Abstract
We present a case of a 77-year-old male patient with a liver tumour diagnosed as hepatic epithelioid haemangioendothelioma (HEHE), a potentially malignant tumour treated with liver resection. The patient is disease-free 3 years after resection. Imaging features using fludeoxyglucose F 18 positron emission tomography CT and MRI with gadoxic acid as well as histopathological findings are discussed.
Keywords: cancer intervention, hepatic cancer, gastrointestinal surgery
Background
Hepatic epithelioid haemangioendothelioma (HEHE) is a rare neoplasm of vascular origin with malignant potential1–3 in the middle of a scale from haemangioma to angiosarcoma.4 It may occur in any soft tissue of the body, but preferential sites are the liver and limbs.5
Recent papers suggest HEHE is a low-grade angiosarcoma.6–8 Differentiating HEHE from high-grade angiosarcoma is challenging4 on both imaging studies and histopathological analysis, especially when increased mitotic activity is observed. However, new nuclear staining techniques for CAMTA1 should facilitate differentiation of HEHE from haemangiosarcoma and angiosarcoma.9 It is important to differentiate HEHE from angiosarcoma because the latter is an aggressive tumour with poor prognosis.1 10 11
HEHE shows a large spread in age of onset,12 so this diagnosis should be considered even in young patients with a non-typical haemangioma on imaging studies.3 Clinical outcomes vary greatly between patients, but previous studies reported an overall 5-year survival of 48%–55% after resection. The only factor identified to influence prognosis is degree of cellularity; high-cellularity correlates with poor clinical outcome.10
Treatment of HEHE may consist of resection, transarterial chemoembolisation or eventually liver transplantation (LTX), which may be indicated in tumours with diffuse growth pattern. This is opposed to cases of angiosarcoma, which are considered a contraindication for LTX.1 10 13 14
On MRI, HEHE may show multiple lesions, with a nodular or coalescent growth pattern. Signal intensity is generally high, and sometimes heterogeneous on T2-weighted imaging. Three types of enhancement patterns on MRI are known: (1) heterogeneous arterial enhancement with progressive enhancement on portal and delayed phases; (2) ring-like enhancement starting in the arterial phase; (3) mild homogeneous arterial enhancement, without washout.15
Case presentation
A 77-year-old male patient was referred to our centre because of three hepatic lesions, incidentally detected at CT colonography in a population screening study for colon cancer. He had no symptoms and his medical history was unremarkable.
The lesions were evaluated with MRI and fludeoxyglucose F 18 positron emission tomography CT (18-FDG PET-CT) and because one of the lesions was suspicious, a US-guided biopsy of the lesion was performed. Histopathological examination revealed a diagnosis within the spectrum of HEHE and angiosarcoma.
A right hemihepatectomy was performed removing all lesions. A final histopathological diagnosis of HEHE was made. The postoperative period was complicated with a deep venous thrombosis, which resolved under anticoagulation therapy. Three years postoperatively, the patient is free of disease.
Investigations
MRI of the liver with gadoxetic acid was done (figures 1, 2 and 3).
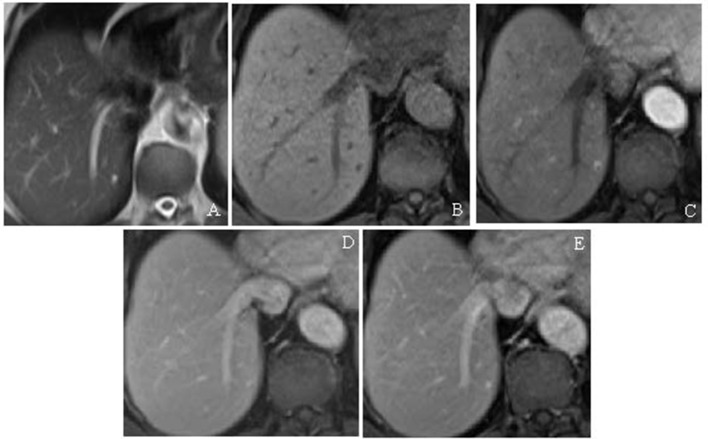
Figure 1.
Small HEHE segment 8. (A) The lesion shows intermediate high signal on T2-weighted half fourier acquisition single shot turbo spin echo (HASTE) series. (B–D) T1-weighted volumetric interpolated breath-hold examination (VIBE) arterial phase, portal venous phase and delayed series, respectively. The lesion shows ring-like enhancement on arterial phase after administration of intravenous contrast, which persisted on delayed series. No central fill-in of the lesion was noted. There was no uptake of contrast during the hepatobiliary phase. HEHE, hepatic epithelioid haemangioendothelioma.
Figure 2.
Haemangioma segment 7. (A) T2-weighted HASTE: the lesion shows very high signal intensity. T1-weighted vibe dynamic series. (B–E) Plain film, arterial phase, portovenous phase and delayed series, respectively. The lesion shows low signal intensity, nodular peripheral enhancement in arterial and venous phases, and complete fill-in on delayed series.
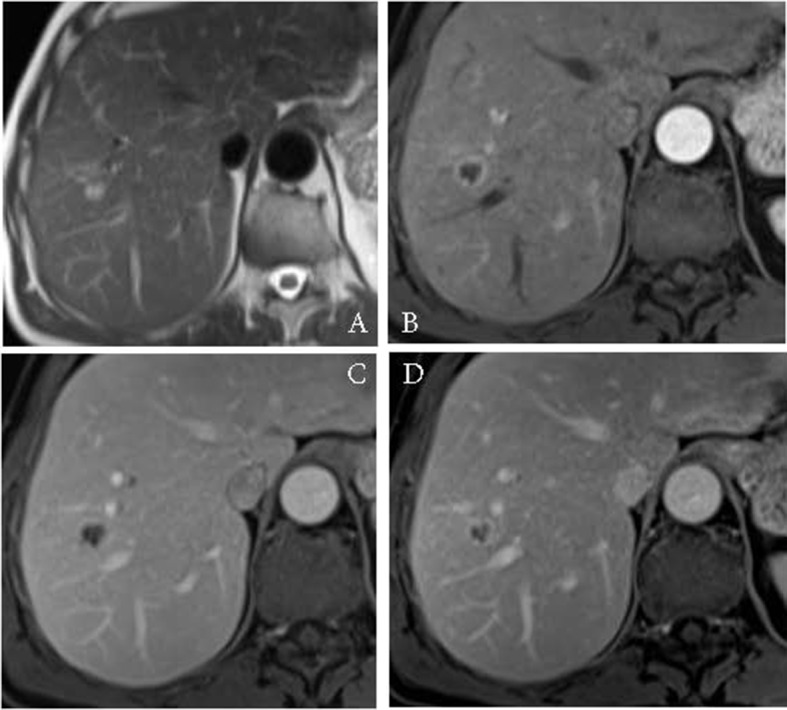
Figure 3.
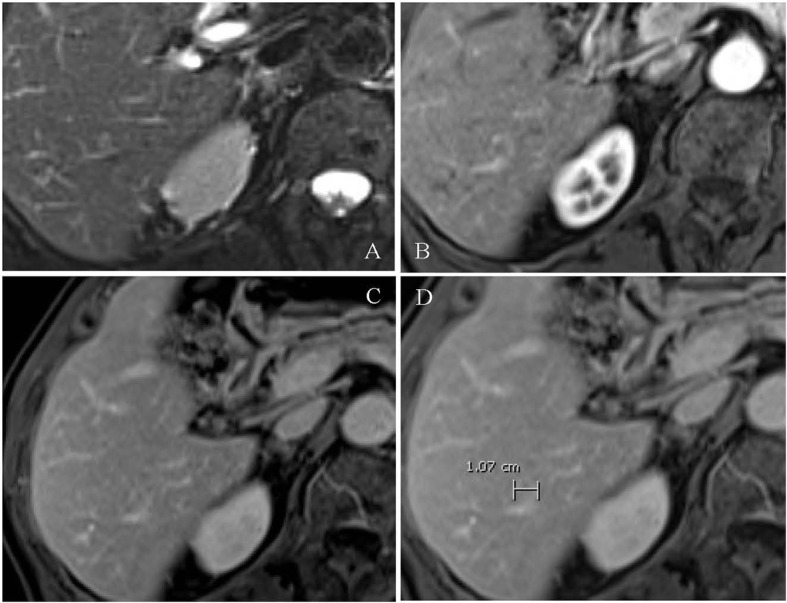
Small HEHE in segment 6. (A) The lesion shows intermediate high-signal intensity on T2-weighted HASTE sequence. (B–D) T1-weighted vibe after intravenous contrast arterial phase, portovenous phase and delayed series, respectively. The lesion shows peripheral ring enhancement. HEHE, hepatic epithelioid haemangioendothelioma.
A focal lesion in segment 8 was found, showing intermediate high signal on T2-weighted series. This lesion also showed no uptake of FDG. This lesion was considered not typical for a cavernous haemangioma but suspicious for a metastasis.
A second lesion was detected in segment 6. This lesion also showed an intermediate signal on T2-weighted series. The lesion showed ring-like arterial enhancement and complete central filling on delayed series. The lesion showed a slight uptake of FDG on PET-CT (figure 4). It was diagnosed as possible haemangioma, with a differential diagnosis of metastasis as well.
Figure 4.
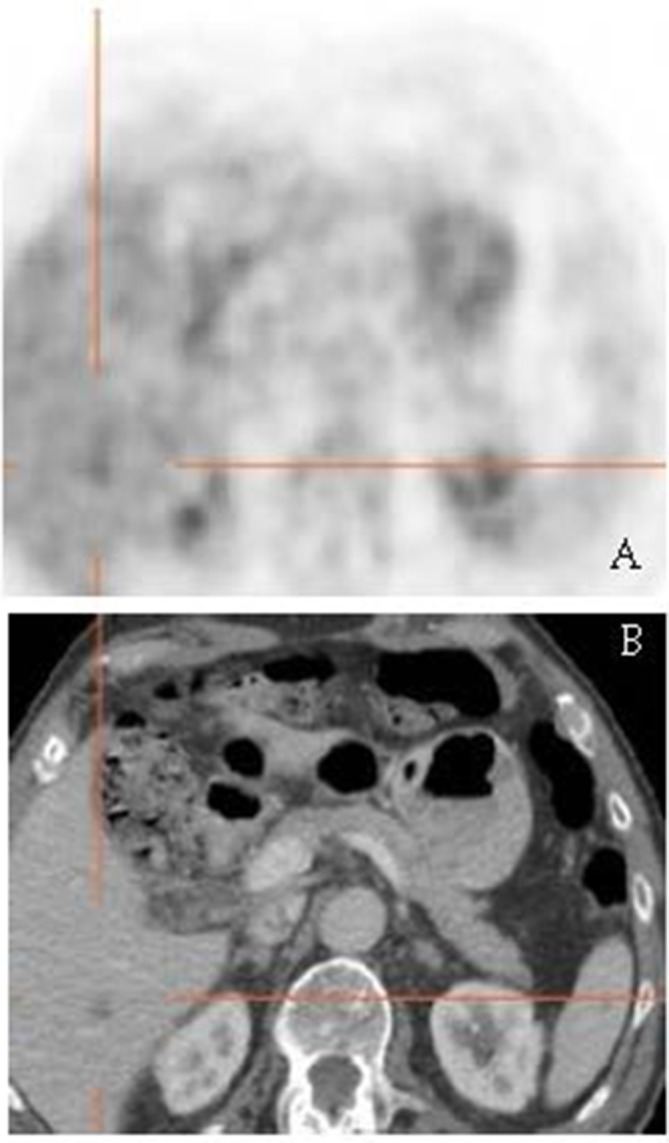
HEHE in segment 6: the lesion shows a slight uptake of FDG. FDG, fludeoxyglucose F; HEHE, hepatic epithelioid haemangioendothelioma.
A third lesion was identified in segment 7 of the liver. It showed typical MR features of a haemangioma; high-signal intensity on T2-weighted series and nodular enhancement with complete fill-in on delayed series.
An FDG PET-CT was made in addition because metastases were suspected. The lesions, however, did not show FDG uptake.
Ultrasound-guided biopsy was performed of the suspicious lesion in segment 8. Histopathological examination characterised the lesion in segment 8 (lesion A at imaging) as atypical vascular proliferation, positive for FLI-1, ERG and CD 34 staining with irregular borders and infiltrating growth pattern into the peritumorous sinusoidal spaces.
Preoperatively, CT volumetry was performed, as well as a hepatobiliary scintigraphy of the liver. Both showed insufficient volume and function of the future liver remnant, for which reason right portal vein embolisation was undertaken before operation.
A right hemihepatectomy was performed for complete removal of the tumour in segment 8. Parenchymal excision was not possible due to the diffuse growth pattern of the tumour in segment 8. The other lesions were removed by this procedure as well. Histopathological examination of the tumour in segment 8 confirmed the diagnosis of HEHE resected with tumour-free margins of 3 cm (figures 5 and 6 show histopathological features). Additionally, the tumour in segment 6 also turned out to be a HEHE and had also been completely removed (figure 4; MRI). The lesion in segment 7 was confirmed to be a haemangioma.
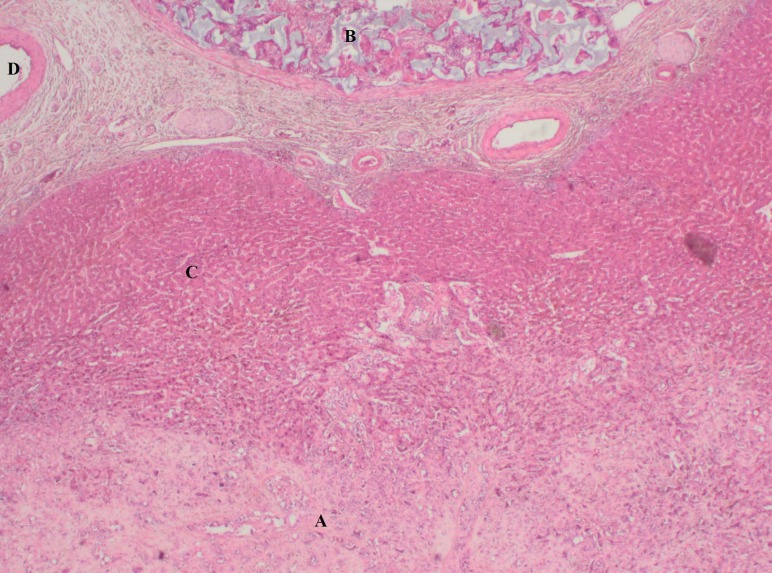
Figure 5.
Image of the surgical resection specimen. Letter A indicates the HEHE in segment 8, showing its diffuse growth pattern and unclearly defined borders. Letter B indicates status after portal vein embolisation. Letter C shows normal liver parenchyma. Letter D shows an artery. HEHE, hepatic epithelioid haemangioendothelioma.
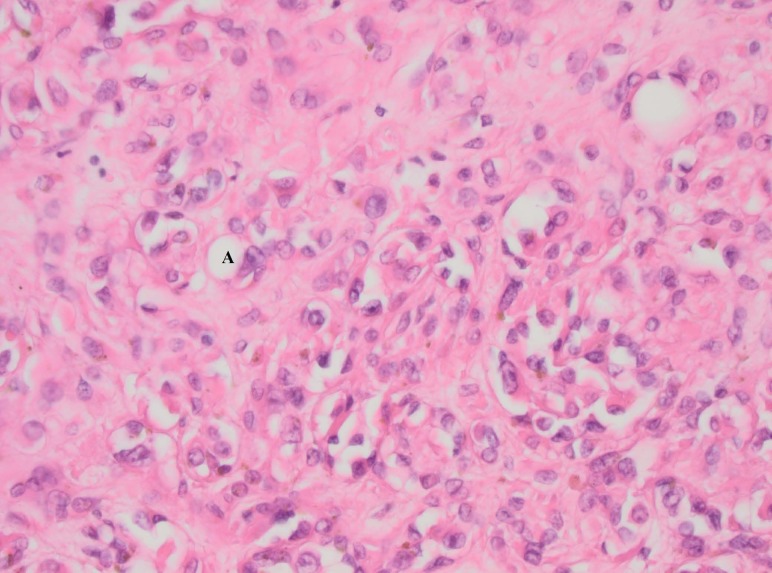
Figure 6.
Detailed picture of the HEHE. The letter A showing an example of vacuolisation which indicates low grade differentiation towards the formation of blood vessels. Also cytonuclear atypia can be observed. HEHE, hepatic epithelioid haemangioendothelioma.
Differential diagnosis
Initially, for both HEHE in segments 8 and 6, the diagnosis haemangioma was considered. However, non-typical findings were intermediate signal on T2-weighted imaging, no ‘light bulb sign’ and ring-like enhancement of the lesion in segment 8.
A diagnosis of HCC was considered unlikely as the patient had no history of liver disease and the imaging features were not compatible with HCC.
Although characteristics of HEHE on PET-CT are relatively unknown, some reports have described diffusely increased uptake.16 The lack of uptake ruled out metastasis, although in this patient a negative PET-CT may have been due to the small size of the lesions.
After biopsy and histopathological investigation, diagnosis shifted towards angiosarcoma or epithelioid haemangioendothelioma, the latter being the correct diagnosis as confirmed on the resection specimen. Both HEHE showed an intermediate cellularity.
Treatment
After portal vein embolisation had increased volume/function of the remnant liver, a right hemihepatectomy was performed with which all lesions including the HEHE were removed completely with a free margin of 3 cm. This is rather unusual because a diffuse growth pattern is often found precluding radical resection and requiring liver transplantation. Postoperative course in the patient was uneventful except for deep venous thrombosis.
Outcome and follow-up
After a period of 3 years, the patient is in good health and is still disease-free on repeated CT scans.
Discussion
Three large series reporting on HEHE, consisting of 32, 137 and 452 patients, respectively, are available.10 17 18 Also a review summarising the data of 434 patients was published in 2006.3 In addition, several case reports and case series have been published, underscoring the problem of establishing the correct diagnosis of this rare tumour.1 19–22
Learning points.
Misdiagnosis of epithelioid haemangioendothelioma based on clinical imaging is not uncommon in the liver. Multiple case reports and studies report a high frequency of atypical findings on imaging and uncertainty of diagnosis.8 10 23–25
When imaging is not conclusive for haemangioma, the diagnosis of HEHE should be considered even in young patients with little or no clinical symptoms.
If several imaging modalities give contradictory results, biopsy and histopathological examination are advised. To determine the appropriate surgical approach, it is important to establish the correct diagnosis beforehand.
HEHE is a diagnosis in the middle of a scale from haemangioma to sarcoma.4 This makes differentiation based on histopathological examination challenging. However, new genetic targets such as CAMTA1 for immunohistochemistry and other methods have shown promising results and may be helpful for the pathologist in the future.9
Footnotes
Contributors: BVvR: writing, information collection, coordination of the project. JV: histopathological examination, writing. SPSSK: interpretation medical Imaging, writing. TMvG: surgical procedure, writing.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Jung DH, Hwang S, Hong SM, et al. Clinicopathological features and prognosis of hepatic epithelioid hemangioendothelioma after liver resection and transplantation. Ann Transplant 2016;21:784–90. 10.12659/AOT.901172 [DOI] [PubMed] [Google Scholar]
- 2.Kobayashi N, Shimamura T, Tokuhisa M, et al. Sorafenib monotherapy in a patient with unresectable hepatic epithelioid hemangioendothelioma. Case Rep Oncol 2016;9:134–7. 10.1159/000443986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehrabi A, Kashfi A, Fonouni H, et al. Primary malignant hepatic epithelioid hemangioendothelioma: a comprehensive review of the literature with emphasis on the surgical therapy. Cancer 2006;107:2108–21. 10.1002/cncr.22225 [DOI] [PubMed] [Google Scholar]
- 4.Antonescu C. Malignant vascular tumors-an update. Mod Pathol 2014;27(Suppl 1):S30–S38. 10.1038/modpathol.2013.176 [DOI] [PubMed] [Google Scholar]
- 5.García-Botella A, Díez-Valladares L, Martín-Antona E, et al. Epithelioid hemangioendothelioma of the liver. J Hepatobiliary Pancreat Surg 2006;13:167–71. 10.1007/s00534-005-1021-0 [DOI] [PubMed] [Google Scholar]
- 6.Lau K, Massad M, Pollak C, et al. Clinical patterns and outcome in epithelioid hemangioendothelioma with or without pulmonary involvement: insights from an internet registry in the study of a rare cancer. Chest 2011;140:1312–8. 10.1378/chest.11-0039 [DOI] [PubMed] [Google Scholar]
- 7.Mehrabi A, Kashfi A, Fonouni H, et al. Primary malignant hepatic epithelioid hemangioendothelioma. Cancer 2006;107:2108–21. 10.1002/cncr.22225 [DOI] [PubMed] [Google Scholar]
- 8.Weiss SW, Enzinger FM. Epithelioid hemangioendothelioma: a vascular tumor often mistaken for a carcinoma. Cancer 1982;50:970–81. [DOI] [PubMed] [Google Scholar]
- 9.Doyle LA, Fletcher CD, Hornick JL. Nuclear expression of CAMTA1 distinguishese epithelioid hemangioendothelioma from histologic mimics. Am J Surg Pathol 2016;40:94–102. 10.1097/PAS.0000000000000511 [DOI] [PubMed] [Google Scholar]
- 10.Makhlouf HR, Ishak KG, Goodman ZD. Epithelioid hemangioendothelioma of the liver. Cancer 1999;85:562–82. [DOI] [PubMed] [Google Scholar]
- 11.Grotz TE, Nagorney D, Donohue J, et al. Hepatic epithelioid haemangioendothelioma: is transplantation the only treatment option? HPB 2010;12:546–53. 10.1111/j.1477-2574.2010.00213.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Remiszewski P, Szczerba E, Kalinowski P, et al. Epithelioid hemangioendothelioma of the liver as a rare indication for liver transplantation. World J Gastroenterol 2014;20:11333–9. 10.3748/wjg.v20.i32.11333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Orlando G, Adam R, Mirza D, et al. Hepatic hemangiosarcoma. Transplantation Journal 2013;95:872–7. 10.1097/TP.0b013e318281b902 [DOI] [PubMed] [Google Scholar]
- 14.Maluf D, Cotterell A, Clark B, et al. Hepatic angiosarcoma and liver transplantation: case report and literature review. Transplant Proc 2005;37:2195–9. 10.1016/j.transproceed.2005.03.060 [DOI] [PubMed] [Google Scholar]
- 15.Zhou L, Cui MY, Xiong J, et al. Spectrum of appearances on CT and MRI of hepatic epithelioid hemangioendothelioma. BMC Gastroenterol 2015;15:69 10.1186/s12876-015-0299-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rest CC, Botton E, Robinet G, et al. FDG PET in epithelioid hemangioendothelioma. Clin Nucl Med 2004;29:789–92. 10.1097/00003072-200412000-00003 [DOI] [PubMed] [Google Scholar]
- 17.Radin DR, Craig JR, Colletti PM, et al. Hepatic epithelioid hemangioendothelioma. Radiology 1988;169:145–8. 10.1148/radiology.169.1.3420251 [DOI] [PubMed] [Google Scholar]
- 18.Zhao XY, Rakhda MI, Habib S, et al. Hepatic epithelioid hemangioendothelioma: a comparison of Western and Chinese methods with respect to diagnosis, treatment and outcome. Oncol Lett 2014;7:977–83. 10.3892/ol.2014.1847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Giardino A, Miller FH, Kalb B, et al. Hepatic epithelioid hemangioendothelioma: a report from three university centers. Radiol Bras 2016;49:288–94. 10.1590/0100-3984.2015.0059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mehrabi A, Hoffmann K, Weiss KH, et al. Long term follow up after resection emphasizes the role of surgery in primary hepatic epithelioid hemangioendothelioma. Ann Med Surg 2016;11:1–4. 10.1016/j.amsu.2016.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khan A, Humayun M, Haider I, et al. Epithelioid haemangioendothelioma (EHE) of the Liver. Journal of the College of Physicians and Surgeons--Pakistan: JCPSP 2016;26:S28–30. [PubMed] [Google Scholar]
- 22.Singh A, Sood N, Puri HK, et al. Primary hepatic epithelioid hemangioendothelioma: diagnostic dilemmas in cytology and histology. J Oncol Pract 2016;12:394–6. 10.1200/JOP.2015.010090 [DOI] [PubMed] [Google Scholar]
- 23.Eckstein RP, Ravich RB. Epithelioid hemangioendothelioma of the liver. Report of two cases histologically mimicking veno-occlusive disease. Pathology 1986;18:459–62. 10.3109/00313028609087569 [DOI] [PubMed] [Google Scholar]
- 24.Hu HJ, Jin YW, Jing QY, et al. Hepatic epithelioid hemangioendothelioma: dilemma and challenges in the preoperative diagnosis. World J Gastroenterol 2016;22:9247 10.3748/wjg.v22.i41.9247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Neofytou K, Chrysochos A, Charalambous N, et al. Hepatic epithelioid hemangioendothelioma and the danger of misdiagnosis: report of a case. Case Rep Oncol Med 2013;2013:1–5. 10.1155/2013/243939 [DOI] [PMC free article] [PubMed] [Google Scholar]