Abstract
We present an unusual and rare complication caused by gastric band erosion into the stomach after band placement 15 years ago. The complication was only picked up after the band had subsequently migrated from the stomach at the site of erosion, to the distal ileum causing acute small bowel obstruction and focal perforation requiring emergency laparotomy.
Abdominal pain in patients with gastric band should always be treated as serious until proven otherwise.
Keywords: General surgery, Gastrointestinal surgery
Background
There has been a substantial increase in the use of bariatric surgery for weight management in Australia and worldwide over the past 15 years.1 Surgical interventions available for obesity include restrictive, malabsorptive and combination procedures. Laparoscopic adjustable gastric band (LAGB) insertion was a frequently employed restrictive approach in Australia. It was favoured for being minimally invasive, effective and reversible.
However, high complication rates resulted in a marked decline in LAGB insertion from 42.3% to 17.8% between 2008 to 2011 in a worldwide survey including over 340 000 bariatric procedures.2 Almost 40% of patients experience major complications, 22% report minor complications and almost 50% require reoperation. The type of complications and incidence rate associated with the LAGB include pouch erosion (11%), band erosions (28%), band infections (1%), incisional hernias (5%), port tubing disconnections (20%) and port infections (2%).3
LAGB has also been shown to be unable to provide long-term solution for obesity. A recent French publication looked at 53 000 patients over 7 years revealed an annual band removal rate of 6% with more than two-thirds of patients requiring revisional surgery after removal.4
Case presentation
A 43-year-old female with a body mass index (BMI) 45 had LAGB performed in 2001 for morbid obesity. The model of gastric band used was not disclosed. She maintained a good weight loss profile with a BMI reduction to 31 requiring only a single band adjustment in 2009. Her medical history included previous abdominoplasty and bilateral breast reduction.
She had a 2-week history of progressively increasing colicky abdominal pain and presented to a local emergency department where she was assessed and discharged with a diagnosis of gastroenteritis. Her symptoms worsened with associated nausea, vomiting, abdominal distension and obstipation for 2 days prior to presentation to our institution.
On admission, she was haemodynamically stable and abdominal examination revealed generalised abdominal tenderness with no peritonism. Her renal function was normal. Her white cell count (WCC) and C-reactive protein (CRP) were 25x10^9/L and 66mg/L, respectively, with a serum lactate that was 1.0mmol/L. The patient was commenced on intravenous fluids and a nasogastric tube.
Investigations
Radiological finding
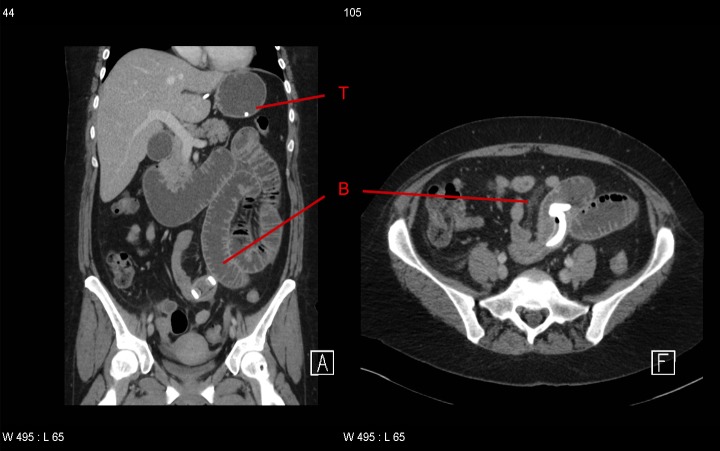
Chest X-ray
A frontal chest X-ray demonstrated the disconnected gastric band tubing in the epigastrium and the band itself not seen in the expected location (figure 1). There was no evidence of pneumoperitoneum and no dilated loops of bowel in the visualised upper abdomen.
Figure 1.
Chest X-ray on admission.
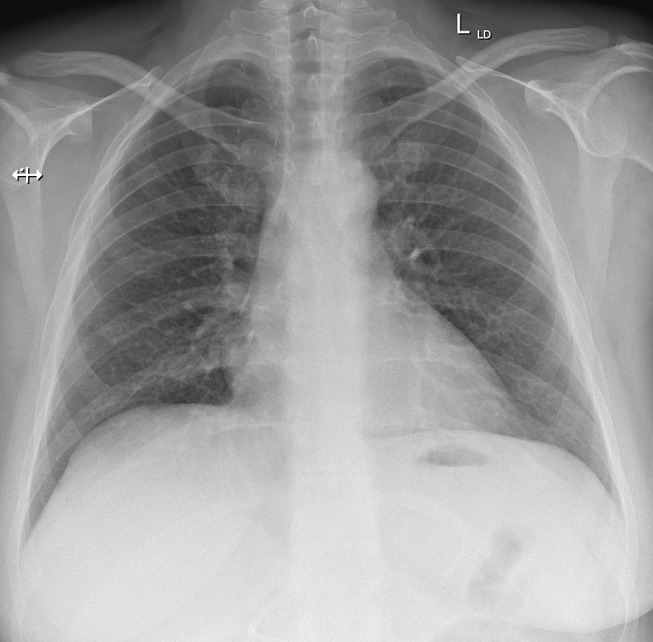
Computed tomography
An abdominopelvic CT was organised with intravenous contrast in portal venous phase which showed marked dilatation of the stomach, duodenum, jejunum and proximal ileal loops which were fluid filled (figure 2). A transition point indicating mechanical obstruction was identified in midline at the level of pelvic brim where there was the dislodged gastric band with attached tubing within the lumen of a loop of ileum. Bowel distal to the point of obstruction was collapsed as expected. The gastric band access port was at its normal position in the anterior subcutaneous tissues and the tip of the fractured connecting tube passed through the gastric wall at the lesser curvature just below the gastro-oesophageal junction and was located within the gastric fundus (figure 2). There was no focal collection adjacent to the stomach at the site of tubing perforation. Only a small amount of free fluid was present in the pelvis and there was no pneumoperitoneum.
Figure 2.
CT scan of abdomen and pelvic on admission; line B indicates laparoscopic adjustable gastric band in lumen of small bowel; line T indicates tip of connecting tube on gastric fundus.
Treatment
Based on the radiological findings, the patient was consented for operation on the next available operating list in daylight hour (8 hours after her initial admission). A laparoscopic approach was not performed as we envisaged the space created by pneumoperitoneum would not provide us with space for a safe procedure in the context of significant small bowel dilatation.
A 6 cm midline laparotomy was then performed with the assistance of a small Alexis O Wound Retractor (Applied Medical Resource, California, USA). During surgery, there was small amount of serous fluid with signs of enteric contamination. The small bowel was thoroughly inspected from duodenojejunal flexure to the ileocaecal valve. The gastric band was identified in the lumen of midileum protruding through the intestinal wall (figure 3). A length of 150 mm of ileum containing gastric band and perforation was resected (figure 4). A stapled side-to-side, functional end-to-end anastomosis was performed using GIA 80 blue (Coviden, Mansfield, Massachusetts, USA). The lap band port was removed along with attached tubing.
Figure 3.

Intraoperative image. Perforation of ileum on view.
Figure 4.
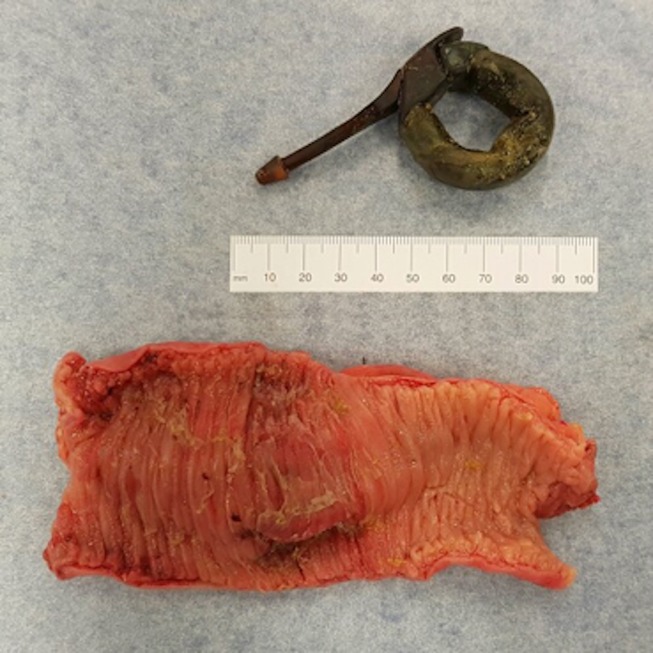
Resected portion of small bowel with gastric band.
Outcome and follow-up
The patient was treated with empirical intravenous antibiotics for 5 days. Her diet was advanced slowly from clear fluid to full diet by postoperative day 4. She had a total 7 days length of stay. She was reviewed a week later in outpatient clinic with complete recovery and tolerating full diet.
Discussion
LAGB although effective, has been shown to have significant complications including pouch enlargement, port site infection, port breakage, band slipping, band erosion and intragastric band migration (IGBM).5 IGBM is rare and rates vary widely across institutions from 0.2% to 11.1%.6 7 These rates may indeed be higher than reported as patients are frequently asymptomatic. Silecchia et al8 showed that 7.5% of patients had IGBM on routine screening with gastroscopy in the years following LAGB. Clinical manifestations of IGBM may include weight gain as a result of loss of band function, port site infection, distal bowel obstruction and rarely bowel perforation.9 10 IGBM is more commonly a late complication; however, studies have documented cases occurring from 1 to 10 years postoperatively.11 12 Endoscopic retrieval of gastric band has been proposed for treatment of asymptomatic patients with IGBM.13 In this patient, however, given the distal location of the band that was causing obstruction and perforation, operative management was required.
This case highlights the presentation and management of a rare, however serious the complication of LAGB. It shows that IGM of LAGB can result in bowel obstruction and perforation over a decade after initial band placement procedure, without any obvious preceding symptoms.
The gastric band appeared shrunken and is likely to have been exposed to prolonged acidic gastric environment. The tubing likely to have snapped off due to erosion, and migration of the band is possible due to smaller size of the band.
With the identification of further long-term complications and little further benefit from long-term placement of LAGB; future investigations would benefit from discussing the appropriate timing of removal of LAGB to prevent such occurrences.
Learning points.
Gastric band erosion needs to be considered as a complication of gastric banding.
A simple erect chest X-ray can often reveal band migration, and confirmation with CT scan is often required to locate band position.
Treatment for gastric band erosion is always a permanent removal, as it can lead to serious complication demonstrated in the case presented.
Distal migration of the band after gastric erosion is possible due to the band which can be partially digested due to prolonged exposure to acidic gastric environment.
Footnotes
Contributors: Dr George Hopkins is a Consultant Bariatric Surgeon at the Royal Brisbane Hospital. AA is the intern who has drafted the report. JL is the surgical registrar and main editor. SG is the bariatric surgical fellow for Dr George Hopkins and has provided supervision for the write up. CH is the radiology consultant who has reported on patient's radiological imaging during admission, edited the article and written the radiological/investigation part of the case report.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.AIHW. Weight loss surgery in Australia. Canberra, 2010. [Google Scholar]
- 2.Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg 2013;23:427–36. 10.1007/s11695-012-0864-0 [DOI] [PubMed] [Google Scholar]
- 3.Himpens J, Cadière GB, Bazi M, et al. Long-term outcomes of laparoscopic adjustable gastric banding. Arch Surg 2011;146:802–7. 10.1001/archsurg.2011.45 [DOI] [PubMed] [Google Scholar]
- 4.Lazzati A, De Antonio M, Paolino L, et al. Natural history of adjustable gastric banding: lifespan and revisional rate: a nationwide study on administrative data on 53,000 patients. Ann Surg 2017;265:439–45. 10.1097/SLA.0000000000001879 [DOI] [PubMed] [Google Scholar]
- 5.Eid I, Birch DW, Sharma AM, et al. Complications associated with adjustable gastric banding for morbid obesity: a surgeon's guides. Can J Surg 2011;54:61–6. 10.1503/cjs.015709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chapman AE, Kiroff G, Game P, et al. Laparoscopic adjustable gastric banding in the treatment of obesity: a systematic literature review. Surgery 2004;135:326–51. 10.1016/S0039-6060(03)00392-1 [DOI] [PubMed] [Google Scholar]
- 7.Egberts K, Brown WA, O'Brien PE. Systematic review of erosion after laparoscopic adjustable gastric banding. Obes Surg 2011;21:1272–9. 10.1007/s11695-011-0430-1 [DOI] [PubMed] [Google Scholar]
- 8.Silecchia G, Restuccia A, Elmore U, et al. Laparoscopic adjustable silicone gastric banding: prospective evaluation of intragastric migration of the lap-band. Surg Laparosc Endosc Percutan Tech 2001;11:229–34. [DOI] [PubMed] [Google Scholar]
- 9.Sapalidis K, Liavas L, Panteli N, et al. Intrajejunal migration of adjustable gastric band: a case report. Curr Health Sci J 2013;39:118–20. [PMC free article] [PubMed] [Google Scholar]
- 10.Owers C, Ackroyd R. A study examining the complications associated with gastric banding. Obes Surg 2013;23:56–9. 10.1007/s11695-012-0760-7 [DOI] [PubMed] [Google Scholar]
- 11.Lemaire J, Dewit O, Navez B. Management of a jejunal obstruction caused by the migration of a laparoscopic adjustable gastric banding. A case report. Int J Surg Case Rep 2017;30:6–8. 10.1016/j.ijscr.2016.11.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Di Lorenzo N, Lorenzo M, Furbetta F, et al. Intragastric gastric band migration: erosion: an analysis of multicenter experience on 177 patients. Surg Endosc 2013;27:1151–7. 10.1007/s00464-012-2566-z [DOI] [PubMed] [Google Scholar]
- 13.Regusci L, Groebli Y, Meyer JL, et al. Gastroscopic removal of an adjustable gastric band after partial intragastric migration. Obes Surg 2003;13:281–4. 10.1381/096089203764467216 [DOI] [PubMed] [Google Scholar]