Abstract
A 49-year-old man presented in the emergency department with altered sensorium and renal failure and was placed on a ventilator. Evaluation with MRI of the brain showed enhancing lesion in the occipital lobe. Biochemical tests revealed elevated calcium and parathyroid hormone (PTH) levels. Further evaluation revealed multiple lesions at both lobes of the lungs and nodular lesion in the right inferior pole of the thyroid. Diagnosis of metastatic parathyroid carcinoma was suspected. Patient was stabilised with bisphosphonates and haemodialysis and planned for surgery. Intraoperatively a hard lesion was found in the right inferior parathyroid infiltrating the surrounding structures. En bloc resection was done. General condition of the patient improved and he was weaned from the ventilator. Histopathology confirmed the diagnosis of parathyroid carcinoma. Postoperatively, there was persistent elevation of PTH in spite of a fall in calcium levels indicating functioning brain and pulmonary metastases. Due to extensive metastases, the patient was given palliative cinacalcet and was kept under follow-up.
Keywords: Calcium and bone, Metabolic disorders
BACKGROUND
Primary hyperparathyroidism (PHPT) is usually a disease of asymptomatic or minimally symptomatic presentation in high-income countries. In low-income countries, it is still a disease with a ‘classic’ pentad of symptoms (ie, kidney stones, painful bones, abdominal groans, psychic moans and fatigue overtones). This wide variation in the presentation is due to routine calcium screening, vitamin D sufficiency, early detection and better referral centres in the developed world. Usually, patients with PHPT have non-specific symptoms to start with. However, bone and renal symptoms are demonstrated in at least 50% of the symptomatic individuals. Few patients with PHPT may have an acute presentation with nausea, vomiting, fatigue, muscle weakness, confusion and altered level of consciousness. This may be due to very high calcium levels which may be lethal if left undiagnosed or untreated. This presentation of hypercalcaemic crisis may lead to multiorgan derangement and failure. Hypercalcaemic crisis is a medical and surgical emergency which require appropriate management. Parathyroid cancer is an uncommon cause of PHPT and can cause hypercalcaemic crisis in an accelerated fashion in selected patients. Parathyroid carcinoma do metastasise to adjacent lymph nodes and distant organs. When presented with synchronous or metachronous metastases, the probability of cure is very limited. These metastases may function producing parathormone contributing to the persistence of hypercalcaemia when not surgically removed. We intend to report an uncommon presentation of hypercalcaemic crisis presenting with encephalopathy in a metastatic parathyroid carcinoma.
CASE PRESENTATION
An apparently healthy 49-year-old man presented in the emergency department with progressive deterioration of sensorium which was associated with vomiting and dehydration. History of recent voice change was observed by his relatives. There was no history of trauma, headache, fever, seizure, weakness or involuntary urination. There was no personal or family history of diabetes, hypertension orcoronary artery disease. Patient warranted ventilator support and was intubated in the intensive care unit (ICU).
INVESTIGATIONS
He was investigated in the ICU for the cause of his coma. MRI of the brain revealed a heterogeneously enhancing multiloculated lesion of 31x23×25 mm in the left occipital lobe with mild surrounding oedema and no midline shift suggestive of metastasis as shown in figure 1A. High-resolution CT of the neck and thorax unravelled a nodular lesion of 31x27×24 mm in the region of the inferior pole of the thyroid gland, indenting trachea and multiple round nodular lesions of varying sizes, the largest measuring 16 mm seen in both lobes of the lungs (figure 1B).
Figure 1.
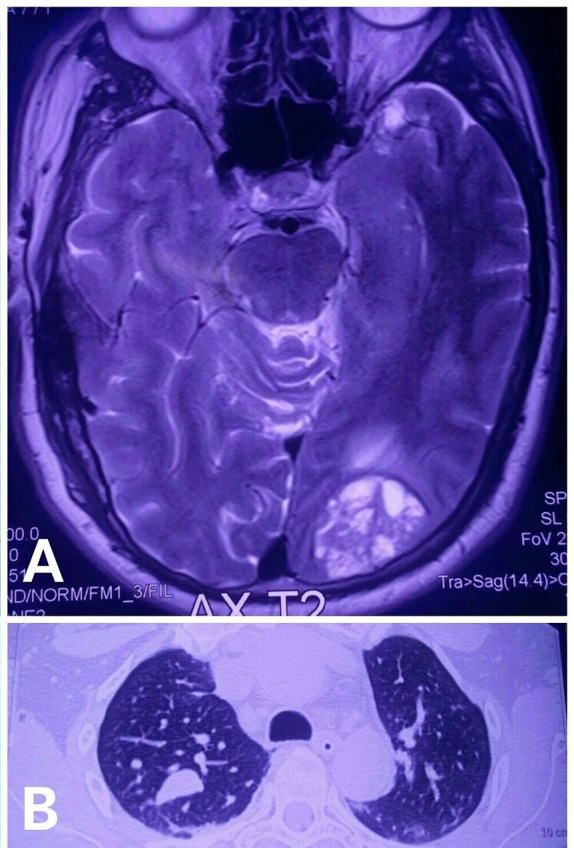
(A) MRI of the brain showing multiloculated hyperintense lesion in the left occipital lobe. (B) High-resolution contrast CT thorax showing multiple nodular lesion at both lobes of the lungs.
Biochemical evaluation revealed a very high serum calcium level of 22.3 mg/dL (normal values 9–11 mg/dL) and low phosphorus level of 2.2 mg/dL. Serum parathormone was markedly elevated to 3560.7 pg/mL (normal values 15–72 pg/mL). Serum 25-hydroxy vitamin D was in the deficient range, 23 ng/mL (>30 ng/mL is normal). Renal parameters were deranged and patient developed acute renal failure. With a high possibility of parathyroid carcinoma with cerebral and pulmonary metastases presenting as hypercalcaemic encephalopathy, patient was scheduled for emergency neck exploration for parathyroidectomy.
TREATMENT
Patient was stabilised initially with hydration, bisphosphonates and haemodialysis prior to surgery. With the above measures, the serum calcium fell to 14.8 mg/dL. Surgical exploration of the neck revealed a hard greyish-white conglomerate mass of size 7.5×4.2×3.8 cm occupying the right lobe of the thyroid in its distal half as in figure 2A. The mass was found infiltrating the strap muscles, with recurrent laryngeal nerve (RLN) on the right side. The tumour was arising from the inferior parathyroid on the right side and found infiltrating the surrounding structures. Few enlarged lymph nodes were found in the right paratracheal area along with the mass. With a very high likelihood of parathyroid carcinoma, en bloc excision of the mass with the right lobe of the thyroid along with the strap muscles and central compartment lymph node dissection (level VI) and RLN was done. Figure 2B shows the neck region after extirpation of the conglomerate mass with the level VI lymph nodes. Lateral neck lymph nodes were not involved. All the other three parathyroids were found to be normal which were preserved in situ. figure 2C,D shows the in vitro specimen of the resected specimen and the cut section of the tumour area which was very hard, gritty with surrounding infiltration. Intraoperative nerve monitoring was not available in our centre and was not used.
Figure 2.
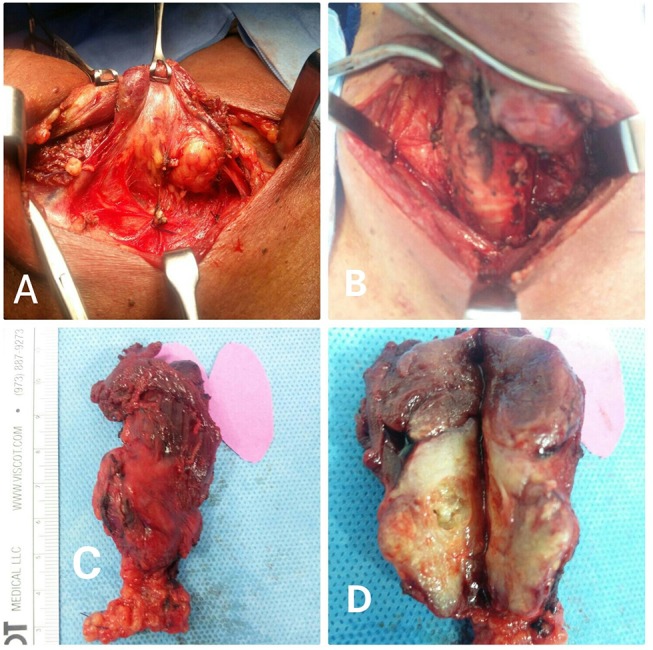
(A) Intraoperative image showing hard lesion in the right inferior parathyroid. (B) Surgical site after en bloc resection of the tumour. (C) Resected specimen image showing tumour along with right thyroid lobe. (D) Cut section of the specimen.
OUTCOME AND FOLLOW-UP
Histological examination of the specimen revealed local tissue invasion, vascular and capsular invasion, trabecular and fibrous stroma and frequent mitoses suggestive of parathyroid carcinoma. Resected margins were negative for tumour. Four of the eight resected lymph nodes were positive for metastatic deposits. Post surgery, the serum calcium values started falling and stabilised to 11.8 mg/dL (normal 9–11 mg/dL) and parathyroid hormone (PTH) levels to 1098 pg/mL (15–72 pg/mL). The calcium and PTH values did not fall to the normal range in spite of complete tumour excision from the neck. His renal function improved, and was weaned from the ventilator in 72 hours. Patient was started on cinacalcet 30 mg twice a day due to persistent elevation of PTH and calcium levels in spite of radical surgery most probably due to the functioning cerebral and pulmonary metastases. We did not perform biopsy of the lung and brain metastases due to logistical reasons. His postoperative voice was hoarse due to the right RLN involvement by the tumour which was sacrificed during en bloc resection of the tumour. Patient was discharged on cinacalcet on the 15th postoperative day and has completed 4 months follow-up with normalisation of calcium and elevated PTH levels (482 pg/mL)(normal 15–72 pg/mL).
DISCUSSION
Hypercalcaemic crisis is an uncommon but not a rare complication of PHPT. Patients usually have profound hypercalcaemia (serum≥14 mg/dL) with palpable neck mass along with rapid deterioration of the central nervous system function along with multiorgan failure and death.1 The incidence of hypercalcaemic crisis varies in the literature from 1.6% to 6%.2 Parathyroid carcinoma is a rare cause of PHPT (<1%) but may contribute up to 5% of hypercalcaemic crisis.3 Differentiating parathyroid carcinoma from benign causes of PHPT is not straightforward in the preoperative setting due to the similarity of clinical features. Few features may be indicative of parathyroid carcinoma such as very high PTH (mostly in thousands), palpable tumours, very high calcium values and sometimes with hypercalcaemic crisis. But the final diagnosis of parathyroid carcinoma rests on the demonstration of local invasion or metastases of these carcinomatous cells.
Anecdotal reports of very high calcium levels (more than 20 mg/dL) in parathyroid carcinoma have been reported by Spinelli et al 4 and Sheikh and Islam.5 Our case also was in accordance with the above two reports with a calcium value of 21.2 mg/dL. Very high calcium levels always expose our body to the risk of multiorgan decompensation, with the development of renal failure, cardiovascular dysfunction like tachyarrhythmias, cardiac arrest, central nervous system manifestations of irritability, psychiatric disturbance, somnolence and ultimately coma and death. Ziegler reported that very high calcium levels with renal and cardiac risk warrants emergency management in a highly specialised unit without any time delay which is of crucial importance.6 Hence, hypercalcaemic crisis should be detected at the earliest time possible and managed appropriately by a multidisciplinary team as early as possible for the reversal of hypercalcaemia before the feasibility of emergency parathyroidectomy.
Parathyroid carcinoma is a morphologically slow-growing tumour but variability exists in its biochemical diversity. Lethal complications of the latter due to mainly neurological and metabolic effects. rvival The survival rates reported in literature is to the tune of 85% at 5 years and 49% to 77% at 10 years.7 Intracranial metastases of parathyroid carcinoma are extremely rare and only few cases have been reported.
Management of hypercalcaemic crisis is of paramount importance and involves rapid intravascular volume expansion, diuretics to induce calciuresis. Pharmacotherapy with bisphosphonates, calcitonin, steroids and calcimimetics may be used based on the response. Acute lowering of calcium levels may be possible by haemodialysis. Continuous renal replacement therapy with citrate anticoagulation is being used sparingly in few centres. We stabilised our patient’s serum calcium with hydration, bisphosphonates, dialysis and calcimimetics before proceeding to emergency parathyroidectomy.
The most important element in the management of parathyroid carcinoma is the completeness of the tumour resection. Incomplete excisions of these rare tumours are associated with very high recurrence rates and persistence of hypercalcaemia. En bloc resection of parathyroid carcinoma including the thyroid lobe and adjacent structures offers the best possible strategy for possible cure and for achieving long-term survival.8
In case of solitary metastasis accessible for surgical removal, metastatectomy of the functioning metastases or surgical debulking may help in alleviating the metabolic overload and its consequences. Chemotherapy and radiotherapy have a very limited role in the palliative management, with residual or recurrent disease not amenable to surgical resection.9 In these residual, recurrent or metastatic parathyroid carcinomas, medical control of hypercalcaemia is the viable safe strategy. Calcimimetics play a major role in the above setting though they do not alter the course of the malignant disease. The advantage of calcimimetics in metastatic parathyroid carcinoma is its utility in patients with renal insufficiency which may occur concomitantly in advanced stages due to its long-standing tumourogenic and hypercalcaemic effects.10
Learning points.
Parathyroid carcinoma may present with aggressive hypercalcaemia, and very rarely with synchronous brain metastases early in the course of the disease.
En bloc resection of this rare malignancy offers the best possible treatment in controlling hypercalcaemia and its metabolic effects.
Parathyroid carcinoma must be considered in the differential diagnosis of acute severe hypercalcaemia when associated with a neck mass.
Footnotes
Contributors: DS and SM have contributed in the management of the case and overseeing the manuscript preparation. JF and KR were involved in the preparation of the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
REFERENCES
- 1. Lew JI, Solorzano CC, Irvin GL, et al. . Long-term results of parathyroidectomy for hypercalcemic crisis. Arch Surg 2006;141:696–9. 10.1001/archsurg.141.7.696 [DOI] [PubMed] [Google Scholar]
- 2. Sarfati E, Desportes L, Gossot D, et al. . Acute primary hyperparathyroidism: experience of 59 cases. Br J Surg 1989;76:979–81. 10.1002/bjs.1800760937 [DOI] [PubMed] [Google Scholar]
- 3. Gasparri G, Camandona M, Mullineris B, et al. . Acute hyperparathyroidism: our experience with 36 cases. Ann Ital Chir 2004;75:321–47. [PubMed] [Google Scholar]
- 4. Spinelli C, Berti P, Miccoli P, et al. . Parathyroid carcinoma. Surgical experience in three cases. Minerva Chirurgica 1994;49:1343–7. [PubMed] [Google Scholar]
- 5. Sheikh A, Islam N. Minimally symptomatic severe hypercalcaemia in a patient with parathyroid carcinoma. J Pak Med Assoc 2006;56:40–1. [PubMed] [Google Scholar]
- 6. Ziegler R. Hypercalcemic crisis. J Am Soc Nephrol 2001;12(Suppl 17):S3–9. [PubMed] [Google Scholar]
- 7. Hundahl SA, Fleming ID, Fremgen AM, et al. . Two hundred eighty-six cases of parathyroid carcinoma treated in the U.S. between 1985-1995: a National Cancer Data Base Report. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer 1999;86:538–44. [DOI] [PubMed] [Google Scholar]
- 8. Wei CH, Harari A. Parathyroid carcinoma: update and guidelines for management. Curr Treat Options Oncol 2012;13:11–23. 10.1007/s11864-011-0171-3 [DOI] [PubMed] [Google Scholar]
- 9. Koea JB, Shaw JH. Parathyroid cancer: biology and management. Surg Oncol 1999;8:155–65. 10.1016/S0960-7404(99)00037-7 [DOI] [PubMed] [Google Scholar]
- 10. Givi B, Shah JP. Parathyroid carcinoma. Clin Oncol 2010;22:498–507. 10.1016/j.clon.2010.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]


