Abstract
We describe a 3-month-old male infant who presented with acute onset fever, irritability and marked tachycardia. ECG was suggestive of atrial tachycardia. He developed erythematous blanchable skin rash on day 2 of illness, which progressed to vesiculobullous lesions over a few days’ time. The child was managed with intravenous adenosine, carefully monitored fluid boluses, oxygen supplementation and close monitoring. Tachycardia improved within 24 hours. Blood for Chikungunya PCR was positive. The child was discharged after 5 days of hospitalisation with bullous lesions evolving into hyperpigmented macules followed by crusts and hypopigmentation by day 10.
Keywords: paediatrics, tropical medicine(infectious Disease), dermatology
Background
Chikungunya fever, caused by Chikungunya virus, is a vector-borne disease transmitted to humans by Aedes mosquito. Although first identified in 1952, historical data suggest epidemics probably linked to Chikungunya disease for at least last three centuries.1 The characteristic clinical manifestations of Chikungunya include acute onset fever associated with joint pain. Other frequent manifestations of Chikungunya include myalgia, headache, skin rash and lymphadenopathy. Apart from adults, children of all ages may be affected. In the presence of classical symptoms, the disease can be diagnosed in adults based on clinical symptoms alone. Children, especially infants, may have varied clinical presentation and may need hospitalisation and further evaluation to rule out other serious infections.2 We describe a 3-month-old infant who presented with acute onset fever with tachycardia and later on developed vesiculobullous rash. This case report highlights the unusual presentation of Chikungunya fever in infants.
Case presentation
A 3-month-old male infant presented to the emergency department with acute onset high grade fever and irritability for 1 day preceded by cough and coryza for 2 days. On examination, child was febrile (temperature 39.3°C) with tachycardia (190 beats per minute) and tachypnoea (62 breaths per minute). Oxygen saturation was 98% on room air. Chest auscultation revealed bilateral expiratory wheeze.
Investigations
Initial blood investigations revealed haemoglobin 8.6 g/dL, total leucocyte count 8200/mm3 (neutrophils 82%, lymphocytes 15% and monocytes 3%) and normal platelet counts. C reactive protein was 4.3 mg/dL. Renal function tests and serum electrolytes were normal. Liver function tests were normal except for mildly increased aspartate aminotransferase levels of 106 U/L. Chest radiograph was normal. ECG was suggestive of atrial tachycardia (figure 1). Echocardiography (ECHO) revealed normal myocardial function and absence of any structural heart disease. Workup for acute onset fever was sent, including relevant cultures, Dengue non-structural protein 1 (NS1) antigen, malarial parasite and Chikungunya PCR.
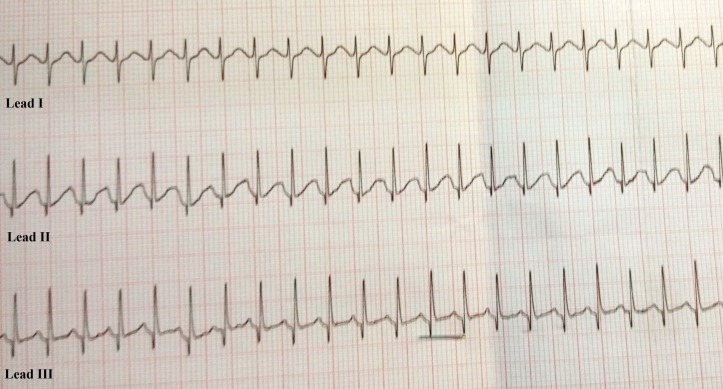
Figure 1.
ECG suggestive of atrial tachycardia.
Treatment
The child was managed with intravenous fluids, oxygen supplementation and close monitoring. The heart rates fluctuated between 210 and 240 beats per minute. There were associated symptoms such as high grade fever, cold extremities and bluish discolouration of extremities. Two doses of intravenous adenosine (first dose at 0.1 mg/kg and second dose at 0.2 mg/kg) were given, which did not lead to any improvement in tachycardia. A clinical possibility of serious bacterial infection was considered and intravenous ceftriaxone was started after sending relevant cultures.
Outcome and follow-up
Immediately after admission, fever increased to 40°C and child developed diffuse erythematous blanchable rash all over the body with acrocyanosis. On the second day of hospitalisation, child developed small fluid-filled vesiculobullous lesions on bilateral lower limbs. Tachycardia resolved in 24 hours with supportive care. Child was managed conservatively with maintenance fluids, oral antipyretics, intravenous ceftriaxone and nebulisation with levosalbutamol. On day 3, Chikungunya PCR was reported positive and antibiotics were discontinued. Sepsis workup was negative. The child was discharged after 5 days of hospitalisation. At discharge, the child had been afebrile for 24 hours and bullous lesions had evolved into hyperpigmented macules. The child was followed in outpatient department twice over 3 weeks, with improved rashes at each visit. Figure 2 shows the clinical evolution of the skin lesions.
Figure 2.
Evolution of skin lesions. (A) Erythematous blanchable rash on day 2. (B) Vesiculobullous lesions on day 3. (C) Hyperpigmented macules on day 5. (D) Crusts leaving hypopigmented scars on day 10.
Discussion
In 2016, New Delhi was grappled with Chikungunya, one of the biggest epidemics in recent times.3 The typical manifestations of Chikungunya in children include acute onset fever, arthralgia, myalgia, skin rash, headache, lymphadenopathy and febrile seizures.1 2 The usual sequence of events include abrupt onset fever accompanied by flushing of skin, which may be followed 3–5 days later with a generalised skin rash and lymphadenopathy. Febrile seizure could be identified in up to one-third of children with Chikungunya.1 Conjunctival congestion, pharyngitis and eyelid swelling may be noted as well. Adults often present with joint pain, usually migratory in nature, which is followed few hours later by high grade fever.
Chikungunya in infancy may present often with non-specific symptoms, including acute onset high grade fever and irritability. Clinically, it is impossible to differentiate it from other serious bacterial infections, including acute pyogenic meningitis. A sepsis workup (including lumbar puncture) is often necessary. However, early identification of Chikungunya fever may help in discontinuing antibiotics early once the sepsis workup is negative. It may also help in counselling the parents regarding the natural history of the illness. Chikungunya in infants and young children may present with cutaneous manifestations that are different from adults.4–7 Even in children, the skin manifestations may vary with age. A recent study from Southern India reported on the cutaneous manifestations in children with Chikungunya.4 The most common lesions were pigmentary (51.9%) followed by vesiculobullous (30.7%) and maculopapular lesions (26.9%). The vesiculobullous lesions were especially limited to infants. The lesions were symmetrical and in the form of flaccid bullae containing clear serous fluid predominantly involving extremities (lower more than upper), buttocks and lower abdomen. The closest differential to such lesions is Staphylococcal scalded skin syndrome, which is a serious illness and may be fatal unless treated urgently. However, the lesions in Chikungunya are usually non-tender and non-toxic looking. The lesions in our case started with flushing of skin on day 2 of illness, which progressed to vesiculobullous lesions limited to lower extremities. The bullous lesions progressed over 3–5 days to scaly lesions, which over a period of 2 weeks resulted in hypopigmented scars (figure 2).
The fever in Chikungunya is typically of abrupt onset and may last for a variable duration. Joint symptoms are often seen in almost all patients with Chikungunya. A recent paediatric series found joint symptoms in almost 99% of patients.8 Infants often present with high grade fever, irritability and fussiness. The irritability in infants may be attributed to the usual constitutional symptoms, including headache, myalgia and arthralgia. The temperature at admission may often exceed 39°C and close to one- third children may develop febrile seizures.1 The extreme tachycardia noticed in some infants may partly be related to fever, incapacitating joint symptoms and myocarditis. The index case had marked tachycardia up to 240 beats per minute. There was associated peripheral cyanosis and hyper fever. The tachycardia in our case was of atrial origin, possibly triggered by Chikungunya infection. The other uncommon manifestations of Chikungunya in children include haemorrhagic manifestations, altered sensorium, meningoencephalitis, retrobulbar neuritis and acute flaccid paralysis.2
This case highlights the unusual presentation of Chikungunya in infants compared with older children and adults. The presentation of Chikungunya may often be confused with serious bacterial infections necessitating sepsis workup. Timely diagnosis and negative sepsis workup may curtail the use of antibiotics. Chikungunya should be considered in the differential diagnosis of acutely febrile infants with irritability and skin manifestations.
Learning points.
The clinical presentation of Chikungunya in children, especially infants, differs from adults.
Chikungunya should be kept as a differential diagnosis in children presenting with acute onset fever, irritability, tachycardia and cutaneous manifestations.
The presentation of Chikungunya may often be confused with serious bacterial infections, thereby necessitating sepsis workup.
Timely diagnosis and negative sepsis workup may curtail the use of antibiotics.
Footnotes
Handling editor: Seema Biswas
Contributors: DR, RK and SW were involved in management of the patient. NC and DR were involved in writing the manuscript. RK was involved in literature search. SW provided overall guidance.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Halstead SB. et al. Chikungunya : Feigin RD, Cherry RD, Demmler-Harrison RD, Kaplan RD, Textbook of Pediatric Infectious Diseases. 7th Edition Philadelphia: Elsevier Saunders, 2014:2241–8. [Google Scholar]
- 2.Sebastian MR, Lodha R, Kabra SK. Chikungunya infection in children. Indian J Pediatr 2009;76:185–9. 10.1007/s12098-009-0049-6 [DOI] [PubMed] [Google Scholar]
- 3.Why Delhi is gripped by chikungunya fears, 2016. (3 Nov 2016) http://www.bbc.com/news/world-asia-india-37358468.
- 4.Seetharam KA, Sridevi K, Vidyasagar P. Cutaneous manifestations of chikungunya fever. Indian Pediatr 2012;49:51–3. 10.1007/s13312-012-0007-7 [DOI] [PubMed] [Google Scholar]
- 5.Pakran J, George M, Riyaz N, et al. Purpuric macules with vesiculobullous lesions: a novel manifestation of Chikungunya. Int J Dermatol 2011;50:61–9. 10.1111/j.1365-4632.2010.04644.x [DOI] [PubMed] [Google Scholar]
- 6.Mohan A, Kiran DH, Manohar IC, et al. Epidemiology, clinical manifestations, and diagnosis of Chikungunya fever: lessons learned from the re-emerging epidemic. Indian J Dermatol 2010;55:54–63. 10.4103/0019-5154.60355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhat RM, Rai Y, Ramesh A, et al. Mucocutaneous manifestations of chikungunya Fever: a study from an epidemic in coastal karnataka. Indian J Dermatol 2011;56:290–4. 10.4103/0019-5154.82483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kumar A, Best C, Benskin G. Epidemiology, clinical and laboratory features and course of Chikungunya among a cohort of children during the first caribbean epidemic. J Trop Pediatr 2016;63 10.1093/tropej/fmw051 [DOI] [PubMed] [Google Scholar]