Abstract
Fascioliasis is a zoonotic disease that can sometimes affect humans. It presents with non-specific signs and symptoms which makes it difficult to establish an early definitive diagnosis. This can be particularly true in non-endemic countries where a high degree of suspicion is needed to make the diagnosis. Another confounding factor is that many of the initial complains and findings are very similar to those of malignancy. We report a case of an otherwise healthy 47 year-old male presenting with abdominal pain, night-time sweating, anorexia, weight loss and loose stools that had several hepatic nodules visible in the abdominal CT scan. Although the initial hypothesis was hepatic malignancy or liver metastasis of unknown primary neoplasm, the workup performed led us to the correct diagnosis. He was treated successfully for hepatic fascioliasis, with a full recovery.
Keywords: Infection (gastroenterology), Liver disease, Foodborne infections, Medical education, Public health
Background
Hepatic fascioliasis is a common infection in ruminants but the cases affecting humans are rare.1–6 The non-specific presentation of this infection makes it difficult to reach a diagnosis based solely on the signs and symptoms. It is usually the imaging abnormalities, namely hepatic nodules, that arouse interest.1–4 7 When this happens, the most common diagnostic hypothesis is that of hepatic malignancy or liver metastasis of unknown primary neoplasm. However, the presence of peripheral eosinophilia should compel us to question this theory. In order to avoid unnecessary exams and invasive procedures when evaluating patients with hepatic nodules and peripheral eosinophilia, one should always collect a complete medical history including epidemiological data such as eating habits, hobbies or place of residency. These can provide important guidance towards the correct diagnosis.
With this case we intend to draw attention to an unlikely cause of hepatic nodules and the importance of collecting a complete medical history thus forgoing invasive procedures to reach the correct diagnosis.
Case presentation
We present the case of a 47 year old man of white ethnicity, residing in the outskirts of a medium-large Portuguese city who was admitted to an Internal Medicine ward because of abdominal pain. He described epigastric and periumbilical colicky pain, radiating to the back, going on for about a month. He also mentioned profuse night-time sweating (without attesting to any fever), overall weakness, anorexia and significant weight loss (30% of total body weight). When questioned, he mentioned frequent loose stools, sometimes even watery dejections, without any blood or mucous during the same period of time. He denied any exanthema or other skin changes and also any respiratory or urinary complaints.
He was a former smoker of 30 units pack-year and maintained sporadic alcohol consumption of about 50g per week. He denied any recent foreign travels. He maintained regular outdoor activities, such as camping and fishing. He was medicated with omeprazole 20 mg once daily since the beginning of this clinical condition because his complaints had originally been interpreted as dyspepsia. He had no family history of malignancies.
In the physical examination, he was haemodynamically stable and had no fever, he was anicteric, slightly dehydrated and had no palpable adenopathies. His heart sounds were normal and his chest was clear. The abdomen was slightly tender on palpation of the right iliac fossa, with no guarding or rebound. There were no identifiable masses or enlarged organs.
The bloodwork revealed eosinophilia, slight cholestasis and elevation of C reactive protein. He had an upper endoscopy and colonoscopy that showed no lesions. The abdominal CT scan showed an enlarged liver and spleen, with nodular, hypodense liver lesions and signs of portal hypertension that was not confirmed on the abdominal ultrasound with Doppler. The MRI scan showed evidences that these nodular images were compatible with infected metastasis of an unknown primary tumour (figure 1). Given this, an eco-guided biopsy of the hepatic nodules was scheduled. However, the interventional radiologist did not perform it since the hepatic lesions seemed smaller and some had even disappeared. We point out that the patient had been medicated with metronidazole 500 mg twice daily since admission to the Internal Medicine ward because of the suspicion of infectious diarrhoea. This had already resulted in improvement of the night-time sweating, anorexia and diarrhoea.
Figure 1.
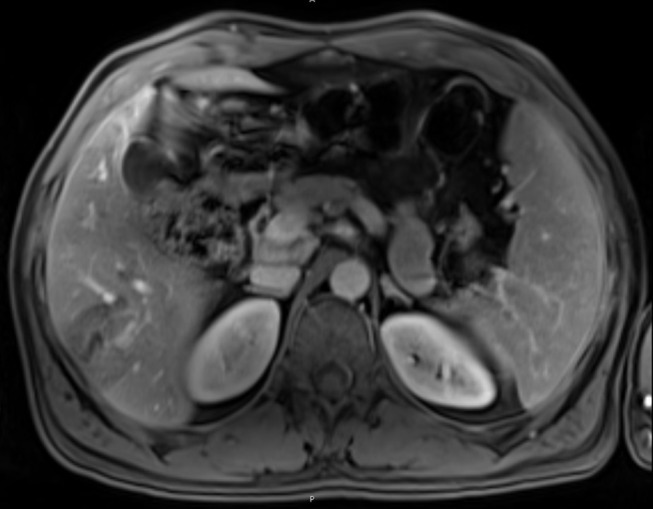
MRI scan showing several hepatic nodules, poorly limited, some of them confluent considered to be infected metastasis.
Meanwhile, the detection of antibodies for Fasciola hepatica (by passive haemagglutination test and western blot analysis) was positive (title 1:1280).
We assumed the infection with F. hepatica was a consequence of eating raw watercress that grew in the land adjacent to where the patient used to go camping.
Investigations
Of all the investigations carried out in this case, we highlight the blood tests with eosinophilia (2 g/L), mild normochromic normocytic anaemia (12.5 g/dL) and cholestasis (alkaline phosphatase 164 U/L and gamma-glutamyl transferase 84 U/L) without hyperbilirubinaemia, thrombocytopaenia, alterations of blood coagulation, renal function or hepatic cytolysis. Also a slightly raised C reactive protein (6.1 mg/dL) with normal sedimentation rate (14 mm/hour). The angiotensin conversion enzyme and the serum protein electrophoresis were normal. The viral hepatitis and HIV serologies were negative as were the tumourous markers (CEA, AFP, CA 19-9 and beta-HCG).
The upper endoscopy did not present any lesions and the total colonoscopy showed only a small intestinal polyp that was excised. The abdominal-pelvic CT scan revealed an enlarged liver and spleen with splenic hilar varices, a large portal vein (15 mm) and hypodense hepatic nodules (30 mm on segment VIII, 45 mm on segment V adjacent to the gallbladder, 43 mm on segment VI). The abdominal ultrasound with Doppler confirmed the existence of a large portal vein but with hepatopetal flow, normal velocities and also normal flow and resistance in hepatic arteries. The MRI scan (figure 1) showed several hepatic nodules, poorly limited, some of them confluent, mainly in segments VIII, IVb, V and VI, hypointense in T1 and hyperintense in T2 with peripheral enhancement in portal phase and also a hepatic hilar adenopathy (11 mm) and another one in the portacaval space (15 mm). The nodules were considered to be infected metastasis.
The eco-guided nodule biopsy was not performed since the nodular lesions had reduced in size and number.
A positive title of 1:1280 for F. hepatica antibodies was detected by passive haemagglutination test and western blot analysis. It was negative for other parasites such as Entamoeba histolytica, Echinococcus, Schistosoma and Leishmania.
Differential diagnosis
Hepatic metastasis of unknown primary tumour
Hepatocellular carcinoma
Schistosomiasis
Fascioliasis
Treatment
The patient was treated with triclabendazole, single dose—10 mg/kg. He had previously fulfilled a 7-day antibiotic course of metronidazole 500 mg twice daily.
Outcome and follow-up
With the treatment prescribed, the complaints of diarrhoea, weight loss and night-time sweating completely resolved. Two months after the diagnosis, the patient repeated the MRI scan (figure 2), which showed improvement of the hepatic lesions.
Figure 2.
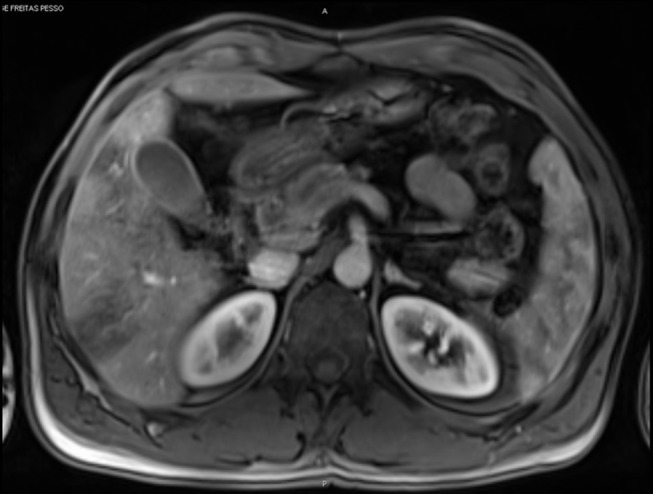
MRI scan showing hepatic nodules smaller in number and size when compared with the previous exam and without peripheral enhancement.
Furthermore, we should report that three family members of our patient were later found to also have been infected with F. hepatica through consumption of infected watercress picked up in the same area. Two of them had digestive complaints (abdominal pain and weight loss) and one was completely asymptomatic. One of the family members, not admitted to our department, was subjected to several diagnostic tests, including two liver biopsies, before the correct diagnosis was made. They were all treated with triclabendazole. The local Public Health Department was notified so they could proceed with disease control.
Discussion
Facioliasis is a common infection in ruminants occurring only rarely in humans.1–6 It usually presents itself in two distinct phases: acute and chronic. The signs and symptoms of acute fascioliasis such as fever, abdominal pain or hepatomegaly are a consequence of the destruction of hepatic tissue due to the migration of parasites through the hepatic parenchyma. Chronic fascioliasis, in which the parasites get wedged into the biliary ducts, is generally subclinical or causes symptoms very similar to those of cholangitis or cholecystitis.2 In endemic regions, such as South America, Nile River Valley and Southeast Asia, fascioliasis can be a recurrent infection, with acute fascioliasis frequently overlapping with chronic disease causing simultaneous clinical manifestations.5 We should clarify that areas of high prevalence of human fascioliasis may not be coincidental with those in which there is a high prevalence of ruminant infection. Besides animal infection, the availability of intermediary hosts and the eating habits of the human population must be considered.5 In Portugal, there are a few cases registered mostly in the northern part of the country,1 2 not where our patient lived.
In human fascioliasis, the manifestations of the disease are extremely variable and unspecific, making it difficult to establish a diagnosis based solely on clinical presentation. For a correct diagnosis, it is essential to include epidemiological data in the medical history, such as eating habits, hobbies and place of residence. It is typically the discovery of hepatic nodules on the imaging exams that draws attention to the disease. In this situation, the first diagnostic hypotheses considered are hepatic malignancy or liver metastasis of unknown primary neoplasm.1–4 7 These were also our main hypotheses but the peripheral eosinophilia led us to consider the possibility of parasitic infection thus testing for Fasciola, E. histolytica, Echinococcus, Schistosoma and Leishmania. Another essential piece of information in this case was the patient’s improvement with initial antibiotic treatment with metronidazole. This strengthened the possibility of parasitic infection. Finally, the definitive diagnosis was made through the confirmation of the presence of F. hepatica antibodies. It was not possible to find Fasciola eggs in the faeces of any of the patients. Treatment with triclabendazole resulted in clinical cure and an improvement of the hepatic lesions on MRI.
Considering that this infection is much more frequent in low-income and middle-income countries than in Europe, we needed a high degree of suspicion to reach a correct diagnosis. Thus, when evaluating patients with hepatic nodules it is essential to take a complete medical history, including epidemiological data and ponder all bloodwork findings, such as eosinophilia. This will allow us to consider alternative diagnosis avoiding mistakes, unnecessary invasive procedures and the stigma of neoplastic disease.
Learning points.
In patients presenting with hepatic nodules and peripheral eosinophilia, it is important to consider parasitic infection in the differential diagnosis, especially if the correct epidemiological context is present.
Not ordering the serological tests can delay the correct diagnosis and lead to unnecessary invasive procedures.
Triclabendazole, although commonly used in the treatment of veterinary fascioliasis, is an effective treatment for the human infection.6 7
Footnotes
Contributors: Dr HT was part of the medical team responsible for diagnosing and treating the patient, wrote and reviewed the manuscript. Dr MO-S was part of the medical team responsible for diagnosing and treating the patient, wrote and reviewed the manuscript. Dr FP was head of the team responsible for diagnosing and treating the patient, reviewed the manuscript. Professor LèS participated in the diagnosis of the patient, reviewed the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Calretas S. Seis casos de Fasciola hepatica. Medicina Interna 2003;10:185–92. [Google Scholar]
- 2.Tavares C. Fascioliase hepática. Acta Médica Portuguesa 1997;10:213–6. [PubMed] [Google Scholar]
- 3.Yilmaz B, Köklü S, Gedikoglu G. Hepatic mass caused by Fasciola hepatica: a tricky differential diagnosis. Am J Trop Med Hyg 2013;89:1212–3. doi:10.4269/ajtmh.13-0085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abdul-Hadi S, Contreras R, Tombazzi C, et al. Hepatic fascioliasis: case report and review. Rev Inst Med Trop Sao Paulo 1996;38:69–73. doi:10.1590/S0036-46651996000100013 [DOI] [PubMed] [Google Scholar]
- 5.Mas-Coma MS, Esteban JG, Bargues MD. Epidemiology of human fascioliasis: a review and proposed new classification. Bull World Health Organ 1999;77:340–4. [PMC free article] [PubMed] [Google Scholar]
- 6.O’Neill SM, Fascioliasis DJP. Epidemiology of human fascioliasis: a review and proposed newclassification. Philadelphia, PA: Lippincott Williams & Wilkins, 2003. [Google Scholar]
- 7.Lin D, Wang X, Wang Z, et al. Diagnosis and management of hepatic fascioliasis mimicking intrahepatic cholangiocarcinoma: a case report. Int J Clin Exp Med 2017;10:1385–92. [Google Scholar]


