Abstract
Introduction: Despite medical advances, preterm delivery remains a global problem in developed and developing countries. The present study was aimed at conducting a systematic review and meta-analysis of studies on the prevalence of preterm delivery in Iran.
Methods: This study was carried out on studies conducted in Iran by searching databases of SID, Magiran, Irandoc, MEDLIB, Iranmedex, PubMed, Web of science, Google Scholar and Scopus. The search was conducted using advanced search and keywords of preterm delivery and equivalents of it in Mesh and their Farsi’s Synonymous in all articles from 2000-2016.After extracting the data, the data were combined using a random model. Heterogeneity of the studies was assessed using Q test I2 index and the data were analyzed using STATA Ver.11 software.
Results: The total number of samples in this study was 41773. In 19 reviewed articles, the overall prevalence of preterm delivery, based on the random effects model, was estimated to be a total of 10% (95% CI, 9-12). The lowest prevalence of preterm labor was 5.4% in Bam and the highest prevalence was 19.85% in Tehran. There was no significant difference between the prevalence of preterm delivery compared to year of study and sample size.
Conclusion: This study reviewed the findings of previous studies and showed that preterm delivery is a relatively prevalent problem in Iran. Therefore, adopting appropriate interventions in many cases including life skills training, self-care and increasing pregnancy care to reduce these consequences and their following complications in high risk patients seem necessary.
Keywords: Prevalence, Preterm birth, Meta- analysis, Iran
Introduction
Premature birth as the main factor of infants’ mortality and determining adverse health effects has urged the World Health Organization to provide a plan of action in different countries.1 Preterm delivery is defined as births less than full 37 weeks or less than 259 days as considered from the first day of the last menstrual period. Based on gestational age groups, preterm delivery is classified into extremely preterm (less than 28 weeks), very preterm (28 to 32 weeks) and moderate preterm (32 to 37 weeks).2-4 According to reports, premature birth accounts for 3.1 percent of the global burden of diseases,5 so that it is the cause of 35 percent of the 1.3 million annual deaths of babies in the world.6After pneumonia, it is the second most common cause of death in children under 5 years.6,7 Out of 15 million annual premature births in the world, 1 million ends in the infant's death.6 In addition to increased mortality, the surviving babies suffer long-term effects such as neural dysfunction, increased risk of cerebral palsy, visual and learning impairments, and increased risk of non-communication,8,9and these complications impose a huge burden on families, communities and the health system,6,8 Considering the etiological perspective, 45-50% of the causes of preterm deliveries are idiopathic.10 Preterm delivery history, as an effect of interaction of genetic, epigenetic and environmental factors, is considered a major risk factor for preterm delivery. Also, other influential factors include multiparous women, twining, maternal diseases and infections,11stress, heavy occupations, smoking, alcohol and so on.12,13 According to the World Health Organization, of 135 million births around the world, 14.9 million babies (11.1%) were born preterm and more than 60 percent of these births which is equivalent to 9.1 million (12.8%) occurred in Africa and Asia.14 Also, according to the studies, the rate of preterm delivery varied considerably in different countries and regions of the world and its prevalence is related to low-income countries (11.8%), middle income (11.3%) and high-income countries (9.3%). From 1.2 million premature births reported in high income areas, more than 0.5 million (42%) occurs in the United States.2 Based on the surveys done, the incidence of premature delivery in developed countries varies from 7.6% to 12%.14-16 It seems that premature birth prevalence, especially in developing countries, is affected by several factors, including the methods of determining gestational age, national differences in the process of birth registration, the heterogeneity of definitions used for premature birth and religious practices such as local burial customs.17 Also, given the long-term outcomes of preterm delivery and its effect on public health, addressing this major public health concern seems necessary. Many studies have examined different aspects of this pregnancy related outcome. Given the prevalence cross-sectional studies are considered a fundamental and applied basis for further studies in the field of prevention and treatment programs and since various reports of the prevalence of this phenomenon have been reported in Iran, the present systematic review and meta-analysis study aimed to integrate and provide an accurate prevalence in this regard with the hope that the results of this study opens the door to further investigations in this field.
Materials and methods
This study was a systematic review and meta-analysis on the prevalence of preterm delivery in Iran. The results of this study were based on studies conducted in Iran and the articles published in national and international journals.
Inclusion criteria to the study were observational and cohort study that reported preterm prevalence were considered for this review and data of review articles, case studies, abstracts, posters and letters to the editor, repeated report of results in other articles, Case-control and intervention studies excluded. Reports based on definition, preterm delivery is birth before 37 weeks and mother without any disease included and articles unrelated to the subject of the study and studies done on specific groups (such as mothers with chronic diseases, working mothers, specific age group) were excluded. Articles were assessed based on the inclusion and exclusion criteria and the appropriate papers were selected by the reviewers. The final evaluation of the articles was carried out, using a checklist of recording title, year and place of studies, sampling methods, sample size, type of study, and the prevalence in total.
In this systematic review, databases of Magiran, SID, Iranmedex, MEDLIB, Irandoc, PubMed, Google Scholar, Web of science and Scopus were searched using advanced search strategies with Boolean and Tag in accordance with any scientific database, by title, keyword and abstract. To collect the study data, keywords of preterm delivery and its equivalent in Mesh (“Birth and Premature”,” Premature Births”, “Preterm Birth”, “Birth and Preterm”, “Preterm Births” and IRAN for English language article and their Farsi synonyms used for Farsi articles was used from 2000-2016 (Table 1). Research papers were filtered in three steps. In the first and second steps, titles and abstracts of articles were retrieved and reviewed to exclude irrelevant articles. In the third step, full-text articles of the selected abstracts were retrieved to determine relevant articles. Two independent investigators (NSH and AFK) performed the three steps. Disagreements between reviewers were resolved by consensus.
Table 1. Search strategy utilized for MEDLINE from 2000 to 2016 .
| Batch Search term |
|
#1 preterm delivery in Mesh #2 Birth, Premature, “Births, Premature”, “Premature Births”, “Preterm Birth” , “Birth, Preterm”, “Births, Preterm”, “Preterm Births” #3 Combination #1 and #2:” preterm delivery” OR “Birth AND Premature” AND “Premature Birth” AND “Preterm Birth” AND “Births OR Preterm” #4 Iran[tiab] OR Iran[PL] OR Iran[ad] #5 Combination #3 and #5 (“Preterm delivery” OR (Birth AND Premature) OR (“Premature Births”) OR “Preterm Birth” OR (Birth AND Preterm)) AND (Iran[tiab] OR Iran[PL] OR Iran[ad]) #6 Combination #5 AND 2000:2016[dp] |
Two independent investigators (NSH and AFK) performed a quality assessment of the eligible articles using the Hoy et al., tool,18and probable disagreements between them were resolved by consensus.
After developed data extraction form two independent reviewers (SKH, RP) the following data were extracted from all relevant articles: general information regarding the study (study design, sampling method, number of center, and study scope), data of study participants (gestational age, sample size, and inclusion and exclusion criteria of participants) disagreements between reviewers were resolved by consensus.
The variance of each study was calculated based on the binomial distribution. Studies were combined according to sample size and variance. Due to the heterogeneity of the studies, the random effects model was used to combine the studies. Also, meta- regression was used to assess changes in the prevalence of preterm birth based on years of study and sample size.
To investigate the heterogeneity of the studies, Q test at the 5% confidence level and the I2 test was used based on the Higgins classification. Based on this classification, the I2 value of more than 75% was considered as heterogeneity. The data were analyzed by the STATA software version 11 (Stata Corp, College Station, TX, USA))
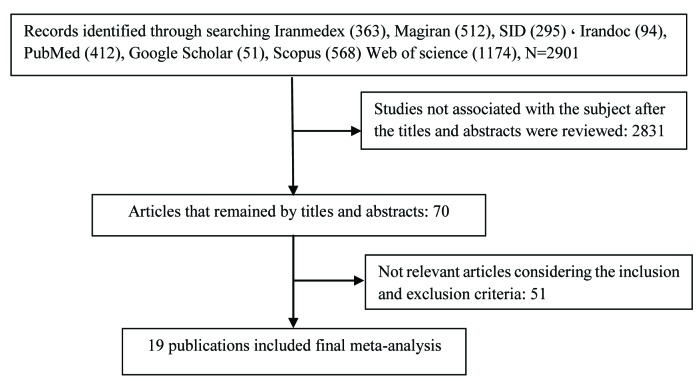
The classification of subjects according to the steps outlined in the procedure is shown in Figure 1. Using the mentioned 6 keywords in combination or alone, 2831 papers were identified and 60 articles were selected by removing unrelated and duplicate studies. After the checking based on the inclusion and exclusion criteria, 51 studies were excluded and finally 19 articles were reviewed.
Figure 1.
Flow diagram showing the different phases involved in searching for relevant publication
Results
In this systematic review and meta-analysis, 14 studies were reviewed, using the cross-sectional method (descriptive, cross-sectional, correlation),19-31 and 5 studies were reviewed using the cohort method.-35 The total number of samples in this study were 41773. Mojibyan et al.,22 had the smallest sample size of 205 in Yazd and Jandaghi et al.,24 had the largest sample size of 10913 in Qom in 2011.
According to the Table 2, the lowest prevalence of low birth weight was 5.4% in Bam (95 CI, 3.9-6.9) and the highest incidence was reported to be 19.85% in Tehran (95 CI, 16-23.7).31-36 The prevalence of less than 10% was reported in most studies,21,24-26,28,31-33 and the prevalence of more than 10% was reported in 9 studies.19,22,23,27,29,34,35,37 The majority of studies (3 studies) were conducted in Tehran, reporting the prevalence of 10 to 19.85 percent.29,34,37 Based on the random effects model, the pooled incidence of preterm labor was 10% in Iran (95%CI, 9-12). The results of Q-test showed significant heterogeneity (Q= 468.49, df=18, P<0.001). Also the results of I2 showed a high heterogeneity between the studies (96.2%).
Table 2. The characteristic of studies were included in the meta-analysis of preterm delivery prevalence in Iran .
| Author | Study location | Type of Study | N (%) | CI 95% |
| Khojaste et al., 201619 | Zahedan | Cross sectional | 227 (19.6) | 14.4-24.8 |
| Akbari et al., 201632 | Esfahan | Cohort | 225 (7) | 3.7-10.3 |
| Gojani et al., 201421 | Rafsanjan | Cross sectional | 5925 (7.5) | 7-14.6 |
| Ajami et al., 201430 | Shahrood | Cross sectional | 4402 (8) | 7.2-8.8 |
| Dolatian et al., 201434 | Tehran | Cohort | 500 (15.5) | 12.3-18.7 |
| Mojibyan et al., 201322 | Yazd | Cross sectional | 205 (13.65) | 9-18.3 |
| Sehhati-Shafaii et al., 201323 | Ardebil | Cross sectional | 3575 (13.6) | 12.5-14.7 |
| Jandaghi et al., 201124 | Ghom | Cross sectional | 10913 (5.6) | 5.2-6 |
| Sohrabi et al., 201125 | Zanjan | Cross sectional | 4528 (7) | 6.3-7.7 |
| Mohsen zadeh et al, 201026 | Khoram abad | Cross sectional | 2179 (8.4) | 7.2-9.6 |
| Tayebi et al., 201036 | Sari | Cohort | 420 (6.2) | 3.9-8.5 |
| Alipure et al., 201033 | Ghom | Cohort | 156 (7.1) | 3.1-11.1 |
| Nematola zadeh et al., 201029 | Tehran | Cross sectional | 512 (10) | 7.4-12.6 |
| Ganji et al., 200927 | Ghom | Cross sectional | 1237 (13.9) | 12-15.8 |
| Shahhosseini et al., 200835 | Sari | Cohort | 262 (10.8) | 7-14.6 |
| Akrami et al., 200637 | Tehran | Cross sectional | 403 (19.85) | 16-23.7 |
| Lotf alizadeh et al., 2005 20 | Yazd | Cross sectional | 1979 (16.4) | 14.8-18 |
| Faramarzi et al., 200528 | Babol | Cross sectional | 3275 (9.6) | 8.6-10.6 |
| Soleymani zadeh et al., 200431 | Bam | Cross sectional | 850 (5.4) | 3.9-6.9 |
Confidence interval
Hence, random effects model was used for the meta-analysis (Figure 1). Figure 1 indicates the prevalence of preterm delivery by year, prevalence and 95% CI, for each of the studies. Based on the meta-regression figures, preterm delivery prevalence decreased by increasing the sample size and year of study, but the difference was not statistically significant (P >0.05) ((Figure 1).,(Figures 2, 3).
Figure 2.
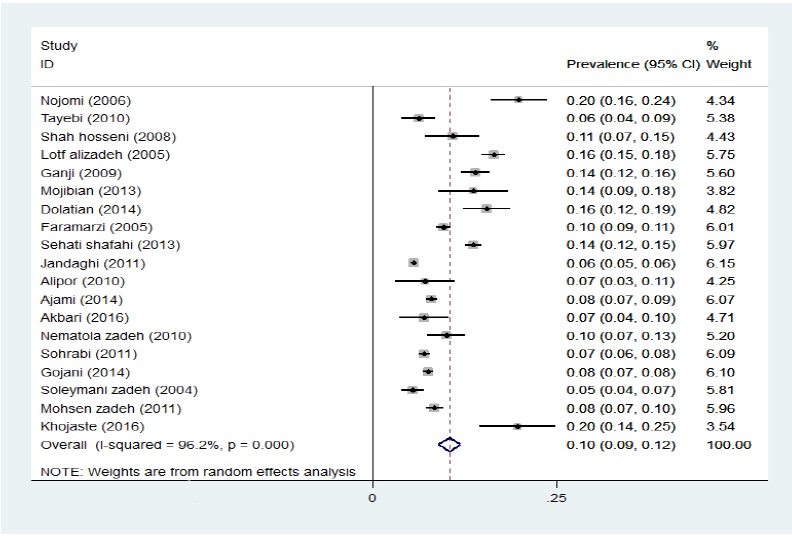
Prevalence ratio preterm labor prevalence based on random effects model; the midpoint of each line segment shows estimating the prevalence rate, and the length of line segment indicates confidence interval of 95% in each study, and diamond mark illustrates the pooled estimate of prevalence rate in all of studies.
Figure3.
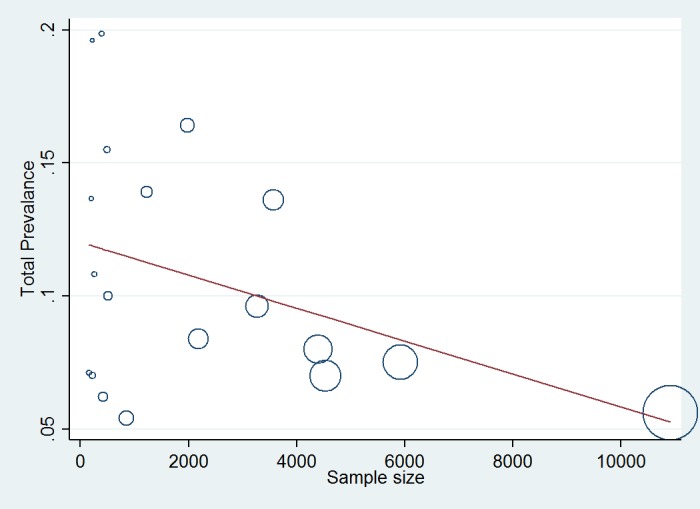
Relationship between preterm delivery prevalence and sample size of studies. The horizontal line represents the slope of the line or beta, and each circle represents a study. The magnitude of each circle indicates the large sample size of the study.
Table 3. Meta-regression coefficient between prevalence of preterm with sample size and year of publication .
| Variable | Meta-regression coefficient | t | SE | P | 95% CI |
| Sample size of study | -9.81×10 -6 | 1.40 | 7.02×10-6 | 0.179 | - 24.5×10-6 –4.89×10-6 |
| Year of publication | -1×10-3 | -0.23 | -5×10-3 | 0.821 | -12.4×10-3 10×10-3 |
Discussion
Despite medical advances in the diagnosis and treatment of diseases, premature births are still a global problem in developed and developing countries.38-40 The present systematic review and meta-analysis study examined the prevalence of preterm delivery in different parts of Iran and after the review, 19 studies that had the inclusion criteria were selected and analyzed. Studies were selected in the period of 2000 to 2016 and the total number of sample consisted of 41773 people. The prevalence of preterm delivery based on studies in different Iranian cities varies from 5.4% (95% CI, 3.9-6.9) to 19.85% (95% CI, 16-23.7).19,21-29,31,34,35,37
World statistics regarding preterm delivery prevalence released by the World Health Organization in 2010 showed that from 135 million live births around the world, 14.9 (11.1 %) were born preterm. The highest percentage of preterm births occur in Africa and Asia which include 9.1 million or 12.8 percent of preterm births per year.14
Available statistics from developed countries like the U.S. and Britain and the Scandinavian countries have shown the growth of this problem in the last twenty years.9 The overall prevalence of preterm deliveries is 9.6% but the distribution of labors is not the same worldwide so that 85% of these cases occur in Asia and Africa.40 The rate of preterm deliveries in the United States seems to be rising faster than that in other developed countries. Also, the prevalence is higher among black infants than whites.40,41In this study, the lowest prevalence was 5.4 percent in the study of Soleimanizadeh et al., in Bam in 2004 and the highest prevalence was 19.85 percent in the study of Akrami et al., in 2006 in Tehran.31,37 The overall prevalence of preterm delivery in Iran was estimated to be 10% (CI% 95, 9-12) and the random effect model based on the I2 test result was used to estimate it, which reflected the high heterogeneity of the studies. In systematic review and meta-analysis study of Vakilian et al., have been conducted to determine the prevalence of preterm birth in Iran, it,s prevalence was 9.2% (95% CI, 7.6-10.7). Chi-square test results based on Q test showed a high heterogeneity and stability (Q=2505.12, P<0.001 and I2= 99.5%). However, in their study the inclusion criteria and definition of the target population for preterm delivery had not been specified.42
Different studies have reported different rates of preterm delivery. The highest incidences were related to low-income countries (11.8%), then came the middle-income countries (11.3%) and the lowest belonged to the high-income countries (9.3 %). Out of 1.2 million premature births reported in high income areas, more than 0.5 million (42%) occur in the United States.2
The prevalence in developed countries have been reported to be approximately 5% and 25% in developing countries.43,44 In reporting the prevalence, certain differences can be seen between the studies which are due to the difference in procedure, different sample size and sampling in different regions with different cultural, social and economic conditions. The results of studies with similar conditions in different regions confirm this point. Among all the country's provinces, information on 16 provinces in relation to the incidence of preterm delivery was available. There have been many studies on preterm delivery in provinces including Tehran (7 studies), Khorasan Razavi (3 studies), Kerman (3 studies), Semnan (2 studies), Isfahan (2 studies), Kohgiluyeh Boyer Ahmad (1 study), West Azarbaijan (1 study), Mazandaran (4 studies), Yazd (2 studies), Ardabil (2 studies), Qom (4 studies), Sistan-Baluchistan (1 study), Lorestan (3 studies), Fars (1 study), Kurdistan (1 study), and Zanjan (1 study). However, there is no available accurate statistics regarding the prevalence of preterm delivery in some other provinces, which stresses the need to do research in this area, using similar methods.
Preterm delivery is the biggest challenge of maternal and perinatal morbidity which leads to complications and mortality in infants. The global estimates suggest that 28 percent of the 4 million annual infants’ deaths worldwide is directly caused by preterm delivery.40 Additionally, preterm delivery is responsible for half of all cases of long-term neurological disorders and high costs of the diagnosis, treatment and care as well as a great challenge in terms of time, energy, economic and equipment for families and employees.43 Complications of preterm delivery are the leading cause of direct and major risk factor for infant death and infant mortality remains a major universal healthcare problem. Given the importance of this issue, one of the main goals of the UN Millennium Development (Goal 4), is to achieve the second cut-third of deaths of children under 5 years between 1990 and 2015 which reflects the significance of this important outcome.44
Achieving this important goal of the Millennium Development Goals depends on complete coverage of evidence-based interventions to prevent preterm delivery and improve survival for premature babies. In the end, it can be concluded that given the high prevalence of this outcome and its importance, this outcome which affects people’s prognosis, survival and quality of life can be prevented by identifying high-risk pregnant mothers and their timely and effective diagnosis and treatment.
Since the purpose of meta-analysis studies was conducting systematic and normative reviews of documents, quantitative summing up of results of each study, combining the results of different studies and providing a general interpretation of the results, presenting an overall conclusion of the studies was one of the benefits of this study. The limitations of this study included 1. Considering only studies in Iran, 2. Lack of access to all articles and unpublished reports, 3. Inability to compare and analyze the results of the studies which was due to 1. Lack of proper, qualified and usable reporting of some articles, 2. Different sampling methods 3. Different size varies, 4. Failure to determine the value of each selected study.
Conclusion
In the present study, despite differences in the study methods, sample size, differences in race, ethnicity and socioeconomic level of samples, etc. which are probably influential in the different reported prevalence in various areas, the results suggest a high prevalence of preterm delivery in the country. Thus, it is essential to carry out further qualitative and quantitative studies on the same terms in all the country by controlling this outcome’s influential factors.
Acknowledgments
The authors are thankful to all researchers whose articles were used in meta-analysis study. Also, the cooperation and help of faculty, library, and computer unit authorities of Ilam University of Medical Sciences in the search for papers is appreciated.
Ethical issues
None to be declared.
Conflict of interest
The authors declare no conflict of interest in this study.
Please cite this paper as: Sharifi N, Khazaeian S, Pakzad R, Fathnezhad kazemi A, Chehreh H. investigating the prevalence of preterm birth in Iranian population: a systematic review and meta-analysis. J Caring Sci 2017; 6 (4): 371-81. doi:10.15171/jcs.2017.035.
References
- 1.Duryea EL, McIntire DD, Leveno KJ. The rate of preterm birth in the United States is affected by the method of gestational age assignment. Am J Obstet Gynecol. 2015;213(2):231 e1–5. doi: 10.1016/j.ajog.2015.04.038. [DOI] [PubMed] [Google Scholar]
- 2.Lee AC, Katz J, Blencowe H, Cousens S, Kozuki N, Vogel JP. et al. National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle-income countries in 2010. Lancet Glob Health. 2013;1(1):e26–36. doi: 10.1016/S2214-109X(13)70006-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Howson CP, Kinney MV, McDougall L, Lawn JE. Born too soon: preterm birth matters. Reprod Health. 2013;10(1):s1. doi: 10.1186/1742-4755-10-S1-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tucker J, McGuire W. Epidemiology of preterm birth. BMJ. 2004;329(7467):675–8. doi: 10.1136/bmj.329.7467.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C. et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–223. doi: 10.1016/S01406736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 6.Howson CP, Kinney MV, McDougall L, Lawn JE. Born too soon: preterm birth matters. Reprod Health. 2013;10(1):S1. doi: 10.1186/1742-4755-10-S1-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE. et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379(9832):2151–61. doi: 10.1016/S0140-6736(12)60560-1. [DOI] [PubMed] [Google Scholar]
- 8.Galinsky R, Polglase GR, Hooper SB, Black MJ, Moss TJM. The consequences of chorioamnionitis: preterm birth and effects on development. J Pregnancy. 2013;(2013):11. doi: 10.1155/2013/412831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, Requejo JH. et al. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ. 2010;88(1):31–8. doi: 10.2471/BLT.08.062554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pennell CE, Jacobsson B, Williams SM, Buus RM, Muglia LJ, Dolan SM. et al. Genetic epidemiologic studies of preterm birth: guidelines for research. Am J Obstet Gynecol. 2007;196(2):107–18. doi: 10.1016/j.ajog.2006.03.109. [DOI] [PubMed] [Google Scholar]
- 11.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371(9606):75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Katz J, Lee AC, Kozuki N, Lawn JE, Cousens S, Blencowe H. et al. Mortality risk in preterm and small-for-gestational-age infants in low-income and middle-income countries: a pooled country analysis. Lancet. 2013;382(9890):417–25. doi: 10.1016/S0140-6736(13)60993-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Plunkett J, Muglia LJ. Genetic contributions to preterm birth: implications from epidemiological and genetic association studies. Ann Med. 2008;40(3):167–95. doi: 10.1080/07853890701806181. [DOI] [PubMed] [Google Scholar]
- 14.Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Narwal R. et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379(9832):2162–72. doi: 10.1016/S0140-6736(12)60820-4. [DOI] [PubMed] [Google Scholar]
- 15.Chang HH, Larson J, Blencowe H, Spong CY, Howson CP, Cairns-Smith S. et al. Preventing preterm births: analysis of trends and potential reductions with interventions in 39 countries with very high human development index. Obstetric Anesthesia Digest. 2014;34(1):16–7. doi: 10.1016/S0140-6736(12)61856-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Abeywardana S, Executive A, Bawden K, Cartwright D, Darlow B, Doran J, et al. Report of the Australian and New Zealand neonatal network. Sydney: ANZNN 2006.
- 17.Graafmans WC, Richardus JH, Macfarlane A, Rebagliato M, Blondel B, Verloove-Vanhorick SP. et al. Comparability of published perinatal mortality rates in Western Europe: the quantitative impact of differences in gestational age and birthweight criteria. BJOG. 2001;108(12):1237–45. doi: 10.1111/j.1471-0528.2001.00291.x. [DOI] [PubMed] [Google Scholar]
- 18.Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C. et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–9. doi: 10.1016/j.jclinepi.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 19.Khojasteh F, Arbabisarjou A, Boryri T, Safarzadeh A, Pourkahkhaei M. The relationship between maternal employment status and pregnancy outcomes. Glob J Health Sci. 2016;8(9):53533. doi: 10.5539/gjhs.v8n9p37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lotf -Alizadeh M, Mohammadzadeh A, Kamandi Sh, Bagheri S. Prevalance and risk factors of preterm labor In Imam Reza hospital 2002-2003. Iranian Journal of Obstetrics, Gynecology and Infertility. Fall-2005;8(2):93–100. (Persian). [Google Scholar]
- 21.Rezaeian M, Goujani R, Sheikh Fathollahi M, Vaziri Nejad R, Manshori A, Razi S. A comparative study on prevalence of preterm birth and low birth weight in Iranians and Afghans races in Rafsanjan Nik-nafs hospital in 2011-2012. Journal of Rafsanjan University of Medical Sciences. 2014;13(1):67–82. (Persian). [Google Scholar]
- 22.Mojibyan M, Karimi M, Bidaki R, Rafiee P, Zare A. Exposure to second-hand smoke during pregnancy and preterm delivery. Int J High Risk Behav Addict. 2013;1(4):149–53. doi: 10.5812/ijhrba.7630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sehhati-Shafaii F, Asadollahy M, Piri R, Naghavi-Behzad M, Farzollahpour F. Prevalence and risk factors of preterm labor in Health Educational Centers of Northwest Iran (2009-2010) Life Science Journal. 2013;10(3):231–6. (Persian). [Google Scholar]
- 24.Jandaghi G, Khalajinia Z, Sadeghi- Moghadam P. Contribution of maternal demographic and medical factors to the risk of prematurity in qom hospitals. Maced J Med Sci. 2011;4(1):60–3. doi: 10.3889/MJMS.1857-5773.2011.0152. [DOI] [Google Scholar]
- 25.Sohrabi D, Ghanbari-Gorkani M. A survey on risk factors and outcomes of women with preterm labor admitted to Valieasr hospital in Zanjan. Journal of Urmia Nursing and Midwifery Faculty. 2011;9(2):84–9. (Persian). [Google Scholar]
- 26.Mohsenzadeh A, Saket S, Karimi A. Prevalence of preterm neonates and risk factors. Iranian Journal of Neonatology. 2011;2(1):38–42. [Google Scholar]
- 27.Ganji T, Einipour Z, Hosseini F. The relationaship of pre-term delivery and stressful life events during pregnancy. Iran Journal of Nursing. 2009;22(57):77–86. [Google Scholar]
- 28.Faramarzi M, Esmaelzadeh S, Mosavi S. Prevalence, maternal complications and birth outcome of physical, sexual and emotional domestic violence during pregnancy. Acta Medica Iranica. 2005;43(2):115–22. [Google Scholar]
- 29.Nematollahzadeh M, Ziaei S, Kazemnejad A. Relationship between body mass index and preterm delivery before and during pregnancy. Zahedan Journal of Research in Medical Sciences. 2011;12(5):89–94. [Google Scholar]
- 30.Ajami M, Nikkhah-shahmirzadi A, Nik-khah A. Prevalence and associated factors of preterm birth in the Shahrood city. Journal of Medical Sciences, Islamic Azad University of Sari. 2014;2(3):43–8. (Presian). [Google Scholar]
- 31.Soleymani-zadeh L, Danesh A, Basari N, Abas-zadeh A, Arab M. survey high-risk pregnancies at Mahdieh maternity hospital in Bam city. Journal of University of Medical Sciences. 2004;6(2):67–73. (Per sian). [Google Scholar]
- 32.Akbari Z, Mansourian M, Kelishadi R. Relationship of the intake of different food groups by pregnant mothers with the birth weight and gestational age: need for public and individual educational programs. J Educ Health Promot. 2015;4:23. doi: 10.4103/2277-9531.154109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alipour Z, Lamyian M, Hajizadeh E. Anxity during pregnancy: a risk factor for neonatal physical outcome? Journal of Nursing and Midwifery Urmia University of Medical Sciences. 2011;9(1) [Google Scholar]
- 34.Dolatian M, Mirabzadeh A, Forouzan AS, Sajjadi H, Alavimajd H, Mahmoodi Z. et al. Relationship between structural and intermediary determinants of health and preterm delivery. J Reprod Infertil. 2014;15(2):78–86. [PMC free article] [PubMed] [Google Scholar]
- 35.Shahhosseini Z, Abedian K, Azimi H. Role of anxiety during pregnancy in preterm delivery. Zanjan University of Medical Sciences. 2008;16(63):85–92. ( Persian). [Google Scholar]
- 36.Tayebi T, Tork Zahrani S, John- Nisar S, Mohammad Por R. Study beneficial relationship adequacy index prenatal care and preterm birth. Journal of Mazandaran University of Medical Sciences. 2010;21(84):87–95. [Google Scholar]
- 37.Akrami MN. Prevalence of physical violence against pregnant women and effects on maternal and birth outcomes. Acta Medica Iranica. 2006;44(2):95–100. [Google Scholar]
- 38.Egan L, Gutierrez AK, Cuevas MP, Lucio JR. Epidemiological profie of premature labor. Ginecol Obstet Mex. 2008;76(9):542–8. [PubMed] [Google Scholar]
- 39.Ghosh JK, Wilhelm MH, Dunkel-Schetter C, Lombardi CA, Ritz BR. Paternal support and preterm birth, and the moderation of effects of chronic stress: a study in Los Angeles County mothers. Arch Womens Ment Health. 2010;13(4):327–38. doi: 10.1007/s00737-009-0135-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Berghella V, Roman A, Daskalakis C, Ness A, Baxter JK. Gestational age at cervical length measurement and incidence of preterm birth. Obstet Gynecol. 2007;110(2 Pt 1):311–7. doi: 10.1097/01.aog.0000270112.05025.1d. [DOI] [PubMed] [Google Scholar]
- 41.Coco L, Giannone TT, Zarbo G. Management of high-risk pregnancy. Minerva Ginecol. 2014;66(4):383–9. [PubMed] [Google Scholar]
- 42.Vakilian K, Ranjbaran M, Khorsandi M, Sharafkhani N, Khodadost M. Prevalence of preterm labor in Iran: a systematic review and meta-analysis. Int J Reprod Biomed (Yazd) 2015;13(12):743–8. [PMC free article] [PubMed] [Google Scholar]
- 43.Johnson TS, Rottier KJ, Luellwitz A, Kirby RS. Maternal prepregnancy body mass index and delivery of a preterm infant in missouri 1998-2000. Public Health Nurs. 2009;26(1):3–13. doi: 10.1111/j.1525-1446.2008.00750.x. [DOI] [PubMed] [Google Scholar]
- 44.Steer P. The epidemiology of preterm labour. BJOG. 2005;112(S1):1–3. doi: 10.1111/j.1471-0528.2005.00575.x. [DOI] [PubMed] [Google Scholar]
- 45.Simmons LE, Rubens CE, Darmstadt GL, Gravett MG. Preventing preterm birth and neonatal mortality: exploring the epidemiology, causes, and interventions. Semin Perinatal. 2010;34(6):408–15. doi: 10.1053/j.semperi.2010.09.005. [DOI] [PubMed] [Google Scholar]