance).4 In addition, a substantial subset of individuals with PTSD (15%–30%) experience symptoms of dissociation, including depersonalization (feeling outside of or as if you do not belong to your own body) and derealization (feeling as though things around you are not real).5–10 Individuals with PTSD who experience depersonalization and/or derealization symptoms are recognized in the DSM-5 as having a dissociative subtype of PTSD (PTSD+DS).4
First-line treatments for PTSD, including prolonged exposure therapy (PE) and cognitive processing therapy (CPT), target symptoms of avoidance, ineffective processing of trauma memories and negative appraisals of traumatic events.11 Although CPT and PE are associated with large effect sizes and clinically important symptom reduction,11,12 a substantial proportion of patients retain their diagnosis of PTSD following treatment (60%–72%)12 or continue to experience considerable residual symptoms.13 Moreover, attrition rates for leading treatment interventions were reported to fall between 35% and 40% in recent studies.14–16 In addition, resistance to use interventions incorporating exposure for PTSD has been noted among some clinicians because of, for example, concerns about potential symptom exacerbation.17 Thus, although trauma-focused treatments, including CPT and PE, are considered effective treatments for PTSD, the need for potential adjunctive or alternative treatments is evident.
A personalized treatment approach would incorporate identification of treatments most appropriate for each individual at a given time, taking into consideration factors such as symptom severity, safety and acceptability of the treatment to the individual. The need for alternative treatment approaches is also evident among those with PTSD+DS, in whom dissociative symptoms have been associated with poorer treatment outcomes18,19 (but see the studies by Wolf and colleagues,20 Cloitre and colleagues21 and Resick and colleagues22). Further, depersonalization and derealization symptoms have been associated with increased disease severity (e.g., suicidality), enhanced chronicity of illness and worse functional outcomes23 among individuals with PTSD.
Mindfulness-based treatments may represent an alternative to trauma-focused treatments, including CPT and PE, where such treatment approaches are considered to be “present-centred,” in that they encourage nonjudgment and acceptance of thoughts and emotions as they occur in the present moment. Of note, a recent review identified that present-centred therapies for PTSD were equally efficacious when compared with evidence-based trauma-focused therapies and had significantly lower drop-out rates.24 Mindfulness, defined as “the awareness that emerges through paying attention on purpose, in the present moment, and nonjudgmentally to the unfolding of experience moment by moment,”25 has emerged over the past decade as an alternative technique for targeting symptoms of avoidance and negative cognitions, including self-blame, shame and guilt among individuals with PTSD.26–28 With its roots in ancient Eastern traditions, the use of mindfulness-based treatments in psychiatric populations has grown exponentially following its introduction to Western psychology in the 1980s and 1990s.29
Mindfulness-based stress reduction (MBSR) is among the most commonly cited mindfulness-based treatment approaches. Treatment consists of 8 weeks of 2- to 2.5-hour group sessions with a full-day silent meditation retreat around week 6. These sessions cover a breadth of approaches, including mindfulness meditation, yoga, discussion about stress and coping, weekly homework assignments and daily mindfulness practice.30,31 Mindfulness-based cognitive therapy (MBCT) is another widely adopted mindfulness-based approach incorporating components of cognitive behavioural therapy (CBT) and MBSR and was initially developed to prevent relapse among individuals with major depressive disorder (MDD).32 Mindfulness-based cognitive therapy focuses on changing awareness of and relationships with thoughts, promoting a “decentred” perspective (i.e., “thoughts are not facts”).32 This approach targets in particular a reduction of residual symptoms and aims to prevent relapse.33,34 Both MBSR and MBCT have shown efficacy across a wide range of psychiatric disorders, including MDD and anxiety disorders, with medium effect sizes observed in both populations.
In this review we investigate the theoretical basis for the utility of mindfulness-based approaches in the treatment of PTSD. In addition, we assess the overlap between neurobiological models of PTSD and the nascent literature outlining the neurobiology of mindfulness, along with emerging work identifying neurobiological changes in individuals with PTSD following mindfulness-based interventions.35,36 Finally, a growing number of studies suggest that mindfulness-based interventions may be effective treatments for PTSD; these studies are also reviewed. We then discuss limitations and future directions.
Theoretical basis of mindfulness-based treatment approaches for PTSD
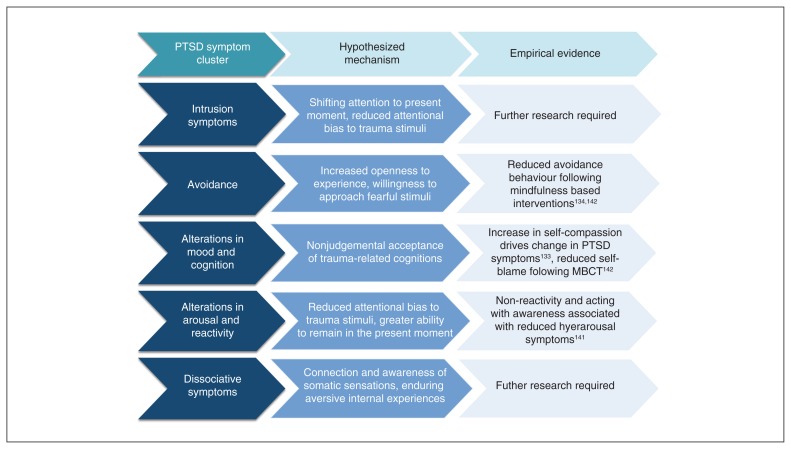
Mindfulness-based approaches, including MBSR and MBCT, are thought to target several core features of PTSD, including avoidance, hyperarousal, emotional numbing, negative emotions such as shame and guilt, and dissociation.26–28,37,38 Lang and colleagues27 discuss 3 components of mindfulness that may promote recovery from PTSD, including attention, a mindful cognitive style, and nonjudgment. Specifically, the authors explain how mindful, intentional shifting of attention to the present moment fosters a capacity for attentional control and may lead to reductions in attentional bias to trauma-related stimuli (see Fig. 1 for a summary of hypothesized mechanisms by which mindfulness-based approaches target symptoms of PTSD). Furthermore, a mindful cognitive style may reduce ruminative tendencies, leading to reductions in anxious arousal and anhedonia, and a nonjudgmental outlook may promote a willingness to approach fear-provoking stimuli, leading to reduced avoidance.27 Similarly, Follette and colleagues28 describe patterns of emotional numbing, suppression of intrusive thoughts and avoidance behaviours among individuals with PTSD as the antithesis of mindful behaviour, suggesting that nonjudgmental acceptance of thoughts, experiences and emotions as taught through mindfulness may reduce these symptoms.
Fig. 1.
Hypothesized mechanisms by which mindfulness-based approaches may target posttraumatic stress disorder (PTSD) symptom clusters along with current evidence and indication of where further research is required. MBCT = mindfulness-based cognitive therapy.
Another avenue through which mindfulness has been explored as an intervention for trauma-related disorders is metta mindfulness, or loving-kindness meditation. In metta meditation, users practise the intentional development of kindness and compassion toward themselves and others through verbal and visual exercises (e.g., imagining the experience of a particular emotional state with mindful awareness and attention).37,39,40 Metta meditation is hypothesized to promote emotional flexibility, or the ability to shift from negative to positive emotional states, and psychological flexibility, or the ability to distance oneself from one’s current mindset (affect, actions or responses, attentional bias) and contemplate other possible mindsets.39,40 These skills may be crucial to recovery from trauma-related disorders, where emotions such as shame, guilt, anger, inability to experience positive emotions (anhedonia) and lack of self-compassion, predominate.41–45 Specifically, by promoting the ability to experience positive emotions toward the self and others, one could expect reductions in anhedonia and negative emotions of shame, guilt and anger while fostering an increase in compassion for self and others.
In addition to being explored as an intervention, mindfulness has been shown to be a protective factor against the development of trauma-related psychopathology.46–52 Indeed, it has been suggested that pretraumatic mindful tendencies promote acceptance and awareness of posttraumatic responses, thereby reducing avoidance, re-experiencing and hyperarousal reactions to trauma-related stimuli and preventing the onset of PTSD.38 In particular, facets of mindfulness, including describing (the ability to label or note observed phenomena, such as emotions), acting with awareness and nonjudgment, mediate the association between childhood and lifetime trauma exposure and the risk for posttraumatic symptoms.46 Similarly, mindfulness has been reported to be predictive of reduced negative affect, rumination, depressive symptoms and posttraumatic stress symptoms via its association with cognitive fusion (the tendency to identify strongly with one’s thoughts and emotions) following trauma exposure.50 Further, a recent report indicated that mindfulness was negatively associated with disability among veterans, even after accounting for PTSD symptomatology, suggesting that mindfulness may influence functional outcomes.48
Dissociative symptoms may also be targeted by mindfulness-based approaches, where mindfulness is thought to foster skills in staying present and cultivating a connection to the self and others, thus reducing dissociative symptoms that are connected by the core feature of disconnection (e.g., from the present moment, others, or the self;53 Fig. 1). Here, Corrigan54 describes dissociation as existing on a continuum with mindfulness, with each concept occupying opposite poles on the continuum. Consistent with this, constructs of trait mindfulness, including describing, acting with awareness, nonjudgment and nonreactivity, have been found to correlate negatively with dissociation.55–57 With respect to treatment, Zerubavel and Messman-Moore53 suggest that mindfulness may be successful in reducing detachment by encouraging patients to endure aversive internal experiences and to reduce absorption (e.g., total immersion of attention to “nothing”; going blank) by increasing attentional control and reducing compartmentalization (e.g., fragmentation of the self). Through these mechanisms, mindfulness may confer increased openness to experience and a sense of connection to the self. Indeed, Frewen and Lanius58 suggest that mindfulness exercises may be particularly integral in facilitating reintegration of the self as a whole and increasing somatosensory and emotional awareness among individuals with prominent dissociative symptoms. Thus, mindfulness-based approaches may be efficacious in targeting both PTSD and PTSD+DS, a critical avenue for treatment development given that dissociative symptoms have been predictive of worse treatment response18,19 (but see the studies by Dahm and colleagues48 and Glück and colleagues49) and chronicity of illness.23
Figure 1 provides a summary of proposed mechanisms by which mindfulness-based approaches may reduce symptoms of PTSD. Intrusive and hyperarousal symptoms are hypothesized to improve via increased attentional control or the ability to shift attention away from trauma-related stimuli and to remain in the present moment. Mindfulness-based approaches are also hypothesized to target symptoms of avoidance by promoting openness to experiences and reducing negative mood states and alterations in cognition (e.g., negative beliefs about the self, the world, and others) by promoting nonjudgmental acceptance of current and past experiences. Finally, dissociative symptoms may also be targeted via increased connection to the self and greater awareness of internal and external experiences.
Despite the promise of mindfulness-based approaches as additional or adjunctive therapies, it is nonetheless critical to consider each patient’s symptom presentation and characteristics to determine if a mindfulness-based approach would be appropriate.58,59 Specifically, mindfulness-based approaches may increase distress or destabilize clients who are particularly prone to flashbacks, rumination, or easily triggered trauma memories, given that they reduce avoidance of trauma-related thoughts and emotions and may increase exposure to traumatic memories and emotional states.59 Similarly, mindfulness-based approaches may also be difficult for patients who have not developed appropriate emotion regulation or distress tolerance skills.59 Frewen and Lanius58 emphasize that although trauma-informed mindfulness interventions can be integral in the treatment of patients with PTSD, particularly those experiencing symptoms of depersonalization and derealization, they can be triggering for survivors of physical or sexual abuse, as exercises such as the body scan ask patients to become aware of different regions of the body. Thus, a paced and cautious approach involving the patient’s fully informed consent is necessary. A personalized medicine approach, whereby the individual characteristics of each patient are considered and integrated with research findings of the appropriateness of certain treatments for individuals with specific symptom presentations may help to identify those who would benefit most from augmentative mindfulness-based approaches to trauma treatment.
Convergence between neurobiological mechanisms of PTSD and mindfulness
Emotional over- and undermodulation in patients with PTSD
Early neurobiological models of PTSD emphasize a loss of top–down inhibition over limbic regions (e.g., amygdala), leading to exaggerated emotional reactivity and contributing to many of the hallmark symptoms of this disorder (e.g., hypervigilance, exaggerated startle response).60 Specifically, hypoactivation of the medial prefrontal cortex (mPFC; including the anterior cingulate cortex [ACC], ventromedial prefrontal cortex [vmPFC], subcallosal cortex and orbitofrontal cortex [OFC]) is associated with hyperreactivity of limbic regions (e.g., amygdala, anterior insula) to emotional stimuli.60 Moreover, abnormal functioning of the hippocampus is posited to lead to a reduced capacity to extinguish fear responses.60 These findings have largely been confirmed by recent meta-analyses of neuroimaging studies in patients with PTSD, where consistent hyperactivation of the amygdala and hypoactivation of cortical midline structures, including the mPFC, rostral ACC and OFC, have been reported.61,62
It is important to note that among individuals with PTSD+DS a contrasting pattern of activation is present, where emotional overmodulation of limbic structures (as opposed to undermodulation) is associated with symptoms of dissociation (e.g., depersonalization, derealization) and emotional numbing (inability to effectively experience emotions).7,63 Specifically, among this patient group, abnormally high activation in prefrontal regions involved in emotion modulation, including the dorsal ACC (dACC) and mPFC, has been noted during emotional script-driven imagery. In contrast, hypoactivation during such tasks is seen in limbic structures, including the amygdala and anterior insula.7,63–65 Notably, emotional over- and undermodulation may exist simultaneously among individuals with PTSD+DS.66 However, the predominant response in those with PTSD+DS is overmodulation, leading to prominent emotional detachment. Thus, PTSD and PTSD+DS are marked by impaired ability of cortical midline structures to accurately modulate the activity of limbic regions, leading to both emotional over- and undermodulation
Prefrontal modulation of limbic structures and mindfulness
Several studies have highlighted associations between mindfulness and changes in patterns of brain activation in regions impacted in patients with PTSD. Specifically, increased activation of the prefrontal cortex (including the dorsomedial PFC [dmPFC]) during expectation of negative pictures and reduced activation in the amygdala and parahippocampal gyrus following perception of negative stimuli has been observed following brief mindfulness training among healthy controls.67 Similarly, a study investigating MBCT in the treatment of bipolar disorder reported increased activity in the mPFC during a mindfulness task following treatment as well as correlations between signal changes in the mPFC and mindfulness, as measured by the Five Factor Mindfulness Questionnaire (FFMQ).68 Further studies have identified reduced amygdala reactivity in response to emotionally valenced images in healthy controls following a mindful attention group69 and during an emotional processing task among novice meditators.70
Critically, a recent study among individuals with generalized anxiety disorder reported increased functional connectivity between the ventrolateral PFC (vlPFC) and amygdala with associated reductions in anxiety symptoms following an 8-week MBSR intervention.71 Tang and colleagues72 suggest that positive coupling between these regions may be indicative of improved arousal monitoring rather than a downregulation of emotional response. Such improved monitoring may be beneficial for individuals with PTSD and with PTSD+DS, who show patterns of emotional under- and overmodulation. In addition, greater insular thickness has been noted among meditators,73 and a course of MBSR was associated with increased insular thickness and reduced alexithymia in meditation-naive individuals.74 Thus, via restoration of insular functioning, mindfulness-based approaches may be beneficial in improving body awareness and awareness of emotions, abilities that are often compromised in those with PTSD75–77 and are associated with emotional overmodulation.7,63
Emerging work has also noted neurobiological changes following a course of mindfulness-based exposure therapy (MBET) among individuals with PTSD. Here, MBET treatment consisted of 16 weeks of nontrauma-focused intervention, including elements of mindfulness training as in MBCT; psychoeducation; and exposure to avoided situations (excluding imaginal exposure or processing of trauma memories).36 Neural responses in an emotional face-viewing paradigm (fearful, angry and neutral faces) were compared between individuals who had completed MBET and individuals who had completed present-centred group therapy (PCGT; control condition focusing on current life stressors contributing to PTSD). Greater posttreatment activation of the left mPFC in response to fearful faces following MBET compared with PCGT was reported, suggesting increased modulation of limbic regions following MBET.
Taken together, these results suggest that mindfulness-based therapies may be effective in restoring top–down modulation of limbic regions with associated increases in modulation of emotional reactivity among individuals with PTSD. It is hypothesized that mindful emotion regulation is mediated by enhanced prefrontal cognitive control and concomitant downregulation of activity in limbic structures, including the amygdala.72,78 It is possible that increased modulation of limbic structures via mindfulness-based approaches36 could lead to further emotional overmodulation in individuals with PTSD+DS; however, it is also possible that mindfulness-based approaches may be associated with enhanced ability to accurately modulate limbic reactivity (e.g., via reducing or increasing top–down inhibition limbic regions, depending on the circumstances), as has been suggested by Tang and colleagues.72 Thus, future work will be necessary to elucidate the relative effectiveness of mindfulness in improving both emotional under- and overmodulation in individuals with PTSD and with PTSD+DS.
The triple network model of psychopathology and PTSD
The triple network model of psychopathology, introduced by Menon,79 details 3 key neural intrinsic connectivity networks (ICNs; brain regions that are temporally and functionally connected) that are implicated in psychiatric disorders and are integral to higher-order cognitive functioning. These include the default mode network (DMN), the salience network (SN) and the central executive network (CEN). The DMN is made up of cortical midline structures and the lateral parietal lobes, with key nodes in the mPFC, posterior cingulate cortex (PCC) and precuneus and connections to the parahippocampal gyri and thalamus. The DMN is thought to be involved in internal mentation, including self-referential processing, autobiographical memory and social cognition.80–82 The SN comprises key nodes in the anterior insula (AI) and dorsal anterior cingulate cortex (dACC), with connections to various subcortical regions, including the amygdala and thalamus.79,83,84 It is implicated in the detection, integration and filtering of salient internal and external stimuli as well as autonomic and emotion regulation and conflict monitoring.84–86 Finally, the CEN is anchored in the dorsolateral prefrontal cortex (dlPFC) and the posterior parietal cortex (PPC), and is heavily involved in processes such as working memory and executive functioning.87–89 Critically, whereas the DMN is thought to be active during rest while individuals engage in self-referential thought processes, including self-reflective thought, envisioning future events, and mind-wandering,90,91 it remains inactive during cognitively demanding tasks. Conversely, the CEN is generally inactive at rest and engaged during cognitively demanding tasks. Finally, the SN (particularly the AI) is thought to play a crucial role in regulating the dynamic interplay between CEN and DMN activation.79,83
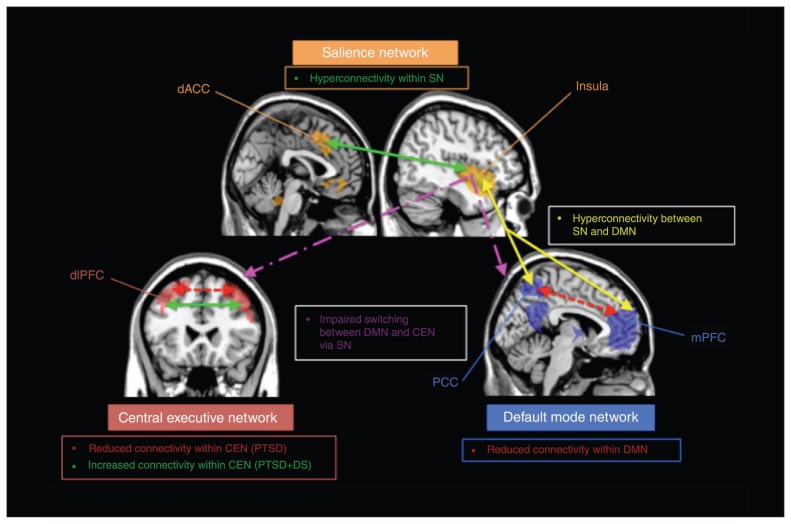
All 3 networks have been implicated in the neuropathology of PTSD. Figure 2 shows alterations in the DMN, CEN and SN in PTSD as they are currently understood. Two recent meta-analyses have highlighted reduced activation in areas of the brain associated with the DMN, including the mPFC, the PCC and posterior inferior parietal lobule, and the parahippocampal gyrus.61,92 Reduced functional connectivity between DMN nodes, including the PCC, posterior hippocampus and vmPFC, has also been reported92 and has been associated with PTSD symptom severity93,94 (Fig. 2). Reduced DMN functional connectivity is thought to underlie impairments in self-referential processes, autobiographical memory and altered sense of self seen in patients with PTSD.75,92 By contrast, increased resting-state functional connectivity among nodes of the SN, such as the amygdala and AI,92,94–96 as well as increased activation in SN regions at rest, including the AI, dACC and amygdala,61,92 have been reported consistently among individuals with PTSD. Such changes in SN nodes are posited to underlie hyperarousal symptoms in patients with PTSD and overall dominance of the threat sensitivity circuit.92 In addition, altered functional connectivity has been consistently noted between nodes of the DMN and SN, where increased connectivity has been reported between the ventral ACC (vACC; generally considered to be part of the mPFC) and PCC with the insula94,97 (Fig. 2). Furthermore, increased connectivity of the amygdala with the PCC/precuneus93,98 and the anterior insula94 has been noted, where connectivity between the amygdala and PCC/precuneus 6 weeks posttrauma predicted severity of PTSD symptoms at 12 weeks.93 Overall, patterns of increased connectivity between nodes of the SN and DMN are posited to reflect increased threat processing and hypervigilance at the expense of appropriate self-referential processing.92
Fig. 2.
Summary of the current literature implicating alterations in functional connectivity within and between the salience network (SN; shown in orange), the central executive network (CEN; shown in red) and the default mode network (DMN; shown in blue) in individuals with posttraumatic stress disorder (PTSD). Reduced connectivity within networks is depicted by red dashed lines, increased connectivity within networks is depicted by solid green lines, reduced connectivity between networks is depicted by pink dashed lines, and increased connectivity between networks is depicted by solid yellow lines. Consistent findings indicate reduced functional connectivity within the DMN among those with PTSD, posited to underlie disruptions in self-referential processes, autobiographical memory and altered sense of self. Conversely, increased connectivity is reported within the SN, thought to underlie hyperarousal and increased threat sensitivity. Similarly, increased connectivity between the DMN and SN is thought to reflect hypersensitivity to threat at the expense of self-referential processing. Individuals with PTSD also show impaired ability to appropriately recruit relevant networks (e.g., activation of DMN rather than CEN during a working memory task), suggesting impaired switching between the DMN and CEN via the SN. Distinct patterns of connectivity within the CEN have emerged among those with PTSD and PTSD with dissociative symptoms (PTSD+DS); those with PTSD+DS showed increased connectivity within the CEN and those with PTSD showed decreased connectivity within the CEN. dACC = dorsal anterior cingulate cortex; dlPFC = dorsolateral prefrontal cortex; mPFC = medial prefrontal cortex; PCC = posterior cingulate cortex.
Activity and connectivity of the CEN is also disrupted in individuals with PTSD, with meta-analytic findings pointing to reduced activity in the dlPFC.61 Interestingly, one study reported inappropriate activation of the DMN during a working memory task among patients with PTSD that contrasted with appropriate activation of the CEN among controls, suggesting an inability to recruit task-positive networks in individuals with PTSD.99 In addition, reduced resting state functional connectivity among frontoparietal regions of the CEN have been associated with PTSD symptoms and trauma history100 (Fig. 2). Notably, increased connectivity between DMN nodes and the dlPFC has been associated with dissociative symptoms in patients with PTSD.98 In addition, increased connectivity within the CEN during supra- and subliminal threat processing was noted among women with PTSD+DS (Fig. 2), suggesting hyperconnectivity of the CEN and potentially increased top–down inhibition of limbic regions.101
Mindfulness and the triple network model of psychopathology
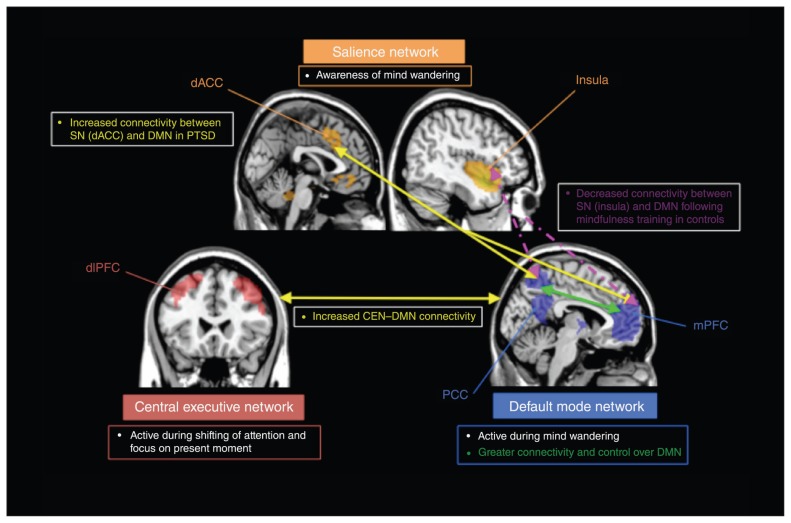
Figure 3 depicts hypothesized mechanisms through which mindfulness-based approaches may improve functioning of the DMN, SN and CEN, and therefore target symptoms of PTSD. Mindfulness has been consistently linked with activity and connectivity within and between the DMN, SN and CEN, with each network responsible for different stages of mindfulness meditation among experienced meditators.102 Specifically, mind wandering has been associated with activity in the DMN, and awareness of mind wandering has been associated with activity in the SN, while shifting of attention back to focus on the present and subsequent focus on present experience has most strongly been associated with activity in the CEN.102 Default mode network activity and connectivity has been suggested as a potential biomarker for monitoring the therapeutic effects of meditation.103 Specifically, whereas self-referential processing and activity within the DMN is associated with mind wandering, the antithesis of mindful awareness of the present moment, mindfulness promotes detachment of identification with the contents of conscious thoughts, known as “reperceiving” or “decentering.”103,104 Activation of the DMN during mindful states is decreased in experienced meditators105,106 and following MBSR training in meditation-naive participants,107 and greater activation of the mPFC and functional connectivity of the mPFC with the DMN during rest (e.g., during self-referential processing) has been shown among meditators compared with controls108 (Fig. 3). Taken together, these findings suggest that mindfulness-based interventions may be associated with increased ability to appropriately bring online the DMN when necessary (e.g., during self-referential processing at rest) and in conferring greater cognitive control over the DMN when its activation is not desired (e.g., during mindful awareness of the present). These findings may translate to individuals with PTSD who typically show reduced resting-state activation and connectivity of this critical network for self-referential processing.
Fig. 3.
Summary of findings suggesting that mindfulness may lead to restoration of functioning of the salience network (SN; shown in orange), central executive network (CEN; shown in red) and defult mode network (DMN; shown in blue). Increased connectivity within networks is depicted by solid green lines, increased connectivity between networks is depicted by solid yellow lines, and reduced connectivity between networks is depicted by dashed pink lines. Emerging work has indicated greater functional connectivity within the DMN during rest among meditators when compared with controls and among veterans with posttraumatic stress disorder (PTSD) following mindfulness intervention, suggesting that it may restore DMN connectivity and appropriate self-referential processing in those with PTSD.35 Increased CEN–DMN connectivity was also reported and may reflect increased ability to shift between internal and external loci of attention. Mixed findings of both increased and decreased DMN–SN connectivity following mindfulness intervention have been reported, depending on the region of the SN. Increased dorsal anterior cingulate cortex (dACC)–DMN connectivity was reported following mindfulness intervention for PTSD,35 which may suggest increased capacity for attentional shifting from internal to external stimuli (dACC implicated in executive control). In contrast, reduced SN (insula)–DMN connectivity was reported among controls, which may result in reduced hyperarousal symptoms and increased self-referential processing if findings were replicated in individuals with PTSD. dlPFC = dorsolateral prefrontal cortex; mPFC = medial prefrontal cortex; PCC = posterior cingulate cortex.
Emerging work among veterans with PTSD who participated in an MBET group (as described earlier) has identified potential neural markers of symptom change within the ICNs.35 Here, MBET was associated with increased DMN connectivity with the dlPFC, a main node of the CEN; no such changes were reported in a PCGT comparison condition (Fig. 3). Furthermore, the authors noted that increased DMN–CEN connectivity was associated with reduced avoidant and hyperarousal symptoms, which the authors suggested may reflect an increased capacity for voluntary control of attention and the ability to shift attention from internal self-referential processing via the DMN (e.g., rumination) to other forms of internal experiences, including interoception via the CEN, thus leading to greater emotional regulation abilities.35 Notably, the authors also reported increased DMN–SN (dACC) connectivity in the MBET group following treatment (Fig. 3). The authors note that this finding may seem contradictory given previous work showing increased SN–DMN connectivity among individuals with PTSD (as described earlier), which is thought to underlie increased sensitivity to threat.93,94,97,98 However, King and colleagues35 suggested that given the role of the dACC in attentional and executive control, increased DMN–SN (dACC) connectivity may reflect an increased capacity for attentional shifting from internal self-referential states to external stimuli, as is suggested in the case of increased DMN–CEN connectivity.
An additional key alteration in ICNs among individuals with PTSD is increased functional connectivity and activity in nodes of the SN at rest. As yet, few studies have examined the impact of mindfulness-based interventions on resting state functional activity of the SN. However, emerging work has suggested that the SN is activated during certain aspects of mindfulness (e.g., awareness of mind wandering), but not during others (e.g., mind wandering or attention to present moment) among experienced meditators compared with inexperienced meditators.102 These findings suggest that mindfulness may lead to selected use of ICNs during specific stages of the mindfulness process and overall greater control over the use of these networks. This is particularly pertinent, given that heightened resting state functional connectivity of the SN may indicate inappropriate use of the network in the absence of salient internal or external stimuli among individuals with PTSD. Conversely, several sources have indicated increased activity of the AI (a main node of the SN) during mindful states,78,109,110 which may be construed as counterproductive given heightened resting-state activation of SN regions in patients with PTSD. Notably, in these studies it is not clear what aspect of mindfulness is used while the AI is active (e.g., attention to external stimuli v. awareness of mind wandering). Furthermore, studies investigating trait mindfulness have reported that individuals with greater trait mindfulness exhibit lower AI activation during expectation of and exposure to negative stimuli. These results point toward reduced automatic emotional responding,67,111 which could be expected to lead to reduced hyperarousal in individuals with PTSD if these results were replicated in this population.
Finally, altered internetwork connectivity has been noted among individuals with PTSD. Specifically, hyperconnectivity between DMN and SN nodes among individuals with PTSD has been cited as a potential cause of increased hyperreactivity and threat processing at the expense of effective self-referential processing.92 Similarly, increased connectivity between the DMN and CEN has been associated with dissociative symptoms.98 Critically, a recent study reported that increased scores on measures of mindfulness following 2 weeks of self-guided attention to breath training among healthy controls was associated with reduced resting state connectivity between the SN (anterior insula) and the DMN.112 Similar findings of decreased connectivity between hubs of the DMN and SN have been reported among experienced meditators102 (Fig. 3). Doll and colleagues112 posit that this reduced interconnectivity between the DMN and SN may represent a clearer distinction between networks, and thus better effective connectivity of individual networks. Doll and colleagues112 also describe trend-level data suggesting reduced connectivity between the CEN and DMN among more mindful individuals that could indicate a greater ability to switch between networks when attending to pertinent sensory experiences. However, other groups have noted increased connectivity of DMN regions (PCC) with CEN (dlPFC) and SN (dACC) regions during meditation among experienced meditators105 (Fig. 3). Notably, a critical difference between these studies is engagement in meditation105 versus rest112 during scanning. Accordingly, among individuals with PTSD, whereas reduced resting state connectivity between the SN and DMN may lead to reduced hyperreactivity responses (particularly to internal stimuli) and the restoration of self-referential processing,92 reduced resting state connectivity between the DMN and CEN may reduce symptoms of dissociation.98
Of note, the cognitive control domain (the ability to flexibly and adaptively use cognitive resources) of the Research Domain Criteria (RDoC) has been closely linked to the functioning of both the CEN and SN and has been highlighted as an important transdiagnostic impairment across psychiatric illnesses.113,114 Thus, the potential for mindfulness-based approaches to increase the functional integrity of the CEN and SN, and hence the ability to accurately bring online pertinent ICNs, should be further studied with respect to the ability to increase cognitive control.
Mindfulness and connectivity of subcortical brain structures
The thalamus has been identified as a key node whose functional connectivity with the DMN may underlie mindfulness. Specifically, Wang and colleagues115 found that the thalamus was the only node within the DMN that was consistently linked with trait mindfulness, where reduced connectivity of the thalamus with the DMN was related to higher trait mindfulness. The authors postulate that excessive connectivity of the thalamus with the DMN may promote mind wandering and reduce the ability of the thalamus to effectively contribute to other networks with which it is involved. Specifically, the thalamus is a key contributor to the ascending reticular activating system (ARAS; a network critical for the regulation of wakefulness and vigilance), and may act as a switch between the DMN and ARAS system.115 Similarly, the pulvinar nucleus of the thalamus is a key node of the innate alarm system (IAS), a network of interconnected brain regions involved in subconscious detection of threat,116–119 allowing rapid activation of defensive responses conferring an evolutionary advantage by rapidly facilitating response to threat.120,121 The IAS has recently been described as a brain-network that shows aberrant functional connectivity among individuals with PTSD during subconscious and conscious threat processing,122–126 including heightened activity of the thalamus, amygdala and parahippocampal gyrus during subconscious threat processing in individuals with PTSD+DS in response to fearful faces, suggesting exaggerated IAS responding to subconscious threat.64 Given the emerging role of thalamus connectivity to the DMN in mindfulness, it will also be important to determine the potential utility of mindfulness-based interventions in targeting dissociative symptoms associated with PTSD. Here, according to the defence cascade model of dissociation, when an organism deems the level of threat in a given situation to be insurmountable, they may engage in tonic or collapsed immobility (states of reduced arousal that may promote survival by mimicking death), whereby “functional sensory de-afferentation” mediated by the thalamus leads to reduced sensory integration and input to the cortex, a process thought to be mirrored by dissociation in traumatized individuals.127,128 Thus, restoration of thalamic connectivity with the ARAS as a consequence of decreased thalamic connectivity with the DMN may promote decreased dissociation among patients with PTSD+DS. Indeed, mindfulness-based skills have been suggested as strategies to shift out of dissociative states by improving awareness of mind–body states (possibly via the thalamus) through focus on interoceptive, proprioceptive and touch sensations (e.g., during a body scan).
Evaluation of the evidence for mindfulness-based treatments of PTSD
A growing number of studies have investigated the efficacy of mindfulness-based treatments, including MBSR and MBCT, among trauma-exposed populations with PTSD and other primary diagnoses. Most of these studies have been completed in veteran samples, with a handful of studies in other trauma-exposed populations (e.g., developmental trauma, interpersonal trauma, natural disasters). Table 1 summarizes the studies reviewed here and their main findings. Figure 1 links hypothesized mechanisms by which mindfulness-based approaches target symptoms of PTSD and current empirical evidence.
Table 1.
Overview of included treatment studies and their main findings
| Study | Sample | Assigned therapy | Assessments | Study type | Attrition | Main findings |
|---|---|---|---|---|---|---|
| Bergen-Cico et al.135 | 40 veterans (90% male) with PTSD | BMP based on MBSR (4 weekly 90-min sessions) plus TAU or to TAU alone (typical primary care for veterans) | Salivary cortisol PCL, PHQ-9 (measure of depression) | RCT, pre/post measures | 20% drop-out rate | BMP completers showed significant reduction in CAR (0.2 μg/dL) TAU and noncompleters did not show a significant decrease in CAR Significant correlation between changes in cortisol levels and PTSD and depression scores |
| Bormann et al.146 | 146 veterans (142 male) with PTSD | MRP (6 weekly 90-min classes) or TAU alone (case management and consultation as needed) | CAPS, PCL-C, BSI-18 (depressive symptom subscale), SF-12 (mental health component), MAAS | RCT, pre/post measures | 95% of MRP+TAU completed treatment | Significantly greater reduction in PCL-C, CAPS hyperarousal and numbing symptoms, depression, and mental HRQOL in MRP+TAU group Significantly greater improvement on MAAS in MRP+TAU group Mindful attention mediated effect of MRP on PTSD, depression and psychological well-being measures Daily mantrum practice mediated effect of MRP on mindful attention |
| Catani et al.145 | 31 children (17 male) exposed to tsunami with working diagnosis of PTSD | Meditation–relaxation (individual psychoeducation and meditation relaxation strategies) or KIDNET (individual narrative exposure therapy adapted for children) | UPID (5 items to assess problems in functioning, 5 items to assess presence of somatic complaints) | RCT, pre/post measures; 6-mo follow-up | 100% completed full treatment | No significant difference between groups on PTSD symptoms Significant reduction in PTSD scores within meditation–relaxation group immediately posttreatment (d = 1.83) and at follow-up (d = 2.20) 71% of meditation–relaxation children did not meet criteria for PTSD at 6-mo follow-up and 81% did not meet criteria in KIDNET group (no significant difference) Significant improvement on functional scores in both treatment groups (no significant difference) |
| Cole et al.129 | 10 veterans with history of mTBI and PTSD | MBSR (1 introductory 2-hr class, 8 weekly 2.5-hr sessions, 1 7-hr retreat) | PCL-C, Cogstate computerized assessment to measure attention | Single arm, uncontrolled study, pre/post measures; 3-mo follow-up | 90% completed treatment | Significant reductions in PCL-C scores immediately posttreatment (d = 1.56) and at follow-up (d = 0.93) Significant improvement on attention measures immediately posttreatment (d = 0.57), not maintained at follow-up |
| Earley et al.130 | 19 women survivors of CSA with general severity index BSI score > 0.50 | MBSR (8 weekly 2.5–4 hr classes and 1 5-hr retreat (augmented for CSA) with concurrent psychotherapy | BDI-II, PCL, BSI-18, MAAS | Single arm, uncontrolled study; 2.5-yr follow-up of previous study133 | NA | Improvements at 1 mo posttreatment maintained at 2.5-yr follow-up for depression (d = 1.10), anxiety (d = 0.90), and PTSD symptoms (d = 0.80) PCL subscales significantly lower from baseline at 2.5-yr follow-up: avoidance/numbing (d = 0.70), re-experiencing (d = 0.50), hyperarousal (d = 0.90) |
| Gallegos et al.139 | 42 women with history of interpersonal violence and high perceived stress | MBSR (8 weekly 2.5-hr sessions, 1 day-long retreat) | TLEQ, STAI, DERS, CDES, MPSS, FFMQ, IL-6, TNF-α, CRP | Single arm, uncontrolled study, pre/mid/post measures; 1-mo follow-up | 57% completed more than 50% of classes | Significant reductions in depressive symptoms at all time points Significant reductions in PTSD symptoms, state and trait anxiety immediately posttreatment and at follow-up Significant improvement in DERS scores immediately posttreatment and at follow-up Significant effect of attendance on IL-6 levels (reduced IL-6 with increased attendance) |
| Goldsmith et al.131 | 10 individuals with exposure to lifetime trauma or childhood abuse (9 female) with primary diagnosis of PTSD or MDD | MBSR (8 weekly 2.5-hr sessions with 1 day-long retreat) | PHQ-9, BDI-II, PCL, CTQ, LEC, AAQ-II (measure of experiential avoidance), TAQ | Single arm, uncontrolled study, pre/mid/post measures | 90% retention | Significant reduction at mid-treatment and post-treatment in PTSD symptoms (d = 0.70, d = 0.73), depression (d = 0.30, d = 0.54) and TAQ shame-based appraisals (d = 0.30, d = 0.70) Significant improvement in AAQ scores mid-treatment and post-treatment (d = 0.77, d = 1.11) |
| Kearney et al.132 | 92 veterans with PTSD | MBSR (8 weekly 2.5-hr sessions and 1 7-hr retreat) | PCL-C, PHQ-9, BADS, SF-8 (mental and physical HRQOL), AAQ-II, FFMQ | Single arm uncontrolled study, pre/post measures; 4-mo follow-up | 74% met minimum compliance (4 of 8 classes) | Significant improvement at baseline and follow-up on PCL total (d = 0.55; d = 0.65), PCL re-experiencing (d = 0.40; d = 0.56), avoidance (d = 0.36; d = 0.35), emotional numbing (d = 0.46; d = 0.54), and hyperarousal (d = 0.64; d = 0.67) Significant improvement at baseline and follow-up on depression score (PHQ-9; d = 0.53; d = 0.70), BADS (d = 0.47; d = 0.62), mental HRQOL (d = 0.62, d = 0.73), and AAQ (d = 0.65; d = 0.68) Clinically significant reductions in PCL scores in 47.7% of participants Changes in FFMQ scores from baseline to post-treatment significantly predicted PCL, PHQ-9, mental HRQOL immediately post-treatment and at follow-up |
| Kearney et al.133 | 47 veterans (37 men) with chronic PTSD | MBSR (8 weekly 2.5-hr sessions and 1 7-hr retreat) plus TAU or TAU (usual care for PTSD within veterans health administration clinics) | PCL-C, LEC, PHQ-9, SF-8, FFMQ, BADS | RCT, pre/post measures; 4-mo follow-up | 84% met minimum compliance in MBSR group (4 of 8 sessions) | No significant difference between MBSR and TAU groups on PTSD, depression or behavioural activation immediately post-intervention or at follow-up Significantly greater improvement in mental HRQOL in MBSR group post-treatment (d = 0.69), but this was not maintained at follow-up Significant within-group improvement in the MBSR group on PTSD (d = 0.64), depression (d = 0.65), and mental HRQOL (d = 0.77) post-treatment (maintained only for mental HRQOL at follow-up) Significant improvement in mindfulness scores immediately post-treatment (d = 0.65) and at follow-up (d = 0.67) in the MBSR group |
| King et al.142 | 37 veterans with long-term (> 10 yr) PTSD or PTSD in partial remission | MBCT adapted for PTSD (8 weekly 8-hr group sessions) or TAU (psychoeducation and skills training, 8 weekly 1-hr sessions) or imagery research therapy (6 weekly 1.5-hr sessions) | CAPS (all groups), PDS (MBSR group only), PTCI (MBSR group only) | Nonrandomized controlled study, pre/post measures | Dropout 25% in MBCT and 23.4% in TAU groups | Significant reduction in CAPS score (d = 2.20) within MBCT group (ITT) Significantly greater improvement on CAPS score in MBCT than in TAU group (d = 1.14; ITT) Improvements on CAPS score in MBCT group explained by significant reduction in avoidant subscale (d = 2.11; ITT) Significant reductions in CAPS intrusive (d = 0.64) and hyperarousal (d = 0.78) symptoms also seen in MBCT group (ITT) 73% in MBCT group attained clinically significant reductions in CAPS score (33% in TAU group; completer analysis) Significant reduction in PDS numbing subscale (d = 0.57) and PTCI self-blame cognitions (d = 1.80) in MBCT group (completer analysis) |
| King et al.35 | 43 veterans with PTSD | MBET (16-wk nontrauma focused intervention; mindfulness, psychoeducation, self-compassion training; in-vivo exposure to avoided situations [no trauma exposure]) or PCGT (16-wk intervention identifying current stressors contributing to PTSD) | CAPS | RCT, pre/post measures | Not reported | MBET participants attended an average of 13.5 of 16 sessions; PCGT group attended an average of 7.5 of 16 sessions No significant differences between groups on PTSD symptom severity differences between pre- and post-treatment assessments MBET group showed significant reduction in total CAPS (d = 0.96), CAPS intrusion (d = 0.72) and CAPS avoidance (d = 0.97) symptoms PCGT group showed significant reduction in CAPS hyperarousal symptoms only (d = 0.79) |
| Kim et al.143 | 22 nurses with PTSD, 7 healthy control nurses | MBX (16 semi-weekly 60-min sessions) or control condition | PCL-C, serum cortisol, plasma ACTH, DHEAS | RCT, pre/post measures; 2-mo follow-up | Not reported | Significantly greater decrease in PTSD symptoms and cortisol levels in MBX group than in controls No significant differences between groups in ACTH and DHEAS levels MBX group showed significant reductions in PTSD symptoms (including re-experiencing, avoidance, and hyperarousal) at 2-mo follow-up Significant association between cortisol levels and PTSD symptoms |
| Kimbrough et al.134 | 27 survivors of CSA (24 women) with general severity index BSI score > 0.50 | MBSR (8 weekly 2.5–4 hr classes and 1 5-hr retreat augmented for CSA) with concurrent psychotherapy | BDI-II, PCL, BSI, MAAS, practice logs and attendance monitoring | Single arm uncontrolled study, pre/mid/post measures; 4-mo follow-up | 85% retention | Significant reduction immediately post-treatment and at follow-up on depression scores (d = 1.8; d = 1.0), anxiety (BSI; d = 1.1; d = 0.90), PTSD symptoms (d = 1.2; d = 1.0) Significant reductions immediately post-treatment and at follow-up on PTSD avoidance/numbing (d = 1.4; d = 0.90), re-experiencing (d = 0.70 both time points), and hyperarousal (d = 1.2; d = 0.60) Significant reduction in individuals meeting criteria for PTSD post-treatment but not at follow-up |
| Niles et al.137 | 33 veterans with current PTSD | MBSR-based telehealth group (2 45-min in-person sessions and 6 20-min weekly phone calls with weekly individual practice) or telehealth psychoeducation with same contact | CAPS, PCL-M, PSQ | RCT, pre/post measures; 6-wk follow-up | 76% completed MBSR treatment | MBSR group showed significant decrease in PCL score (d = 0.84) and decrease in CAPS score (d = 0.70) At 6-wk follow-up, changes in PTSD in MBSR group were not sustained (d = 0.16) Significantly greater improvement in MBSR group at posttreatment on PCL (d = 1.95) and CAPS scores (d = 1.27) |
| Polusny et al.138 | 116 veterans with PTSD or subthreshold PTSD | MBSR (8 weekly 2.5-hr sessions and 1 day-long retreat) or PCT (9 weekly 1.5-hr sessions) | PCL, CAPS, PHQ-9, FFMQ, WHOQOL | RCT, pre/post measures; 2-mo follow-up | Dropout 22.4% in MBSR and 6.9% in PCT | Significantly greater reductions in PCL (d = 0.40), CAPS (d = 0.41), WHOQOL (d = 0.41) scores in MBSR group between baseline and 2-mo follow-up Nonsignificant differences between groups on depressive scores (similar improvement in both groups) Improvements of FFMQ scores significantly correlated with PTSD (PCL), depression and WHOQOL scores |
| Possemato et al.136 | 62 veterans with PTSD or subthreshold PTSD | BMP (based on MBSR, 4 weekly 90-min sessions) plus TAU or TAU alone (typical primary care for veterans) | CAPS, PCL, PHQ-9, FFMQ, MAAS | RCT, pre/post measures; 1-mo follow-up | 20% dropout rate | No significant difference between BMP+TAU and TAU groups using ITT analysis for CAPS and PCL scores Significantly greater improvement in BMP+TAU group on depression scores (d = 0.86) BMP+TAU completers showed significantly larger decreases in PTSD severity (CAPS; d = 0.72) and depression scores (PHQ-9; d = 0.99) FFMQ describing, nonjudgment and acting with awareness and MAAS scores accounted for 30% of total effect of BMP completion on PTSD severity |
| Rosenthal et al.144 | 7 veterans with PTSD (all men) | TM (taught in 2 information lectures, brief personal interview, individual instruction and 3 follow-up sessions on 3 consecutive days; participants asked to meditate at home for 20 min twice daily for 12 wk) | CAPS, PCL-M, Q-LES-Q, BDI, CGI-S, CGI-I, CES | Single arm uncontrolled trial, pre-treatment measures; 8-wk follow-up | 71% completed | Significant improvement on CAPS, Q-LES-Q, PCL-M, CGI-I at week 8 |
AAQ-II = Acceptance and Action Questionnaire-II; ACTH = adrenocorticotropic hormone; BADS = Behavioural Activation for Depression Scale; BDI-II = Beck Depression Inventory-II; BMP = Brief Mindfulness Program; BSI-18 = 18-item Brief Symptom Inventory; CAPS = Clinician-Administered PTSD scale; CAR = cortisol-awakening response; CDES = Center for Epidemiological Studies Depression Scale; CES = Combat Exposure Scale; CGI-I = Clinical Global Impression Improvement; CGI-S = Clinical Global Impression Severity; CRP = C-reactive protein; CSA = childhood sexual abuse; CTQ = Childhood Trauma Questionnaire; DERS = Difficulties in Emotion Regulation Scale; DHEAS = dehydroepiandrosterone sulfate; FFMQ = Five Factor Mindfulness Questionnaire; HRQOL = health-related quality of life; IL-6 = interleukin-6; ITT = intention to treat; MAAS = Meditation Attention and Awareness Scale; MBSR = mindfulness-based stress reduction; MBX = mindfulness-based stretching and deep breathing exercises; MDD = major depressive disorder; MPSS = Modified PTSD Symptom Scale; LEC = Life Events Checklist; MBET = mindfulness-based exposure therapy: MRP = mantram repetition practice; mTBI = mild traumatic brain injury; NA = not applicable; PCGT = present-centred group therapy; PCL = PTSD Check List; PCL-C = PTSD Check List–Civilian; PCL-M = PTSD Check List–Military; PDS = PTSD Diagnostic Scale; PHQ-9 = Patient Health Questionnaire-9; PSQ = Patient Satisfaction Questionnaire; PTCI = Post-traumatic cognitions inventory; PTSD = posttraumatic stress disorder; Q-LES-Q = quality of life enjoyment and satisfaction questionnaire; RCT = randomized controlled trial; SF-8/SF-12 = 8-item/12-item Short-Form Health Survey; STAI = Spielberger State-Trait Anxiety Inventory; TAQ = Trauma Appraisals Questionnaire; TAU = treatment as usual; TLEQ = Traumatic Life Events Questionnaire; TM = transcendental meditation; TNF-α; tumour-necrosis factor-α; UPID = University of California, Los Angeles PTSD index for DSM-IV; WHOQOL = World Health Organization Quality of Life.
Mindfulness-based stress reduction for PTSD
Standard and trauma-adapted MBSR are the most frequently assessed mindfulness-based therapies among trauma-exposed populations, with 2 pilot studies, 3 larger uncontrolled studies and 5 randomized controlled trials (RCTs) reviewed here.129–139 In a recent pilot study Cole and colleagues129 investigated standard MBSR as a treatment for both PTSD symptoms and attention difficulties among veterans with PTSD and a history of mild traumatic brain injury (mTBI), reporting low drop-out rates (10%), significant reductions in self-reported PTSD symptoms and significant improvements on attention measures posttreatment. In that study, PTSD symptom reduction was maintained at 3-month follow-up, although attention improvements were not.129 Similarly, Gallegos and colleagues139 reported significant reductions in self-reported depressive and PTSD symptoms and improvements in emotion regulation immediately following standard MBSR treatment and at 1-month follow-up among women with a history of interpersonal violence and high perceived stress. However, the authors noted lower retention, with 43% of participants classified as noncompleters.
A number of larger uncontrolled studies have also reported favourable outcomes following standard and trauma-adapted MBSR treatment among individuals with PTSD.130–132,134 Goldsmith and colleagues131 reported significant improvements following a course of standard MBSR at midtreatment and posttreatment on self-report measures of PTSD, depressive symptoms and shame-based trauma appraisals among individuals with PTSD of mixed etiology. Similarly, Kearney and colleagues132 reported significant improvements immediately posttreatment and at follow-up following standard MBSR on PTSD re-experiencing, avoidance, emotional numbing and hyperarousal symptoms and on measures of depression, experiential avoidance and mental health–related quality of life (HRQOL) among a sample of veterans. Another study investigating treatment with MBSR modified to emphasize safety and positive growth experiences found particularly large reductions on self-reported PTSD avoidance/numbing symptoms and re-experiencing, hyperarousal, depression and anxiety symptoms among women with PTSD as a result of childhood sexual abuse.134 These gains were maintained 2.5 years later,130 showing the potential long-term utility of MBSR. Moreover, these studies reported low drop-out rates (10%–16%), suggesting high treatment acceptability.131,132,134
A handful of RCTs investigating the efficacy of MBSR have been completed among trauma-exposed populations.133,136–138 The largest of these was a recent study in which 116 veterans with full or subthreshold PTSD were randomly assigned to receive MBSR (augmented to include psychoeducation about trauma) or present-centred therapy (PCT; focused on current problems as manifestations of PTSD).138 Significantly greater reductions in self-report and clinician-rated (Clinician Administered PTSD Scale [CAPS]140) PTSD symptoms and improvements in quality of life were noted in the MBSR group (medium effect sizes) with adequate retention rates (78%). Importantly, group differences emerged at the 2-month follow-up, but were not present posttreatment (equivalent symptom reduction was seen in both groups), suggesting that MBSR may be more effective than PCT at maintaining symptom reduction. Similarly, Niles and colleagues137 reported high treatment acceptability (18% dropout rate) and significantly greater improvements on self-report and clinician-rated (CAPS) PTSD symptoms (large effect size) among veterans who participated in a telephone MBSR program compared with those who participated in a telephone psychoeducation program; however, these results were not maintained at follow-up.
In contrast to those studies, Possemato and colleages136 did not find significant differences on PTSD symptom severity (using intention to treat [ITT] analysis) among veterans who participated in a brief mindfulness program (4 wk) based on MBSR compared with those who received treatment as usual (TAU). However, completer analysis (including participants who attended all classes) showed significantly greater improvements on PTSD severity (CAPS) and depressive symptoms among the mindfulness group compared with the TAU group, with medium to large effect sizes.136 The authors posited that a minimum of 4 treatment sessions was needed to attain significant symptom reduction.136 Similarly, Kearney and colleagues133 reported significant within-group improvements on measures of PTSD and depressive symptoms posttreatment among veterans taking part in a standard MBSR program (not maintained at follow-up). However, this study did not show significant differences between veterans receiving MBSR in addition to TAU and those receiving only TAU on any clinical measure except for an assessment of mental HRQOL.
In summary, MBSR has emerged as a promising treatment approach for PTSD, with recent studies reporting significant reductions in PTSD symptomatology following standard MBSR compared with PCT,138 brief MBSR compared with TAU when a minimum number of treatment sessions was met136 (but see the study by Kearney and colleagues133), and telephone MBSR compared with psychoeducation.137 In addition, MBSR appears to have a high level of acceptability among patients, with most studies reporting low drop-out rates of 10%–22%129,131,132,134,137,138 (but see the study by Gallegos and colleagues139). With respect to mechanisms of change, aggregate data from 2 studies by Kearney and colleagues132,133 and 2 unpublished studies reported changes in nonreactivity and acting with awareness on the FFMQ to be most strongly associated with improvements in PTSD symptoms, particularly hyperarousal symptoms.141
Mindfulness-based cognitive therapy for PTSD
In addition to investigations of the utility of MBSR among individuals with PTSD, one study has investigated the efficacy of MBCT augmented for treatment of PTSD. In that study, King and colleagues142 assigned (nonrandomized) 37 veterans with chronic PTSD (> 10 yr) to receive either MBCT for PTSD or to 1 of 2 control conditions, psychoeducation with skills training or imagery rehearsal therapy (focuses on reframing nightmare content). The authors found significantly greater improvements on PTSD symptoms (CAPS) in the MBCT group than in the control groups using ITT analysis (large effect size), which was largely explained by reductions in scores on the CAPS avoidance subscale. In addition, the authors found that a significantly greater number of veterans in the MBCT group than in the control groups achieved clinically significant reductions in PTSD symptoms (73% v. 33%). Moreover, among those who completed treatment (75% of the MBCT group), significant reductions in numbing symptoms and self-blame cognitions were noted. Thus, MBCT shows promise as an additional mindfulness-based approach to treating PTSD, with reductions in avoidance symptoms emerging as a key mechanism of change.
Additional mindfulness-based approaches for PTSD
Alternative mindfulness-based approaches for the treatment of PTSD, including metta mindfulness approaches,143–148 have also been studied. A recent pilot study of a 12-week loving-kindness meditation intervention for veterans with PTSD reported increased self-compassion and mindfulness skills and reductions in PTSD symptoms (large effect size) and depressive symptoms (medium effect size) at the 3-month follow-up, with 74% attending at least 9 of 12 classes.147 Further, mediation analyses identified changes in self-compassion as a driver of changes in PTSD and depressive symptoms,147 while additional analysis revealed increased feelings of mastery, personal growth, life purpose, self-acceptance and decentring.148
Mantrum repetition practice (MRP), the silent repeating of a sacred word or phrase, which is thought to reduce stress, anxiety and anger and to increase mindful attention, was recently studied in a large sample of veterans with PTSD assigned to receive TAU or MRP+TAU.146 The authors reported significantly greater reductions in self-reported and clinician-rated (CAPS) PTSD symptomatology and hyperarousal and numbing symptoms as well as decreased self-reported depression symptoms and improved mental HRQOL in the MRP+TAU compared with the TAU group. Critically, the authors found this approach to be highly acceptable among veterans, with 95% of the sample completing treatment.146 Similarly, Rosenthal and colleagues144 studied the effectiveness of a transcendental meditation (a form of mantra meditation) program in a sample of 7 veterans with PTSD (5 completed treatment) and reported significant improvements on CAPS scores as well as a quality of life measure. Another recent study compared the effectiveness of a meditation–relaxation program (including mantra repetition and breathing exercises) to a validated narrative exposure therapy for children (KIDNET)149 among children with probable PTSD (all criteria except duration met) following exposure to a tsunami.145 The authors reported 100% participant retention and equivalent reductions in PTSD symptoms immediately post-treatment and at 6-month follow-up, with large effect sizes for both treatment modalities as well as improvements in functional outcomes (e.g., self-reported school performance). At the 6-month follow-up 71% of children in the meditation–relaxation treatment (81% in KIDNET) no longer met criteria for PTSD, and there were no significant differences between groups on remission rates. A similar intervention using mindfulness-based stretching and deep breathing exercises (MBX) compared with a control group among intensive care unit (ICU) nurses led to significantly greater reductions in PTSD re-experiencing, hyperarousal and avoidance symptoms.143
Thus, mantra repetition and meditation–relaxation treatments are also emerging as efficacious approaches to the treatment of PTSD compared with TAU146 and control conditions.143 Moreover, a recent study reported equivalent symptom improvement when compared with an exposure-based therapy for children.145 Loving-kindness meditation has also emerged as a promising approach, with increases in self-compassion as a putative driver of symptom improvement.147
Mindfulness-based exposure therapy for PTSD
King and colleagues35,36 recently presented a novel approach to mindfulness-based treatment for PTSD. Specifically, they developed a 16-week MBET that incorporates mindfulness training as in MBCT and nontrauma in vivo exposures to avoided situations. The approach consists of 4 modules — including PTSD psychoeducation, mindfulness of the body and in vivo exposure, mindfulness of emotions and in vivo exposure — and self-compassion training. The authors compared MBET with PCGT focused on current life stressors contributing to PTSD. They reported results from a subsample of patients who also participated in an fMRI study,35 and found that although both treatments led to reductions in PTSD symptom severity, only the MBET led to statistically significant reductions. Despite promising initial findings, future work will be necessary to confirm the efficacy of this approach.
Impact of mindfulness approaches on endocrine function
Two studies have investigated the impact of mindfulness-based treatments on endocrine function.135,143 Bergen-Cico and colleagues135 reported significant reductions in cortisol awakening response (CAR) among veterans who completed a brief mindfulness intervention as compared with those receiving TAU. Importantly, CAR reduction was associated with changes in PTSD and depression symptom severity. Conversely, Kim and colleagues143 reported a significant increase in basal cortisol levels among ICU nurses with PTSD taking part in MBX treatment as compared with the control condition. Further, higher cortisol levels were associated with reduced PTSD symptoms in the combined MBX and control samples.143 Critically, these 2 studies used different methodology to measure cortisol, with Kim and colleagues143 measuring cortisol in the early morning a few hours after wakening via phlebotomy and Bergen-Cico and colleagues135 measuring salivary cortisol after participants first awoke to determine the CAR. In addition, although it is well established that PTSD impacts negatively on the regulation of the hypothalamic–pituitary–adrenal (HPA) axis,150,151 there has been substantial variability in reports of the directionality of this association, with many studies reporting lower basal cortisol levels among individuals with PTSD, some reporting high levels of basal cortisol in individuals with PTSD and others concluding that there may be a loss of the normal circadian rhythm of cortisol release among those with PTSD.151 Although the directionality of the association between cortisol levels and PTSD symptomatology is not clear, the studies reviewed here suggest that mindfulness-based approaches may be effective in normalizing cortisol response in individuals with PTSD.135,143 Furthermore, Gallegos and colleagues139 observed reductions in circulating interleukin-6 (IL-6; an inflammatory biomarker) as a function of increased attendance at MBSR treatment sessions among women with a history of interpersonal trauma. These findings are important in light of consistent reports of increased inflammatory biomarkers among individuals with PTSD and given that proinflammatory cytokines, such as IL-6, have been shown to increase depressive and anxiety symptoms.152
Discussion
Mindfulness-based approaches in the treatment of PTSD
On balance, an emerging and rapidly growing literature on mindfulness-based treatment for PTSD shows considerable promise. The studies reviewed here suggest that mindfulness-based treatments are effective in reducing symptoms of PTSD, with medium to large within-group effect sizes.129,131–134,136–138,142,145 Critically, most of these studies reported low dropout rates (0%–29% attrition),129,131–134,137,138,142,144–146 although higher rates were reported by Gallegos and colleagues,139 (43% dropout) who cited reasons such as difficulty with childcare and transportation among a sample of mostly women of low socioeconomic status. Such low drop-out rates suggest high acceptability of mindfulness-based treatments among individuals with PTSD and are important given that recent studies highlight 35%–40% dropout rates among individuals receiving evidence-based treatments for PTSD (e.g., CPT, PE),14–16 with PE having significantly higher dropout rates.16 At present, MBSR is the most evidence-supported approach, with 2 RCTs reporting significantly greater improvements in PTSD and related symptomatology with MBSR than with active comparison therapies among veteran populations137,138 (but see the studies by Kearney and colleagues133 and Possemato and colleagues136). Additionally, several single-arm uncontrolled trials reported significant improvements in PTSD and related symptomatology following MBSR treatment among veterans129,132 and victims of interpersonal or developmental trauma.131,134,139 Importantly, across these studies, treatment gains were largely maintained at follow-up ranging from 1 month to 2.5 years129,130,132,134,138,139 (but see the studies by Kearney and colleagues133 and Niles and colleagues137). Critically, the study by Niles and colleagues,137 which did not report maintained improvement at follow-up, used a telehealth approach, suggesting that more intensive, in-person treatment may be necessary to maintain treatment gains. Additional mindfulness-based treatments have been assessed, including a recent investigation of MBCT modified for PTSD142 and MBET36 in comparison to standard treatment protocols, showing promising results indicating greater efficacy of these approaches over control treatments.36,142 In addition, MRP and meditation–relaxation techniques have been studied among individuals with PTSD.143–146 In those studies, initial evidence shows enhanced efficacy of MRP over TAU146 and comparable efficacy of a meditation–relaxation approach to first-line narrative exposure therapy among children.145 Moreover, emerging evidence indicates that mindfulness-based approaches may target neuroendocrine dysfunction that is characteristic of PTSD by normalizing cortisol levels135,143 and reducing circulating inflammatory cytokines.139
Of the studies reviewed here, most did not report on changes in specific PTSD symptom domains (e.g., intrusions, avoidance, alterations in cognitions and mood, and arousal and reactivity). However, among those that did, significant reductions were noted across symptoms of re-experiencing, avoidance, numbing, and hyperarousal.132,134,142,143 Further work will be necessary to elucidate the mechanisms of action by which mindfulness-based approaches lead to changes in PTSD symptomatology. However, preliminary research has begun to explore this question (Fig. 1). For example, Kimbrough and colleagues134 noted particularly strong reductions in the CAPS avoidance/numbing subscale, whereas King and colleagues142 posited that improvements on the CAPS following MBCT were driven by reductions in the avoidance subscale. These findings support hypotheses that suggest a reduction in avoidance as a mechanism by which mindfulness may reduce PTSD symptom severity through promotion of nonjudgmental acceptance of traumatic memories, thoughts and stimuli in the external and internal environment.27,28 Similarly, significant increases in acceptance, reductions in shame-based cognitions131 and improvements in emotion regulation139 have been reported following MBSR treatment for PTSD. King and colleagues142 reported significant reduction in self-blame cognitions and emotional numbing following MBCT, suggesting that mindfulness may improve acceptance (i.e., nonavoidance) and regulation of emotions and acceptance of trauma-related cognitions, leading in turn to decreased shame, self-blame and emotional dysregulation.131,139,142 These findings are of particular importance given recent models emphasizing the importance of shame and guilt-based cognitions in the development and maintenance of PTSD.41,153 Finally, improvements in facets of mindfulness, namely nonreactivity and acting with awareness, have been associated with reduction in hyperarousal symptoms, suggesting that a greater ability to remain in the present moment and be nonreactive to environmental stimuli is a mechanism of change for this symptom cluster.
Neurobiological evidence for mindfulness-based approaches in the treatment of PTSD
There is considerable overlap between neurobiological models of PTSD and neurobiological findings in the mindfulness literature. Recent research shows that mindfulness-based treatments have the potential to target emotional undermodulation (associated with hyperarousal and intrusion symptoms) and emotional overmodulation (associated with dissociative symptoms).7,60,61,63 Specifically, evidence suggests that mindfulness-based therapies may be effective in increasing activity in prefrontal regions (e.g., mPFC) and reducing activity in limbic regions (e.g., amygdala), and thus may effectively target intrusion and hyperarousal symptoms.72,78 Moreover, increased connectivity between the vlPFC and amygdala has been associated with reduced anxiety symptoms following MBSR treatment71 and may indicate improvements in arousal monitoring that lead to reductions in both hyperarousal and intrusion symptoms as well as dissociative responses to traumatic stimuli.72
Furthermore, evidence indicates that mindfulness fosters appropriate use and integrity of the DMN, SN and CEN, given that different phases of mindfulness practice are associated with distinct use of different networks.102 Indeed, mindfulness-based interventions show promise in restoring activity and functional connectivity within and between the CEN, DMN and SN in individuals with PTSD. Recent work indicates that mindfulness may be effective in increasing resting state functional connectivity and activity within the DMN.108 These findings are particularly important given reduced resting state activation and connectivity of the DMN in individuals with PTSD that is thought to lead to disruptions in self-referential processing.61,92 Additionally, mindfulness may be effective in targeting the hyperactivity in the SN and hyperconnectivity between the DMN and SN seen among individuals with PTSD61,92 by fostering reduced neural responding to emotional cues (i.e., reduced AI activation in response to negative stimuli)67,111 and decreased internetwork connectivity between the DMN and SN.112 These alterations may lead, in turn, to reduced hyperarousal symptoms and restoration of self-referential processing among individuals with PTSD. Critically, future work will need to confirm these hypotheses regarding both the neurocircuitry and triple network models among individuals with PTSD who are receiving treatment via mindfulness-based approaches.
Limitations and future directions
Although the studies reviewed here provide promising initial evidence for the utility of mindfulness-based approaches in reducing symptoms of PTSD among military and other trauma-exposed populations, additional work is needed before these treatments can be considered as potential first-line interventions. Indeed, just 1 study has compared the usefulness of mindfulness-based approaches as a first-line, evidence-based treatment for PTSD,145 and no studies have compared these approaches to CPT or PE; however, as reviewed, mindfulness-based treatments appear to have similar effect sizes (medium to large), suggesting similar efficacy. Moreover, initial findings are promising, with Catani and colleagues145 reporting equivalent symptom reductions following either a meditation–relaxation intervention or narrative exposure therapy among children with symptoms of PTSD.
A further avenue for future research is the use of mindfulness-based treatments as a means of preventing relapse and reducing residual symptoms among those who have completed CPT, PE, or other first-line treatments for PTSD, as has been shown with MBCT in the depression literature.32,154,155 This emerging avenue for the use of mindfulness-based treatments may be crucial given that a substantial proportion of individuals with PTSD retains their diagnosis following first-line psychotherapy12 or has substantial residual symptoms.13 Additional work should also investigate the general utility of MBCT adapted for PTSD, as only 1 study to date has done so.142 Critically, as mentioned earlier, personalized approaches to treatment are emerging as a gold-standard approach where clinicians take into account the specific characteristics of each patient to determine what treatment approaches may best fit their specific constellation of symptoms and needs. Further work will be critical to gaining a better understanding of exactly what participant characteristics predict response to different treatment modalities (e.g., primarily hyperarousal or dissociative symptoms), so that patients can be guided to the treatment approach that would be most effective for them.
Importantly, no work to date has investigated whether dissociative symptoms associated with PTSD can be ameliorated through mindfulness-based interventions despite theoretical models suggesting that mindfulness is opposed to dissociative states and may improve pathological dissociative symptoms (e.g., by improved connectedness to the self and present moment awareness).53,54 This is a crucial avenue to explore, as alternative treatment approaches may be particularly indicated among individuals with PTSD+DS in light of potentially reduced treatment response18,19 and increased disease severity.23
Another crucial area for future research is the use of metta mindfulness or loving-kindness approaches, which have garnered recent interest because of their potential to assist patients with PTSD in emotional and psychological flexibility and to foster compassion and empathy for oneself and others.37,39,40 Preliminary work indicates that this form of meditation is effective in improving symptoms of PTSD and promotes increased self-acceptance, life purpose and decentring among veterans.133,148 Furthermore, research suggests that changes in self-compassion mediated changes in symptoms of PTSD among those who participated in a loving-kindness mediation intervention.147,148 These results are critical given recent conceptualizations of PTSD as a disorder driven by shame, guilt and lack of self-compassion41,42 and findings that reduced self-compassion is associated with worse symptom severity among those with PTSD.156
In addition, future work should be aimed at gaining a better understanding of the neurobiological mechanisms underlying the capacity of mindfulness-based approaches to ameliorate symptoms of PTSD. Particularly, further study of changes in functional connectivity between and within the DMN, SN and CEN following mindfulness interventions in those with PTSD is required.
Finally, a better understanding of the ability of mindfulness-based approaches to target specific symptom dimensions of PTSD (e.g., avoidance, hyperarousal, dissociative symptoms) is needed and will be critical to helping clinicians understand the mechanisms of actions underlying these treatments and what individual patients might benefit most from a mindfulness-based approach.
Conclusion
Existing evidence indicates that mindfulness-based therapies, including MBSR,129,131–134,136–139 MBCT,142 MBET,36 meditation–relaxation143,145 and mantrum repetition144,146 approaches are effective in reducing PTSD symptomatology, with preliminary evidence showing that reductions in avoidance134,143 and improvements in shame-based appraisals131 and self-blame cognitions142 may be key mechanisms underlying treatment efficacy. Furthermore, there is considerable overlap between neurobiological models of PTSD and the neurobiology of mindfulness,72,102,112,115 lending strong support to the potential utility of these treatment approaches. Further work is needed to determine the effectiveness of mindfulness-based approaches in comparison to first-line psychotherapies for PTSD, including PE and CPT. In addition, future studies should aim to investigate alterations in neurobiological activity and functional connectivity in areas associated with the neurocircuitry model of PTSD (e.g., mPFC, amygdala) and within and between ICNs, including the DMN, CEN and SN, in order to improve our understanding of the neurobiological mechanisms underlying mindfulness-mediated alterations in PTSD symptomatology.
Acknowledgements
Support for this work was provided by grants from the Canadian Institutes of Health Research and the Canadian Institutes of Military and Veteran’s Health Research awarded to R. Lanius and M. McKinnon. J. Boyd was supported by a studentship from the Homewood Research Institute, an Ontario Graduate Scholarship, and by a Father Sean O’Sullivan Studentship Award from the Research Institute at St. Joseph’s Healthcare Hamilton.
Footnotes
Competing interests: None declared.
Contributors: All authors designed the review, wrote and reviewed the article, approved the final version to be published and can certify that no other individuals not listed as authors have made substantial contributions to the paper.
References
- 1.Kessler RC. Posttraumatic stress disorder: the burden to the individual and to society. J Clin Psychiatry. 2000;61:4–12. [PubMed] [Google Scholar]
- 2.Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the national comorbidity survey. Arch Gen Psychiatry. 1995;52:1048–60. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 3.Van Ameringen M, Mancini C, Patterson B, et al. Post-traumatic stress disorder in Canada. CNS Neurosci Ther. 2008;14:171–81. doi: 10.1111/j.1755-5949.2008.00049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th Ed. Washington (DC): APA; 2013. [Google Scholar]
- 5.Armour C, Karstoft KI, Richardson JD. The co-occurrence of PTSD and dissociation: differentiating severe PTSD from dissociative-PTSD. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1297–306. doi: 10.1007/s00127-014-0819-y. [DOI] [PubMed] [Google Scholar]
- 6.Bennett DC, Modrowski CA, Kerig PK, et al. Investigating the dissociative subtype of posttraumatic stress disorder in a sample of traumatized detained touth. Psychol Trauma. 2015;7:465–72. doi: 10.1037/tra0000057. [DOI] [PubMed] [Google Scholar]
- 7.Lanius RA, Brand B, Vermetten E, et al. The dissociative subtype of posttraumatic stress disorder: rationale, clinical and neurobiological evidence, and implications. Depress Anxiety. 2012;29:701–8. doi: 10.1002/da.21889. [DOI] [PubMed] [Google Scholar]
- 8.Spiegel D, Lewis-Fernández R, Lanius R, et al. Dissociative disorders in DSM-5. Annu Rev Clin Psychol. 2013;9:299–326. doi: 10.1146/annurev-clinpsy-050212-185531. [DOI] [PubMed] [Google Scholar]
- 9.Wolf EJ, Miller MW, Reardon AF, et al. A latent class analysis of dissociation and posttraumatic stress disorder: evidence for a dissociative subtype. Arch Gen Psychiatry. 2012;69:698–705. doi: 10.1001/archgenpsychiatry.2011.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wolf EJ, Lunney CA, Miller MW, et al. The dissociative subtype of PTSD: a replication and extension. Depress Anxiety. 2012;29:679–88. doi: 10.1002/da.21946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cahill SP, Rothbaum BO, Resick PA, et al. Cognitive-behavioural therapy for adults. In: Foa EB, Keane TM, Friedman MJ, et al., editors. Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress Studies. 2nd ed. New York (NY) and London (UK): The Guilford Press; 2012. pp. 139–222. [Google Scholar]
- 12.Steenkamp MM, Litz BT, Hoge CW, et al. Psychotherapy for military-related PTSD. JAMA. 2015;314:489–500. doi: 10.1001/jama.2015.8370. [DOI] [PubMed] [Google Scholar]
- 13.Bradley R, Greene J, Russ E, et al. A multidimensional meta-analysis of psychotherapy for PTSD. Am J Psychiatry. 2005;162:214–27. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- 14.Schottenbauer MA, Glass CR, Arnkoff DB, et al. Nonresponse and dropout rates in outcome studies on PTSD: review and methodological considerations. Psychiatry. 2008;71:134–68. doi: 10.1521/psyc.2008.71.2.134. [DOI] [PubMed] [Google Scholar]
- 15.Goetter EM, Bui E, Ojserkis RA, et al. A systematic review of dropout from psychotherapy for posttraumatic stress disorder among Iraq and Afghanistan combat veterans. J Trauma Stress. 2015;28:401–9. doi: 10.1002/jts.22038. [DOI] [PubMed] [Google Scholar]
- 16.Kehle-Forbes SM, Meis LA, Spoont M, et al. Treatment initiation and dropout from prolonged exposure and cognitive processing therapy in a VA outpatient clinic. Psychol Trauma. 2015;8:107–14. doi: 10.1037/tra0000065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zayfert C, DeViva JC, Becker CB, et al. Exposure utilization and completion of cognitive behavioral therapy for PTSD in a “real world” clinical practice. J Trauma Stress. 2005;18:637–45. doi: 10.1002/jts.20072. [DOI] [PubMed] [Google Scholar]
- 18.Bae H, Kim D, Park CP. Dissociation predicts treatment response in eye movement desensitization and reprocessing (EMDR) for posttraumatic stress disorder. J Trauma Dissociation. 2016;17:112–30. doi: 10.1080/15299732.2015.1037039. [DOI] [PubMed] [Google Scholar]
- 19.Price M, Kearns M, Houry D, et al. Emergency department predictors of posttraumatic stress reduction for trauma-exposed individuals with and without an early intervention. J Consult Clin Psychol. 2014;82:336–41. doi: 10.1037/a0035537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wolf EJ, Lunney CA, Schnurr PP. The influence of the dissociative subtype of posttraumatic stress disorder on treatment efficacy in female veterans and active duty service members. J Consult Clin Psychol. 2016;84:95–100. doi: 10.1037/ccp0000036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cloitre M, Petkova E, Wang J, et al. An examination of the influence of a sequential treatment on the course and impact of dissociation among women with PTSD related to childhood abuse. Depress Anxiety. 2012;29:709–17. doi: 10.1002/da.21920. [DOI] [PubMed] [Google Scholar]
- 22.Resick PA, Suvak MK, Johnides BD, et al. The impact of dissociation on PTSD treatment with cognitive processing therapy. Depress Anxiety. 2012;29:718–30. doi: 10.1002/da.21938. [DOI] [PubMed] [Google Scholar]
- 23.Stein DJ, Koenen KC, Friedman MJ, et al. Dissociation in posttraumatic stress disorder: evidence from the world mental health surveys. Biol Psychiatry. 2013;73:302–12. doi: 10.1016/j.biopsych.2012.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frost KD, Laska KM, Wampold BE. The evidence for present-centered therapy as a treatment for posttraumatic stress disorder. J Trauma Stress. 2014;27:1–8. doi: 10.1002/jts.21881. [DOI] [PubMed] [Google Scholar]
- 25.Kabat-Zinn J. Mindfulness-based interventions in context: past, present, and future. Clin Psychol Sci Pract. 2003;10:144–56. [Google Scholar]
- 26.Banks K, Newman E, Saleem J. An overview of the research on mindfulness-based interventions for treating symptoms of posttraumatic stress disorder: a systematic review. J Clin Psychol. 2015;71:935–63. doi: 10.1002/jclp.22200. [DOI] [PubMed] [Google Scholar]
- 27.Lang AJ, Strauss JL, Bomyea J, et al. The theoretical and empirical basis for meditation as an intervention for PTSD. Behav Modif. 2012;36:759–86. doi: 10.1177/0145445512441200. [DOI] [PubMed] [Google Scholar]
- 28.Follette V, Palm KM, Pearson AN. Mindfulness and trauma: implications for treatment. J Ration-Emot Cogn-Behav Ther. 2006;24:45–61. [Google Scholar]
- 29.Baer RA. Mindfulness training as a clinical intervention: a conceptual and empirical review. Clin Psychol Sci Pract. 2003;10:125–43. [Google Scholar]
- 30.Kabat-Zinn J. Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. New York (NY): Bantam Dell; 1990. [Google Scholar]
- 31.Kabat-Zinn J, Massion A, Kristeller J, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry. 1992;149:936–43. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- 32.Teasdale JD, Segal SV, Williams JMG, et al. Prevention of relpase/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol. 2000;68:615–23. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- 33.Chiesa A, Serretti A. Mindfulness based cognitive therapy for psychiatric disorders: a systematic review and meta-analysis. Psychiatry Res. 2011;187:441–53. doi: 10.1016/j.psychres.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 34.Fjorback LO, Arendt M, Ornbol E, et al. Mindfulness-based stress reduction and mindfulness-based cognitive therapy: a systematic review of randomized controlled trials. Acta Psychiatr Scand. 2011;124:102–19. doi: 10.1111/j.1600-0447.2011.01704.x. [DOI] [PubMed] [Google Scholar]
- 35.King AP, Block SR, Sripada RK, et al. Altered default mode network (DMN) resting state functional connectivity following a mindfulness-based exposure therapy for posttraumatic stress disorder (PTSD) in combat veterans of Afghanistan and Iraq. Depress Anxiety. 2016;33:289–99. doi: 10.1002/da.22481. [DOI] [PubMed] [Google Scholar]
- 36.King AP, Block SR, Sripada RK, et al. A pilot study of mindfulness-based exposure therapy in OEF/OIF combat veterans with PTSD: altered medial frontal cortex and amygdala responses in social–emotional processing. Front Psychiatry. 2016;7:154. doi: 10.3389/fpsyt.2016.00154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Frewen P, Rogers N, Flodrowski L, et al. Mindfulness and metta-based trauma therapy (MMTT): initial development and proof-of-concept of an internet resource. Mindfulness. 2015;6:1322–34. doi: 10.1007/s12671-015-0402-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thompson RW, Arnkoff DB, Glass CR. Conceptualizing mindfulness and acceptance as components of psychological resilience to trauma. Trauma Violence Abuse. 2011;12:220–35. doi: 10.1177/1524838011416375. [DOI] [PubMed] [Google Scholar]
- 39.Hinton DE, Ojserkis RA, Jalal B, et al. Loving-kindness in the treatment of traumatized refugees and minority groups: a typology of mindfulness and the nodal network model of affect and affect regulation. J Clin Psychol. 2013;69:817–28. doi: 10.1002/jclp.22017. [DOI] [PubMed] [Google Scholar]
- 40.Hofmann SG, Grossman P, Hinton DE. Loving-kindness and compassion meditation: potential for psychological interventions. Clin Psychol Rev. 2011;31:1126–32. doi: 10.1016/j.cpr.2011.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Herman JL. Posttraumatic stress disorder as a shame disorder. In: Dearing RL, Tangney JP, editors. Shame in the therapy hour. Washington (DC): American Psychological Association; 2011. [Google Scholar]
- 42.Lee DA, Scragg P, Turner S. The role of shame and guilt in traumatic events: a clinical model of shame-based and guilt-based PTSD. Br J Med Psychol. 2001;74:451–66. doi: 10.1348/000711201161109. [DOI] [PubMed] [Google Scholar]
- 43.Frewen PA, Dean JA, Lanius RA. Assessment of anhedonia in psychological trauma: development of the Hedonic Deficit and Interference Scale. Eur J Psychotraumatol. 2012;3:8585. doi: 10.3402/ejpt.v3i0.8585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Frewen PA, Dozois DJA, Lanius RA. Assessment of anhedonia in psychological trauma: psychometric and neuroimaging perspectives. Eur J Psychotraumatol. 2012;3:8587. doi: 10.3402/ejpt.v3i0.8587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Etter DW, Gauthier JR, McDade-Montez E, et al. Positive affect, childhood adversity, and psychopathology in psychiatric inpatients. Eur J Psychotraumatol. 2013;4:20771. doi: 10.3402/ejpt.v4i0.20771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Boughner E, Thornley E, Kharlas D, et al. Mindfulness-related traits partially mediate the association between lifetime and childhood trauma exposure and PTSD and dissociative symptoms in a community sample assessed online. Mindfulness. 2016;7:672–9. [Google Scholar]
- 47.Chopko BA, Schwartz RC. The relation between mindfulness and posttraumatic growth: a study of first responders to trauma-inducing incidents. J Ment Health Couns. 2009;31:363–76. [Google Scholar]
- 48.Dahm KA, Meyer EC, Neff KD, et al. Mindfulness, self-comparssion, posttraumatic stress disorder, and functional disability in U.S. Iraq and Afghanistan war veterans. J Trauma Stress. 2015;28:460–4. doi: 10.1002/jts.22045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Glück TM, Tran US, Raninger S, et al. The influence of sense of coherence and mindfulness on PTSD symptoms and posttraumatic cognitions in a sample of elderly Austrian survivors of World War II. Int Psychogeriatr. 2016;28:435–41. doi: 10.1017/S104161021500143X. [DOI] [PubMed] [Google Scholar]
- 50.Nitzan-Assayag Y, Aderka IM, Bernstein A. Dispositional mindfulness in trauma recovery: prospective relations and mediating mechanisms. J Anxiety Disord. 2015;36:25–32. doi: 10.1016/j.janxdis.2015.07.008. [DOI] [PubMed] [Google Scholar]
- 51.Smith BW, Ortiz JA, Steffen LE, et al. Mindfulness is associated with fewer PTSD symptoms, depressive symptoms, physical symptoms, and alcohol problems in urban firefighters. J Consult Clin Psychol. 2011;79:613–7. doi: 10.1037/a0025189. [DOI] [PubMed] [Google Scholar]
- 52.Thompson BL, Waltz J. Mindfulness and experiential avoidance as predictors of posttraumatic stress disorder avoidance symptom severity. J Anxiety Disord. 2010;24:409–15. doi: 10.1016/j.janxdis.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 53.Zerubavel N, Messman-Moore TL. Staying present: incorporating mindfulness into therapy for dissociation. Mindfulness. 2015;6:303–14. [Google Scholar]
- 54.Corrigan FM. Mindfulness, dissociation, EMDR and the anterior cingulate cortex: a hypothesis. Contemp Hypn. 2002;19:8–17. [Google Scholar]
- 55.Michal M, Beutel ME, Jordan J, et al. Depersonalization, mindfulness, and childhood trauma. J Nerv Ment Dis. 2007;195:693–6. doi: 10.1097/NMD.0b013e31811f4492. [DOI] [PubMed] [Google Scholar]
- 56.Baer RA, Smith GT, Hopkins J, et al. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- 57.Walach H, Buchheld N, Buttenmüller V, et al. Measuring mindfulness — the Freiburg Mindfulness Inventory (FMI) Pers Individ Dif. 2006;40:1543–55. [Google Scholar]
- 58.Frewen P, Lanius R. Healing the traumatized self: consciousness, neuroscience, treatment. New York (NY) and London (UK): WW Norton & Company; 2015. [Google Scholar]
- 59.Follette VM, Briere J, Rozelle D, et al., editors. Mindfulness-oriented interventions for trauma: integrating contemplative practices. New York (NY): The Guildford Press; 2015. [Google Scholar]
- 60.Rauch SL, Shin LM, Phelps EA. Neurocircuitry models of posttraumatic stress disorder and extinction: human neuroimaging research — past, present, and future. Biol Psychiatry. 2006;60:376–82. doi: 10.1016/j.biopsych.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 61.Patel R, Spreng RN, Shin LM, et al. Neurocircuitry models of posttraumatic stress disorder and beyond: a meta-analysis of functional neuroimaging studies. Neurosci Biobehav Rev. 2012;36:2130–42. doi: 10.1016/j.neubiorev.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 62.Hayes JP, Hayes SM, Mikedis AM. Quantitative meta-analysis of neural activity in posttraumatic stress disorder. Biol Mood Anxiety Disord. 2012;2:9. doi: 10.1186/2045-5380-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lanius RA, Vermetten E, Loewenstein RJ, et al. Emotion modulation in PTSD: clinical and neurobiological evidence for a dissociative subtype. Am J Psychiatry. 2010;167:640–7. doi: 10.1176/appi.ajp.2009.09081168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Felmingham K, Kemp AH, Williams L, et al. Dissociative responses to conscious and non-conscious fear impact underlying brain function in posttraumatic stress disorder. Psychol Med. 2008;38:1771–80. doi: 10.1017/S0033291708002742. [DOI] [PubMed] [Google Scholar]
- 65.Hopper JW, Frewen PA, van der Kolk BA, et al. Neural correlates of reexperiencing, avoidance, and dissociation in PTSD: symptom dimensions and emotion dysregulation in responses to script-driven trauma imagery. J Trauma Stress. 2007;20:713–25. doi: 10.1002/jts.20284. [DOI] [PubMed] [Google Scholar]
- 66.Lanius RA, Vermetten E, Loewenstein RJ, et al. Emotion modulation in PTSD: clinical and neurobiological evidence for a dissociative subtype. Am J Psychiatry. 2010;167:640–7. doi: 10.1176/appi.ajp.2009.09081168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lutz J, Herwig U, Opialla S, et al. Mindfulness and emotion regulation — an fMRI study. Soc Cogn Affect Neurosci. 2013;9:776–85. doi: 10.1093/scan/nst043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ives-Deliperi VL, Howells F, Stein DJ, et al. The effects of mindfulness-based cognitive therapy in patients with bipolar disorder: a controlled functional MRI investigation. J Affect Disord. 2013;150:1152–7. doi: 10.1016/j.jad.2013.05.074. [DOI] [PubMed] [Google Scholar]
- 69.Desbordes G, Negi LT, Pace TWW, et al. Effects of mindful-attention and compassion meditation training on amygdala response to emotional stimuli in an ordinary, non-meditative state. Front Hum Neurosci. 2012;6:1–15. doi: 10.3389/fnhum.2012.00292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Taylor VA, Grant J, Daneault V, et al. Impact of mindfulness on the neural responses to emotional pictures in experienced and beginner meditators. Neuroimage. 2011;57:1524–33. doi: 10.1016/j.neuroimage.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 71.Hölzel BK, Hoge EA, Greve DN, et al. Neural mechanisms of symptom improvements in generalized anxiety disorder following mindfulness training. NeuroImage Clin. 2013;2:448–58. doi: 10.1016/j.nicl.2013.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tang YY, Hölzel BK, Posner MI. The neuroscience of mindfulness meditation. Nat Rev Neurosci. 2015;16:1–13. doi: 10.1038/nrn3916. [DOI] [PubMed] [Google Scholar]
- 73.Hölzel BK, Ott U, Gard T, et al. Investigation of mindfulness meditation practitioners with voxel-based morphometry. Soc Cogn Affect Neurosci. 2008;3:55–61. doi: 10.1093/scan/nsm038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Santarnecchi E, D’Arista S, Egiziano E, et al. Interaction between neuroanatomical and psychological changes after mindfulness-based training. PLoS ONE. 2014;9:e108359. doi: 10.1371/journal.pone.0108359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lanius RA, Frewen PA, Tursich M, et al. Restoring large-scale brain networks in PTSD and related disorders: a proposal for neuroscientifically-informed treatment interventions. Eur J Psychotraumatol. 2015;6:27313. doi: 10.3402/ejpt.v6.27313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Krystal H. Integration and self-healing: affect, trauma, alexithymia. New York (NY): Routledge; 1988. [Google Scholar]
- 77.Frewen PA, Lanius RA, Dozois DJA, et al. Clinical and neural correlates of alexithymia in posttraumatic stress disorder. J Abnorm Psychol. 2008;117:171–81. doi: 10.1037/0021-843X.117.1.171. [DOI] [PubMed] [Google Scholar]
- 78.Marchand WR. Neural mechanisms of mindfulness and meditation: evidence from neuroimaging studies. World J Radiol. 2014;6:471–9. doi: 10.4329/wjr.v6.i7.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Menon V. Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn Sci. 2011;15:483–506. doi: 10.1016/j.tics.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 80.Greicius MD, Krasnow B, Reiss AL, et al. Functional connectivity in the resting brain: a network analysis of the default mode hypothesis. Proc Natl Acad Sci U S A. 2003;100:253–8. doi: 10.1073/pnas.0135058100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Qin P, Northoff G. How is our self related to midline regions and the default-mode network? Neuroimage. 2011;57:1221–33. doi: 10.1016/j.neuroimage.2011.05.028. [DOI] [PubMed] [Google Scholar]
- 82.Spreng RN, Mar RA, Kim ASN. The common neural basis of autobiographical memory, prospection, navigation, theory of mind, and the default mode: a quantitative meta-analysis. J Cogn Neurosci. 2009;21:489–510. doi: 10.1162/jocn.2008.21029. [DOI] [PubMed] [Google Scholar]
- 83.Menon V, Uddin LQ. Saliency, switching, attention and control: a network model of insula function. Brain Struct Funct. 2010;214:655–67. doi: 10.1007/s00429-010-0262-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Seeley WW, Menon V, Schatzberg AF, et al. Dissociable intrinsic connectivity networks for salience processing and executive control. J Neurosci. 2007;27:2349–56. doi: 10.1523/JNEUROSCI.5587-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dosenbach NUF, Fair DA, Miezin FM, et al. Distinct brain networks for adaptive and stable task control in humans. Proc Natl Acad Sci U S A. 2007;104:11073–8. doi: 10.1073/pnas.0704320104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lovero KL, Simmons AN, Aron JL, et al. Anterior insular cortex anticipates impending stimulus significance. Neuroimage. 2009;45:976–83. doi: 10.1016/j.neuroimage.2008.12.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Seeley WW, Menon V, Schatzberg AF, et al. Dissociable intrinsic connectivity networks for salience processing and executive control. J Neurosci. 2007;27:2349–56. doi: 10.1523/JNEUROSCI.5587-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Habas C, Kamdar N, Nguyen D, et al. Distinct cerebellar contributions to intrinsic connectivity networks. J Neurosci. 2009;29:8586–94. doi: 10.1523/JNEUROSCI.1868-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Koechlin E, Summerfield C. An information theoretical approach to prefrontal executive function. Trends Cogn Sci. 2007;11:229–35. doi: 10.1016/j.tics.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 90.Sheline YI, Barch DM, Price JL, et al. The default mode network and self-referential processes in depression. Proc Natl Acad Sci U S A. 2009;106:1942–7. doi: 10.1073/pnas.0812686106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mason MF, Norton MI, Van Horn JD, et al. Wandering minds: the default mode network and stimulus-independent thought. Science. 2007;315:393–5. doi: 10.1126/science.1131295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Koch SBJ, van Zuiden M, Nawijn L, et al. Aberrant resting-state brain activity in posttraumatic stress disorder: a meta-analysis and systematic review. Depress Anxiety. 2016;33:592–605. doi: 10.1002/da.22478. [DOI] [PubMed] [Google Scholar]
- 93.Lanius RA, Bluhm RL, Coupland NJ, et al. Default mode network connectivity as a predictor of post-traumatic stress disorder symptom severity in acutely traumatized subjects. Acta Psychiatr Scand. 2010;121:33–40. doi: 10.1111/j.1600-0447.2009.01391.x. [DOI] [PubMed] [Google Scholar]
- 94.Sripada R, King AP, Welsh RC, et al. Neural dysregulation in post-traumatic stress disorder: evidence for disrupted equilibrium between salience and default mode brain networks. Psychosom Med. 2012;29:997–1003. doi: 10.1097/PSY.0b013e318273bf33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Rabinak CA, Angstadt M, Welsh RC, et al. Altered amygdala resting-state functional connectivity in post-traumatic stress disorder. Front Psychiatry. 2011;2:1–8. doi: 10.3389/fpsyt.2011.00062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sripada RK, King AP, Garfinkel SN, et al. Altered resting-state amygdala functional connectivity in men with posttraumatic stress disorder. J Psychiatry Neurosci. 2012;37:241–9. doi: 10.1503/jpn.110069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Jin C, Qi R, Yin Y, et al. Abnormalities in whole-brain functional connectivity observed in treatment-naive post-traumatic stress disorder patients following an earthquake. Psychol Med. 2014;44:1927–36. doi: 10.1017/S003329171300250X. [DOI] [PubMed] [Google Scholar]
- 98.Bluhm RL, Williamson PC, Osuch EA, et al. Alterations in default network connectivity in posttraumatic stress disorder related to early-life trauma. J Psychiatry Neurosci. 2009;34:187–94. [PMC free article] [PubMed] [Google Scholar]
- 99.Daniels JK, Mcfarlane AC, Bluhm RL, et al. Switching between executive and default mode networks in posttraumatic stress disorder: alterations in functional connectivity. J Psychiatry Neurosci. 2010;35:258–66. doi: 10.1503/jpn.090175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Cisler JM, Scott Steele J, Smitherman S, et al. Neural processing correlates of assaultive violence exposure and PTSD symptoms during implicit threat processing: a network-level analysis among adolescent girls. Psychiatry Res Neuroimaging. 2013;214:238–46. doi: 10.1016/j.pscychresns.2013.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Rabellino D, Tursich M, Frewen PA, et al. Intrinsic connectivity networks in post-traumatic stress disorder during sub- and supraliminal processing of threat-related stimuli. Acta Psychiatr Scand. 2015;132:365–78. doi: 10.1111/acps.12418. [DOI] [PubMed] [Google Scholar]
- 102.Hasenkamp W, Barsalou LW. Effects of meditation experience on functional connectivity of distributed brain networks. Front Hum Neurosci. 2012;6:38. doi: 10.3389/fnhum.2012.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Simon R, Engström M. The default mode network as a biomarker for monitoring the therapeutic effects of meditation. Front Psychol. 2015;6:776. doi: 10.3389/fpsyg.2015.00776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hölzel BK, Lazar SW, Gard T, et al. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect Psychol Sci. 2011;6:537–59. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- 105.Brewer JA, Worhunsky PD, Gray JR, et al. Meditation experience is associated with differences in default mode network activity and connectivity. Proc Natl Acad Sci U S A. 2011;108:20254–9. doi: 10.1073/pnas.1112029108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Garrison KA, Zeffiro TA, Scheinost D, et al. Meditation leads to reduced default mode network activity beyond an active task. Cogn Affect Behav Neurosci. 2015;15:712–20. doi: 10.3758/s13415-015-0358-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Farb NAS, Segal ZV, Mayberg H, et al. Attending to the present: mindfulness meditation reveals distinct neural modes of self-reference. Soc Cogn Affect Neurosci. 2007;2:313–22. doi: 10.1093/scan/nsm030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Jang JH, Jung WH, Kang DH, et al. Increased default mode network connectivity associated with meditation. Neurosci Lett. 2011;487:358–62. doi: 10.1016/j.neulet.2010.10.056. [DOI] [PubMed] [Google Scholar]
- 109.Farb NAS, Segal ZV, Anderson AK. Mindfulness meditation training alters cortical representations of interoceptive attention. Soc Cogn Affect Neurosci. 2013;8:15–26. doi: 10.1093/scan/nss066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zeidan F, Martucci KT, Kraft RA, et al. Neural correlates of mindfulness meditation-related anxiety relief. Soc Cogn Affect Neurosci. 2013;9:751–9. doi: 10.1093/scan/nst041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Paul NA, Stanton SJ, Greeson JM, et al. Psychological and neural mechanisms of trait mindfulness in reducing depression vulnerability. Soc Cogn Affect Neurosci. 2013;8:56–64. doi: 10.1093/scan/nss070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Doll A, Hölzel BK, Boucard CC, et al. Mindfulness is associated with intrinsic functional connectivity between default mode and salience networks. Front Hum Neurosci. 2015;9:461. doi: 10.3389/fnhum.2015.00461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.McTeague LM, Goodkind MS, Etkin A. Transdiagnostic impairment of cognitive control in mental illness. J Psychiatr Res. 2016;83:37–46. doi: 10.1016/j.jpsychires.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Downar J, Blumberger DM, Daskalakis J. The neural crossroads of psychiatric illness: an emerging target for brain stimulation. Trends Cogn Sci. 2016;20:107–20. doi: 10.1016/j.tics.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 115.Wang X, Xu M, Song Y, et al. The network property of the thalamus in the default mode network is correlated with trait mindfulness. Neuroscience. 2014;278:291–301. doi: 10.1016/j.neuroscience.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 116.Liddell BJ, Brown KJ, Kemp AH, et al. A direct brainstem-amygdala-cortical “alarm” system for subliminal signals of fear. Neuroimage. 2005;24:235–43. doi: 10.1016/j.neuroimage.2004.08.016. [DOI] [PubMed] [Google Scholar]
- 117.Phillips ML, Williams LM, Heining M, et al. Differential neural responses to overt and covert presentations of facial expressions of fear and disgust. Neuroimage. 2004;21:1484–96. doi: 10.1016/j.neuroimage.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 118.Williams LM, Liddell BJ, Kemp AH, et al. Amygdala-prefrontal dissociation of subliminal and supraliminal fear. Hum Brain Mapp. 2006;27:652–61. doi: 10.1002/hbm.20208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Williams LM, Liddell BJ, Rathjen J, et al. Mapping the time course of nonconscious and conscious perception of fear: an integration of central and peripheral measures. Hum Brain Mapp. 2004;21:64–74. doi: 10.1002/hbm.10154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Porges SW. The polyvagal theory: neurophysiological foundations of emotions, attachment, communication, and self-regulation. New York (NY): Norton; 2011. [Google Scholar]
- 121.Porges SW. The polyvagal perspective. Biol Psychol. 2007;74:116–43. doi: 10.1016/j.biopsycho.2006.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Rabellino D, Densmore M, Frewen PA, et al. The innate alarm circuit in post-traumatic stress disorder: conscious and subconscious processing of fear- and trauma-related cues. Psychiatry Res Neuroimaging. 2016;248:142–50. doi: 10.1016/j.pscychresns.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 123.Rabellino D, Densmore M, Frewen PA, et al. Aberrant functional connectivity of the amygdala complexes in PTSD during subconscious processing of trauma-related stimuli. PLoS ONE. 2016;15:e0163097. doi: 10.1371/journal.pone.0163097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Harricharan S, Rabellino D, Frewen P, et al. fMRI functional connectivity of the periaqueductal gray in PTSD and its dissociative subtype. Brain Behav. 2016;6:e00579. doi: 10.1002/brb3.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Steuwe C, Daniels JK, Frewen PA, et al. Effect of direct eye contact in PTSD related to interpersonal trauma: an fMRI study of activation of an innate alarm system. Soc Cogn Affect Neurosci. 2014;9:88–97. doi: 10.1093/scan/nss105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Steuwe C, Daniels JK, Frewen PA, et al. Effect of direct eye contact in women with PTSD related to interpersonal trauma: psycho-physiological interaction analysis of connectivity of an innate alarm system. Psychiatry Res Neuroimaging. 2015;232:162–7. doi: 10.1016/j.pscychresns.2015.02.010. [DOI] [PubMed] [Google Scholar]
- 127.Schauer M, Elbert T. Dissociation following traumatic stress. Zeitschrift für Psychol J Psychol. 2010;218:109–27. [Google Scholar]
- 128.Kozlowska K, Walker P, McLean L, et al. Fear and the defense cascade. Harv Rev Psychiatry. 2015;23:263–87. doi: 10.1097/HRP.0000000000000065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Cole MA, Muir JJ, Gans JJ, et al. Simultaneous treatment of neurocognitive and psychiatric symptoms in veterans with posttraumatic stress disorder and history of mild traumatic brain injury: a pilot study of mindfulness-based stress reduction. Mil Med. 2015;180:956–63. doi: 10.7205/MILMED-D-14-00581. [DOI] [PubMed] [Google Scholar]
- 130.Earley MD, Chesney MA, Frye J, et al. Mindfulness intervention for child abuse survivors: a 2.5-year follow-up. J Clin Psychol. 2014;70:933–41. doi: 10.1002/jclp.22102. [DOI] [PubMed] [Google Scholar]
- 131.Goldsmith RE, Gerhart JI, Chesney SA, et al. Mindfulness-based stress reduction for posttraumatic stress symptoms: building acceptance and decreasing shame. J Evid Based Complementary Altern Med. 2014;19:227–34. doi: 10.1177/2156587214533703. [DOI] [PubMed] [Google Scholar]
- 132.Kearney DJ, McDermott K, Malte C, et al. Association of participation in a mindfulness program with measures of PTSD, depression and quality of life in a veteran sample. J Clin Psychol. 2012;68:101–16. doi: 10.1002/jclp.20853. [DOI] [PubMed] [Google Scholar]
- 133.Kearney DJ, Mcdermott K, Malte C, et al. Effects of participation in a mindfulness program for veterans with posttraumatic stress disorder: a randomized controlled pilot study. J Clin Psychol. 2013;69:14–27. doi: 10.1002/jclp.21911. [DOI] [PubMed] [Google Scholar]
- 134.Kimbrough E, Magyari T, Langenberg P, et al. Mindfulness intervention for child abuse survivors. J Clin Psychol. 2010;66:17–33. doi: 10.1002/jclp.20624. [DOI] [PubMed] [Google Scholar]
- 135.Bergen-Cico D, Possemato K, Pigeon W. Reductions in cortisol associated with primary care brief mindfulness program for veterans with PTSD. Med Care. 2014;52:S25–31. doi: 10.1097/MLR.0000000000000224. [DOI] [PubMed] [Google Scholar]
- 136.Possemato K, Bergen-Cico D, Treatman S, et al. A randomized clinical trial of primary care brief mindfulness training for veterans with PTSD. J Clin Psychol. 2016;72:179–93. doi: 10.1002/jclp.22241. [DOI] [PubMed] [Google Scholar]
- 137.Niles BL, Klunk-Gillis J, Ryngala DJ, et al. Comparing mindfulness and psychoeducation treatments for combat-related PTSD using a telehealth approach. Psychol Trauma. 2012;4:538–47. [Google Scholar]
- 138.Polusny MA, Erbes CR, Thuras P, et al. Mindfulness-based stress reduction for posttraumatic stress disorder among veterans a randomized clinical trial. JAMA. 2015;314:456–65. doi: 10.1001/jama.2015.8361. [DOI] [PubMed] [Google Scholar]
- 139.Gallegos AM, Lytle MC, Moynihan JA, et al. Mindfulness-based stress reduction to enhance psychological functioning and improve inflammatory biomarkers in trauma-exposed women: a pilot study. Psychol Trauma. 2015;7:525–32. doi: 10.1037/tra0000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Blake DD, Weathers FW, Nagy LM, et al. The development of a clinician-administered PTSD scale. J Trauma Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- 141.Stephenson KR, Simpson TL, Martinez ME, et al. Changes in mindfulness and posttraumatic stress disorder symptoms among veterans enrolled in mindfulness-based stress reduction. J Clin Psychol. 2017;73:201–17. doi: 10.1002/jclp.22323. [DOI] [PubMed] [Google Scholar]
- 142.King AP, Erickson TM, Giardino ND, et al. A pilot study of group mindfulness-based cognitive therapy (MBCT) for combat veterans with posttraumatic stress disorder (PTSD) Depress Anxiety. 2013;30:638–45. doi: 10.1002/da.22104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Kim SH, Schneider SM, Bevans M, et al. PTSD symptom reduction with mindfulness-based stretching and deep breathing exercise: randomized controlled clinical trial of efficacy. J Clin Endocrinol Metab. 2013;98:2984–92. doi: 10.1210/jc.2012-3742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Rosenthal JZ, Grosswald S, Ross R, et al. Effects of transcendental meditation in veterans of operation enduring freedom and operation Iraqi freedom with posttraumatic stress disorder: a pilot study. Mil Med. 2011;176:626–30. doi: 10.7205/milmed-d-10-00254. [DOI] [PubMed] [Google Scholar]
- 145.Catani C, Kohiladevy M, Ruf M, et al. Treating children traumatized by war and Tsunami: a comparison between exposure therapy and meditation-relaxation in north-east Sri Lanka. BMC Psychiatry. 2009;9:22. doi: 10.1186/1471-244X-9-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Bormann JE, Oman D, Walter KH, et al. Mindful attention increases and mediates psychological outcomes following mantram repetition practice in veterans with posttraumatic stress disorder. Med Care. 2014;52:S13–8. doi: 10.1097/MLR.0000000000000200. [DOI] [PubMed] [Google Scholar]
- 147.Kearney DJ, Malte CA, McManus C, et al. Loving-kindness meditation for posttraumatic stress disorder: a pilot study. J Trauma Stress. 2013;26:426–34. doi: 10.1002/jts.21832. [DOI] [PubMed] [Google Scholar]
- 148.Kearney DJ, Mcmanus C, Malte CA, et al. Loving-kindness meditation and the broaden-and-build theory of positive emotions among veterans with posttraumatic stress disorder. Med Care. 2014;52:S32–8. doi: 10.1097/MLR.0000000000000221. [DOI] [PubMed] [Google Scholar]
- 149.Neuner F, Catani C, Ruf M, et al. Narrative exposure therapy for the treatment of traumatized children and adolescents (KidNET): from neurocognitive theory to field intervention. Child Adolesc Psychiatr Clin N Am. 2008;17:641–64. doi: 10.1016/j.chc.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 150.Yehuda R, Hoge CW, McFarlane AC, et al. Post-traumatic stress disorder. Nat Rev Dis Prim. 2015;1:15057. doi: 10.1038/nrdp.2015.57. [DOI] [PubMed] [Google Scholar]
- 151.Zoladz PR, Diamond DM. Current status on behavioral and biological markers of PTSD: a search for clarity in a conflicting literature. Neurosci Biobehav Rev. 2013;37:860–95. doi: 10.1016/j.neubiorev.2013.03.024. [DOI] [PubMed] [Google Scholar]
- 152.Baker DG, Nievergelt CM, O’Connor DT. Biomarkers of PTSD: neuropeptides and immune signaling. Neuropharmacology. 2012;62:663–73. doi: 10.1016/j.neuropharm.2011.02.027. [DOI] [PubMed] [Google Scholar]
- 153.Nazarov A, Jetley R, McNeely H, et al. Role of morality in the experience of guilt and shame within the armed forces. Acta Psychiatr Scand. 2015;132:4–19. doi: 10.1111/acps.12406. [DOI] [PubMed] [Google Scholar]
- 154.Ma SH, Teasdale JD. Mindfulness-based cognitive therapy for depression: replication and exploration of differential relapse prevention effects. J Consult Clin Psychol. 2004;72:31–40. doi: 10.1037/0022-006X.72.1.31. [DOI] [PubMed] [Google Scholar]
- 155.Piet J, Hougaard E. The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: a systematic review and meta-analysis. Clin Psychol Rev. 2011;31:1032–40. doi: 10.1016/j.cpr.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 156.Hiraoka R, Meyer EC, Kimbrel NA, et al. Self-compassion as a prospective predictor of PTSD symptom severity among trauma-exposed U.S. Iraq and Afghanistan war veterans. J Trauma Stress. 2015;28:127–33. doi: 10.1002/jts.21995. [DOI] [PMC free article] [PubMed] [Google Scholar]